Abstract
Background
Insulin-treated diabetes patients are at high risk of developing lipohypertrophy, which can negatively impact treatment outcomes. Early detection of lipohypertrophy is crucial to preventing blood glucose fluctuation. Unfortunately, this clinical issue is often overlooked by nurses, causing the development of vascular complications, which leads to an increase in the morbidity and mortality of the type 2 diabetes mellitus population.
Objective
This study was conducted to identify lipohypertrophy prevalence and to establish the association between the presence of lipohypertrophy and its associated risk factors, including years on injection, total injection in a day, total insulin unit per day, often change needle, insulin injection site and move to a different area.
Methods
This cross-sectional study included 128 patients with type 2 diabetes mellitus who received insulin therapy in an outpatient diabetic clinic. Questionnaires on socio-demographic and lipohypertrophy-associated risk factors were distributed among patients, and lipohypertrophy-assessment was done using a checklist. Descriptive statistics and Pearson Chi-square were used for statistical analysis.
Results
The prevalence of lipohypertrophy was 51.6% (95% CI: 42.6, 60.5). Swelling on fatty tissue (46.1%) exhibited the highest percentage of lipohypertrophy features during the assessment. Pearson Chi-Square revealed a significant relationship between the presence of LH and BMI categories (χ2 = 10.059, df = 3, p = 0.018), duration of injection (χ2 = 15.001, df = 3, p = 0.002), frequency of needle replacement (χ2 = 9.525, df = 3, p = 0.023) and rotation of injection site (χ2 = 5.914, df = 1, p = 0.015).
Conclusion
The high prevalence of lipohypertrophy indicates a need for a prevention strategy. Thus, nurses should play an important role in educating patients regarding the proper administration of insulin injections and performing a routine lipohypertrophy assessment and health education on the correct method of insulin injection.
Keywords: lipohypertrophy, insulin, risk factor, type II diabetes mellitus, prevalence, Malaysia, nursing
Background
Type 2 diabetes mellitus is one of the fastest-escalating health issues currently affecting approximately 463 million people globally. The total number of adult patients type 2 diabetes mellitus is predicted to rise to almost 700 million by 2045 (Sun et al., 2022). Out of that 700 million, 15% of the patients-initiated insulin treatment after five years of being diagnosed with type 2 diabetes mellitus (Gentile et al., 2018). Nurses play an important role in providing education and information related to proper insulin injection techniques to reduce the prevalence of LH.
Lipohypertrophy (LH) is a common complication among insulin-treated diabetic patients (Pozzuoli et al., 2018) as a result of the lipogenic action of insulin or injection-related tissue trauma (Barola et al., 2018). LH is a clinical sequela of insulin injection because evidence confirms that patients with LH have a greater risk of glycaemic variability and require higher insulin dosage (Kalra et al., 2016). The side effect of insulin and injection-related tissue trauma is augmented by repeated subcutaneous insulin administration in a skin site resulting in LH, which is characterised by the formation of fatty lumps under the skin site of injection (Barola et al., 2018). This leads to decreased insulin absorption; as a result, the patient will show poor glycaemic control (Buyruk et al., 2019; Famulla et al., 2016). However, the frequency of episodes of unexplained hyperglycemia and severe hypoglycemia requiring assistance was higher in patients with LH (Arora et al., 2021).
The correct injection technique is essential for the success of insulin therapy in people with diabetes (Gorska-Ciebiada et al., 2020). Furthermore, a subcutaneous insulin therapy study showed a significant effect of injection sites linked to pharmacokinetic problems that lead to glycemic fluctuation (Arora et al., 2021). Empirical evidence suggests that proper use of insulin injection techniques is crucial to optimise the efficacy of the therapy (Gorska-Ciebiada et al., 2020; Spollett et al., 2016). The recommendations of proper insulin injection techniques by diabetes associations are based on the multi-national studies’ results of the Injection Technique Questionnaire (ITQ) (Gorska-Ciebiada et al., 2020). Nevertheless, patients’ adherence to proper insulin injection techniques is still lacking despite being educated, reflecting their disregard for healthcare providers’ instructions regarding insulin administration (Benson et al., 2017; Calliari et al., 2018).
Several studies have been conducted on patients with type 2 diabetes mellitus to determine the worldwide prevalence of LH (AlJaber et al., 2020; Buyruk et al., 2019; Deng et al., 2018; Ji et al., 2017; Rahim et al., 2020). It is reported that the pooled prevalence of LH was 38%, out of which type 2 diabetes mellitus and type 1 diabetes mellitus patients constitute 49% and 34%, respectively (Deng et al., 2018). In a study by Arora et al. (2021), out of 500 patients on insulin therapy, 44.6% of them had LH on clinical examination. They further reported that the prevalence of LH was higher in Asian countries than in European countries. National studies in Malaysia from 1996 to 2015 reported that the prevalence of diabetes in 2015 was 17.5%, doubling its figure since 1996. Females, older age groups, Indians, and urban residents had the highest risk of diabetes (Tee & Yap, 2017). A recent study also reported that the approximate figure for diabetes prevalence is 19.6% (Rahim et al., 2020). The rise in numbers substantiated that early initiation of insulin therapy is vital in maintaining the glucose level to prevent diabetic complications. However, insufficient knowledge and poor attitude toward insulin self-administration remain the current challenge among insulin-treated diabetes patients (Gerensea et al., 2015), resulting in complications such as LH (Cunningham & McKenna, 2013).
