Abstract
Aim:
To explore patients’ follow-up preferences.
Background:
Optimal follow-up strategies for patients with coeliac disease remain a subject of debate. Research suggests patients’ prefer review by dietitians with a doctor available as required.
Methods:
Patients with coeliac disease under review at our centre, completed a questionnaire assessing their views on what makes follow-up useful based on specific criteria. Bloods tests, symptoms review, dietary assessment, opportunity to ask questions and reassurance. Patients’ preferences between follow-up with a hospital doctor, a hospital dietitian, a hospital dietitian with a doctor available, a general practitioner, no follow-up or access when needed were also evaluated.
Results:
138 adult patients completed the questionnaire, 80% of patients reported following a strict gluten free diet (mean diagnosis was 7.2 years). Overall, 60% found their follow-up to be ‘very useful’ valuing their review of blood tests and symptoms (71%) reassurance (60%) and opportunity to ask questions (58%). Follow-up by a dietitian with a doctor available was the most preferred option of review (p<0.001) except when compared to hospital doctor (p=0.75). Novel modalities of follow-up such as telephone and video reviews were regarded as of equal value to face-to-face appointments (65% and 62% respectively). Digital applications were significantly less preferable (38%, p<0.001).
Conclusion:
Follow-up by a dietitian with a doctor available as needed was the most preferred follow-up method. However, in this study follow-up by a dietitian with doctor available and hospital doctor alone was statistically equivalent. Many patients consider telephone and video follow-up of equal value to face-to-face reviews.
Key Words: Celiac disease, Follow up, Gluten-free diet
Introduction
Coeliac disease (CD) is an autoimmune disorder that results from the consumption of gluten in genetically susceptible individuals and is increasing in prevalence (1). Once diagnosis has been established by a gastroenterologist, the cornerstone of treatment remains a lifelong strict gluten-free (GFD) (2, 3). Coeliac disease is routinely described as a ‘clinical chameleon’ in that it may present both symptomatically, asymptomatically as well as in potential or in refractory forms (4). The heterogeneity of its presentation is also reflected in the way CD is managed in clinical follow up, with patients being reviewed across primary and secondary care by various healthcare practitioners.
International guidelines endorse involvement of specialist dietitians at the time of diagnosis to educate patients on a successful transition to the GFD whilst maintaining overall healthy dietary patterns. As well as regular (usually annual) follow-up of patients to support ongoing adherence and minimise the risk of comorbidities associated with CD (5, 6). Suggested elements of follow-up in patients with coeliac disease include anthropometrics, serological review, assessment of dietary adherence, nutritional adequacy and treatment burden (7). A previous study from 2006 demonstrated that patients preferred modality of follow-up was with a specialist dietitian supported by an ‘interested’ gastroenterologist as required (8).
There has been much debate in the published literature as to the optimal timing and components of follow-up. Particularly in relation to the clinicians involved, location (primary versus secondary care) time between appointments, and CD outcome measures (8–11). Equally several international surveys have demonstrated current guidelines are not being achieved, with up to as many as 40% of patients receiving no dietetic input and often being lost to follow-up in primary care (10, 12–14). Finally, it is crucial to state that whilst there is no high-quality evidence to suggest that regular follow-up improves adherence or reduces the development of complications, a high proportion of patients value follow up appointments (8, 15).
Adherence to a GFD has been shown to be between 42% and 91% globally (16). A recent review of barriers and facilitators to the GFD employed a social ecological model and identified poor labelling laws, lower-incomes, cultural barriers, and the perceived difficulty of the GFD as some of the main barriers to the approach. Conversely adequate follow-up and on-going support with the GFD were considered important facilitators to long term adherence (17).
The variable rates of adherence to the gluten-free diet could be, at least partially, explained by the inconsistent approaches to follow-up. A large national survey of follow-up in CD care demonstrated up to UK 50% of hospital trusts have no specific pathway for patients with CD (12, 17). This is despite international guidelines emphasising the importance of patients having a thorough education of the gluten-free approach by a specialist dietitian on diagnosis as well as ongoing dietetic support at follow-up (18, 19).
