Abstract
Rationale
To identify barriers and opportunities for Ph.D., basic and translational scientists to be fully integrated into clinical units.
Objectives
In 2022, an ad hoc committee of the American Thoracic Society developed a project proposal and workshop to identify opportunities and barriers for scientists who do not practice medicine to develop successful careers and achieve tenure-track faculty positions in clinical departments and divisions within academic medical centers (AMCs) in the United States.
Methods
This document focuses on results from a survey of adult and pediatric pulmonary, critical care, and sleep medicine division chiefs as well as a survey of workshop participants, including faculty in departmental and school leadership roles in both basic science and clinical units within U.S. AMCs.
Results
We conclude that full integration of non-clinically practicing basic and translational scientists into the clinical units, in addition to their traditional placements in basic science units, best serves the tripartite mission of AMCs to provide care, perform research, and educate the next generation. Evidence suggests clinical units do employ Ph.D. scientists in large numbers, but these faculty are often hired into non-tenure track positions, which do not provide the salary support, start-up funds, research independence, or space often associated with hiring in basic science units within the same institution. These barriers to success of Ph.D. faculty in clinical units are largely financial.
Conclusions
Our recommendation is for AMCs to consider and explore some of our proposed strategies to accomplish the goal of integrating basic and translational scientists into clinical units in a meaningful way.
Keywords: Ph.D., clinical departments, basic science, translational science, academic medical center
Contents
Overview
Introduction
Methods
- Body
- The Tripartite Mission of AMCs
- Research Is an Expensive Investment, and the Workforce Is Changing
- Basic Scientists, Like Physician- Scientists, Are at Risk
- To Tenure or Not?
- The Case for Hiring Ph.D. and Nonpracticing Clinician Scientists in Clinical Departments
- Barriers to Hiring Ph.D. Scientists in Clinical Departments
Conclusions and Recommendations
Overview
The American Thoracic Society (ATS) Ph.D., Basic and Translational Sciences working group conducted a survey of adult and pediatric pulmonary and sleep medicine division chiefs to inform an ATS project proposal. This project ultimately assembled a group of 25 scientists representing deans, department chairs, division chiefs, and basic and translational scientists in basic science units, clinical units, and industry. The group completed additional surveys, conducted a literature review, and held discussion sessions to research barriers and opportunities for full integration of basic and translational scientists in clinical departments and divisions within academic medical centers (AMCs) within the United States. Our main summary and conclusions are as follows:
-
•
Research is an investment.
-
•
The tripartite mission of AMCs is best accomplished by integration of basic and translational scientists (often Ph.D.s) into clinical divisions and departments.
-
•
Clinical units, being larger than basic science units, employ most Ph.D. scientists in AMCs (∼60%); however, most of these hold non–tenure-track positions, which do not provide institutional support for salary or research needs.
-
•
In contrast, basic science departments house only 38% of Ph.D. faculty within AMCs, yet these positions are generally tenure track, with institutional support for salary and start-up.
-
•
Within the same AMC, opportunities for Ph.D.s in clinical versus basic science units often differ significantly, with Ph.D.s in clinical units often having less stable employment, lack of resources, and lower job satisfaction.
-
•
Basic science units, which offer better opportunities for tenure-track Ph.D. scientists, often have hiring constraints.
-
•
The challenging academic job market has led to the number of life science graduates choosing to pursue postdoctoral fellowships and possible careers in academics to dwindle in recent years, and this represents a threat to the academic research mission of all AMC departments.
-
•
Financial challenges are the biggest barrier to the full integration of Ph.D. scientists into clinical units.
-
•
AMCs should consider providing institutional support for salary, start-up, and the opportunity to be hired on the tenure track to Ph.D.s in both basic and clinical units.
-
•
New algorithms for funding must acknowledge that most National Institutes of Health (NIH)-funded investigators will have only a single research grant at a time; thus, internal salary support for other training and service missions will be needed.
-
•
Suggested models to support Ph.D.s in clinical units are targeted philanthropy, redistribution of clinical margins to support Ph.D.s in both clinical and basic science units, and lobbying for programs that provide central campus resources to enhance the translational research mission within the clinical units of AMCs.
-
•
Professional organizations like ATS can help to raise awareness about these disparities, provide better support for their non–clinically practicing scientists, and advance the research missions critical to AMCs and professional scientific societies.
Introduction
The ATS is home to both clinicians and researchers interested in lung health and disease. Basic scientists made up 19% of attendees to the 2016–2019 ATS international conferences but only 6.2% of ATS members. To understand this gap and the needs of basic scientists in the society, and to develop a more tailored program that serves this group, the Ph.D., Basic and Translational Scientists working group was formed and evolved this project to gain deeper insight into the opportunities and barriers for scientists who do not generate clinical revenue to be fully integrated into the faculty and build successful careers within adult and pediatric pulmonary, critical care, and sleep units in AMCs in the United States. This report details the results of this research and highlights several recommendations to reinvigorate the research missions in AMCs.
Methods
A survey was developed by the working group and sent to all adult and pediatric division chiefs in the ATS membership (>125), and 29 responses were received in July, 2021. Survey results were the basis for an ATS project proposal approved in January, 2022. This project convened a virtual workshop with 25 participants chosen because they represented deans, department chairs, and institute directors, as well as both clinical and nonclinical faculty engaged in laboratory or translational research in many domains in both basic science and clinical departments as well as industry. An organizational meeting was held in January, 2022. Participants disclosed potential conflicts of interest, which were managed according to ATS policies and procedures. Surveys to collect additional data from the 25 participants were distributed in February, 2022. A Dropbox site collected survey data, references, and discussion materials. The Chair and Co-Chair compiled data for two virtual presentations and discussions in June, 2022 with the entire project team. Based on these meetings, the Chair and Co-Chair drafted the manuscript by October, 2022 and sent it to the project team for feedback/editing. The manuscript was submitted in November, 2022. Feedback was received in December, 2022. Revisions were made and sent to the project committee in January, 2023 for approval, and a final document was submitted to the ATS.
Body
The Tripartite Mission of AMCs
Modern-day AMCs have three components: health care, research, and education. Uniting these missions is a strong commitment to service. Benefits of such a model are obvious: AMCs often care for the most complex patients, making them a rich environment for training medical students, residents, and clinical fellows. Wet laboratory–based or computational researchers who seek to understand basic principles of biology, health, and disease can leverage the rich patient-derived materials, data, and resources to inform their work, which can speed new discoveries back to the bedside. In addition, basic scientists provide foundational training and teaching on how to address problems from a mechanistic perspective. Fundamental research on basic biology processes can lead to new insights with clinical importance, and physicians integrate this knowledge into clinical care. Such a fruitful and interactive environment that spans basic biology to first-in-human treatment trials is the perfect home for educating the next generation of scholars, researchers, and practitioners. Hence, AMCs are touted as centers of excellence and often have vibrant educational programs for medical students, graduate students, medical residents, clinical fellows, and postdoctoral scholars. Many also provide programs for nursing, dental, or public health professions; masters students; and even undergraduate education.
