Abstract
Background:
Global evidence-based recommendations for hypertension management are periodically updated, and ensuring adherence to the guidelines is imperative. Furthermore, the current high prevalence of hypertension effectuates a high health-care cost.
Purpose:
To evaluate the prescribing patterns of antihypertensive drugs and other factors affecting blood pressure (BP) with the objective of assessing the proportion of patients achieving the target BP and to perform a pharmacoeconomic analysis in a South Indian population.
Materials and Methods:
In a cross-sectional study, 650 patients previously diagnosed with hypertension and already on treatment with one or more drugs were included. A prospective interview of patients was done using a prevalidated questionnaire on various factors in BP control. Prescribing patterns and pharmacoeconomic analyses, namely, cost acquisition, cost of illness, and cost-effectiveness analyses were carried out.
Results:
Of 650 subjects, 257 (39.54%) achieved the target BP, while 393 (60.46%) did not. A significant association of age, occupational status, monthly family income, and area of residence in addition to physical activity and diet scores, with achieving target BP was noted. A significantly higher cost of anti-hypertensive drug treatment in achieving target BP (P = 0.02) was observed. Among patients who achieved target BP, 37.35% were on monotherapy and 48.25% on multiple drug therapy compared to 46.31% and 35.62%, respectively, in patients who did not. Average cost-effectiveness ratio were found to be Rs. 20.45 and Rs. 57.27, respectively, for single and multiple drug therapies, with incremental cost-effectiveness of Rs. 194.14 per additional patient treated with multiple free drug combinations.
Conclusion:
This study identified the anti-hypertensive prescribing pattern and provided insight into the various pharmacoeconomic factors that play a significant role in attaining target BP in the treated population.
Keywords: Antihypertensive treatment, hypertension, pharmacoeconomic analysis, prescribing pattern, target blood pressure
INTRODUCTION
Hypertension contributes significantly to the burden of heart disease, stroke, renal failure, and premature death.[1] The prevalence of hypertension in India is 29.8% and epidemiological data states that hypertension is seen in 33% of urban and 25% of rural Indians, respectively.[2]
Antihypertensive pharmacotherapy in addition to lifestyle modifications effectively reduces hypertension-related morbidity and mortality.[3] Over the past decade, a range of clinical guidelines on antihypertensive treatment has been published with contributions from multiple clinical trials and studies.[4,5]
The cost of medications has always been a barrier to effective treatment. Increasing prevalence and the incessantly rising expense of treatment influence the compliance of the patients and also the prescribing patterns. Keeping in view, the present study was conducted to evaluate the prescribing patterns of antihypertensive drugs and to perform a pharmacoeconomic analysis with the objective of evaluating the proportion of patients achieving target BP according to the current guideline.[5]
MATERIALS AND METHODS
This study was conducted in a tertiary care teaching medical college hospital. The duration of the study was about 8 months. After obtaining approval from the institutional ethics committee, 650 patients (325 each from the general medicine and cardiology outpatient department) previously diagnosed with hypertension of stage 1 or 2 as defined by the JNC 8 classification[5] and already on treatment with one or more drugs, were included for the study. Patients hospitalized for complications of hypertension or other comorbidities, patients with known secondary hypertension, patients with hypertension but not on medical therapy, pregnant and pediatric patients <18 years were excluded from the study.
Sample size calculation was done with “Epitools Online calculator” considering a prevalence of 30%, desired precision 0.05, and 95% confidence interval. A prospective interview of the study participants was conducted with a pre-validated questionnaire. Written informed consent was obtained before the interview. Demographic details such as age, gender, body mass index, occupational status, marital status, and area of residence were collected. The BP recorded during the present visit was noted down. Information on comorbid conditions such as chronic kidney disease (CKD), coronary artery disease (CAD), including prior myocardial infarction, diabetes mellitus, cerebrovascular accident (CVA) dyslipidemia, hypothyroidism, and heart failure (HF) were obtained. Socioeconomic status details, including monthly family income[6] and questions on lifestyle such as smoking, alcohol, and salt restriction, were also noted. The short version of the International Physical Activity Questionnaire (IPAQ) consisting of 9 items that provided information on the time spent walking, in vigorous and moderate intensity activity and sedentary activity. Data on physical activity were expressed as metabolic equivalents hour/week (METs-h/week), in which 9 different MET levels scaled from sleep/rest (0.9 METs) to high-intensity physical activities (>6 METs). The total MET time for each subject was calculated by summating the values obtained by multiplying the time spent on each activity level by the MET value of each level.[7] The participants were further divided into low, moderate, and high physical activity groups based on their total MET minutes of physical activity per week.