A combination of underfunding and lack of consensus regarding the optimal components of follow-up has led to the consideration of new treatment modalities that acknowledge the heterogeneity in this cohort of patients in relation to different levels of dietary adherence and perceived treatment burden (20, 21). There is an emerging view that limited resources should be targeted towards patients with the most barriers to successful disease management (22).
Equally, in recent years (and accelerated during the COVID-19 pandemic) there has been a shift towards the use of group education as well as digital modalities to support patients with CD (23, 24). Since these major changes in healthcare delivery, UK patient preferences for follow-up have not been assessed. This current study aimed to provide an updated analysis of patients’ views on the follow-up of their coeliac disease with an additional focus on newer approaches to patient review.
Methods
We are designated by NHS England as the National Centre for Coeliac Disease (NCCD), a tertiary referral centre for non-responsive, refractory and complex coeliac disease cases. However, we also provide services for our local region. Our coeliac database contains more than 3000 patients (10% of which are from across England), it includes demographics as well as referral, serological and histological data. Locally we diagnose approximately 100 - 160 patients per year. Once the diagnosis is confirmed patients are first seen by a gastroenterologist (at their discretion a DXA scan may be arranged). Thereafter, patients are seen in two dietetic appointments. The dietitian covering the coeliac clinic is able to order serology related to coeliac disease follow up. This includes coeliac antibodies as well as haematinics and vitamin D. If the patient is deemed to be stable, they are discharged to community with access to our secondary services if required.
Patients were selected to be representative of a range of time since diagnosis, in conjunction with serologically and histopathology confirmed disease. Three hundred and twenty-three patients were contacted and 138 patients were included (43% response rate). The participants completed a paper-based questionnaire that explored their current adherence to the GFD (using the validated Biagi adherence score) and views on the ‘overall usefulness’ of their follow-up; they were asked to grade specific elements: (1) General reassurance; (2) Annual review of symptoms and blood tests; (3) Opportunity for dietary review; (4) Chance to ask questions about their condition; (5) Chance to ask questions about their diet (8, 25).
Furthermore, their preferences in relation to methods of follow up; clinicians, location, frequency, and acceptability of non-traditional approaches were also surveyed. This incorporated acceptability of follow-up by telephone, video appointments and mobile digital applications from a conceptual perspective. We compared these preferences in patients who had been diagnosed for more than 5 years against those with a more recent diagnosis (<5 years). This approach was replicated from the methodology of Bebb et al (2006) (8).
Statistical analysis
All data was analysed using EXCEL version 16.42 (Microsoft 2020) and were summarized using descriptive statistics. Continuous demographic and serological data were compared using t-tests and presented with means and ± standard deviations (SD). Statistical significance was considered when p <0.05. We used the Wilcoxon signed rank test to statistically assess differences in response when analysing preferred mode of follow-up. Comparisons between categorical data were performed using Fishers exact test.
Ethics
The database is approved by the Yorkshire and Humber Research Ethics committee and registered with the local research and development department of Sheffield Teaching Hospital NHS Foundation Trust (REC reference 19/YH/0095 and CEU ref 11075).
Results
A hundred and thirty-eight patients completed the questionnaire during the COVID-19 pandemic. The demographics of the patients are summarised in Table 1. Mean length of diagnosis was 7.2 years.
Table 1.
The demographics of the patients
| Age (yr), Mean ± SD | 53 ± 18.6 |
|---|---|
| Sex [M:F] | 52:86 |
| Weight (kg), mean ± SD | 69.9 ± 17.4 |
| BMI (kg/m2), mean ± SD | 24.9 ± 5.3 |
| Mean length of diagnosis (yr) Percent diagnosed <5 years Percent diagnosed >5 years |
7.2 61% 39% |
| Education (%) | |
| MSc or Higher BSc HND A Levels GCSE / O Levels NVQ No Qualifications |
22 19 9 12 20 13 5 |
| Marital Status (%) | |
| Married (or living as married) Divorced Single Widow |
57 22 16 5 |
| Comorbidities on Diagnosis (%) | |
| Type 1DM Type 2DM Anaemia Hypothyroidism Hyperthyroidism Osteoporosis Migraines Diverticular disease Reflux Bowel disease† |
4 4 34 14 2 23 20 8 33 8 |
| Ethnicity (%) | |
| White Afro Caribbean African Asian Chinese Other |
95 0 1 1 1 2 |
†All patients specifying, they had some form of ‘bowel disease’ was related to a diagnosis of IBS prior to they’re diagnosis of CD.
