ABSTRACT
BACKGROUND:
Fingertip amputations are common injuries presenting to the emergency room. However, all amputations do not have a chance of replantation, and composite graft is among the salvage treatments in this case. This treatment is both easy to apply and economical. Our study compares the success and cost of composite grafting in the emergency and operating rooms.
METHODS:
Thirty-six patients who met the criteria were included in the study. The decision on the repair site was made by the surgeon according to patient compliance and the intensity of the emergency clinic. Demographic and disease information of the patients were recorded. P<0.05 was accepted as the significance level.
RESULTS:
Twenty-two cases were pediatric patients. Eighteen cases of crush injuries and 22 cases were treated in the emergency room. There was no significant difference in terms of complications, need for additional intervention, and short fingers related to interventions performed in the emergency room and operating room. Interventions in the emergency department were significantly lower in cost and shorter hospitalization times. There was no significant difference in terms of patient satisfaction.
CONCLUSION:
Composite grafting is a simple and reliable method in fingertip injuries and gives satisfactory results in terms of patient satisfaction. In addition, composite graft application in fingertip injuries in the emergency department will both reduce the cost and prevent hospital infections that may occur due to the reduction in hospitalization.
Keywords: Composite graft, cost-effectiveness, emergency room, fingertip injury, operating room
INTRODUCTION
Distal finger amputations are common injuries in children and adults. Best results can be obtained with microanastomoses, but functional and aesthetical repair may be impossible because of serious crush injuries, very thin vascular structures to replant, insufficient number of surgeons to operate, long hours of operation and long hospital stay, and high cost of repair. The amputated distal part can be used as a composite graft and local flap or left for secondary intervention in cases where microanastomoses are impossible.[1-4]
Composite grafts can contain tissues, such as bone, cartilage, and skin. One of the important points in composite grafting is that the graft is >1 cm close to the amputated part. The type of injury and the level of amputation are important parameters in graft success and also affect graft survival.[5-7] Therefore, the patient’s tissue is used in the injury area, and the loss of a limb in the finger is minimized with the composite graft method. However, the finger can be healed in a more esthetically pleasing way.[5,8]
Emergency departments are often the first point of contact for finger injuries. Amputations are one of the most common types of finger injuries and are often quickly and effectively treated with joint intervention by the emergency physician and hand surgeons. Early intervention of emergency physicians also contributes to composite graft success.
The composite graft method is simple and can be performed under local anesthesia and sometimes even in the emergency room. However, considering the crowd of emergency services, the clinician may choose to perform this repair under operating room conditions in some cases. Our study aimed to examine the recovery processes, complications, and treatment costs of patients who were admitted to the emergency department with finger amputation and were repaired with the composite graft method in the emergency room or operating room conditions.
MATERIALS AND METHODS
Study Design and Population
The study was retrospectively conducted from the prospectively collected data pool between January 1, 2021, and June 1, 2021. Ethics committee approval was obtained from a Tertiary Hospital Ethics Committee (Date: May 26, 2021, the decision number is; 89). The entire study was conducted following the Declaration of Helsinki. The study was conducted with 36 patients who met the study criteria from 43 patients who were admitted to the emergency department of our tertiary hospital due to distal finger amputation and were treated with a composite grafting method.
The study was planned to be performed at our tertiary hospital emergency department, plastic surgery, and hand surgery clinics. Patients who did not bring an amputated part to be used as a composite graft or whose amputated finger parts were evaluated as dirty and infected, or who could not be followed up after composite grafting were excluded from the study.
Data Collection
From the patient pool of 43 patients who underwent distal amputation and repair with composite graft, 2 with missing data and 5 who could not be followed up were excluded from the study. Thus, 36 patients were included in the study. Children were included in the study not to disturb the randomization and increase the number of cases.
All of the patients in the study were first evaluated by an emergency medicine specialist in the emergency department, then repaired with plastic surgery and/or hand surgery and followed up.
Hospitalization was recommended by the surgeon when choosing the emergency room or the operating room for composite grafting; Patients who agreed had the repair performed in the operating room, and those who did not accept were repaired in the emergency room.
