Introduction
First described by Burns in 1915, keratitis-ichthyosis-deafness (KID) syndrome was later characterized and named by Skinner et al in 1981.1 KID syndrome is a rare ectodermal dysplasia (OMIM #148210). It is caused by heterozygous missense mutations on the connexin-26 gene gap junction beta-2 protein (GJB2) and connexin-30 gene gap junction beta-6 protein.2 The mutations cause a disturbance in the gap junction system which may affect epithelial homeostasis, differentiation, immune response, and carcinogenesis in ectodermal epithelia.2
Follicular occlusion occurs in a number of diseases, most notably acne. It is also the connecting sign of follicular occlusion triad (co-occurrence of hidradenitis suppurativa [HS], cystic acne, and dissecting cellulitis of the scalp) and tetrad (triad + pilonidal sinus disease).3
The association of HS and KID syndrome has been reported in 6 cases, 4 of which exhibited the triad by also presenting with cystic acne and dissecting cellulitis of the scalp (Table I).4
Table I.
Associated features of keratitis-ichthyosis-deafness and hidradenitis suppurativa in literature
| Reference | KID-cutaneous features | KID-systemic features | HS | Additional features of follicular occlusion and skin disease | Genetic mutation |
|---|---|---|---|---|---|
| Current case | Dystrophic nails, follicular hyperkeratosis | Congenital sensorineural hearing loss | Axillary—Hurley Stage III | Severe cicatricial cystic acne, pilonidal cyst, recurrent abscess on posterior neck, keratosis pilaris, acanthosis nigricans, severe atopic dermatitis | Heterozygous missense mutation, 32 G to A transition of exon 2 on GJB2 gene |
| Bettoli et al11 | Palmoplantar keratoderma, widespread scales, fingernail and toenail dystrophy, hyperkeratotic plaque of the scalp | Congenital sensorineural bilateral hearing loss | Recurrent inguinal abscesses starting in adolescence, at age 39 developed nodules, abscesses, and fistulas in genital and groin areas | None | D50N on GJB2 gene |
| Maintz et al12 | Ichthyosis, transgrediens palmoplantar keratoderma, fine hyperkeratosis and erythrokeratoderma of the hips and thighs, Toenail dystrophy | Congenital sensorineural deafness, vascularizing keratitis | Abscesses in axillae and groin | Dissecting cellulitis of the scalp with cicatricial alopecia, acne conglobata | Heterozygous missense mutation D50N on GJB2 gene |
| Nyquist et al13 | Patient 1—dry skin, palmoplantar keratoderma with 'stippled' appearance | Bilateral sensorineural hearing loss, photophobia, corneal vascularization | Groin | Dissecting cellulitis of the scalp with diffuse scarring alopecia, cystic acne, multiple epidermal cysts, moderately differentiated SCC with metastatic tumor nests in 2 inguinal lymph nodes, primary malignant proliferating pilar tumor (PPT) with metastatic spread | Heterozygous missense mutation D50N on GJB2 gene |
| Prasad and Bygum14 | Red and dry skin since birth, red-brown hyperkeratotic plaques on face and extremities, and sparse hair | Congenital sensorineural deafness | Axillary and groin | Dissecting cellulitis of the scalp, cystic acne | Heterozygous missense mutation D50N (148 G>A) in GJB2 |
| Montgomery et al10 | Mild palmoplantar keratoderma, ichthyosis, follicular hyperkeratosis, leukonychia without nail pitting | Congenital deafness, mild keratitis, Leukonychia | Axillae, suprapubic, inguinal and intergluteal areas—interconnected draining sinuses surrounded by macerated nearly verrucous hyperkeratotic skin | Dissecting folliculitis of the scalp with extensive scarring, chronically recurrent cystic acne on face and torso starting at 5 y of age | Novel heterozygous point mutation (C119T) A40V on GJB2 gene |
| Lazic et al6 | Palmoplantar keratoderma, 20-nail dystrophy, gingival swelling, hyperemia and chronic lip fissuring, soft pedunculated papules on buccal mucosa and lateral edges of tongue | Congenital sensorineural deafness, photophobia, corneal abrasions, scarring, vascularizing keratitis, keratoconjunctivitis sicca. | Recurrent sterile abscesses with sinus tracts and scarring in the axillae, mons pubis and submammary folds. | Dissecting cellulitis of the scalp with diffuse scarring alopecia, partial eyebrow and eyelash alopecia, complete axillary and pubic alopecia, and porokeratotic eccrine ostial and dermal duct nevus (PEODDN), atopic dermatitis | G12R mutation on the GJB2 gene |
HS, Hidradenitis suppurativa; KID, keratitis-ichthyosis-deafness; SCC, squamous cell carcinoma. Adapted from Bettoli et al (2021). KID and HS association features in the literature. Skin Appendage Disord. https://doi.org/10.1159/000509042.