The food frequency questionnaire is designed to assess the dietary approaches to stop hypertension (DASH) score based on food and nutrients emphasized or minimized in the DASH diet, focusing on eight components: high intake of fruits, vegetables, nuts and legumes, low-fat dairy products, whole grains with low intake of sodium, sweetened beverages, and red/processed meats were used to obtain data on dietary habits.[8] Possible frequency-of-consumption responses, ranging from “never or less than once per month” to “6 or more times/day” were given for each food item. Quintile score was assigned according to their intake ranking and food component. Quintile 1 was assigned 1 point and quintile 5, 5 points for food whose desired intake is high and vice-versa for low intake foods for which the lowest quintile was given a score of 5 points. The component scores obtained were summated to an overall DASH score ranging from 8 to 40.[8] A DASH score <20, 21 to 25, and >25 were arbitrarily chosen to represent participants with low, intermediate, and poor adherence to DASH diet, respectively. Awareness of the need for diet modification, and motivation to lose weight were also recorded.
Drug therapy details with regard to brand name, generic name, dose, formulation, frequency, and duration, and other drugs taken for other concurrent clinical conditions were also noted.
Statistical analysis
Based on the JNC 8 guideline,[5] the participants were categorized into those who achieved and had not achieved target BP with the currently prescribed antihypertensive therapy. The patient characteristics, including demography, diet, physical activity, lifestyle modifications, duration of disease, and therapy, were compared, in addition to prescribed medications between those achieving and not achieving target BP. Data were analyzed using R software version 4.1.2. Descriptive statistics were used for categorical variables and presented in the form of frequency tables, comparing patients who achieved their BP goals with those who did not. Differences between these groups were tested using Chi-square test for categorical variables. Continuous variables were given as mean ± standard deviation (SD) and Mann–Whitney U test was used to compare the mean differences of different variables overachieving target BP. Chi-square test was used to check the dependency between categorical variables. A logistic regression analysis was used to identify the adjusted odds ratio of factors associated with BP control. P ≤ 0.05 indicated statistical significance.
RESULTS
Among the 650 study participants, 257 (39.54%) achieved target BP while 393 (60.46%) did not. A significant association between patient’s age, occupational status of the head of the family, monthly family income in addition to area of residence with achieving target BP was observed. There was no significant association between the gender, marital status, or educational status of the head of the family, with achieving target BP. Furthermore, occupation (P = 0.4357) and nature of employment (P = 0.1736) of the participants did not differ significantly between those with controlled and uncontrolled hypertension [Table 1].
Table 1.
Comparison of demographic and socioeconomic variables with achieving the target blood pressure
| Variables | Sub category | Achieved, n (%) | Not achieved, n (%) | Total, n (%) | P |
|---|---|---|---|---|---|
| Age (years) | <40 | 3 (1.17) | 25 (6.36) | 28 (4.31) | 0.03899* |
| 40-49 | 28 (10.89) | 44 (11.2) | 72 (11.08) | ||
| 50-59 | 67 (26.07) | 102 (25.95) | 169 (26) | ||
| 60-69 | 92 (35.8) | 116 (29.52) | 208 (32) | ||
| 70-79 | 52 (20.23) | 82 (20.87) | 134 (20.62) | ||
| >80 | 15 (5.84) | 24 (6.11) | 39 (6) | ||
| Gender | Male | 153 (59.53) | 210 (53.44) | 363 (55.85) | 0.1258 |
| Female | 104 (40.47) | 183 (46.56) | 287 (44.15) | ||
| Educational status (of head of family) | Profession/honours | 10 (3.89) | 22 (5.6) | 32 (4.92) | 0.2676 |
| Graduate/postgraduate | 33 (12.84) | 69 (17.56) | 102 (15.69) | ||
| Intermediate/diploma | 55 (21.4) | 84 (21.37) | 139 (21.38) | ||
| High school | 65 (25.29) | 107 (27.23) | 172 (26.46) | ||
| Middle school | 40 (15.56) | 52 (13.23) | 92 (14.15) | ||
| Primary school | 25 (9.73) | 31 (7.89) | 56 (8.62) | ||
| Illiterate | 29 (11.28) | 28 (7.12) | 57 (8.77) | ||
