Abstract
Background:
Attention-deficit/hyperactivity disorder (ADHD) is a common neurodevelopmental disorder with onset as early as preschool and impairment across the lifespan. Temperament factors, specifically those that theoretically map onto ADHD symptoms, may be early markers of risk for developing later childhood ADHD that could be identifiable in infancy or toddlerhood. This meta-analysis examined the associations between these early temperamental factors and later symptoms and diagnosis of ADHD and mapped early temperament constructs onto the three ADHD symptom dimensions.
Methods:
A systemic review of the literature was conducted to identify prospective longitudinal studies that included theoretically relevant temperament constructs (sustained attention, activity level, inhibition, and negative emotionality) examined from birth to 36 months old and ADHD (symptoms or diagnosis) in preschool or childhood. The association between each temperament construct and ADHD outcomes were examined using pooled standardized estimates in meta-analyses.
Results:
Forty-eight articles (n=112,716 infants/toddlers) prospectively examined temperament and the relation to childhood ADHD symptoms or diagnosis. Activity level (k =18) in infancy and toddlerhood was moderately associated with childhood ADHD (r = .39, CI= 0.27, 0.51, p < .001). Moderate effect sizes were also observed for sustained attention (k = 9; r = −.28, CI= −0.42, −0.12, p < .001) and negative emotionality (k =33; r = .25, CI= 0.16, 0.34, p < .001) with ADHD. The specificity of each temperament construct for later ADHD symptom dimensions was such that activity level and negative emotionality were predictive of all three symptom dimensions (i.e., inattention, hyperactivity/impulsivity, and combined), whereas sustained attention was only associated with combined symptoms.
Conclusions:
Infant and toddler temperament is an early risk factor for the development of childhood ADHD that could be utilized for early intervention identification. Yet, this systematic review found that relatively few prospective longitudinal studies have examined sustained attention (k = 9) and inhibition (k =15) in infancy and toddlerhood in relation to later ADHD highlighting the need for further research.
INTRODUCTION
Attention-deficit/hyperactivity disorder (ADHD) is the most common neurodevelopmental disorder with an estimated worldwide prevalence of 5% (Polanczyk, de Lima, Horta, Biederman, & Rohde, 2007). Children with ADHD are most often identified for evaluation and treatment at school age, after impairment in social and academic functioning has become apparent (Visser et al., 2014). Longitudinal studies of children treated for ADHD have found continued adverse outcomes in adulthood including lower educational achievement, greater occupational difficulties, interpersonal conflict, more frequent motor vehicle accidents and traffic violations, substance use problems, and suicide (Barkley, 2014; Chronis-Tuscano et al., 2010; Molina et al., 2009; Shaw et al., 2012). More recently, it has been suggested that individuals with childhood ADHD have a 9–13-year reduction in healthy life expectancy (Barkley, 2018; Schiavone et al., 2022). Given the significant negative long-term outcomes of ADHD, there is a growing interest in identifying early signals of risk for ADHD before the full onset of the disorder. These signals of risk could inform targets for early prevention and interventions to delay or prevent the onset of ADHD diagnosis, associated impairments, and the development of comorbidity.
The neurodevelopmental nature of ADHD, with onset as young as preschool-age, suggests that the disorder begins early in life and markers of risk for developing ADHD could be identifiable even in infancy or toddlerhood (Nigg, Sibley, Thapar, & Karalunas, 2020; Schmidt & Petermann, 2009). One potential early emerging marker of ADHD is temperament. Temperament is characterized as individual differences in behavior in response to the environment, that is relatively stable beginning at 4 months of age, and is driven by neurophysiological underpinnings (Carranza, González-Salinas, & Alto, 2013; Rothbart & Bates, 2006). Thus, temperament is one possible early marker of risk for later development of childhood ADHD (Nigg, Sibley, Thapar, & Karalunas, 2020). Nigg, Goldsmith, and Sachek (2004) have conceptualized a theoretical model with impaired regulation and reactivity as temperamental risk factors for developing ADHD.
Attention develops rapidly in infancy with the capacity for sustained attention (attending to a stimulus while ignoring distractors for an extended period) emerging by the second half of the first year of life (Hendry et al., 2018; Putnam, Gartstein, & Rothbart, 2006; Rothbart, 1981). Individual differences in attention during infancy and toddlerhood have been found to be moderately stable and are associated with later cognitive abilities suggesting a potential predictive value of early developing attention to later childhood outcomes of interest to ADHD (Bornstein & Sigman, 1986; Colombo, 1993; Sigman, Cohen, & Beckwith, 1997). Moreover, infants and toddlers at high familial risk for ADHD have been noted to have less sustained attention as early as 7 months of age as compared to infants and toddlers without a familial history of ADHD (Auerbach, Atzaba-Poria, Berger, & Landau, 2004; M. Miller et al., 2020). Thus, difficulty with sustained attention in the first two years of life may be an early signal of risk for developing childhood ADHD. Yet, only a few longitudinal studies have examined sustained attention or attention problems in infancy or toddlerhood as predictors of later symptoms of ADHD and with mixed results. For example, Papageorgiou and colleagues (2014) found that greater sustained attention, eye-tracking generated mean duration of fixation, at 7 months of age was associated with fewer ADHD symptoms at age 3.5 years, whereas Frick and colleagues (2019) reported that 10-month sustained attention, measured via behaviorally-coded attention during toy play, did not predict inattentive or hyperactive symptoms at age 3. These mixed findings may indicate that the measurement method of sustained attention is important, such that some measures of sustained attention may be more sensitive to differences than others.
Activity level as a temperament trait is the child’s natural tendency towards more or less motor activity. High activity levels are described as frequently moving arms and legs, squirming, kicking, or rolling in infancy (Gartstein & Rothbart, 2003) and being full of energy or exuberant in toddlerhood (Putnam et al., 2006). These behaviors emulate hyperactivity, a core symptom of ADHD. Thus, it is of no surprise that activity level has been examined as a possible early predictor of childhood ADHD. The meta-analysis by Kostyrka-Allchorne and colleagues (2020) found a small but significant correlation between parent reported infant activity level and later symptoms of ADHD. Age was a significant moderator such that activity level was more strongly associated with childhood ADHD when measured later in infancy (13–24 months). This moderation effect may be in part due to greater recognition of a child’s activity level by parents as mobility increases into the second year of life. It is possible that the predictive value of activity level could continue to increase into toddlerhood. Additionally, despite the increased cost relative to parent report measures, observational methods may be important in more precisely quantifying early motor activity. Interestingly, activity level assessed multiple times across the first two years of life was consistently significantly associated with hyperactivity/impulsivity, but not attention problems at age 7 (Shephard et al., 2019). Therefore, activity level in infancy and toddlerhood may have greater predictive power for hyperactivity/impulsivity symptoms than the inattentive symptoms of childhood ADHD.
Inhibition is often characterized as the ability to control, regulate, or inhibit approach and avoidance behaviors (Rothbart, 1989), sometimes referred or including effortful control. The temperamental construct of inhibition shares conceptual similarities to the construct of impulsivity underlying ADHD, along with self-regulation which is also examined via affective constructs such as negative emotionality (discussed below). Early emerging inhibitory control deficits have been associated with the development of ADHD (e.g., Gewirtz, Stanton-Chapman, & Reeve, 2009; Jacobson, Schneider, & Mahone, 2018), with most studies examining cross-sectional and longitudinal designs of school-age children through adolescence. The literature on infant and toddler inhibition and later ADHD outcomes is limited, with only a handful of studies examining early childhood inhibition measured using behavioral observations and parent-report as a predictor of later ADHD, resulting in mixed findings. For example, studies by Frick and colleagues did not identify a significant relation between early inhibition (measured starting at 10 and 12 months) and later ADHD (measured at 3 and 6 years) in typically developing samples (Frick, Bohlin, Hedqvist, & Brocki, 2019; Frick, Forslund, et al., 2019). On the other hand, several others have found early inhibition to be associated with later ADHD and related symptoms. In a sample of same-sex twins, Gagne and colleagues (2020) found that early inhibition was related to later ADHD, although much of the covariance was accounted for by genetic variance. Inhibition may have some specificity regarding the development of ADHD, as inhibition in infancy and toddlerhood has been shown to be predictive of ADHD symptoms, but not autism or anxiety symptoms (Shephard et al., 2019). Furthermore, early inhibition has been associated with later attention problems and as a mediator in the relation between preterm birth and later attention problems (Jaekel, Eryigit-Madzwamuse, & Wolke, 2016). However, there is limited research examining the specificity of early inhibition on attention vs hyperactive impulsive dimensions of ADHD.