The association of LH with age, gender, period of therapy, body mass index, glycated haemoglobin, the total daily dose of insulin, insulin form, injection frequency, needle reuse, injection sites, and missed rotation sites has been investigated by several researchers (Barola et al., 2018; Buyruk et al., 2019; Calliari et al., 2018; Gorska-Ciebiada et al., 2020; Pozzuoli et al., 2018). Although these observations have made substantial contributions to the current body of knowledge, further studies are needed for several reasons.
First, when this study was conducted, there was very little information available regarding the features of LH caused by insulin injection; searching online revealed that no Sabah-based studies of this kind had been carried out. Much evidence signify the prevalence of LH among type 2 diabetes mellitus patients; however, data regarding the characteristics of LH was very limited. Best to our knowledge, there are no published studies on the prevalence of LH in type 2 diabetes mellitus patients in North Borneo of Malaysia. Therefore, there is a knowledge gap in identifying LH among insulin-treated diabetes mellitus, particularly in North Borneo Malaysia. Therefore, our study aims to fill the information gap related to LH and identify the characteristics of LH lesions using a structured method of palpation technique. The palpation technique in the identification of LH has been recognised and favoured over the ultrasound method (Abu Ghazaleh et al., 2018) due to its low cost and accuracy (Gentile et al., 2016).
Methods
Study Design
This cross-sectional study was conducted in an outpatient diabetic clinic in North Borneo, Malaysia.
Participants/Samples
This study was conducted within the vicinity of Kota Kinabalu at one of the endocrine and diabetes outpatient clinics of a public hospital in North Borneo, Malaysia. The clinic serves as the primary referral of 19 districts and public health clinics in North Borneo, Malaysia. Convenience sampling was used by inviting all patients with type 2 diabetes mellitus under regular follow-up at endocrine and diabetes outpatient clinics to participate in the study. The patient who attended the clinic during the study period were screened for eligibility. All patients 18 years and above undergoing insulin therapy are included in this study. Patients who had been initiated on insulin therapy for less than two weeks, continuous insulin infusion therapy, pregnant or lactating and on other regular medication that needs to be administered subcutaneously were excluded from this study.
The sample size calculation was calculated using STATA 12.0 program. To calculate the sample size, the power was 80%, and the alpha was pre-set at 0.05. The LH prevalence of 49% was extracted from a previous study by Deng et al. (2018). Based on the calculation, a total of 130 eligible samples were required. Considering the estimated attrition rate of 15%, the final sample size is 160. A total of 160 participants were invited to the study. However, only 130 agreed to participate, resulting in an 81.3% completion rate. Figure 1 shows the flowchart of data collection.
Figure 1.

Flow chart of data collection
Instruments
LH-associated risk factors questionnaire
Self-administered questionnaire of LH-associated risk factors by Cunningham and McKenna (2013) was adopted. Permission to adopt the questionnaire had been requested prior to the research. The questionnaire consists of six LH-associated risk factors, including years on injection, total injection in a day, total insulin unit per day, frequency of changing the needle, insulin injection site, and rotation of injection. In addition, forward-backwards translation was conducted by one language expert from our institution and one diabetes educator residing in the North Borneo region for more than ten years to ensure the translated questionnaire to the targeted language (Bahasa Malaysia) can be understood by the target population of interest. The Cronbach’s alpha coefficient was 0.82, exhibiting good internal consistency; therefore, the self-administered LH-associated risk factors questionnaire was deemed reliable.
LH-assessment checklist development
This study developed an LH-assessment checklist for insulin-treated patients with type 2 DM based on consensus among experts to obtain content validity. The developed LH-assessment checklist was intended to help diabetes nurse educators identify LH occurrence among insulin-treated type 2 DM.
The instrument development process consists of three phases, summarised in Figure 2. In phase one, a team (consisting of one clinician and two diabetes educators) was established to perform a literature search via CINAHL, PubMed, Cochrane Library and Medline databases for relevant articles on the characteristics of insulin-related LH. Then preliminary checklist covering five items was extracted based on the studies by De Coninck et al. (2010), Hajheydari et al. (2011), Cunningham and McKenna (2013), Kadiyala et al. (2014), Gentile et al. (2016), and Kalra et al. (2016).
Figure 2.