Case
A 33-year-old male with a history of HS, cystic acne, pilonidal sinus treated surgically, and acanthosis nigricans since the onset of puberty was referred to Department of Dermatology, Zealand University Hospital for diagnosis and treatment at 22 years of age. He had no family history of HS on the maternal branch and no contact with the paternal branch of his family, was overweight (body mass index of 42.4), and smoked. His worst affected area (axillae) reached Hurley stage III with a modified Sartorius score of 59. Other clinical features included keratosis pilaris of his back and limbs, keratotic spiny papules (more white and without inflammation as compared with keratosis pilaris), dystrophic nails, congenital hearing loss, and scoliosis (Fig 1). Patient history further revealed that he had keratitis in childhood, and was currently being treated for blepharitis. He had had multiple hospital admissions for treatment of severe atopic dermatitis with fungal and bacterial skin infections. Jobs syndrome was ruled out by normal serum-IgE.
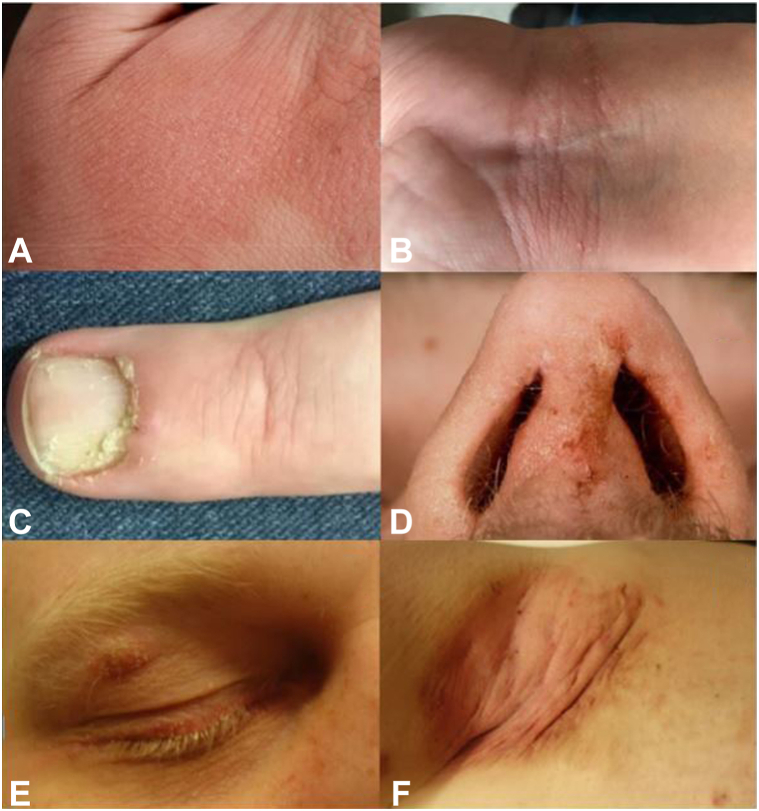
Fig 1.
Pictures of our patient’s dermatological findings associated with keratitis-ichthyosis-deafness syndrome. A and B, Lichenified eczematous patches on the dorsal hand and wrist—possible ichthyosis. C, Nail dystrophy. D,Staphylococcus colonization. E, Inflamed cyst on the right eyelid with overlying impetiginization. F, Acanthosis nigricans.