However, for all the upsides to AMCs, there are notable drawbacks, most of which can be summed up as financial. To run a world-class operation in the hospital, laboratory, and classroom is expensive. Main sources of AMC revenue involve clinical billing, external grants, tuition, philanthropy, and, in some cases, state government. Fundamentally, faculty and staff in AMCs often realize and accept their compensation may be diminished to create a clinical operating margin to support the education and research missions. However, as market forces have changed, the ability to recruit and retain talented clinical and research-oriented faculty and staff, to provide competitive scholarships, to perform community outreach, and to fund the ever-increasing costs of experimental equipment, reagents, and regulatory compliance has outpaced the revenue-generation models. These challenges have strained the tripartite mission of AMCs.
Research Is an Expensive Investment, and the Workforce Is Changing
Most AMCs have both clinical and basic science departments that employ researchers. According to the Blue Ridge Institute for Medical Research (1), NIH funding can roughly be categorized as awarded to 19 clinical department and 8 basic science department types. Table 1 shows the total NIH awards to the top 10 medical school departments in 2021. Of these, four are basic science departments (microbiology/immunology/virology, genetics, biochemistry, and pharmacology). The rest are clinical departments, with internal medicine being the largest recipient, consistent with the fact that internal medicine departments house many divisions and often hold the most faculty and researchers.
Table 1.
Total National Institutes of Health awards to all medical school departments of a given discipline in 2021
| Rank | Department | Award |
|---|---|---|
| 1 | Internal medicine/medicine | $5,328,464,759 |
| 2 | Pediatrics | $1,190,967,486 |
| 3 | Psychiatry | $1,072,161,069 |
| 4 | Neurology | $1,006,414,709 |
| 5 | Microbiology/immunology/virology | $815,503,798 |
| 6 | Pathology | $746,946,955 |
| 7 | Genetics | $696,819,686 |
| 8 | Biochemistry | $675,154,505 |
| 9 | Pharmacology | $602,975,557 |
| 10 | Radiation-diagnostic/oncology | $576,440,388 |
Data from Reference 1.
Research is an investment that takes significant resources. Although AMCs tout research as a key pillar of their missions and national rankings, the ability to fund research has dwindled. One reason is more of the clinical margin is needed to fund clinical operations at the level of the AMCs themselves. In terms of external funding, federal grants are the major source of funding for research equipment, personnel, and supplies. As discussed elsewhere (2), the NIH budget grew from 1950 to 2000, but since the early 2000s it has been stagnant and, when adjusted for inflation, even declining. Within the National Heart, Lung, and Blood Institute, which funds the majority of pulmonary and sleep-related research, there has been a well-documented loss of funding to midcareer scientists, leading to a real loss of 155 multiyear grants awarded in these fields between 2009 and 2014 (2). Competition for NIH grants continues to intensify, putting new pressure on AMCs that in the past may have projected margins based on research-oriented faculty holding an average of two NIH awards. However, such assumptions are likely false. In 2009, only 27% of principal investigators (PIs) held more than one NIH grant (3), and in 2021, 67% of funded PIs held a single research project grant (4). Diminished federal funding success leads to loss of protected time for research, resulting in many physician-scientists being squeezed to do more clinical work. This has reduced the time physicians or medical trainees can engage in research, thus setting up a vicious cycle that has endangered the future of physician-scientists working in clinical departments (5) and has changed opportunities for non–clinically practicing scientists as well.
The stagnant NIH budget also affects basic science departments. Although basic science departments may obtain small amounts of revenue from tuition if they offer courses to medical, graduate, or undergraduate students, these dollars are generally limited and rarely create a surplus margin to fund research. Moreover, options to generate tuition revenue beyond medical students rarely exist in clinical departments. That is not to say clinical departments do not have teaching needs. Clinical units often provide didactic and literature-based instruction to their members, but these teaching efforts are seldom compensated in the way that traditional tuition models are in basic science units. As such, basic scientists in clinical departments may be perceived as financial risks if they cannot cover their salary entirely from grants, even if they do participate in the clinical unit teaching missions. For clinical departments, clinical care can generate revenue. This had led to a growing trend in AMCs of hiring clinical faculty on nontenure tracks, most of which do not participate in laboratory-based research, to expand the clinical operations, missions, and margin. However, a physician primarily involved in clinical care is ripe for recruitment to private practice, where salaries can easily be two to three times or more than a typical AMC salary for similar workloads and hours. As these market forces have forced AMC margins to accommodate larger clinical salaries for clinical practitioners and retentions, the research mission has been negatively affected.
In thinking about the tripartite mission, one might anticipate housing basic and translational science researchers in clinical departments and divisions of AMCs might be mission-forward, yet financial pressures noted above have had the opposite effect. Largely, they have decreased opportunities for Ph.D. and nonpracticing clinicians and scientists in clinical departments. For example, to limit financial risk, clinical departments often hire Ph.D. scientists into nontenure tracks without salary, space, research freedom, or institutional start-up funds to adequately support the fundamental research mission.
Basic Scientists, Like Physician-Scientists, Are at Risk
According to the National Center for Science and Engineering Statistics, National Science Foundation Survey of Earned Doctorates (6), U.S. colleges and universities awarded 55,283 doctorates in 2020. Looking at fields of study, 8,418 were in biological and biomedical sciences and 2,671 were in health sciences. Surprisingly, 55.8% of doctoral recipients in life sciences combined were female, suggesting the pipeline is strong for gender diversity in AMCs. However, of doctorates awarded to U.S. citizens and permanent residents, <15% went to American Indian, Alaska Native, Black, African American, or Hispanic/Latinx persons, indicating the need for continued outreach to those underrepresented in science.
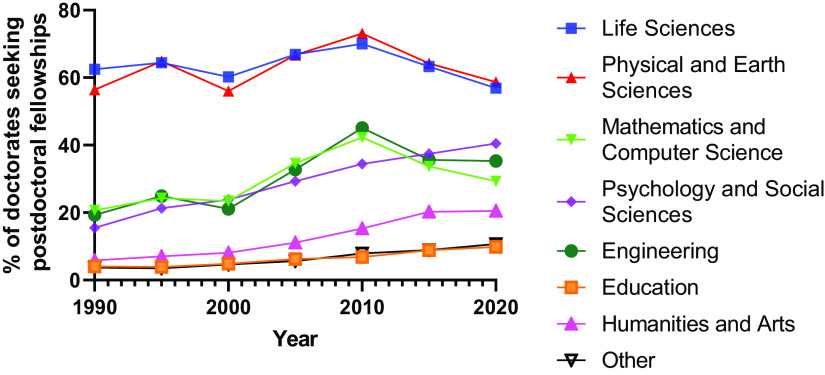
Regarding where life science doctoral recipients go after earning a degree, the same dataset (6) showed that among 11,714 doctoral recipients who responded, only 66.6% had firm plans for post-graduate commitments. This was down from 74.6% in 1990 and 72.4% in 2000 and similar to the 65.9% in 2010. Of 7,784 graduates who provided information, 56.9% had plans for postdoctoral fellowships and 43.1% had plans for employment. Shockingly, this was the lowest percentage of doctoral graduates in life sciences seeking a postdoctoral fellowship in surveys administered since 1990, a trend mirrored in physical and earth sciences and more recently in mathematics and computer sciences. Importantly, the number of people seeking postdoctoral fellowships in every other field except life sciences has risen or remained stable since 1990 (Figure 1). These data strongly suggest doctoral talent in life sciences is being driven away from academic careers.
