ABSTRACT
We report a case of a metallic intraocular foreign body (IOFB) retained in the anterior chamber (AC) angle that was masquerading as herpetic stromal keratitis. A 41-year-old male construction worker was referred to our ophthalmology clinic with the complaint of consistent blurred vision for 3 days in his left eye. He had no history of ocular trauma. The best-corrected visual acuity was found to be 10/10 in the right eye and 8/10 in the left eye. On slit-lamp examination of the anterior segment, the right eye was normal, while the left eye showed unilateral corneal edema and scarring, anterior lens capsule opacification, +2 cells in the AC, and the Seidel test was negative. Fundus examination was normal bilaterally. Despite there not being history of it, we still suspected ocular trauma considering the patient’s occupational risk. Consequently, an orbital computed tomography imaging was performed which revealed a metallic-IOFB in the inferior iridocorneal angle. On the second follow-up day, the corneal edema regressed, and a gonioscopic examination of the affected eye was performed, showing a small foreign body embedded in the inferior iridocorneal angle of the AC. Subsequently, the IOFB was surgically removed using Barkan lens, and excellent visual results were achieved. This case emphasizes the importance of considering IOFB in the differential diagnosis of patients with unilateral corneal edema and anterior lens capsule opacification. Furthermore, the presence of IOFB should be definitely excluded in patients with occupational risk of ocular trauma even if there is no history of trauma. More awareness about the proper use of eye protection should be raised to circumvent penetrating ocular-trauma.
Keywords: Anterior capsule opacification, anterior chamber, corneal edema, herpetic keratitis, intraocular foreign body, ocular trauma
INTRODUCTION
Penetrating ocular trauma with intraocular foreign body (IOFB) is a potentially vision-threatening injury that requires prompt diagnosis and treatment. Estimates of the incidence of IOFBs in cases of open globe injury vary from 16% to 41%.[1] The occurrence of IOFBs is mostly associated with work-related injuries and is predominantly found in young male patients (92%–100%).[2] The majority (58%–88%) of IOFBs are seen in the posterior segment, whereas only 10%–15% reside in the anterior chamber (AC).[2] Detecting IOFBs in the AC angle can be particularly challenging.[2] It is imperative to have a high degree of clinical suspicion for IOFBs in patients with ocular trauma or engage in high-risk activities, as some occult IOFBs may be asymptomatically retained.[1-3]
CASE REPORT
A 41-year-old male patient who works in construction was referred to our ophthalmic clinic with an initial diagnosis of herpetic stromal keratitis. He complained of persistent blurred vision in his left eye for 3 days with no history of ocular trauma, pain, or foreign body sensation in the affected eye. The patient admitted to not using protective eyewear while working. On initial examination, the patient’s best-corrected visual acuity was 10/10 in the right eye and 8/10 in the left eye. Examination of the AC of the patient’s right eye using a slit-lamp biomicroscope was unremarkable. In contrast, examination of the left eye revealed corneal edema and scarring, as shown in Figure 1a. The Seidel test was negative, +2 cells were present in the AC, with minimal opacification observed in the anterior lens capsule, as depicted in Figure 1b. He had sensation in the left cornea upon stimulation with a cotton wisp. Fundoscopic examination of both eyes did not reveal any abnormalities.
Figure 1.
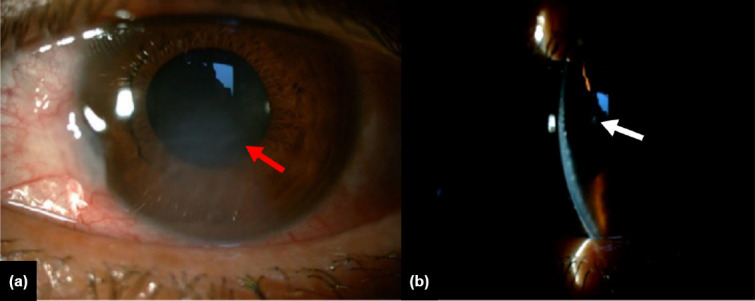
Biomicroscopic image of the patient’s left eye: (a) showing corneal edema and scarring (red arrow); and (b) showing anterior lens capsule opacification (white arrow).