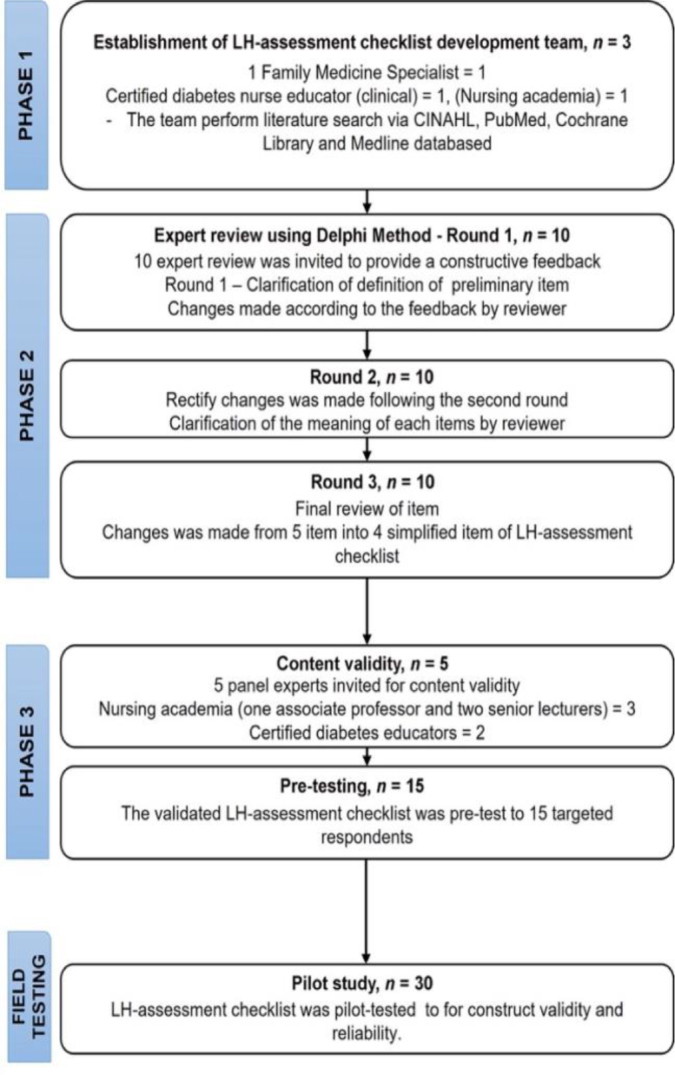
Flowchart of instrument development
Then in phase two, the preliminary checklist consisted of five items of the LH-assessment checklist undergone by the Delphi technique. The Delphi technique was widely accepted as an effective method to secure consensus from experts of different backgrounds and perspectives. Three review rounds were carried out, which included ten experts each round. The first round includes clarification of the definition of all five items, and changes were made based on the panel member suggestions made in the first review, which included clarification of the definition for ‘rubbery’, ‘swelling of fatty tissue’ and ‘swelling of the tissue that is soft. Changes made following the second round included clarification of the meaning of “swelling of fatty tissue around injection site”, “thickened ‘rubbery’ feeling”, and “swelling of the tissue that is soft and firm” and the design of the checklist. In the final round, the two-term was combined into one item as “thickened ‘rubbery’ swelling of the tissue that is soft and firm”, which finalised the four items in our LH-assessment checklist.
Then, the four items of the LH-assessment checklist were further evaluated for their content validity in phase 3. The process of obtaining content validity was crucial to finding an expert to validate the final content of the checklist (Gunawan et al., 2021). Thus, five panels were invited to exercise the process, including three nursing academia (one associate professor and two senior lecturers) and two certified diabetes educators working in a public hospital in North Borneo, Malaysia. All 4-items in the checklist showed excellent content validity in their representativeness, relevancy, and clarity (Mean I-CVI = 1.0; Kappa = 1.0; S-CVI = 1.0). Before field testing the newly developed checklist, we pre-tested the checklist for 15 diabetes nurse educators. During the pre-test, all participants understood the sentence and item; the feedback gained from the pre-test was very positive and user-friendly.
Construct validity was then carried out using Exploratory Factor Analysis (EFA) to determine the structure of the LH assessment checklist. A total of 40 respondents were invited to participate in the field testing. The sample size calculation was based on item to response ratio (1:10) as recommended by Nunnally (1978) and Watson and Thompson (2006).
Of the 40 participants invited, only 30 consented, indicating a 75.0% response rate. The Principal Component Analysis (PCA) using a Varimax rotation method was utilised, assuming a correlation between domains. The Kaiser-Meyer-Olkin (KMO) measure was 0.90, with individual KMO measures all greater than 0.8, which fall under’ meritorious’ to’ marvellous’ (Kaiser, 1974). Bartlett’s test of sphericity was statistically significant with a Chi-square of 444.17 and p < 0.001, indicative that data was likely factorable and the factor analysis was appropriate.
PCA revealed one factor with an eigenvalue set at 3.0. The proportion of the total variance explained for the factor was 76.35% (Table 1). The mean, standard deviation and factor loading of each item were summarised in Table 2. All factor loading was above 0.4 and ranged between 0.71 - 0.80. The Cronbach’s alpha coefficient was 0.89, exhibiting an acceptable internal consistency; therefore, the LH- identification checklist was deemed reliable. The stability of the LH-assessment checklist revealed the intra-correlation coefficient average measure, ICC of 0.89 (95% CI [0.82 – 0.95], p = 0.00).
Table 1.
Total variance explained for LH-assessment checklist (n = 30)
| Components | Initial Eigenvalues | Extraction Sums of Squared Loadings | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Total | % of Variance | Cumulative % | Total | % of Variance | Cumulative % | |
| 1 | 3.05 | 76.35 | 76.35 | 3.05 | 76.35 | 76.35 |
| 2 | 0.74 | 18.61 | 94.95 | |||
| 3 | 0.12 | 3.00 | 97.96 | |||
| 4 | 0.08 | 2.04 | 100 | |||
Table 2.
Mean, standard deviation and factor loading of the LH-assessment checklist (n = 30)
| Factors | Mean | SD | Factor loading |
|---|---|---|---|
| Item 1 | 1.23 | 0.42 | 0.75 |
| Item 2 | 1.47 | 0.50 | 0.79 |
| Item 3 | 1.27 | 0.44 | 0.80 |
| Item 4 | 1.53 | 0.50 | 0.71 |
Data Collection
Data collection in this study consists of two parts. The first part involves the self-administration questionnaire of LH-associated risk factors by Cunningham and McKenna (2013). A patient who met the inclusion criteria and gave consent to participate in the study was given the self-administered questionnaire. Next, the patient was brought to a procedure room for LH assessment. The LH assessment was conducted by a certified diabetes educator guided by the LH assessment checklist. The patient was given a gown to change into, and an LH assessment was carried out in the procedure room to ensure patient privacy. The location of LH was identified by asking about the insulin injection site of the patients.