Negative emotionality is a temperament profile often characterized by high rates of negative affect and reactivity such as anger, distress, or irritability (Rothbart & Bates, 2006). Infants with intensified negative emotionality are often described by parents as “difficult” and at times described and measured in the literature as difficult temperament. Predictively, higher levels of negative emotionality have been associated with poorer emotional and behavioral outcomes, and often considered a transdiagnostic risk factor for psychopathology, with several studies supporting the link between negative emotionality and ADHD. Infant and toddler negative emotionality has been associated with higher rates of ADHD diagnosis, hyperactivity, inattention, as well as increasing trajectories of symptoms (Galéra et al., 2011) through to age 10, with most studies focusing on outcomes in young children, 3–7-years-old (Becker, Holtmann, Laucht, & Schmidt, 2004; K. Lawson & H. Ruff, 2004; N. V. Miller, Hane, Degnan, Fox, & Chronis-Tuscano, 2019; Williams, Nicholson, Walker, & Berthelsen, 2016). However, some studies have not found a significant association between negative emotionality and ADHD, in predominately typically developing samples (Arnett, Macdonald, & Pennington, 2013; Elberling et al., 2014; Jorm et al., 2001). These mixed findings may highlight the overlap of negative emotionality as an underlying factor among multiple disorders, including ADHD, oppositional defiant disorder, and depression, as well as some normative variations throughout early childhood.
The current study is a systematic review and meta-analysis that aimed to clarify the mixed findings in the literature by examining the longitudinal association between temperament (sustained attention, activity level, inhibition, and negative emotionality) in infancy and toddlerhood (0–36 months) and later development of childhood ADHD symptoms and/or diagnosis (3–13 years). Additionally, this meta-analysis aimed to examine the association between these early temperament constructs and the specific ADHD symptom dimensions which could potentially help disentangle the heterogenous developmental trajectories of ADHD. A recent meta-analysis examined temperament (negative emotionality, self-regulation, behavioral inhibition, surgency, and activity) as reported by parents in infancy (0–24 months) as predictors of later psychopathology (Kostyrka-Allchorne, Wass, & Sonuga-Barke, 2020). They concluded that some temperament traits (i.e., negative emotionality) may confer transdiagnostic risk whereas others (e.g., activity level) may provide greater disorder specificity. Importantly, all associations were weak and concerns about shared method variance may arise, suggesting screening by parent report may have limited predictive power. Shephard and colleagues (2021) also conducted a systematic review and meta-analysis that aimed to identify all neurocognitive and behavioral measures examined between birth and five years of age among children at elevated risk for ADHD. However, this meta-analysis included studies of familial risk for ADHD as well as cross-sectional studies of children with ADHD, therefore limiting the interpretation of which of these markers measured in infancy and toddlerhood may be predictive of later development of ADHD. The current review builds upon this foundational work by (1) expanding the temperament traits measured to include sustained attention and inhibition given conceptual overlap with the inattention and hyperactivity/impulsivity, (2) extending the age of temperament assessment through toddlerhood, a period of development found to be important for maturation of self-regulation and early identification, (3) considering observational assessments of temperament, in addition to questionnaires, and (4) specifically focusing on prospective longitudinal designs to examine the predictive value of identifying early infant and toddler temperament on the development of ADHD or ADHD symptoms in childhood and adolescence.
This systematic review and meta-analysis focus on four temperament constructs that can be identified as early as 4 months that theoretically map onto ADHD symptom dimensions. We hypothesized that less sustained attention, more activity, poorer inhibition, and greater negative emotionality in the first 3 years of life would each predict later childhood ADHD symptoms and diagnosis. We tested the specificity of each temperament trait to (1) the three ADHD symptom dimensions (inattention, hyperactivity/impulsivity, and combined), and (2) ADHD symptoms vs. ADHD diagnosis. We expected sustained attention to be related with inattention, inhibition and activity level to be related with hyperactivity, and negative emotionality to be related with combined symptom dimensions. Regarding ADHD symptom vs. diagnosis, we hypothesized that all temperament constructs would be more strongly related to ADHD symptoms, given the increased variability of symptoms and limited range of diagnosis. Given the wide developmental age range of the ADHD outcome assessment, we examined age at ADHD outcome (i.e., preschool 3–5 vs school-age 6–13) as a moderator between the relation of each temperament construct and later ADHD. We expected stronger effects for preschool ADHD outcomes given the temporal proximity of assessment between infancy/toddlerhood and preschool. However, given that the temperament constructs were assessed within a narrow range (0–36 months), we did not examine age at which temperament was collected as a moderator. Finally, we conducted two exploratory moderator analyses (1) reporter of the ADHD outcome variable, and (2) percentage of the sample identified as male children.
METHODS
This systematic review and meta-analysis was preregistered with PROSPERO (CRD42020158739). Comprehensive literature searches were performed in the PubMed, EMBASE.com, and PsycINFO (Ovid) electronic databases on May 6, 2020, and were re-run on December 17, 2021. Search strings for each database were developed by a health sciences librarian (JF), using controlled vocabulary (Medical Subject Headings, Emtree terms, Thesaurus of Psychological Index Terms) and natural language words or phrases to reflect the concepts of “attention deficit and hyperactivity disorder,” “temperament,” and “infancy/toddlerhood.” The search strings are shown in the Supporting Information (Appendix S1). The search was limited to English language studies only, humans only, and the publication years from 1980 to 2021. The beginning of the literature search was set to 1980 reflecting the publication of the 3rd edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III; American Psychiatric Association, 1980) which described the initial diagnostic criteria for attention deficit disorder. A total of 16,839 citations were retrieved from the three databases (Figure 1, Moher, Liberati, Tetzlaff, & Altman, 2009). Citations were exported from each database into EndNote and duplicates were removed by the librarian (JF) using the Bramer Method (Bramer, Giustini, de Jonge, Holland, & Bekhuis, 2016). The remaining citations were then uploaded to DistillerSR (DistillerSR, Evidence Partners, Ottawa, Canada). All search procedures in the current study followed rigorous standards for conducting systematic reviews and meta-analyses (Polanin, Pigott, Espelage, & Grotpeter, 2019).
Figure 1.

PRISMA Flow Diagram
Prospective longitudinal studies and retrospective studies that included archival data collected during infancy or toddlerhood (e.g., medical records) were included. All studies that relied on retrospective recall of infant and toddler temperament were excluded. Prospective longitudinal studies were eligible for inclusion if temperament was examined from birth to 36 months old and ADHD outcome was reported in preschool, childhood, or adolescence. The ADHD outcomes included ADHD diagnosis or ADHD symptoms such as attention problems, hyperactivity, and impulsivity. The temperament and ADHD data could be determined by a clinician, observation, task or as rated by a parent, caregiver, or teacher informant. All abstracts were independently reviewed by two authors for eligibility criteria. All articles meeting inclusion after abstract reviewer were full text reviewed by two authors and selected for inclusion based on consensus. Any disagreements were discussed with a third author. References of included manuscripts were then reviewed for additional papers to consider.
Adequacy of report and risk of bias was assessed for all included studies using the STROBE checklist for cohort, case control and cross-sectional studies (Von Elm et al., 2007). Funnel plots were used to assess the risk of publication bias, see the Supporting Information (Figures S1–S4).
For the primary analyses, a single effect size was obtained from each study for each temperament construct, ensuring the assumption of independence of effect sizes across studies. The effect size measure chosen for our primary analyses was correlation, specifically between early temperament constructs and later ADHD symptoms or diagnoses, as most of the included studies reported such associations using the correlation metric. When studies reported differences in means (i.e., the difference in mean early temperament between low and high ADHD symptom or diagnosis groups), the standardized mean difference (Cohen’s d) was first computed using the pooled standard deviation. The standardized mean difference was then converted to the correlation metric using established methods (Borenstein, Hedges, Higgins, & Rothstein, 2021). For studies that reported odds ratios for the association between early temperament and later ADHD, the log odds ratio was computed and converted to a standardized mean difference, which was ultimately converted to a correlation (Borenstein, Hedges, Higgins, & Rothstein, 2021). Correlations were interpreted using Cohen’s d conventions r = .10 small, r = .25 medium, and r = .50 large. Once all effect sizes were converted to correlations, Fisher’s z-transformation was employed as a variance-stabilizing transformation when performing the meta-analyses and combining effects across studies (Silver & Dunlap, 1987), see the Supporting Information (Figures S5–S8).
Random effects (RE) meta-analysis models were constructed and fitted via restricted maximum likelihood (REML) to estimate the mean of the distribution of effect sizes on the Fisher’s z-scale (Hedges, 1983). Separate models were used to estimate the mean effect along with 95% confidence intervals (CIs) for each of the four temperament constructs. Results were back-transformed to the original correlation scale for ease of reporting and interpretation. Heterogeneity measures such as between-study variance (τ2) and the proportion of total variability attributable to between-study variability (I2) were calculated, and Cochran’s Q heterogeneity statistics were used to formally test for heterogeneity. To investigate factors that may explain high between-study heterogeneity, we performed subgroup analyses based on ADHD symptom dimension (inattentive, hyperactive, and combined symptoms), ADHD symptom versus diagnosis, categorized age (preschool versus school age), and rater of ADHD symptoms (parent versus observer), separately for each temperament construct. Meta-regression was also performed to determine whether continuous age and percentage of male children were moderators that account for a significant portion of between-study heterogeneity, separately for each temperament construct. To test for small study effects and potential publication bias, regression-based Egger tests were performed using a RE meta-analysis model fit via REML while accounting for between-study heterogeneity by controlling for potential moderators (ADHD symptom versus diagnosis, categorized age, reporter, ADHD symptom dimension, and percentage of male children). To provide publication bias-adjusted effect sizes, the trim-and-fill technique was employed using the linear (L0) estimator for the number of potentially missing studies. Bias-adjusted effect sizes are reported when the number of imputed studies was greater than zero. Outliers were defined as effect sizes whose Fisher’s z-transformed correlation was below the first quartile minus 1.5 times the interquartile range, or above the third quartile plus 1.5 times the interquartile range. All analyses were performed using Stata/SE 16.1 (StataCorp LLC, College Station, TX).
