Highlights
-
•
Longitudinal study of remote self-weighing data in diverse childbearing cohort.
-
•
Pre-pregnancy weight not associated with regular self-weighing during or after pregnancy.
-
•
Regular self-weighing more likely during pregnancy compared to postpartum period.
-
•
Regular self-weighing less likely among low-income Black childbearing people.
Keywords: Body weight, Ecological momentary assessment, Pregnancy, Postpartum weight retention, Treatment adherence, Self-weighing
Abstract
Black childbearing individuals in the US experience a higher risk of postpartum weight retention (PPWR) compared to their White counterparts. Given that PPWR is related to adverse health outcomes, it is important to investigate predictors of weight-related health behaviors, such as self-weighing (i.e., using a scale at home). Regular self-weighing is an evidence-based weight management strategy, but there is minimal insight into sociodemographic factors related to frequency. The Postpartum Mothers Mobile Study (PMOMS) facilitated longitudinal ambulatory weight assessments to investigate racial inequities in PPWR. Our objective for the present study was to describe self-weighing behavior during and after pregnancy in the PMOMS cohort, as well as related demographic and psychosocial factors. Applying tree modeling and multiple regression, we examined self-weighing during and after pregnancy. Participants (N = 236) were 30.2 years old on average (SD = 4.7), with the majority being college-educated (53.8%, n = 127), earning at least $30,000 annually (61.4%, n = 145), and self-identifying as non-Hispanic White (NHW; 68.2%, n = 161). Adherence to regular self-weighing (at least once weekly) was highest among participants during pregnancy, with a considerable decline after giving birth. Low-income Black participants (earning < $30,000) were significantly less likely to reach a completion rate of ≥ 80% during pregnancy (AOR = 0.10) or the postpartum period (AOR = 0.16), compared to NHW participants earning at least $30,000 annually. Increases in perceived stress were associated with decreased odds of sustained self-weighing after delivery (AOR = 0.79). Future research should consider behavioral differences across demographic intersections, such as race and socioeconomic status, and the impact on efficacy of self-weighing.
1. Introduction
Black childbearing people in the United States (US) experience a higher risk of inadequate gestational weight gain (GWG) and increased postpartum weight retention (PPWR) compared to their White counterparts. (Headen et al., 2012, Parker and Abrams, 1993, Keppel and Taffel, 1993, Endres et al., 2015, Siega-Riz et al., 2010, Whitaker et al., 2014) Also referred to as weight gain during pregnancy, GWG represents the difference between a childbearing individual’s pre-pregnancy weight and that at the onset of labor. PPWR is typically defined as an individual’s weight after giving birth minus their pre-pregnancy weight and may be operationalized as a continuous (e.g., absolute change in pounds) or categorical measure (e.g., at least 10 lb retained). (Medicine) IIo. , 2009) Both GWG and PPWR are impacted by pre-pregnancy weight with associations varying by race. (Headen et al., 2012, Headen et al., 2015, Schneider et al., 2018) Endres, et al. demonstrated that participants retaining more than 20 lb at one year postpartum were more likely to be Black. (Endres et al., 2015) Other studies have shown that adequate or moderate GWG is associated with reduced prevalence of preterm birth (<37 weeks’ gestation) (Leonard et al., 2017) and obesity later in life (Abrams et al., 2017) for Black childbearing people.
Self-monitoring, a method of systematic self-observation and recording of target behaviors, is the cornerstone of weight management. (Burke et al., 2011) Self-weighing, a form of self-monitoring, is defined as weighing oneself on a regular basis and recording the weight manually or digitally via smart devices. (Butryn et al., 2007, Steinberg et al., 2015) Regular self-weighing is a strategy based on empirical evidence demonstrating its efficacy in helping individuals achieve or maintain a desired weight. (Nezami et al., 2021, Zheng et al., 2016, Linde et al., 2007, Shieh et al., 2016, Lohr et al., 2023, Vuorinen et al., 2021, Zheng et al., 2015, Ross et al., 2019, Yu et al., 2022, Burke et al., 2008, Steinberg et al., 2013).
Studies examining self-weighing behavior in pregnant and postpartum cohorts report moderate to high completion rates (Daley et al., 2021, Krukowski et al., 2021, Daley et al., 2020, Shieh et al., 2017, Daley et al., 2015) and associations between self-weighing and weight loss (Lohr et al., 2023, Huseinovic et al., 2018) or eating behaviors. (Yu et al., 2022) Most of these studies defined regular self-weighing as at least once per week. Secondary analysis of data from an intervention study demonstrated demographic differences in self-weighing behavior during pregnancy: Medicaid-eligible participants were less likely to engage in regular self-weighing over a 45-day interval, whereas older individuals, White individuals, and those with more education were more likely to engage in consistent self-weighing, defined as once every 30-day period. (Olson et al., 2017) The evidence linking self-weighing behavior and GWG in relation to postpartum weight change, rather than net weight loss, is limited and inconclusive. (Fealy et al., 2020) One randomized controlled trial (RCT) showed no significant link between self-weighing and GWG, but reported benefits of self-weighing if paired with another lifestyle intervention for childbearing people with obesity. (Harrison et al., 2014).
Leveraging the infrastructure of a longitudinal study using ecological momentary assessment (EMA) to examine a diverse, clinic-based sample from late pregnancy through the first postpartum year, the present study aimed to describe weekly self-weighing completion rates in pregnant and postpartum populations and to identify associated demographic and psychosocial factors.
2. Methods
2.1. Study design & participants
The Postpartum Mothers Mobile Study (PMOMS) was a longitudinal investigation applying EMA to examine contextual exposures and racial inequities in PPWR. EMA is a data collection method that captures individuals’ behaviors and mood in their natural environment in real time, often using electronic devices (e.g., smartphones) and thereby reducing recall bias and lending ecological validity to study results. (Stone and Shiffman, 1994, Shiffman et al., 1998, Stone et al., 2007) EMA facilitates real-time assessment of weight, as well as self-reported psychosocial and contextual variables, not commonly reported in the existing literature. (Zheng et al., 2015).
PMOMS was ancillary to the GDM2 Study (Comparison of Two Screening Strategies for Gestational Diabetes), an RCT based in a southwestern Pennsylvania hospital. (Abebe et al., 2017, Davis et al., 2021, Scifres et al., 2015) PMOMS recruited participants between 18 and 32 weeks’ gestation and followed them through one year postpartum. Participants completed baseline surveys and staff provided them with a smart scale, as well as a smartphone if the participant did not have one. For approximately 15 months, participants were asked to complete daily EMA surveys (covering a broad range of contextual, emotional, and social variables) via smartphone; and weigh themselves at least once per week using the study-provided smart scale with its companion mobile app, which transmitted data to a secure server in real time. PMOMS was designed to investigate racial disparities, so recruitment of willing pregnant participants that self-identified as non-Hispanic Black/African American (hereafter referred to as “Black”) was prioritized. Although Black participants make up just 28% (n = 87) of the entire PMOMS cohort, this proportion is greater than that of Pittsburgh (23%) or surrounding Allegheny County (14%) according to the US Census. Additional details regarding the PMOMS protocol are published elsewhere. (Mendez et al., 2019) The Institutional Review Board of the Human Research Protection Office at the University of Pittsburgh approved the study protocol.