The injection sites were examined by certified diabetes educators who have undergone formal accredited training as diabetic educators. The site of insulin injection was examined using palpation techniques, as stated by Gentile et al. (2016). The patient was instructed to be in a lying position, with the site of insulin injection exposed. Then the area of injection was palpated gently using the tip of the fingers. Then, a pinching manoeuvre was performed when perceiving harder skin to confirm their first impression and to determine the pain sensation. This step will be repeated to compare the thickness of the suspected spot to that of surrounding areas.
The presence of LH was indicated by swelling of fatty tissue around the subcutaneous insulin injection sites, palpable lump and thickened ‘rubbery’ swelling of tissue which is soft to a firm or less pain sensation at the insulin injection sites (Cunningham & McKenna, 2013). The absence of LH indicated a regular injection site.
Data Analysis
Data were analysed using the IBM SPSS (Statistical Package for the Social Sciences) version 26.0, Statistics software for Windows. In our analysis, descriptive statistics was used to present patient demographic, LH-associated risk factors, and characteristics of LH were evaluated and displayed in the form of frequency and percentage. We used to estimate the association using the Chi-square test, considering that both independent and dependent variables were categorical (Agresti, 2013). Statistical significance was set at a p-value less than 0.05. The data set was cleaned and reviewed without any missing data for all variables. The demographic characteristics of the subjects were described using descriptive analysis. Two extreme outliers were excluded from the study.
Ethical Consideration
This research study was ethically approved by the National Institutional Health and Medical Research Ethics Committee, Ministry of Health Malaysia (NMRR-16-2534-3323(IIR) and was conducted in conformity with the 2008 Declaration of Helsinki ethical guidelines. Informed consent was also conducted in each participant prior to data collection. The study objectives and procedures were explained to all participants, and they were able to withdraw from the study at any time without penalty. All data were kept confidential and stored in a secured computer.
The research was consistent with strengthening the reporting claims for observational studies of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist (von Elm et al., 2014).
Results
A total of 128 out of 130 questionnaires were included in the analysis and presented in a table. Descriptive statistics for patient demographic (Table 3), LH-associated risk factors (Table 4) and characteristics of LH (Table 5) were evaluated and displayed in the form of frequency and percentage. The total number of patients with LH is 66; thus, the overall prevalence of LH was 51.6% [95% CI: 42.6, 60.5].
Table 3.
Patients socio-demographic characteristics (N = 128)
| Characteristics | n | % | p-value |
|---|---|---|---|
| Age | 0.22 | ||
| 18-28 years | 5 | 3.9 | |
| 29-39 years | 12 | 9.4 | |
| 40-49 years | 20 | 15.6 | |
| 50-59 years | 67 | 52.3 | |
| 60 years and above | 24 | 18.8 | |
| Gender | 0.75 | ||
| Male | 69 | 53.9 | |
| Female | 59 | 46.1 | |
| Marital status | 0.42 | ||
| Single | 23 | 18.0 | |
| Married | 98 | 76.6 | |
| Divorcee | 7 | 5.5 | |
| Race | 0.10 | ||
| Malay | 35 | 27.3 | |
| Chinese | 52 | 40.6 | |
| Sabahan Natives | 18.0 | 14.1 | |
| Others | 23 | 18 | |
| Level of education | 0.25 | ||
| No formal education | 5 | 3.9 | |
| Primary school | 3 | 2.3 | |
| Secondary school | 116 | 90.6 | |
| Tertiary school | 4 | 3.1 | |
| Classification BMI (kg/m2) | 0.018* | ||
| 18.5 - 24.9 (Normal) | 25 | 19.5 | |
| 25.0 – 29.9 (Overweight) | 67 | 52.3 | |
| 30.0 -39.9 (Obese) | 32 | 25.0 | |
| ≥ 40.0 (Morbid obesity) | 4 | 3.1 |
p <0.05
Note: Body Mass Index (BMI) in adults according to WHO classification
Table 4.
Lipohyperthropy-associated risk factors (N = 128)
| Risk Factor | Frequency (%) | Lipohypertrophy |
p-value | |
|---|---|---|---|---|
| Not presence | Presence | |||
| Years on Injection | 0.002* | |||
| 0-5 years | 50 (39.1) | 34(26.6) | 16(12.5) | |
| 6-10 years | 44 (34.4) | 13(24.2) | 31(24.2) | |
| 10-19 years | 21 (16.4) | 8(6.3) | 13(10.2) | |
| 20 years and above | 13 (10.2) | 7(5.5) | 6(4.7) | |
| Total injection in a day | 0.07 | |||
| Once-daily | 7 (5.5) | 5(3.9) | 2(1.6) | |
| Twice daily | 31 (24.2) | 14(10.9) | 17(13.3) | |
| Three times daily | 63 (49.2) | 25(19.5) | 38(29.7) | |
| Four times a day or more | 27 (21.1) | 18(14.1) | 9(7.0) | |
| Total insulin unit per day | 0.07 | |||
| Less than 30 unit | 25(19.5) | 8(6.3) | 17(13.3) | |
| Between 30-60 unit | 69(53.9) | 34(26.6) | 35(27.3) | |
| Between 61-100 unit | 32(25.0) | 20(15.6) | 12(9.4) | |
| Greater than 100 unit | 2(1.6) | 0(0) | 2(1.6) | |
| Often change needle | 0.023* | |||
| At every injection | 4(3.1) | 0(0) | 4(3.1) | |
| Every 2-3 injection | 39(30.5) | 22(17.2) | 17(13.3) | |
| Every 4-5 injection | 80(62.5) | 40(31.3) | 40(31.3) | |
| When cartridge/pen is finished | 5(3.9) | 0(0) | 5(3.9) | |
| Insulin injection site | 0.09 | |||
| Abdomen | 117(91.4) | 54(42.2) | 63(49.2) | |
| All above by rotation | 11(8.6) | 8(6.3) | 3(2.3) | |
| Move to a different area | 0.015* | |||
| Yes, I move | 122(95.3) | 62(48.4) | 60(46.9) | |
| Move around the site occasionally | 6(4.7) | 0(0) | 6(4.7) | |
p <0.05
Table 5.
