Abstract
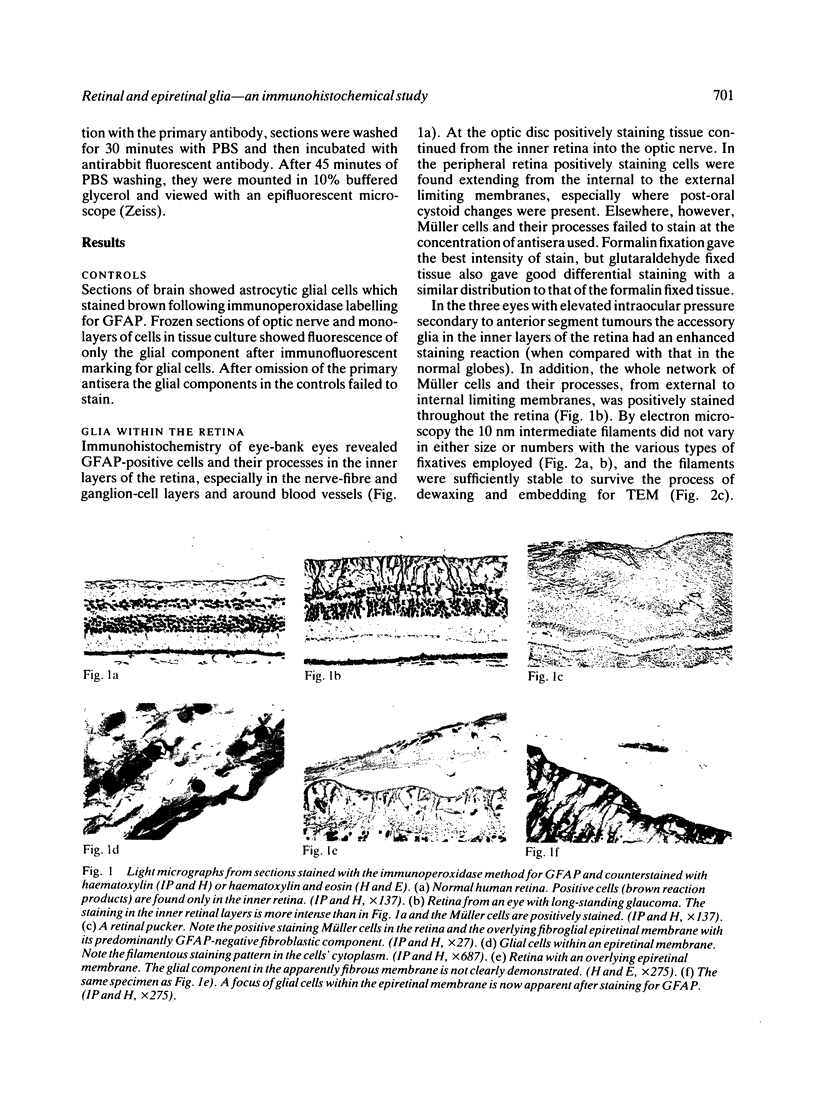
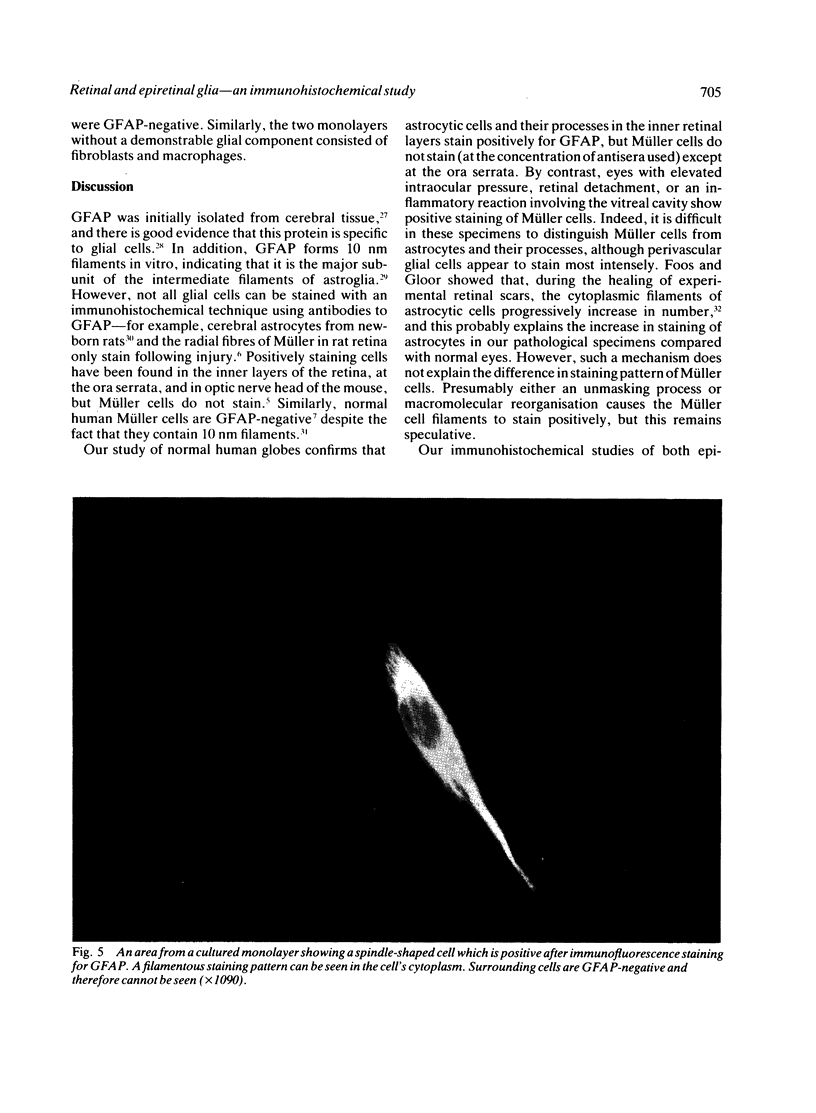
Immunohistochemical techniques were used to examine the distribution of cells containing glial fibrillary acidic protein (GFAP) in normal and pathological human specimens, including 22 globes (13 of which contained epiretinal membranes 'in situ'), 16 surgically excised epiretinal membranes, and monolayers of cells obtained from five epiretinal membranes placed in tissue culture. The astrocytic cells of normal and pathological retinae stained with the glial-cell marker, but Müller cells were GFAP-negative in normal retinae at the antisera dilutions used. Müller cells did, however, stain in retinae from glaucomatous eyes and in eyes with prolonged retinal detachment. Electron microscopy did not reveal any obvious morphological difference between the intermediate filaments of normal (GFAP-negative) and GFAP-positive Müller cells. Ten of the 13 epiretinal membranes 'in situ', all 16 excised membranes, and three of the five monolayers contained glial cells. Purely glial membranes were not associated with retinal puckering or detachment, while all membranes causing tractional complications had a prominent fibrous, non-glial component. Our findings suggest that glial cells do not contribute significantly to the contractile forces generated by epiretinal membranes. They may, however, provide a scaffold on which other cells proliferate and contract and an anchorage by means of which tangential forces are transmitted into and through the retina.
