Abstract
Objective: This study explored cancer caregivers' individual and communal coping through their use of personal and communal pronouns during naturally occurring conversations. Methods: Nurse-home hospice visits involving cancer patients and their partner caregivers were audio recorded and then transcribed. Pronoun use was analyzed using Linguistic Inquiry Word Count (LIWC) software and descriptive statistics compared patient and partner caregivers' pronoun use. Personal and communal pronoun use was examined within six identified topics of caregiver speech: patient medical care, daily life, emotion, criticism/disagreement, relationships with family/friends, and asserting needs. Results: Dyads (N = 76) had an average of 35.8 years in their relationship. Caregivers used proportionately more first-person singular (I-talk) than first-person plural (we-talk). However, they used significantly less I-talk than patients and less I-talk than LIWC measures in naturally occurring speech. Caregivers were most likely to discuss patient medical care (41.9%) and least likely to discuss their own needs (3.8%). Conclusion: Partner caregivers may find it easier to express emotions related to communal stressors, rather than their individual ability to cope with end-of-life caregiving. Innovation: Examining personal and communal pronoun use by partner caregivers during nurse-home hospice visits may provide a more objective measure of caregiver coping than standard self-report measures.
Keywords: cancer, Caregiving, Communication, Communal coping, Personal agency, Pronoun use
Highlights
-
•
Pronoun use (I, we) may indicate individual and dyadic coping.
-
•
Partner caregivers used less I-talk than cancer patients in hospice visits.
-
•
Partners were least likely to discuss their own needs.
1. Introduction
Caregivers of hospice patients with cancer are more likely to be a spouse or partner than other types of caregivers, [1,2]. This can place a great deal of emotional and physical strain on the partner who is often tasked with caregiving after little or no training [1]. Caregivers of hospice patients with cancer report high levels of depression and anxiety [3] which can lead to negative bereavement adjustment [4]. In fact, 50% of hospice cancer caregivers reported clinically significant symptoms of depression one year after the death of their family member [5]. Further placing cancer caregivers at risk of negative psychological outcomes is the fact that only 29% report being asked about their self-care needs [1].
One way to assess hospice cancer caregivers' wellbeing and needs is through communal coping. The theory of communal coping suggests that individuals faced with a stressor—such as life-limiting cancer—appraise their situation as a shared responsibility and develop collaborative ways to address the stressor [6,7]. Communal coping is associated with higher relationship quality, lower stress, and better psychological and physical wellbeing for couples facing cancer [8,9]. However, research into communal coping during palliative or hospice care is sparse [9] and often requires participants to self-report information, which may introduce bias [10].
Examining couples' use of pronouns in natural conversation may provide a more objective measure of communal coping [11,12]. Previous research has found that among couples facing chronic illness, greater “we-talk” is associated with more benefit-finding [11], and better relationship quality [13], psychological well-being [14] [6] and illness specific self-care [15,16].
However, when care demands increase and the health of an individual with cancer declines, a communal approach to managing cancer may no longer be realistic. As cancer progresses, hospice patients can experience greater distress and symptoms [17] as well as a decreased ability to communicate [18]. As the patient's health declines, a formerly shared sense of responsibility may fall more towards the caregiver who must manage the patient's end-of-life care as well as their own anticipated grief. Examining the context of pronoun-use may help better understand the complexities of using pronouns as a proxy measure of communal and individual coping.
For example, a caregiver's use of we-talk may indicate better communal coping in some conversations (when discussing how the couple manages the patient's everyday needs for example) while their use of I-talk may reflect better individual coping in other contexts (such as when the hospice patient is no longer communicative). Dyadic interventions involving the hospice cancer patient and the caregiver are more likely to target caregivers' wellbeing than traditional patient-centric interventions, but many of these interventions have no significant benefit for partner caregivers [19]. Thus, even dyadic interventions may leave little room for the caregiver to attend to their own personal needs as the patient nears the end of life. Just as the use of we-talk can reflect communal coping [11], the use of I-talk may reflect hospice caregivers' individual coping, including their ability to identify and voice their personal needs. Therefore, examining pronoun use during nurse home hospice visits might aid in understanding communal coping as well as caregivers' individual ability to express needs and cope with their caregiving situation. Ultimately, this greater understanding can lead to better support of couples receiving hospice cancer care, as well as improved outcomes for hospice cancer caregivers.
1.1. Study purpose
Given the potential negative consequences of hospice cancer caregiving, the lack of current research on communal coping at the end of life and caregivers' use of “I-talk”, there is a need to address caregivers' ability to express needs as their partner nears death. The purpose of this study was to explore cancer caregivers' individual and communal coping through examining personal and communal pronouns utilized in naturally occurring conversation. The objectives included: 1) Describe the frequency and proportion of pronoun use by cancer patients and partner caregivers during nurse home hospice visits as an indicator of individual and communal coping; 2) Describe the most frequently discussed topics of caregiver conversations during nurse home hospice visits; and 3) Examine caregiver pronoun use within these identified topics to describe caregivers' coping and ability to assert needs.
