The croissant repair for congenital tricuspid valve dysplasia.
Central Message.
Repair of a severely dysplastic tricuspid valve can be successfully performed by 2-leaflet, 1-patch augmentation using a crescent-shaped patch traversing the anteroseptal commissure.
Repair of non-Ebsteinoid tricuspid valve dysplasia (TVD) is often challenging due to severe leaflet restriction and lack of usable leaflet tissue.1 Few studies have investigated optimal surgical management strategies for this lesion.1, 2, 3 Many surgical techniques have been borrowed from mitral valve repair, such as division of restrictive chordae, papillary muscle splitting, and pericardial patch splinting.4,5 Herein, we describe a repair technique that addresses severe leaflet and commissure restriction with a 2-leaflet, 1-patch augmentation through the anteroseptal commissure itself and resection of restrictive secondary and primary chordae without the use of artificial chordae. Written informed consent was obtained for publication of this report. Approval was obtained from the Columbia University Medical Center Internal Review Board under protocol No. AAAR3476 (approved August 12, 2022).
Case Summary
The patient is a 4-year-old boy (weight, 18 kg) with a prenatal diagnosis of pulmonary atresia with intact ventricular septum and TVD who underwent a transannular patch with right ventricular overhaul during the neonatal period. During an admission for COVID-19 pneumonia, the patient was found to have severe right ventricle dysfunction, free pulmonary regurgitation, and severe tricuspid regurgitation secondary to TVD. He was taken to the operating room for pulmonary valve replacement and a croissant repair of the TV.
Surgical Technique
A midline sternotomy was performed and cardiopulmonary bypass was established. Pulmonary valve replacement was performed using a 21-mm Inspiris bioprosthesis (Edwards Lifesciences). The TV was inspected and repair was deemed feasible (Video 1).
The septal and anterior leaflets were detached from the annulus, traversing across the anteroseptal commissure (Figure 1, D and E). Restrictive secondary chordae to both leaflets were divided. Restrictive secondary chordae to the posterior leaflet were also divided without taking down this leaflet. The anteroposterior papillary muscle was split to provide extra leaflet mobility (Figure 1, F).
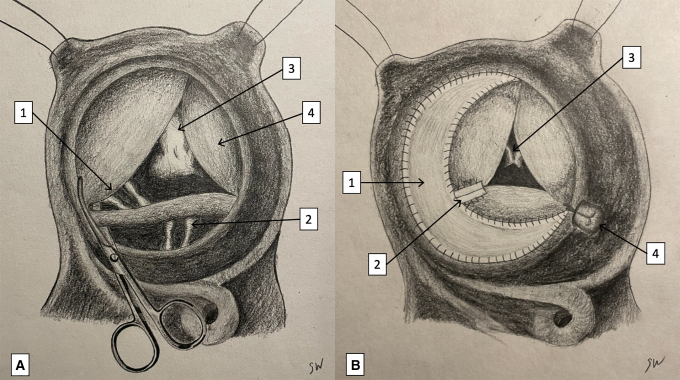
Figure 1.
Steps in the croissant repair of a severely dysplastic tricuspid valve. The patient's head is toward the left of figure. Mechanism of tricuspid regurgitation in this patient is due to foreshortened leaflets (A), restrictive primary and secondary chordae (B), and papillary muscle insertion at the anteroposterior commissure (C). D and E, Detachment of the septal and anterior leaflet and anteroseptal commissure from the annulus and resection of secondary chordae. F, Splitting the papillary muscle with Metzenbaum scissors. G, Patch being sutured to the annulus of the anterior leaflet. H, Completion of the 2-leaflet patch augmentation traversing the anteroseptal commissure. Crescent-shaped patch indicated with dashed line. I and J, Splint support of the augmented leaflets using two strips of bovine pericardium. K, Suture plication at the posteroseptal aspect of the annulus. L, Excellent saline test at the conclusion of the repair. Crescent-shaped patch indicated with dashed line.
A croissant-shaped bovine pericardial patch was sutured to the annulus of the anterior and septal leaflets in a counterclockwise direction through the anteroseptal commissure (Figure 1, G). The free edge of the patch was trimmed in the shape of a croissant and sutured to the cut edge of both leaflets (Figure 1, H).
Highly restrictive primary chordae at the anteroseptal commissure were divided. The septal and anterior leaflets in this region were splinted using thin strips of bovine pericardium (Figure 1, I and J). The annulus was then plicated at the posteroseptal aspect (Figure 1, K).
A Hegar dilator (normal diameter for body surface area) was passed through the TV orifice without difficulty and saline testing revealed excellent leaflet mobility with trivial incompetence (Figure 1, L). The patient was weaned off bypass without difficulty in normal sinus rhythm. Postoperative transesophageal echocardiography demonstrated trace regurgitation without stenosis. The patient had an uneventful recovery. Interval echocardiograms have shown stable trivial tricuspid regurgitation and mild tricuspid stenosis (mean gradient, 2-3 mm Hg) at 12 months’ follow-up.