Images sourced from Zealand University Hospital, Roskilde, Denmark.
The patient was referred for genetic evaluation and sequencing analysis was performed using the Sanger method. A heterozygous 32G->A transition of exon 2 in the GJB2 gene was found: GJB2, NM_004004.5 c.32G>A, p.Gly11Glu. The missense variant p.Gly11Glu has previously been described as an autosomal dominant form of KID syndrome.5
During childhood and adolescence, our patient had numerous skin infections with Staphylococcus aureus and Candida and had recurrent pneumonia. During his treatment at our institution, he was treated for the skin infections with topical fucidin acid and oral dicloxacillin, amoxicillin-clavulanic acid, and tetracyline.
For the recalcitrant and progressive HS, he was treated with isotretinoin 20 to 40 mg daily for 1.5 years but developed worsening xerosis, dryness of the lips, blepharitis, and cheilitis. Due to these side effects, the dosage was decreased to 20 mg every other day. Metformin was given at a higher than normal dosage of 1g twice a day, combined with topical resorcinol and surgery (pilonidal cyst excision, deroofing, and CO2 laser).
At 30 years of age, our patient was treated for nodular lymphocyte-predominant Hodgkin lymphoma and was also subsequently diagnosed with a microadenoma of the pituitary gland causing pituitary gland dysfunction. He developed a recurrent abscess on his upper back, after the lymphoma treatment was discontinued. The patient was not a candidate for adalimumab because of his history of Hodgkin lymphoma.
Discussion
Syndromes may provide a serendipitous insight into the genetic background of co-occurring diseases. KID syndrome was originally defined by the features implied by the acronym: keratitis causing visual impairment, with fine scale, ichthyosis, and deafness (OMIM #148210). However, this has since been challenged as the skin lesions appear more lichenified than scaly and are therefore not true ichthyoses, hearing loss is only partial, and keratitis develops with a late onset. Furthermore, the usual presentation of KID syndrome includes a variety of symptoms absent in the acronym: erythrokeratoderma, corneal vascularization, photophobia, recurrent bacterial and fungal infections, dystrophic nails, dental abnormalities, and susceptibility to squamous cell carcinomas and other mucocutanous tumors.6,7 Patients with KID syndrome have an increased rate of malignancies, the most common being squamous cell carcinoma. Additionally, KID syndrome has been grouped with other cancer-associated genodermatoses including Cowden syndrome, Gorlin syndrome, and xeroderma pigmentosum.8
KID syndrome is caused by connexin-26 gene (GJB2) mutations.5 Connexin is a 4-pass transmembrane protein involved in the assembly of gap junctions and intercellular communication.9 Connexins have typically been regarded as tumor suppressive proteins. The finding of increased expression and membrane localization of connexins, including connexin-26 (Cx26), in metastases appears relevant.9 There are several reports of Cx26 abnormalities in different internal malignancies such as breast, lung, prostate, colorectal and hepatic cancer. It is unknown if our patient’s nodular lymphocyte-predominant Hodgkin lymphoma is related to his Cx26 mutation.
