Abstract
Background
Tuberculosis (TB) is an ancient infection and a major public health problem in many low- and middle-income countries (LMICs). Active case finding (ACF) programs have been established to effectively reduce TB in endemic global communities. However, there is little information about the evidence-based benefits of active case finding at both the individual and community levels. Accurately identifying the facilitators and barriers to TB-ACF provides information that can be used in planning and design as the world aims to end the global TB epidemic by 2035. Therefore, this study aimed to identify the facilitators and barriers to tuberculosis ACF in LMICs.
Methods
A systematic search was performed using recognized databases such as PubMed, Google Scholar, SCOPUS, HINARI, and other reference databases. Relevant studies that assessed or reported the ACF of TB conducted in LMICs were included in this study. The Joanna Briggs Institute’s (JBI) Critical Appraisal Tool was used to assess the quality of the selected studies. The Statement of Enhancing Transparency in Reporting the Synthesis of Qualitative Research (ENTREQ) was used to strengthen the protocol for this systematic review. The Confidence of Evidence Review Quality (CERQual) approach was also used to assess the reliability of the review findings.
Results
From 228 search results, a total of 23 studies were included in the final review. Tuberculosis ACF results were generated under two main themes: barriers and facilitators in LMICs, and two sub-themes of the barriers (healthcare-related and non-healthcare-related barriers). Finally, barriers to active TB case finding were found to be related to (1) the healthcare workers’ experience, knowledge, and skills in detecting TB-ACF, (2) distance and time; (3) availability and workload of ACF healthcare workers; (4) barriers related to a lack of resources such as diagnostic equipment, reagents, and consumables at TB-ACF; (5) the stigma associated with TB-ACF detection; (6) the lack of training of existing and new healthcare professionals to detect TB-ACF; (7) communication strategies and language limitations associated with TB ACF; and (8) poor or no community awareness of tuberculosis. Stigma was the most patient-related obstacle to detecting active TB cases in LMICs.
Conclusion
This review found that surveillance, monitoring, health worker training, integration into health systems, and long-term funding of health facilities were key to the sustainability of ACF in LMICs. Understanding the elimination of the identified barriers is critical to ensuring a maximum tuberculosis control strategy through ACF.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12879-023-08502-7.
Keywords: LMICs, Tuberculosis, Facilitators and barriers, Active case finding, Systematic review
Introduction
Background
Tuberculosis (TB) is a widespread and chronic infectious disease that is globally spread and is caused by the pathogen Mycobacterium tuberculosis [1]. In accordance with estimations, approximately 40 million individuals are afflicted with TB in the year 2022, with 3.5 million of those being children [2]. Low-and middle-income countries (LMICs) bear a disproportionate burden of high morbidity and mortality associated with TB [3]. The Southeast Asia and Western Pacific regions accounted for the highest number of TB cases, followed by the African region. In these regions, the morbidity rates can reach as high as 95%, with mortality rates up to 98% [4]. Tuberculosis case-finding mechanism is mostly passive in low- and middle-income countries due to the presence of potential obstacles. This system relies on individuals reporting for diagnosis rather than active outreach programs [5, 6].
Active case detection is a novel methodology for tuberculosis screening that exhibits significant potential to augment the timely identification of cases in underserved communities [7]. This approach is largely directed towards demographic groups that are considered high-risk, comprising individuals who are homeless, incarcerated, receiving care in nursing homes, and residing in economically disadvantaged regions [8]. Unlike passive case-finding, ACF involves actively searching for TB in individuals who would not seek care spontaneously. The strategy aimed to eradicate tuberculosis, as acknowledged by the World Health Organization, recognizes ACF as a vital methodology for the identification of tuberculosis cases that are currently being disregarded by healthcare facilities [9].
In nations like the United States, Northern America, Canada, and the European Union, where the occurrence of tuberculosis is low, there are policies in place that aim to proactively identify incidences of the disease. Conversely, a majority of lower and middle-income countries with substantial TB burdens depend on passive case detection. This reliance on passive case detection has contributed to the current failure to prevent transmission at the necessary level [10, 11]. Despite the potential that ACF holds for amplifying the early detection of cases among marginalized populations, there exist substantial barriers to the adoption of ACF strategies in low and middle-income countries. These barriers may include inadequate capacity-building for healthcare workers, limited accessibility to healthcare facilities, and insufficient community involvement [12]. Moreover, while some studies have investigated ACF interventions, there is a lack of summarized results about the barriers and facilitators of ACF.
This systematic review is necessary to provide evidence-based recommendations for ACF interventions that can increase the detection of TB cases in low and middle-income countries. The findings of this study will have significant implications for policymakers, healthcare professionals, and researchers, enabling them to plan and design effective TB ACF interventions that improve TB control in these countries. In addition, this investigation will contribute to the global efforts aimed at achieving the WHO End TB strategy and the sustainable development goals.
The present review highlights the significance of addressing the challenge of active case finding for tuberculosis (TB-ACF) in low- and middle-income countries (LMICs) through thorough investigation and evidence-based proposals as evidenced by the existing literature.
While it is acknowledged that TB remains a major public health challenge worldwide, with LMICs bearing a disproportionate burden of high morbidity and mortality, the current passive case-finding mechanism in these countries is insufficient to effectively identify and treat cases [10, 12].
The purpose of this study is to investigate the barriers and facilitators of TB-ACF in LMICs, providing insights and recommendations for future ACF policy development. By conducting a systematic review of existing studies, this research aims to fill the gap in summarized results and generate evidence-based findings that can guide policymakers, healthcare professionals, and researchers in planning and designing effective ACF interventions. The implications of this study are significant, as it has the potential to improve TB control in LMICs by enhancing case detection rates. The findings will inform the development of targeted interventions and strategies that overcome the identified barriers and leverage the facilitators of TB-ACF. Policymakers can use these recommendations to implement evidence-based policies that support proactive case identification, ultimately reducing transmission rates and improving patient outcomes.
Furthermore, this investigation aligns with global efforts to achieve the World Health Organization’s End TB strategy and the sustainable development goals. By focusing on TB-ACF in LMICs, where the burden of the disease is particularly high, this research contributes to the broader objective of eliminating TB as a global public health threat.
In summary, this systematic review is essential to justify the need for investigating TB-ACF in LMICs. By identifying barriers, facilitators, and providing evidence-based recommendations, this study aims to improve ACF policy development, enhance case detection rates, and contribute to global efforts in combating TB.
Objective
To identify the facilitators and barriers of tuberculosis to ACF in low- and middle-income countries (LMICS).
Review questions
What are the facilitating factors for TB -ACF in low and middle-income countries?
What are the barriers to active TB case detection in low- and middle-income countries?
What are the healthcare system and non-healthcare system -related barriers to TB-ACF in LMICS?
Methodology
Synthesis methods
Enhancing transparency in reporting the synthesis of qualitative research (ENTREQ) statement was used for strengthening the protocol for the systematic review [13] (Additional file 2).The items have been meticulously collated and systematically classified into five distinct categories, namely: introduction, methods and methodology, literature search and selection, appraisal, and synthesis of findings.
Inclusion criteria
The current systematic review included studies with any qualitative study design, which can be conducted using either qualitative studies or mixed methods. Criterion (1): research question the paper is based on a clearly defined research question, which is clearly discussed and referenced throughout the paper. Criteria 2: Internal validity: the design of the study is suitable for the posed research inquiry and has unambiguously enunciated the study objectives. Selection bias has been minimized; confounding factors have been identified and/or controlled; explanatory variables are based on sound scientific principles; and outcome measures are complete and reliable. Criteria 3: Clarity of Results: Well-described and appropriate analytical methods were used. The precision of association is given or calculable and is meaningful. Criteria 4: External validity: The source population is well described, and the eligible population represents the source population. Selected participants represent an eligible population, and the results are consistent with results from other studies. The study results are generalizable to the source population. Any study that used qualitative methods of data collection (individual interviews, focus group discussions, and observation) and data analysis (thematic analysis) was included. The articles examining barriers and/or facilitators have been included. Healthcare providers involved in active case finding, community health workers (HCWs) and volunteer health managers, peer volunteers, policymakers, suspected TB patients, activists, academics, and other stakeholders encountered in the studies on ACF were included in the review. All studies conducted in WHO Member States grouped into low- and middle-income countries were included. Articles on barriers and promoters examining factors related to active TB case finding at the health system, individual, and community levels in low- and middle-income countries were included.