Adherence to the gluten-free diet
Assessment of the patient’s adherence to the GFD indicated 80% (109 of 136) reported following a strict gluten-free diet, 3% (4 of 136) reported partial adherence and 17% (23 of 136) were not following a GFD.
Follow up pattern
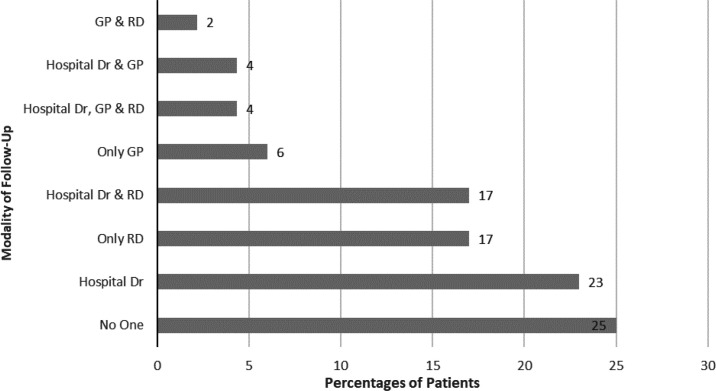
The frequency of different follow-up modalities is summarised in Figure 1. Overall, 75% of patients were under some form of regular follow-up. The most common modality of ‘single’ clinician follow-up was hospital doctor (23%), dietitians were involved in follow-up care in 34% of cases (17% were solely under review by dietitians). Twenty-seven percent of patients were under follow-up of more than one clinician with 10% occurring across both primary and secondary care.
Figure 1.
Reported modalities of coeliac follow up clinics (n=138) (GP – General Practitioner, RD – Register Dietitian)
Patients who were followed up by hospital doctors saw the same doctor 60% of the time. When patients who saw multiple doctors at hospital follow-up 41 % reported this lack of continuity made the consultations less useful.
Patients views on usefulness of follow-up
Table 2 summarises patients’ views on their follow-up. 75% percent of patients found follow-up overall useful or very useful. Specific aspects of follow-up that patients reported as most helpful were review of their symptoms and relevant serology (71%), general reassurance (60%) and opportunities to ask questions about their CD (58%). Opportunity for dietary review and to ask questions in relation to the GFD were considered very useful by 45% and 41% of the patients respectively.
Table 2.
Patient views on usefulness of various aspects of all coeliac follow-up clinics
| Aspect of Clinic | Usefulness of Different Clinic Aspects (5 = Very Useful, 1 = Not Useful at All) |
||||
|---|---|---|---|---|---|
| 5 | 4 | 3 | 2 | 1 | |
| Overall usefulness (n=126) | 76 (60) | 19 (15) | 16 (13) | 6 (5) | 9 (7) |
| General reassurance (n=133) | 80 (60) | 14 (11) | 13 (10) | 10 (8) | 16 (12) |
| Symptom’s review / blood test (n=129) | 91 (71) | 11 (9) | 12 (9) | 6 (5) | 9 (7) |
| Opportunity for dietary review (n=130) | 58 (45) | 21 (16) | 20 (15) | 7 (5) | 24 (18) |
| Opportunity to ask questions about the condition (n=132) | 77 (58) | 19 (14) | 15 (11) | 7 (5) | 14 (11) |
| Opportunity to ask questions about diet (n=120) | 49 (41) | 15 (13) | 19 (16) | 11 (9) | 26 (22) |
Patients were asked to grade each aspect of the clinic from 5 (very useful) to 1 (not useful at all).
Percentage values are given in parentheses.
A sub-analysis of follow up by dietitian alone, indicated dietary review was considered useful by patients at 53%.