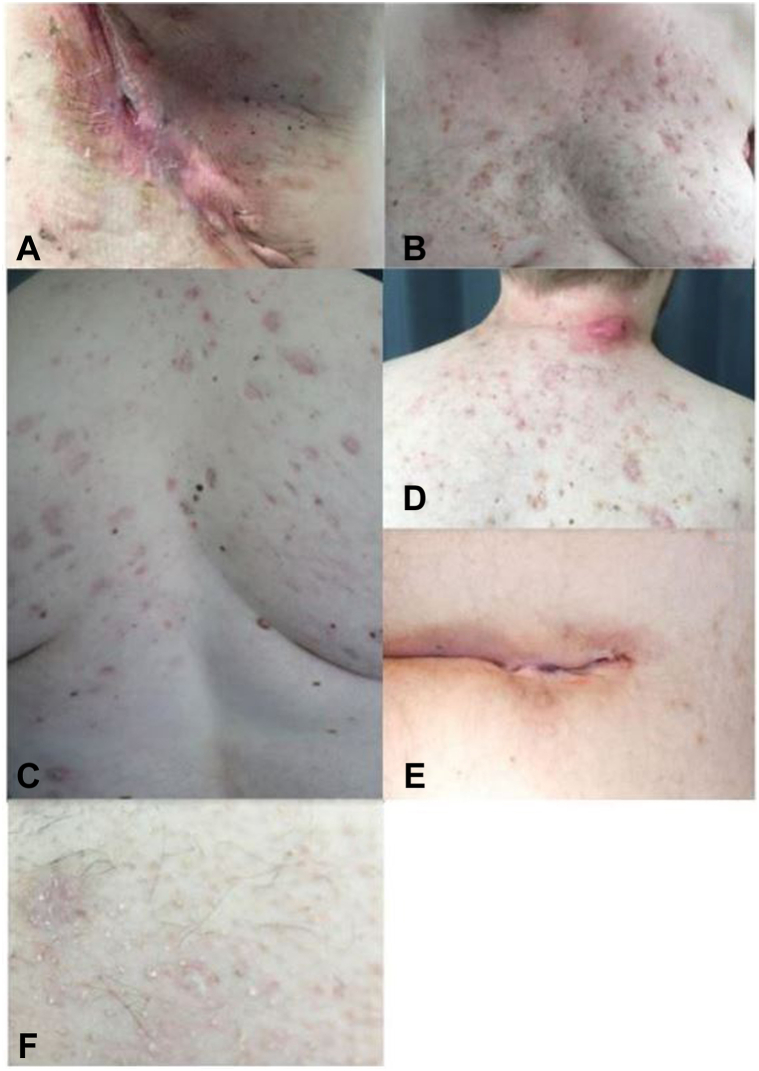
Multiple epithelial organs including hair follicles, palmoplantar epidermis, sweat glands and ducts, and cochlea have gap junctions which are formed by Cx26. The hyperproliferative tendency of the epidermis of patients with KID syndrome may contribute to follicular plugging with subsequent cyst formation, rupture, and an inflammatory response seen in HS and the follicular occlusion disorders.10 Although previous cases have shown variants in Asp50, Ala40, and Gly12 associated with KID syndrome and HS, further studies must be conducted to determine if they play a role in Cx26 function. Our patient has KID syndrome and 3 of the 4 diagnoses of the follicular occlusion tetrad; HS, acne conglobata, and pilonidal disease but not dissecting cellulitis of the scalp. He further presented with keratotic spiny papules on his trunk and upper arms, as shown in Fig 2. In another reported case of KID syndrome with a GJB2 connexin 26 mutation, the patient developed yellow keratotic spiny papules at the age of 15. This patient was diagnosed with porokeratotic eccrine ostial and dermal duct nevus from biopsies of 3 sites.4 She was also diagnosed soon after with HS and had a history of atopic dermatitis, similar to our patient. In summary, this case provides further evidence of the link between KID syndrome and follicular occlusion. The co-occurrence of 2 rare clinical presentations that both link with connexin mutations and the finding of similar mutations in HS implies a new genetic venue for further studies of HS.
Fig 2.
Pictures of our patient’s clinical characteristics consistent with follicular occlusion. A, Hidradenitis suppurativa of the left axillae. B and C, Cystic acne and subsequent scarring. D, Recurrent abscess on the right posterior neck. E, Pilonidal sinus. F, Follicular spiny papules on the back.
Images sourced from Zealand University Hospital, Roskilde, Denmark.
Conflicts of interest
None disclosed.
Acknowledgments
Mathias Vig Jakobsen, MD, participated in the early collection of data for this manuscript.
Footnotes
Authors Jemec and Saunte shared senior authorship.
Funding sources: None.
IRB approval status: Not applicable.
Patient consent: Consent was obtained for the publication of all patient photographs and medical information to be published in print and online, with the understanding that the information may be publicly available.