Distal finger amputations are classified according to the Hirase classification as follows: DP-I: the most distal region, where arterial and venous structure repair is impossible; DP-II: the region extending between the base of the nail and the distal ends of the arterial structures, which is divided into two levels as DP-IIA with distal arterial injury and DP-IIB with proximal arterial injury; and DP-III: the region close to the nail base.[9] Our study classified the injury site according to this classification (Fig. 1).
Figure 1.
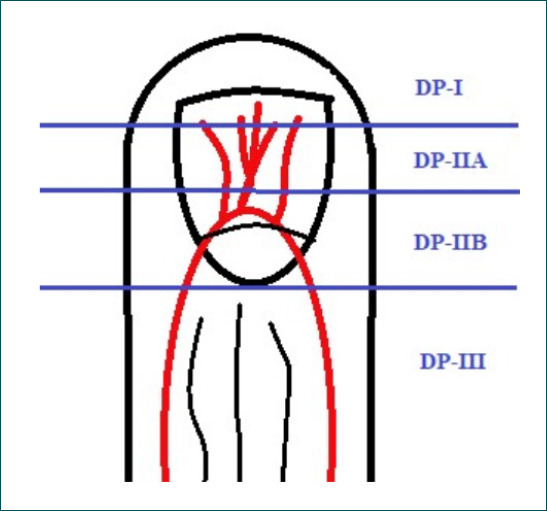
Hirase distal finger amputation classification
The study obtained the demographic characteristics of patients, injured finger information, length of inpatient stay, complications, and cost analyses from the pool of patients and hospital information systems.
Nerve blockade was performed by the anesthesiologist to provide surgical comfort and pain control for the patients who were admitted to hospitalization and repaired in the operating room. The level was chosen according to the region’s suitability for nerve blockage in these patients. In the emergency department, pain control, and comfort were provided by sedoanalgesia with ketamine (ketamine hydrochloride; 1mg/kg dose) for pediatric patients and midazolam (0.1 mg/kg) for adult patients.
Statistical Analyses
Analyzes were performed using the Statistical Package for the Social Sciences version 23.0 for Windows® statistical program (IBM Inc. Chicago, IL, USA). Number, percentage, mean, standard deviation, median, minimum, and maximum were used in the descriptive data presentation. The Kolmogorov–Smirnov test was used to evaluate the conformity of data with normal distribution. The Pearson Chi-square test and Fisher’s exact test were used to compare categorical data. The T-test was used to compare two independent numerical data, and the Kruskal–Wallis test for triple numerical data. Results were considered statistically significant at P<0.05, with a 95% confidence interval.
RESULTS
Our study included 36 patients who met the study criteria who were divided into zones according to the Hirase classification. The obtained examination results are presented (Table 1). The oldest age was 63 years and the youngest age was 1 in the patients included in our study.
Table 1.
Comparison of patient data by zones of injury
| Parameter | Zone I | Zone IIA | Zone IIB | Zone III | P-value |
|---|---|---|---|---|---|
| Case type, n (%) | |||||
| Adult | 3 (60.0) | 3 (23.1) | 5 (41.7) | 3 (50.0) | 0.448b |
| Child | 2 | (40.0) | 10 (76.9) | 7 (58.3) | 3 (50.0) |
| Injury type, n (%) | |||||
| Cut | 4 (80.0) | 6 (46.2) | 6 (50.0) | 2 (33.3) | 0.467b |
| Crush | 1 (20.0) | 7 (53.8) | 6 (50.0) | 4 (66.7) | |
| Injuried hand, n (%) | |||||
| Right | 2 (40.0) | 8 (61.5) | 9 (75.0) | 3 (50.0) | 0.527b |
| Left | 3 (60.0) | 5 (38.5) | 3 (25.0) | 3 (50.0) | |
| Injured finger, n (%) | |||||
| Thumb | 0 | 6 (46.2) | 3 (25.0) | 1 (16.7) | 0.063b |
| Forefinger | 2 (40.0) | 3 (23.1) | 1 (16.7) | 0 | |
| Middle finger | 2 (40.0) | 4 (30.8) | 4 (33.3) | 1 (16.7) | |
| Ring finger | 1 (16.7) | 0 | 3 (50.0) | 2 (33.3) | |
| Little finger | 0 | 0 | 1 (16.7) | 2 (33.3) | |
| Repair site, n (%) | |||||
| Emergency department | 4 (80.0) | 9 (69.2) | 6 (50.0) | 3 (50.0) | 0.563b |