Figure 1.
Percentage of life science doctorates with commitments to pursue postdoctoral fellowships has declined since 2010 and is currently below levels from 1990. This suggests a major threat to the pipeline of basic scientists who will be available to staff academic medical centers. (Data from Reference 6.)
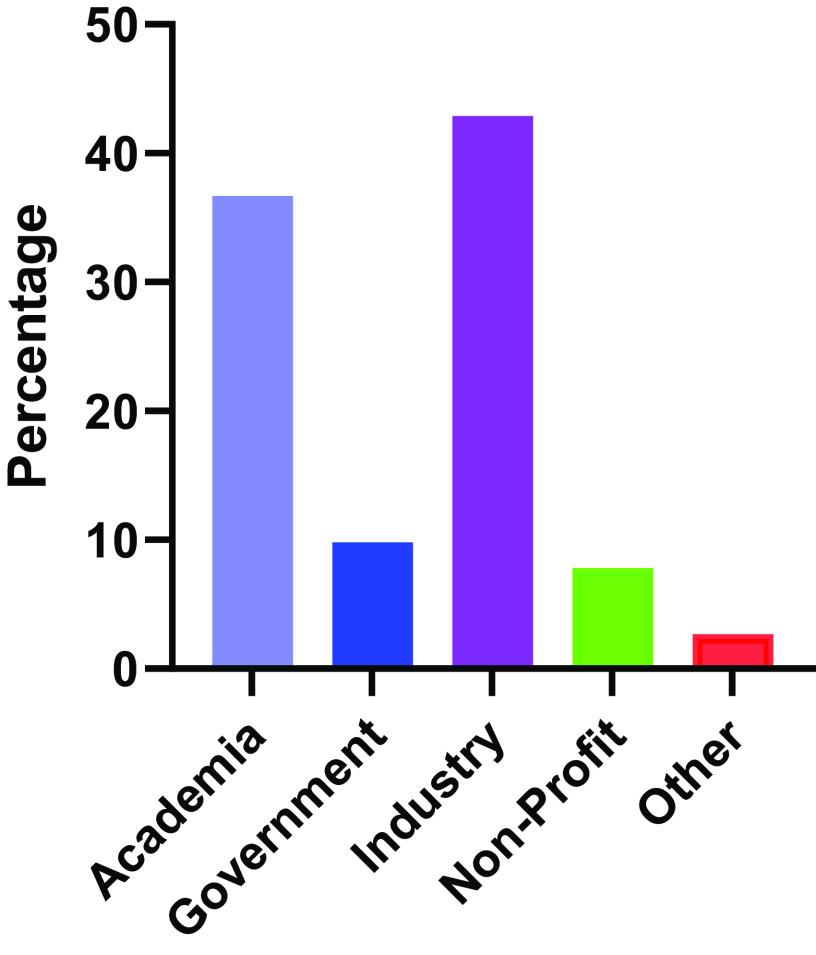
Analysis of 2,969 life science graduates with commitments for employment show only 36.7% had commitments for employment in an academic setting, whereas 42.9%, 9.8%, 7.8%, and 2.7% held commitments for employment in industry, government, nonprofit organizations, or elementary and secondary schools, respectively (Figure 2). Note the 36.7% self-reporting plans for employment in academia was the lowest reported in the past 30 years (e.g., 48.5% in 1990, 46.0 in 2000, and 48.9% in 2020). Thus, there is a shrinking pool of investigators (both basic scientists and physician-scientists) available to staff AMCs, and efforts are needed to stem this tide.
Figure 2.
Commitments of the Ph.D. graduates in Life Sciences for 2020 with plans for employment. These data represent self-reported plans for post-graduation. (Data from Reference 6.)
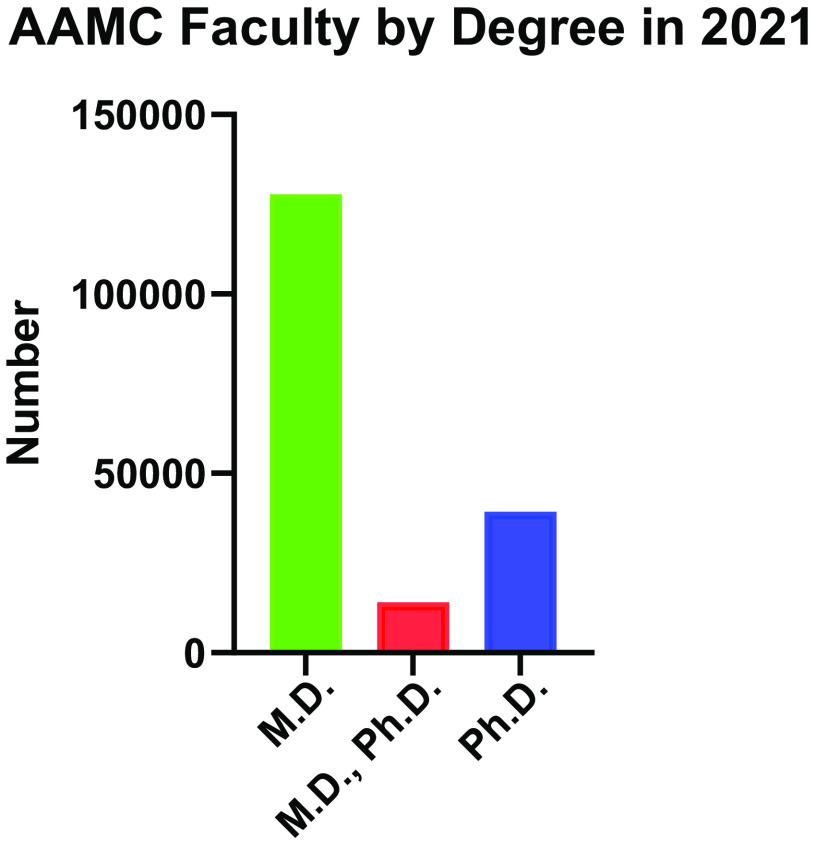
Data from the Association of Academic Medical Centers (AAMC) Faculty Roster 2021 report (7) show the composition of medical school faculty in AMCs by degree and rank. There were 127,862 physicians holding M.D. degrees with a faculty position in an AAMC school. A total of 39,349 faculty held a Ph.D. or other doctoral degree. An additional 14,048 faculty held the dual M.D., Ph.D. or equivalent degree (Figure 3).
Figure 3.
