Highlights
-
•
Rate of preventive care use is 48.94% for middle-aged and elderly in China.
-
•
Individual-level social activities participation is associated with preventive care use.
-
•
There is a positive correlation between community facility richness and preventive care use.
Abstract
This study explores the status quo of preventive care use and social capital among middle-aged and elderly people (≥45 years old) in China, and employs a multi-level model to analyze whether social capital at different levels is associated with preventive care use. The data are derived from the 2018 China Health and Retirement Longitudinal Study (CHARLS), which includes 11,503 respondents and 450 communities. Preventive care use covers the utilization of routine physical examination services. Individual social capital is measured by the level of social network and social activities participation. Social network includes contacting with children or other people, for example, by phone, text message. Social activities participation is measured by the involvement in social activities, for example, playing mahjong, going to community club. Community social capital is evaluated by the richness of community facilities. Results reveals that the utilization of preventive care is 48.94% among middle-aged and elderly in China. The most used preventive service is routine blood test. The intra-class correlation (ICC) coefficient indicates that preventive health behaviors of the respondents are clustered at communities where they live. Multi-level regression shows that influence of social network is not significant to preventive care use (p > 0.05). Community facilities and individual social activities participation are significantly associated with preventive care use (p < 0.05). The association between social capital and preventive care use could be considered as an important factor when making policies to promote preventive care use.
1. Introduction
There are more than 200.56 million aged (age ≥ 65) adults at the end of 2021 in China, accounting for 14.2% of the total population (National Bureau of Statistics of China, 2022). With 14% (age ≥ 65) as the dividing line for advanced stage of aging, China has become “in-depth aging society” at the end of 2021. As populations age, the incidence of age-related non-communicable diseases—for example, ischemic heart disease, cancer, stroke, arthritis and Alzheimer's disease—will continue to increase (Prince et al., 2015). Chronic diseases are characterized by long periods of suffering throughout the afflicted person's life and consume more health resources—thereby bringing a heavy burden to the patients and society.
Preventive care can promote health and save health resources in different ways, such as reducing the occurrence and spread of diseases through vaccines (D’Souza and Dempsey, 2011, Imai et al., 2018); avoiding sudden cardiovascular disease by using blood pressure monitoring (Bosio et al., 2003, Fuchs et al., 2013); achieving the early diagnosis and treatment of diseases and reducing the possibility of disease deterioration; decreasing the use of hospitalization services; and saving medical costs through biochemical indicators and imaging tests (Hale et al., 2015, Tomazelli and Silva, 2017).
Studies have shown that social capital is essential to increase people's enthusiasm for using preventive care as it standardizes individual health behaviors through group pressure and promotes the dissemination of health information (Peng and Chan, 2020). Psychosocial support can be provided and enhanced through individual and community social capital, thereby encourage beneficial health activities and promote health service utilization (Scheffler et al. 2008). Studies have demonstrated that social capital has positive effects on cancer screening (Dean et al., 2014, Moudatsou et al., 2014, Dean et al., 2015, Crookes et al., 2016), vaccination (Nagaoka et al., 2012, Chuang et al., 2015, Palanisamy et al., 2018, Shobugawa et al., 2018), health-promoting behavior (Nieminen et al., 2013, Wiltshire et al., 2017), and medical check-ups (Bender et al., 2015).
Researchers have defined social capital in a variety of ways. Bourdieu (1983) points out that social capital is the sum of resources available to individuals, and that social networks are an integral part of social capital, and it can be maintained by certain institutional rules. Coleman (1988) believes that social capital mainly provides welfare to individuals through social culture, shared trust, and certain social norms and systems. Putnam (1993) combines Bourdieu and Coleman's views on social capital. He believes that social capital should include the social network itself and various social common values formed to maintain the social network, such as trust and norms. Fukuyama (1995) holds that social capital is a set of informal values and codes of conduct that members follow together, including honesty, reciprocity and trust. The concept of social capital continues to be developed and enriched, but it has not been integrated into a unified one. The view that “social capital should include core elements such as social network, social participation, trust and reciprocity” has been recognized by most researchers in related fields of study (Wang et al., 2013, p336).
Studies have focused on the impact of social capital on the utilization of maternal and child health services (Story, 2014); the effect of social capital on self-rated health status (Ichida et al., 2009, Meng and Chen, 2014). Few studies have focused on preventive services. Only one study using data from Taiwan Province in China examined the role of social capital in medical examinations among older adults during insurance coverage (Peng and Lin, 2018). We conduct multi-level model based on the China Health and Retirement Longitudinal Study (CHARLS) 2018 to explore the relationship between social capital and preventive care use among middle-aged and elderly people in China.
2. Material and methods
2.1. Data
The data for this study is from the China Health and Retirement Longitudinal Study (CHARLS). It aims to collect a set of high-quality microdata representing families and individuals of middle-aged and elderly people aged 45 and over in China to analyze the problem of population aging and promote interdisciplinary research on aging (https://charls.pku.edu.cn/). The CHARLS covers 150 counties and 450 communities (villages) in 28 provinces (autonomous regions and municipalities) in China. It contains the following information: demographic backgrounds, health behaviors and conditions, preventive care use, healthcare costs, medical insurance, family economic status, and community conditions.
We use the cross-sectional data of the CHARLS 2018 which contains a sample of 19,816 people. Due to the lack of community data in the CHARLS 2018, we collect community data from the CHARLS 2011. These community indicators are matched with individual indicators obtained from the CHARLS 2018. After excluding missing value, the final sample consists of 11,503 respondents.