| Operation room | 1 (20.0) | 4 (30.8) | 6 (50.0) | 3 (50.0) | |
| Complication, n (%) | |||||
| None | 4 (80.0) | 11 (84.6) | 9 (75.0) | 3 (50.0) | 0.439b |
| Necrosis | 1 (20.0) | 2 (22.2) | 3 (25.0) | 3 (50.0) | |
| Additional intervention, n (%) | |||||
| None | 4 (80.0) | 11 (84.6) | 9 (75.0) | 3 (50.0) | 0.540b |
| Spontan epitelisation | 0 | 1 (7.7) | 1 (8.3) | 2 (33.3) | |
| Debridement | 1 (20.0) | 1 (7.7) | 1 (8.3) | 0 | |
| Skin greft | 0 | 0 | 1 (8.3) | 1 (16.7) | |
| Deformity, n (%) | |||||
| None | 5 (100.0) | 13 (100.0) | 11 (91.7) | 3 (50.0) | 0.009b |
| Hook nail | 0 | 0 | 1 (8.3) | 3 (50.0) | |
| Hospitalization, n (%) | |||||
| No | 4 (80.0) | 8 (61.5) | 5 (41.7) | 3 (50.0) | 0.492b |
| Yes | 1 (20.0) | 5 (38.5) | 7 (58.3) | 3 (50.0) | |
| Age (years), median (IQR) | 17 (16–18) | 24 (18–41) | 23.5 (7.5–29.5) | 20.5 (3.0–40.0) | 0.461d |
| Shortening of finger (mm), median (IQR) | 3.0 (2.0–3.0) | 5.0 (4.0–6.0) | 5.0 (4.0–8.0) | 8.0 (6.0–10.0) | 0.013d |
| Cost ($)a, median (IQR) | 51.8 (47.2–53.4) | 55.5 (47.9–120.2) | 124.8 (51.2–180) | 166.7 (158.4–280.7) | 0.035d |
| Length of hospitalization (h), median (IQR) | 1.5 (1–1.5) | 2.5 (2.0–48.0) | 48.0 (2.0–60.0) | 25.5 (1.5–48.0) | 0.120d |
$ calculated based on the current exchange rate;
Pearson Chi-square test; cFisher’s exact test;
Kruskall–Wallis test. IQR: Interquartile range
The composite graft was preserved and cleaned in all cases. Four of the cases were admitted to the hospital after a cut, and one was seen as a result of a crush injury. Four cases were treated in the emergency department and one case was operated in the operating room. Necrosis was later observed in the patient who was performed in the operating room. This necrotic tissue was debrided at control examinations and allowed to heal secondarily. No complications were observed after the secondary intervention. Patients were completely satisfied in terms of comfort and esthetics. A median shortening of 3 mm (2–3 mm) was observed in the repaired fingers.
Of the cases, seven were admitted due to crush injury and six had a clean incision. Composite grafting was performed in all cases. Of the cases, nine were treated in the emergency department and four under the operating room conditions. Necrosis was observed in two of the patients who were called for control after the repair. When examined, 1 of the cases with necrosis was spontaneously epithelialized, while the other one was healed after debridement. A median shortening of 5 mm (4–6 mm) was observed in the repaired fingers. The recovery of patients was completed, which revealed good patient comfort and satisfaction.
Of the injuries, six were due to crushing, while the other six were due to cutting. Composite grafting was performed in all cases. Of the cases, six were treated in the emergency room and the other six under operating room conditions. Necrosis was observed in 3 of the patients who were called for control after the repair; of whom, one was spontaneously epithelialized and another one was healed after debridement. The third case was repaired again by placing a full-thickness skin graft. A median shortening of 6 mm (4–8 mm) was observed in these cases. The patients’ recovery was completed. Hook nail deformity was observed in one of the cases, and the comfort and satisfaction of these cases were good after recovery (Fig. 2).