Follow-up preference and alternative modalities of follow-up
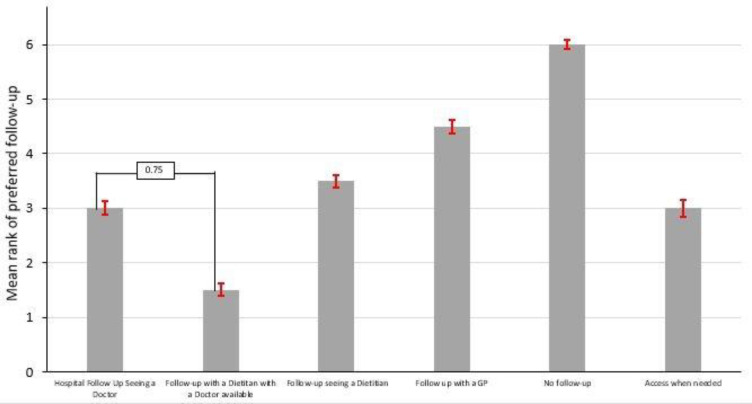
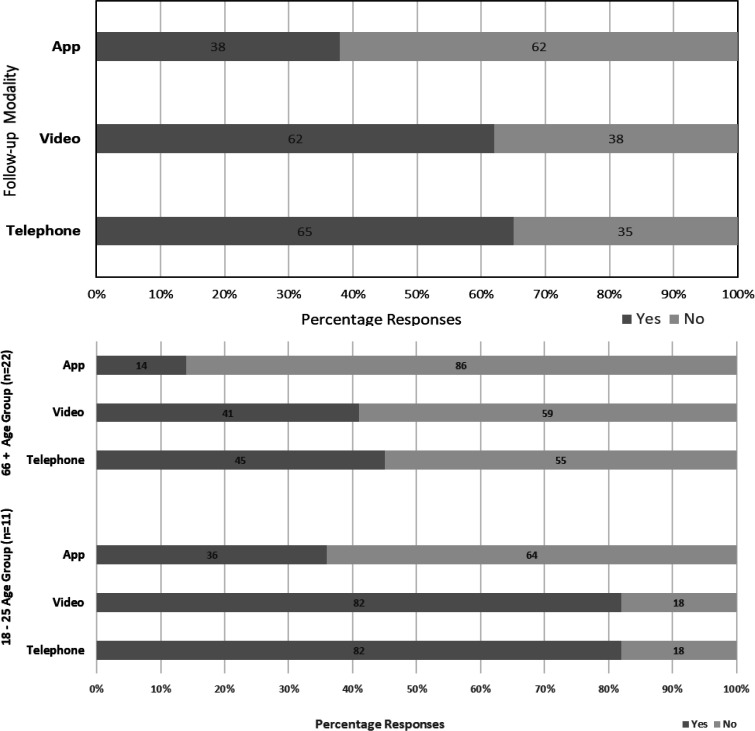
Follow-up by a dietitian with a doctor available when necessary was the statistically preferred option over most other choices (P<.001. Figure 2). However, this option was not statistically preferable to follow-up by a hospital doctor alone (P=0.75). There were no differences in response pattern between those diagnosed more recently (<5 years) to those diagnosed more than 5 years ago. In relation to novel methods of follow up; telephone and video appointments (65% and 62% respectively) were preferred over the use of digital applications (38%. Figure 3 upper), P<.001.
Figure 2.
Patients preferred follow-up pattern (n=122). Data are expressed as standard error of the mean (±S.E.M). Patients graded preferred follow options from 1 to 6 (1 = most preferred, 6 = least preferred). Follow up by a dietitian with a doctor available as needed was the most preferred follow-up method. Statistically this was preferable against all other follow-up modalities, except for follow-up by a hospital doctor
Figure 3 (Upper figure).