2. Methods
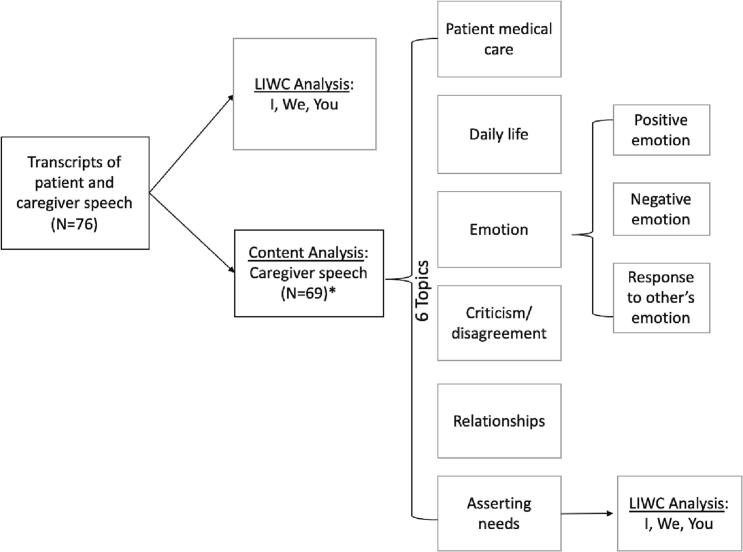
As part of a secondary data analysis of a multi-site prospective observational longitudinal study, we examined audio recordings from hospice nurses' home visits with cancer patients and their partner caregivers (N = 76). (See Fig. 1 for the study design of this secondary analysis.) Partner caregivers were defined as the patient's significant other who was involved in some aspect of their care. All procedures were approved by the University of Utah Institutional Review Board (IRB # 00088662) and by all home hospice agencies. Nurses and participating dyads provided written consent prior to any study procedures. Nurses also reminded dyads before beginning to record the home hospice visits.
Fig. 1.
Study Design.
This figure depicts the different components involved in the study including the LIWC analysis and content analysis. It then shows how further LIWC analysis was performed on the pronouns identified in the topic “asserting needs”. ⁎7 transcripts were excluded for content analysis as they contained no caregiver speech.
2.1. Sample
Home hospice nurses were recruited from participating hospice agencies. Patient-caregiver dyads were recruited through participating nurse caseloads. From the larger parent project (P01CA138317; PI Mooney), we selected partner caregivers of individuals with a cancer diagnosis receiving home hospice [20]. Inclusion criteria for partner caregivers included being 45 years or older, English-speaking, and cognitively able to participate in all study procedures. In our sample, all couples were heterosexual and were living as married or legally married. Enrollment began in August 2011 and was completed by December 2014. Participating hospices were located in the Intermountain West (8) and in the Northeast (2).
2.2. Procedures and data sources
For a more detailed description of study methods see the parent study [20]. Upon study enrollment, nurses were provided digital recorders, trained in their use, and then asked to audio-record all home hospice visits with participating dyads. Nurses received reminders of scheduled visits with participating dyads to ensure they remembered to record. Audio recordings began with nurses identifying themselves, the patient's initials, and stating the date. Nurses reminded patient-caregiver dyads that the visit was being recorded and that the digital recorder could be turned off at any time.
Of note, nurses were asked to record their interactions with hospice cancer patients and caregivers due to their consistent presence in home hospice care. It is possible that asking nurses to record home hospice visits may have been beneficial for assessing individual and communal coping given that nurses are often viewed as the most trustworthy profession [21]. Conversely, nurses' primary objective is to provide medical care and support and their clinical focus may have impeded their ability to engage in conversation related to topics such as communal and individual coping.
After nurse home hospice visits were recorded, the recording devices were collected by study staff and visit recordings were uploaded to a secure server. Each recording was transcribed verbatim to list individual speakers such as nurse, patient, caregiver, and other family members present. Once transcribed, all transcripts were reviewed and speech from patients and caregivers was aggregated separately into two independent documents. Transcripts were reviewed by study staff who verified that all the language from each transcript had been included. Transcripts were then cleaned by removing any identifying information and non-speech. Transcripts were reviewed again by study staff to verify that each document had been cleaned.
Verified transcripts were imported into Linguistic Inquiry Word Count (LIWC), a computerized word pattern analysis program that uses word count strategies based on the supposition that an individual's word choice not only delivers a literal meaning, but also communicates psychological information [22]. LIWC utilizes language categories to analyze written material or transcribed speech. Pennebaker and colleagues, the developers of LIWC, suggest that personal pronouns are more resistant than other nouns and verbs to conscious word choice [23]. Personal pronouns may therefore serve as better markers of fundamental psychosocial processes such as emotional states, cognitive styles, and social identity [10].
2.3. Variables
Demographic data collected from partner caregivers of hospice recipients included gender, ethnicity, race, employment status, education, religious affiliation, annual household income, primary insurance, marital status, age, and length of relationship. Information about hospice enrollment, the number of days on hospice, and the patient's date of death were extracted from hospice records by trained staff. In addition, after study completion, caregivers and nurses rated their comfort with recording the hospice visit and the degree it affected the interaction. First-person singular (I, me, my), plural (we, us, our) and second-person (you, your) pronouns were extracted from transcripts using LIWC [23] and NVivo 12 software [24].