The present study provides separate analyses of self-weighing behavior during pregnancy and one year postpartum. The inclusion criteria were at least one self-weighing assessment during the relevant pregnancy or postpartum period, and self-reported racial identity as Black or non-Hispanic White (NHW). In this study, we conceptualize race as a social construct and not a biological one. (Ford and Airhihenbuwa, 2010) Our analysis includes a Black-White comparison to assess racial inequities and investigate social and demographic factors that may explain them.
2.2. Measures
Outcome Variables. We examined the following main outcomes in the present study: regular self-weighing during pregnancy (≥80% of weekly intervals with ≥ one weight during pregnancy); regular self-weighing after pregnancy (≥80% of weekly intervals with ≥ one weight during postpartum period); and sustained self-weighing after giving birth (≥nine months’ duration from first to last weight during postpartum period). The completion thresholds were based on the PMOMS protocol (Mendez et al., 2019), which required at least a 60% completion rate for participant compensation and included additional compensation opportunities for those who achieved ≥ 80% completion. The nine-month postpartum cut-off was selected because its proportion to 12 months approximated the priori 80% cut-off (9/12 = 0.75).
Participants received weekly prompts on Fridays to remind them to step on the smart scale, but they could self-weigh at any time throughout study participation. Weekly interval rates were calculated based on self-weighing at least once between Thursday to the following Friday for each participant. We calculated the self-weighing completion rate during pregnancy and postpartum periods (first and second outcomes), computed as the number of weekly intervals with at least one weight divided by the total number of intervals for which they were followed. For example, if a participant weighed themselves at least once within five weekly intervals over a 10-week period, their completion rate would be 50%. Additional weigh-ins within an interval were not counted. Lastly, we computed the duration of self-weighing as the number of weeks between the first and last weight within the postpartum period (third outcome).
Demographic, Behavioral, and Psychosocial Variables. Exposure variables and covariate data were extracted from self-administered questionnaires and participant medical records. Participants completed non-EMA surveys at the baseline visit (18–32 weeks’ pregnant), during which they reported age, income, educational attainment, and race/ethnicity. At this baseline visit, participants also completed the Perceived Stress Scale (PSS), a well-validated tool for rating the frequency of certain feelings (e.g., felt nervous or stressed) over the last month on a scale of zero (never) to four (very often). (Cohen et al., 1983) At 14 days after the baseline visit, participants completed a non-EMA questionnaire that included items from the Major Discrimination Scale, assessing exposure to unfair treatment (e.g., unfairly denied a promotion). (Williams et al., 2008) Eight days after delivery, participants completed another non-EMA questionnaire that assessed breastfeeding initiation within 24 h of giving birth. Breastfeeding is included as a covariate in this study because we theorized the behavior could affect a childbearing person’s capability of self-weighing regularly. More comprehensive information about survey content and timeline is published elsewhere. (Mendez et al., 2019) We did not include any EMA constructs other than self-weighing in these analyses because we primarily focused on baseline predictors.
Information extracted from participants’ medical records included pre-pregnancy weight (self-reported or measured in-clinic); weeks’ gestation at birth; type of birth (vaginal vs. surgical); and maternal morbidity (binary), which was a composite measure developed by GDM2 that represents the incidence of perinatal complications (hypertensive disorder of pregnancy, postpartum hemorrhage, or third- or fourth-degree perineal laceration). (Davis et al., 2021).
Because of collinearity and the patterning of income by race in this sample (i.e., a large proportion of Black participants were low income and a large proportion of NHW participants were high income), we created a race-income composite measure to be used for regression analyses, consisting of four categories (Black and earning <$30,000 annually; Black and earning ≥$30,000; NHW and earning <$30,000; and NHW and earning ≥$30,000). This approach ensures that these patterns by race and income can be explicitly modeled and will facilitate clearer interpretation of associations.
2.3. Data analysis
We included the following variables in regression models for regular self-weighing (≥80% completion) during pregnancy: age (years, continuous); annual income (binary, using the empirical $30,000 threshold); education level (binary, college degree or less); pre-pregnancy weight (kilograms, continuous); change in weight (kilograms, continuous) from pre-pregnancy to the first study visit for applicable participants; PSS score (continuous); self-reported race (binary, Black or NHW); major discrimination score (continuous); and the race*income composite variable (categorical). The same predictor variables were included in regression models for regular postpartum self-weighing (≥80% completion) and sustained self-weighing after delivery (≥9 months between first and last postpartum assessments), with the addition of birth type (binary), breastfeeding initiation (binary), gestational age at birth (weeks, continuous), and maternal complications (binary).
We used two exploratory modeling strategies to identify predictors of each of our three self-weighing outcomes (≥80% completion during pregnancy; ≥80% completion after giving birth; and sustained self-weighing ≥ 9 months after giving birth). First, we performed logistic regression to evaluate the association between each variable and outcome in an additive context, examining both univariable models (i.e., including each variable in a separate model) and multivariable models (i.e., including all features simultaneously). In both univariable and multivariable models, we used post-hoc pairwise comparisons to examine pairwise differences when categorical measures (e.g., the race-income composite measure) were statistically significant. In models for regular self-weighing during pregnancy and postpartum, participants contributed data over different numbers of weeks. In order for the total sum of weights to be equivalent to the total number of participants, we weighted the analyses by the number of weeks, which were scaled by the proportion of the total sample to the total number of person-weeks contributed.
Second, we used conditional inference tree-structured models (Hothorn et al., 2006) to evaluate the association between the variables and outcome in a more complex and non-linear context. This was implemented using the “ctree” function in R (partykit package). (R: A language and environment for statistcal computing [computer program], 2020) These tree-structured models empirically identify the variables most strongly associated with the outcome and then identify the specific binary cut-point that results in two subgroups (i.e., nodes) that are most homogenous with respect to the outcome. This splitting procedure continues iteratively on each node until a minimum node size is reached, or there are no more significant exposure variables within a given subgroup. Here, we conservatively set the maximum node size as 20% of sample size to reduce spurious findings. Scaling or weighting, as described in the previous paragraph, is not available for these algorithms. To limit variability in the length of time that participants contributed data, we included only those participants with at least five weeks of study participation (allowing computation of 80% completion rate) in tree modeling. These analyses were conducted separately for each of our three outcomes.