Responses to the question “Are telephone, video and digital application follow up equally useful to face-to-face appointments?” (n=92) (*Telephone and video follow-up were statistically preferable over digital applications (P<.001)). (Lower figure). Responses to the question “Are telephone, video and digital application follow up equally useful to face-to-face appointments?” by youngest to oldest age groups (n=33) (* Difference in preferences statistically significant (P=0.03) Fisher Exact Test)
However, preferences were different between the youngest (18- to 25-year-olds; n=11) to the oldest (>66 years old; n=22) age groups; 82% of 18 to 25-year-olds considered telephone or video follow-up as useful as traditional appointments whereas in the over 66-year-old group only 45% and 41% considered telephone and video reviews equally as useful (Figure 3 (lower figure)). The differences in preferences for video consultation between these age groups where statistically significant (P=0.03).
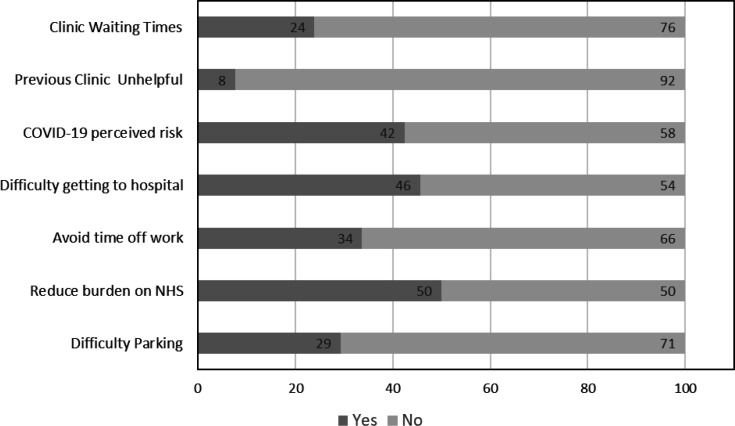
The most common stated reason for considering alternatives to traditional face-to-face follow-up appointments were to reduce the burden on the NHS (50%), difficulty getting to hospital (46%) and reduction of perceived COVID-19 risk (42%. Figure 4). An annual review was the preferred frequency of follow up (68%), compared with more than once a year (8%) or less than once a year (24%).
Figure 4.
Responses to the question “What are your reasons for considering alternatives to traditional face-to-face follow-up appointments?” (n = 92)
A sub-analysis of the participants not following the GFD did not demonstrate any statistical difference in preference for “no follow-up’ as an option.
Discussion
This is the first study to describe follow-up preferences for patients with coeliac disease with specific reference to novel modalities since the start of the Covid-19 pandemic. Our study demonstrated that a majority of patients were willing to accept follow-up through non-traditional methods such as telephone or video reviews (65% and 62% respectively). Follow-up via mobile digital application was the least preferred non-traditional option at 38%. Disparities in the preference for non-traditional follow-up methods became more distinct when comparing the youngest (18-25 years old) versus the oldest age group (>66 years old). This may represent some aspect of the digital divide; low levels of digital literacy, poor access to information and communication technology, as well as concerns about privacy of data are established reasons that may potentially limit the uptake of these non-traditional methods of follow up with subsets of the coeliac population (26, 27). As the patient population in the current study was 95% white no inferences could be made about follow-up preference based on ethnicity, this is an area future research needs to focus on.
Previous work has identified the potential benefit of novel, non-face-to-face, clinics for both patients and clinical services including cost effectiveness, extended access to specialist services and mitigation against clinician shortages (28, 29). Telephone clinics specifically have been demonstrated to improve adherence to the GFD (24). The current study demonstrates patient support for these approaches, although interestingly the most stated reason for patients wishing to use novel approaches to follow up was to reduce the burden on the NHS.
Annual follow up appointments were the preferred frequency for the majority (68%), previous studies have indicated 61% want annual follow up appointments, and 85% considered annual reviews important in managing their coeliac disease.15,30 Given the current study and others consistently demonstrated patient’s preference for annual review, coupled with existing limits in dietetic resources, further research is required to substantiate the need for novel forms of review to support patients preferred level of follow up.
Studies generally show a wide range of heterogeneity and adherence to the GFD. The 17% non-adherence rate in this study is a lower figure compared to some of the published literature on adherence (31, 32). The relatively high rate of adherence (80% strict and 3% partial) amongst this cohort maybe partially explained; as the NHS England National Centre for Coeliac Disease, we have historically offered ongoing yearly review for patients diagnosed with coeliac disease and 75% of patients reported being under regular follow up.