Exclusion criteria
Study types like clinical trials, case-control, and cohort study types were excluded, and studies with comments from quantitative surveys, editorials, and opinion pieces were also excluded. Studies conducted within groups in high-income countries were also excluded. Studies not reported in English were excluded.
Search strategy and data sources
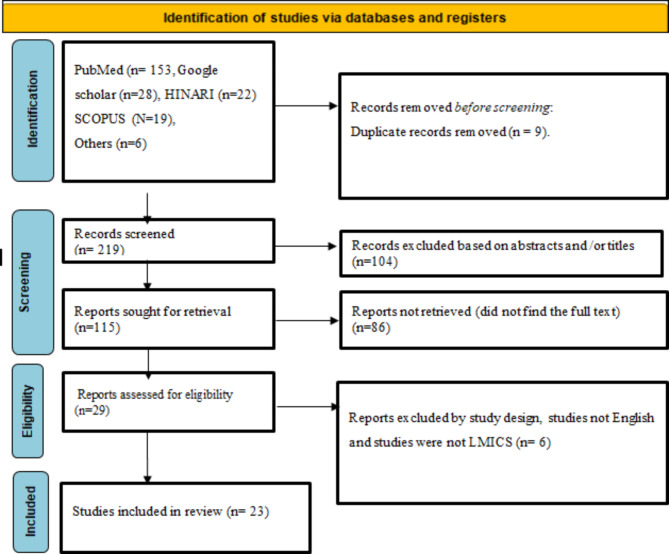
Electronic databases, including PubMed, Google Scholar, Scopus, HINARI, and other sources, were searched using Endnote Manager for sorting and filtering the articles for review. In addition, Microsoft Excel was used to facilitate the screening of the imported articles. The search strategy incorporated the key terms of the review question and utilized Boolean search operators. The key terms were: facilitators, enablers, barriers, challenges, “active case finding” “systematic screening” “community-based case finding” OR “community-based case detection” “tuberculosis,“ and “low and middle-income countries”. The search results were presented in the form of a flow diagram, as recommended by the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) (Fig. 1). A total of 228 articles were browsed through these electronic databases and other methods. A total of 9 articles were removed for duplicates, being marked as ineligible, or for other reasons. A total of 104 articles were excluded through title and abstract screening. One hundred fifteen (115) article reports were sought for retrieval, and 29 were evaluated for eligibility. Finally, only 23 full-text articles were deemed suitable for qualitative and quantitative synthesis.
Fig. 1.
PRISMA flow diagram to investigate the facilitators and barriers of TB ACF in LMICs.
Quality assessment
The included relevant studies were critically assessed by two independent authors (AA and MD). The JBI Critical Appraisal Tool was used to assess the quality of the qualitative studies included in this review [14] (see additional file 1). In addition, we graded the final synthesized qualitative findings according to the CERQual approach to rate the level of confidence and certainty of the findings [15].
Data extraction and analysis
In brief, the entirety of the retrieved publications in various databases underwent initial screening. The abstracts of the aforementioned publications were scrutinized by two independent reviewers (MD and OA) acting individually. Instances, where judgments conflicted, were subsequently resolved by the authors who made the initial screening decisions. The screening of full texts was executed in a comparably to that of abstracts. Then they were shared online with another reviewer (AA). The reviewers used a customized JBI data abstraction format. As members are located in different countries, online Zoom meetings were scheduled once a week for this process. For urgent purposes, phone calls, emails, and internet account group SMS were used as means of contact. These communications should discuss solutions to unclear points regarding the eligibility criteria and other confusing issues. For example, there was a disagreement between two reviewers (AA and MD) regarding the classification of barriers and promoters in low- and middle-income countries. This was resolved during one of our online engagements that all group members attended. We developed a standardized form to identify included studies and settings (publication year, published journals, study design, interventions, and country) and participant characteristics (type of participants, e.g., health workers, number of participants, etc.) and the primary outcome measures (key barriers and facilitators) in LMICs.
After conducting data extraction for each paper, the studies were categorically grouped according to the outcomes of interest. Subsequently, narrative summaries for each outcome were presented and analyzed. The data was then analyzed and summarized using both pictorial and tabular representations. Firstly, the findings were classified into two categories, namely, barriers related to low- and middle-income countries. Secondly, the theme was summarized into the main findings. Subsequently, the quality assessment tool was applied. Concurrently, the findings, especially the barriers, were categorized into theme 1 as healthcare system-related and non-healthcare system-related barriers. Finally, patient-related, health-related, resource-related, and implementation-related factors were considered. Ultimately, the quality assessment tool CERQual was applied to the findings. Six out of the total eight preliminary findings have been chosen as the “key findings” to undergo further analysis through the Confidence in the Evidence from Reviews of Qualitative Research (CERQual) tool. The selection process was based on a consensus between three authors (AG, AA), where the strength of evidence, number of supporting reviews, level of variability in review findings, and significance of the findings as indicated in the included reviews were taken into consideration.
Results
Review description
A total of 23 studies from 2013 to 2020 were included in the final review. These studies were organized according to the title of the article, study location or country, methods, sample characteristics, and author(s) with the year of publication (see Table 1). The results were presented based on the major themes of barriers and facilitators that emerged from the analysis and synthesis. The barriers are further presented as healthcare system and non-healthcare system related barriers. Of the included studies, it was noted that two of the articles in question did not explicitly mention the ethical considerations that were taken into account when formulating their research protocols.
Table 1.
Summary of study characteristics (n = 23)
| Title of the article | Study Location | Methods | Ethical Approval | Participants | Settings | Data collection | Author |
|---|---|---|---|---|---|---|---|
| Identifying barriers to and facilitators of TB contact investigation in Kampala | Uganda | Qualitative | Not specified | HCW from seven health centers | Clinic-based health staff, clinic-affiliated LHWs, and adult household contacts of index patients | Group discussions and interviews | [16] |
| Experts’ insights into the development and implementation of active tuberculosis case-finding policies globally | Nepal | Exploratory qualitative | Yes |
Female Community Health Volunteers and TB-infected people |
Four districts of Nepal with a high prevalence of poverty and TB | Semi-structured and key-informant interviews | [17] |
| Analysis of factors that influence early TB case detection among aged 15 years and above | Liberia | Qualitative | Not specified | Senior directors, managers of National Leprosy and TB Control centers | 15 years and above in Liberia | Internet | [18] |
| Patient and community experiences of tuberculosis diagnosis and care within a community-based intervention in Ethiopia: a qualitative study | Ethiopia | Qualitative | Yes | Clients of the community-based intervention | Treatment-seeking behavior and Perceptions of the Community Six districts | In-depth interviews | [19] |
| Barriers for tuberculosis active case finding | Ethiopia | Qualitative | Yes | TB treatment providers, program managers and TB patients | Governmental health facilities, urban health centers and rural health centers | In-depth interviews | [20] |
| Peer-led active tuberculosis case-finding among people living with HIV | Nepal | Peer-led method and clinical observation | Yes | Peer volunteers | Community districts | Screening tools and Clinical diagnosis | [21] |
| A yield and cost comparison of TB contact investigation and intensified case finding | Uganda | Qualitative | Yes | [22] | |||
| Challenges from tuberculosis diagnosis to care in community-based active case finding among the urban | Cambodia | Mixed-Methods | Yes | TB-infected village volunteers and health workers | Poor urban settlements | In-depth interviews and cross-sectional survey | [23] |
| Enablers and challenges in the implementation of active case findings in a selected district. | India | Qualitative | Yes | Healthcare providers | TB diagnostic units of Bengaluru rural district | In-depth interviews | [24] |
| Barriers to the access, diagnosis, and treatment completion for tuberculosis patients | Nepal | Qualitative | Yes | Patients, traditional healers, community members, and healthcare workers | Tanahuh, Kaski, Parsa, Nawal parasi, Mustang and Kathmandudistricts in Nepal | In-depth interviews, focus group discussions, and semi-structured interviews | [25] |
| Exploration of barriers and facilitators to household contact tracing of index tuberculosis cases | Ethiopia | Descriptive qualitative | Yes | HEWs, index TB patients, household contacts of TB patients, health center TB focal and district TB coordinators | Alamo District | In-depth and key informant interview | [26] |
| Turning off the tap: stopping tuberculosis transmission through active case-finding and prompt effective treatment. | Pakistan | RE-AIM strategy | Yes | Mobile unit attendees | Three-district region of Lima, Peru | In-depth interviews, Chest radiography | [11] |
| Improving active case finding for tuberculosis | South Africa | Qualitative | Yes | TB patients and community members | Vhembe and Waterberg districts | Semi-structured, in-depth interviews and focus group discussions | [27] |
| Patient-led active tuberculosis case-finding | Democratic Republic of Congo(DRC) | Patient-led strategy | Yes | Volunteer patients | DRC selected districts | Family history clerking | [28] |
| Optimizing tuberculosis contact investigation and linkage to care in Nairobi | Kenya | Multi-method qualitative | Yes | TB patients and healthcare workers | Study sites in Nairobi | Individual interview, focus group discussions, and key informant review | [29] |
| Capitalizing on facilitators and addressing barriers when implementing active tuberculosis case-finding in six districts of Ho Chi Minh City | Vietnam | Exploratory qualitative | Yes | Community members, healthcare staff and volunteers | Ho Chi Minh City districts | Semi-structured and key-informant interviews | [30]. |