3. Results
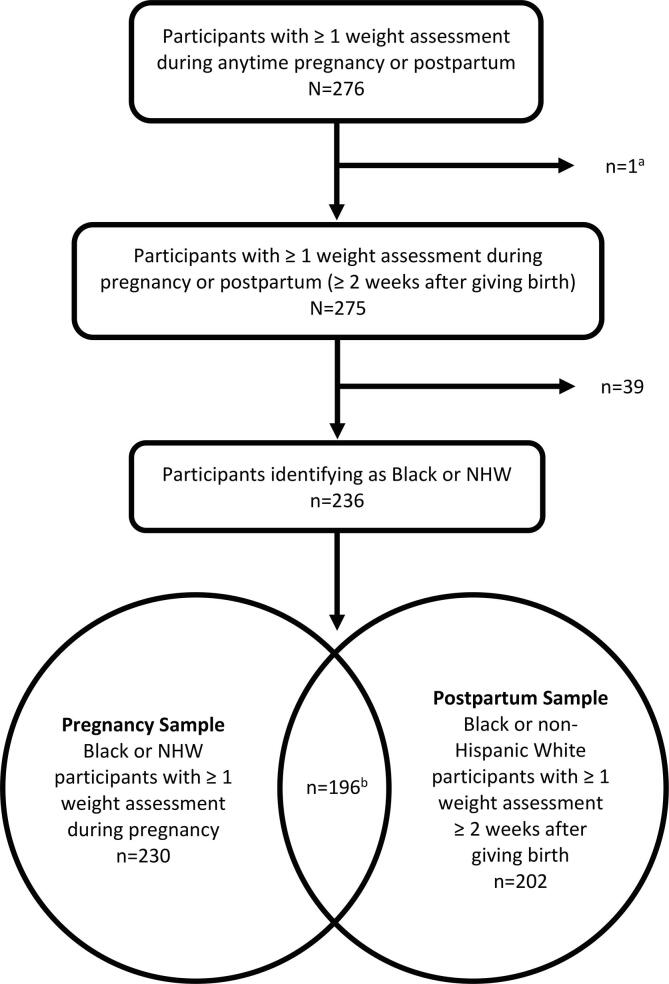
The flow chart in Fig. 1 illustrates how analytic samples were selected and how the pregnancy and postpartum samples overlap. After excluding participants without any weights (n = 48), those without weights in the established timeframes (n = 1), and those that did not identify as Black or NHW (n = 39), we arrived at our pregnant (n = 230) and postpartum samples (n = 202). Compared to those in the analytic sample, those who did not self-weigh at all during their study participation (described in Supplemental Table 1) were older, college-educated, lower income, and predominantly NHW. At baseline, those who did not self-weigh reported similar baseline stress levels, slightly higher levels of discrimination, and lower pre-pregnancy weight.
Fig. 1.
Flow chart illustrating how pregnancy (n = 230) and postpartum samples (n = 202) were selected for analyses from the PMOMS cohort. aOne participant self-weighed once between 0 and 14 days after giving birth and not at any other time. bThe pregnancy and postpartum samples are overlapping in that some participants may be included in only the pregnancy sample (n = 34), only the postpartum sample (n = 6), or both (n = 196). NHW: non-Hispanic White; PMOMS: Postpartum Mothers Mobile Study.
Table 1.
Descriptive statistics for pregnancy and postpartum samples used in analyses.
| Variable | Overall (N = 236) | Pregnancy completion |
Postpartum completion |
Sustained self-weighing after delivery |
|||
|---|---|---|---|---|---|---|---|
| ≥80% (n = 186) |
<80% (n = 44) |
≥80% (n = 115) |
<80% (n = 87) |
≥9 months(n = 132) | <9 months(n = 70) | ||
| Age, mean ± SD | 30.2 ± 4.7 | 30.6 ± 4.4 | 28.7 ± 5.7 | 31.3 ± 3.9 | 29.8 ± 4.9 | 31.4 ± 4.0 | 29.3 ± 4.8 |
| Education, n (%) | |||||||
| Less than college degree | 109 (46.2) | 77 (41.4) | 30 (68.2) | 38 (33.0) | 48 (55.2) | 43 (32.6) | 43 (61.4) |
| College degree | 127 (53.8) | 109 (58.6) | 14 (31.8) | 77 (67.0) | 39 (44.8) | 89 (67.4) | 27 (38.6) |
| Income, n (%) | |||||||
| < $30,000 annually | 91 (38.6) | 55 (29.6) | 32 (72.7) | 26 (22.6) | 43 (49.4) | 30 (22.7) | 39 (55.7) |
| ≥ $30,000 annually | 145 (61.4) | 131 (70.4) | 12 (27.3) | 89 (77.4) | 44 (50.6) | 102 (77.3) | 31 (44.3) |
| Race, n (%) | |||||||
| Non-Hispanic Black | 75 (31.8) | 46 (24.7) | 27 (61.4) | 21 (18.3) | 37 (42.5) | 26 (19.7) | 32 (45.7) |
| Non-Hispanic White (NHW) | 161 (68.2) | 140 (75.3) | 17 (38.6) | 94 (81.7) | 50 (57.5) | 106 (80.3) | 38 (54.3) |
| Race – Income Combination Variable, n (%) | |||||||
| Black + < $30,000 annually | 59 (25.0) | 33 (17.7) | 24 (54.5) | 15 (13.0) | 29 (33.3) | 17 (12.9) | 27 (38.6) |
| Black + ≥ $30,000 annually | 16 (6.8) | 13 (7.0) | 3 (6.8) | 6 (5.2) | 8 (9.2) | 9 (6.8) | 5 (7.1) |
| NHW + < $30,000 annually | 32 (13.6) | 22 (11.8) | 8 (18.2) | 11 (9.6) | 14 (16.1) | 13 (9.8) | 12 (17.1) |
| NHW + ≥ $30,000 annually | 129 (54.7) | 118 (63.4) | 9 (20.5) | 83 (72.2) | 36 (41.4) | 93 (70.5) | 26 (37.1) |
| Gestational age at birth (weeks), mean ± SD | 39.1 ± 1.7 | 39.2 ± 1.7 | 38.9 ± 1.6 | 39.2 ± 1.5 | 38.7 ± 2.0 | ||
| Cesarean birth, n (%) | 53 (22.5) | 29 (25.2) | 24 (27.6) | 35 (26.5) | 18 (25.7) | ||
| Maternal composite, n (%) | 30 (12.7) | 14 (12.2) | 16 (18.4) | 21 (15.9) | 9 (12.9) | ||
| Breastfeeding initiation within 24 h of delivery, n (%) | 164 (69.5) | 99 (86.1) | 65 (74.7) | 113 (85.6) | 51 (72.9) | ||
| Stress (baseline), mean ± SD | 7.1 ± 2.0 | 6.9 ± 2.0 | 7.6 ± 2.1 | 6.8 ± 1.9 | 7.3 ± 2.0 | 6.6 ± 1.8 | 7.6 ± 2.1 |
| Discrimination (baseline), mean ± SD | 1.0 ± 1.2 | 1.0 ± 1.3 | 1.0 ± 1.2 | 1.0 ± 1.3 | 0.9 ± 1.3 | 0.9 ± 1.2 | 1.1 ± 1.4 |
| Pre-pregnancy weight (kilograms), mean ± SD | 72.9 ± 20.6 | 72.6 ± 18.9 | 75.5 ± 27.1 | 73.4 ± 19.0 | 72.2 ± 18.2 | 73.6 ± 18.2 | 71.6 ± 19.5 |
| Weight change from pre-pregnancy to first study visit (kilograms), mean ± SD | 8.5 ± 5.3 | 8.5 ± 5.4 | 8.6 ± 4.9 | 8.2 ± 4.5 | 8.9 ± 6.1 | 8.7 ± 5.2 | 8.1 ± 5.4 |
SD: standard deviation.