Numbers of Association of Academic Medical Centers faculty rosters in 2021 based on degree. (Data from Reference 7.)
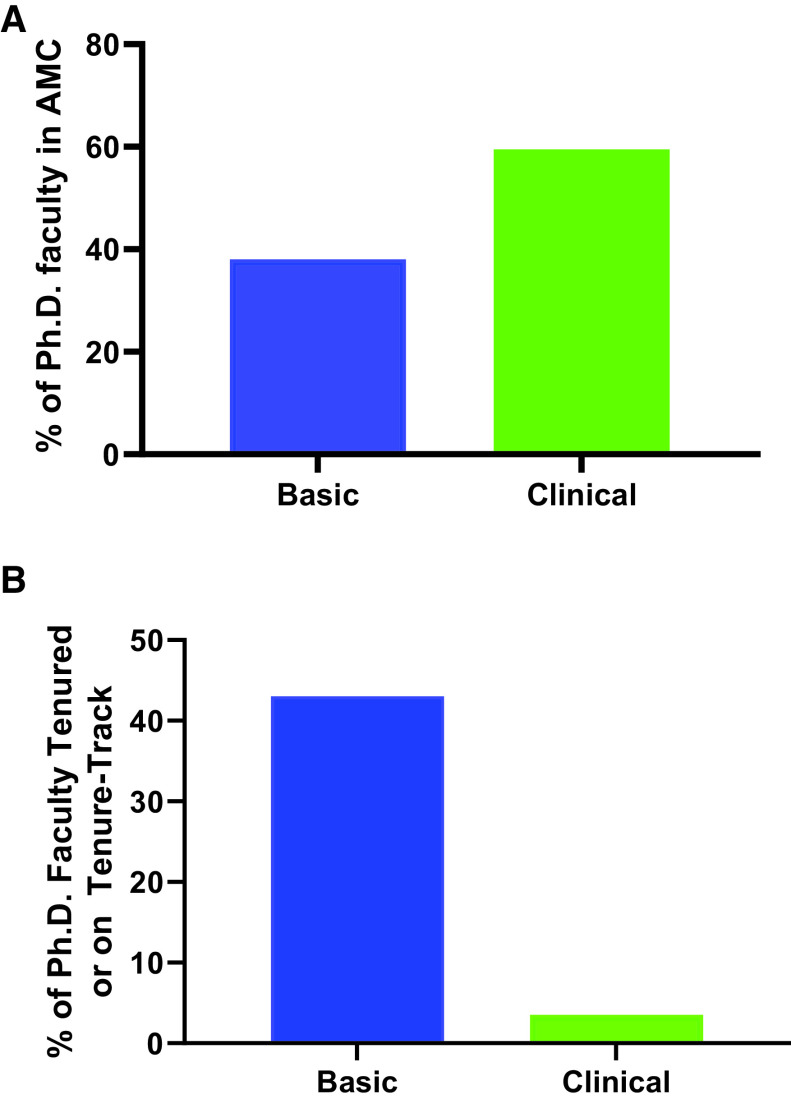
Considering degree by department types, AAMC reported on 191,512 faculty in AMCs (7). Focusing on basic science and clinical departments, of the 19,730 total faculty in basic science units, 76% hold Ph.D. or other doctoral degrees (15,009), whereas 1,959 (<10%) held M.D. degrees. In clinical departments, 23,428 of 170,116 total faculty (<14%) hold a Ph.D. or other doctoral degree, ∼74% (125,640) hold M.D. degrees, and 12,400 (7.3%) hold M.D., Ph.D. degrees. These data in aggregate highlight several important points. Overall, ∼21% of AAMC institution–affiliated faculty hold Ph.D. or other non–clinically practicing doctoral degrees. Basic science units house approximately 38% of these faculty, and clinical departments house 59.5% of these faculty. Thus, most Ph.D. scientists in AMCs are employed in clinical, not basic science departments (Figure 4A). This fact is often underappreciated because clinical departments are so much larger, but within these larger departments, basic scientists may feel underrepresented. This may lead to a diminished sense of support or belonging in their work community.
Figure 4.
(A) Distribution of Ph.D. faculty within academic medical centers (AMCs) based on unit of appointment. These data show that clinical units house more Ph.D. faculty than do basic science units at AMCs (Data from Reference 7). (B) Percentage of Ph.D. faculty in each type of unit who are tenured or tenure-seeking (extrapolated from data in Reference 7). These data show that despite clinical units housing more Ph.D. faculty, they are rarely hired onto the tenure-seeking track in clinical units.
In terms of tracks, 58% of basic science department faculty were tenured or on tenure-seeking tracks. In stark contrast, in clinical departments, only 24.9% of faculty were tenured or on tenure-seeking tracks. If we assume the ratio of tenure-seeking positions is equivalent to the ratio of Ph.D.s in each department type, that extrapolates to ∼43% of Ph.D. faculty in basic science departments being tenured or tenure seeking, whereas only about 3.5% of Ph.D. faculty in clinical departments have that option (Figure 4B). This is consistent with earlier analyses showing similar trends (8). Why are the fates of Ph.D. or other non–clinically practicing degree holders so different between basic science and clinical departments in the same AMC structure?
To Tenure or Not?
Major factors to explain why tenure-track options for basic science faculty in clinical units are decreasing are financial commitments associated with tenure and diminishing revenue streams available for paying faculty salaries (8, 9). As mentioned, patient care revenues in clinical departments can be used to cover research effort or unfunded salaries as well as institutional overhead to support basic science department shortfalls and educational expenditures. Physician-scientists who bring in grant dollars to protect research effort can make up unfunded effort for themselves through somewhat flexible clinical care duties, which often still generate a surplus. In contrast, Ph.D. faculty members in a clinical department often have no formal teaching revenue and will be expected to cover most of their salary with research grants. Any unfunded salary becomes a departmental commitment funded from clinical or departmental reserves or philanthropy. In addition, given that NIH salaries have a salary cap (currently $203,700 for fiscal year [FY] 2022), a salary above this cap for any faculty would have to be covered by departmental discretionary funds as well. In our survey of Ph.D.s in clinical departments, there was a wide range of salary coverage expectations, ranging from 50% up to 100% of effort expected on external funding. Although tenure was originally meant to protect academic freedom of faculty, in practical terms it has equated to a promise of not being fired regardless of productivity metrics after tenure (8). That could leave departments financially responsible for substantial salary and benefits packages for faculty who may decline in research impact and productivity as they age, resulting in little to no external funding. This is a perceived risk for Ph.D. faculty, who would have few or no other ways to generate salary coupled with the expectation for clinical departments to generate a clinical margin to fund other AMC missions. All of this has led to the decline in the willingness of clinical departments to hire Ph.D. faculty on the tenure track (8–10). Anecdotally, some tenure-track Ph.D. scientists in clinical units in our survey reported their departments had taken steps to reduce salary and lay off staff for those scientists almost immediately during times of funding lapse, leading to a vicious cycle of grant submissions, often without resources needed to improve preliminary data required to secure the funding. The tenure issue has the same implications in basic science departments as well, but in these departments, salaries are generally lower, and there may be teaching duties that can be increased when research productivity wanes. In addition, basic science departments do not have the same pressures to operate with a surplus given their limited revenue potential, but their overall size or number of tenured faculty lines are often constrained for sustainability. Our survey of salary coverage expectations across basic science units generally ranged from 50–70% expected coverage on external funds. In general, this was lower than expectations in clinical units in the same institutions, because it often assumes protected time for teaching.