| Active TB case finding in a high burden setting; comparison of community and facility-based strategies | Zambia | Mixed-Method | Yes | Community healthcare workers | Peri-urban settlements in Lusaka district | Digital chest x-ray, sputum analysis, and community engagement via symposia and media communications | [31] |
| Developing strategies to address barriers for tuberculosis case finding and retention in care among refugees in slums | Uganda | COMB-B model | Yes | Health care workers, community leaders, refugee TB patients and caregivers of TB patients |
Urban slum in Kampala City |
Key informant and in-depths interviews | [32] |
|
Factors associated with DELAY in diagnosis among tuberculosis patients in Hohoe Municipality |
Ghana | Mixed | Yes | New TB patients | Healthcare facilities at Hohoe Municipality | Patients’ records and interviews | [33] |
| Barriers to tuberculosis case finding in primary and secondary health facilities in Ghana: perceptions, experiences and practices of healthcare workers | Ghana | Qualitative | Yes | Healthcare workers | Rural health centers | Clinical observations and in-depth interviews | [34] |
| Factors affecting tuberculosis health message recall 2 years after active case finding in Blantyre | Malawi | Mixed-methods | Yes | Community peer group and TB monitoring officers | Urban slums of Blantyre | In-depth interviews and focus group discussions | [35] |
| Facilitators and Farriers to the implementation of a childhood tuberculosis control program | Bangladesh | Triangulation Design and Mixed | Yes | Policymakers, program managers, healthcare workers, and consumers | Urban and DOTS centers | In-depth interviews and key informant interview | [36] |
| Factors influencing the implementation of TB screening among PLHIV in selected HIV clinics | Ghana | Qualitative | Yes | HIV care providers | Regions, districts and facilities with TB/HIV coordinators | Indepth interviews and focus group discussions | [37] |
Healthcare system and governmental related barriers
The challenges in implementing ACF in healthcare have been inadequate healthcare worker training and staff shortages. The main gaps in tuberculosis control have been recognized as the limited availability of healthcare facilities and insufficient community involvement [12, 38]. Funding subsistence for tuberculosis care is a long-term challenge in many countries. To alleviate this financial burden, specific measures are needed at different levels, including linking tuberculosis to the overall social protection system [26, 39]. Resource constraints in LMICs limit TB contact investigation despite its benefits outweighing its cost and its increased efficiency when compared with intensified case finding (see Tables 2 and 3). Inadequate laboratory infrastructure for maintaining functional Xpert equipment further challenges implementation and scale-up [40]. Generally, shortages of healthcare providers, inadequate basic infrastructure, and inadequate diagnostic equipment and supplies were identified as barriers to TB case finding [41]. Also included was limited access to TB diagnostic services, which can be absent or characterized by delays in the diagnostic process.
Table 2.
Key barriers and facilitators of active TB case findings in low-income countries identified from the included studies (n = 11)
| Study location | Facilitators | Barriers | Authors |
|---|---|---|---|
| Ethiopia | Social support and training of health workers | Distance, shortage of money, stigma, discrimination, the workload of household contacts and health workers, shortage of reagents, absence of well-ventilated TB class, and the lack of regular monitoring and supervision | [26] |
| Uganda | Education, persuasion, enablement, modeling of health-positive behaviors, incentivization,and restructuring of the health service environment | Stigma, limited knowledge about TB among contacts, insufficient time and space in clinics for counseling, mistrust of health center staff among index patients and contacts, and high travel costs for LHWs and contacts | [16] |
| Liberia | Develop a TB communication strategy, strengthen community-based DOTs, and intensify screening, knowledge and awareness of TB | No regular monitoring of household contacts, screening for index TB cases, longer distances, transportation cost, stigma, misconception about TB signs, outdated protocols, limited laboratory supplies, poor data quality and feedback system | [18] |
| Ethiopia | Embedding TB services within communities was an acceptable approach for vulnerable groups experiencing poor access to health facilities. | Difficulties faced in accessing district-level health facilities | [19] |
| Ethiopia | Inadequate resources, limited access to diagnostic services, and inadequate diagnostic equipment and supplies | [20] | |
| Uganda | The ability of LHWs to persuade index patients, communicate with patients via mobile phones, trust between index patients and LHWs, flexible scheduling of home visits, evaluation, the reduce risk associated with the transport of LHWs, family social support for contacts and payment for LHWs. | Lack of local contact investigation guidelines, lack of travel funds for contacts, stigma, lack of TB knowledge among contacts, the language barrier between LHWs and contacts, difficulties in locating households, avoidant behaviors of contacts, and fear of TB diagnosis among contacts | [22] |
| Kenya | Invitation of TB patients to bring contacts and HWS close and patients understanding the transmission of TB as a proactive measure by HWS | Long waiting times, inconducive clinic hours, poor community awareness about TB, and stigma. | [29] |
| DRC | Peer-led increase in active TB cases finding | [28] | |
| Zambia | Patients screened at the facility level, increased awareness and demand creation activities, and the use of more sensitive screening and diagnostic tools | Patients screened from the general community and long waiting time | [31] |
| Uganda | Physical capability (availability of free TB services in public health facilities), social opportunity (availability of translators), identified education, incentivization, and training | Unavailability and easily accessible private facilities with no capacity to diagnose and treat TB in the community, lack of knowledge about TB among refugees, and widespread of TB stigmatization and language barrier, poor living conditions, mobility of refugees, lack of facilitation for health workers, discrimination and rejection of TB patients | [32] |
| Malawi | Community education, sensitization and engagement, community need to ACF when service is at their home | Fear of HIV diagnosis and association, health care seeking behavior barriers | [35] |
Table 3.
Key barriers and facilitators of active TB case findings in middle income countries identified from the included studies (n = 12)
| Study location /Country | Facilitators | Barriers | Authors |
|---|---|---|---|
| Cambodia | Build trust and facilitate communication, a patient-centered approach and community involvement | High indirect costs, privacy and stigma issues, and anticipated treatment side effects | [23] |
| Nepal | The utility of education for providers and appointments in which physicians use Xpert in TB diagnosis was noted to have improved the acceptability | Re-evaluation by pulmonologists at the government hospitals, even if they had positive Xpert, and the lack of knowledge about diagnostic tests | [17] |
| South Africa | Door-to-door activities giving access to respected leaders of the community, such as chiefs and civic leaders; Incentivization | Lack of TB knowledge, social (TB stigma), and structural factors (distance, time and lack of money for transportation) | [27] |
| India | Involving local leaders and panchayat members, issuing identity cards to field staff, increasing monetary incentives, training ASHA in counseling and sputum collection, and financial support to patients for chest X-ray examination and travel | Inadequate training, shortage of staff, stigma, lack of awareness about TB, illiteracy, inability to convince patients for sputum tests, and delay in getting CBNAAT. | [24] |
| Nepal | Lack of trained health personnel, lack of equipment ,and irregular presence of health workers | [25] | |
| Pakistan | The inclusion of targeted active case-finding in a comprehensive epidemic-control strategy for tuberculosis | [11] | |
| Vietnam | Communication and awareness-raising, preparation and logistics, data systems and processes, and incentives. Strengths of employees and volunteers to capitalize on experience, skills, and communication. | Stigma, discrimination, and mistrust | [32] |
| Ghana | Lack of medical insurance, perceived stigma, and making multiple healthcare encounters. | [33] | |
| Ghana | Health system barriers include lack of TB diagnostic laboratories in rural health facilities and no standard referral system to the municipal hospital for further assessment and TB testing. Heath worker- related barriers such as lack of training on case detection guidelines, fear of infection (exacerbated by lack of appropriate personal protective equipment and lack of motivation among HWS for TB work | [34] | |
| Bangladesh | Government stewardship, presence of specific guidelines, knowledge and capacity building of frontline health workers | Lack of diagnostic facilities, lack of diagnostic facilities, and poor engagement of private practitioners | [36] |
| Ghana | Good communication and referral channels, health workers recognizing the need for interventions and the role of chemical sellers | Low commitment of the implementers to screen for TB. | [37] |
Access and health service delays, longer distances, transportation costs, poor quality of services, understaffing, poor motivation, outdated protocols, limited laboratory supplies, limited screening among high-risk groups, and poor data quality and feedback systems were the major constraints to TB diagnosis and implementation of services in Liberia [42]. Commonly noted barriers in Uganda included insufficient time and space in clinics for counseling and mistrust of health-center staff among index patients and contacts [43]. Logistics and infrastructure, waiting time and institutional readiness, referral, feedback, human resources, charges for using some laboratories, workloads, and distance to TB facilities were barriers to TB contact tracing and investigation in Ethiopia [44].