Full text
PDF







Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baines P. S., Hiscott P. S., McLeod D. Posterior non-vascularized proliferative extraretinopathy and peripheral nodular retinal telangiectasis. Trans Ophthalmol Soc U K. 1982;102(Pt 4):487–491. [PubMed] [Google Scholar]
- Bellhorn M. B., Friedman A. H., Wise G. N., Henkind P. Ultrastructure and clinicopathologic correlation of idiopathic preretinal macular fibrosis. Am J Ophthalmol. 1975 Mar;79(3):366–373. doi: 10.1016/0002-9394(75)90608-x. [DOI] [PubMed] [Google Scholar]
- Bock E. Nervous system specific proteins. J Neurochem. 1978 Jan;30(1):7–14. doi: 10.1111/j.1471-4159.1978.tb07028.x. [DOI] [PubMed] [Google Scholar]
- Clarkson J. G., Green W. R., Massof D. A histopathologic review of 168 cases of preretinal membrane. Am J Ophthalmol. 1977 Jul;84(1):1–17. [PubMed] [Google Scholar]
- Eng L. F., Vanderhaeghen J. J., Bignami A., Gerstl B. An acidic protein isolated from fibrous astrocytes. Brain Res. 1971 May 7;28(2):351–354. doi: 10.1016/0006-8993(71)90668-8. [DOI] [PubMed] [Google Scholar]
- Foos R. Y., Gloor B. P. Vitreoretinal juncture; healing of experimental wounds. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1975 Sep 5;196(3):213–220. doi: 10.1007/BF00410033. [DOI] [PubMed] [Google Scholar]
- Foos R. Y. Vitreoretinal juncture--simple epiretinal membranes. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1974 Jan 28;189(4):231–250. doi: 10.1007/BF02384852. [DOI] [PubMed] [Google Scholar]
- Green W. R., Kincaid M. C., Michels R. G., Pederson J. E., Kenyon K. R., Maumenee A. E. Pars planitis. Trans Ophthalmol Soc U K. 1981 Sep;101(3):361–367. [PubMed] [Google Scholar]
- Hamilton C. W., Chandler D., Klintworth G. K., Machemer R. A transmission and scanning electron microscopic study of surgically excised preretinal membrane proliferations in diabetes mellitus. Am J Ophthalmol. 1982 Oct;94(4):473–488. doi: 10.1016/0002-9394(82)90241-0. [DOI] [PubMed] [Google Scholar]
- Harada T., Chauvaud D., Pouliquen Y. An electron microscopic study of the epiretinal membrane of human eyes. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1981;215(4):327–339. doi: 10.1007/BF00407670. [DOI] [PubMed] [Google Scholar]
- Kenyon K. R., Michels R. G. Ultrastructure of epiretinal membrane removed by pars plana vitreoretinal surgery. Am J Ophthalmol. 1977 Jun;83(6):815–823. doi: 10.1016/0002-9394(77)90908-4. [DOI] [PubMed] [Google Scholar]
- Kenyon K. R., Pederson J. E., Green W. R., Maumenee A. E. Fibroglial proliferation in pars planitis. Trans Ophthalmol Soc U K. 1975;95(3):391–397. [PubMed] [Google Scholar]
- LESSELL S., KUWABARA T. RETINAL NEUROGLIA. Arch Ophthalmol. 1963 Nov;70:671–678. doi: 10.1001/archopht.1963.00960050673017. [DOI] [PubMed] [Google Scholar]
- Ogden T. E. Nerve fiber layer astrocytes of the primate retina: morphology, distribution, and density. Invest Ophthalmol Vis Sci. 1978 Jun;17(6):499–510. [PubMed] [Google Scholar]
- Rueger D. C., Huston J. S., Dahl D., Bignami A. Formation of 100 A filaments from purified glial fibrillary acidic protein in vitro. J Mol Biol. 1979 Nov 25;135(1):53–68. doi: 10.1016/0022-2836(79)90340-1. [DOI] [PubMed] [Google Scholar]
- WOLTER J. R. The astroglia of the human retina and other glial elements of the retina under normal and pathologic conditions. Am J Ophthalmol. 1955 Nov;40(5 Pt 2):88–100. [PubMed] [Google Scholar]