| Occupational status (of head of family/earning member) | Professional | 18 (7) | 57 (14.5) | 75 (11.54) | 0.0225* |
| Semi professional | 24 (9.34) | 28 (7.12) | 52 (8) | ||
| Clerical/shop-owner/farmer | 66 (25.68) | 124 (31.55) | 190 (29.23) | ||
| Skilled | 47 (18.29) | 48 (12.21) | 95 (14.62) | ||
| Semi-skilled | 17 (6.61) | 22 (5.6) | 39 (6) | ||
| Unskilled | 27 (10.51) | 31 (7.89) | 58 (8.92) | ||
| Unemployed | 29 (11.28) | 46 (11.7) | 75 (11.54) | ||
| Retired | 29 (11.28) | 37 (9.41) | 66 (10.15) | ||
| Monthly family income | Up to Rs. 2099 | 3 (1.17) | 4 (1.02) | 7 (1.08) | 0.0245$,* |
| 2100-6200 | 6 (2.33) | 11 (2.8) | 17 (2.62) | ||
| 6201-10,300 | 32 (12.45) | 42 (10.69) | 74 (11.38) | ||
| 10,301-15,500 | 66 (25.68) | 64 (16.28) | 130 (20) | ||
| 15,501-20,700 | 71 (27.63) | 101 (25.7) | 172 (26.46) | ||
| 20,701-41,000 | 66 (25.68) | 143 (36.39) | 209 (32.15) | ||
| Above 41,100 | 13 (5.06) | 28 (7.12) | 41 (6.31) | ||
| Marital status | Married | 239 (93) | 354 (90.08) | 593 (91.23) | 0.3628$ |
| Unmarried | 2 (0.78) | 7 (1.78) | 9 (1.38) | ||
| Widower | 16 (6.23) | 32 (8.14) | 48 (7.38) | ||
| Occupation of patient | Government/public sector employee | 16 (6.23) | 18 (4.58) | 34 (5.23) | 0.4357 |
| Private sector employee | 34 (13.23) | 65 (16.54) | 99 (15.23) | ||
| Self-employed | 67 (26.07) | 86 (21.88) | 153 (23.54) | ||
| Unemployed/housewife | 110 (42.8) | 183 (46.56) | 293 (45.08) | ||
| Retired | 30 (11.67) | 41 (10.43) | 71 (10.92) | ||
| Nature of employment of the patient (n=291) | Professional | 6 (5.13) | 29 (16.67) | 35 (12.03) | 0.1736 |
| Semi-professional | 7 (5.98) | 12 (6.9) | 19 (6.53) | ||
| Clerical/shop-owner/farmer | 5 (4.27) | 9 (5.17) | 14 (4.81) | ||
| Business | 24 (20.51) | 25 (14.37) | 49 (16.84) | ||
| Farmer | 27 (23.08) | 38 (21.84) | 65 (22.34) | ||
| Skilled | 27 (23.08) | 35 (20.11) | 62 (21.31) | ||
| Semi-skilled | 10 (8.55) | 13 (7.47) | 23 (7.9) | ||
| Unskilled | 11 (9.4) | 13 (7.47) | 24 (8.25) | ||
| Area of residence | Rural | 88 (34.24) | 94 (23.92) | 182 (28) | 0.0079* |
| Semi urban | 76 (29.57) | 117 (29.77) | 193 (29.69) | ||
| Urban | 93 (36.19) | 182 (46.31) | 275 (42.31) | ||
| BMI (n=534) | Underweight | 8 (3.67) | 10 (3.16) | 18 (3.37) | 0.2514 |
| Normal | 98 (44.95) | 170 (53.8) | 268 (50.19) | ||
| Overweight | 83 (38.07) | 99 (31.33) | 182 (34.08) | ||
| Obese | 29 (13.3) | 37 (11.71) | 66 (12.36) |
*Statistically significant, $Chi-square test with Monte Carlo simulation, Total number of subjects is 650 unless and otherwise mentioned. BMI=Body mass index
A small fraction of study subjects (1.38%) had low IPAQ scores, out of which those who did not achieve target BP were marginally higher. A significant difference between the distribution of physical activity scores over achievement of target BP (excluding subjects with low physical activity) was noted. The mean MET time ± SD was significantly higher in those who achieved target BP [Table 2].
Table 2.
Comparison of international physical activity questionnaire scores and dietary approaches to stop hypertension scores in patients with controlled and uncontrolled hypertension
| Variable | Achieved | Not achieved | Total | P |
|---|---|---|---|---|
| Moderate IPAQ score, n (%) | 70 (27.24) | 143 (36.39) | 213 (32.77) | 0.0158* |
| High IPAQ score, n (%) | 183 (71.21) | 245 (62.34) | 428 (65.85) | |
| Mean±SD, median (minimum-maximum) | 7241.6±5165.93, 6300 (810-31410) | 6243.66±4892.64, 5167.5 (693-26640) | 6637.54±5022.07, 5640 (693-31410) | 0.0057* |
| Low DASH score, n (%) | 92 (32.80) | 188 (47.84) | 280 (43.08) | 0.0015* |
| Intermediate DASH score, n (%) | 131 (50.97) | 178 (45.29) | 309 (47.54) | |
| High DASH score, n (%) | 34 (13.23) | 27 (6.87) | 61 (9.38) | |
| Mean±SD, median (minimum-maximum) | 21.38±3.64, 21 (9-30) | 20.65±3.55, 21 (10-31) | 20.94±3.6, 21 (9-31) | 0.0042* |
*Statistically significant. IPAQ=International physical activity questionnaire, SD=Standard deviation, DASH=Dietary approaches to stop hypertension
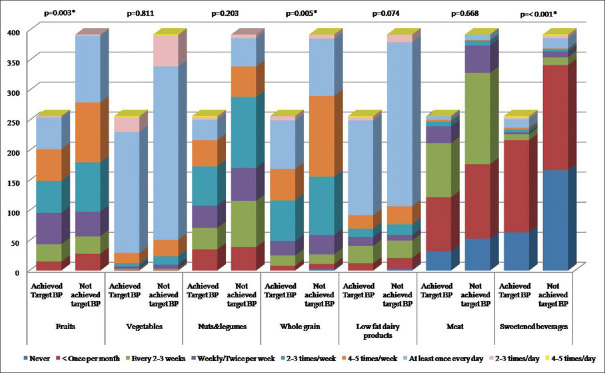
A significant difference in the distribution of consumption of fruit, whole grains, and sweetened beverages over achievement of target BP among the study participants was found [Figure 1]. A significant difference in the mean DASH score as well as the distribution of scores between controlled and uncontrolled hypertensive patients was observed [Table 2].