2.2. Variables
Preventive care use is measured by the utilization of any of the fifteen items in the routine physical examination services, for example, routine blood examination, liver function examination and blood glucose examination.
Social capital is classified as individual social capital (ISC) and community social capital (CSC) in this study. ISC is measured by social network and social activities participation.
Social network is the frequency with which respondents contact their children. We assess social network with two items: 1) In the past year, how often did you and your spouse live with your children (not include short visits)?; 2) When your child is not living with you, how often do you contact with him/her on phone/by message/on wechat/ by mail/ by email? The options for the second question are “almost every day”, “2-3 times a week”, “once a week”, “once every half month”, “once a month”, “once every three months”, “once every six months”, “once a year”, “almost never”, and “other”. In our study, we categorize the frequency of contact with children and assigned the values of “1 = contact every day”, “2 = contact at least once a month”, and “3 = contact once a quarter or more”. If the respondents have been living with their children, they are considered to be in contact every day. The respondents may have more than one child, we use the frequency of contact between respondents and their child who is most closely connected to represent the frequency of contact between respondents and their children.
Social activities participation is measured by 10 social activities that respondents participated in the past month. It includes “interacted with friends”, “played Ma-jong, played chess, played cards, or went to community club”, “provided help to family, friends, or neighbors who do not live with you”, “went to a sport, social, or other kind of club”, “took part in a community-related organization”, “done voluntary or charity work”, “cared for a sick or disabled adult who does not live with you”, “attended an educational or training course”, “stock investment”, “used the Internet”. In our study, the types of social activities that the respondents participated in are classified and assigned “1 = deprived (0 types of activities)”, “2 = general (1–3 types of activities)”, and “3 = Rich (types of activities are greater than 3)”.
CSC is evaluated by the types of activity venues in the respondent's village/community. It includes 14 items such as basketball courts, swimming pools, and open-air fitness equipment. In our study, we categorize and assign values: 0 = deprived (activity venue type = 0), 1 = general (activity venue types = 1–3), 2 = rich (activity venue types > 3).
2.3. Control variables
The control variables include respondent gender; age; marital status; education; employment; insurance; health condition (chronic diseases, instrumental activities of daily living [IADL], activities of daily living [ADL], and the Center for Epidemiologic Studies Depression Scale [CES-D]); the level of income; and region and area type. There are 14 kinds of chronic diseases, of which included hypertension, dyslipidemia, and other diseases.
We use IADL, ADL, and the CES-D to reflect the physical and mental health of the sample, respectively. The IADL scale is used to measure whether there is an instrumental disorder in their daily lives. There are 6 items: household chores, cooking, shopping, making phone calls, taking medication, and managing finances (Connolly et al., 2017). The options of the scale are “no difficulty”, “difficulty but still able to do it”, “difficulty and need help”, and “unable to do it”. The ADL scale is used to measure whether there is an activities disorder in their daily lives. There are 6 items: dressing, bathing, eating, getting in/out of bed, going to the toilet, and controlling urination or defecation (Silverstein et al., 2020). The answer items of both ADL and IADL scales are the same, the score of options are 1–4 points (1 = no difficulty, 2 = difficulty but can still do it, 3 = difficulty and need help, 4 = can't do it). The IADL and ADL score between 6 and 24. If respondents report difficulty with any items of IADL or ADL scale (i.e., when IADL or ADL score is more than 6), the older adult will be considered to have instrumental or activity disorder (Yan et al., 2023). In our study, IADL and ADL are defined as binary variables, assigned a value of 1 if the respondents had an instrumental or activity disorder, and 0 otherwise (Connolly et al., 2017).
The CES-D is reported through 10 entries, including feeling annoyed by trifles, difficulties in concentration, feeling down in the dumps, encountering difficulties in doing anything, being hopeful for the future, feeling frightened, experiencing poor sleep, feeling happy, feeling lonely, and encountering difficulties in continuing life. The higher the score, the higher the degree of depression (Wang et al., 2019). If the score is greater than 10 (Andresen et al., 1994, Zhou et al., 2021), there is a tendency for depression and vice versa. Household income is transformed into per capita income and divided into three income groups.
2.4. Statistical methods
The chi-square test is used to verify the differences between the groups with different characteristics. The data we use have a hierarchical structure at the county (district)-village (residence)-household-individual level. Individuals are not independent, and the data at each level are similar or clustering in terms of economic level, lifestyle, eating habits, social capital, and so on. A two-level multi-level logistic model is employed to analyze the influence of individual social capital and community social capital on preventive care use. The use of multi-level statistical modeling allows the researcher to simultaneously analyze the effect of individual and cluster level variables while taking into account the unobserved group level heterogeneity (Rabehesketh and Skrondal, 2012). The intra-class correlation coefficient (ICC) shows the percentage of variation in preventive care use among communities as a whole. Cohen (1988) believes that when ICC is equal or greater than 0.059, it can be considered highly correlated within the group, and the multi-level model is applicable. In order to observe the influence of different variables on preventive care use, the following four models are constructed: Null Model (Model 1), Demographic Model (Model 2), Individual-level Model (Model 3), and Full Model (Model 4).