RESULTS
Sample
Forty-eight articles including 112,716 infant and toddler participants followed longitudinally to childhood (3–13 years old) were included in the meta-analyses. Of the 48 studies, 33 evaluated negative emotionality, 18 reported on activity level, 15 assessed inhibition, 9 examined sustained attention in relation to later developing ADHD symptoms or diagnosis. Twelve studies obtained data from participants on multiple temperament constructs. Study characteristics are reported in Table 1. Outlier analyses identified two studies as outliers (one negative emotionality and one inhibition) and removal of these outliers did not change the significance of any results. Compliance with the STROBE statement for adequate reporting of observational studies was 83% (range 58–97%) overall for the included studies.
Table 1.
Characteristics of included studies
| ID Author (Year) | N | Country | Temperament Construct | Temperament Assessment | ADHD Outcome Age | ADHD Assessment | ADHD Type | Rater |
|---|---|---|---|---|---|---|---|---|
| 1. Abulizi et al. (2017) | 1184 | France | AL, NE | EAS | 5.5 | SDQ | COM | P |
| 2. Arnett et al. (2013) | 1016 | US | NE | CITS | 8 | DBD | COM | P |
| 3. Becker et al. (2004) | 319 | Germany | NE | Interview, Behavioral Coding | 11 | MPI | COM | O |
| 4. Ben-Sasson et al. (2017) | 924 | US | AL, AT | ITSEA | 8 | CBCL | COM | P |
| 5. Bilgin et al. (2020) | 342 | Germany | NE | Clinical Interview | 6 | CBCL | IN | P |
| 6. Bunford et al. (2021) | 354 | US | NE | Behavioral Coding | 9,12 | K-SADS | IN/HYP/COM | P |
| 7. Davies et al. (2011) | 201 | US | NE | Behavioral Coding | 3 | CCQ | COM | O |
| 8. Desantis et al. (2004) | 28 | US | NE | Daily Diary | 5.5 | CBCL | IN | P |
| 9. Einziger et al. (2018) | 64 | Israel | AL, IN, NE | CBQ | 13.5 | CPRS | IN/HYP/COM | P |
| 10. Elberling et al. (2014) | 1585 | Denmark | AL, NE | Behavioral Coding | 6 | DAWBA | COM | O |
| 11. Flouri et al. (2016) | 8302 | UK | NE | CITS | 3 | SDQ | COM | P |
| 12. Frick et al. (2019) | 47 | Sweden | AL, IN | CCTI, Behavioral Coding | 6 | ADHD RS | IN | T |
| 13. Frick et al. (2019) | 112 | Sweden | IN, AT, NE | Behavioral Coding, IBQ | 3 | ADHD RS | IN | P/T |
| 14. Gagne et al. (2020) | 628 | US | IN | Behavioral Coding | 3 | CBCL | COM | P |
| 15. Galéra et al. (2011) | 2057 | Canada | NE | ICQ | 8 | ECBS | COM | P |
| 16. Goldsmith et al. (2006) | 429 | US | AL, IN, AT, NE | TBAQ | 7 | DISC | COM | P |
| 17. Goodwin et al. (2021) | 113 | UK | AL | IBQ, Behavioral Coding | 3 | CBCL | COM | P |
| 18. Gurevitz et al. (2014) | 116 | Israel | NE | Behavioral Coding | 8 | Chart Review | COM | O |
| 19. Jaekel et al. (2016) | 558 | Germany | IN | Behavioral Coding | 8 | CBCL | IN | P |
| 20. Johnson et al. (2014) | 136 | UK | AL | Motion Tracking | 7 | DAWBA | COM | O |
| 21. Jorm et al. (2001) | 660 | Australia | NE | STSI | 12 | RPBQ | HYP | P |
| 22. Joseph et al. (2021) | 312 | US | NE | Behavioral Coding | 6 | CBCL | IN | P |
| 23. Lawson et al. (2004) | 55 | US | AT | Behavioral Coding | 5 | CPRS, CBCL | COM | P |
| 24. Lawson et al. (2004) | 75 | US | NE | Behavioral Coding | 3.5 | CPRS | HYP | P |
| 25. Leblanc et al. (2008) | 1112 | Canada | AL, IN | SBQ | 5 | SBQ | HYP | P |
| 26. Lemcke et al. (2016) | 76286 | Denmark | AL, NE | Parent Interview | 11 | Chart Review | COM | O |
| 27. Levine et al. (2018) | 156 | New Zealand | IN | Behavioral Coding | 4.5 | SDQ | COM | P |
| 28. Meeuwsen et al. (2018) | 312 | UK | AL, IN, AT, NE | IBQ, Behavioral Coding | 7 | PAPA | COM | O |
| 29. Miller et al. (2018) | 47 | US | NE | Clinical Interview | 10 | CASI | COM | P/O |
| 30. Miller et al. (2019) | 291 | US | AL, NE | Behavioral Coding | 7.5 | SNAP-IV | IN | P |
| 31. Miller et al. (2019) | 291 | US | NE | Behavioral Coding | 7 | SNAP-IV | IN | P/T |
| 32. Miller et al. (2020) | 145 | US | AL, IN, AT, NE | Behavioral Coding | 3 | ADHD RS | COM | P |
| 33. Morrell et al. (2003) | 59 | UK | NE | Behavioral Coding | 8 | RPBQ | HYP | P |
| 34. Olson et al. (2002) | 89 | US | NE | ICQ | 8 | Behavioral Coding | HYP | O |
| 35. Papageorgiou et al. (2014) | 120 | London | IN | ECBQ | 3.5 | SDQ | COM | P |
| 36. Rende et al. (1993a)* | 91 | US | NE, AL | CCTI | 7 | CBCL | IN | P |
| 37. Rende et al. (1993b)* | 73 | US | NE, AL | CCTI | 7 | CBCL | IN | P |
| 38. Robson et al. (1997) | 85 | Canada | AT | CITS | 5.5 | Behavioral Coding | IN | O |
| 39. Sanson et al. (1992) | 252 | Australia | AL, NE | ITQ | 6 | CBQ | HYP | P |
| 40. Schmid et al. (2014) | 1120 | Germany | NE | Clinical Interview | 8.5 | MPI | COM | O |