Figure 1.
Comparison of food frequency with achieving the target BP. BP = Blood pressure
While comparing the salt consumption in quintiles 1 to 5 (Q1 to Q5) and dietary modification with achieving the target BP, a significant association of salt consumption-related variables with achieving target BP was noted using Chi-square test (P = 0.003) [Figure 2].
Figure 2.
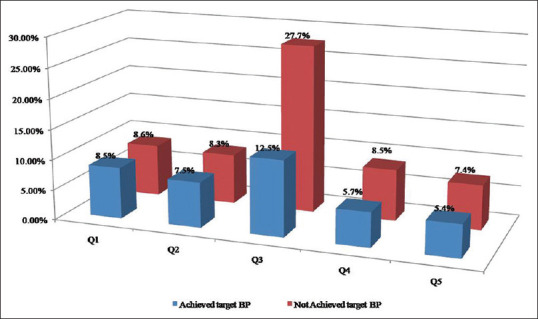
Comparison of salt consumption between the proportion of patients achieving and not achieving target BP. BP = Blood pressure
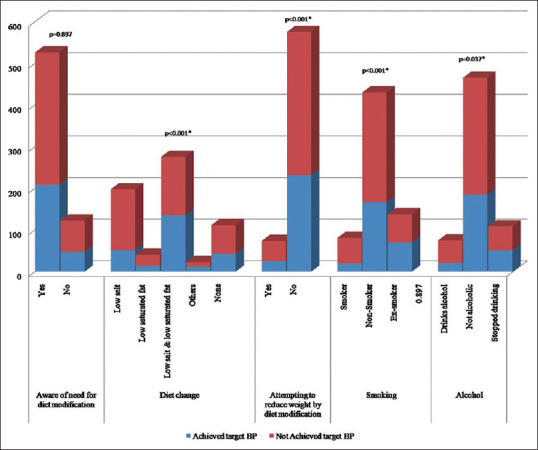
In addition, there were a significantly higher proportion of the study participants with changes in diet pattern like reduction in salt, saturated fat, or both among those who achieved target BP. A similar result was noted for practices such as attempting weight loss, alcohol intake, and smoking [Figure 3].
Figure 3.
Comparison of dietary modification and habits between subjects with controlled and uncontrolled hypertensive patients
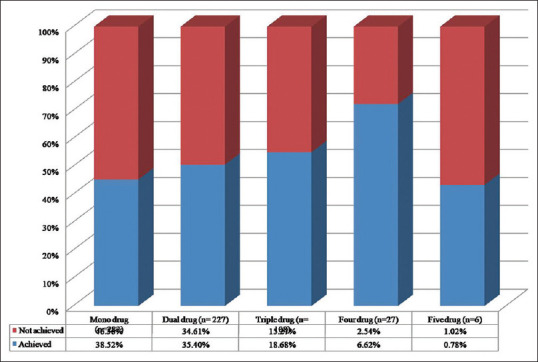
There was no significant difference in the proportion of patients with and without comorbidities between the controlled (n = 222) and uncontrolled (n = 322) hypertensive patients (P = 0.133). A total of 43.38% of patients were on monotherapy followed by 34.92%, 16.61%, and 4.15% receiving two-drug, three-drug, and four-drug combinations, respectively. Compared to monotherapy, the proportion of controlled hypertensives was higher in the multidrug groups. Furthermore, there was a minute fraction (0.9%) treated with five drugs and represented the population with resistant hypertension with a large majority in that group falling in the uncontrolled category. No considerable variation in the median duration of therapy in years was noticed between those with controlled 4 (0.08–30) and uncontrolled hypertension 5 (0.08–40).
Analyzing the prescription pattern revealed that the calcium channel blockers (CCB) were the most commonly prescribed antihypertensives (42%) for monotherapy (n=282). In dual drug therapy (n=227), the combination of an angiotensin-converting enzyme inhibitor (ACEI) with beta-blocker ranked the highest with 21%. Another significantly common antihypertensive combination prescribed was angiotensin receptor blocker (ARB) with CCB (11%). A diminutive fraction of 4% was on combinations including second-line drugs such as alpha-blockers, vasodilators, or loop diuretics [Others in Figure 4]. It was found that among patients on three-drug combinations (n = 108), one was either ACEI or ARB, and the second being a beta-blocker. Triple drug combinations including second-line drugs were 18% [Figure 4].