Interestingly, 27% of the patients were under follow-up of more than one clinician and 10% was occurring across both primary and secondary care. Although this may be partially explained by the need for both dietetic and medical review with some patients it also suggests the possibility that services could be further restructured to ensure continuity and reduction in of duplication of care. Certainly, patients in secondary care (41%) considered continuity of follow up to be important and found review by multiple doctors reduced its usefulness, a previous study reported the preference for the same healthcare professional to be as high as 75% (15).
Irrespective of location or clinician 60% of patients found follow-up very useful, specifically the opportunity for general reassurance as well as a review of symptoms and serology. This is interesting particularly in relation to two aspects. Patients’ preference to have the repeat measures of their coeliac serology (tissue transglutaminase and endomysial antibodies) may reflect historical clinical practice that viewed them as a reliable measure of dietary adherence and mucosal recovery. However, a systematic review has demonstrated that negative serology should not be used as a surrogate marker in this way (33). Equally this highlights the on-going need for specialist dietitians within CD follow up who can contextualise serological results in relation to individual’s dietary intake (31). The opportunity to ask questions about the GFD and undergo dietary review were considered somewhat less useful at 41 and 45% respectively, this could reflect the variable levels of dietary expertise available within the GP or hospital doctor clinic appointments.
As with previous surveys we demonstrated that patients prefer to have specialist dietetic follow-up in secondary care with a hospital doctor available as required. However the difference in the current survey was this option was not statistically preferred over follow-up by hospital doctor alone (8). We hypothesise possible reasons for this may include the greater percentage of patients who have been receiving doctor follow-up alone (23% vs 17%) and some element of selection bias due to the specialist nature of our centre.
Given the increase in the prevalence of coeliac disease and, the substantial shift towards digital technology in healthcare, a significant proportion of patients view novel methods of follow-up such as telephone, video and (to a lesser extent) digital mobile application as of equal value to traditional face-to-face follow-up.
However, it is possible, the unique circumstances of the COVID pandemic may have influenced patients’ preferences.
Conclusion
In conclusion the current study supports previous work that follow-up by a dietitian with a doctor available as needed was the most preferred follow-up method. However, in this study follow-up by a dietitian with doctor available and hospital doctor alone was statistically equivalent. These findings could support the follow up of patients with coeliac disease in a nutrition clinic.
Equally, it is important to note that ‘access when required’ was also rated highly as a follow a preference. This deviates from the recommendation in many guidelines for annual review. If a subset of patients with quiescent disease would prefer access when required, this could improve the capacity of coeliac services to manage complex and non-responsive cases.
Future studies should be undertaken to clarify the acceptability of these modalities post the COVID pandemic and in different subsets of patient populations as well as additional clinical trials to determine their overall efficacy.
Conflict of interests
D.S.S. receives an educational grant from Schär (a gluten-free food manufacturer). The remaining authors disclose no conflicts.