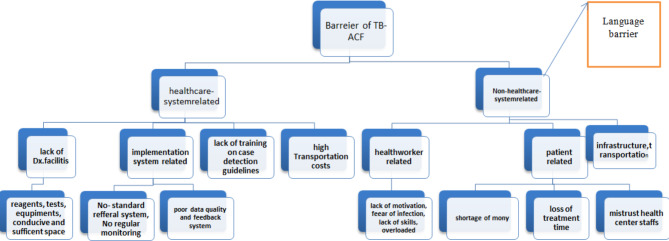
Healthcare system-related and non- healthcare system-related barriers
The identification of active tuberculosis is impeded by two main categories of obstacles, namely health system-related and non-health system-related barriers, as illustrated in Table 4; Fig. 2. The studies analyzed in this research revealed several health system-related barriers, among which a dearth of diagnostic resources (including equipment, reagents, and tests), as well as inadequate TB awareness, were the most frequently observed ones. Conversely, barriers not associated with the healthcare system encompassed stigmatization, transportation costs, insufficient education, limited awareness concerning diagnostic testing, and the presence of a language barrier.
Table 4.
Healthcare system and non- healthcare system-related barriers to tuberculosis active case findings in LMICS (n = 21)
| S. No | Barriers | Author | |
|---|---|---|---|
| Theme-1: Healthcare system related | Theme − 2: Non- healthcare system | ||
| 1 | privacy and stigma issues ,anticipated treatment side effects, High indirect costs | [23] | |
| 2 | Re-evaluation by pulmonologists at the government hospitals, even if they had positive Xpert, and | the lack of knowledge about diagnostic tests | [17] |
| 3 | Stigmatization | [21] | |
| 4 | Stigma, time, Lack of TB Knowledge, Distance and lack of money for transportation | [27] | |
| 5 | lack of awareness about TB, shortage of staff, Inadequate training | stigma, illiteracy, inability to convince patients to sputum test | [24] |
| 6 | lack of equipment | Lack of trained health personnel ,irregular presence of health workers | [25] |
| 7 | --------------------- | Stigma, discrimination, and mistrust | [32] |
| 8 | Lack of medical insurance, making multiple healthcare encounters. | perceived stigma, | [33] |
| 9 | lack of TB diagnostic laboratories, no standard referral system to the municipal hospital for further assessment and TB testing, lack of training on case detection guidelines | fear of infection, lack of motivation among HWS for TB workers | [34] |
| 10 | lack of diagnostic facilities, and poor engagement of private practitioners | -------- | [36] |
| 11 | The low commitment of the implementers to screen for TB | ------ | [37] |
| 12 | shortage of reagents, absence of well-ventilated TB class, the lack of regular monitoring and supervision and the workload on health workers, | Shortage of money, stigma, discrimination, workload of household contacts and distance | [16] |
| 13 | insufficient space in clinics, high travel costs for LHWs ,insufficient time | Stigma, limited knowledge about TB among contacts, mistrust of health center staff among index patients and contacts | [18] |
| 14 | limited laboratory supplies, No regular monitoring of household contacts, poor data quality and feedback system | stigma, screening for index TB cases &misconception about TB signs, transportation cost | [19] |
| 15 | Difficulties faced in accessing district level health facilities | --------------------------- | [20] |
| 16 | limited access to diagnostic services, inadequate diagnostic equipment and supplies, as well asinadequate resources | --------- | [16] |
| 17 | language barrier between LHWs and contacts, difficulties in locating households, avoidant behaviors of contacts, fear of TB diagnosis among contacts, lack of travel funds for contacts | [29] | |
| 18 | Long waiting times, in conducive clinics, poor community awareness about TB | Stigma | [28] |
| 19 | Patients screened from the general community and long waiting time | ---------------- | [31] |
| 20 | Unavailability and easily accessible private facilities with no capacity to diagnose and treat TB in the community | language barrier, mobility of refugees, wide spread of TB stigmatization, lack of knowledge about TB among refugees | [32] |
| 21 | health care seeking behavior barriers | Fear of HIV Diagnosis and Association | [35] |
Fig. 2.
The major barberries classified under healthcare and non-healthcare systems in LMICS
Limited understanding and awareness regarding the identification of signs and symptoms, as well as misconceptions surrounding tuberculosis, have proven to be the primary contributing factors to the delay in patients accessing tuberculosis services [44]. Nevertheless, the familiarity and knowledge of the community demonstrated by village health volunteers have been crucial in facilitating the initial access to active case-finding participants. However, at times, this familiarity has negatively impacted their perceived legitimacy among community members who are aware of their lack of medical training. To gain respect among their peers in the community, village health volunteers recognize the importance of affiliating with tuberculosis workers and other trained healthcare providers [45].
According to Marangu et al.[29], the key barriers to CI were the failure of HCWs to educate and invite TB patients to bring close contacts for TB screening, sub-optimal processes and flow of TB patients, HCW and community TB-related stigma [46]. In another study, knowledge, commitment and motivation, and stigma and discrimination for household contact-tracing of index TB cases were also identified [47]. One practical consideration for the implementation of targeted ACF activities was convincing individuals to undergo screening for a stigmatized disease, especially if the screening requires time and effort on the part of the individuals[24]. Seeking private health care and self-medication before TB diagnosis, lack of perceived risk, threat, susceptibility, and stigma derived qualitatively further explained the quantitative findings [41]. The different attitude of the community due to stigma, lack of awareness about TB, illiteracy and inability to convince patients for sputum tests were challenges to conduct ACF [42]. High travel costs for LHWs and contacts were also noted as barriers to TB contact investigation [43].
Facilitators
The most important facilitators identified were the personalized and enabling services provided by LHWs. The study identified education, persuasion, enablement, modeling of health-positive behaviors, incentivization, and restructuring of the service environment as relevant intervention functions with potentials to alleviate barriers to and enhance facilitators of TB contact investigations[26]. Implementers’ motivation and incentives fostered active case-finding policy implementation[48]. Public health providers were motivated by the increased early case detection and expedited sequence from screening to treatment. TB workers were motivated by the increased awareness, improved health-seeking behaviors among TB patients and strengthened competence of village health volunteers in target communities [49].
To address the challenge of TB “missing cases”, policies, effective strategies, and implementation of active case interventions for TB key populations are highly essential globally [17]. By bringing TB services closer to the community, participants reported that ACF had removed barriers to access and cost. This was particularly appreciated by the elderly and severely ill, whose physical conditions prevented them from traveling to the health centers for screening and treatment [50]. Ensuring and outlining good health outcomes, and limiting TB transmission within hard-to-reach groups, can prove challenging. The reason is that the hard-to-reach groups may experience difficulties in accessing care, and if they do access it, they may experience difficulties remaining in it[51].
Approaches such as improving TB diagnostic tools and algorithms, and engaging all care providers are suggested to find missing TB patients[52]. The involvement of HCWs in the general activities of counseling patients, and issuing of identity cards to them for ease of recognition, was recommended to foster ACF [53]. To maintain benefits from different approaches, there is a need to distinguish between CHWs that are trained and remunerated to be a part of an existing health system and those who, with little training, take on roles and are motivated by a range of contextual factors. Governments and planners can benefit from understanding the program that can best be supported in their communities, thereby maximizing motivation and effectiveness[54].