2.4. Analysis
2.4.1. Descriptive analysis
LIWC software and descriptive statistics were used to compare patient and partner caregiver pronoun use as a way to assess communal coping and caregivers' coping and ability to express needs during home hospice visits. LIWC produced separate tallies of all pronoun types utilized by the patient and their partner caregiver throughout each recording. Descriptive statistics were used to analyze demographic data and visit characteristics, and to summarize LIWC pronoun use. A text processing feature of LIWC resulted in a count of all the words used in a transcript that fit in each category of pronoun. The use of first-person singular (I, me, my), plural (we, us, our) and second-person (you, your) pronouns was operationalized as an indicator of focus on self, communal, or other. Chi-square analyses were conducted to examine the differences in self, communal, and other pronoun use between patients and partner caregivers.
2.4.2. Content analysis
To examine caregivers' coping and ability to express needs during home hospice visits, only caregivers' speech was utilized in our qualitative content analysis. Transcripts were coded using a combination of deductive and inductive approaches. The coders utilized previous literature to form the following initial overarching categories: health-related issues, psychological processes, and social/interpersonal processes [14]. Within each of these categories were sub-categories of topics relevant to patient-caregiver discussion during home hospice visits. For example, the theme of patient medical care was comprised of caregiver challenges, physical symptoms, medical decisions, and coordinating care [14].
Using these categories and sub-categories, a random sample of five transcripts were coded by three independent coders (SB, MH, SH) [14]. Coders met to compare categories, collapse similar categories, remove unused categories, and then developed a codebook with definitions and exemplar quotes for each category (Table 1). Additional categories arose spontaneously during data analysis. The categories included: patient medical care, daily life, emotion (e.g., positive emotion such as appreciation, negative emotion such as distress, and response to another's emotion), criticism/disagreement, relationships with family/friends, and asserting needs.
Table 1.
Topic definitions and exemplar quotes.
| Code | Definition | Examples |
|---|---|---|
| Patient medical care | Caregiver identifies medical questions or medical issues i.e. physical symptoms, problem-solving medical issues, medical decision-making, & the dyad's interaction with other healthcare providers. | “Maybe we are ready for a wheelchair” “No, she never had headaches” “She had some bloodwork done yesterday” |
| Positive emotion | Caregiver expresses optimism, love, gratitude, solidarity, or compliments others. | “You're pretty wonderful” “We have been blessed” |
| Response to another's emotion | Caregiver responds to other people's emotions with support, reassurance, empathy, concern, legitimizing, and/or negotiating. | “Those are some pretty good guidelines” “That's a great way to get rid of it” |
| Distress | Caregiver expresses feelings of distress, worries, unease, etc.; can be related to patient wants/needs | “I don't know if I can stand this” “Drives me crazy to sit here” “It's very sad for me” |
| Relationships with family & friends | Caregiver discusses relationships with dyad, family, and other social relationships. | “I don't want to be the overbearing grandparent. But I just wanna be with him 24/7” |
| Lifestyle | Caregiver engages in casual conversation including weather, pets, small talk, and plans that do not fall under other categories. | “Someday it's going to warm up” “I have no idea how to take care of his cactus.” “So these cats, I actually put a little leash on them” |
| Criticism/Disagreement | Caregiver engages in criticism or blame of another or justification/defending of self | “Just carried an attitude with him” “She simply didn't seem to have knowledge of anything she was doing” |
| Asserting needs | Caregiver asserts needs concerning patient care, employment, health care, time, support. | “I have to clean the house, make the food” “I have also missed so many days of work this year that I will be doing some work through the summer” |
Using this codebook, each transcript was coded using NVivo 12 software. Ten-percent of transcripts (n = 7) were randomly selected for coding by three doctoral student coders (SB, MH, SH) and one bachelor's student coder (collaborating with MH), and were assessed for coder drift [25]. Codes were defined by speaker turn and topic of conversation. For example, if a caregiver switched from discussing one topic to another while speaking, each topic was tallied separately. If a caregiver continued to discuss a topic in more than one sentence, this was counted as one code until either the speaker or the topic changed.
To prevent overlapping codes, and keeping in mind the objective of assessing caregiver's ability to express needs, coding rules were developed in which caregivers expressing needs superseded the use of all other codes, and caregiver emotions took priority over other coding categories. In intercoder agreement checks, discrepancies were addressed by a majority vote (if three out of four coders agreed). After all transcripts were coded, NVivo 12 software was used to perform text searchers for counts of pronouns used within each topic of conversation. (See Table 2 for a complete list of search terms.)
Table 2.
Complete list of pronouns searched for using NVivo 12.
| Self | Other | Communal |
|---|---|---|
| I, I'd, I'll, I'm, I've, id, me, mine, my, myself | You, U, Ur, Y'all, You'd, You'll, You're, You've, You'd, You'll, Your, Youre, Yours, Yourself, Yourselves, You've | Let's, lets, our, ours, ourselves, us, we, we'd, we'll, we're, we've, weve |
3. Results
3.1. Demographics
Our study sample consists of 76 patient-partner caregiver dyads with 35.8 average years in their relationship. The majority of partner caregivers were female (59.2%) and slightly younger than patients (M = 64.7 vs. 67.4). The majority of patients were male (59.2%). Partner caregivers were primarily white (96.1%) and had an associate's degree or higher (74.4%). Forty-two (55.3%) caregivers reported their health as very good (on a scale from very poor to excellent) and six (7.9%) reported their health as excellent. (See Table 3 for demographics.)