References
- 1.Skinner B.A., Greist M.C., Norins A.L. The keratitis, Ichthyosis, and deafness (KID) syndrome. Arch Dermatol. 1981;117:285. [PubMed] [Google Scholar]
- 2.Gaspris J., Riis Theut P., Jemec G.B. Recognizing syndromic hidradenitis suppurativa: a review of the literature. J Eur Acad Dermatol Venereol. 2017;31:1809–1816. doi: 10.1111/jdv.14464. [DOI] [PubMed] [Google Scholar]
- 3.Jemec G.B.E. Hidradenitis suppurativa. N Engl J Med. 2012;366(2):158–164. doi: 10.1056/NEJMcp1014163. [DOI] [PubMed] [Google Scholar]
- 4.Lazic T., Li Q., Frank M., Uitto J., Zhou L.H. Extending the phenotypic spectrum of keratitis-ichthyosis-deafness syndrome: report of a patient with GJB2(G12R) connexin 26 mutation and unusual clinical findings. Pediatr Dermatol. 2012;29(3):349–357. doi: 10.1111/j.1525-1470.2011.01425.x. [DOI] [PubMed] [Google Scholar]
- 5.Terrinoni A., Codispoti A., Serra V., et al. Connexin 26 (GJB2) mutations as a cause of the KID syndrome with hearing loss. Biochem Biophys Res Commun. 2010;395(1):25–30. doi: 10.1016/j.bbrc.2010.03.098. [DOI] [PubMed] [Google Scholar]
- 6.Lazic T., Horii K.A., Richard G., Wasserman D.I., Antaya R.J. A report of GJB2 (N14K) connexin 26 mutation in two patients - a new subtype of KID syndrome? Pediatr Dermatol. 2008;25(5):535–540. doi: 10.1111/j.1525-1470.2008.00767.x. [DOI] [PubMed] [Google Scholar]
- 7.Coggshall K., Farsani T., Ruben B., et al. Keratitis, ichthyosis, and deafness (KID) syndrome: a review of infectious and neoplastic complications. J Am Acad Dermatol. 2013;69(1):127–134.e3. doi: 10.1016/j.jaad.2012.12.965. [DOI] [PubMed] [Google Scholar]
- 8.Brose M.S., Smyrk T.C., Weber B., Lynch H.T. In: Holland-Frei cancer medicine. 6th ed. Kufe D.W., Pollack R.E., Weichselbaum R.R., et al., editors. BC Decker Inc; 2003. Cancer-associated genodermatoses. [Google Scholar]
- 9.Wu J.I., Wang L.-H. Emerging roles of gap junction proteins connexins in cancer metastasis, chemoresistance and clinical application. J Biomed Sci. 2019;26(8) doi: 10.1186/s12929-019-0497-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Montgomery J.R., White T.W., Martin B.L., Turner M.L., Holland S.M. A novel connexin 26 gene mutation associated with features of the keratitis-ichthyosis-deafness syndrome and the follicular occlusion triad. J Am Acad Dermatol. 2004;51(3):377–382. doi: 10.1016/j.jaad.2003.12.042. [DOI] [PubMed] [Google Scholar]
- 11.Bettoli V., Forconi R., Pezzini I., et al. KID syndrome and hidradenitis suppurativa: a rare association responding to surgical treatment. Skin Appendage Disord. 2021;7(1):21–24. doi: 10.1159/000509042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maintz L., Betz R.C., Allam J.P., et al. Keratitis-ichthyosis-deafness syndrome in association with follicular occlusion triad. Eur J Dermatology. 2005;15(5):347–352. [PubMed] [Google Scholar]
- 13.Nyquist G.G., Mumm C., Grau R., et al. Malignant proliferating pilar tumors arising in KID syndrome: a report of two patients. Am J Med Genet A. 2007;143A(7):734–741. doi: 10.1002/ajmg.a.31635. [DOI] [PubMed] [Google Scholar]
- 14.Prasad S.C., Bygum A. Successful treatment with alitretinoin of dissecting cellulitis of the scalp in keratitis-ichthyosis-deafness syndrome. Acta Derm Venereol. 2013;9(4):473–474. doi: 10.2340/00015555-1499. [DOI] [PubMed] [Google Scholar]