Characteristics of Lipohyperthrophy (N = 128)
| Characteristics | Injection Site Examination Checklist |
|
|---|---|---|
| Not Presence | Presence | |
| Palpable lump | 100 (78.1) | 28 (21.9) |
| Swelling of fatty tissue around the injection site | 69 (53.9) | 59 (46.1) |
| Thickened ‘rubbery’ swelling of the tissue that is soft and firm | 128 (100) | 0 (0) |
| Less pain sensation | 96 (75.0) | 32 (25.0) |
Note: Lipohypertrophy indicated as the presence of any of these characteristics
Further, the Pearson Chi-Square test was utilised to examine the relationship between the presence of LH and the patient’s socio-demographic and associated risk factors. The results revealed that there is a significance relationship between the presence of LH and BMI categories (χ2 = 10.059, df = 3, p = 0.018), duration of injection (χ2 = 15.001, df = 3, p = 0.002), frequency of needle replacement (χ2 = 9.525, df = 3, p = 0.023) and rotation of injection site (χ2 = 5.914, df = 1, p = 0.015) (Table 4).
Discussion
Prevalence of Lipohypertrophy
This cross-sectional study demonstrated that the LH prevalence of 51.6% (95% CI: 42.6, 60.5) is consistent with the pooled prevalence rates of LH among type 2 diabetes mellitus 49%, (95% CI 23 – 74%), reported in a recent systematic review and meta-analyses by Deng et al. (2018). In the recent study of (Wang et al., 2021), the overall prevalence of LH was 41.8% (95% CI: 35.9% to 47.6%), which was consistent with the range of LH prevalence in our study. Previous studies on LH in Asian countries were conducted in China and India; however, our findings represent LH prevalence in the widely diverse Malaysian population. Although there are many similarities in the previous findings on the prevalence of LH, to the best of our knowledge, this is the first published study on its prevalence in type 2 diabetes mellitus patients in the Sabah, Malaysian population.
Patient Characteristics and Associated Risk Factors of Lipohypertrophy
We investigated whether the patient’s demographic factors (age categories, gender, race, marital status, education level and BMI) and LH-associated factors (years of insulin injection, total number of injections/day, total insulin unit/day, frequency of needle replacement, site of insulin injection and rotation of injection site) were associated with the development of LH. Of the twelve factors, only four factors exhibit a statistically significant relationship with the formation of LH. The four risk factors are BMI category, duration of insulin injection, frequency of changing insulin needle and rotation of injection site. Binomial logistic regression analysis reported that of the four factors, BMI obese categories and insulin injection for more than six years increase the risk of having LH. This finding is similar to previous studies, which indicate that the longer duration of insulin injection raises the chances of developing LH (Hajheydari et al., 2011; Pozzuoli et al., 2018). A similar study in West India also confirms the high prevalence of LH (68%) in diabetes who is on a longer duration of insulin therapy (Pahuja et al., 2019). This might be explained by the fact that insulin has a proliferating effect on the fat tissue (Vardar & Kızılcı, 2007). The histopathology findings also show that the number of fat cells in LH areas doubles that of the surrounding skin (Kadiyala et al., 2014).
In our study, 59 (89.4 %) cases of LH were found in those patients with higher BMI values. Logistic regression predicts that those in the obese BMI category have an increased risk of having LH by 3.44 times. Several studies did not find any significant association between BMI and the presence of LH (Hajheydari et al., 2011; Pozzuoli et al., 2018; Vardar & Kızılcı, 2007). Barola et al. (2018) reported that being underweight is highly connected with the development of LH, contrary to the empirical evidence from Ji et al. (2017), which stated that LH is higher among patients with higher BMI values (Al Hayek et al., 2016; De Coninck et al., 2010; Vardar & Kızılcı, 2007). We observed that varying association was reported between BMI and the occurrence of LH throughout the literature. These inconsistencies might be due to the types of diabetes patients studied in each literature (e.g., type 1 diabetes mellitus and type 2 diabetes mellitus) and the lack of a gold standard to measure the presence of LH. Besides, the identification of LH in most prevalence studies relies on observation and palpation techniques by a certified health practitioner, which many other factors may influence. Ultrasounds are too expensive and not practical for a routine examination; thus, specific training on the identification of LH, which is cost-effective, is essential (Gentile et al., 2016).
Gentile et al. (2016) have proven that proper training of HP, specifically in identifying LH, increased the consistency rate among HPs to 97%, similar to the gold standard of skin ultrasound. In our study, the area under the ROC curve (AUROC) of the LH checklist test, which involves observation and palpation of the injection site by a certified diabetes educator, indicates a good discriminative ability in identifying LH. One-to-one diabetic education and close monitoring of glycemic reading effectively achieve the target metabolic control values (Eroglu & Sabuncu, 2021).