Table 3.
Participant Characteristics.
| Patient |
Caregiver |
Nurse |
|
|---|---|---|---|
| N = 76 |
N = 76 |
N = 63 |
|
| n(%) | n(%) | n(%) | |
| Gender | |||
| Male | 45 (59.2%) | 30 (39.5%) | 6 (9.4%) |
| Female | 30 (39.5%) | 45 (59.2%) | 58 (90.6%) |
| Missing | 1 (1.3%) | 1 (1.3%) | 1 (1.5%) |
| Ethnicity | |||
| Hispanic | ⎯ | 5 (6.6%) | 1 (1.6%) |
| Non-Hispanic | ⎯ | 69 (90.8%) | 58 (92.1%) |
| Missing | ⎯ | 1 (1.3%) | 4 (6.3) |
| Race | |||
| Asian | ⎯ | 0 (0%) | 4 (6.2%) |
| Black/African American | ⎯ | 1 (1.3%) | 4 (6.2%) |
| White | ⎯ | 73 (96.1%) | 57 (87.7%) |
| Other | ⎯ | 0 (0%) | 1 (1.6%) |
| Education | |||
| HS graduate or equivalent | ⎯ | 17 (22.4%) | ⎯ |
| Associate | ⎯ | 27 (35.5%) | ⎯ |
| Bachelors | ⎯ | 17 (22.4%) | ⎯ |
| Some graduate/professional school | ⎯ | 4 (5.3%) | ⎯ |
| Graduate or professional degree | ⎯ | 10 (13.2%) | ⎯ |
| Religious Affiliation | |||
| Catholic | ⎯ | 13 (17.1%) | 8 (12.5%) |
| Jewish | ⎯ | 2 (2.6%) | 4 (6.3%) |
| Protestant | ⎯ | 7 (9.2%) | 6 (9.4%) |
| Latter Day Saint (LDS) | ⎯ | 31 (40.8%) | 21 (32.8%) |
| Other | ⎯ | 6 (7.9%) | 8 (12.5%) |
| No religious affiliation | ⎯ | 15 (19.7%) | 17 (26.6%) |
| Prefer not to answer | ⎯ | 1 (1.3%) | ⎯ |
| Annual Household Income | |||
| Less than $10,000 | ⎯ | 1 (1.3%) | ⎯ |
| $10,000-24,999 | ⎯ | 11 (14.5%) | ⎯ |
| $25,000-39,999 | ⎯ | 8 (10.5%) | ⎯ |
| $40,000-49,999 | ⎯ | 11 (14.5%) | ⎯ |
| $50,000-74,999 | ⎯ | 22 (28.9%) | ⎯ |
| $75,000 or more | ⎯ | 17 (22.4%) | ⎯ |
| Prefer not to answer | ⎯ | 5 (6.6%) | ⎯ |
| Primary Insurance | |||
| Private | 26 (34.2%) | ⎯ | ⎯ |
| Medicaid | 3 (3.9%) | ⎯ | ⎯ |
| Medicare | 41 (53.9%) | ⎯ | ⎯ |
| Other | 4 (5.3%) | ⎯ | ⎯ |
| Missing | 2 (2.6%) | ⎯ | ⎯ |
| Marital Status | |||
| Married | ⎯ | 69 (90.8%) | ⎯ |
| Other | ⎯ | 6 (7.9%) | ⎯ |
| M (SD) Range | M (SD) Range | M (SD) Range | |
| Age | ⎯ | 65.24 (10.9) 39–88 | 41.9 (10.5) 23–68 |
| Length of Relationship | ⎯ | 35.78 (17.9) 2–68 | ⎯ |
| Days on Hospice | 137.96 (303.4) 8–2562 | ⎯ | ⎯ |
3.2. Visit and recording data
Cancer patients were enrolled in hospice for approximately 138 days (M = 137.96 days, Median = 71 days, SD = 303.4). If a patient-caregiver dyad had more than one recorded nurse hospice visit, one visit was randomly selected. Visits therefore represent different points over the course of hospice care as early as the second visit to the day of death. Recordings on average began at the third nurse visit (median) after enrollment in hospice and each recording lasted on average 41.3 min (Median = 40, SD = 19.4, R = 14–114). Our sample for LIWC analysis consisted of 76 recorded visits with 65 different hospice nurses. In the examination of caregiver's coping and ability to express needs, seven transcripts were excluded due to a lack of caregiver speech (the caregiver stepped out or was not present at the time of the nurse visit) for a final total of N = 69 recorded nurse visits.
3.3. Descriptive analysis
Partner caregivers spoke a total of 106,316 words and patients spoke 56,209 words. In both patient and caregiver speech, the proportion of “I-talk” was the greatest, followed by “you-talk” and then “we-talk”. Caregivers demonstrated proportionately more first-person singular (I-talk) than first person plural (we-talk) (5.11% vs. 1.27%, χ2 = 2538.16, DF = 1, p < 0.001). However, caregivers used significantly less I-talk than patients (5.11% vs. 7.85%; χ2 = 485.09; DF = 1; p < 0.0001) and less I-talk than LIWC measures in naturally occurring conversation (5.11% vs. 7.03% χ2 = 5.98; DF = 1; p < 0.05) [23]. See Table 4 for differences between patient and partner caregivers' proportion of pronoun use compared with naturally occurring speech.