Assessment of confidence in the evidence of the review findings
Two of the reviewer authors (MD and AG) applied the confidence of evidence review quality (CERQual) approach to assess the confidence in the findings of the review independently. Then, the evidence review quality approach assesses confidence in the review findings and is conducted based on four components namely; the methodological limitations of included studies, the relevance of the included studies to the review question, the coherence of the review findings and the adequacy of data contributing to the review findings [55] as shown Fig. 3. Every issue or phenomenon that was relevant to the four components was noted in the review results and taken into account when determining the overall CERQual assessment as high, moderate, low, or extremely low as depicted in Table 5.
Fig. 3.
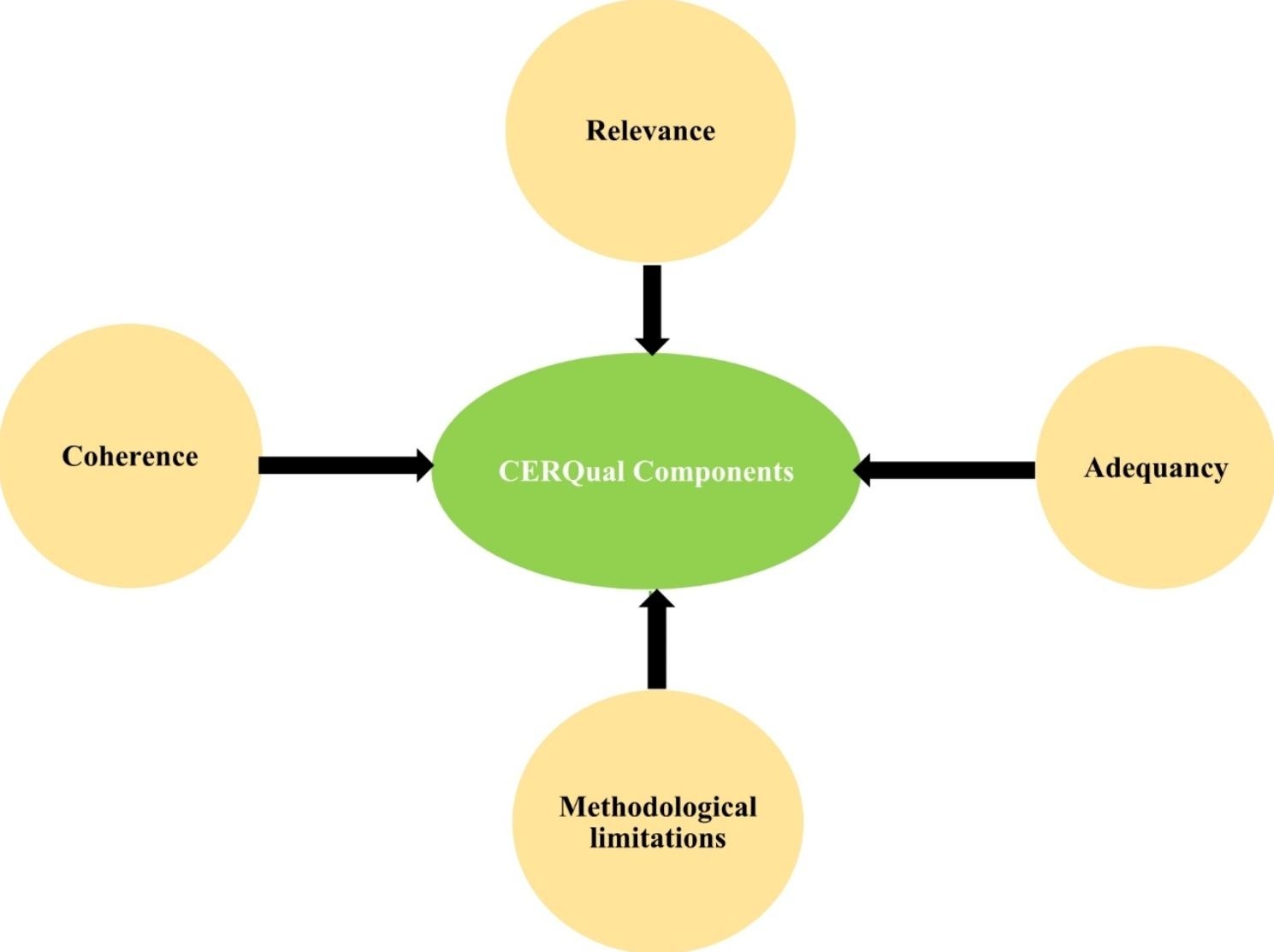
The components of CERQual
Table 5.
Summary of CERQual Confidence Rating on the main findings
| Key findings | CERQual Rating | Explanation of the evidence assessment rating |
|---|---|---|
| Health workers encounter barriers pertaining about their experiences, knowledge, and skill set in identifying tuberculosis through active case finding, even when situated in healthcare establishments. | Moderate confidence | Although half of the articles raise important methodological issues (2/4), it is noteworthy that the principal discovery is consistent in all articles have significant methodological concerns, yet the key finding is consistently supported by directly relevant data in reviews with only minor |
| Direct and indirect costs of the patients | High confidence | All of the articles presented in this study provide supporting evidence for the primary findings. However, it is important to note that one (1/4) of articles have brought to light significant methodological flaws. In contrast, assessments that exhibit other methodological issues are can offer direct and valuable insights into both the primary findings |
| The present study investigates the accessibility and the magnitude of workloads that health workers face in the context of tuberculosis active case finding (ACF). | high confidence | The data evaluated in this investigation is of great significance (3/3) and has been thoroughly documented. The evaluations present unequivocal proof that is methodologically sound. |
| The lack of essential resources such as diagnostic equipment, reagents, and TB ACF supplies is a significant hindrance to effective tuberculosis control efforts. | Very low confidence | The methodology-related problems addressed by the present study relate to the indirect or partial applicability of earlier reviews that provided support for the primary finding. |
| Barriers related to stigma in the detection of TB ACF | Moderate confidence | In general, the included studies were moderately conducted (5/6). The review findings cut across many study settings and scientific procedures. |
| Barriers pertaining to the communication strategy and language limitations in the context of tuberculosis active case finding pose significant challenges. | Moderate confidence | The methodologies of the three studies were very critical and followed scientific procedures. Some of the studies have direct and indirect relevance. |
The barriers that were identified during our review have been consolidated into eight overarching themes. These themes were derived from general concepts and through consensus among the review authors, as detailed in Table 6. In addition, our summary of qualitative findings included a CERQual assessment and a written justification, as outlined previously. It is important to note that the findings presented in our review are contingent upon various factors, such as the review question, the synthesis techniques employed, the intended application or target of the synthesis, and the depth of the data provided. These factors collectively influence the conclusions that we have drawn from our analysis [56].
Table 6.