Although it is easy to see how practices of clinical and basic science departments have diverged over time, these decisions are driven by finances more than mission. This has fostered a growing sense of separate and unequal opportunities for Ph.D. and non–clinically active faculty in the same AMC, depending on the primary departmental home (basic science vs. clinical unit). This can be a source of faculty dissatisfaction and burnout (8, 9) and potentially deepens the cultural divide between physician-scientists and non–clinically active faculty (11). Thus, it is important to revisit mission-driven advantages of having basic and translational scientists in clinical departments.
The Case for Hiring Ph.D. and Nonpracticing Clinician Scientists in Clinical Departments
Perhaps the most compelling argument for basic and translational scientists in clinical departments is synergy. There are often structural and perceived barriers for clinicians to interact with basic scientists. In addition, interests of basic science units may not align well with goals of a clinical division or department (11). For instance, a pulmonary division focused on asthma/allergy might benefit clinically from interacting with immunologists studying immune responses to allergens, cell biologists expert in epithelial biology, or pharmacologists interested in allergic disease–modifying drugs. These areas of focus may be less commonly found in basic science units, which are often disease agnostic. Basic scientists embedded in clinical departments tend to develop more translationally relevant research programs (10) and are more likely to use clinical biorepositories and to play more active roles in mentoring residents and clinical fellows than their basic science counterparts. Daily interactions and interdisciplinary exposure lead to shared understandings of challenges with diagnosis or treatment and a pooled lexicon for discussing human disease and animal models of disease. Our surveys suggested embedded basic scientists in clinical units contribute to mechanistic and translational insights and often improve the chances of landing and administering NIH T32 training grants, which favor multidisciplinary, rich, and diverse interactions.
Our survey noted basic scientists are often leading important service and teaching roles in clinical divisions, such as running research seminars and serving on advisory committees for trainees, and are more likely to run core service laboratories or process clinical samples. Collaborations with basic science laboratories often allow early career clinicians an opportunity to generate key preliminary data for career development awards. Notably, cultural competency and improved communication among physician-scientists, Ph.D., and non–clinically active faculty facilitate successful collaboration, which has been mentioned as a major advantage in a previous report (11). Table 2 identifies advantages to having basic scientists in clinical departments that were uncovered in our survey.
Table 2.
Advantages to having basic and translational scientists in clinical divisions
| Advantages to the Clinical Unit | Advantages to the Ph.D., Basic or Translational Scientist |
|---|---|
|
|
Definition of abbreviations: NIH = National Institutes of Health; USNWR = U.S. News and World Report.
Barriers to Hiring Ph.D. Scientists in Clinical Departments
This section is devoted to potential barriers or disadvantages of hiring basic scientists in clinical divisions. From the perspective of basic scientists, although access to and synergy with clinical colleagues may be advantageous for their work, there are downsides to consider. These include lack of familiarity with career development and promotion metrics or knowledge of strong external evaluators for promotion packages by clinical unit leadership, a sense of isolation if there are few basic scientists in the unit, and potential for administrative staff in clinical units to be less familiar with research grant submission processes. As clinical departments are rarely degree-granting entities, Ph.D. faculty in clinical departments may not have access to graduate students to train in their laboratories. Finding opportunities for leadership may be more challenging for basic scientists in clinical units, necessitating Ph.D. faculty to look to medical school or university-wide opportunities for leadership or within their professional scientific societies. Finally, norms for start-up costs and space allocation may be different between basic science and clinical departments, which may disadvantage Ph.D. faculty in clinical units. Given these cultural and financial differences, clinical departments that want to embed basic scientists may have difficulty attracting the most competitive candidates. It can be dispiriting for clinical departments to repeatedly lose top basic and translational talent to basic science units, where indefinite hard money for salary is a strong lure. Given time and political capital invested in failed recruitments, such disappointments may negatively impact future willingness to recruit tenure-track Ph.D. scientists to clinical departments.
From the perspective of the clinical unit, the most common disadvantage mentioned was the financial need to cover unfunded salary without the ability of the basic scientist to generate clinical care revenue and limitations on research space (Table 3). One key difference between funding for effort allocation between faculty in clinical versus basic science units is the source of funds to cover teaching missions. Although teaching revenue may come from the dean’s office in basic science units, many teaching needs in clinical units are not tuition-based classes and thus are covered out of department funds, which may skew the perception of cost and benefit for Ph.D. teaching effort in clinical units.
Table 3.
Reasons preventing hiring of Ph.D. and nonclinician scientists in clinical units
| Reason | Percentage of Responses | Number of Respondents out of 29 Total |
|---|---|---|
| Fear of covering unfunded salary | 41.38 | 12 |
| Limited funding or space to hire Ph.D. and basic science faculty | 41.38 | 12 |
| Unit is primarily focused on clinical care | 31.03 | 9 |
| Other (clinical needs, lack of start-up funds) | 20.69 | 6 |
| Institutional policy at division or department level | 6.9 | 2 |
| Preference for partnering with basic science units over internal hiring | 3.45 | 1 |
| Unclear benefit to division or department | 0 | 0 |
To alleviate this perceived financial risk, many AMCs have recently instituted a non–tenure-seeking research track. On this track, Ph.D. scientists who are still primarily affiliated with a PI with the resources to pay their salary can enter a faculty track that requires nearly 100% salary coverage using grants, contracts, or philanthropic sources. This track offers a faculty title for Ph.D. scientists who may age out of the usual 5-year postdoctoral fellowship category but may not be ready to leave the laboratory where they conducted their postdoctoral training. The advantages for those research-track faculty can be the opportunity to remain in the PI’s lab long enough to finish critical studies or to have faculty status needed to submit grant applications in hopes of becoming more competitive in the job market elsewhere. Most research-track faculty positions are not long term, given the criteria for promotion often match the tenure-track faculty expectations, yet research-track faculty are rarely given any start-up funds or technical support staff to advance their independent work. As such, they generally do not offer the long-term benefits truly embedded tenure-eligible basic scientists can bring to clinical units. It can also be more challenging for research-track faculty to compete for NIH funding if study sections do not perceive institutional commitment to these faculty. Table 4 identifies disadvantages to the clinical unit and the basic scientist regarding work in a clinical department.
Table 4.