Daily insulin dose is highly associated with LH development (AlJaber et al., 2020; Blanco et al., 2013; Ji et al., 2017; Pozzuoli et al., 2018). In this study, the total insulin unit per day lacks any statistically significant effect on the occurrence of LH. We found that in our study, the prevalence of LH was higher in the group- “change needle every 4-5 injections” than in other groups. Similar to this, earlier studies discovered a link between the occurrence of LH and multiple reuses of needles (Blanco et al., 2013). Failure to frequently change the needle causes damage to the needle tip, which leads to silicone coating loss. Therefore, it may cause tissue damage and subsequent development of LH (Vardar & Kızılcı, 2007).
Six studies were consistent with our findings that rotation of insulin injection is a statistically significant effect of insulin injection rotation on the presence of LH (Al Hayek et al., 2016; Barola et al., 2018; Cunningham & McKenna, 2013; Ji et al., 2017; Pozzuoli et al., 2018). The correct injection site is the most studied and emphasises the prevention of LH (Barola et al., 2018). A study in China showed that patients who refrain from the systematic rotation of insulin injections are 8.4 times at higher risk of developing LH (Ji et al., 2017). The prevalence of LH was higher for patients who neither remembered to change their injection site nor did so. However, one study reported conflicting results. The earlier study discovered that the frequency of LH was not affected by the rotation of the injection site (Omar et al., 2011). They suggested that many young patients without LH do not comply with the instruction to rotate their injection site (Omar et al., 2011).
Implications to Nursing Practice
The findings provide empirical evidence on a validated assessment checklist in the identification of LH among insulin-treated type 2 diabetes. Therefore, nurses can utilise this checklist as a routine assessment in the diabetic clinic. In addition, the assessment findings can be used to guide proper patient education related to insulin. Therefore, nurses can provide diabetes education efficiently to the targeted individual thus, increase the quality of nursing care.
Study Limitations and Recommendations
We acknowledged that this study is not free from limitations. First, we do not have a large sample to determine the association between race and the presence of LH. Second, the cross-sectional design allowed only a temporal snapshot of LH criteria at a given time. There was also a logistic limitation to consider during the LH assessment. Due to room limitations in the outpatient clinic, the LH assessment was performed in the procedure room by-turn basis to ensure patient privacy was maintained. We could have performed the LH assessment meticulously, which would have been useful in interpreting the ‘rubbery’ swelling of LH. Nevertheless, the assessment procedure was maintained to be objective and straight to the point.
We recommend including LH assessment among patients with insulin-treated diabetes as part of the routine evaluation of adherence in rotating the insulin injection site. For instance, the nurse-led Joint Asia Diabetes Evaluation (JADE) program is one of the multi-national programs in the Asia-Pacific region that aim to encourage patient empowerment and engagement in diabetes self-management (Lim et al., 2021). The outcome of the JADE program suggested that patients who are highly engaged and well-informed of their diabetes status showed reduced cardiometabolic risk factors. Nevertheless, the LH assessment was not mentioned in the published study as part of the routine evaluation. Therefore, we recommend that future studies include LH assessment to gain more data on LH-associated risk factors. We also recommend that future studies look into the knowledge and competency level of LH-assessment skills among nurses and diabetes educators to gain more information and better management of LH among insulin-treated type 2 diabetes mellitus in the Malaysian context.
Conclusion
The high prevalence of LH in this study indicates a need for a prevention strategy, which includes LH assessment for all insulin-treated type 2 diabetes mellitus patients, identification of LH and health education on the correct method of insulin injection. In addition, health education to all insulin-treated type 2 diabetes mellitus patients should incorporate LH identification during self-assessment of insulin site injection and the importance of changing the needle and rotating the injection site. Thus, study findings can be incorporated into the nursing or post-basic diabetic management curricula. This is to raise nurses’ awareness of the importance of identifying lipohyperthrophy and expand nurses’ knowledge regarding insulin injection techniques.
Acknowledgment
The authors thank all nurses participating in this research.
Declaration of Conflicting Interest
The authors declare no conflicts of interest.
Funding
None.
Authors’ Contributions
RAN initiated the study conceptualisation, design and writing of the main article. DCT reviewed the quality and revised the manuscript. RAN was in charge of the coordination of data collection in the clinical setting and entering data in statistical software. DCT performed data cleaning and data analysing. RAN and DCT interpreted the data. All authors made final approval of the manuscript and agreed with the final version of the manuscript.
Authors’ Biographies
Rose A Nain, RN, CDE, MNSc is a Nursing Lecturer at the Nursing Department, Faculty of Medicine and Health Sciences, Universiti Malaysia Sabah, Malaysia.
Deena Clare Thomas, CDE, RN, MNSc is a Nursing Lecturer at the Nursing Department, Faculty of Medicine and Health Sciences, Universiti Malaysia Sabah, Malaysia.