Figure 4.
Prescription pattern of anti-hypertensive therapy in South Indian population
The mean cost of antihypertensive drugs per day in Indian Rupees was significantly higher (P = 0.022) in the controlled group (12.46 ± 9.58) compared to patients who did not achieve the target BP (10.95 ± 8.73) using Mann–Whitney U test though the cost of illness per visit which included both the direct cost and indirect cost did not vary significantly (P = 0.212) between the two groups.
A significant difference was found in the distribution of single drug/multiple free drug/fixed-dose combinations that the patients were prescribed for control of hypertension between the controlled and uncontrolled groups (P = 0.0059). Hence, a cost-effectiveness analysis was done to analyze the average cost-effectiveness ratio (ACER) and incremental cost-effectiveness (ICER) in the use of multiple free drug combinations over single-drug therapy in achieving the target BP. Among the controlled group, we detected that the ACER calculated by the ratio of cost of antihypertensives to the number of patients for each category receiving drug/multiple free drug/fixed-dose combinations was 20.45, 57.27, and 119.20, respectively. The incremental cost-effectiveness in achieving target BP using multidrug therapy was Rs. 194.14 per additional patient achieving target BP compared to single-drug therapy with the exception of fixed-dose combination [Table 3].
Table 3.
Pharmacoeconomic analysis comparing patients with controlled and uncontrolled hypertension in achieving target blood pressure
| Pharmacoeconomic analysis | |||||
|---|---|---|---|---|---|
|
| |||||
| Variables | Frequency distribution | Achieved (Rs.) | Not achieved (Rs.) | Total (Rs.) | P |
| Cost acquisition analysis: Cost of antihypertensive therapy | Mean cost per day±SD | 12.46±9.58 | 10.95±8.73 | 11.55±9.1 | 0.0224* |
| Median cost per day | 10.31 | 8.89 | 9.45 | ||
| Cost of illness: Direct and indirect cost | Mean cost per visit±SD | 1417.56±769.78 | 1340.15±715.26 | 1370.76±737.68 | 0.2127 |
| Median cost per day | 1350 | 1300 | 1350 | ||
|
| |||||
| Cost-effectiveness analysis | Frequency distribution | Achieved (Rs.) | Not achieved (Rs.) | ACER of achieved (Rs.) | ICER of multiple over single (Rs.) |
|
| |||||
| Single (n=278) | Mean annual cost in rupees (number of patients) | 1963.47 (96) | 1981.19 (182) | 20.45 | 194.14 |
| Multiple (n=264) | 7399.42 (124) | 8018.19 (140) | 57.27 | ||
| Fixed (n=108) | 4410.38 (37) | 5223.82 (71) | 119.20 | ||
*Statistically significant. SD=Standard deviation, ACER=Average cost-effectiveness ratio, ICER=Incremental cost-effectiveness
The mean cost of antihypertensives in Rupees was significantly higher (P = 0.022) in the controlled group though there was no such difference for the total cost which is the sum of direct cost and indirect cost [Table 3].
Among the single-drug therapy, results indicated that the mean annual cost on the purchase of thiazide diuretic (Rs. 642.40) was the lowest followed by calcium channel blockers (Rs. 1195.75). However, comparing the mean annual cost of multidrug therapy prescribed as individual drugs, the overall cost of regimens including calcium channel blockers (Rs. 9394.60) ranked highest followed by ARBs (Rs. 9152.79) and beta-blockers (Rs. 8248.37). For the fixed-dose combinations, the mean annual cost of those including ACE inhibitor was the greatest (Rs. 7162.11).
Health insurance significantly affected achieving the target BP goal though whether whole or part of the expenses was covered lacked significance [Tables 4 and 5].
Table 4.
Association of insurance related variables with achieving the target blood pressure
| Variables | Sub category | Achieved, n (%) | Not achieved, n (%) | Total, n (%) | P |
|---|---|---|---|---|---|
| Health insurance | Public health insurance scheme | 82 (31.91) | 87 (22.14) | 169 (26) | <0.001* |
| Insurance scheme of you/your family member employer | 37 (14.4) | 34 (8.65) | 71 (10.92) | ||
| Private health insurance scheme you have opted | 11 (4.28) | 37 (9.41) | 48 (7.38) | ||
| Nil | 127 (49.42) | 235 (59.8) | 362 (55.69) | ||
| Is whole or part of medical expenses covered by insurance policy? | Whole | 26 (10.12) | 31 (7.89) | 57 (8.77) | 0.0676 |
| Part | 99 (38.52) | 124 (31.55) | 223 (34.31) | ||
| Not at all | 132 (51.36) | 238 (60.56) | 370 (56.92) |
*Statistical significance
Table 5.