Figure 2.
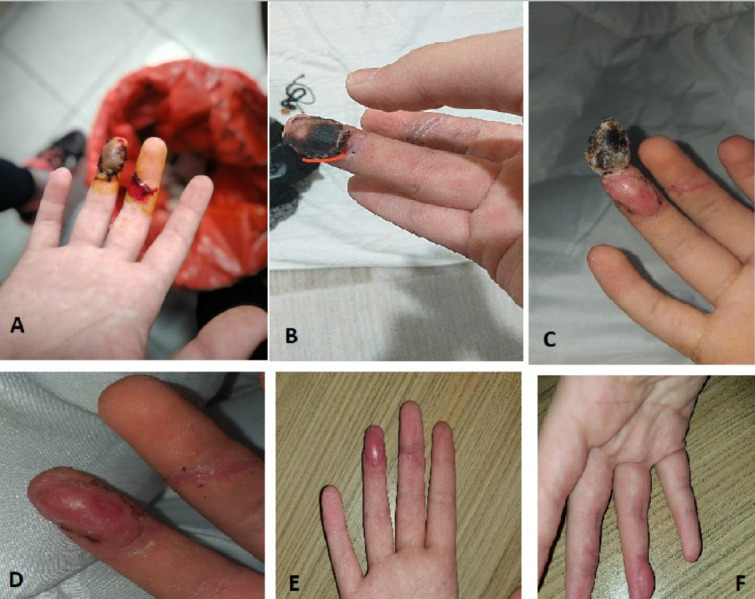
Healing steps in the repair and follow-up after zona III injury. (a) Composite graft repair after Zone III injury; (b) Day 7 image after repair; (c) Day 10 image after repair; (d) Day 14 image after repair; (e) Day 28 image after repair (anterior-posterior view); (f) Day 28 image after repair (lateral view)
Of the injuries, four were due to crushing while two were due to cutting. Composite grafting was performed in all cases. Of the cases, three were treated in the emergency room and the other three under operating room conditions. Necrosis was observed in three of the patients who were called for control after the repair; of whom, two had spontaneous epithelialization and the other one was repaired by placing a full-thickness skin graft. A median shortening of 8 mm (6–10 mm) was observed in these cases. The patients’ recovery was completed. Hook nail deformity was observed in 3 of the cases. The shortness of the fingers is macroscopically noticeable compared to the other hand; however, the comfort and satisfaction of the patients were good after recovery.
Comparative Results of the Groups
The obtained data after case evaluation according to the injury zones are presented in Table 2. The presence of hook nails was observed in Zones IIB and III injuries. Compared to other groups, the incidence of hook nail deformity statistically significantly increases as the level of injury increases (P=0.009).
Table 2.
The decision of the repair site of the injuries of the cases and the evaluation of the results
| Parameter | Emergence room | Operation room | P-value |
|---|---|---|---|
| Case type, n (%) | |||
| Adult | 7 (31.8) | 7 (50.0) | 0.277b |
| Child | 15 (68.2) | 7 (50.0) | |
| Injury type, n (%) | |||
| Cutting injury | 11 (50.0) | 7 (50.0) | 0.987b |
| Crush injury | 11 (50.0) | 7 (50.0) | |
| Injury direction, n (%) | |||
| Right hand | 13 (59.1) | 9 (64.3) | 0.755b |
| Left hand | 9 (40.9) | 5 (35.7) | |
| Injured finger row, n (%) | |||
| Thumb | 6 (27.3) | 4 (28.6) | 0.644c |
| Forefinger | 5 (22.7) | 1 (7.1) | |
| Middle finger | 5 (22.7) | 6 (42.9) | |
| 4th finger | 4 (18.2) | 2 (14.39 | |
| 5th finger | 2 (9.1) | 1 (7.1) | |
| Complication state, n (%) | |||
| None | 19 (86.4) | 8 (29.6) | 0.111b |
| Necrosis | 3 (13.6) | 6 (42.9) | |
| Additional interference, n (%) | |||
| None | 19 (86.4) | 8 (57.1) | 0.141c |
| Spontaneous epithelialization | 1 (4.5) | 3 (21.4) | |
| Debridement | 1 (4.5) | 2 (14.3) | |
| Skin graft | 1 (4.5) | 1 (7.1) | |
| Deformity, n (%) | |||
| None | 20 (90.9) | 12 (85.7) | 0.634c |
| Hook nail | 2 (9.1) | 2 (14.3) | |
| Age (years), median (IQR) | 24.5 (16.0–40.0) | 19.0 (6.0–26.0) | 0.150d |
| Finger shortness, median (IQR) | 5.0 (4.0–7.0) | 5.0 (3.0–7.0) | 0.689d |
| Cost ($)a, median (IQR) | 51.6 (47.3–57.3) | 156.7 (123.3–205.6) | <0.001d |
| Length of hospital stay (h), median (IQR) | 2.0 (1.5–2.5) | 48.0 (48.0–72.0) | <0.001d |
$ calculation converted according to the exchange rate of that day;
Pearson Chi-square test;
Fisher’s exact test;
Mann–Whitney U-Test; IQR: Interquartile range.