| 41. Shephard et al. (2019) | 104 | Britain | AL, IN, AT | IBQ, ECBQ | 7 | CPRS | IN/HYP | P |
| 42. Silberg et al. (2015) | 624 | US | NE | ICQ | 3 | DISC-YC | COM | O |
| 43. Silverman et al. (1992) | 69 | US | AL, IN | EAS | 4 | YCI | COM | P |
| 44. Slinning (2004) | 92 | Norway | AT | CBCL | 4.5 | ADHD RS | COM | P/T |
| 45. Smarius et al. (2017) | 3389 | Netherlands | NE | WQ | 5 | SDQ | COM | P |
| 46. Stephens et al. (2021) | 229 | US | IN | FYI | 4.5 | ADHD RS | IN/HYP/COM | P |
| 47. Williams et al. (2016) | 2880 | Australia | NE | ATS | 6 | SDQ | HYP | T |
| 48. Williams et al. (2016) | 4109 | Australia | NE | ATS | 7 | SDQ | IN | P |
| 49. Willoughby et al. (2017) | 1074 | US | AL, IN, AT, NE | Behavioral Coding | 6 | DBD | COM | P |
Notes Activity Level (AL), Inhibition (IN), Attention (AT), Negative Emotionality (NE), Carey Infant Temperament Scale (CITS), Emotionality Activity and Sociability (EAS), Infant Toddler Social and Emotional Assessment (ITSEA), Colorado Childhood Temperament Inventory (CCTI), Infant Behavior Questionnaire (IBQ), Infant Characteristics Questionnaire (ICQ), Short Temperament Scale for Infants (STSI), Social Behavior Questionnaire (SBQ), Early Childhood Behavior Questionnaire (ECBQ), Child Behavior Checklist (CBCL), Wessel’s Questionnaire (WQ), Australian Temperament Scale (ATS), Disruptive Behavior Disorder Rating Scale (DBD), Strengths and Difficulties Questionnaire (SDQ), Mannheim Parent Interview (MPI), California Child Q-Set (CCQ), Developmental and Well-Being Assessment (DAWBA), ADHD Rating Scale (ADHD RS), Early childhood behavior scale from the Canadian National Longitudinal Study of Children and Youth (ECBS), Rutter Problem Behavior Questionnaire (RPBQ), Conner’s parent rating scale (CPRS); Preschool Age Psychiatric Assessment (PAPA), Child and Adolescent Symptom Inventory (CASI), Swanson, Nolan, and Pelham-IV (SNAP-IV), Young Diagnostic Interview Schedule for Preschool Children (DISC-YC), Hyperactivity Symptoms (Hyp), Combined ADHD Symptoms (COM), (CBQ) Children’s Behavior Questionnaire, (ITQ) Infant Temperament Questionnaire, (YCI) Yale Children’s Inventory, (FYI) First Year Inventory
This manuscript reported separate correlations by child sex
Primary Analyses
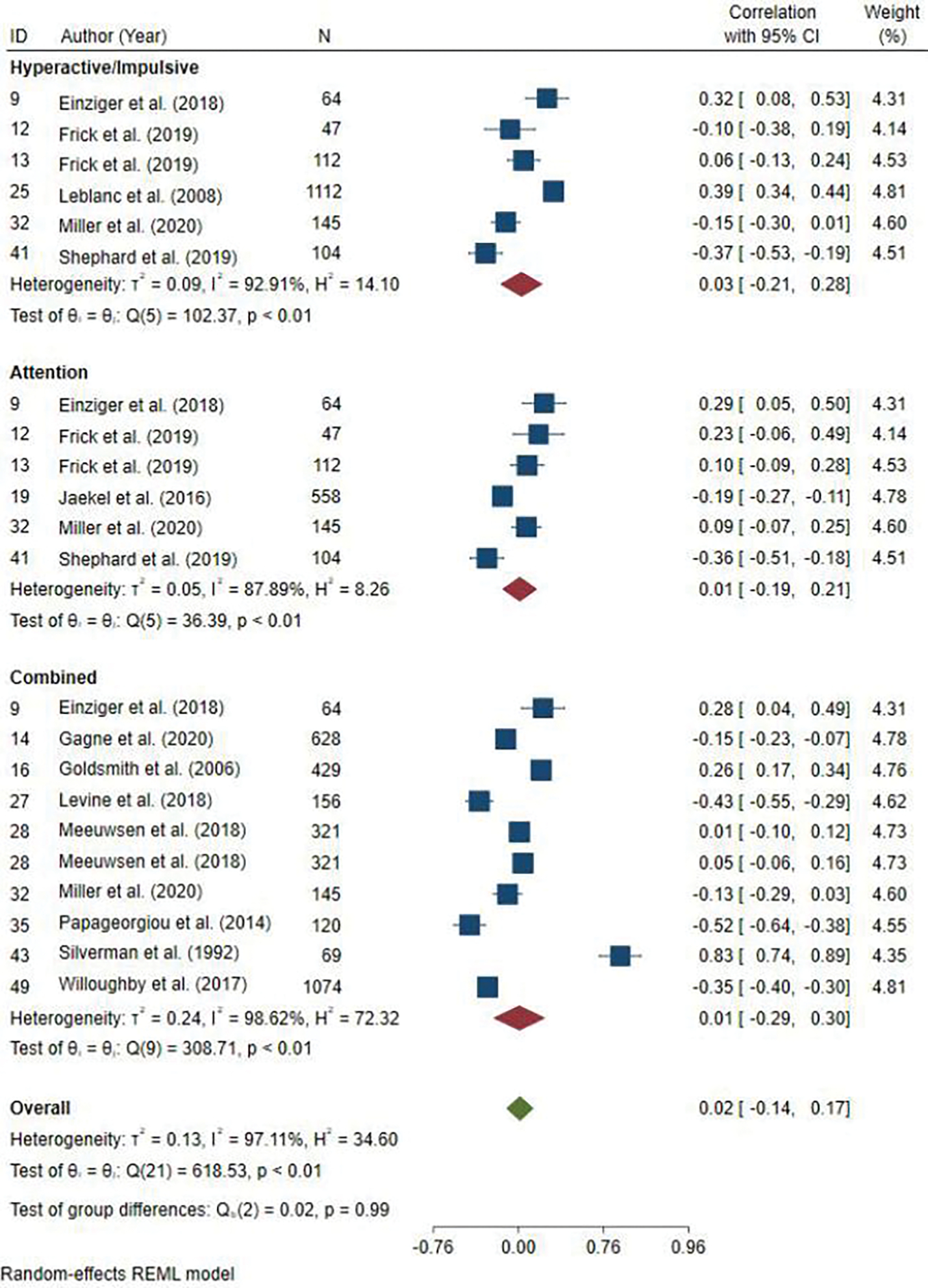
Table 2 presents the effect sizes for the associations between each temperament and later ADHD (symptoms and/or diagnosis) as well as the tests of heterogeneity. Sustained attention, activity level and negative emotionality were significantly associated with later ADHD (Figures 2–4). The effect size was moderate for activity level, r = .393, CI [0.268, 0.505], sustained attention, r = −.277, CI [−0.420, −0.120], and negative emotionality, r = .251, CI [0.156, 0.342]. The relation between inhibition and ADHD was not significant, r = .032, CI [−0.200, 0.260] (Figure 5). There was significant heterogeneity for all temperament constructs based on Cochran’s Q with 92–99% of the variation across studies due to heterogeneity (Table 2). Egger tests revealed insufficient evidence to conclude significant small-study effects for all four temperament constructs (p-values between 0.127–0.737). The trim-and-fill technique detected no missing studies for sustained attention and activity level; however, two missing studies were identified and imputed for both negative emotionality and inhibition. Bias-adjusted effect sizes for negative emotionality and inhibition were radj = 0.278, CI [0.182, 0.367], and radj = 0.123, CI [−0.114, 0.348], respectively (Table 2). Thus, adjustment for publication bias produced negligible or nonexistent changes in effect sizes for all four temperaments.
Table 2.
Meta-analyses results of overall association between infant/toddler temperament and childhood ADHD symptoms and/or diagnosis.
| Temperament | K | N | r | 95% CI | r adj | 95% CIadj | Q | I2 (%) |
|---|---|---|---|---|---|---|---|---|
| Sustained Attention | 9 | 2,267 | −.28* | −0.42, −0.12 | -- | --- | 87.87* | 92.13 |
| Activity Level | 18 | 88,306 | .39* | 0.27, 0.51 | -- | --- | 1283.56* | 99.12 |
| Inhibition | 14 | 4,939 | .03 | −0.20, 0.26 | .12 | −0.11, 0.35 | 585.22* | 98.41 |
| Negative Emotionality | 33 | 114,817 | .25* | 0.16, 0.34 | .28* | 0.18, 0.37 | 1729.07* | 99.37 |
Note:
p < 0.001; All studies in Table 1 were included in these meta-analyses; radj is the bias-adjusted effect size
Figure 2:

Forest plot of effect sizes of the association between sustained attention and later ADHD symptoms/diagnosis.
Figure 4:
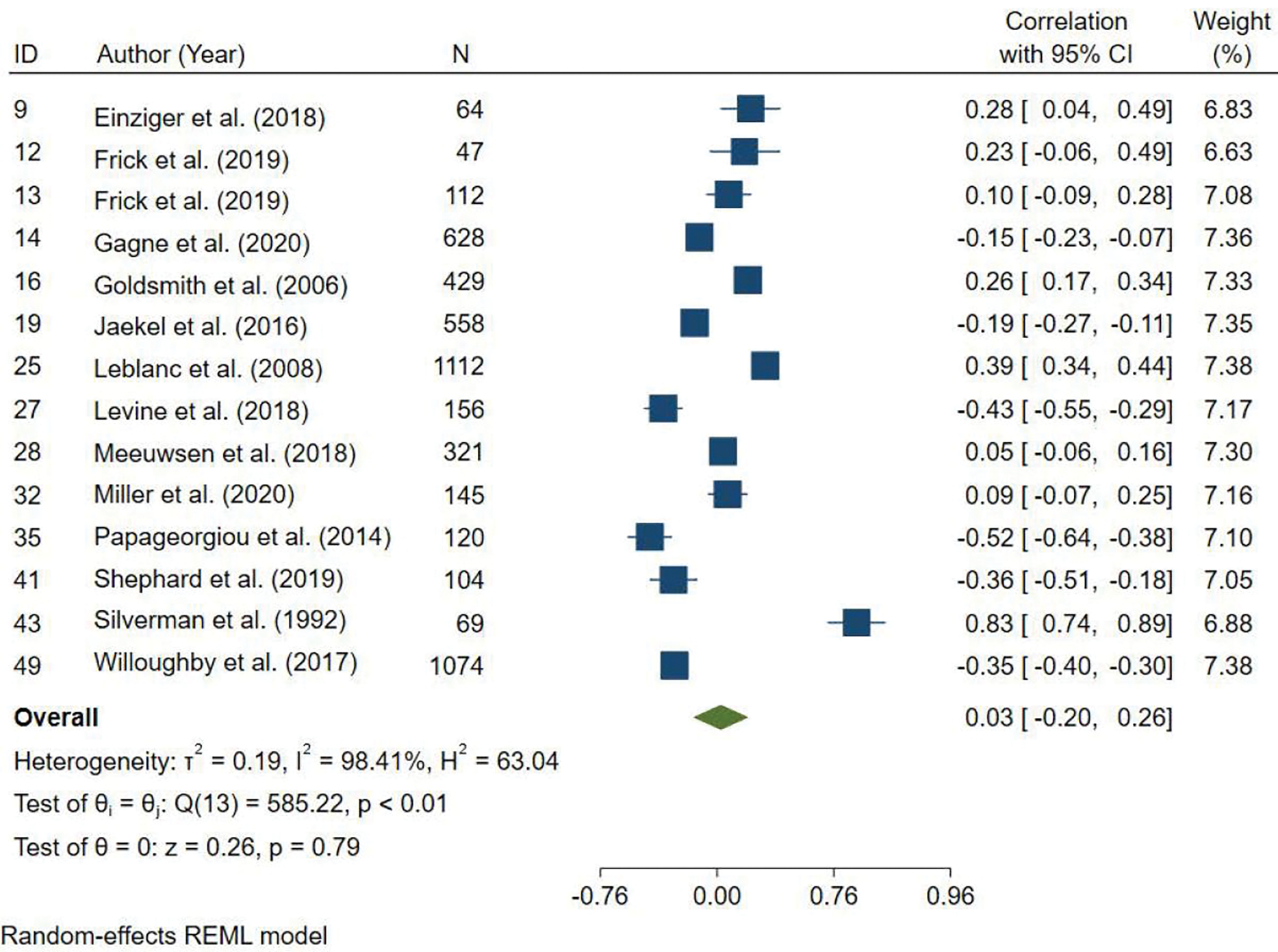
Forest plot of effect sizes of the association between inhibitory control and later ADHD symptoms/diagnosis.