Data Availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
References
- Abu Ghazaleh, H., Hashem, R., Forbes, A., Dilwayo, T. R., Duaso, M., Sturt, J., Halson-Brown, S., & Mulnier, H. (2018). A systematic review of ultrasound-detected lipohypertrophy in insulin-exposed people with diabetes. Diabetes Therapy, 9(5), 1741-1756. 10.1007/s13300-018-0472-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agresti, A. (2013). Categorical data analysis (3rd ed.). Hoboken, NJ: John Wiley & Sons. [Google Scholar]
- Al Hayek, A. A., Robert, A. A., Braham, R. B., & Al Dawish, M. A. (2016). Frequency of lipohypertrophy and associated risk factors in young patients with type 1 diabetes: A cross-sectional study. Diabetes Therapy, 7(2), 259-267. 10.1007/s13300-016-0161-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- AlJaber, A. N., Sales, I., Almigbal, T. H., Wajid, S., & Batais, M. A. (2020). The prevalence of lipohypertrophy and its associated factors among Saudi patients with type 2 diabetes mellitus. Journal of Taibah University Medical Sciences, 15(3), 224-231. 10.1016/j.jtumed.2020.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arora, S., Agrawal, N. K., Shanthaiah, D. M., Verma, A., Singh, S., Patne, S. C. U., Kalra, S., Singh, P., & Goyal, S. (2021). Early detection of cutaneous complications of insulin therapy in type 1 and type 2 diabetes mellitus. Primary Care Diabetes, 15(5), 859-864. 10.1016/j.pcd.2021.06.004 [DOI] [PubMed] [Google Scholar]
- Barola, A., Tiwari, P., Bhansali, A., Grover, S., & Dayal, D. (2018). Insulin-related lipohypertrophy: Lipogenic action or tissue trauma? Frontiers in Endocrinology, 9, 638. 10.3389/fendo.2018.00638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benson, E.-o. N., Okeke, N. T., & Okeke, C. B. (2017). Factors that influence insulin adherence in self-administration and actions that could improve it. Journal of Nursing and Palliative Care Services, 1(1), 16-22. [Google Scholar]
- Blanco, M., Hernández, M. T., Strauss, K. W., & Amaya, M. (2013). Prevalence and risk factors of lipohypertrophy in insulin-injecting patients with diabetes. Diabetes & Metabolism, 39(5), 445-453. 10.1016/j.diabet.2013.05.006 [DOI] [PubMed] [Google Scholar]
- Buyruk, B. A., Kebapci, N., Yorulmaz, G., Alaguney, E. S., Akalin, A., & Efe, B. (2019). 59-LB: Prevalence and risk factors of lipohypertrophy and lipoatrophy in diabetes patients receiving insulin therapy. Diabetes, 68(Supplement_1). 10.2337/db19-59-LB [DOI] [Google Scholar]
- Calliari, L. E., Cudizio, L., Tschiedel, B., Pedrosa, H. C., Rea, R., Pimazoni-Netto, A., Hirsch, L., & Strauss, K. (2018). Insulin Injection Technique Questionnaire: Results of an international study comparing Brazil, Latin America and World data. Diabetology & Metabolic Syndrome, 10(1), 1-7. 10.1186/s13098-018-0389-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham, M. T., & McKenna, M. (2013). Lipohypertrophy in insulin-treated diabetes: Prevalence and associated risk factors. Journal of Diabetes Nursing, 17(9), 340-343. [Google Scholar]
- De Coninck, C., Frid, A., Gaspar, R., Hicks, D., Hirsch, L., Kreugel, G., Liersch, J., Letondeur, C., Sauvanet, J. P., & Tubiana, N. (2010). Results and analysis of the 2008–2009 Insulin Injection Technique Questionnaire survey. Journal of Diabetes, 2(3), 168-179. 10.1111/j.1753-0407.2010.00077.x [DOI] [PubMed] [Google Scholar]
- Deng, N., Zhang, X., Zhao, F., Wang, Y., & He, H. (2018). Prevalence of lipohypertrophy in insulin‐treated diabetes patients: A systematic review and meta‐analysis. Journal of Diabetes Investigation, 9(3), 536-543. 10.1111/jdi.12742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eroglu, N., & Sabuncu, N. (2021). The effect of education given to type 2 diabetic individuals on diabetes self-management and self-efficacy: Randomized controlled trial. Primary Care Diabetes, 15(3), 451-458. 10.1016/j.pcd.2021.02.011 [DOI] [PubMed] [Google Scholar]
- Famulla, S., Hövelmann, U., Fischer, A., Coester, H.-V., Hermanski, L., Kaltheuner, M., Kaltheuner, L., Heinemann, L., Heise, T., & Hirsch, L. (2016). Insulin injection into lipohypertrophic tissue: Blunted and more variable insulin absorption and action and impaired postprandial glucose control. Diabetes Care, 39(9), 1486-1492. 10.2337/dc16-0610 [DOI] [PubMed] [Google Scholar]
- Gentile, S., Guarino, G., Giancaterini, A., Guida, P., & Strollo, F. (2016). A suitable palpation technique allows to identify skin lipohypertrophic lesions in insulin-treated people with diabetes. Springerplus, 5(1), 1-7. 10.1186/s40064-016-1978-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentile, S., Strollo, F., Viazzi, F., Russo, G., Piscitelli, P., Ceriello, A., Giorda, C., Guida, P., Fioretto, P., & Pontremoli, R. (2018). Five-year predictors of insulin initiation in people with type 2 diabetes under real-life conditions. Journal of Diabetes Research, 2018, 7153087. 10.1155/2018/7153087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerensea, H., Moges, A., Shumiyee, B., Abrha, F., Yesuf, M., Birihan, T., Birhanu, T., & Getahun, Z. (2015). Knowledge and attitude on insulin self administration among type one diabetic patients in Mekele hospital, Tigray, Ethiopia. Advances in Surgical Sciences, 3(5), 32-36. 10.11648/j.ass.20150305.11 [DOI] [Google Scholar]