The shortness of the fingers significantly increased as the injury level of the cases increased (from Zone I to Zone III) (P=0.013), and it was the highest in the Zone III cases. In addition, the cost for the cases significantly increased according to the injury site classification (maximum in Zone III and minimum in Zone I). No significant difference was found between the zones in terms of length of emergency department and hospital stay (Table 2).
The relationship between the injury and the repair done in the emergency department or the operating room and its effect on complications, hospital stay, and cost are presented in Table 2. The age of patients did not affect the type of injury, the direction of injury, and the finger on which the injury occurred, as well as intervention in the emergency or operating room. In addition, no significant difference was found between the patients whose injuries were repaired in the emergency room and those in the operating room in terms of complications, need for additional intervention, deformity, and short finger. However, a statistically significant difference was found in terms of hospital stay duration and cost in patients who underwent repair in the emergency department (P<0.001 for both parameters).
In the comparison of pediatric patients and adult patients, no significant difference was found in terms of complications, additional intervention, and deformity. Crush injuries in children were significantly higher than in adult patients (71.4% in pediatric vs. 36.4% in adults; P=0.040). In addition, finger shortness was significantly lower in pediatric patients compared to adult patients (mean: 3 mm in children [interquartile range (IQR): 2–5 mm] vs. 6.5 mm in adults [IQR: 5–8]; P<0.001).
DISCUSSION
Fingertip amputations cause serious aesthetic and functional problems, which are difficult to manage. In addition, management becomes more difficult in injuries distal to the distal interphalangeal joint.
Treatment methods depend on the type of injury (smooth cut, crush injuries, etc.), time of admission after injury (necrosis of the amputate, etc.), condition of the amputate (contaminated, multi-part, etc.), the experience of the micro surgeon, and functional need of the patient (manual worker, office worker, artist, etc.). Therefore, fingertip amputation management goes from simple to complex. Since the beginning of microsurgery’s first activities in 1960, many developments (instruments, techniques, knowledge of surgical anatomy, vascular physiological developments, etc.) related to microsurgery have been experienced.[10] In addition, alternative methods have emerged for patients who cannot be replanted with microsurgery. A composite graft is one of these alternative methods. When choosing alternative methods, differences should be considered not only in terms of skill and technique but also in terms of surgical time, hospital stay, and cost. As a general rule, treatment goals should include maximum function restoration with minimal pain, rapid recovery, and short rehabilitation time.[11] Functional evaluation is frequently performed in the literature;[5,7,12] thus, our study aimed to provide information on both cost and length of hospital stay, together with functional evaluation of composite graft cases repaired in the emergency room and operating room.