Data from the postpartum sample were used to describe regular self-weighing after giving birth (≥80% completion) and sustained self-weighing during the first postpartum year (≥9 months between first and last postpartum assessments).
3.1. Sociodemographic characteristics by self-weighing outcomes
Table 1 describes the demographic and clinical characteristics across the three outcomes. The overall sample had a mean age of 30 years, with the majority being college-educated (53.8%, n = 127), earning ≥$30,000 annually (61.4%, n = 145), and identifying as NHW (68.2%, n = 161). The mean gestational age at birth was 39.1 weeks. An estimated 22.5% (n = 53) had cesarean births, while just 12.7% (n = 30) experienced a complication. Most (69.5%, n = 164) reported breastfeeding initiation within 24 h of giving birth. Participant reports indicated a mean PSS score of 7.1 (SD = 2.0; i.e., low stress) and an average of one (1.0; SD = 1.2) experience of major discrimination over their lifetime.
3.2. Pregnancy completion
Table 2 provides results of logistic regression models explaining the associations between the key exposure variables and the outcome of completing ≥ 80% self-weighing assessments during pregnancy. In univariable models that examined each feature separately, higher income (≥$30,000 annually), NHW (vs. Black) race, college education, NHW with higher income, and lower stress were all significantly associated (p < 0.05) with increased odds of reaching 80% completion during pregnancy. In the multivariable model including all features simultaneously, only the race-income composite variable remained significant. Based on Tukey’s adjusted pairwise comparisons from the adjusted model, the odds of completing ≥ 80% self-weighing assessments during pregnancy for Black and NHW participants earning less than $30,000 were 65% (AOR = 0.35) and 90% (AOR = 0.10) lower, respectively, than the odds for NHW participants earning ≥$30,000.
Table 2.
Regression results for at least an 80% completion rate in pregnancy sample, including odds ratios and 95% confidence interval values.
| Outcome: ≥ 80% Completion Rate During Pregnancy (Weighted by Scaled Number of Weeks)a | ||
|---|---|---|
| Univariate Logistic | Multivariable Logistic | |
| OR [95% CI] | OR [95% CI] | |
| Income | 1.53 [1.33–1.79] | – |
| Black vs. Non-Hispanic White | 0.16 [0.08–0.32] | – |
| Education | 1.90 [1.46–2.52] | – |
| Race-Income Compositeb | ||
| NHW + ≥ $30,000 annually | REF | REF |
| NHW + < $30,000 annually | 0.18 [0.06–0.49] | 0.18 [0.06–0.58] |
| Black + ≥ $30,000 annually | 0.37 [0.09–2.00] | 0.35 [0.08–1.99] |
| Black + < $30,000 annually | 0.07 [0.03–0.17] | 0.10 [0.03–0.26] |
| Pre-pregnancy weight | 1.00 [0.99–1.01] | 1.00 [0.99–1.01] |
| Weight change: pre-pregnancy to first study visit | 0.99 [0.96–1.02] | 0.99 [0.96–1.03] |
| Age | 1.14 [1.06–1.23] | 1.06 [0.96–1.17] |
| Discrimination | 1.05 [0.81–1.39] | 1.20 [0.88–1.70] |
| Stress (PSS) (Cohen et al., 1983) | 0.82 [0.69–0.96] | 0.84 [0.69–1.03] |
CI: confidence interval; GDM2: OR: odds ratio; PSS: Perceived Stress Scale.
n = 215 with complete data across all covariates (multivariable model); n = 230 possible.
x2 = 23.80, df = 3, p < 0.0001 in multivariable logistic model; x2 = 44.61, df = 3, p < 0.001 in univariate logistic model.
For the pregnancy sample tree model, we included participants with at least five weeks of ambulatory weight measures during pregnancy (n = 191, 83%). Participants excluded from tree model analysis were younger (t = -2.82, df = 52.87, p = 0.0007), but otherwise did not differ from participants included in the model. The only split occurred using the race-income composite measure, with participants earning ≥$30,000 annually, of either race, being more likely to reach ≥ 80% completion during pregnancy, compared to those earning <$30,000. Among those earning ≥$30,000 annually (n = 121), 90% (n = 109) had a completion rate of ≥ 80%, compared to only 55% (n = 38) among participants earning <$30,000 annually (n = 69).
3.3. Postpartum completion
Table 3 provides results of logistic regression models explaining the associations between exposure variables and the outcome of ≥ 80% completion in the first year after giving birth. Based on univariable models, earning ≥$30,000 annually, being NHW (vs. Black), reported breastfeeding initiation within 24 h of giving birth, and having a college education or higher were significantly associated with increased odds of reaching a completion rate of ≥ 80% during the postpartum period. Only the race-income composite measure remained significant in the multivariable regression model that included all predictors simultaneously. Tukey’s adjustment in the multivariable model showed that Black participants earning <$30,000 had 84% lower odds (AOR = 0.16) of reaching ≥ 80% completion, compared to NHW participants earning ≥$30,000 annually.
Table 3.
Logistic regression results for at least an 80% completion rate in postpartum sample, including odds ratios and 95% confidence interval values.
| Outcome: ≥ 80% Completion Rate During Post-Partum (Weighted by Scaled Number of Weeks)a | ||
|---|---|---|
| Univariate | Multivariable | |
| OR [95% CI] | OR [95% CI] | |
| Income | 1.26 [1.13–1.40] | – |
| Black | 0.23 [0.11–0.45] | – |
| Education | 1.46 [1.16–1.87] | – |
| Race-Income Compositeb | ||
| NHW + ≥ $30,000 annually | REF | REF |
| NHW + < $30,000 annually | 0.41 [0.16–1.02] | 0.41 [0.14–1.21] |
| Black + ≥ $30,000 annually | 0.36 [0.12–1.11] | 0.28 [0.08–0.97] |
| Black + < $30,000 annually | 0.14 [0.06–0.33] | 0.16 [0.05–0.44] |
| Pre-pregnancy weight | 1.00 [0.99–1.01] | 1.01 [1.00–1.02] |
| Weight change: pre-pregnancy to first study visit | 0.99 [0.96–1.01] | 0.99 [0.96–1.02] |
| Age | 1.07 [1.00–1.15] | 1.02 [0.93–1.12] |
| Discrimination | 1.02 [0.81–1.30] | 1.09 [0.83–1.44] |
| Stress (PSS) (Cohen et al., 1983) | 0.87 [0.75–1.02] | 0.85 [0.69–1.03] |
| Maternal Morbidityc | 0.69 [0.32–1.51] | 0.62 [0.25–1.59] |
| Cesarean | 0.81 [0.43–1.53] | 0.76 [0.35–1.65] |
| Gestational age at birth (continuous, weeks) | 1.17 [0.97–1.41] | 1.21 [0.96–1.54] |
| Breastfeeding initiation | 2.67 [1.16–6.33] | 1.96 [0.71–5.59] |
CI: confidence interval; NHW: non-Hispanic White; OR: odds ratio; PSS: Perceived Stress Scale.