3. Results
Of the 11,503 respondents, a greater proportion are female (53.14%), married (74.68%), with a junior high school or lower level of education (86.94%). The physical health level is low, the mental one, by contrast, is high (the prevalence of chronic diseases is 81.19%, IADL ≤ 6 accounted for 72.68%, and CESD greater than 10 accounted for 33.56%). The rates of preventive care use among those who contacted with their children daily are 47.57%, 49.55% per month and 51.71% quarterly or above. The higher the frequency of participation in social activities, the higher rate of preventive care use: 44.36% for those who never participated, 51.39% for those who sometimes participated, and 71.12% for those who regularly participated. When the number of community facility reached more than three, the utilization rate of preventive care is higher than 50%. The Chi-square test results show that the difference of preventive care use between respondents with different levels of variables (except IADL and region variables) are statistically significant (Table 1).
Table 1.
Basic characteristics and preventive care use among middle-aged and elderly people in 2018.
| Variables | Definition | Sample(N) | % | Preventive care use (%) | P value | |
|---|---|---|---|---|---|---|
| Dependent variable | ||||||
| Preventive care use | =1 take preventive care in the past two years; =0 otherwise. | |||||
| Independent variables | ||||||
| Total | 11,503 | 48.94 | ||||
| Gender | Male | =1 if male; =0 if female. | 5390 | 46.86 | 50.35 | <0.01** |
| Female | 6113 | 53.14 | 47.69 | |||
| Age | Age < 65 years | =1 if age < 65 years; =0 if age ≥ 65 years. | 6711 | 58.34 | 40.99 | <0.001*** |
| Age ≥ 65 years | 4792 | 41.66 | 60.06 | |||
| Married | Being married | =1 if being married; =0 otherwise. | 8590 | 74.68 | 48.29 | <0.05* |
| Otherwise | 2913 | 25.32 | 50.84 | |||
| Education | Less than high school | =1 if the highest level of education is less than high school; =0 otherwise. | 10,001 | 86.94 | 46.63 | <0.001*** |
| Otherwise | 1502 | 13.06 | 66.31 | |||
| Work status | Employed | =1 if work status is employed; =0 otherwise. | 6815 | 59.25 | 45.41 | <0.001*** |
| Unemployed | =1 if work status is unemployed; =0 otherwise. | 4360 | 37.90 | 53.28 | ||
| Retired | =1 if work status is retired; =0 otherwise. | 328 | 2.85 | 64.33 | ||
| Insurance | Insurances | =1 if have any kind of insurances; =0 if have zero kind of insurances. | 11,117 | 96.64 | 49.64 | <0.001*** |
| No insurances | 386 | 3.36 | 28.50 | |||
| Chronic disease | Suffered Chronic diseases | =1 if suffer from chronic diseases: High blood pressure, Asthma, or Stroke, etc.; =0 if have zero kind of chronic diseases. | 9339 | 81.19 | 51.56 | <0.001*** |
| No chronic diseases | 2164 | 18.81 | 37.62 | |||
| IADL | IADL ≤ 6 | =1 if IADL > 6 means having any difficulties with shopping, doing household chores, preparing hot meals, making phone calls, taking medications, managing money; =0 don’t have difficulty with these activities. | 8360 | 72.68 | 48.85 | 0.77 |
| IADL > 6 | 3143 | 27.32 | 49.16 | |||
| ADL | ADL ≤ 6 | =1 if ADL > 6 means having any difficulties with dressing, showering, eating, getting into or out of bed, using the toilet, controlling urination and defecation; =0 don’t have difficulty with these activities. | 9225 | 80.20 | 48.38 | <0.05* |
| ADL > 6 | 2278 | 19.80 | 51.19 | |||
| CES - D | CES - D ≤ 10 | =1 if CESD-10 > 10 means participant is prone to depression; =0 participant isn’t prone to depression. | 7643 | 66.44 | 50.33 | <0.001*** |
| CES - D > 10 | 3860 | 33.56 | 46.17 | |||
| Income level | Income level 1 | =1 if the first group of three equal income groups; =0 otherwise. | 3835 | 33.34 | 43.55 | <0.001*** |
| Income level 2 | =1 if the second group of three equal income groups; =0 otherwise. | 3834 | 33.33 | 46.53 | ||
| Income level 3 | =1 if the third group of three equal income groups; =0 otherwise. | 3834 | 33.33 | 56.73 | ||
| Region | East | =1 if east; =0 otherwise. | 4239 | 36.85 | 50.06 | 0.132 |
| Middle | =1 if middle; =0 otherwise. | 4308 | 37.45 | 47.89 | ||
| West | =1 if west; =0 otherwise. | 2956 | 25.70 | 48.85 | ||
| Area | City | =1 if city; =0 if town. | 3169 | 27.55 | 58.44 | <0.001*** |
| Town | 8334 | 72.45 | 45.32 | |||
| Social network (Frequency of contacting with children) | Daily | =1 if contact with children daily; =0 otherwise. | 5512 | 47.92 | 47.57 | <0.01** |
| Monthly | =1 if contact with children monthly; =0 otherwise. | 4212 | 36.62 | 49.55 | ||
| Quarterly or above | =1 if contact with children quarterly or above; =0 otherwise. | 1779 | 15.46 | 51.71 | ||
| Social activities participation (Abundance of participation in social activities) | Deprived | =1 if participate in 0 kinds of activity; =0 otherwise. | 5300 | 46.07 | 44.36 | <0.001*** |
| General | =1 if participate in 1to3 kinds of activities; =0 otherwise. | 5746 | 49.95 | 51.39 | ||
| Rich | =1 if participate in more than 3 kinds of activities; =0 otherwise. | 457 | 3.97 | 71.12 | ||
| Community facility (Abundance of Community facilities) | Deprived | =1 if own 0 kinds of equipment; =0 otherwise. | 3102 | 26.97 | 44.13 | <0.001*** |
| General | =1 if own 1 to 3 kinds of equipment; =0 otherwise. | 3509 | 30.51 | 42.69 | ||
| Rich | =1 if own more than 3 kinds of equipment; =0 otherwise. | 4892 | 42.52 | 56.46 | ||
*p < 0.05; **p < 0.01; ***p < 0.001.