The most basic method of repair in fingertip amputations is to leave it to the secondary intervention. However, this approach is not possible in cases where the bone tissue is exposed, or the injury defect is >1 cm2. Studies reported on cold intolerance, soft-tissue loss, and hypersensitivity if preferred in these cases.[13] Amputation revision and primary closure can be tried in these cases, but they are not the methods used in the first stage because they can cause short fingers. In addition, the literature revealed that the composite grafting method is popular because it is both simple and fast, and more economical. Moreover, composite grafting has yielded good results in pediatric cases, but not so much in adult cases.[14]
Replantation is often a method to be considered in the case of a clean and identifiable vessel and a sharp amputation on both sides. Unfortunately, most distal finger amputations come with crush injuries in the form of crushing and squeezing. This situation generally prevents the repair of the case by the replantation method. Skin graft or V-Y flap methods disrupt the formation or shape of the nail. Due to the difficulties of these methods, the composite graft method still maintains its applicability.
A study by Hattori et al. on the process of repairing distal finger amputations in the operating room revealed a very difficult replantation, long follow-up, and a cost of $14.379 on average.[13] Therefore, we think that composite grafting in cases where replantation cannot be performed, will be economical, easier to follow, and more aesthetically pleasing. Our study examined the effects of composite grafting repairs in the emergency room and the operating room after hospitalization on hospital stay and cost. Comparing the repair of composite grafting cases in the emergency room with inpatient surgery, a statistically significantly more economical (emergency repair average of $51.6 vs. operating room repair average of $156.7) and a significantly shorter length of stay in the hospital was found (emergency repair on average of 2 h vs. an average of 48 h in the operating room). In addition, no difference was found in terms of finger shortness, complications, additional intervention, and deformity in cases repaired in the emergency room compared with those repaired in the operating room. The average age of patients was considered, and some literature reports stated that composite grafting is successful in children with distal fingertip amputations, and this method should be limited to children only. However, this study revealed that age was not a risk factor.[14] Our study revealed no difference between the pediatric cases and the adult cases in terms of complications, additional interventions, deformities, and hospital stay. In addition, finger shortness was found to be significantly lower in pediatric patients.[15] However, in addition to the significantly lower finger length, children’s fingers are shorter than adult patients’ fingers; although the shortness of the fingers is significantly lower, it is obvious that pediatric patients will show variability in loss of function compared to adult patients.
The study by Moiemen and Elliot reported that the success of the repair is 61% if the time from injury to the repair in the operating room is <5 h, and all of the composite grafts fail in cases where the repair takes >5 h.[14] Our study revealed no significant difference between the time between the hospital admission and the repair completion and the complication status. However, the average hospital stays after admission in cases repaired in the emergency room is 2 h and 48 h in cases repaired in the operating room, which is statistically significantly shorter in the emergency room. This situation shows that the hospital stay duration is short in cases repaired in the emergency department, but no significant difference in terms of complication status. Therefore, it would be advantageous for the patient to have the repair done in the emergency room in these cases.
Our study has several limitations. First, this is a retrospective study and was conducted with data obtained through retrospective scanning. Second, a two-point discrimination test could not be performed after the injured distal fingertip repair of the patients in the study due to its retrospective nature, thus, these results could not be presented in our study.
Conclusion
Our study revealed that the composite grafting method in distal fingertip amputations is a simple, easy-to-follow, and economical alternative method in cases where replantation cannot be performed. Additionally, the use of the composite grafting method in the emergency department both reduced the cost and shortened the hospital stay. Moreover, no significant difference was found between the repair in the emergency room and the operating room in terms of complications, additional intervention, and shortening of the finger. Therefore, we recommend that patients with distal fingertip amputation should be repaired with composite grafting in the emergency department.
Footnotes
Ethics Committee Approval: This study was approved by the Başaksehir Çam and Sakura City Hospital Clinical Research Ethics Committee (Date: 10.06.2021, Decision No: 2021.05.89)
Peer-review: Externally peer-reviewed.
Authorship Contributions: Concept: K.S., R.G., A.Ç., A.A., M.İ.; Design: K.S.; Supervision: K.S., R.G., A.Ç.; Materials: K.S., M.İ., A.A.; Data: K.S., M.İ., A.A., A.Ç.; Analysis: R.G., K.S., A.Ç., N.D.H.; Literature search: K.S., A.Ç., A.A.; Writing: K.S., A.Ç., N.D.H.; Critical revision: A.A., R.G., K.S.