Confidence of Evidence Review quality (CERQual) summary of review findings, appraisal, and synthesis of qualitative research evidence on the barriers and facilitators to tuberculosis active case findings in low- and middle-income countries
| S/N | key review findings | Contributing studies | Methodological limitation | Coherence | Adequacy | Relevance | Confidence in evidence | Explanation of the evidence assessment | ||
|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Barriers related to experiences, knowledge, and skills of health workers to detect TB ACF, even in health facilities | [17, 25–27] | Moderate concern | Very minor concern | Minor concern | Very minor concern | High | The data were from three middle and one low income countries. There are direct and indirect relevance in the studies also. | ||
| 2. | Barriers related to distance and time, including funds related to transportation and incentives for the patients | [16, 23, 26, 27] | Very minor concern | Very minor concern | Very minor concern | Very minor concern | High | The methodologies of the three studies were very critical and follow scientific procedures. The studies had 50% distribution between low and middle income countries covering Ethiopia, Cambodia, South Africa and Uganda. | ||
| 3. | Barriers related to the availability and workloads of health workers in TB ACF | [22, 24, 25] | Moderate concern | Very minor concern | Serious concern | Moderate concern | Very low | The methodological limitations of two of the studies were unclear study designs, inappropriate data collection technique and very thin data. The data was generated from low income country (Ethiopia) and middle income countries (Nepal and India). | ||
| 4. | Barriers related to the absence of resources like diagnostic equipment, reagents and supplies for TB ACF | [17, 22, 25, 26, 36] | Moderate concern | Very minor concern | Serious concern | Serious concern | Very low | Some of the studies had direct and indirect relevance, very thin data, and lack ethical considerations. Data were collected from studies from low (Ethiopia and Uganda) and middle income countries (Nepal and Bangladesh). | ||
| 5. | Barriers related to stigma in the detection of TB ACF | [16, 17, 21, 22, 26, 32] | Very minor concern | Very minor concern | Very minor concern | Very minor concern | Moderate | In general, the included studies were moderately conducted. The review findings cut across many study settings and scientific procedures. Data were sourced from four low (between Ethiopia and Uganda) and three middle (between Nepal and Bangladesh) income countries. | ||
| 6. | Barriers related to lack of training for existing and new health workers on the detection of TBACF | [22,24, 25,29 ] | Very minor concern | Very minor concern | Very minor concern | Very minor concern | The methodology of the study was very critical and follows scientific procedures. The data sources were from low and middle income countries such as Ethiopia, Cambodia, South-Africa and Uganda | |||
| 7. |
Barriers related to communication strategy and language restrictions for tuberculosis ACF |
[22, 32, 37] | Very minor concern | Very minor concern | Very minor concern | Very minor concern | The methodologies of the three studies were very critical and follow scientific procedures. Some of the studies have direct and indirect relevance. The data sources were from low and middle income countries such as Ethiopia, Cambodia, South-Africa and Uganda. | |||
| 8. | Barriers related to inadequate or lack of community awareness about TB among contacts | [11, 16, 18] | In general, studies were moderately executed. However, the findings were sourced from 2 countries. | |||||||
Discussion
In this qualitative systematic review, we identified 23 studies (12 from middle-income countries and 11 from low-income countries), of which 19 reported qualitative data methods on barriers and facilitators of TB case finding to earlier detection in LMICs. All studies of these LMICs identified hard-to-reach communities as the main carriers of this disease. Advanced and effective TB programs are needed given the disease’s contagiousness, airborne transmission and rising TB incidence in some countries. In terms of the study design, five of the investigations delineated mixed-method barriers and facilitators [23, 31, 33, 36].
In general, the overall evidence supporting the factors influencing tuberculosis ACF in low- and middle-income countries were high at present, despite several interventions and varying types of tools adopted in different patient populations in the LMICs. This study reported a slightly positive influence associated with facilitators of TB contact investigation and ACF. There were a few overlapping explanations for the factors influencing TB ACF [16, 22–24, 26, 27, 32] and for positive psycho-social interventions used as the facilitators of ACF. In tuberculosis ACF, systematic identification and screening of people with presumptive TB symptoms, in a pre-determined target group, using tests, examinations, or other procedures that can be applied rapidly [57]. Interventions relating more to the psycho-social factors in persons, who were asymptomatic for TB, such as group-based psychotherapy, are important to boost and give confidence to stigmatized persons. This way could improve interpersonal and self-esteem as well as public health value by influencing positively psycho-social factors like mood, thereby affecting interpersonal barriers.
Inadequate resources, limited access to diagnostic services, inadequate diagnostic equipment and supplies were the most important factors influencing active case findings both low and middle-income countries [17, 20, 25, 36], while TB communication strategy and language were the key barriers for tuberculosis ACF [16, 18]. Peer-led, patient-centered approaches and community involvement increased the active finding of TB cases [23, 28].
This study suggested that TB case identification may be improved if the community could easily access health facilities with TB diagnostic services. Similarly, studies show that case notification increase in areas where community members have better access to facilities with TB diagnostic services [20, 58]. In most low income countries, health extension workers are intentionally placed at the community level to reinforce the accessibility of the rural population to different health services, including TB care. Still, health extension workers lack, so to alleviate the lack of transportation facilities to reach TB services and increase the ACF strategies the number of health extension workers and community-based identification methods should be scaled up in rural and remote areas.
The use of an active case-finding approach, which includes conducting household symptom screening through door-to-door community visits coupled with the integration of laboratory testing, has resulted in improved detection of tuberculosis cases in rural areas. This finding is supported by reference [59]. Moreover, active case finding through community outreach improved the speed of TB case finding, which indicated a possibility to reduce delays in TB diagnosis [60]. This strategy could help in solving problems related to unmet health needs in general, and undiagnosed TB cases in particular, for the rural population. The current review has ascertained that stigma is frequently encountered and functions as an impediment to obtaining care for those with ACF-TB; this may plausibly be attributed to the lack of health advocacy and awareness initiatives. Stigmatization and discrimination pose significant risks to individuals undergoing TB screening or diagnosed with TB, potentially undermining the success of the screening process.
The needs of vulnerable people must be served by increasing access to healthcare services while simultaneously minimizing the direct and indirect costs of seeking medical care. This can be achieved by strengthening primary health-care services, providing additional outreach services that cater to these populations, and implementing social protection schemes where necessary. In order to ensure that individuals with prevalent active TB cases seek care at facilities capable of diagnosing and treating TB, community engagement and demand in communities at a higher risk of TB must be increased. The implementation and adaptation of bidirectional screening, as demonstrated by this investigation, provides valuable proof to enhance the outcomes of TB-active case detection.
The findings of this qualitative systematic review have significant implications for policy modification and development in the context of tuberculosis active case finding (TB-ACF) in low- and middle-income countries (LMICs). The identified studies highlight various barriers and facilitators that influence TB case detection and earlier diagnosis in LMICs [21].
One key implication is the need for advanced and effective TB-ACF programs, considering the contagiousness and airborne transmission of the disease, as well as the rising TB incidence in certain countries. The study emphasizes the importance of targeted interventions and tools to reach hard-to-reach communities, which have been identified as the main carriers of TB [22].
The study also highlights the value of psychosocial interventions, such as group-based psychotherapy, to help stigmatized people overcome interpersonal barriers, increase their confidence, and boost their self-esteem. By influencing psychosocial aspects such as mood and promoting improved access to diagnostic services, these interventions can have a positive impact on TB-ACF outcomes [23]. The review also highlights specific barriers that need to be addressed, including failure of health workers to educate and invite TB patients to bring their close contacts to be screened, suboptimal processes and patient flows, TB-related stigma and knowledge gaps among HCWs, discrimination in contact tracing in the Budget, insufficient resources and limited access to diagnostic services, and communication barriers [26].
In order to surmount the barriers impeding TB-ACF and to amplify its facilitators, the present study suggests a range of measures. Firstly, enhancing community access to health facilities with TB diagnostic services is recommended. Secondly, there is a need to scale up the number of health extension workers in rural and remote areas. Furthermore, active case finding through community outreach and door-to-door visitation should be implemented. Lastly, addressing stigma through health advocacy and awareness programs is crucial. Thirdly, it is imperative to address these challenges by means of providing adequate training to healthcare workers [61].
Additionally, this review stresses the significance of improving access to care, reducing costs associated with seeking care, strengthening primary health-care services, providing outreach services for vulnerable populations, and implementing social protection schemes where necessary. These findings are in line with other studies conducted in LMICs, which have also adopted multiple interventions and strategies to enhance TB-ACF. However, more comprehensive and coordinated efforts are required to address the identified barriers and utilize the facilitators of TB-ACF effectively.
The strength and limitation of the study
Active case finding represents the most prominent approach in controlling and preventing tuberculosis. Given its significance, this finding offers a critical source of information in the global efforts to eradicate TB, as it constitutes the first summary of active case finding. However, it should be noted that these findings cannot be universally applied across all populations and diseases. The strength of this systematic review is rooted in the use of different guidance and qualitative check tools, such as PRISMA, CEQual, BJI, and ENTREQ, thus underscoring its status as an evidence-based study. One of the limitations of this review is its small sample size, which only includes 23 studies, thereby potentially reducing its generalizability. Another limitation pertains to the analysis methods employed for the qualitative data, as the review relied solely on narrative summaries presented in tables and diagrams. The other basic limitation of this manuscript is lack of PROSPERO Registration number.