References
- 1.King JA, Jeong J, Underwood FE, Quan J, Panaccione N, Windsor JW, Coward S, et al. Incidence of celiac disease is increasing over time: a systematic review and meta-analysis. Am J Gastroenterol. 2020;115:507–525. doi: 10.14309/ajg.0000000000000523. [DOI] [PubMed] [Google Scholar]
- 2.Oxentenko AS, Rubio-Tapia A. Celiac disease. Mayo Clin Proc. 2019;94:2556–2571. doi: 10.1016/j.mayocp.2019.02.019. [DOI] [PubMed] [Google Scholar]
- 3.Baggus EMR, Hadjivassiliou M, Cross S, Penny H, Urwin H, Watson S, Woodward JM, Sanders DS. How to manage adult coeliac disease: perspective from the NHS England Rare Diseases Collaborative Network for Non-Responsive and Refractory Coeliac Disease. Frontline Gastroenterol. 2020;11:235–242. doi: 10.1136/flgastro-2019-101191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ben HT, Admou B. Celiac disease: understandings in diagnostic, nutritional, and medicinal aspects. Int J Immunopathol Pharmacol. 2021;35:1–22. doi: 10.1177/20587384211008709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Husby S, Murray JA, Katzka DA. AGA clinical practice update on diagnosis and monitoring of celiac disease - changing utility of serology and histologic measures: expert review. Gastroenterology. 2019;156:885–889. doi: 10.1053/j.gastro.2018.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ludvigsson JF, Bai JC, Biagi F, Card TR, Ciacci C, Ciclitira PJ, Green PHR, et al. Diagnosis and management of adult coeliac disease: Guidelines from the British society of gastroenterology. Gut. 2014;63:1210–1228. doi: 10.1136/gutjnl-2013-306578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Husby S, Bai JC. Follow-up of celiac disease. Gastroenterol Clin North Am. 2019;48:127–136. doi: 10.1016/j.gtc.2018.09.009. [DOI] [PubMed] [Google Scholar]
- 8.Bebb JR, Lawson, Knight AT, Long RG. Long-term follow-up of coeliac disease - What do coeliac patients want? Aliment Pharmacol Ther. 2006;23:827–831. doi: 10.1111/j.1365-2036.2006.02824.x. [DOI] [PubMed] [Google Scholar]
- 9.Lexner J, Hjortswang H, Ekesbo R, Sjöberg K. Well-being and dietary adherence in patients with coeliac disease depending on follow-up. Scand J Gastroenterol. 2021;56:382–390. doi: 10.1080/00365521.2021.1889024. [DOI] [PubMed] [Google Scholar]
- 10.Pritchard L, Waters C, Murray IA, Bebb J, Lewis S. Comparing alternative follow-up strategies for patients with stable coeliac disease. Frontline Gastroenterol. 2020;11:93–97. doi: 10.1136/flgastro-2018-101156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Muhammad H, Reeves S, Ishaq S, Jeanes Y. Experiences of outpatient clinics and opinions of telehealth by Caucasian and South Asian patients’ with celiac disease. J. Patient Exp. 2021;8:1–7. doi: 10.1177/23743735211018083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rej A, Buckle RL, Shaw CC, Trott N, Urwin H, McGough N, et al. National survey evaluating the provision of gastroenterology dietetic services in England. Frontline Gastroenterol. 2020;5:380–384. doi: 10.1136/flgastro-2020-101493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nelson M, Mendoza N, McGough N. A survey of provision of dietetic services for coeliac disease in the UK. J Hum Nutr Diet. 2007;20:403–11. doi: 10.1111/j.1365-277X.2007.00813.x. [DOI] [PubMed] [Google Scholar]
- 14.Halmos EP, Deng M, Knowles SR, Sainsbury K, Mullan B, Tye-Din JA. Food knowledge and psychological state predict adherence to a gluten-free diet in a survey of 5310 Australians and New Zealanders with coeliac disease. Aliment Pharmacol Ther. 2018;48:78–86. doi: 10.1111/apt.14791. [DOI] [PubMed] [Google Scholar]
- 15.S Kallos, Jeanes Y. Cross-sectional survey of the dietetic provision for adults with coeliac disease in the UK. J Hum Nutr Diet. 2020;33:6–15. [Google Scholar]
- 16.Hall NJ, Rubin G, Charnock A. Systematic review: adherence to a gluten-free diet in adult patients with coeliac disease. Aliment Pharmacol Ther. 2009;30:315–330. doi: 10.1111/j.1365-2036.2009.04053.x. [DOI] [PubMed] [Google Scholar]
- 17.Abu‐Janb N, Jaana M. Facilitators and barriers to adherence to gluten‐free diet among adults with celiac disease: a systematic review. J Hum Nutr Diet. 2020;33:786–810. doi: 10.1111/jhn.12754. [DOI] [PubMed] [Google Scholar]