Table 4.
Patient and family caregiver's pronoun use (%) compared with naturally occurring speech.
| LIWC natural corpus | Patient speech | Difference | p-value | LIWC natural corpus | Partner caregiver speech | Difference | p-value | |
|---|---|---|---|---|---|---|---|---|
| I | 7.03 | 7.85 | 0.82 | 0.3933 | 7.03 | 5.11 | −1.92 | 0.0145⁎ |
| We | 0.87 | 1.06 | 0.19 | 0.6032 | 0.87 | 1.27 | 0.40 | 0.3154 |
| You | 4.04 | 2.1 | −1.94 | 0.0003⁎⁎ | 4.04 | 2.4 | −1.64 | 0.0030⁎⁎ |
Significant at p < 0.05 (two-tailed).
Significant at p < 0.01 (two-tailed).
3.4. Content analysis
With a purpose of examining the context in which caregivers' used I-, we- and you-talk, the following categories were used to code transcripts of caregivers' speech: patient medical care, daily life, emotion (e.g., positive emotion such as appreciation, negative emotion such as distress, response to another's emotion), criticism/disagreement, relationships with family/friends, and asserting needs (when caregivers assert needs related to the patient's care, their employment, health, time, or support). Using the codebook which defined each of these eight categories, a total of 9012 codes—or instances of these topics—were identified. Interrater reliability was calculated using NVivo 12 software, resulting in a Cohen's Kappa of 0.68, which is deemed adequate [26].
The largest number of codes (n = 3774, 41.9%) fell under the category of patient medical care in which the caregiver identified medical questions or medical issues including physical symptoms, problem-solving issues regarding the patient's medical care, medical decision-making, or the dyad's interaction with other healthcare providers. Emotion was the topic with the second-highest frequency (2261, 25%): Positive emotion, in which the caregiver expressed optimism, love, gratitude, solidarity, or complimented others occurred 993 times (11.0%). Emotional response, defined as the caregiver responding to other people's emotions with support, reassurance, empathy, concern, legitimizing, and or negotiating occurred 832 times (9.2%). Distress, in which caregivers expressed feelings of distress, worries, or discuss the patient's wants or needs related to distress, occurred 436 times (4.8%).
Daily life was the third most frequent topic of discussion (1406 codes, 15.6%). Daily life was defined as the caregiver engaging in casual conversation including discussions regarding the weather, pets, small talk, and plans that did not fall under other categories. Criticism or disagreement, in which the caregiver engaged in correcting, clarifying, criticism, blame, justification or defending, was coded 619 times (6.9%). Following closely behind is the topic of relationships with family/friends (614 codes, 6.8%). This topic occurred when the caregiver discussed the dyad's relationship, family, or other social relationships and could pertain to past or current actions or behaviors. The topic least discussed was asserting needs which entailed the caregiver asserting their own needs related to the patient's care, their employment, health, time, or support; (338 codes, 3.8%) of asserting needs were identified in the transcripts.
3.5. Caregivers' pronoun use when expressing needs
In order to examine caregivers' ability to express their needs near the end of a patient's life, pronoun use within the category of “asserting needs” was further examined. Caregivers uttered a total of 653 pronouns when discussing their asserting needs: 523 (80.1%) of these were I-talk, 52 (8.0%) were we-talk, and 78 (11.9%) were you-talk (See Table 5 for exemplar quotes). Compared with other categories of caregiver speech, asserting needs contained the second lowest proportion of we-talk (5.0%) (with emotional response containing 4.9%) and the lowest proportion of you-talk (6.1%) among all eight categories (see Table 6 for a table showing the frequency and proportion of pronoun use by topic of conversation).
Table 5.
Exemplar Quotes of Caregivers' Pronoun Use when Asserting Needs.
| I-talk | You-talk | We-talk |
|---|---|---|
| “I was just wondering who can I call” “I've had all these things on the back burner that I needed to address” |
“Will you call? Just tell them…” “Can you take these and give them to somebody else?” |
“Okay, let's go, you don't have pain? We can go, it's easy” “We never even need it” |
Table 6.