an = 186 with complete data across all covariates (multivariable model); n = 202 possible.
bx2 = 14.69, df = 3, p = 0.002 in multivariable logistic model; x2 = 24.30, df = 3, p < 0.001 in univariate logistic model.
bComposite variable indicating at least one maternal morbidity condition.
The tree model for this postpartum sample included participants with at least five weeks of ambulatory weight measures during the postpartum period (n = 191, 83%). The race-income composite variable differed significantly (p-value = 0.002 from Fisher’s Exact Test) between participants with at least a five-week self-weighing duration and those without. Black participants (OR = 0.13, 95% CI = [0.02, 0.59]) and those earning <$30,000 annually (OR = 0.10, 95% CI = [0.01, 0.52]) were less likely to have at least five weeks of data after giving birth. Only the race-income composite measure split the model, separating out NHW participants earning ≥$30,000 annually versus Black or NHW participants earning <$30,000. Among NHW participants earning ≥$30,000 annually (n = 117), 70% (n = 82) reached ≥ 80% completion. Among Black or NHW participants earning <$30,000 (n = 74), 32% (n = 24) reached ≥ 80% completion.
3.4. Sustained self-weighing after delivery
Table 4 provides logistic regression results for participants who continued to self-weigh for at least nine months after giving birth. In univariable analyses, the following variables were significantly associated with increased odds of sustained self-weighing after delivery: earning ≥$30,000 annually, self-identifying as NHW (vs. Black), increased age, lower stress, increased gestational age at birth, and college education (or higher). In multivariable models, only the race-income composite and stress variables remained significantly associated. The adjusted odds of sustained self-weighing after delivery among Black participants earning <$30,000 were 75% (AOR = 0.25) lower compared to NHW participants earning ≥$30,000 annually. Increased PSS scores were associated with 21% lower adjusted odds (AOR = 0.79) of sustained self-weighing after delivery.
Table 4.
Logistic regression results for sample of participants that self-weighed for at least nine months after giving birth, including odds ratios and 95% confidence interval values.
| Outcome: ≥9 Months from First to Last Weight during Postpartuma | ||
|---|---|---|
| Univariable | Multivariable | |
| OR [95% CI] | OR [95% CI] | |
| Income | 1.30 [1.17–1.45] | – |
| Black | 0.29 [0.15–0.55] | – |
| College education (or higher) | 1.59 [1.26–2.04] | – |
| Race-Income Compositeb | ||
| NHW + ≥ $30,000 annually | REF | REF |
| NHW + < $30,000 annually | 0.30 [0.12–0.75] | 0.36 [0.12–1.05] |
| Black + ≥ $30,000 annually | 0.50 [0.16–1.76] | 0.39 [0.11–1.52] |
| Black + < $30,000 annually | 0.18 [0.08–0.37] | 0.25 [0.09–0.65] |
| Pre-pregnancy weight | 1.00 [1.00–1.01] | 1.01 [1.00–1.02] |
| Weight change: pre-pregnancy to first study visit | 1.01 [0.98–1.04] | 1.01 [0.98–1.04] |
| Age | 1.12 [1.05–1.21] | 1.04 [0.96–1.14] |
| Discrimination | 0.90 [0.71–1.13] | 0.94 [0.71–1.24] |
| Stress (PSS) (Cohen et al., 1983) | 0.76 [0.65–0.89] | 0.79 [0.65–0.96] |
| Maternal Morbidityc | 1.28 [0.57–3.11] | 1.11 [0.42–3.10] |
| Cesarean | 1.04 [0.54–2.05] | 0.93 [0.42–2.13] |
| Gestational age at birth (continuous, weeks) | 1.20 [1.01–1.43] | 1.21 [0.96–1.54] |
| Breastfeeding initiation | 2.08 [0.95–4.54] | 1.20 [0.45–3.09] |
CI: confidence interval; NHW: non-Hispanic White; OR: odds ratio; PSS: Perceived Stress Scale.
an = 186 with complete data across all covariates (multivariable model); n = 202 possible.
bx2 = 23.80, df = 3, p < 0.0001 in multivariable logistic model; x2 = 44.61, df = 3, p < 0.001 in univariate logistic model.
cComposite variable indicating at least one maternal morbidity condition.
In tree modeling for the sustained self-weighing outcome, the race-income composite split the sample. Among participants earning ≥$30,000 annually (n = 133), approximately 77% (n = 102) continued self-weighing for at least nine months after giving birth. Among those earning < $30,000 (n = 69), only 43% (n = 30) continued self-weighing for at least nine months.
4. Discussion
To our knowledge, this study represents the first observational investigation of regular self-weighing behavior during pregnancy and postpartum in overlapping analytic cohorts. Participants were more likely to reach an 80% completion rate for weekly self-weighing during pregnancy, with a considerable decline during the postpartum period. Approximately 80% (n = 186) of the participants reached the 80% completion threshold during pregnancy and about 57% (n = 115) reached it during the 12-month postpartum period. In comparison, two feasibility trials reported 100% weekly adherence to a self-weighing protocol among pregnant participants and 63% adherence among postpartum participants. (Daley et al., 2021, Shieh et al., 2017).
PMOMS participants were given the same incentive opportunity upon reaching the 80% threshold during pregnancy and postpartum periods. This was in addition to an incentive received for achieving a completion rate of at least 60%. (Mendez et al., 2019) Even so, participants were less likely to reach at least 80% completion during the postpartum period. The perceived value of self-weighing during pregnancy relative to health decision-making, as evidenced in qualitative research by Ferrey, et al. (Ferrey et al., 2021), may help explain the increased completion rates during pregnancy (compared to postpartum). Childbearing people may perceive weight monitoring as less valuable after giving birth. A recent systematic review of postpartum care guidelines indicated that weight management received less attention than other topics, such as infant feeding and contraception. (Yang et al., 2021).