Discussion
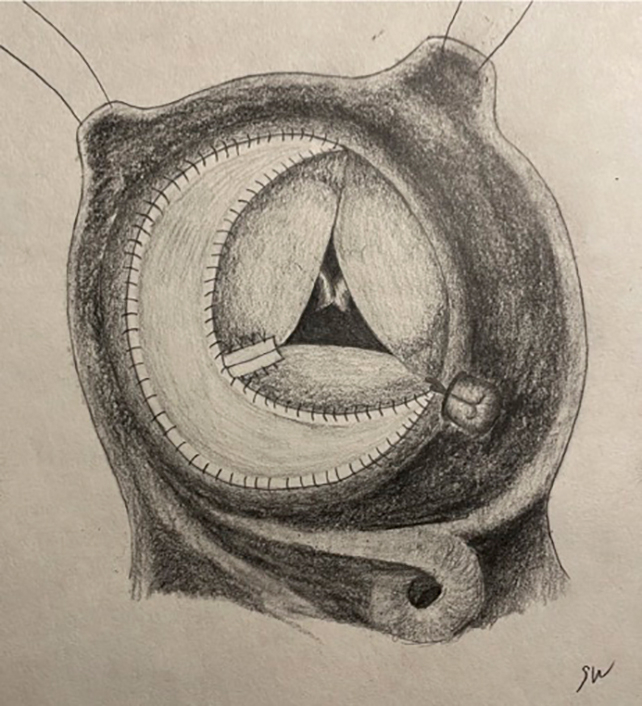
The croissant technique for repair of congenital TVD combines 1 crescent-shaped patch for 2-leaflet augmentation crossing the anteroseptal commissure, along with resection of restrictive secondary and primary chordae and splint plasty for support of the augmented leaflets (Figure 2). This technique is innovative in that it untethers not only the leaflets but the anteroseptal commissure itself.
Figure 2.
A graphic depiction of the mechanism of tricuspid regurgitation in this case and the elements of the croissant technique. The patient's head is toward the left of figure. A, The mechanism of tricuspid regurgitation in this case of severe tricuspid valve dysplasia. 1, Scissors shown taking down the anteroseptal commissure. 2, Restrictive primary chordae to the anterior and septal leaflets. 3, Restrictive secondary chordae to the septal leaflet shown behind leaflet detached from the annulus (present in all 3 leaflets). 4, Papillary muscle insertion at the anteroposterior commissure. Foreshortened leaflets (present in all 3 leaflets). B, The elements of the croissant technique for repair of tricuspid valve dysplasia. 1, Crescent-shaped patch augmentation of the anterior and septal leaflets through the anteroseptal commissure. 2, Splint with 2 thin strips of bovine pericardium on the free edge of the leaflet at the septal aspect of the anterior leaflet and anterior aspect of the septal leaflet. 3, Split papillary muscle at the anteroposterior commissure. 4, Suture annuloplasty at the posteroseptal aspect of the annulus.
Restriction of the mobility of the leaflets at the commissure is not well addressed with surgical techniques currently used to repair dysplastic TVs, even after extensive resection of the secondary chordae. Cutting primary chordae is often necessary to provide full mobility. Artificial chordae can be challenging in small children, do not have growth potential, and do not provide with a durable repair for this specific anatomy. Detaching the commissure itself from the annulus and patch-enlarging the commissure region, along with cutting primary chordae, gives full mobility to the leaflets. Buttressing the superior aspect of the septal leaflet and the inferior aspect of the anterior commissure with 2 thin strips of bovine pericardium sutured to the neoleaflet provides splint support to this tissue and enables resection of the primary chordae without inducing leaflet prolapse. The TV is thus bicuspidized, keeping the anteroposterior and posteroseptal commissures functional. This technique requires posterior leaflet mobility to be able to coapt with the neoanteroseptal leaflet, which in this case was provided by division of restrictive secondary chordae and splitting the anteroposterior papillary muscle. A similar technique could be applied to the posteroseptal commissure if this is the commissure with the greatest amount of restriction. The outcome of this repair is to untether and lengthen not only the restricted anterior and septal leaflets but also the anteroseptal commissure itself, producing a bicuspidized valve with excellent coaptation.
Acknowledgments
The authors thank Sydney Williams for providing the illustrations.
Footnotes
Disclosures: The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Read at the 103rd Annual Meeting of The American Association for Thoracic Surgery, Los Angeles, California, May 6-9, 2023.
IRB No. AAAR3476 (approved August 12, 2022).
Informed written consent was obtained for the publication of this report.
Supplementary Data
The croissant repair for congenital tricuspid valve dysplasia. Video available at: https://www.jtcvs.org/article/S2666-2507(23)00133-5/fulltext.
References
- 1.Cleuziou J., Pringsheim M., Stroh A., Burri M., Lange R., Hörer J. Surgical treatment of tricuspid valve dysplasia in children. Eur J Cardio Thorac Surg. 2022;62:212. doi: 10.1093/ejcts/ezac212. [DOI] [PubMed] [Google Scholar]
- 2.Reddy V.M., McElhinney D.B., Brook M.M., Silverman N.H., Stanger P., Hanley F.L. Repair of congenital tricuspid valve abnormalities with artificial chordae tendineae. Ann Thorac Surg. 1998;66:172–176. doi: 10.1016/s0003-4975(98)00351-8. [DOI] [PubMed] [Google Scholar]
- 3.Mizuno M., Hoashi T., Sakaguchi H., Kagisaki K., Kitano M., Kurosaki K., et al. Application of cone reconstruction for neonatal Ebstein anomaly or tricuspid valve dysplasia. Ann Thorac Surg. 2016;101:1811–1817. doi: 10.1016/j.athoracsur.2015.11.029. [DOI] [PubMed] [Google Scholar]
- 4.Bakir I., Onan B., Onan I.S., Gul M., Uslu N. Is rheumatic mitral valve repair still a feasible alternative?: indications, technique, and results. Tex Heart Inst J. 2013;40:163–169. [PMC free article] [PubMed] [Google Scholar]
- 5.Gritti M., Ferris A., Shah A., Bacha E., Kalfa D. “Splint” mitral valve repair for destructive endocarditis in children. World J Pediatr Congenit Heart Surg. 2019;10:121–124. doi: 10.1177/2150135117751914. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The croissant repair for congenital tricuspid valve dysplasia. Video available at: https://www.jtcvs.org/article/S2666-2507(23)00133-5/fulltext.