Chronic diseases: Hypertension; Dyslipidemia; Diabetes or high blood suga; Cancer or malignant tumor; Chronic lung diseases; Liver disease; Heart problems; Stroke; Kidney disease; Stomach or other digestive diseases; Psychiatric problems; Memory-related disease; Arthritis or rheumatism; Asthma.
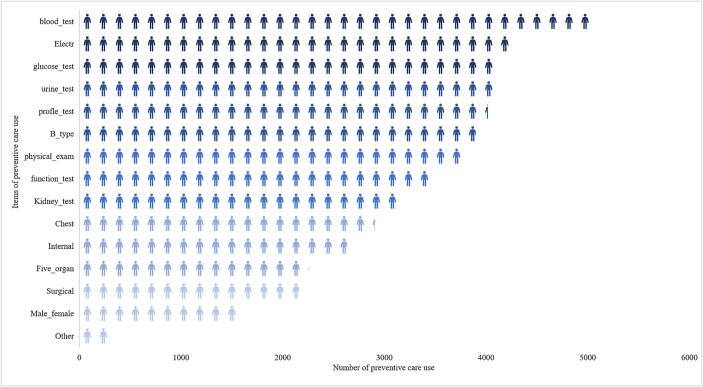
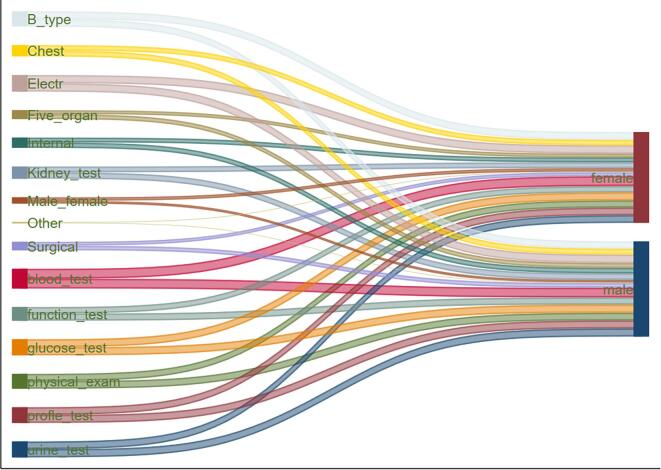
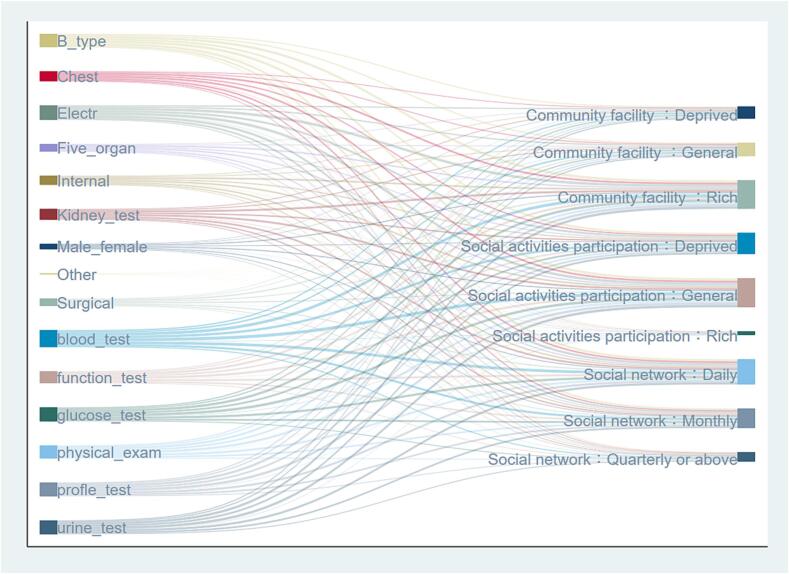
The top five preventive care services used are routine blood test, electrocardiogram, blood glucose test, lipids profile test and routine urine test (Fig. 1). Routine blood test, electrocardiogram, blood glucose test, physical examination, lipids profile test, routine urine test are the six most frequently used preventive care for both genders (Fig. 2). The node sizes and arc widths of routine blood tests are greatest in each group when community facilities, social activity participation, and social networks serve as the target nodes for preventive care use, that is, the frequency of flow to each group through routine blood test is the highest (Fig. 3).
Fig. 1.
Number of middle-aged and elderly people using items of preventive care in 2018. Physical_exam, physical examination; blood_test, routine blood test; urine_test, routine urine test; function_test, liver function test; Kidney_test, kidney function test; profle_test, lipids profile test; glucose_test, blood glucose test; Internal, internal medicine; Five_organ, five sense organ test; Electr, electrocardiogram; B_type, B_type ultrasonic; Chest, chest fluoroscopy; Male_female, male or female specialist.
Fig. 2.
Preventive care use in different gender middle-aged and elderly people in 2018.
Fig. 3.
Preventive care use in different social capital middle-aged and elderly people in 2018.