Frequency and Proportion of Pronoun Use Per Topic Discussed.
| Topic of Conversation | “I” pronouns | “We” pronouns | “You” pronouns | Total pronouns |
|---|---|---|---|---|
| Asserting Needs | 523 (80.1) | 52 (8.0) | 78 (11.9) | 653 |
| Criticism/Disagreement | 337 (64.7) | 79 (15.2) | 105 (20.1) | 521 |
| Distress | 546 (71.2) | 88 (11.5) | 133 (17.3) | 767 |
| Emotional Response | 262 (62.2) | 51 (12.1) | 108 (25.7) | 421 |
| Health-Related Issues | 1303 (64.5) | 383 (19.0) | 332 (16.5) | 2018 |
| Lifestyle | 315 (53.5) | 86 (14.6) | 188 (31.9) | 589 |
| Positive Emotion | 309 (56.1) | 105 (19.0) | 137 (24.9) | 551 |
| Psychosocial | 661 (63.0) | 187 (17.8) | 202 (19.2) | 1050 |
4. Discussion and conclusion
4.1. Discussion
While linguistic analysis of hospice visits demonstrated that partner caregivers used more personal pronouns than communal pronouns, caregivers used fewer personal pronouns than did patients and fewer than what was expected in naturally occurring conversations [23]. Qualitative analyses of naturally occurring hospice visits also demonstrated the infrequency with which caregivers use I-talk in conversation, potentially indicating difficulty in asserting their needs and cognitively processing the impending death of their partner. These findings reflect research which found that cancer patients used more I-talk than their spouses and that cancer patients and partners used I-talk when distinguishing their personal thoughts and feelings from that of their partner [14]. Our findings suggest that caregivers may feel better able to express emotions related to communal stressors, but struggle to express emotions related to their own needs towards the end of a patient's life. Even though we-talk can signify better overall communal coping and relationship functioning [13], caregivers' use of we-talk in discussing their needs may suggest that the interdependent relationship may hinder them from asserting their own needs and successfully adapting to the stressful experience of cancer. Future research on the association between caregivers' use of pronouns, coping, and ability to assert their needs is needed, as prior research measured the association between pronoun use and benefit-finding [11], better relationship quality [13], psychological well-being [14] [6] and illness specific self-care [15,16], which are related but distinct concepts from coping or asserting needs.
This is especially important for partner caregivers of hospice cancer patients who are at risk of caregiver burden and distress as the patient's health declines and caregiving demands increase [27]. If partner caregivers cannot assert their needs during this highly stressful time, they are not only at greater risk for distress, anxiety, and depression, but also risk providing compromised care to the patient [28] and experiencing bereavement problems after the patient's death [5,29]. Since caregivers tend to neglect their own wellbeing [30] and often do not seek help when faced with these psychological issues [1], it may therefore be beneficial to better integrate assessment of caregiver needs into home hospice visits. While communal coping continues to benefit couples who are faced with chronic illness, once on hospice, caregivers may benefit from separate efforts to support their individual coping as the hospice cancer patient nears the end of life. In fact, a study of cancer caregivers found that their priorities included better integration into the patient's healthcare delivery and a greater focus on caregiver health and wellbeing [31].
While hospice care typically views the family as the unit of care [32] due to a variety of barriers, routine caregiver assessment and support may not occur. For example, many hospice nurses have large caseloads and may not have the time to address both the patient's and the caregiver's needs [33]. Other barriers may include late referral of cancer patients to hospice [34], limiting the ability to properly assess caregiver needs, as well as a discomfort or lack of knowledge regarding how to conduct such an assessment and provide the appropriate support [35]. Thus, while integration of caregivers into hospice is the ideal, the consistency with which this occurs should be assessed and steps taken to reduce barriers to this family approach.
4.1.1. Limitations
While word count strategies such as LIWC have the ability to perform reliably and efficiently through computers [22] there are limitations to their use as a linguistic analysis tool. Although LIWC can tally pronoun use, it cannot detect negations such as “NOT me” [22]. It also is unable to consider context, multiple meanings of words, or what is considered a linguistically significant amount of difference compared with naturally occurring speech [22] [23]. Thus, we are unable to determine if the statistically significant differences we found in pronoun use translate to meaningful differences. Furthermore, this study did not account for mis-utterances in which a caregiver may have changed their pronoun use, and although likely to be infrequent, this could potentially introduce bias into the data. These limitations may be offset by the reduction in self-report bias that linguistic software provides, and by incorporating supplemental qualitative methods of examining communal coping [10]. These limitations are also offset by qualitatively providing the topic of conversation for use of each pronoun. During the qualitative coding and analysis, only the written transcripts were read by coders—since the recordings were not listened to, some of the meaning or emotion may have been lost. Cancer patients were on hospice an average of 137.96 days (Median = 71 days) which is larger than the National Hospice and Palliative Care Organization's finding that cancer patients stay on hospice for an average of 92.6 days (Median = 18 days) [32]. Our sample clearly reflects cancer patients who had a longer length of stay than the national average. It is likely that patients who enter hospice with imminent death are not represented in this sample. Furthermore, it is possible that the hospice agencies that were already more successful in enrolling patients into hospice earlier were also those who agreed to participate in the study, which could account for longer lengths of hospice enrollment. Unfortunately, due to power and the initial preparation of the data, the role of gender and pronoun use in this study was unable to be explored. Future research should consider controlling for gender, as it is possible that females (regardless of their role as patient or caregiver) utilize communal pronouns more frequently than males.
4.2. Innovation
Despite these potential limitations, this study's use of natural language processing software not only enhances the trustworthiness of our findings, but extends new methods to the study of caregiver coping and preparedness for their partner's end of life (specific framing for innovation). Rather than rely on caregivers to self-report, this study utilizes pronoun use as a more objective and accurate indicator of coping and caregivers' ability to assert their needs [12]. Furthermore, few studies have examined hospice cancer caregivers' pronoun use during the end of life nor during medical encounters (e.g. home hospice visits with nurses) as a measure of individual coping or ability to assert needs. Examination of pronoun use by cancer patients and partner caregivers has typically focused on the period following cancer treatment typically referred to as ‘adjustment’ [13,14,36]. This specific innovation broadens our understanding of the contexts and individuals with which natural language processing may be utilized to gain a greater depth of knowledge regarding human behavior and communication.