Figure 5:

Forest plot of effect sizes of the association between negative emotionality and later ADHD symptoms/diagnosis.
Moderator Analyses
ADHD Symptom Dimensions.
The analyses for symptom dimension included symptom level data and did not examine differences between diagnostic level specifier data as that was not available for most studies. The association between sustained attention in infancy and toddlerhood and later ADHD was only significant for the combined symptoms, r = −.265, CI [−0.371, −0.153] and not for the hyperactive, CI [−0.143, 0.133], or inattentive, CI [−0.546, 0.130], symptom dimensions (Figure 6). The association between activity level and later ADHD was significant for the hyperactive symptom dimension, r = .390, CI [0.188, 0.561], inattention symptom dimension, r = .332, CI [0.133, 0.505], and combined symptom dimension, r = .381, CI [0.209, 0.531] (Figure 7). The association between inhibition and later ADHD was not significant for any of the three ADHD symptom dimensions: hyperactive symptoms, r = .033, CI [−0.214, 0.276], inattentive symptoms, r = .012, CI [−0.190, 0.213], and combined symptoms, r = .007, CI [−0.291, 0.303], Figure 8. The association between negative emotionality and later ADHD was significant for all three symptom dimensions: hyperactive symptoms, r = .257, CI [0.105, 0.396], inattentive symptoms, r = .321, CI [0.141, 0.480], and combined symptoms, r = .256, CI [0.135, 0.369], Figure 9.
Figure 6:

Forest plot of effect sizes for activity level associations with symptoms vs. diagnosis of ADHD.
Figure 7:

Forest plot of effect sizes for negative emotionality associations with symptoms vs. diagnosis of ADHD.
Figure 8:

Forest plot of effect sizes for sustained attention associations by ADHD symptom dimensions.
Figure 9:

Forest plot of effect sizes for activity level associations by ADHD symptom dimensions.
ADHD Symptom vs. Diagnosis.
In comparing ADHD symptoms vs. ADHD diagnoses, activity level and negative emotionality remained significantly positively associated with both ADHD symptoms and diagnosis, see Figures 10–11. The strength of the relation for activity level and negative emotionality did not differ for later diagnosis compared to symptoms of ADHD. The effect size was moderate to large for the association between activity level with later symptoms of ADHD, r = .388, CI [0.246, 0.514] and later ADHD diagnosis, r = .418, CI [0.102, 0.658]. The effects were small to moderate for both the relations between negative emotionality with ADHD symptoms, r = .255, CI [0.145, 0.358] and diagnosis, r = .237, CI [0.029, 0.426]. No studies measuring sustained attention or inhibition in infancy and toddlerhood included ADHD diagnosis as an outcome so this could not be examined.
Figure 10:
Forest plot of effect sizes for inhibitory control associations by ADHD symptom dimensions.
Figure 11:

Forest plot of effect sizes for negative emotionality associations by ADHD symptom dimensions.
Age of Outcome.
The associations between sustained attention and later ADHD symptoms or diagnosis were significant when examining outcomes in preschool, r = −.282, CI [−0.518, −0.007], and childhood/adolescence, r = −.277, CI [−0.441, −0.094]. Activity level also remained significantly associated with later ADHD outcomes at both preschool-aged, r = .293, CI [0.070, 0.489], and childhood/adolescence, r = 0.426, CI [0.277, 0.555]. The association between inhibition and both the preschool-aged and childhood/adolescence ADHD outcomes were not significant, r = .084, CI [−0.338, 0.477] and r = −0.025, CI [−0.237, 0.189], respectively. The association with negative emotionality was significant for both preschool-aged ADHD outcomes, r = .184, CI [0.120, 0.246], and ADHD outcomes in childhood/adolescence, r = .274, CI [0.146, 0.393]. Age as a continuous variable was not a significant moderator of the associations between any of the temperament constructs and later ADHD, see the Supporting Information (Figures S9–S12).
Reporter of ADHD Outcome.
The associations between infant/toddler temperament and observer vs. parent reported childhood ADHD symptoms or diagnosis were examined, see the Supporting Information (Figures S13–S14). Sustained attention in infancy/toddlerhood was significantly associated with parent report of ADHD symptoms, r = −0.234, CI [−0.369, −0.090]. Activity level in infancy/toddlerhood continued to be moderately associated with childhood ADHD symptoms and/or diagnoses when determined by observation and parent report, r = 0.354, CI [0.083, 0.576] and r = 0.406, CI [0.250, 0.542], respectively. The strength of the association between negative emotionality in infancy/toddlerhood and childhood ADHD symptoms and/or diagnosis varied by reporter such that the association was small when ADHD outcome was determined by an observer, r = 0.168, CI [0.025, 0.304], and moderate when reported by parent, r = 0.293, CI [0.174, 0.404]. Infant and toddler inhibition was not significantly associated with parent report of childhood ADHD symptoms, CI [−0.252, 0.280]. Too few studies of sustained attention (2 studies) and inhibition (1 study) included observer report to conduct meta-analyses.
Child Sex.
The percent of the sample identified as male children was not a significant moderator of the associations between any of the temperament constructs and later ADHD.
DISCUSSION
Identifying early temperamental precursors to ADHD could help connect children to early intervention services with the potential of improving the developmental trajectory of symptoms and impairment associated with ADHD and comorbid conditions. Given the potential benefits of early identification of risk factors for ADHD, the goal of the current study was to systematically examine the extent to which four theoretically derived temperament constructs identified in infancy and toddlerhood were associated with later ADHD. Focusing on prospective longitudinal designs to examine the developmental unfolding of ADHD, our systematic review revealed that several studies have demonstrated a link between early temperament and later ADHD, with negative emotionality being the most common temperament construct examined (k = 33) in the literature and few studies examining early attention (k = 9). The meta-analyses found a moderate effect size for the relation between activity level, sustained attention, and negative emotionality in infancy and toddlerhood and ADHD in childhood and adolescence. There was no significant effect for inhibition in infancy and toddlerhood on ADHD in childhood and adolescence.
Given the developmental trajectory of ADHD, with younger children displaying more hyperactive symptoms and older children displaying inattentive and/or combined symptoms, we examined the association between infant and toddler temperament constructs and ADHD symptom dimensions in childhood and adolescence, as well as differences between ADHD symptoms versus diagnosis. Infant and toddler activity level predicted all symptom dimensions of ADHD (i.e., hyperactivity, inattention, combined). This finding aligns with the potential overlap or early presentation of hyperactive symptoms in early childhood. Additionally, activity level had moderate to large effect sizes for diagnosis and symptom level outcome of ADHD. These findings may suggest that activity level can be identified early, as it is probably more noticeable in young children and supports the idea of stability of hyperactivity beginning in infancy and toddlerhood.
Negative emotionality predicted hyperactivity, inattentive, and combined symptom dimensions. The small to moderate effect sizes of negative emotionality and effect on all symptom dimensions could suggest the possibility of negative emotionality as a predictor of other co-occurring disorders (e.g., anxiety, ODD; Kostyrka-Allchorne, Wass, & Sonuga-Barke, 2020; Vogel et al., 2019). High rates of negative emotionality have been demonstrated in children with ADHD but can overlap with constructs such as irritability or difficulties with emotion regulation which are often characterized as transdiagnostic factors of psychopathology. Additionally, there was a small to moderate effect of negative emotionality and both ADHD diagnosis and symptom level outcomes, suggesting that although it may help identify early risk for ADHD, it may also predict other common co-occurring disorders.