ICC shows the variation in preventive care use of Model 1 represents 12.7% of the overall variation, greater than 0.059, which can be considered to be highly correlated within the group and suitable for multi-level model analysis. Preventive care use of the middle-aged and the elderly people are related to the community where they live in, therefore, the multi-level model estimation is more accurate. Model 2 takes into account individual level variables by including individual social characteristics. In Model 2, age, marital status, education, chronic disease, income, region are significantly associated with preventive care use (p < 0.05). Model 3, on the basis of Model 2, adds individual social capital variables. The results show individual-level social activities participation is associated with preventive care use (p < 0.05). Preventive care use in the Deprived group and the General group are significantly reduced when compared with the Rich group. No evidence put in place suggests any effect of individual-level social network (p > 0.05). When reviewing all of the individual characteristics, individual social capitals, and community facilities in Model 4, the association between community facility and preventive care use remains statistically significant (p < 0.05). For community facilities, compared with Rich group, the odds ratio (OR) of General group is 0.62 (95 %CI: 0.52–0.73), and that of Deprived group is 0.70 (95 %CI: 0.59–0.84). The variance components of the multi-level model provide valuable information regarding the variation between community levels (Table 2).
Table 2.
Multi-level logistic regression estimates (odds ratios and 95% confidence intervals) and variance components of preventive care use, N = 11,503 individuals nested within N = 450 communities.
| Variables | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|
| Preventive care use | ||||
| Male vs Female | 0.92(0.85–1.01) | 0.94(0.86–1.02) | 0.94(0.87–1.03) | |
| Age ≥ 65 years vs Age < 65 years | 2.68(2.44–2.95)*** | 2.78(2.53–3.06) *** | 2.76(2.51–3.04) *** | |
| Married vs Otherwise | 1.11(1.00–1.23)* | 1.10(0.99–1.22) | 1.10(0.99–1.22) | |
| Less than high school vs Otherwise | 0.43(0.38–0.50)*** | 0.46(0.41–0.53) *** | 0.47(0.41–0.54) *** | |
| Employment | ||||
| Employed vs Unemployed | 1.07(0.96–1.19) | 1.06(0.95–1.18) | 1.06(0.95–1.18) | |
| Retired vs Unemployed | 1.45(1.12–1.87) ** | 1.43(1.11–1.85) ** | 1.41(1.09–1.82) ** | |
| Insurances vs No Insurances | 2.39(1.87–3.06) *** | 2.36(1.84–3.02) *** | 2.34(1.83–2.99) *** | |
| Health condition | ||||
| Chronic vs No Chronic | 1.68(1.51–1.87) *** | 1.66(1.49–1.86) *** | 1.67(1.50–1.86) *** | |
| ADL > 6 vs ADL ≤ 6 | 1.07(0.95–1.20) | 1.08(0.96–1.22) | 1.09 (0.97–1.23) | |
| IADL > 6 vs IADL ≤ 6 | 0.94(0.84–1.04) | 0.96(0.86–1.07) | 0.97(0.87–1.08) | |
| CES-D > 10 vs CES-D ≤ 10 | 0.95(0.87–1.04) | 0.96(0.86–1.05) | 0.96(0.88–1.05) | |
| Income level 2 vs Income level 1 | 1.15(1.04–1.27)* | 1.14(1.03–1.26)* | 1.13(1.03–1.26)* | |
| Income level 3 vs Income level 1 | 1.47(1.31–1.64) *** | 1.41(1.26–1.58) *** | 1.39(1.24–1.56) *** | |
| Region | ||||
| Middle vs East | 0.84(0.72–0.99) * | 0.83(0.70–0.97) * | 0.87(0.74–1.02) | |
| West vs East | 1.00(0.84–1.20) | 1.01(0.84–1.20) | 1.09(0.91–1.30) | |
| City vs Town | 1.25(1.11–1.41) ** | 1.22(1.08–1.37) ** | 1.11(0.98–1.26) | |
| Social network | ||||
| Monthly vs Daily | 1.03(0.94–1.13) | 1.04(0.95–1.14) | ||
| Quarterly or above vs Daily | 0.98(0.86–1.10) | 0.97(0.86–1.10) | ||
| Social activities participation | ||||
| General vs Rich | 0.50(0.40–0.63) *** | 0.51(0.40–0.64) *** | ||
| Deprived vs Rich | 0.38 (0.30–0.48) *** | 0.39 (0.31–0.49) *** | ||
| Community facility | ||||
| General vs Rich | 0.62(0.52–0.73) *** | |||
| Deprived vs Rich | 0.70(0.59–0.84) *** | |||
| Variance components | ||||
| Level 2 variance, σ2μ(S.E.) | 0.48(0.049) | 0.355(0.041) | 0.347(0.040) | 0.314 (0.037) |
| Intra-class correlation, p | 0.127 |
*p < 0.05; **p < 0.01; ***p < 0.001.
In order to test the robustness of the research results, we analyze the impact of social capital on the preventive care use of middle-aged and elderly people. Research further divide the sample population into two groups according to age (<65 years old or ≥ 65 years old) and perform multi-level model regression respectively. The robustness test results show that the impact of social capital on preventive health care use is consistent with the overall regression results (Supplementary:Table S1 and Table S2). Community facilities and individual social activities participation are significantly associated with preventive care use (p < 0.05). Social networks is not significantly associated with preventive care use (p>0.05).