Due to the patient’s occupation, a penetrating eye injury was suspected, and a non-contrast orbital computed tomography (CT) scan was ordered to exclude the possibility of an IOFB. The CT scan revealed a single small radiopaque IOFB (Fig. 2a). The patient was given topical moxifloxacin, prednisolone acetate, cyclopentolate; tetanus prophylaxis; and oral moxifloxacin as prophylaxic measure against endophthalmitis. On the second follow-up day, the corneal edema regressed, and a gonioscopic examination of the affected eye was performed. The examination revealed the presence of a small foreign body embedded in the inferior iridocorneal angle of the AC at the 6 o’clock position (Fig. 2b).
Figure 2.

(a) Non-contrast CT scan showing an intraocular foreign body (red arrow) (b), Gonioscopic photo of the foreign body in the angle of the anterior chamber of the left eye (white arrow) (c), Imaging of the foreign body at the iridocorneal angle with the Barkan lens during the surgical operation (blue arrow). CT: Computed tomography.
The patient underwent surgery in a timely manner, and with the assistance of a Barkan lens, the metallic foreign body was successfully extracted (Fig. 2c). At his 1-year postoperative follow-up visit, the patient’s visual acuity was 10/10 in his left eye, with no complications (e.g., infections or any sign of traumatic cataract).
DISCUSSION
There is a paucity of reports in the literature that document cases with IOFBs located in the AC. This patient had a metallic foreign-body pierce through the cornea, then collide against the anterior lens capsule before descending into the inferior chamber angle, which was impossible to detect on slit-lamp examination. The patient’s occupation suggests that this injury was likely work related and went unnoticeable. The patient denies any history of ocular trauma, pain, or foreign body sensation in his affected eye. Therefore, it is of paramount importance that physicians maintain a high level of suspicion for IOFBs in all patients with significant occupational risk (e.g. construction workers, metal workers, and stone cutters) who complain of any ocular symptoms, even if they deny ocular trauma or the possibility of IOFBs.[1]
When suspecting an IOFB, all physicians should begin by obtaining a thorough medical history, paying special attention to potential occupational risks that may provide insight into the possible mechanism of the injury, and the nature and location of the IOFB.[4] If a patient describes a high-velocity mechanism such as hammering or grinding, the physician should become increasingly suspicious of an IOFB. A comprehensive ocular examination should be performed; this includes external inspection of the affected eye, visual acuity, slit-lamp examination, and fundus examination. Gonioscopy should also be performed to visualize IOFBs that might be missed by slit examination, as long there is no risk of extrusion of intraocular content.[1,2]
Finally, proper ocular imaging modalities are essential to corroborate the diagnosis and rule out additional IOFBs. CT has become the predominant imaging technique in cases of ocular trauma.[4] Alternatively, ultrasonography (US) could be used in cases where the IOFB cannot be visualized with a CT scan (e.g. glass or plastic). It may also be used in adjunct with CT. US offers the added advantage of real-time, high-resolution (0.01–0.1mm) imaging from various angles and detecting coexisting intraocular pathologies (retinal/choroidal detachment or vitreous hemorrhage). Extra care should be taken when selecting eyes for the US examination as the probe’s pressure poses the risk of extruding globe contents.[2,4] Magnetic resonance imaging is generally contraindicated to avoid the risk of inadvertent damage to the intraocular structures by the movement of a ferromagnetic foreign body.[4]
As a general rule, it is recommended that all patients with IOFBs are immediately prescribed broad-spectrum antibiotics to circumvent the development of post-traumatic endophthalmitis.[1] Besides the direct mechanical damage ensued by the penetration of IOFBs into the eye, their chronic retention can lead to adverse sequel such as endophthalmitis, periretinal- and vitreous-hemorrhage, cataract formation, and retinal detachment.[5] Patients with IOFBs may also present with chronic uveitis[6] or bullous keratopathy.[7] Similar to our present case, a previous report described that an IOFB may also masquerade as herpetic stromal keratitis.[8]
When asymptomatic, IOFBs may be easily overlooked and retained for several years before the onset of these complications.[9] Furthermore, metallic IOFBs predispose patients to developing metallosis. Iron- or copper-containing IOFBs can lead to siderosis and chalcosis, respectively, which are vision-threatening diseases that warrant urgent IOFB removal. Contrarily, inert substances such as glass, plastic, gold, and silver are better tolerated and, if asymptomatic, may be managed conservatively with regular monitoring.[2]
This report emphasizes the importance of suspecting and ruling out IOFBs in patients presenting with unilateral corneal edema and anterior lens capsule opacification, particularly in patients engaged in high-risk activity.[7,8,10] In addition, fundamental principles when evaluating potential IOFBs were highlighted. Comprehensive ophthalmologic examination including gonioscopy and CT should be performed to avoid missed IOFBs, undetected by slit-lamp examination. Moreover, this report contributes to the pool of literature aiming to reinforce the need to raise awareness regarding occupational hazards and promote the proper use of personal protective equipment by those at the highest risk due to their occupation.