Comparison of mean systolic/diastolic blood pressure between those achieved and not achieved target blood pressure for insurance related variables
| Variable | Achieved (mm Hg) | Not achieved (mm Hg) | P |
|---|---|---|---|
| Public health insurance scheme | 122.65/69.5±13.59/9.05 | 153.25/81.26±16.65/12.19 | <0.001* |
| Insurance scheme of you/your family member employer | 120.14/69.19±14.65/10.03 | 155.71/79.68±14.33/14.77 | 0.0011* |
| Private health insurance scheme you have opted | 121.73/65.91±13.49/12.46 | 148.11/89.14±16.27/7.68 | <0.001* |
| Whole | 119.88/66.96±14.51/10.97 | 150.87/84.32±13.79/10.44 | <0.001* |
| Part | 123.35/69.65±12.24/9.31 | 152.22/83.85±17.83/13.66 | <0.001* |
*Statistically significant. Data expressed as Mean +/- Standard deviation
From stepwise logistic regression, it has been observed that age, diet change, smoking, and DASH score have a significant effect on achieving target BP adjusted to other variables. The odds of achieving target BP was highest for those aged 60–69 years with 8.61 times compared to those <40 years adjusted to other variables. The OR of achieving the target BP was 2.12 (95% confidence interval [CI] 1.35–3.37) among those who changed their diet to low salt and low saturated fat compared to those who changed their diet to low salt diet adjusted for other variables. Although the non-alcoholics did not achieve a significantly higher odds in achieving target BP, the OR of achieving target BP among nonsmokers was 2.08 (95% CI 1.18-3.81) and among ex-smokers 2.41(95% CI 1.25-4.75) compared to smokers adjusted to other variables. Likewise, the odds for achieving target BP was 1.91 (95% CI 1.2–3.08) times higher among those following DASH diet which was significant, whereas in those with moderate and high physical activity, despite a higher odds of 1.44 times compared to those with low IPAQ score, was not statistically significant in the study population [Table 6].
Table 6.
Logistic regression for achieving target blood pressure
| Variables | OR (95% CI) | P |
|---|---|---|
| Age (years) (reference: <40 years) | ||
| 40-49 | 6.63 (1.91-31.63) | 0.0066* |
| 50-59 | 6.43 (1.98-29.4) | 0.0053* |
| 60-69 | 8.61 (2.64-39.53) | 0.0013* |
| 70-79 | 7.36 (2.18-34.43) | 0.0035* |
| >80 | 8.08 (1.99-42.52) | 0.0061* |
| Diet change (reference: Low salt) | ||
| Low salt and low saturated fat | 2.12 (1.35-3.37) | 0.0012* |
| Low saturated fat | 1.2 (0.55-2.55) | 0.6426 |
| Smoking (reference: Smoker) | ||
| Nonsmoker | 2.08 (1.18-3.81) | 0.0142* |
| Ex-smoker | 2.41 (1.25-4.75) | 0.0095* |
| Alcohol (reference: Drinks alcohol) | ||
| Not alcoholic | 1.09 (0.53-2.26) | 0.8222 |
| Others | ||
| IPAQ score (reference: Low) | 1.44 (0.74-2.75) | 0.2638 |
| DASH score (reference: Low) | 1.91 (1.2-3.08) | 0.0067* |
*Statistically significant. OR=Odds ratio, CI=Confidence interval, IPAQ=International physical activity questionnaire, DASH=Dietary approaches to stop hypertension
DISCUSSION
In this study, out of 650 subjects, 39.54% achieved the target BP. This is in agreement with studies conducted in Singapore which recorded 49.7%[9] and in Ethiopia 25.6%.[10] On the other hand, studies conducted in Australia[11] reported higher BP control. This discrepancy in research findings can be attributed to a multitude of factors ranging from ethnicity,[12] socioeconomic status, compliance to treatment, physician inertia, deficiencies of health-care systems in their approach to chronic diseases, lack of drug availability at the health facility, unaffordability of drugs by patients, and less aggressive treatment.[11,12,13]
This study showed a significant association between age, occupational status of family head, monthly family income, and area of residence with achieving target BP. This was in line with the study conducted by Romday et al. which found the most common age group as 50–59 years.[14] This study also replicated the findings of Koh et al.[9] in which no significant association of gender, educational status, occupation of patient with achieving target BP. However, significantly larger proportion of patients with lower BMI had attained target BP goal compared to those with higher BMI in the study; this was not detected in the present study population.[9] This difference probably stems from the fact that the participants included in the study had concomitant dyslipidemia unlike this research.
The association of statistically significant gender differential effects of marital status on hypertension control previously reported[15] was not apparent in this study. The lack of significant difference can be ascribed to the changing gender-specific norms and roles which would otherwise escalate prevalence and vitiate control. It was interesting to note that a significantly larger proportion of professionals were head of the family in those with unattained target BP. Surprisingly, the distribution of body mass index did not demonstrate a statistically significant difference between the study population achieving and not achieving the target BP.