The present study found significant demographic differences in regular self-weighing behavior, which is in agreement with previous investigations of both childbearing (Olson et al., 2017) and non-childbearing populations. (Gavin et al., 2015, Kong et al., 2012) Our study showed that low-income Black participants were significantly less likely to reach the 80% completion rate during pregnancy or postpartum, compared to NHW participants earning ≥ $30,000 annually. The race and class differences may signify how intersecting systems of oppression uniquely and disproportionately impact low-income Black populations, presently and historically. (Williams, 1999, Beech et al., 2021) In the same vein, it is important to consider the intersections of social disadvantage for low-income Black childbearing populations, as well as how it may impact health behaviors. (Elder et al., 2016, Braveman et al., 2015) Black women and birthing people living in poverty are more likely to face racial and gendered discrimination, barriers to desired care, and poor health outcomes. (Okoro et al., 2022) Even so, participants excluded from analyses due to not having any self-weighing assessments were older, college-educated, higher income, and NHW (Supplemental Table 1). This may indicate demographic differences in motivation to engage at all with the self-weighing component of the study, regardless of compensation thresholds.
Perceived stress was not significantly associated with self-weighing completion rates during pregnancy or postpartum periods in this study. However, higher levels of perceived stress were associated with lower levels of sustained self-weighing after delivery (≥9 months between first and last weight), adjusting for other demographic and clinical factors. This finding may implicate changes in mood or stress levels during the postpartum period that impact self-weighing. The limited literature suggests a relationship between self-weighing frequency and mood or stress (Hahn et al., 2021, Benn et al., 2016), but the unique impacts for childbearing populations are unclear, presenting an area for future research.
5. Strengths & limitations
While the present study is innovative in its exploration of self-weighing patterns in an observational cohort during and after pregnancy, our interpretation of findings is not without limitations. This analysis did not include follow-up assessments or EMA measures of stress. It is likely that these longitudinal data, including real-time contextual assessments, would change the findings presented here. Variation in self-weighing behavior may be predicted by day-to-day changes in exposure to different stressors, including those related to parenting, discrimination, and COVID-19. Even so, our description of the interaction between race and income provides a valuable analytic foundation for future studies examining how demographic characteristics impact beneficial health behaviors.
In addition, this study did not consider other relevant factors, such as attitudes about self-weighing or weight management counseling, which may have impacted self-weighing frequency during study periods. Even so, our study prompted participants to self-weigh at least once every week and provided additional incentives to those who maintained completion rates of at least 80%.
Lastly, we did not include information about participants’ technical problems (e.g., broken smart scale, dead battery), which would likely affect self-weighing completion rates. Although we regularly documented participants’ experiences with these types of issues to troubleshoot throughout the study, we did not prepare these data to be included in the present analyses.
6. Conclusions
The present study was innovative in its examination of self-weighing behavior in a diverse sample, from pregnancy to approximately one year postpartum. Leveraging the mobile-based data collection infrastructure of PMOMS, we demonstrated longitudinal patterns in self-weighing and variation by demographic and psychosocial factors. Specifically, we identified significantly lower odds of regular self-weighing (completion rates of ≥ 80%) during pregnancy and after delivery among low-income Black childbearing participants. This finding points to the racial and income inequities that impact this population, as well as their engagement in recommended or desired health behaviors. Furthermore, this study sets the foundation for deeper investigation of how self-weighing (or other self-monitoring behaviors) is related to individual mood and experiences of stress, particularly for childbearing populations.
CRediT authorship contribution statement
Sarah Annalise Sanders: Project administration, Writing – original draft. Meredith L. Wallace: Data curation, Formal analysis, Methodology, Writing – review & editing. Lora E. Burke: Investigation, Writing – review & editing. Amanda L. Tapia: Data curation, Writing – review & editing. Stephen L. Rathbun: Methodology, Writing – review & editing. Andrea D. Casas: Project administration, Writing – review & editing. Tiffany L. Gary-Webb: Investigation, Writing – review & editing. Esa M. Davis: Investigation, Writing – review & editing. Dara D. Méndez: Conceptualization, Funding acquisition, Investigation, Supervision, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The PMOMS study is funded by the National Institutes of Health, National Heart Lung and Blood Institute (R01HL135218; Principal Investigator: DDM). The authors thank the study participants who generously gave their time and effort. The authors would also like to thank Terri Washington, study coordinator; Maura Dugan, Dr. Yu-Hsuan Lai, Dr. Serwaa Omowale, Marquita Smalls, and Gabriella Mendez for study recruitment and follow-up; Er Wang, Pedram Gharani, Meirman Syzdykbayev, and Bradley Wheeler, and Dr. Hassan Karimi for technology and app development and support; and John Gianakas for database development and management. Finally, the authors thank all the staff and investigators of the GDM2 trial.
Disclosures
ED is a member of the US Preventative Services Task Force (USPSTF), this article does not necessarily represent the views and policies of the USPSTF. MLW is a consultant for Noctem and Health Rhythms, but the author's work is not related to the present project.
Data availability
The data that has been used is confidential.