Disadvantages to having basic and translational scientists in clinical divisions
| Disadvantages to the Clinical Unit | Disadvantages to the Ph.D., Basic or Translational Scientist |
|---|---|
|
|
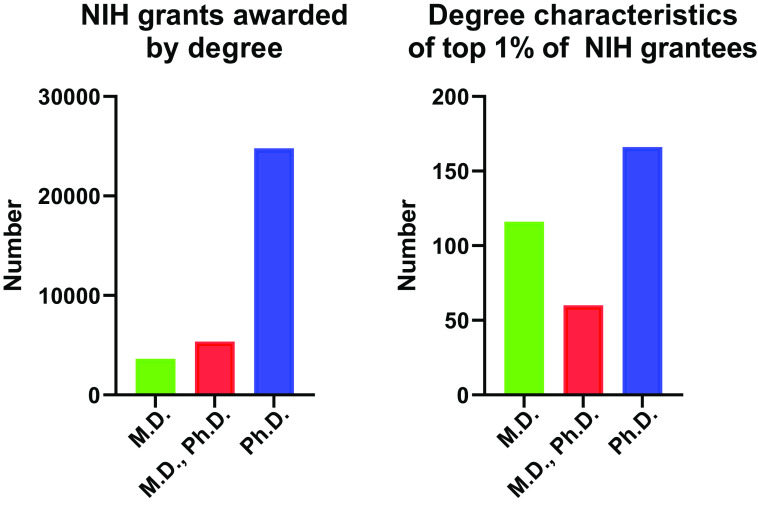
Fear of financial pressures and space resources were the most commonly noted barriers to hiring basic scientists in clinical units (Table 3). Paradoxically, funding fears are partially at odds with the success of funding at the NIH by degree. For a roughly 25-year period (1986–2009), ∼70% of PIs on NIH grants held a Ph.D. degree, whereas about 10% held an M.D., Ph.D. degree. The M.D.-only percentage of PIs was around 20% (12). Recently released analyses by the NIH show in 2020 the number of NIH grants awarded to M.D. degree holders dropped to 15%, whereas the numbers awarded to M.D., Ph.D. degree holders held steady at 10%, and awards to Ph.D. holders rose slightly to 71% (13) (Figure 5, left). Interestingly, if you look at investigator characteristics of the top 1% of NIH-funded investigators, M.D., Ph.D. scientists make up 17.2%, M.D. scientists make up 33.2%, and Ph.D. scientists make up 47.6% (Figure 5, right). Adding the M.D. and M.D., Ph.D. statistics together, there is a slight edge for a clinical degree in the top 1% of funded investigators (50.4% hold an M.D. degree vs. 47.6% who hold a Ph.D. degree alone), but this difference is quickly lost when you consider the bottom 99% of grant holders where >71% are Ph.D.-only degree holders. There is no doubt the top 1% of NIH awardees are an impressive group of researchers, averaging a median of $4.8 million in funding each, with >80% of these investigators holding two or more research grants (13). In contrast, the bottom 99% of investigators averaged $400,000 median funding, with only 32.7% of these investigators holding more than one research grant (13). Thus, these statistics raise an important question: can AMCs reasonably expect any of their faculty in either clinical or basic science units to regularly hold more than one research award from the NIH? The data suggest this is unlikely and make the case for new algorithms for support of the research missions in AMCs. Moreover, data also show <8% of these awards went to faculty underrepresented in sciences, again highlighting the need to increase the diversity of faculty who are applying for these awards in AMCs overall.
Figure 5.
Distribution of National Institutes of Health (NIH) principal investigators by degree type in fiscal year 2020 for all awards (left) and awards to the top 1% of NIH grants by award amount (right).
In FY 2021, the NIH had 35,179 grant awardees out of 92,044 applicant investigators, which was a 2.0% and 2.3% increase over FY 2020, respectively (14). This made for a 38.2% cumulative investigator success rate. Of funded awards, 68,370 were R01 equivalents, 40,532 were R21 equivalents, and 1,191 were P01 grants. Assuming the same distribution by degree type present in 2009, then ∼70% of these awards would be to basic scientists.
Similar data can be found for career development awards/funding. If looking at outcomes of Parker B. Francis fellows (15), 42% of awards have gone to Ph.D. recipients, and 82% of those awardees remained engaged in research after the fellowship. This is compared with 49% of M.D.s who were funded, only 55% of whom remain in research. When looking at later R01 funding, 38% of M.D. awardees went on to obtain an R01, whereas 50% of Ph.D. awardees did so. Thus, if a clinical division wanted to maximize chances of funding success to drive research and training missions, leadership should be aware of these measures and consider hiring at least some faculty who are basic and translational scientists. The NIH data book, updated in 2022, also indicates funding success for basic and translational scientists who have been supported by a Kirschstein–National Research Service Award fellowship is 16.2% for obtaining an NIH grant within 15 years of the degree. This is compared with only 8.3% for trainees from those same fields and institutions that were not funded by National Research Service Award grants (16). Thus, striving to hire the most qualified applicants with a focus on those who have obtained previous career development fellowship support, whether from within or outside the NIH, should further increase chances of successful independent funding when clinical units are considering which basic scientists to hire.
One thing our discussions made clear is that the reasons limiting the hiring of nonpracticing clinicians with Ph.D. or other degrees in clinical divisions are primarily financial in nature and not driven by the tripartite mission of AMCs. Given the synergistic strengths multidisciplinary teams can achieve by working together for research goals, extramural funding, and training missions (e.g., strong research-relevant T32 and fellowship programs), these policies must be reevaluated. Much has been made about the shrinking physician-scientist workforce (5, 10), and one of the main suggested contributors to this trend has been shrinking basic science curriculums in residency and fellowship programs (5). To reverse this trend, clinical divisions and departments should consider enriching the basic science training offered within their clinical divisions and develop appropriate compensation opportunities. Doing so could pay huge dividends to essentially “grow their own” workforce. Data from the University of Michigan shown in Table 5 demonstrate that approximately 70% of new tenure-track hires in clinical departments at the assistant professor level come from internal hires (University of Michigan residency and fellowship programs). Although we do not know if this is generalizable, we anticipate it is, and these figures demonstrate that it is critical to educate our clinical residents and trainees in all aspects of the tripartite mission. Our recommendations below suggest one way to do this by embedding basic scientists in clinical units. As already discussed, there is a trend toward basic scientists moving away from postdoctoral training, and much has been made of the “postdoctoral shortage” now occurring (17, 18). A dedicated approach to hiring basic scientists into attractive positions with sustainable career development opportunities in clinical departments could encourage more scientists to remain in academia.
Table 5.
Tenure-track assistant professor new hire cohorts (all clinical departments)
| 2008–2012 Cohort (n = 148) | 2013–2015 Cohort (n = 73) | 2016–2020 Cohort (n = 116) | 2021–2022 Cohort (n = 38) | Combined (n = 337) | |
|---|---|---|---|---|---|
| External hires | 27% | 37% | 27% | 29% | 29% |
| Internal hires | 73% | 63% | 73% | 71% | 71% |
Data provided by the University of Michigan ADVANCE program.