4. Discussion
Our study shows that less than half (48.94%) of middle-aged and older adults use preventive care. This ratio is lower than the annual medical examination rate for the elderly in Shandong (76.2%) and Beijing (46.7%). It shows middle-aged and elderly people have insufficient preventive care use and cannot effectively play its role in promoting the health of middle-aged and elderly people. The higher rate of preventive care use among people aged 65 and above may be related to the free physical examination provided in basic public health services. Since the implementation of the China's New Healthcare Reform in 2009, preventive care has been provided free to seniors aged 65 and above in rural and urban areas.
In regard to community level social capital, the richness of facilities creates more opportunities for residents to interact and socialize. People from the group of rich in community facility use more preventive care services. The result is similar with previous studies that points out that investing in attractive playgrounds and recreations areas (i.e., material infrastructure) could potentially increase children's access to health promoting places and arenas for increasing social capital in their local environment (Eriksson and Dahlblom, 2020).
People from the group of rich in social activities participation use more preventive care services. This result is consistent with some of the previously studies, which found significant positive effects of social participation on preventive care use (Nieminen et al., 2013, Tashiro et al., 2017). The increase of social participation is related to more information exchanges, trust, and reciprocity. This is likely to come from players in community chess rooms and users of sports facilities. These people gather, share information, and exchange resources via common hobbies and fixed community places. Some residents not only stay at the level of participating in social activities but become organizers of the association. The intimacy and reciprocity of members in the association will be higher than ordinary neighbors. So, trust may have secretly planted seeds in people's hearts (Musalia, 2016) to change information and share resources on the basis of trust.
As an emotional dimension of social capital, social network is used to measure the degree of intimacy and trust of individuals in the social circle (Peng et al., 2019). Our results show social network has insignificant influence on preventive care use. The finding is similar with previous studies that found no significant association between social network and health promotion behaviors (Marquez et al., 2014) and most disease-specific preventive care uses, including flu shot, fecal occult blood test, colonoscopy, bone density test, pap test, breast exam (Peng and Lin, 2018). The effect of social networks on preventive care use may differ by gender and age. It is valuable to examine other aspects of social network that may influence preventive care use, such as specific interactions with network members in the further study.
Consistent with previous studies, we find that income, education, and marital status are positively correlated with preventive care use. The increase of income improves the economic accessibility of a person's preventive care use; in addition, the improvement of education level enhances a person's health awareness of using preventive care, thus generating a higher level of health investment. Spouses may provide information and companionship to individuals or motivate them to improve their health (Lau and Kirby, 2009). The existence of chronic diseases is related to most preventive care use. After suffering from a chronic disease, a person's health awareness may be stronger, so the probability of seeking preventive care is higher. At the same time, patients suffered from chronic diseases will also visit the hospital regularly, which is another channel for them to obtain knowledge and information related to preventive care use (Chen et al., 2013).
This study has some limitations. Firstly, due to the availability of data, preventive care includes only routine physical examinations in our study. Secondly, we focus on the overall preventive care use, did not consider specific preventive care items. In the end, due to the use of community data from 2011, there may be differences compared to real situation. However, the change in community facilities may not be excessive considering facility lifespan and stability of community facility planning (The People's Government of Beijing Municipality, 2022).
5. Conclusion
A total of 48.94% of the respondents have utilized preventive care. Our study provides evidence that community social capital and individual social activities participation are associated with the elderly's behavior of preventive care use. The association between social capital and preventive care use found in our study could be considered as an important factor when making policies to promote preventive care use. However, whether there is a causal relationship between the two requires further cohort studies to confirm.
CRediT authorship contribution statement
Liangru Zhou: Writing – original draft, Conceptualization, Methodology, Visualization, Investigation, Writing – review & editing. Peiyan Ju: Writing – original draft, Conceptualization, Methodology, Visualization, Investigation, Writing – review & editing. Yi Li: Writing – original draft, Conceptualization, Methodology, Visualization, Investigation, Writing – review & editing. Bingjie Liu: Data curation. Yan Wang: Data curation. Xin Zhang: Supervision, Writing – review & editing. Hui Yin: Supervision, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Liangru Zhou, Peiyan Ju and Yi Li contributed equally as the first authors. We thank the China Center for Economic Research, the National School of Development of Peking University for providing the data. https://charls.charlsdata.com/users/sign_up/agreement/en.html
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2023.102329.
Contributor Information
Xin Zhang, Email: zhangxinzhx0801@126.com.
Hui Yin, Email: enxuemama@163.com.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
The datasets analysed during the current study are available from the corresponding authors on reasonable request.
References
- Andresen E.M., Malmgren J.A., Carter W.B., Patrick D.L. Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am. J. Prev. Med. 1994;10(2):77–84. [PubMed] [Google Scholar]
- Bender A.M., Kawachi I., Jørgensen T., Pisinger C. Neighborhood social capital is associated with participation in health checks of a general population: A multilevel analysis of a population-based lifestyle intervention- the Inter99 study. BMC Public Health. 2015;15:694. doi: 10.1186/s12889-015-2042-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosio P., Blackwell C.N., Bowler G., Boyce T., Thurston H., Waugh J.J.S. Automated postnatal home blood pressure monitoring identifies significant cardiovascular disease. J. Obstet. Gynaecol. 2003;23(sup1):S15–S. [Google Scholar]
- Bourdieu P. The field of cultural production, or: The economic world reversed. Poetics. 1983;12(4-5):311–356. [Google Scholar]
- Chen C.-C., Lin Y.-J., Lin Y.-T. Awareness and utilization of preventive care services among the elderly under National Health Insurance. Int. J. Health Care Finance Econ. 2013;13(3-4):247–260. doi: 10.1007/s10754-013-9128-3. [DOI] [PubMed] [Google Scholar]
- Chuang Y.-C., Huang Y.-L., Tseng K.-C., Yen C.-H., Yang L.-H., Tang J.W. Social capital and health-protective behavior intentions in an influenza pandemic. PLoS One1. 2015;10(4):e0122970. doi: 10.1371/journal.pone.0122970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. 2nd ed. Lawrence Erlbaum Associates Publishers; 1988. Statistical power analysis for the behavioral sciences. https://doi.org/10.4324/9780203771587. [Google Scholar]
- Coleman, J.S., 1988. Social capital in the creation of human capital. 94, S95–- S120.