Sustained attention in infancy and toddlerhood only predicted later combined symptom dimension of ADHD (k = 7). It may be that the combined symptoms dimension captures more of the variability in ADHD symptoms and account for the heterogenous nature of ADHD. It is also possible that there may not have been enough power to detect significant associations with inattentive (k = 4) or hyperactive/impulsive symptoms (k = 3) individually given that only a few studies examined these symptom dimensions. Sustained attention, as suggested by Barkley (Barkley, 1997), is at the core of ADHD, impacting one’s ability to maintain focus and ignore distractions. However, in our extensive review of literature, there was still a limited number of studies examining either sustained attention in infancy and toddlerhood as a predictor of ADHD. Additionally, none of the studies measuring sustained attention in infancy and toddlerhood examined ADHD diagnosis as an outcome and were all with community samples, suggesting a large gap in the literature and promising avenues for future research. Lastly, inhibition was not significantly associated with ADHD, including all sub-analyses examining child age at the ADHD outcome measurement. Given the limited number of studies examining inhibition and varied measurement methods (e.g., different coding of behavioral tasks), it is possible that inhibition is a risk factor for ADHD that requires further investigation.
Moderation analyses revealed similar associations when comparing preschool age outcomes to the school age outcomes. Specifically, small to moderate effects were found for negative emotionality across both age groups, Additionally, a moderate effect was found for activity level and preschool age outcomes and moderate to large effect was found for childhood and adolescent age outcomes. Given the developmental trajectory of ADHD symptom dimensions and reliability of identifying children in preschool for ADHD, significant predictors in infancy and toddlerhood of preschool and childhood ADHD would provide a unique opportunity to intervene early to prevent reduce the significant cascade of negative familial, social, and academic outcomes of children with ADHD.
In line with previous work, including recent reviews (Kostyrka-Allchorne et al., 2020; Shephard et al., 2021), the current systematic review and meta-analysis found significant associations between infant and toddler temperament constructs and child and adolescent ADHD. Specifically, the findings support associations between infant and toddler negative emotionality and child/adolescent activity level. Furthermore, the current study extends our understanding of infant and toddler temperament constructs by specifically focusing on prospective longitudinal designs to highlight the developmental trajectory beyond concurrent associations or cross-sectional designs. Additionally, the examination and findings associating infant and toddler sustained attention and inhibition with child and adolescent ADHD symptoms emphasizes other unique temperament profiles that can help increase early identification of ADHD. Lastly, the current study contributes to our knowledge on the specificity of these early risk markers to identify the unique and well-known heterogenous profiles of ADHD by examining the unique relations between the infant and toddler temperament constructs and the inattentive and hyperactive/impulsive symptom dimensions of ADHD.
Despite the strengths of the current study, we also acknowledge its limitations, which highly overlap with systematic reviews and meta-analytic designs. First, the findings may have limited generalizability given that most studies included either did not specify race/ethnicity and/or socioeconomic status (SES), and those that did largely relied on predominantly well-educated, mid- high SES samples. Future work should include more representative samples to encompass diversity in participant race/ethnicity, SES, and education. Additionally, measurement of constructs varied significantly ranging from observation to different reporters which makes it difficult to ascertain consistency between studies. We attempted to examine measurement based on reporter and found no moderation effects. However, infant negative emotionality demonstrated a small effect size for observed outcomes and a small-moderate effect size for parent report outcomes. Too few studies examined teacher reported outcomes of ADHD to be included in the moderator analyses. Second, unlike the recently published systematic review (Kostyrka-Allchorne et al., 2020; Shephard et al., 2021) who found limited variation due to heterogeneity, our findings suggest significant variation due to heterogeneity between studies. These findings highlighting the need for development of more refined measures of temperament and behavior. Third, although we aimed to examine more specificity regarding temperament constructs and ADHD, we did not examine individual level data and therefore may not capture the heterogeneity of the samples included in each study. Although it would be a taxing and challenging task, a meta-analysis with individual level data could strengthen the current findings and emphasize the associations between the early temperament constructs and ADHD symptom dimensions. Consequently, given the focus on ADHD, we were unable to examine the heterogeneity of the infant and toddler temperament constructs beyond ADHD (e.g., ODD, depression, anxiety). Fourth, several studies have been published since the last date of search and are therefore not included in the current study. Lastly, there are several factors that may have moderated the associations that we were unable to examine given that there were either not enough studies that examined each factor (e.g., measurement method, parental psychopathology) or they were measured differently (e.g., parenting). Future research should consider examining factors such as parental psychopathology which can influence the heritability of ADHD, as well as parenting that may impact the developmental unfolding of ADHD symptoms.
There are several clinical implications of the current findings. Specifically, findings support temperament constructs (i.e., sustained attention, activity level, inhibition, negative emotionality) that can be identified early in infancy and toddlerhood as risk factors for ADHD. Early identification of these temperament constructs can help to identify at high risk for ADHD prior to the development of more serious behaviors, potentially leading to early interventions to help reduce the known long-term negative outcomes associated with ADHD. The findings suggest that activity level may be the most prominent or at least most easily identifiable and specific risk factor in infancy and toddlerhood, although further research is needed to examine attention and inhibition. It is important to note that given the significant heterogeneity, that future research is needed and that the associations imply risk, not causality.
Although we do not yet have normative temperament scores, information on infant/toddler temperament can aid in identifying those who could benefit from further assessment and monitoring. Based on these findings, families could be informed on how to monitor the temperament and providers could support parents with positive parenting skills (praise, positive reinforcement) as an early prevention method. Tracking and monitoring behavior is a great first step for families who may eventually need further behavioral and mental health supports for themselves and their child. Furthermore, several parenting interventions have demonstrated support for changing early toddler behavior including Incredible Years and Parent Child Interaction Therapy (PCIT), as well as research support for intervention strategies targeting self-regulation in preschool (see Graziano & Hart, 2016).
In conclusion, the current study provides additional and extended support for utilizing infant and toddler temperament as an early risk factor for the development of ADHD which provides an avenue for early identification. Furthermore, our systematic review highlights the need for further research on several temperamental constructs and the need to examine longer-term outcomes into adolescence and adulthood. Given the neurodevelopmental nature, stability, and associated negative long-term outcomes associated with ADHD, it is imperative to understand early individual differences that can be easily identified and reliably assessed.
Supplementary Material
Figure 3:

Forest plot of effect sizes of the association between activity level and later ADHD symptoms/diagnosis.
Key points.
ADHD is a prominent neurodevelopmental disorder with onset as early as preschool. Certain types of temperament in infancy and toddlers are associated with subsequent ADHD.
The current systematic review and meta-analysis included 48 prospective longitudinal studies included temperament in infancy and toddlerhood as a predictor of later ADHD, suggesting high interest in early predictors of ADHD.
Activity level measured in infancy and toddlerhood had a moderate effect size on later ADHD symptoms and diagnosis. Fewer studies examined inhibition and sustained attention in infancy and toddlerhood as predictors of childhood ADHD.
Given the cascade of negative outcomes for children with ADHD, early identification and monitoring of child temperament may provide a valuable early indicator for early intervention and prevention.
Footnotes
Conflict of interest statement: No conflicts declared.
Supporting information
Additional supporting information may be found online in the Supporting Information section at the end of the article:
Appendix S1. SEARCH TERMS.