Conclusions and Recommendations
The results of our surveys and literature review highlight the educational and research value that comes from well-integrated basic science and translational researchers embedded with the physicians and physician-scientists in clinical units. Although financial challenges are also apparent, this working group encourages AMC leadership to explore creative ways to accomplish this goal. An important conceptual framework is to view research as an investment that cannot be expected to be revenue neutral. Therefore, budget models must account for this investment in both clinical and basic science departments. For basic scientists to contribute fully, it is important they have access to start-up packages, salary coverage, and tenure-track opportunities commensurate with basic science units. It is imperative AMCs strive to create algorithms for funding that acknowledge most scientists will only hold one NIH grant at a time and that institutional models funding uncovered salary in basic science units should be extended to translational and basic scientists in clinical units. Table 6 outlines suggestions to achieve this goal. We recommend AMCs establish practices that promote similar norms for Ph.D. faculty in clinical and basic science units. Thus, for Ph.D. faculty hired on the tenure track in clinical units, salary coverage required from grants should not exceed 50%, and adequate office space, laboratory space, and start-up funds should be provided. This practice could level the playing field to allow clinical departments to better compete for top basic science talent and could encourage more discovery science in the translational arena. Just as basic science units assign teaching and service, clinical units could identify relevant teaching and service missions for their Ph.D. faculty as well. Given basic science units are often subsidized by clinical revenue, allocation models could be adjusted to support Ph.D.s in clinical units using this same revenue. Such a reorganization would require careful negotiations among the dean, chief financial officer, and chairs of both basic science and clinical departments, as faculty size and composition would have to be carefully managed across all units to stay within budgetary parameters. Such AMC-wide cooperation could open opportunities for more collaboration across basic and clinical units for teaching and service missions. Another way to increase funding for Ph.D. faculty in clinical units is to consider targeted philanthropy to endow chairs and salary coverage for basic scientists in clinical units and provide start-up packages. Some universities provide central administration support for provost or presidential programs to diversify faculty or support cluster hires around thematic areas. Developing proposals for thematic areas that could enhance basic and translational science recruitments to multiple clinical departments could be advantageous. Overall, investments to promote full integration of basic and translational scientists in clinical departments should reap more creative and collaborative partnerships to advance the AMC tripartite mission.
Table 6.
Recommendations for clinical units to support basic scientists
|
Definition of abbreviations: AMC = academic medical center; EVPMA = executive vice president for medical affairs; NIH = National Institutes of Health; PI = principal investigator.
Acknowledgments
Acknowledgment
The authors thank ATS staff members Miriam Rodriquez for help sending out the Division Chief survey, Kimberly Lawrence for help with conflict of interest forms, and Dr. Kevin C. Wilson, who is the ATS Documents Editor, for helpful advice. Dr. Jeanne Nerbonne (Washington University) also provided data for the surveys.
This official workshop report was the result of an ATS project proposal developed by an ad hoc subcommittee of the Assembly on Respiratory Structure and Function known as the Ph.D., Basic and Translational Sciences working group.
Members of the subcommittee are as follows:
Bethany B. Moore, Ph.D. (Chair)1-3
Melanie Königshoff, M.D., Ph.D. (Co-Chair)4
Megan N. Ballinger, Ph.D.5*‡§
Natalie N. Bauer, Ph.D.6,7*‡§
Timothy S. Blackwell, M.D.8,10,11*‡§
Zea Borok, M.D.12*‡§
G. R. Scott Budinger, M.D.13*‡§
Blanca Camoretti-Mercado, Ph.D., M.B.A.I.S.15*‡§
Serpil C. Erzurum, M.D.16*‡§
Blanca E. Himes, Ph.D.17*‡§
Richard A. Johnston, Ph.D.18*‡§
Venkateshwar G. Keshamouni, Ph.D.2,3*‡§
Hrishikesh S. Kulkarni, M.D., M.S.C.I.19*‡§
Rama K. Mallampalli, M.D.5*‡§
Thomas J. Mariani, Ph.D.20*‡§
Fernando J. Martinez, M.D., M.S.22*‡§
Janet E. McCombs, Ph.D.23*‡§
Dawn C. Newcomb, Ph.D.8,10,11,9*‡§
Michael A. O’Reilly, Ph.D.20,21*‡§
Y. S. Prakash, M.D., Ph.D.24,25*‡§
Karen M. Ridge, Ph.D.13,14*‡§
Patricia J. Sime, M.D.26*‡§
Anne I. Sperling, Ph.D.27*‡§
Shelia Violette, Ph.D.28*‡§
David S. Wilkes, M.D.27*‡§
1Department of Microbiology and Immunology, 2Division of Pulmonary and Critical Care Medicine, 3Department of Internal Medicine, University of Michigan, Ann Arbor, Michigan; 4Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Medicine, University of Pittsburgh, Pittsburgh, Pennsylvania; 5Department of Internal Medicine, Ohio State University, Columbus, Ohio; 6Department of Pharmacology and 7Center for Lung Biology, University of South Alabama, Mobile, Alabama; 8Division of Allergy, Pulmonary and Critical Care Medicine, Department of Medicine, and 9Department of Pathology, Microbiology and Immunology, Vanderbilt University Medical Center, Nashville, Tennessee; 10Department of Veterans Affairs Medical Center, Nashville, Tennessee; 11Department of Cell and Developmental Biology, Vanderbilt University School of Medicine, Nashville, Tennessee; 12Division of Pulmonary, Critical Care and Sleep Medicine, Department of Medicine, University of California San Diego, San Diego, California; 13Division of Pulmonary Medicine and 14Department of Cell and Developmental Biology, Feinberg School of Medicine, Northwestern University, Chicago, Illinois; 15Division of Allergy and Immunology, Department of Internal Medicine, Morsani College of Medicine, University of South Florida, Tampa, Florida; 16The Cleveland Clinic Foundation, Cleveland, Ohio; 17Department of Biostatistics, Epidemiology and Informatics, University of Pennsylvania, Philadelphia, Pennsylvania; 18Section of Pulmonary, Critical Care, and Sleep Medicine, Department of Medicine, School of Medicine, West Virginia University, Morgantown, West Virginia; 19Division of Pulmonary and Critical Care Medicine, Washington University, St. Louis, Missouri; 20Department of Pediatrics and 21Department of Environmental Medicine, University of Rochester Medical Center, Rochester, New York; 22Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Weill Cornell Medicine and New York-Presbyterian Weill Cornell Medical Center, New York, New York; 23Department of Medicine, Center for Translational Research in Infection and Inflammation, Tulane University School of Medicine, New Orleans, Louisiana; 24Department of Physiology and Biomedical Engineering and 25Department of Anesthesiology and Perioperative Medicine, Mayo Clinic, Rochester, Minnesota; 26Division of Pulmonary Disease and Critical Care Medicine, Department of Medicine, Virginia Commonwealth University Richmond, Richmond, Virginia; 27Division of Pulmonary and Critical Care Medicine, Department of Medicine, University of Virginia, Charlottesville, Virginia; and 28Q32 Bio, Waltham, Massachusetts
*Discussant.
‡Provided survey data and literature review.