Footnotes
Informed Consent: Written informed consent was obtained from the patient for the publication of the case report and the accompanying images.
Peer-review: Externally peer-reviewed.
Authorship Contributions: Concept: H.H., E.Ç., S.A.; Design: H.H., E.Ç., S.A.; Supervision: H.H., E.Ç., S.A.; Materials: E.Ç., S.A.; Data: J.H.H., E.Ç., S.A.; Analysis: H.H., E.Ç., S.A.; Literature search: H.H., E.Ç., S.A.; Writing: H.H., E.Ç.; Critical revision: H.H., E.Ç., S.A.
Conflict of Interest: None declared.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Jung HC, Lee SY, Yoon CK, Park UC, Heo JW, Lee EK. Intraocular foreign body:Diagnostic protocols and treatment strategies in ocular trauma patients. J Clin Med. 2021;10:1861. doi: 10.3390/jcm10091861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Loporchio D, Mukkamala L, Gorukanti K, Zarbin M, Langer P, Bhagat N. Intraocular foreign bodies:A review. Surv Ophthalmol. 2016;61:582–96. doi: 10.1016/j.survophthal.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 3.He N, Lv Z. A rare asymptomatic metallic intraocular foreign body retained in the anterior chamber for 15?years:A case report. Medicine (Baltimore) 2021;100:e26470. doi: 10.1097/MD.0000000000026470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yeh S, Colyer MH, Weichel ED. Current trends in the management of intraocular foreign bodies. Curr Opin Ophthalmol. 2008;19:225–233. doi: 10.1097/ICU.0b013e3282fa75f1. [DOI] [PubMed] [Google Scholar]
- 5.Liu Y, Wang S, Li Y, Gong Q, Su G, Zhao J. Intraocular foreign bodies:Clinical characteristics and prognostic factors ınfluencing visual outcome and globe survival in 373 eyes. J Ophthalmol. 2019;2019:5208092. doi: 10.1155/2019/5208092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Albano J, Pires MC, Paccola M. Unnoticed metallic foreign body in the camerular angle inducing chronic uveitis. Arq Bras Oftalmol. 2021;84:267–70. doi: 10.5935/0004-2749.20210038. [DOI] [PubMed] [Google Scholar]
- 7.Dong PN, Duong NT, Cung LX, Huong DN, Ngan ND, Thien CD, et al. Bullous keratopathy secondary to anterior chamber angle foreign body. Open Access Maced J Med Sci. 2019;7:4311–5. doi: 10.3889/oamjms.2019.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Han ER, Wee WR, Lee JH, Hyon JY. A case of retained graphite anterior chamber foreign body masquerading as stromal keratitis. Korean J Ophthalmol. 2011;25:128–31. doi: 10.3341/kjo.2011.25.2.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ali NA, Buscombe CP, Jones DH. Intraocular foreign body in the anterior chamber angle of the eye-a 30-year-old “emergency”. Oxf Med Case Reports. 2021;2021:omab032. doi: 10.1093/omcr/omab032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Galvis V, Tello A, Frederick GA, Laiton AN. UUnilateral corneal edema caused by a hidden foreign body. Arch Soc Esp Oftalmol. 2017;92:436–8. doi: 10.1016/j.oftal.2016.06.004. [DOI] [PubMed] [Google Scholar]