References
*Denotes references included in meta-analyses
- *Abulizi X., Pryor L., Michel G., Melchior M., Van Der Waerden J., & Group EMCCS. (2017). Temperament in infancy and behavioral and emotional problems at age 5.5: The EDEN mother-child cohort. PloS One, 12(2), e0171971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (APA). (1980). Diagnostic and statistical manual of mental disorders (3rd ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- *Arnett AB., Macdonald B., & Pennington BF. (2013). Cognitive and behavioral indicators of ADHD symptoms prior to school age. Journal of Child Psychology and Psychiatry and Allied Disciplines, 54(12), 1284–1294. doi: 10.1111/jcpp.12104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach JG, Atzaba-Poria N, Berger A, & Landau R (2004). Emerging developmental pathways to ADHD: Possible path markers in early infancy. Neural Plasticity, 11(1–2), 29–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkley RA (1997). Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychological Bulletin, 121(1), 65. [DOI] [PubMed] [Google Scholar]
- Barkley RA (2014). Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment: Guilford Publications. [Google Scholar]
- Barkley RA (2018). ADHD Likely Reduces Estimated Life Expectancy by Young Adulthood1. In. [Google Scholar]
- *Becker K., Holtmann M., Laucht M., & Schmidt M. (2004). Are regulatory problems in infancy precursors of later hyperkinetic symptoms? Acta Paediatrica, 93(11), 1463–1469. [DOI] [PubMed] [Google Scholar]
- *Ben-Sasson A., Soto TW., Heberle AE., Carter AS., & Briggs-Gowan MJ. (2017). Early and concurrent features of ADHD and sensory over-responsivity symptom clusters. Journal of Attention Disorders, 21(10), 835–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Bilgin A., Baumann N., Jaekel J., Breeman LD., Bartmann P., Bäuml JG., . . . Wolke D. (2020). Early crying, sleeping, and feeding problems and trajectories of attention problems from childhood to adulthood. Child Development, 91(1), e77–e91. [DOI] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgins JP, & Rothstein HR (2021). Introduction to meta-analysis: John Wiley & Sons. [Google Scholar]
- Bornstein MH, & Sigman MD (1986). Continuity in mental development from infancy. Child Development, 251–274. [DOI] [PubMed] [Google Scholar]
- Bramer WM, Giustini D, de Jonge GB, Holland L, & Bekhuis T (2016). De-duplication of database search results for systematic reviews in EndNote. Journal of the Medical Library Association: JMLA, 104(3), 240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Bunford N., Kujawa A., Dyson M., Olino T., & Klein DN. (2021). Examination of developmental pathways from preschool temperament to early adolescent ADHD symptoms through initial responsiveness to reward. Development and Psychopathology, 1–13. [DOI] [PubMed] [Google Scholar]
- Carranza JA, González-Salinas C, & Ato E (2013). A longitudinal study of temperament continuity through IBQ, TBAQ and CBQ. Infant Behavior and Development, 36(4), 749–761. [DOI] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Molina BS, Pelham WE, Applegate B, Dahlke A, Overmyer M, & Lahey BB (2010). Very early predictors of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Archives of General Psychiatry, 67(10), 1044–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colombo J (1993) Infant Cognition: Predicting Later Intellectual Functioning. Sage Publications, London, UK. [Google Scholar]
- *Davies PT., Sturge-Apple ML., & Cicchetti D. (2011). Interparental aggression and children’s adrenocortical reactivity: Testing an evolutionary model of allostatic load. Development and Psychopathology, 23(3), 801–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *DeSantis A., Coster W., Bigsby R., & Lester B. (2004). Colic and fussing in infancy, and sensory processing at 3 to 8 years of age. Infant Mental Health Journal: Official Publication of The World Association for Infant Mental Health, 25(6), 522–539. [Google Scholar]
- * Einziger T., Levi L., Zilberman-Hayun Y., Auerbach JG., Atzaba-Poria N., Arbelle S., & Berger A. (2018). Predicting ADHD symptoms in adolescence from early childhood temperament traits. Journal of abnormal child psychology, 46(2), 265–276. [DOI] [PubMed] [Google Scholar]
- *Elberling H., Linneberg A., Olsen EM., Houmann T., Rask CU., Goodman R., & Skovgaard AM. (2014). Infancy predictors of hyperkinetic and pervasive developmental disorders at ages 5–7 years: results from the Copenhagen Child Cohort CCC 2000. Journal of Child Psychology and Psychiatry, 55(12), 1328–1335. [DOI] [PubMed] [Google Scholar]
- *Flouri E., Midouhas E., & Narayanan MK. (2016). The relationship between father involvement and child problem behaviour in intact families: A 7-year cross-lagged study. Journal of Abnormal Child Psychology, 44(5), 1011–1021. [DOI] [PubMed] [Google Scholar]
- *Frick MA., Bohlin G., Hedqvist M., & Brocki KC. (2019). Temperament and cognitive regulation during the first 3 years of life as predictors of inattention and hyperactivity/impulsivity at 6 years. Journal of Attention Disorders, 23(11), 1291–1302. [DOI] [PubMed] [Google Scholar]
- *Frick MA., Forslund T., & Brocki KC. (2019). Can reactivity and regulation in infancy predict inattentive and hyperactive/impulsive behavior in 3-year-olds? Development and Psychopathology, 31(2), 619–629. [DOI] [PubMed] [Google Scholar]
- *Gagne JR., Asherson P., & Saudino KJ. (2020). A Twin Study of Inhibitory Control at Age Two and ADHD Behavior Problems at Age Three. Behavior Genetics, 50(4). [DOI] [PubMed] [Google Scholar]
- *Galéra C., Côté SM., Bouvard MP., Pingault J-B., Melchior M., Michel G., . . . Tremblay RE. (2011). Early risk factors for hyperactivity-impulsivity and inattention trajectories from age 17 months to 8 years. Archives of General Psychiatry, 68(12), 1267–1275. [DOI] [PubMed] [Google Scholar]
- Gartstein MA, & Rothbart MK (2003). Studying infant temperament via the revised infant behavior questionnaire. Infant Behavior and Development, 26(1), 64–86. [Google Scholar]
- Gewirtz S, Stanton-Chapman TL, & Reeve RE (2009). Can inhibition at preschool age predict attention-deficit/hyperactivity disorder symptoms and social difficulties in third grade? Early Child Development and Care, 179(3), 353–368. [Google Scholar]
- *Goldsmith HH., Lemery-Chalfant K., Schmidt NL., Arneson CL., & Schmidt CK. (2007). Longitudinal analyses of affect, temperament, and childhood psychopathology. Twin Research and Human Genetics, 10(1), 118–126. [DOI] [PubMed] [Google Scholar]
- *Goodwin A., Hendry A., Mason L., Bazelmans T., Begum Ali J., Pasco G., . . . Johnson MH. (2021). Behavioural Measures of Infant Activity but Not Attention Associate with Later Preschool ADHD Traits. Brain sciences, 11(5), 524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graziano PA, & Hart K (2016). Beyond behavior modification: Benefits of social–emotional/self-regulation training for preschoolers with behavior problems. Journal of school psychology, 58, 91–111. [DOI] [PubMed] [Google Scholar]
- *Gurevitz M., Geva R., Varon M., & Leitner Y. (2014). Early markers in infants and toddlers for development of ADHD. Journal of Attention Disorders, 18(1), 14–22. [DOI] [PubMed] [Google Scholar]
- Hedges LV (1983). A random effects model for effect sizes. Psychological Bulletin, 93(2), 388. [Google Scholar]
- Hendry A, Jones EJ, Bedford R, Gliga T, Charman T, Johnson MH, & Team B (2018). Developmental change in look durations predicts later effortful control in toddlers at familial risk for ASD. Journal of Neurodevelopmental Disorders, 10(1), 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson LA, Schneider H, & Mahone EM (2018). Preschool inhibitory control predicts ADHD group status and inhibitory weakness in school. Archives of Clinical Neuropsychology, 33(8), 1006–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Jaekel J., Eryigit-Madzwamuse S., & Wolke D. (2016). Preterm toddlers’ inhibitory control abilities predict attention regulation and academic achievement at age 8 years. The Journal of pediatrics, 169, 87–92. e81. [DOI] [PubMed] [Google Scholar]
- *Johnson P., Ahamat B., Mcconnachie A., Puckering C., Marwick H., Furnivall D., . . . Wilson P. (2014). Motor activity at age one year does not predict ADHD at seven years. International Journal of Methods in Psychiatric Research, 23(1), 9–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Jorm AF., Prior M., Sanson A., Smart D., Zhang Y., & Easteal S. (2001). Association of a polymorphism of the dopamine transporter gene with externalizing behavior problems and associated temperament traits: A longitudinal study from infancy to the mid-teens. American Journal of Medical Genetics, 105(4), 346–350. [DOI] [PubMed] [Google Scholar]
- *Joseph HM., McKone KM., Molina BS., & Shaw DS. (2021). Maternal Parenting and Toddler Temperament: Predictors of Early School Age Attention-Deficit/Hyperactivity Disorder-Related Behaviors. Research on Child and Adolescent Psychopathology, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kostyrka-Allchorne K, Wass SV, & Sonuga-Barke EJ (2020). Research Review: Do parent ratings of infant negative emotionality and self-regulation predict psychopathology in childhood and adolescence? A systematic review and meta-analysis of prospective longitudinal studies. Journal of Child Psychology and Psychiatry, 61(4), 401–416. [DOI] [PubMed] [Google Scholar]
- *Lawson K., & Ruff H. (2004). Early attention and negative emotionality predict later cognitive and behavioural function. International journal of behavioral development, 28(2), 157–165. [Google Scholar]
- *Lawson KR., & Ruff HA. (2004). Early focused attention predicts outcome for children born prematurely. Journal of Developmental and Behavioral Pediatrics, 25(6), 399–406. [DOI] [PubMed] [Google Scholar]
- *Leblanc N., Boivin M., Dionne G., Brendgen M., Vitaro F., Tremblay RE., & Pérusse D. (2008). The development of hyperactive–impulsive behaviors during the preschool years: the predictive validity of parental assessments. Journal of Abnormal Child Psychology, 36(7), 977–987. [DOI] [PubMed] [Google Scholar]
- *Lemcke S., Parner ET., Bjerrum M., Thomsen PH., & Lauritsen MB. (2016). Early development in children that are later diagnosed with disorders of attention and activity: a longitudinal study in the Danish National Birth Cohort. European Child and Adolescent Psychiatry, 25(10), 1055–1066. [DOI] [PubMed] [Google Scholar]