- Gorska-Ciebiada, M., Masierek, M., & Ciebiada, M. (2020). Improved insulin injection technique, treatment satisfaction and glycemic control: Results from a large cohort education study. Journal of Clinical & Translational Endocrinology, 19, 100217. 10.1016/j.jcte.2020.100217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunawan, J., Marzilli, C., & Aungsuroch, Y. (2021). Establishing appropriate sample size for developing and validating a questionnaire in nursing research. Belitung Nursing Journal, 7(5), 356-360. 10.33546/bnj.1927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajheydari, Z., Kashi, Z., Akha, O., & Akbarzadeh, S. (2011). Frequency of lipodystrophy induced by recombinant human insulin. European Review for Medical and Pharmacological Sciences, 15(10), 1196-1201. [PubMed] [Google Scholar]
- Ji, L., Sun, Z., Li, Q., Qin, G., Wei, Z., Liu, J., Chandran, A. B., & Hirsch, L. J. (2017). Lipohypertrophy in China: Prevalence, risk factors, insulin consumption, and clinical impact. Diabetes Technology & Therapeutics, 19(1), 61-67. 10.1089/dia.2016.0334 [DOI] [PubMed] [Google Scholar]
- Kadiyala, P., Walton, S., & Sathyapalan, T. (2014). Insulin induced lipodystrophy. British Journal of Diabetes, 14(4), 131-133. 10.15277/bjdvd.2014.036 [DOI] [Google Scholar]
- Kaiser, H. F. (1974). An index of factorial simplicity. Psychometrika, 39(1), 31-36. 10.1007/BF02291575 [DOI] [Google Scholar]
- Kalra, S., Kumar, A., & Gupta, Y. (2016). Prevention of lipohypertrophy. Journal of the Pakistan Medical Association, 66(7), 910-911. [PubMed] [Google Scholar]
- Lim, L.-L., Lau, E. S. H., Fu, A. W. C., Ray, S., Hung, Y.-J., Tan, A. T. B., Chamnan, P., Sheu, W. H. H., Chawla, M. S., & Chia, Y.-C. (2021). Effects of a technology-assisted integrated diabetes care program on cardiometabolic risk factors among patients with type 2 diabetes in the Asia-Pacific region: the JADE program randomized clinical trial. JAMA Network Open, 4(4), e217557-e217557. 10.1001/jamanetworkopen.2021.7557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunnally, J. C. (1978). Psychometric theory. New York: McGraw-Hill. [Google Scholar]
- Omar, M. A., El-Kafoury, A. A., & El-Araby, R. I. (2011). Lipohypertrophy in children and adolescents with type 1 diabetes and the associated factors. BMC Research Notes, 4(1), 1-3. 10.1186/1756-0500-4-290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pahuja, V., Punjot, P., Fernandes, G., & Chatterjee, N. (2019). Exploring the factors associated with lipohypertrophy in insulin-treated type 2 diabetes patients in a tertiary care hospital in Mumbai, India. International Journal of Diabetes in Developing Countries, 39(3), 426-431. 10.1007/s13410-019-00735-0 [DOI] [Google Scholar]
- Pozzuoli, G. M., Laudato, M., Barone, M., Crisci, F., & Pozzuoli, B. (2018). Errors in insulin treatment management and risk of lipohypertrophy. Acta Diabetologica, 55(1), 67-73. 10.1007/s00592-017-1066-y [DOI] [PubMed] [Google Scholar]
- Rahim, F. F., Abdulrahman, S. A., Kader Maideen, S. F., & Rashid, A. (2020). Prevalence and factors associated with prediabetes and diabetes in fishing communities in penang, Malaysia: A cross-sectional study. PloS One, 15(2), e0228570. 10.1371/journal.pone.0228570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spollett, G., Edelman, S. V., Mehner, P., Walter, C., & Penfornis, A. (2016). Improvement of insulin injection technique: Examination of current issues and recommendations. The Diabetes Educator, 42(4), 379-394. 10.1177/0145721716648017 [DOI] [PubMed] [Google Scholar]
- Sun, H., Saeedi, P., Karuranga, S., Pinkepank, M., Ogurtsova, K., Duncan, B. B., Stein, C., Basit, A., Chan, J. C. N., & Mbanya, J. C. (2022). IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Research and Clinical Practice, 183, 109119. 10.1016/j.diabres.2021.109119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tee, E., & Yap, R. W. K. (2017). Type 2 diabetes mellitus in Malaysia: Current trends and risk factors. European Journal of Clinical Nutrition, 71(7), 844-849. 10.1038/ejcn.2017.44 [DOI] [PubMed] [Google Scholar]
- Vardar, B., & Kızılcı, S. (2007). Incidence of lipohypertrophy in diabetic patients and a study of influencing factors. Diabetes Research and Clinical Practice, 77(2), 231-236. 10.1016/j.diabres.2006.12.023 [DOI] [PubMed] [Google Scholar]
- von Elm, E., Altman, D. G., Egger, M., Pocock, S. J., Gøtzsche, P. C., & Vandenbroucke, J. P. (2014). The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. International Journal of Surgery, 12(12), 1495-1499. 10.1016/j.ijsu.2014.07.013 [DOI] [PubMed] [Google Scholar]
- Wang, K., Zhang, S., Liu, C., & Chen, Y. (2021). A meta-analysis and meta-regression on the prevalence of lipohypertrophy in diabetic patients on insulin therapy. Therapies, 76(6), 617-628. 10.1016/j.therap.2021.04.002 [DOI] [PubMed] [Google Scholar]
- Watson, R., & Thompson, D. R. (2006). Use of factor analysis in Journal of Advanced Nursing: Literature review. Journal of Advanced Nursing, 55(3), 330-341. 10.1111/j.1365-2648.2006.03915.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.