- 18.National Institute for Health, Care Excellence (NICE) Coeliac disease: recognition, assessment and management. NG20. 2015 [PubMed] [Google Scholar]
- 19.Rubio-Tapia A, Hill ID, Kelly CP, Calderwood AH, Murray JA. American college of gastroenterology clinical guideline: diagnosis and management of celiac. Am J Gastroenterol. 2013;108:656–76. doi: 10.1038/ajg.2013.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lundin KE, Kelly CP, Sanders DS, Chen K, Kayaniyil S, Wang S. Understanding celiac disease monitoring patterns and outcomes after diagnosis: a multinational, retrospective chart review study. World J Gastroenterol . 2021;27:2603–2614. doi: 10.3748/wjg.v27.i20.2603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Megen FV, Skodje GI, Skodje GI, Stendahl M, Veierød MB, Lundin KEA, eat al. High disease burden in treated celiac patients – a web-based survey. Scand J Gastroenterol. 2021;0:1–7. doi: 10.1080/00365521.2021.1930146. [DOI] [PubMed] [Google Scholar]
- 22.Rodríguez-Herrera A, Reyes-Andrade J, Rubio-Escudero C. Rationale for timing of follow-up visits to assess gluten-free diet in celiac disease patients based on data mining. Nutrients. 2021;13:1–8. doi: 10.3390/nu13020357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rej A, Trott N, Kurien M, Branchi F, Richman E, Subramanian S, et al. Is peer support in group clinics as effective as traditional individual appointments? the first study in patients with celiac disease. Clin Transl Gastroenterol. 2020;11:1–6. doi: 10.14309/ctg.0000000000000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Muhammad H, Reeves S, Ishaq S, Mayberry JF, Jeanes YM. Telephone clinic improves gluten-free dietary adherence in adults with coeliac disease: sustained at 6 months. Frontline Gastroenterol. 2020;7:586–592. doi: 10.1136/flgastro-2020-101643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Biagi F, Bianchi PI, Marchese A, Trotta L, Vattiato C, Balduzzi D, et al. A score that verifies adherence to a gluten-free diet: A cross-sectional, multicentre validation in real clinical life. Br J Nutr. 2012;108:1884–1888. doi: 10.1017/S0007114511007367. [DOI] [PubMed] [Google Scholar]
- 26.Mackert M, Mabry-Flynn A, Champlin S, Donovan EE, Pounders K. Health literacy and health information technology adoption: the potential for a new digital divide. J Med Internet Res. 2016;18:1–16. doi: 10.2196/jmir.6349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ellins J, Land D, Sieff A, Coulter A. Making the case for information. Patient Information Forum (PIF) 2013 [Google Scholar]
- 28.Kichloo A, Albosta M, Dettloff K, Wani F, El-Amir Z, Singh J, et al. Telemedicine, the current COVID-19 pandemic and the future: a narrative review and perspectives moving forward in the USA. Fam Med Community Health. 2020;8:1–9. doi: 10.1136/fmch-2020-000530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stuckey, C Management of adult coeliac disease with a dietitian-led virtual clinic. Gastrointest Nurs. 2015;13:38–43. [Google Scholar]
- 30.Crocker H, Jenkinson C, Peters M. Healthcare experiences and quality of life of adults with coeliac disease: a cross-sectional study. J Hum Nutr Diet. 2020;33:741–751. doi: 10.1111/jhn.12757. [DOI] [PubMed] [Google Scholar]
- 31.Sanders DS, Karajeh MA, Hurlstone DP. Letter to the editor: Empathy, empowerment, political will and a coeliac specialist dietitian in every hospital? J Hum Nutr Diet. 2005;18:467–468. doi: 10.1111/j.1365-277X.2005.00653.x. [DOI] [PubMed] [Google Scholar]
- 32.See JA, Kaukinen K, Makharia GK, Gibson PR, Murray JA. Practical insights into gluten-free diets. Nat. Rev. Gastroenterol Hepatol. 2015;12:580–591. doi: 10.1038/nrgastro.2015.156. [DOI] [PubMed] [Google Scholar]
- 33.Silvester JA, Kurada S, Szwajcer A, Kelly CP, Leffler DA, Duerksen DR. Tests for serum transglutaminase and endomysial antibodies do not detect most patients with celiac disease and persistent villous atrophy on gluten-free diets: a meta-analysis. Gastroenterology. 2017;153:689–701. doi: 10.1053/j.gastro.2017.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]