References
- Abebe K.Z., Scifres C., Simhan H.N., Day N., Catalano P., Bodnar L.M., Costacou T., Matthew D., Illes A., Orris S., Duell J., Ly K., Davis E.M. Comparison of two screening strategies for gestational diabetes (GDM(2)) trial: design and rationale. Contemp Clin Trials. 2017;62:43–49. doi: 10.1016/j.cct.2017.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abrams B., Coyle J., Cohen A.K., Headen I., Hubbard A., Ritchie L., Rehkopf D.H. Excessive gestational weight gain and subsequent maternal obesity at age 40: a hypothetical intervention. Am J Public Health. 2017;107(9):1463–1469. doi: 10.2105/AJPH.2017.303881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beech B.M., Ford C., Thorpe R.J., Jr., Bruce M.A., Norris K.C. Poverty, racism, and the public health crisis in America. Front Public Health. 2021;9 doi: 10.3389/fpubh.2021.699049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benn Y., Webb T.L., Chang B.P., Harkin B. What is the psychological impact of self-weighing? A meta-analysis. Health Psychol Rev. 2016;10(2):187–203. doi: 10.1080/17437199.2016.1138871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman P.A., Heck K., Egerter S., Marchi K.S., Dominguez T.P., Cubbin C., Fingar K., Pearson J.A., Curtis M. The role of socioeconomic factors in Black-White disparities in preterm birth. Am J Public Health. 2015;105(4):694–702. doi: 10.2105/AJPH.2014.302008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke L.E., Sereika S.M., Music E., Warziski M., Styn M.A., Stone A. Using instrumented paper diaries to document self-monitoring patterns in weight loss. Contemp Clin Trials. 2008;29(2):182–193. doi: 10.1016/j.cct.2007.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke L.E., Wang J., Sevick M.A. Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc. 2011;111(1):92–102. doi: 10.1016/j.jada.2010.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butryn M.L., Phelan S., Hill J.O., Wing R.R. Consistent self-monitoring of weight: a key component of successful weight loss maintenance. Obesity (Silver Spring) 2007;15(12):3091–3096. doi: 10.1038/oby.2007.368. [DOI] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Daley A.J., Jolly K., Jebb S.A., Lewis A.L., Clifford S., Roalfe A.K., Kenyon S., Aveyard P. Feasibility and acceptability of regular weighing, setting weight gain limits and providing feedback by community midwives to prevent excess weight gain during pregnancy: randomised controlled trial and qualitative study. BMC Obes. 2015;2(1) doi: 10.1186/s40608-015-0061-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daley A.J., Jolly K., Bensoussane H., Ives N., Jebb S.A., Tearne S., Greenfield S.M., Yardley L., Little P., Tyldesley-Marshall N., Pritchett R.V., Frew E., Parretti H.M. Feasibility and acceptability of a brief routine weight management intervention for postnatal women embedded within the national child immunisation programme in primary care: randomised controlled cluster feasibility trial. Trials. 2020;21(1) doi: 10.1186/s13063-020-04673-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daley A.J., Jolly K., Ives N., Jebb S.A., Tearne S., Greenfield S.M., Yardley L., Little P., Tyldesley-Marshall N., Bensoussane H., Pritchett R.V., Frew E., Parretti H.M. Practice nurse-supported weight self-management delivered within the national child immunisation programme for postnatal women: a feasibility cluster RCT. Health Technol. Assess. 2021;25(49):1–130. doi: 10.3310/hta25490. [DOI] [PubMed] [Google Scholar]
- Davis E.M., Abebe K.Z., Simhan H.N., Catalano P., Costacou T., Comer D., Orris S., Ly K., Decker A., Mendez D., Day N., Scifres C.M. Perinatal outcomes of two screening strategies for gestational diabetes mellitus: A randomized controlled trial. Obstet. Gynecol. 2021;138(1):6–15. doi: 10.1097/AOG.0000000000004431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder T.E., Goddeeris J.H., Haider S.J. Racial and ethnic infant mortality gaps and the role of socio-economic status. Labour Econ. 2016;43:42–54. doi: 10.1016/j.labeco.2016.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endres L.K., Straub H., McKinney C., Plunkett B., Minkovitz C.S., Schetter C.D., Ramey S., Wang C., Hobel C., Raju T., Shalowitz M.U. Postpartum weight retention risk factors and relationship to obesity at 1 year. Obstet. Gynecol. 2015;125(1):144–152. doi: 10.1097/AOG.0000000000000565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fealy S., Davis D., Foureur M., Attia J., Hazelton M., Hure A. The return of weighing in pregnancy: A discussion of evidence and practice. Women Birth. 2020;33(2):119–124. doi: 10.1016/j.wombi.2019.05.014. [DOI] [PubMed] [Google Scholar]
- Ferrey A.E., Astbury N.M., Kenworthy Y., Mackillop L., Frie K., Jebb S.A. Exploring women's thoughts on self-weighing during pregnancy: results of the Self-Weighing in Pregnancy: Experiences (SWIPE) study. BMC Pregnancy Childbirth. 2021;21(1):154. doi: 10.1186/s12884-021-03636-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford C.L., Airhihenbuwa C.O. The public health critical race methodology: praxis for antiracism research. Soc. Sci. Med. 2010;71(8):1390–1398. doi: 10.1016/j.socscimed.2010.07.030. [DOI] [PubMed] [Google Scholar]
- Gavin K.L., Linde J.A., Pacanowski C.R., French S.A., Jeffery R.W., Ho Y.Y. Weighing frequency among working adults: cross-sectional analysis of two community samples. Prev. Med. Rep. 2015;2:44–46. doi: 10.1016/j.pmedr.2014.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn S.L., Pacanowski C.R., Loth K.A., Miller J., Eisenberg M.E., Neumark-Sztainer D. Self-weighing among young adults: who weighs themselves and for whom does weighing affect mood? A cross-sectional study of a population-based sample. J. Eat Disord. 2021;9(1):37. doi: 10.1186/s40337-021-00391-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison C.L., Teede H.J., Lombard C.B. How effective is self-weighing in the setting of a lifestyle intervention to reduce gestational weight gain and postpartum weight retention? Aust. N. Z. J. Obstet. Gynaecol. 2014;54(4):382–385. doi: 10.1111/ajo.12207. [DOI] [PubMed] [Google Scholar]
- Headen I.E., Davis E.M., Mujahid M.S., Abrams B. Racial-ethnic differences in pregnancy-related weight. Adv Nutr. 2012;3(1):83–94. doi: 10.3945/an.111.000984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Headen I., Mujahid M.S., Cohen A.K., Rehkopf D.H., Abrams B. Racial/ethnic disparities in inadequate gestational weight gain differ by pre-pregnancy weight. Matern Child Health J. 2015;19(8):1672–1686. doi: 10.1007/s10995-015-1682-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hothorn T., Hornik K., Zeileis A. Unbiased recursive partitioning: A conditional inference framework. J. Comput. Graph. Stat. 2006;15(3):651–674. [Google Scholar]
- Huseinovic E., Bertz F., Brekke H.K., Winkvist A. Two-year follow-up of a postpartum weight loss intervention: Results from a randomized controlled trial. Matern Child Nutr. 2018;14(2):e12539. doi: 10.1111/mcn.12539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keppel K.G., Taffel S.M. Pregnancy-related weight gain and retention: implications of the 1990 Institute of Medicine guidelines. Am J Public Health. 1993;83(8):1100–1103. doi: 10.2105/ajph.83.8.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong A., Beresford S.A.A., Imayama I., Duggan C., Alfano C.M., Foster-Schubert K.E., Neuhouser M.L., Johnson D.B., Wang C.-Y., Xiao L., Bain C.E., McTiernan A. Adoption of diet-related self-monitoring behaviors varies by race/ethnicity, education, and baseline binge eating score among overweight-to-obese postmenopausal women in a 12-month dietary weight loss intervention. Nutr Res. 2012;32(4):260–265. doi: 10.1016/j.nutres.2012.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krukowski R., Johnson B., Kim H., Sen S., Homsi R. A pragmatic intervention using financial incentives for pregnancy weight management: feasibility randomized controlled trial. JMIR Form Res. 2021;5(12):e30578. doi: 10.2196/30578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard S.A., Petito L.C., Stephansson O., Hutcheon J.A., Bodnar L.M., Mujahid M.S., Cheng Y., Abrams B. Weight gain during pregnancy and the black-white disparity in preterm birth. Ann Epidemiol. 2017;27(5):323–328. doi: 10.1016/j.annepidem.2017.05.001. e321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linde J.A., Jeffery R.W., Finch E.A., Simon G.E., Ludman E.J., Operskalski B.H., Ichikawa L., Rohde P. Relation of body mass index to depression and weighing frequency in overweight women. Prev Med. 2007;45(1):75–79. doi: 10.1016/j.ypmed.2007.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lohr A.N., Hoppe K.K., Mei C.C., Antony K.M. Does daily self-weighing contribute to postpartum weight loss? A secondary analysis of daily postpartum weights among women with hypertensive disorders of pregnancy. Am J Perinatol. 2023;40(03):319–325. doi: 10.1055/s-0041-1727217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medicine) IIo. Weight Gain During Pregnancy: Reexamining the Guidlines 2009 The National Academies of Press Washington, DC. [PubMed]
- Mendez D.D., Sanders S.A., Karimi H.A., Gharani P., Rathbun S.L., Gary-Webb T.L., Wallace M.L., Gianakas J.J., Burke L.E., Davis E.M. Understanding pregnancy and postpartum health using ecological momentary assessment and mobile technology: protocol for the postpartum mothers mobile study. JMIR Res Protoc. 2019;8(6) doi: 10.2196/13569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nezami B.T., Valle C.G., Nulty A.K., Espeland M., Wing R.R., Tate D.F. Predictors and outcomes of digital weighing and activity tracking lapses among young adults during weight gain prevention. Obesity (Silver Spring) 2021;29(4):698–705. doi: 10.1002/oby.23123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okoro O.N., Hillman L.A., Cernasev A. Intersectional invisibility experiences of low-income African-American women in healthcare encounters. Ethn Health. 2022;27(6):1290–1309. doi: 10.1080/13557858.2021.1899138. [DOI] [PubMed] [Google Scholar]
- Olson C.M., Strawderman M.S., Graham M.L. Association between consistent weight gain tracking and gestational weight gain: Secondary analysis of a randomized trial. Obesity (Silver Spring) 2017;25(7):1217–1227. doi: 10.1002/oby.21873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker J.D., Abrams B. Differences in postpartum weight retention between black and white mothers. Obstet Gynecol. 1993;81(5 (Pt 1)):768–774. [PubMed] [Google Scholar]
- R: A language and environment for statistcal computing [computer program]. Vienna, Austria: R Foundation for Statistical Computing; 2020.