Conclusion
This qualitative systematic review examines that stigma is the top patient- and community-related barrier, followed by health-system-related barriers such as lack of resources, including lack of diagnostic equipment, reagents, and consumables for the detection of cases with active TB. In this review, supervision, health worker training, leadership, integration into health systems, and long-term funding are key to the sustainability of tuberculosis-ACF. Financial support for staff time and program costs associated with expanding patient enrollments were seen as important factors in maintaining public sector commitment. In addition, government leadership, the existence of specific policies, the knowledge, clinical skills, and capacity building of frontline health workers are also key enablers for ACF in LMICs. The risks of stigmatization should be carefully assessed prior to initiating screening of the patients.
In conclusion, this review provides valuable evidence to support the modification and development of policies related to TB-ACF in LMICs. By addressing the identified barriers, promoting community engagement, and implementing bidirectional screening, policymakers can enhance TB case detection, reduce delays in diagnosis, and improve overall outcomes of TB-ACF programs.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Not applicable.
Abbreviations
- ACF
Active Case Finding
- JBI
Joanna Briggs Institute’s
- ENTREQ
Enhancing Transparency in Reporting the Synthesis of Qualitative Research
- CERQual
Confidence of Evidence Review Quality
- PROSPERO
International Prospective Register of Systematic Reviews
- CRD
Central Registration Depository
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-analysis
- LHW
Lay Health Worker
- HW
Health Worker
- ASHA
Accredited Social Health Activists
- CBNAAT
Catridege Based Nucleic Acid Amplification Test
Authors’ contributions
Melkie Dagnaw Fenta and Oluwaseun Adeolu Ogundijo conducted the method, data extraction, abstract, and introduction. Melkie Dagnaw Fenta and Ahmed Abi Abdi Warsame also performed the classification of the findings and reference citation part of the manuscript. Melkie Dagnaw Fenta and Abebaw Getachew Belay applied the confidence of evidence review quality (CERQual). Melkie Dagnaw Fenta, Oluwaseun Adeolu Ogundijo, Ahmed Abi Abdi Warsame, and Abebaw Getachew Belay, critically assessed the quality assessments part of the manuscript. All authors participated in all preparation and writing procedures and approved the final manuscript.
Funding
No specific funding for this review.
Data Availability
All important data and results are included in this manuscript.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization (WHO). Global Tuberculosis Report 2017. Geneva, Switzerland. 2017. 10.1001/jama.2014.11450.
- 2.Petersen E et al. International Journal of Infectious Diseases; 2022. World TB Day 2022: Revamping and Reshaping Global TB Control Programs by Advancing Lessons Learnt from the COVID-19 Pandemic. [DOI] [PMC free article] [PubMed]
- 3.Kyu HH, Maddison ER, Henry NJ, Mumford JE, Barber R, Shields C, et al. The global burden of tuberculosis: results from the global burden of Disease Study 2015. Lancet Infect Dis. 2018;18(3):261–84. doi: 10.1016/S1473-3099(17)30703-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Vries SG, Cremers AL, Heuvelings CC, Greve PF, Visser BJ, Bélard S, et al. Barriers and facilitators to the uptake of tuberculosis diagnostic and treatment services by hard-to-reach populations in countries of low and medium tuberculosis incidence: a systematic review of qualitative literature. Lancet Infect Dis. 2017;17(5):e128–43. doi: 10.1016/S1473-3099(16)30531-X. [DOI] [PubMed] [Google Scholar]
- 5.Ho J, Fox GJ, Marais BJ. Passive case finding for tuberculosis is not enough. Int J Mycobact. 2016;5:374–8. doi: 10.1016/j.ijmyco.2016.09.023. [DOI] [PubMed] [Google Scholar]
- 6.Golub JE, Mohan CI, Comstock GW, Chaisson RE. Active case finding of tuberculosis: historical perspective and future prospects. Int J Tuberc Lung Dis. 2005;9:1183–203. [PMC free article] [PubMed] [Google Scholar]
- 7.Saunders MJ, Tovar MA, Collier D, Baldwin MR, Montoya R, Valencia TR, Gilman RH, Evans CA. Active and passive case-finding in tuberculosis-affected households in Peru: a 10-year prospective cohort study. Lancet Infect Dis. 2019;19(5):519–28. doi: 10.1016/S1473-3099(18)30753-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zenner D, Southern J, Van Hest R, DeVries G, Stagg HR, Antoine D, Abubakar I. Active case finding for tuberculosis among high-risk groups in low-incidence countries [State of the art series. Case finding/screening. Number 3 in the series] Int J Tuberc Lung Dis. 2013;17(5):573–82. doi: 10.5588/ijtld.12.0920. [DOI] [PubMed] [Google Scholar]
- 9.Li J, Chung PH, Leung CL, Nishikiori N, Chan EY, Yeoh EK. The strategic framework of tuberculosis control and prevention in the elderly: a scoping review towards end TB targets. Infect Dis poverty. 2017;6(03):16–279. doi: 10.1186/s40249-017-0284-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ho J, Fox GJ, Marais BJ. Passive case finding for tuberculosis is not enough. Int J mycobacteriology. 2016;5(4):374–8. doi: 10.1016/j.ijmyco.2016.09.023. [DOI] [PubMed] [Google Scholar]
- 11.Yuen CM, et al. Turning off the tap: stopping tuberculosis transmission through active case-finding and prompt effective treatment. Lancet. 2015;386(10010):2334–43. doi: 10.1016/S0140-6736(15)00322-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Indira Krishnan AK, Mini GK, Aravind LR. Evidence based interventions and implementation gaps in control of tuberculosis: a systematic review in low and middle-income countries with special focus on India. Indian J Tuberc. 2019;66(2):268–78. doi: 10.1016/j.ijtb.2019.04.006. [DOI] [PubMed] [Google Scholar]
- 13.Tong A, et al. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;12:181. doi: 10.1186/1471-2288-12-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aromataris E, et al. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc. 2015;13(3):132–40. doi: 10.1097/XEB.0000000000000055. [DOI] [PubMed] [Google Scholar]
- 15.Lewin S, et al. Using qualitative evidence in decision making for health and social interventions: an approach to assess confidence in findings from qualitative evidence syntheses (GRADE-CERQual) PLoS Med. 2015;12(10):e1001895. doi: 10.1371/journal.pmed.1001895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ayakaka I, et al. Identifying barriers to and facilitators of tuberculosis contact investigation in Kampala, Uganda: a behavioral approach. Implement Sci. 2017;12(1):33. doi: 10.1186/s13012-017-0561-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Biermann O, et al. Power plays plus push’: experts’ insights into the development and implementation of active tuberculosis case-finding policies globally, a qualitative study. BMJ Open. 2020;10(6):e036285. doi: 10.1136/bmjopen-2019-036285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dunbar N. Analysis of factors that influence early tuberculosis case detection analysis of factors that influence early tuberculosis case detection among aged 15 years and above in Liberia. 2014.