There was a significant difference in the distribution of IPAQ scores between the study participants with controlled and uncontrolled hypertension. In addition, there was a significant difference in the DASH score with significant differences in the distribution of consumption of fruit, whole grains, and sweetened beverages over achieving the target BP. Similarly, Lee et al.[16] observed that both active dietary practices and exercise are needed for effective reduction of BP. It has been reported in literature that, a reduction in dietary sodium decreases the BP,[17] and accordingly, the findings of this study showed a significant association of salt consumption-related variables with achieving target BP. The present study indicated that there is a significant association between adopting weight loss measures, smoking, and alcohol consumption with attaining target BP goal which have been illustrated in prior studies that current cigarette smoking and alcohol consumption were associated with poor hypertension control.[18] Thus, the finding of this research bears testimony to the well-established fact that lifestyle modifications including physical activity, DASH diet combined with a reduction in alcohol and salt, adopting measures for weight loss, and quitting smoking have significant beneficial effects on hypertension control. Time and again, multiple studies have proven that lifestyle interventions can optimize therapeutic benefits in hypertension management by enhancing the effect of antihypertensive drugs, reducing the need for multiple drug regimens, and favorably influencing overall cardiovascular risk.[19]
Participants of this study had comorbidities such as CAD, diabetes mellitus, dyslipidemia, CVA, congestive HF, and CKD which are known to be commonly associated with hypertension. Studies have shown that despite high treatment rates among participants with these conditions, the rates of hypertension control from the treatment were low.[20] In stark contrast, evidence that having a comorbidity was associated with a higher probability of control, possibly due to more frequent interaction with the health-care system and/or appropriate management of those at greater cardiovascular risk is also supported by literature.[21] This is reflected in patients with CAD in the present study population.
The present study showed a significant difference in the proportion of controlled and uncontrolled hypertensives prescribed single drug/multiple free drug/fixed-dose combinations antihypertensives. Calcium channel blockers constituted the single largest prescribed monotherapy (42%) and a nearly equal percentage (41%) when considering the renin-angiotensin-aldosterone axis inhibitors namely ACE and ARB as a single group and in accordance to the JNC 8 guideline, all patients with CKD were on either ACE or ARB. Although beta-blockers are not considered first-line antihypertensives, patients receiving them as monotherapy were those with compelling indications, especially CAD. A small fraction of patients received thiazide as monotherapy though in drug combinations, thiazide diuretic was commonly used. This can be primarily attributed to its potentiating effect on other anti-hypertensives despite being a mild anti-hypertensive on its own. The prescription pattern observed in this study was similar to that by Koh et al.[9] The mean cost of antihypertensive therapy in our study participants was within the range described by Das et al.[22]
Combination therapy in hypertension has distinct advantages with better long-term outcomes beyond hypertension control.[23] The ratio of controlled to uncontrolled hypertensive patients demonstrated an incremental rise with a progressively increasing number of drugs from monotherapy to four-drug combinations, which obviously results from the action at multiple pharmacodynamic targets by the combined use of different antihypertensives. It is comprehensible that the advantage of fixed-dose combinations is better adherence resulting from a lower pill load whereas, in free drug combinations, there is the ease of dose titration.[24] Our analysis also emphasizes the use of drug combinations to improve the proportion of hypertensive patients achieving the target BP. This is in line with the recommendation by JNC 8 that initiation of drug combinations being advocated as a strategy in treatment plan for patients requiring >20 mmHg and 10 mmHg reductions in systolic and diastolic BP, respectively.[5]
A significant association of health insurance with achieving target BP was observed in this study. Similarly in the United States, studies have shown that among patients treated for hypertension, uninsured individuals were at lower odds of adequate BP control.[23] Few other reports state that insurance status did not have a significant association with BP control as the one reported from Tanzania.[25]
The present study revealed several key aspects of antihypertensive drug utilization in addition to improving our understanding on the pharmacoeconomic perspectives in hypertension management which was not clearly established previously.