§Edited and approved the final manuscript draft.
Footnotes
This official Workshop Report of the American Thoracic Society was approved February 2023
Subcommittee Disclosures: B.B.M. served on advisory committee for Galapogos; served as consultant for Boehringer Ingelheim, Pulmonary Fibrosis Foundation, Scleroderma Foundation. M.N.B. received research support from NIH. T.S.B. served on advisory board for Novartis; served as consultant for Boehringer Ingelheim, Janssen, Orinove, Pliant; received research support from Boehringer Ingelheim, Bristol Meyers Squibb, Department of Defense, Department of Veterans Affairs, Morphic, NIH. G.R.S.B. received research support from Department of Veterans Affairs and NIH. S.C.E. served on advisory board for NIH; served as chair of ABIM Pulmonary Disease Board; served in leadership role for Cleveland Clinic; received research support from Cleveland Clinic and NIH. B.E.H. received research support from NIH. R.K.M. served as consultant for Koutif; received royalties from Generian. F.J.M. served as consultant for Abbvie, AstraZeneca, Bayer, Biogen, Boehringer Ingelheim, Bristol Meyers Squibb, Csl Behring, DevPro, GlaxoSmithKline, IQVIA, Novartis, Polarean, ProTerrix Bio, Pulmatrix, Pulmonx, Raziel, Regeneron, Sanofi, Shionogi, Teva, Theravance/Viatris, twoXAR, Veracyte, Verona; served on data safety and monitoring board for Biogen and Medtronic; served as speaker for Academy for Continuing Healthcare Learning, Brooklyn Methodist Hospital, France Foundation, GlaxoSmithKline, Integritas, Integrity Communication, Medscape, NACE/Haymarket, National Association of Managed Care Physicians, Paradigm, PeerView, Physician Education Resource, Projects in Knowledge, United Therapeutics, UpToDate, Vindico, WedMD/MedScape; received research support from Chiesi, DevPro, Gilead, Nitto, Patara/Respivant, ProMedior/Roche, Sanofi/Regeneron. J.E.M. has financial stake in Affinivax. D.C.N served as consultant for University of Indiana; served as speaker for Oklahoma State University; received research support and served as reviewer for NIH; received travel support from ICAN Network and FOCIS. P.J.S. served as consultant for Boehringer Ingelheim, UCB, Three Lakes Partners; served on scientific board for Parker B. Francis; received honorarium from Grand Rounds McGill University, Ground Rounds University of Kentucky, Grand Rounds University of Nebraska, Grand Rounds University of Virginia; received research support from NIH, UCB, PFF, Ford Foundation; received travel support from Boehringer Ingelheim; issued US Patent 10,765,376; patent application 60/567,397; 60/5653,657; 60/513,372; 63/264276; holds stock for Galecto. A.I.S. received research support from NIH. S.V. employee of Q32 Bio; served on advisory committee for Apie, Cytimmune, Kymera, Mediar, Morphic Therapeutics, Scholar Rock; served as consultant for Biogen, Mediar, Morphic Therapeutics, Scholar Rock; holds intellectual property with Biogen and Q32 Bio; holds stock in Apie, Kymera, Mediar, Morphic Therapeutics, Q32 Bio, Scholar Rock. D.S.W. served as consultant for Cartesian Therapeutics and DevPro; served as national director of Harold Amos Medical Faculty Development Program for the Robert Wood Johnson Foundation; holds intellectual property with ImmuneWorks. N.N.B., Z.B., B.C.M., V.G.K., H.S.K., T.J.M., R.A.J., M.A.O., Y.S.P., K.M.R., M.K. reported no commercial or relevant non-commercial interests from ineligible companies.
References
- 1.Roskoski R, Jr, Parslow TG.https://brimr.org/brimr-rankings-of-nih-funding-in-2021/
- 2. Charette MF, Oh YS, Maric-Bilkan C, Scott LL, Wu CC, Eblen M, et al. Shifting demographics among research project grant awardees at the National Heart, Lung, and Blood Institute (NHLBI) PLoS One . 2016;11:e0168511. doi: 10.1371/journal.pone.0168511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rockey S.2011. https://nexus.od.nih.gov/all/2011/05/13/update-on-myth-busting-number-of-grants-per-investigator/
- 4.Lauer M.2022. https://nexus.od.nih.gov/all/2022/09/26/data-on-number-of-research-project-grants-per-principal-investigator/
- 5. Utz PJ, Jain MK, Cheung VG, Kobilka BK, Lefkowitz R, Yamada T, et al. Translating science to medicine: the case for physicianscientists. Sci Transl Med . 2022;14:eabg7852. doi: 10.1126/scitranslmed.abg7852. [DOI] [PubMed] [Google Scholar]
- 6.National Center for Science and Engineering Statistics, National Science Foundation. 2022. https://ncses.nsf.gov/pubs/nsf23300
- 7.Association of American Medical Colleges. 2021. https://www.aamc.org/data-reports/faculty-institutions/interactive-data/2021-us-medical-school-faculty
- 8. Bunton SA, Mallon WT. The continued evolution of faculty appointment and tenure policies at U.S. medical schools. Acad Med . 2007;82:281–289. doi: 10.1097/ACM.0b013e3180307e87. [DOI] [PubMed] [Google Scholar]
- 9. Schweitzer L, Eells TD. The forgotten faculty: challenges for Ph.D.s in clinical medical school departments. J Clin Psychol Med Settings . 2008;15:7–11. doi: 10.1007/s10880-008-9095-x. [DOI] [PubMed] [Google Scholar]
- 10. Fang D, Meyer RE. Ph.D. faculty in clinical departments of U.S. medical schools, 1981-1999: their widening presence and roles in research. Acad Med . 2003;78:167–176. doi: 10.1097/00001888-200302000-00011. [DOI] [PubMed] [Google Scholar]
- 11. Restifo LL, Phelan GR. The cultural divide: exploring communication barriers between scientists and clinicians. Dis Model Mech . 2011;4:423–426. doi: 10.1242/dmm.008177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rockey S.2011. https://nexus.od.nih.gov/all/2011/06/23/who-are-we/
- 13. Lauer MS, Roychowdhury D. Inequalities in the distribution of National Institutes of Health research project grant funding. eLife . 2021;10:e71712. doi: 10.7554/eLife.71712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lauer M.2022. https://nexus.od.nih.gov/all/2022/05/03/how-many-researchers-the-fy-2021-cumulative-investigator-rate/
- 15. Martin TR, Snapp DL, Tomita DM. The Parker B. Francis Fellowship Program: analysis of 31 years of career development support. Am J Respir Crit Care Med . 2012;185:479–485. doi: 10.1164/rccm.201108-1390PP. [DOI] [PubMed] [Google Scholar]
- 16.National Institutes of Health. https://report.nih.gov/nihdatabook/report/274
- 17. Langin K. US labs face severe postdoc shortage. Science . 2022;376:1369–1370. [Google Scholar]
- 18.Woolston C.2022. [DOI]