- Connolly D., Garvey J., McKee G. Factors associated with ADL/IADL disability in community dwelling older adults in the Irish longitudinal study on ageing (TILDA) Disabil. Rehabil. 2017;39(8):809–816. doi: 10.3109/09638288.2016.1161848. [DOI] [PubMed] [Google Scholar]
- Crookes D.M., Shelton R.C., Tehranifar P., Aycinena C., Gaffney A.O., Koch P., Contento I.R., Greenlee H. Social networks and social support for healthy eating among Latina breast cancer survivors: Implications for social and behavioral interventions. J. Cancer Surviv. 2016;10(2):291–301. doi: 10.1007/s11764-015-0475-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dean L., Subramanian S.V., Williams D.R., Armstrong K., Charles C.Z., Kawachi I. The role of social capital in African-American wome's use of mammography. Soc Sci Med. 2014;104:148–156. doi: 10.1016/j.socscimed.2013.11.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dean L.T., Subramanian S.V., Williams D.R., Armstrong K., Zubrinsky Charles C., Kawachi I. Getting black men to undergo prostate cancer screening: The role of social capital. Am. J. Mens Health. 2015;9(5):385–396. doi: 10.1177/1557988314546491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Souza, G., Dempsey, A., 2011. The role of HPV in head and neck cancer and review of the HPV vaccine[J]. Other 53 (Suppl 1). [DOI] [PMC free article] [PubMed]
- Eriksson M., Dahlblom K. Childre's perspectives on health-promoting living environments: The significance of social capital. Soc Sci Med. 2020;258 doi: 10.1016/j.socscimed.2020.113059. [DOI] [PubMed] [Google Scholar]
- Fuchs S.C., Alencastro P.R., Ike Da M., et al. Risk of coronary heart disease among HIV-infected patients: A multicenter study in Brazil[J] Sci. World J. 2013;2013 doi: 10.1155/2013/163418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukuyama, F., 1995. Social Capital and the Global Economy. 74, 89.
- Hale N.L., Smith M., Hardin J., Brock-Martin A. Rural populations and early periodic screening, diagnosis, and treatment services: Challenges and opportunities for local public health departments. Am. J. Public Health. 2015;105(Suppl 2):S330–S336. doi: 10.2105/AJPH.2014.302449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ichida Y., Kondo K., Hirai H., Hanibuchi T., Yoshikawa G., Murata C. Social capital, income inequality and self-rated health in Chita peninsula, Japan: A multilevel analysis of older people in 25 communities. Soc Sci Med. 2009;69:489–499. doi: 10.1016/j.socscimed.2009.05.006. [DOI] [PubMed] [Google Scholar]
- Imai C., Toizumi M., Hall L., et al. A systematic review and meta-analysis of the direct epidemiological and economic effects of seasonal influenza vaccination on healthcare workers[J] PloS one. 2018;13(6) doi: 10.1371/journal.pone.0198685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau D.T., Kirby J.B. The relationship between living arrangement and preventive care use among community-dwelling elderly persons. Am. J. Public Health. 2009;99(7):1315–1321. doi: 10.2105/AJPH.2008.151142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquez B., Elder J.P., Arredondo E.M., Madanat H., Ji M., Ayala G.X. Social network characteristics associated with health promoting behaviors among Latinos. Health Psychol. 2014;33(6):544–553. doi: 10.1037/hea0000092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng T., Chen H. A multilevel analysis of social capital and self-rated health: Evidence from China. Health Place. 2014;27:38–44. doi: 10.1016/j.healthplace.2014.01.009. [DOI] [PubMed] [Google Scholar]
- Moudatsou M.M., Kritsotakis G., Alegakis A.K., Koutis A., Philalithis A.E. Social capital and adherence to cervical and breast cancer screening guidelines: A cross-sectional study in rural Crete. Health Soc. Care Commun. 2014;22(4):395–404. doi: 10.1111/hsc.12096. [DOI] [PubMed] [Google Scholar]
- Musalia J. Social capital and health in Kenya: A multilevel analysis. Soc Sci Med. 2016;167:11–19. doi: 10.1016/j.socscimed.2016.08.043. [DOI] [PubMed] [Google Scholar]
- Nagaoka K., Fujiwara T., Ito J. Do income inequality and social capital associate with measles-containing vaccine coverage rate? Vaccine. 2012;30:7481–7488. doi: 10.1016/j.vaccine.2012.10.055. [DOI] [PubMed] [Google Scholar]
- National Bureau of Statistics of China. Statistical Bulletin of the People's Republic of China on National Economic and Social Development in 2021. Retrieved December 10, 2022 from http://www.gov.cn/xinwen/2022-02/28/content_5676015.htm.