- Ross K.M., Qiu P., You L., Wing R.R. Week-to-week predictors of weight loss and regain. Health Psychol. 2019;38(12):1150–1158. doi: 10.1037/hea0000798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider C.R., Biggio J.R., Chandler-Laney P.C. Association of early pregnancy body mass index with post-partum weight change among African-American women. Clin. Obes. 2018;8(3):170–175. doi: 10.1111/cob.12241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scifres C.M., Abebe K.Z., Jones K.A., Comer D.M., Costacou T., Freiberg M.S., Simhan H.N., Day N.L., Davis E.M. Gestational diabetes diagnostic methods (GD2M) pilot randomized trial. Matern Child Health J. 2015;19(7):1472–1480. doi: 10.1007/s10995-014-1651-4. [DOI] [PubMed] [Google Scholar]
- Shieh C., Knisely M.R., Clark D., Carpenter J.S. Self-weighing in weight management interventions: A systematic review of literature. Obes. Res. Clin. Pract. 2016;10(5):493–519. doi: 10.1016/j.orcp.2016.01.004. [DOI] [PubMed] [Google Scholar]
- Shieh C., Yang Z., Haas D.M., Carpenter J.S. Feasibility and potential benefits of a self-monitoring enhanced lifestyle intervention to prevent excessive gestational weight gain in women who are overweight or obese. J. Obstet. Gynecol. Neonatal. Nurs. 2017;46(2):182–196. doi: 10.1016/j.jogn.2016.09.006. [DOI] [PubMed] [Google Scholar]
- Shiffman S., Stone A. In: Technology and Methods in Behavioral Medicine. Kratz D., Baum A., editors. Erlbaum; Philadelphia: 1998. Ecological momentary assessment: A new tool for behavioral medicine research; pp. 117–132. [Google Scholar]
- Siega-Riz A.M., Herring A.H., Carrier K., Evenson K.R., Dole N., Deierlein A. Sociodemographic, perinatal, behavioral, and psychosocial predictors of weight retention at 3 and 12 months postpartum. Obesity (Silver Spring) 2010;18(10):1996–2003. doi: 10.1038/oby.2009.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg D.M., Tate D.F., Bennett G.G., Ennett S., Samuel-Hodge C., Ward D.S. The efficacy of a daily self-weighing weight loss intervention using smart scales and e-mail. Obesity (Silver Spring) 2013;21(9):1789–1797. doi: 10.1002/oby.20396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg D.M., Bennett G.G., Askew S., Tate D.F. Weighing every day matters: daily weighing improves weight loss and adoption of weight control behaviors. J. Acad. Nutr. Diet. 2015;115(4):511–518. doi: 10.1016/j.jand.2014.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone A., Shiffman S. Ecological momentary assessment (EMA) in behavioral medicine. Ann. Behav. Med. 1994;16:199–202. [Google Scholar]
- Stone A., Shiffman S., Atienza A., Nebeling L. Oxford University Press; New York: 2007. The Science of Real-time Data Capture: Self-reports in Public Health. [Google Scholar]
- Vuorinen A.L., Helander E., Pietila J., Korhonen I. Frequency of self-weighing and weight change: Cohort study With 10,000 smart scale users. J. Med. Internet Res. 2021;23(6):e25529. doi: 10.2196/25529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitaker K., Young-Hyman D., Vernon M., Wilcox S. Maternal stress predicts postpartum weight retention. Matern. Child Health J. 2014;18(9):2209–2217. doi: 10.1007/s10995-014-1470-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R. Race, socioeconomic status, and health. The added effects of racism and discrimination. Ann. N Y Acad. Sci. 1999;896:173–188. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- Williams D.R., Gonzalez H.M., Williams S., Mohammed S.A., Moomal H., Stein D.J. Perceived discrimination, race and health in South Africa. Soc. Sci. Med. 2008;67(3):441–452. doi: 10.1016/j.socscimed.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang M., Yue W., Han X., Hu C., Sun X., Luo J. Postpartum care indications and methodological quality:a systematic review of guidelines. Z. Gesundh Wiss. 2021:1–15. doi: 10.1007/s10389-021-01629-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu Y., Ma Q., Fernandez I.D., Groth S.W. Mental health, behavior change skills, and eating behaviors in postpartum women. West J. Nurs. Res. 2022;44(10):932–945. doi: 10.1177/01939459211021625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng Y., Klem M.L., Sereika S.M., Danford C.A., Ewing L.J., Burke L.E. Self-weighing in weight management: a systematic literature review. Obesity (Silver Spring) 2015;23(2):256–265. doi: 10.1002/oby.20946. [DOI] [PubMed] [Google Scholar]
- Zheng Y., Burke L.E., Danford C.A., Ewing L.J., Terry M.A., Sereika S.M. Patterns of self-weighing behavior and weight change in a weight loss trial. Int. J. Obes. (Lond). 2016;40(9):1392–1396. doi: 10.1038/ijo.2016.68. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that has been used is confidential.