Conflict of Interest: None declared.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Johnson D, Giele H. Restoration of the nail apparatus following fingertip amputation by perionychial grafts supported by local flaps, in children and adults. J Plast Reconstr Aesthet Surg. 2011;64:776–81. doi: 10.1016/j.bjps.2010.08.032. [DOI] [PubMed] [Google Scholar]
- 2.Hwang E, Park BH, Song SY, Jung HS, Kim CH. Fingertip reconstruction with simultaneous flaps and nail bed grafts following amputation. J Hand Surg Am. 2013;38:1307–14. doi: 10.1016/j.jhsa.2013.03.032. [DOI] [PubMed] [Google Scholar]
- 3.Lee SM, Rahman MF, Thirkannad S. Combination V-Yadvancement flap and composite graft for reconstruction of an amputated fingertip. Hand Surg. 2012;17:145–9. doi: 10.1142/S0218810412970015. [DOI] [PubMed] [Google Scholar]
- 4.Kim KS, Eo SR, Kim DY, Lee SY, Cho BH. A new strategy of fingertip reattachment:sequential use of microsurgical technique and pocketing of composite graft. Plast Reconstr Surg. 2001;107:73–9. doi: 10.1097/00006534-200101000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Eo S, Hur G, Cho S, Azari KK. Successful composite graft for fingertip amputations using ice-cooling and lipo-prostaglandin E1. J Plast Reconstr Aesthet Surg. 2009;62:764–70. doi: 10.1016/j.bjps.2007.09.064. [DOI] [PubMed] [Google Scholar]
- 6.Lee KS, Lim YS, Choi J, Kim NG, Kim JS. Composite graft including bone tissue:A case report of successful reattachment of multiple fingertip oblique amputation. J Plast Reconstr Aesthet Surg. 2013;66:e43–6. doi: 10.1016/j.bjps.2012.10.017. [DOI] [PubMed] [Google Scholar]
- 7.Dagregorio G, Saint-Cast Y. Composite graft replacement of digital tips in adults. Orthopedics. 2006;29:22–4. doi: 10.3928/01477447-20060101-03. [DOI] [PubMed] [Google Scholar]
- 8.Alper N, Sood A, Granick MS. Composite graft repair for distal fingertip amputation. Eplasty. 2013;13:ic32. [PMC free article] [PubMed] [Google Scholar]
- 9.Adani R, Marcoccio I, Tarallo L. Treatment of fingertips amputation using the Hirase technique. Hand Surg. 2003;8:257–64. doi: 10.1142/s0218810403001777. [DOI] [PubMed] [Google Scholar]
- 10.Scheker LR, Becker GW. Distal finger replantation. J Hand Surg Am. 2011;36:521–8. doi: 10.1016/j.jhsa.2010.12.017. [DOI] [PubMed] [Google Scholar]
- 11.Martin C, del Pino JG. Controversies in the treatment of fingertip amputations, Conservative versus surgical reconstruction. Clin Orthop Relat Res. 1998;353:63–73. doi: 10.1097/00003086-199808000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Uysal A, Kankaya Y, Ulusoy MG, Sungur N, Karalezli N, Kayran O, et al. An alternative technique for microsurgically unreplantable fingertip amputations. Ann Plast Surg. 2006;57:545–51. doi: 10.1097/01.sap.0000226944.08332.41. [DOI] [PubMed] [Google Scholar]
- 13.Hattori Y, Doi K, Ikeda K, Estrella EP. A retrospective study of functional outcomes after successful replantation versus amputation closure for single fingertip amputations. J Hand Surg. 2006;31A::811–8. doi: 10.1016/j.jhsa.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 14.Moiemen NS, Elliot D. Composite graft replacement of digital tips. 2. A study in children. J Hand Surg Br. 1997;22:346–52. doi: 10.1016/s0266-7681(97)80400-7. [DOI] [PubMed] [Google Scholar]
- 15.Borrelli MR, Landin ML, Agha R, Greig A. Composite grafts for fingertip amputations:A systematic review protocol. Int J Surg Protoc. 2019;16:1–4. doi: 10.1016/j.isjp.2019.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