- *Levine TA., & Woodward LJ. (2018). Early inhibitory control and working memory abilities of children prenatally exposed to methadone. Early Human Development, 116, 68–75. [DOI] [PubMed] [Google Scholar]
- *Meeuwsen M., Perra O., Van Goozen SH., & Hay DF. (2019). Informants’ ratings of activity level in infancy predict ADHD symptoms and diagnoses in childhood. Development and Psychopathology, 31(4), 1255–1269. [DOI] [PubMed] [Google Scholar]
- *Miller M., Iosif A-M., Bell LJ., Farquhar-Leicester A., Hatch B., Hill A., . . . Ozonoff S. (2020). Can Familial Risk for ADHD Be Detected in the First Two Years of Life? Journal of Clinical Child and Adolescent Psychology, 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Miller M., Iosif A-M., Young GS., Hill MM., & Ozonoff S. (2018). Early detection of ADHD: Insights from infant siblings of children with autism. Journal of Clinical Child and Adolescent Psychology, 47(5), 737–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Miller NV., Degnan KA., Hane AA., Fox NA., & Chronis-Tuscano A. (2019). Infant temperament reactivity and early maternal caregiving: Independent and interactive links to later childhood attention-deficit/hyperactivity disorder symptoms. Journal of Child Psychology and Psychiatry, 60(1), 43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Miller NV., Hane AA., Degnan KA., Fox NA., & Chronis-Tuscano A. (2019). Investigation of a developmental pathway from infant anger reactivity to childhood inhibitory control and ADHD symptoms: interactive effects of early maternal caregiving. Journal of Child Psychology and Psychiatry, 60(7), 762–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, & Group P (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine, 6(7), e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BS, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS, . . . Abikoff HB. (2009). The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study. Journal of the American Academy of Child and Adolescent Psychiatry, 48(5), 484–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Morrell J., & Murray L. (2003). Parenting and the development of conduct disorder and hyperactive symptoms in childhood: A prospective longitudinal study from 2 months to 8 years. Journal of Child Psychology and Psychiatry, 44(4), 489–508. [DOI] [PubMed] [Google Scholar]
- Nigg JT, Blaskey LG, Stawicki JA, & Sachek J (2004). Evaluating the endophenotype model of ADHD neuropsychological deficit: results for parents and siblings of children with ADHD combined and inattentive subtypes. Journal of Abnormal Psychology, 113(4), 614. [DOI] [PubMed] [Google Scholar]
- Nigg JT, Sibley MH, Thapar A, & Karalunas SL, (2020). Development of ADHD: Etiology, heterogeneity, and early life course. Annual review of developmental psychology 2: 559–583. doi: 10.1146/annurev-devpsych-060320-093413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Olson SL., Bates JE., Sandy JM., & Schilling EM. (2002). Early developmental precursors of impulsive and inattentive behavior: From infancy to middle childhood. Journal of Child Psychology and Psychiatry, 43(4), 435–447. [DOI] [PubMed] [Google Scholar]
- *Papageorgiou KA., Smith TJ., Wu R., Johnson MH., Kirkham NZ., & Ronald A. (2014). Individual differences in infant fixation duration relate to attention and behavioral control in childhood. Psychological Science, 25(7), 1371–1379. doi: 10.1177/0956797614531295 [DOI] [PubMed] [Google Scholar]
- Polanczyk G, de Lima MS, Horta BL, Biederman J, & Rohde LA (2007). The worldwide prevalence of ADHD: a systematic review and metaregression analysis. American Journal of Psychiatry, 164(6), 942–948. [DOI] [PubMed] [Google Scholar]
- Polanin JR, Pigott TD, Espelage DL, & Grotpeter JK (2019). Best practice guidelines for Abstract screening large-evidence systematic reviews and meta-analyses. Research Synthesis Methods, 10(3), 330–342. [Google Scholar]
- Putnam SP, Gartstein MA, & Rothbart MK (2006). Measurement of fine-grained aspects of toddler temperament: The Early Childhood Behavior Questionnaire. Infant Behavior and Development, 29(3), 386–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Rende RD. (1993). Longitudinal relations between temperament traits and behavioral syndromes in middle childhood. Journal of the American Academy of Child & Adolescent Psychiatry, 32(2), 287–290. [DOI] [PubMed] [Google Scholar]
- *Robson AL., & Pederson DR. (1997). Predictors of individual differences in attention among low birth weight children. Journal of Developmental and Behavioral Pediatrics: JDBP, 18(1), 13–21. [DOI] [PubMed] [Google Scholar]
- Rothbart M (1981). Measurement of temperament in infancy child development. Child Develop, 52, 569–578. [Google Scholar]
- Rothbart MK (1989). Temperament in childhood: A framework. In Kohnstamm GA, Bates JA, & Rothbart MK (Eds.), Temperament in childhood. Wiley; New York, pp. 59–73. [Google Scholar]
- Rothbart MK & Bates JE (2006). Temperament. In: Eisenberg N, Damon W, editors. Handbook of child psychology: Vol. 3. Social, emotional, and personality development. 6th ed. Wiley; New York, pp. 99–166. [Google Scholar]
- *Sanson A., Smart D., Prior M., & Oberklaid F. (1993). Precursors of hyperactivity and aggression. Journal of the American Academy of Child & Adolescent Psychiatry, 32(6), 1207–1216. [DOI] [PubMed] [Google Scholar]
- Schiavone N, Virta M, Leppämäki S et al. Mortality in individuals with childhood ADHD or subthreshold symptoms – a prospective perinatal risk cohort study over 40 years. BMC Psychiatry 22, 325 (2022). 10.1186/s12888-022-03967-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Schmid G., & Wolke D. (2014). Preschool regulatory problems and attention-deficit/hyperactivity and cognitive deficits at school age in children born at risk: different phenotypes of dysregulation? Early Human Development, 90(8), 399–405. [DOI] [PubMed] [Google Scholar]
- Schmidt S, & Petermann F (2009). Developmental psychopathology: Attention deficit hyperactivity disorder (ADHD). BMC Psychiatry, 9(1), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw M, Hodgkins P, Caci H, Young S, Kahle J, Woods AG, & Arnold LE (2012). A systematic review and analysis of long-term outcomes in attention deficit hyperactivity disorder: effects of treatment and non-treatment. BMC Medicine, 10(1), 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Shephard E., Bedford R., Milosavljevic B., Gliga T., Jones EJ., Pickles A., . . . Baron-Cohen S. (2019). Early developmental pathways to childhood symptoms of attention-deficit hyperactivity disorder, anxiety and autism spectrum disorder. Journal of Child Psychology and Psychiatry, 60(9), 963–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shephard E, Zuccolo PF, Idrees MI, Godoy MPB, Salomone E, Ferrante MC, . . . Bolton PF. (2021). Systematic Review and Meta-analysis: The Science of Early-Life Precursors and Interventions for Attention-Deficit/Hyperactivity Disorder. Journal of the American Academy of Child and Adolescent Psychiatry. [DOI] [PubMed] [Google Scholar]
- Sigman M, Cohen SE, & Beckwith L (1997). Why does infant attention predict adolescent intelligence? Infant Behavior and Development, 20(2), 133–140. [Google Scholar]
- *Silberg JL., Gillespie N., Moore AA., Eaves LJ., Bates J., Aggen S., . . . Canino G. (2015). Shared genetic and environmental influences on early temperament and preschool psychiatric disorders in Hispanic twins. Twin Research and Human Genetics, 18(2), 171–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silver NC, & Dunlap WP (1987). Averaging correlation coefficients: should Fisher’s z transformation be used? Journal of Applied Psychology, 72(1), 146. [Google Scholar]
- *Silverman IW., & Ragusa DM. (1992). A short-term longitudinal study of the early development of self-regulation. Journal of Abnormal Child Psychology, 20(4), 415–435. [DOI] [PubMed] [Google Scholar]
- *Slinning K (2004). Foster placed children prenatally exposed to poly-substances. European Child and Adolescent Psychiatry, 13(1), 19–27. [DOI] [PubMed] [Google Scholar]
- *Smarius LJCA., Strieder TG., Loomans EM., Doreleijers TA., Vrijkotte TG., Gemke RJ., & van Eijsden M. (2017). Excessive infant crying doubles the risk of mood and behavioral problems at age 5: evidence for mediation by maternal characteristics. European Child and Adolescent Psychiatry, 26(3), 293–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Stephens RL., Elsayed HE., Reznick JS., Crais ER., & Watson LR. (2021). Infant attentional behaviors are associated with ADHD symptomatology and executive function in early childhood. Journal of Attention Disorders, 25(13), 1908–1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser SN, Danielson ML, Bitsko RH, Holbrook JR, Kogan MD, Ghandour RM, . . . Blumberg SJ. (2014). Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. Journal of the American Academy of Child and Adolescent Psychiatry, 53(1), 34–46 e32. doi: 10.1016/j.jaac.2013.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel AC, Jackson JJ, Barch DM, Tillman R, & Luby JL (2019). Excitability and irritability in preschoolers predicts later psychopathology: The importance of positive and negative emotion dysregulation. Development and psychopathology, 31(3), 1067–1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, & Vandenbroucke JP (2007). The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Bulletin of the World Health Organization, 85, 867–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Williams KE., Nicholson JM., Walker S., & Berthelsen D. (2016). Early childhood profiles of sleep problems and self-regulation predict later school adjustment. British Journal of Educational Psychology, 86(2), 331–350. [DOI] [PubMed] [Google Scholar]
- *Williams KE., & Sciberras E. (2016). Sleep and self-regulation from birth to 7 years: a retrospective study of children with and without attention-deficit hyperactivity disorder at 8 to 9 years. Journal of Developmental and Behavioral Pediatrics, 37(5), 385–394. [DOI] [PubMed] [Google Scholar]
- *Willoughby MT., Gottfredson NC., & Stifter CA. (2017). Observed temperament from ages 6 to 36 months predicts parent-and teacher-reported attention-deficit/hyperactivity disorder symptoms in first grade. Development and Psychopathology, 29(1), 107–120. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