4.3. Conclusion
In sum, communal coping may be more beneficial for couples earlier on in the cancer trajectory [12,13,37]. Taking a “we” approach can not only improve a patient's overall wellbeing, but may also contribute to the partner's wellbeing, and the couple's overall relationship functioning [13,37]. However, emphasizing a “we” approach in the hospice care phase may lead partner caregivers to ignore or devalue their own personal needs. As the patient with cancer progresses towards the end of their life, it is imperative that caregivers feel empowered to assert their individual needs. Hospice care team members should be 1) cognizant of partner caregivers' potential unaddressed needs, 2) purposefully assess caregivers' confidence and comfort in providing care to the patient, and 3) assess caregivers' ability to care for themselves emotionally and physically while managing a home and other responsibilities during their partners' end of life. Kent and colleagues suggest standardizing formal recommendations for integrating caregivers into diverse clinical settings, developing and testing models of caregiver integration, and evaluating caregivers' capacity to provide care [27]. By better integrating caregiver assessment and routine support into regular hospice visit interactions and reducing barriers to standard caregiver integration, providers can take a proactive approach to supporting partner caregivers' personal expression of needs. Ultimately, supporting cancer caregivers' coping and preparedness can have positive, long-lasting effects.
Funding
This work was supposed by: The National Institute of Nursing Research (5R01NR016249) and Interdisciplinary Training in Cancer, Caregiving, and End-of-Life Care (2T32NR013456). Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR002538 and TL1TR002540. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Declaration of Competing Interest
The authors report there are no competing interests to declare.
Acknowledgements
The authors would like to thank Kalen Gunter for her assistance with the qualitative content analysis.
Contributor Information
Sara Bybee, Email: sara.bybee@utah.edu.
Megan Hebdon, Email: megan.hebdon@nursing.utexas.edu.
Kristin Cloyes, Email: cloyes@ohsu.edu.
Shirin Hiatt, Email: shirin.hiatt@utah.edu.
Eli Iacob, Email: eli.iacob@nurs.utah.edu.
Maija Reblin, Email: maija.reblin@med.uvm.edu.
Margaret Clayton, Email: margaraet.clayton@nurs.utah.edu.
Lee Ellington, Email: lee.ellington@nurs.utah.edu.
References
- 1.National Alliance for Caregiving . AARP; Washington, DC: 2020. Caregiving in the United States 2020. [Google Scholar]
- 2.Washington K.T., et al. Unique characteristics of informal hospice cancer caregiving. Support Care Cancer. 2015;23(7):2121–2128. doi: 10.1007/s00520-014-2570-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reblin M., et al. Spouse cancer caregivers’ burden and distress at entry to home hospice: the role of relationship quality. J Soc Pers Relat. 2016;33(5):666–686. doi: 10.1177/0265407515588220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bernard L.L., Guarnaccia C.A. Two models of caregiver strain and bereavement adjustment: a comparison of husband and daughter caregivers of breast cancer hospice patients. Gerontologist. 2003;43(6):808–816. doi: 10.1093/geront/43.6.808. [DOI] [PubMed] [Google Scholar]
- 5.Allen J.Y., et al. Bereavement among hospice caregivers of cancer patients one year following loss: predictors of grief, complicated grief, and symptoms of depression. J Palliat Med. 2013;16(7):745–751. doi: 10.1089/jpm.2012.0450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Helgeson V.S., Jakubiak B., Van Vleet M., Zajdel M. Communal coping and adjustment to chronic illness: theory update and evidence. Pers Soc Psychol Rev. 2018:1–26. doi: 10.1177/1088868317735767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lyons R.F., et al. Coping as a communal process. J Social Personal Relat. 1998;15(5):579–605. [Google Scholar]
- 8.Badr H., et al. Dyadic coping in metastatic breast cancer. Health Psychol. 2010;29(2):169–180. doi: 10.1037/a0018165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen M., et al. A literature review of the relationship between dyadic coping and dyadic outcomes in cancer couples. Eur J Oncol Nurs. 2021;54 doi: 10.1016/j.ejon.2021.102035. [DOI] [PubMed] [Google Scholar]
- 10.Rohrbaugh M.J., Shoham V., Skoyen J.A., Jensen M., Mehl M.R. We-talk, communal coping, and cessation success in a couple-focused intervention for health-compromised smokers. Fam Process. 2012;51:107–121. doi: 10.1111/j.1545-5300.2012.01388.x. [DOI] [PubMed] [Google Scholar]
- 11.Zajdel M., et al. Links of we-talk to caregiver social network systems and health. J Fam Psychol. 2022;36(8):1386–1396. doi: 10.1037/fam0001013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karan A., Wright R.C., Robbins M.L. Everyday emotion word and personal pronoun use reflects dyadic adjustment among couples coping with breast cancer. Personal Relat. 2017;24(1):36–48. [Google Scholar]