- Nieminen T., Prättälä R., Martelin T., Härkänen T., Hyyppä M.T., Alanen E., et al. Social capital, health behaviors and health: A population-based associational study. BMC Public Health. 2013;13:613. doi: 10.1186/1471-2458-13-613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palanisamy B., Gopichandran V., Kosalram K. Social capital, trust in health information, and acceptance of Measles-Rubella vaccination campaign in Tamil Nadu: A case-control study. J. Postgrad. Med. 2018;64:212–219. doi: 10.4103/jpgm.JPGM_249_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng Y.-I., Chan Y.-S. Do Internet users lead a healthier lifestyle? J. Appl. Gerontol. 2020;39(3):277–284. doi: 10.1177/0733464818785797. [DOI] [PubMed] [Google Scholar]
- Peng Y.I., Lin T.F. Social capital and preventive care use among the elderly under Taiwan's National Health Insurance. Arch. Gerontol. Geriatr. 2018;75:28–36. doi: 10.1016/j.archger.2017.11.002. [DOI] [PubMed] [Google Scholar]
- Peng S., Yang X.Y., Rockett I.R.H. A typology of social capital and its mixed blessing for suicidal ideation: A multilevel study of college students. Soc. Sci. Med. 2019;243 doi: 10.1016/j.socscimed.2019.112640. [DOI] [PubMed] [Google Scholar]
- Prince M.J., Wu F., Guo Y., Gutierrez Robledo L.M., O'Donnell M., Sullivan R., Yusuf S. The burden of disease in older people and implications for health policy and practice. Lancet. 2015;385(9967):549–562. doi: 10.1016/S0140-6736(14)61347-7. [DOI] [PubMed] [Google Scholar]
- Putnam, R.D., 1993. The prosperous community: Social capital and public life. 13(Spring), Vol. 4.
- Rabehesketh, S., Skrondal, A., 2012. Multilevel and longitudinal modeling using Stata (3rd Edition). Stata Press. Volume I, Continuous Responses.
- Scheffler R.M., Brown T.T., Syme L., Kawachi I., Tolstykh I., Iribarren C. Community-level social capital and recurrence of acute coronary syndrome. Soc Sci Med. 2008;66:1603–1613. doi: 10.1016/j.socscimed.2007.12.007. [DOI] [PubMed] [Google Scholar]
- Shobugawa Y., Fujiwara T., Tashiro A., Saito R., Kondo K. Social participation and risk of influenza infection in older adults: A cross-sectional study. BMJ Open. 2018;8(1):e016876. doi: 10.1136/bmjopen-2017-016876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstein M., Gong C.H., Kendig H. Perceived availability of future care and depressive symptoms among older adults in China: Evidence from CHARLS. BMC Geriatr. 2020;20:31. doi: 10.1186/s12877-020-1435-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Story W.T. Social capital and the utilization of maternal and child health services in India: A multilevel analysis. Health Place. 2014;28:73–84. doi: 10.1016/j.healthplace.2014.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tashiro A., Aida J., Shobugawa Y., Fujiyama Y., Yamamoto T., Saito R., et al. Association between income inequality and dental status in Japanese older adults: Analysis of data from JAGES2013. Nihon Koshu Eisei Zasshi. 2017;64:190–196. doi: 10.11236/jph.64.4_190. [DOI] [PubMed] [Google Scholar]
- The People’s Government of Beijing Municipality. 2022. What is the service life of outdoor fitness facilities in the community? Retrieved March 20, 2023 from http://www.beijing.gov.cn/hudong/bmwd/jsjbmyyt/2022jmwd/tyjs2022/sqjsssygl2022/202210/t20221026_2845148.html.
- Tomazelli J.G., Silva G.A.E. Breast cancer screening in Brazil: An assessment of supply and use of Brazilian National Health System health care network for the period 2010–2012. Epidemiol. Serv. Saude. 2017;26:713–724. doi: 10.5123/S1679-49742017000400004. [DOI] [PubMed] [Google Scholar]
- Wang R., Chen Z., Zhou Y., Shen L., Zhang Z., Wu X. Melancholy or mahjong? Diversity, frequency, type, and rural-urban divide of social participation and depression in middle- and old-aged Chinese: A fixed-effects analysis. Soc. Sci. Med. 2019;238 doi: 10.1016/j.socscimed.2019.112518. [DOI] [PubMed] [Google Scholar]
- Wang H., Ying M.A., Meng C., Wei X.L., Zhao Y., Chen R., et al. A systematical review of social capital and mental health study for Chinese older people. Chin. J. Disease Control Prevent. 2013;17(4):336–340. [Google Scholar]
- Wiltshire G., Lee J., Evans J. ‘You don’t want to stand out as the bigger one’: Exploring how PE and school sport participation is influenced by pupils and their peers. Phys. Educ. Sport Pedagog. 2017;22(5):548–561. [Google Scholar]
- Yan Y., Du Y., Li X., Ping W., Chang Y. Physical function, ADL, and depressive symptoms in Chinese elderly: Evidence from the CHARLS. Front. Public Health. 2023;11:1017689. doi: 10.3389/fpubh.2023.1017689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou L., Ma X., Wang W. Relationship between cognitive performance and depressive symptoms in Chinese older adults: The China Health and Retirement Longitudinal Study (CHARLS) J. Affect. Disord. 2021;281:454–458. doi: 10.1016/j.jad.2020.12.059. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets analysed during the current study are available from the corresponding authors on reasonable request.