- 19.Tulloch O, et al. Patient and community experiences of tuberculosis diagnosis and care within a community-based intervention in Ethiopia: a qualitative study. BMC Public Health. 2015;15(1):1–9. doi: 10.1186/s12889-015-1523-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ereso BM, et al. Barriers for tuberculosis case finding in Southwest Ethiopia: a qualitative study. PLoS ONE. 2020;15(1):e0226307. doi: 10.1371/journal.pone.0226307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joshi D, Sthapit R, Brouwer M. Peer-led active tuberculosis case-finding among people living with HIV: lessons from Nepal. Bull World Health Organ. 2017;95(2):135–9. doi: 10.2471/BLT.16.179119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kakinda M, Matovu JKB. A yield and cost comparison of tuberculosis contact investigation and intensified case finding in Uganda. PLoS ONE. 2020;15(6):e0234418. doi: 10.1371/journal.pone.0234418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lorent N, et al. Challenges from Tuberculosis diagnosis to Care in Community-Based active case finding among the Urban Poor in Cambodia: a mixed-methods study. PLoS ONE. 2015;10(7):e0130179. doi: 10.1371/journal.pone.0130179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shamanewadi AN et al. Enablers and Challenges in the implementation of active case findings in a selected District of Karnataka, South India: a qualitative study. Tuberc Res Treat. 2020:9746329. [DOI] [PMC free article] [PubMed]
- 25.Marahatta SB, et al. Barriers in the access, diagnosis and treatment completion for tuberculosis patients in central and western Nepal: a qualitative study among patients, community members and health care workers. PLoS ONE. 2020;15(1):e0227293. doi: 10.1371/journal.pone.0227293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tesfaye L, et al. Exploration of barriers and facilitators to household contact tracing of index tuberculosis cases in Anlemo district, Hadiya zone, Southern Ethiopia: qualitative study. PLoS ONE. 2020;15(5):e0233358. doi: 10.1371/journal.pone.0233358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kerrigan D, et al. Improving active case finding for tuberculosis in South Africa: informing innovative implementation approaches in the context of the Kharitode trial through formative research. Health Res Policy Syst. 2017;15(1):42. doi: 10.1186/s12961-017-0206-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.André E, et al. Patient-led active tuberculosis case-finding in the Democratic Republic of the Congo. Bull World Health Organ. 2018;96(8):522–30. doi: 10.2471/BLT.17.203968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marangu D, et al. Stakeholder perspectives for optimization of tuberculosis contact investigation in a high-burden setting. PLoS ONE. 2017;12(9):e0183749. doi: 10.1371/journal.pone.0183749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Biermann O, et al. Capitalizing on facilitators and addressing barriers when implementing active tuberculosis case-finding in six districts of Ho Chi Minh City, Vietnam: a qualitative study with key stakeholders. Implement Sci. 2021;16(1):54. doi: 10.1186/s13012-021-01124-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kagujje M, et al. Active TB case finding in a high burden setting; comparison of community and facility-based strategies in Lusaka, Zambia. PLoS ONE. 2020;15(9):e0237931. doi: 10.1371/journal.pone.0237931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Buregyeya E, et al. Developing strategies to address barriers for tuberculosis case finding and retention in care among refugees in slums in Kampala, Uganda: a qualitative study using the COM-B model. BMC Infect Dis. 2022;22(1):301. doi: 10.1186/s12879-022-07283-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Osei E, Akweongo P, Binka F. Factors associated with DELAY in diagnosis among tuberculosis patients in Hohoe Municipality, Ghana. BMC Public Health. 2015;15:721. doi: 10.1186/s12889-015-1922-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Der JB, et al. Barriers to tuberculosis case finding in primary and secondary health facilities in Ghana: perceptions, experiences and practices of healthcare workers. BMC Health Serv Res. 2022;22(1):368. doi: 10.1186/s12913-022-07711-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Monk EJM, et al. Factors affecting tuberculosis health message recall 2 years after active case finding in Blantyre, Malawi. Int J Tuberc Lung Dis. 2018;22(9):1007–15. doi: 10.5588/ijtld.18.0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pantha S, et al. Facilitators and barriers to implementation of a Childhood Tuberculosis Control Program in Bangladesh: a mixed-methods study from BRAC Urban DOTS Centres in Dhaka. Nurs Rep. 2022;12(2):371–86. doi: 10.3390/nursrep12020036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Narh-Bana SA, et al. Factors influencing the implementation of TB screening among PLHIV in selected HIV clinics in Ghana: a qualitative study. BMC Health Serv Res. 2022;22(1):898. doi: 10.1186/s12913-022-08295-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zumla A, Abubakar I. Improving access to multi-drug resistant tuberculosis diagnostic and health services for refugees and migrants. BMC Med. 2018;16(1):221. doi: 10.1186/s12916-018-1218-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rahevar K, et al. Implementing the end TB strategy in the Western Pacific Region: translating vision into reality. Respirology. 2018;23(8):735–42. doi: 10.1111/resp.13308. [DOI] [PubMed] [Google Scholar]
- 40.Naidoo K, et al. Addressing challenges in scaling up TB and HIV treatment integration in rural primary healthcare clinics in South Africa (SUTHI): a cluster randomized controlled trial protocol. Implement Sci. 2017;12(1):129. doi: 10.1186/s13012-017-0661-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Oga-Omenka C et al. Factors influencing diagnosis and treatment initiation for multidrug-resistant/rifampicin-resistant tuberculosis in six sub-saharan african countries: a mixed-methods systematic review. BMJ Glob Health, 2020;5(7). [DOI] [PMC free article] [PubMed]
- 42.Baluku JB, et al. Tuberculosis contact tracing yield and associated factors in Uganda. BMC Pulm Med. 2022;22(1):64. doi: 10.1186/s12890-022-01860-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gashu Z, et al. The yield of community-based “Retrospective” Tuberculosis Contact Investigation in a high Burden setting in Ethiopia. PLoS ONE. 2016;11(8):e0160514. doi: 10.1371/journal.pone.0160514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Eltayeb D, et al. Factors associated with tuberculosis diagnosis and treatment delays in Middle East and North Africa: a systematic review. East Mediterr Health J. 2020;26(4):477–86. doi: 10.26719/2020.26.4.477. [DOI] [PubMed] [Google Scholar]
- 45.Ismail H et al. Compliance of Healthcare Worker’s toward Tuberculosis Preventive Measures in Workplace: A Systematic Literature Review. Int J Environ Res Public Health, 2021;18(20). [DOI] [PMC free article] [PubMed]
- 46.Bresenham D, Kipp AM, Medina-Marino A. Quantification and correlates of tuberculosis stigma along the tuberculosis testing and treatment cascades in South Africa: a cross-sectional study. Infect Dis Poverty. 2020;9(1):145. doi: 10.1186/s40249-020-00762-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Martinson NA, et al. Household Contact tracing with intensified tuberculosis and human immunodeficiency virus screening in South Africa: a cluster-randomized trial. Clin Infect Dis. 2022;75(5):849–56. doi: 10.1093/cid/ciab1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sami Siva ST, Wendy Marijnissen MS. Out of Step 2015 TB Policies in 24 Countries: A survey of diagnostic and treatment practices. 2015.
- 49.Abongo T, Ulo B, Karanja S. Community health volunteers’ contribution to tuberculosis patients notified to National Tuberculosis program through contact investigation in Kenya. BMC Public Health. 2020;20(1):1184. doi: 10.1186/s12889-020-09271-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Caraux-Paz P et al. Tuberculosis in the Elderly. J Clin Med, 2021. 10(24). [DOI] [PMC free article] [PubMed]
- 51.Feachem RG, Jamison DT, Bos ER. Changing patterns of Disease and Mortality in Sub-Saharan Africa. Disease and Mortality in Sub-Saharan Africa; 1993. [PubMed]
- 52.Arthur H. NHS England TECS evidence base review. Find recommendations. 2017.
- 53.Betty Luu ACW. & Susan Collings, Evidence Review of Permanency Practices In partnership with Parenting Research Centre. 2019.
- 54.Wulf G, Lewthwaite R. Optimizing performance through intrinsic motivation and attention for learning: the OPTIMAL theory of motor learning. Psychon Bull Rev. 2016;23(5):1382–414. doi: 10.3758/s13423-015-0999-9. [DOI] [PubMed] [Google Scholar]
- 55.Bauer M, Leavens A, Schwartzman K. A systematic review and meta-analysis of the impact of tuberculosis on health-related quality of life. Qual Life Res. 2013;22(8):2213–35. doi: 10.1007/s11136-012-0329-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sohn H, et al. Determining the value of TB active case-finding: current evidence and methodological considerations. Int J Tuberc Lung Dis. 2021;25(3):171–81. doi: 10.5588/ijtld.20.0565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Getnet F, Hashi A, Mohamud S, Mowlid H, Klinkenberg E. Low contribution of health extension workers in identification of persons with presumptive pulmonary tuberculosis in Ethiopian Somali Region pastoralists. BMC Health Serv Res. 2017;17:1–9. doi: 10.1186/s12913-016-1943-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yassin MA, Datiko DG, Tulloch O, Markos P, Aschalew M, Shargie EB, Dangisso MH, Komatsu R, Sahu S, Blok L, Cuevas LE. Innovative community-based approaches doubled tuberculosis case notification and improve treatment outcome in Southern Ethiopia. PLoS ONE. 2013;27(5):63174. doi: 10.1371/journal.pone.0063174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Chen C, Yang C-G, Gao X, Lu Z-Z, Tang F-X, Cheng J, et al. Community-based active case finding for tuberculosis in rural western China: a cross-sectional study. Int J Tuberc Lung Dis. 2017;21:1134–9. doi: 10.5588/ijtld.17.0123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shargie EB, Mørkve O, Lindtjørn B. Tuberculosis case-finding through a village outreach programme in a rural setting in southern Ethiopia: Community randomized trial. Bull World Health Organ. 2006;84. [DOI] [PMC free article] [PubMed]
- 61.World Health Organization. Global tuberculosis report 2017. Geneva. World Health Organization; 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All important data and results are included in this manuscript.