- 13.Karan A., Rosenthal R., Robbins M.L. Meta-analytic evidence that we-talk predicts relationship and personal functioning in romantic couples. J Social Personal Relat. 2019;36(9):2624–2651. [Google Scholar]
- 14.Badr H., et al. Natural language use and couples’ adjustment to head and neck cancer. Health Psychol. 2016;35(10):1069–1080. doi: 10.1037/hea0000377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee J., et al. Implications of we-talk for relationships and health among patients with type 1 diabetes and their spouses. J Social Personal Relat. 2020;37(1):345–354. [Google Scholar]
- 16.Rohrbaugh M.J., et al. Prognostic significance of spouse we talk in couples coping with heart failure. J Consult Clin Psychol. 2008;76(5):781–789. doi: 10.1037/a0013238. [DOI] [PubMed] [Google Scholar]
- 17.Chen M.L., Chu L., Chen H.C. Impact of cancer patients’ quality of life on that of spouse caregivers. Support Care Cancer. 2004;12(7):469–475. doi: 10.1007/s00520-004-0636-z. [DOI] [PubMed] [Google Scholar]
- 18.Hui D., et al. Symptom expression in the last seven days of life among cancer patients admitted to acute palliative care units. J Pain Symptom Manage. 2015;50(4):488–494. doi: 10.1016/j.jpainsymman.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li M., et al. Effects of couple-based dyadic interventions on breast cancer patients and their intimate partners: a systematic review and meta-analysis. J Adv Nurs. 2023 Mar 14 doi: 10.1111/jan.15639. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 20.Ellington L., Clayton M.F., Reblin M., Donaldson G., Latimer S. Communication among cancer patients, caregivers, and hospice nurses: content, process and change over time. Patient Educ Couns. 2018;101(3):414–421. doi: 10.1016/j.pec.2017.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nurses again rank most trustworthyNursing 2023. 2007;37(3) [Google Scholar]
- 22.Pennebaker J.W., Mehl M.R., Niederhoffer K.G. Psychological aspects of natural language use: our words. Our Selves Annu Rev Psychol. 2003;54(1):547–577. doi: 10.1146/annurev.psych.54.101601.145041. [DOI] [PubMed] [Google Scholar]
- 23.Pennebaker J.W., et al. 2015. The development and psychometric properties of LIWC2015. [DOI] [Google Scholar]
- 24.QSR International Pty Ltd . 2018. NVivo qualitative data analysis software. [Google Scholar]
- 25.O’Connor C., Joffe H. Intercoder reliability in qualitative research: debates and practical guidelines. Int J Qual Methods. 2020;19 p. 1609406919899220. [Google Scholar]
- 26.Landis J.R., Koch G.G. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 27.Kent E.E., et al. Caring for caregivers and patients: research and clinical priorities for informal cancer caregiving. Cancer. 2016;122(13):1987–1995. doi: 10.1002/cncr.29939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prevention, C.f.D.C.a For Caregivers, Family, and Friends. 2022 June 28. https://www.cdc.gov/aging/caregiving/index.htm 2022 June 7, 2023]; Available from:
- 29.Caserta M., et al. Cancer caregivers’ preparedness for loss and bereavement outcomes: do Preloss caregiver attributes matter? Omega (Westport) 2019;80(2):224–244. doi: 10.1177/0030222817729610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lopez V., Copp G., Molassiotis A. Male caregivers of patients with breast and gynecologic cancer: experiences from caring for their spouses and partners. Cancer Nurs. 2012;35(6):402–410. doi: 10.1097/NCC.0b013e318231daf0. [DOI] [PubMed] [Google Scholar]
- 31.Thomas T.H., et al. Priorities to improve cancer caregiving: report of a caregiver stakeholder workshop. Support Care Cancer. 2021;29(5):2423–2434. doi: 10.1007/s00520-020-05760-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Organization, N.H.a.P.C . National Hospice and palliative care organization; Alexandria, VA: 2021. Hospice facts and figures. [Google Scholar]
- 33.Washington K.T., et al. Team functioning in hospice interprofessional meetings: an exploratory study of providers’ perspectives. J Interprof Care. 2017;31(4):455–462. doi: 10.1080/13561820.2017.1305950. [DOI] [PubMed] [Google Scholar]
- 34.Teno J.M., et al. Dying trajectory in the last year of life: does cancer trajectory fit other diseases? J Palliat Med. 2001;4(4) doi: 10.1089/109662101753381593. [DOI] [PubMed] [Google Scholar]
- 35.Clayton M.F., et al. Hospice nurse identification of comfortable and difficult discussion topics: associations among self-perceived communication effectiveness, nursing stress, life events, and burnout. Patient Educ Couns. 2019;102(10):1793–1801. doi: 10.1016/j.pec.2019.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Robbins M.L., et al. Linguistic indicators of patient, couple, and family adjustment following breast cancer. Psychooncology. 2013;22(7):1501–1508. doi: 10.1002/pon.3161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zajdel M., Helgeson V.S. Communal coping: a multi-method approach with links to relationships and health. J Social Personal Relat. 2020;37(5):1700–1721. [Google Scholar]