CONCLUSION
The study has highlighted the importance of lifestyle modification in achieving target BP and identified the antihypertensive prescribing pattern and provided insight into the various pharmacoeconomic factors that play a significant role in attaining target BP in the treated population.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16:223–37. doi: 10.1038/s41581-019-0244-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anchala R, Kannuri NK, Pant H, Khan H, Franco OH, Di Angelantonio E, et al. Hypertension in India: A systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32:1170–7. doi: 10.1097/HJH.0000000000000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Musini VM, Gueyffier F, Puil L, Salzwedel DM, Wright JM. Pharmacotherapy for hypertension in adults aged 18 to 59 years. Cochrane Database Syst Rev. 2017;8(CD008276) doi: 10.1002/14651858.CD008276.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 5.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the eighth joint national committee (JNC 8) JAMA. 2014;311:507–20. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 6.Singh T, Sharma S, Nagesh S. Socio-economic status scales updated for 2017. Int J Res Med Sci. 2017;5:3264–7. [Google Scholar]
- 7.Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire:12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 8.Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168:713–20. doi: 10.1001/archinte.168.7.713. [DOI] [PubMed] [Google Scholar]
- 9.Koh KH, Goh CC, Goh SC, Koh YL, Tan NC. Blood pressure goal attainment in multi-ethnic Asian patients with hypertension and dyslipidaemia in primary care. Singapore Med J. 2020;61:469–75. doi: 10.11622/smedj.2019102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tesfaye F, Byass P, Wall S. Population based prevalence of high blood pressure among adults in Addis Ababa: Uncovering a silent epidemic. BMC Cardiovasc Disord. 2009;9:39. doi: 10.1186/1471-2261-9-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chowdhury EK, Owen A, Krum H, Wing LM, Ryan P, Nelson MR, et al. Barriers to achieving blood pressure treatment targets in elderly hypertensive individuals. J Hum Hypertens. 2013;27:545–51. doi: 10.1038/jhh.2013.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Umscheid CA, Gross R, Weiner MG, Hollenbeak CS, Tang SS, Turner BJ. Racial disparities in hypertension control, but not treatment intensification. Am J Hypertens. 2010;23:54–61. doi: 10.1038/ajh.2009.201. [DOI] [PubMed] [Google Scholar]
- 13.Goverwa TP, Masuka N, Tshimanga M, Gombe NT, Takundwa L, Bangure D, et al. Uncontrolled hypertension among hypertensive patients on treatment in Lupane District, Zimbabwe, BMC Res Notes. 2012;2014;7:703. doi: 10.1186/1756-0500-7-703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Romday R, Gupta AK, Bhambani P. An assessment of antihypertensive drug prescription patterns and adherence to joint national committee-8 hypertension treatment guidelines among hypertensive patients attending a tertiary care teaching hospital. Int J Res Med Sci. 2016;4:5125–33. [Google Scholar]
- 15.Ramezankhani A, Azizi F, Hadaegh F. Associations of marital status with diabetes, hypertension, cardiovascular disease and all-cause mortality: A long term follow-up study. PLoS One. 2019;14:e0215593. doi: 10.1371/journal.pone.0215593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee CJ, Kim JY, Shim E, Hong SH, Lee M, Jeon JY, et al. The effects of diet alone or in combination with exercise in patients with prehypertension and hypertension: A randomized controlled trial. Korean Circ J. 2018;48:637–51. doi: 10.4070/kcj.2017.0349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grillo A, Salvi L, Coruzzi P, Salvi P, Parati G. Sodium intake and hypertension. Nutrients. 2019;11:1970. doi: 10.3390/nu11091970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cherfan M, Vallée A, Kab S, Salameh P, Goldberg M, Zins M, et al. Unhealthy behavior and risk of hypertension: The CONSTANCES population-based cohort. J Hypertens. 2019;37:2180–9. doi: 10.1097/HJH.0000000000002157. [DOI] [PubMed] [Google Scholar]
- 19.Nicoll R, Henein MY. Hypertension and lifestyle modification: How useful are the guidelines? Br J Gen Pract. 2010;60:879–80. doi: 10.3399/bjgp10X544014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong ND, Lopez VA, L’Italien G, Chen R, Kline SE, Franklin SS. Inadequate control of hypertension in US adults with cardiovascular disease comorbidities in 2003-2004. Arch Intern Med. 2007;167:2431–6. doi: 10.1001/archinte.167.22.2431. [DOI] [PubMed] [Google Scholar]
- 21.Tapela N, Collister J, Clifton L, Turnbull I, Rahimi K, Hunter DJ. Prevalence and determinants of hypertension control among almost 100 000 treated adults in the UK. Open Heart. 2021;8:e001461. doi: 10.1136/openhrt-2020-001461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Das H, Moran AE, Pathni AK, Sharma B, Kunwar A, Deo S. Cost-effectiveness of improved hypertension management in India through increased treatment coverage and adherence: A mathematical modeling study. Glob Heart. 2021;16:37. doi: 10.5334/gh.952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Duru OK, Vargas RB, Kermah D, Pan D, Norris KC. Health insurance status and hypertension monitoring and control in the United States. Am J Hypertens. 2007;20:348–53. doi: 10.1016/j.amjhyper.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 24.Guerrero-García C, Rubio-Guerra AF. Combination therapy in the treatment of hypertension. Drugs Context. 2018;7:212531. doi: 10.7573/dic.212531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maginga J, Guerrero M, Koh E, Holm Hansen C, Shedafa R, Kalokola F, et al. Hypertension control and its correlates among adults attending a hypertension clinic in Tanzania. J Clin Hypertens (Greenwich) 2016;18:207–16. doi: 10.1111/jch.12646. [DOI] [PMC free article] [PubMed] [Google Scholar]