Abstract
Total hip arthroplasties (THAs) are usually performed in older patients. Despite a growing number of THAs in younger adults, it is unclear whether they have similar priorities in recovery compared with their older counterparts. The purpose of this systematic review was to explore younger patients' priorities when undergoing a THA. Multiple databases were searched in September 2021 prioritizing qualitative data. This review was reported using the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines. Of 14,495 articles screened, nine remained for analysis. Four common themes were discovered: improving function and mobility; pain; relationships; and patient expectations and education. However, there was insufficient information to clarify whether these themes could be attributed directly to younger adults undergoing a THA. The absence of research on THA patients younger than 50 years results in the loss of the voices of these patients. Further research is essential to ensure their needs are identified, addressed, and met.
Introduction
Rationale
The objectives of total hip arthroplasty (THA) surgery are to reduce pain, increase function, and improve the patient's quality of life (QOL; Jourdan et al., 2012; Knight et al., 2011; Markatos et al., 2020). The U.K. National Joint Registry (NJR) reported that a total of 101,384 THAs were performed in 2019 (NJR, 2019). This number is predicted to increase year by year as the age of the general population increases (Kurtz et al., 2009). The mean age of patients undergoing a THA is 68 years (Ben-Shlomo et al., 2020), with the majority taking place in patients older than 65 years (Ben-Shlomo et al., 2020; Crowninshield et al., 2006). The incidence of THA in younger adults is increasing, similar to that for the overall population (Aalund et al., 2017; Kurtz et al., 2009). In total, 5,708 (5.6%) patients undergoing a THA recorded in 2019 were younger than 50 years and 14,376 (14%) recorded patients were between 50 and 59 years of age. This presents a significant increase from the numbers recorded in 2011, when 4,828 patients (6%) were younger than 50 years and 10,516 patients (14%) were between 50 and 59 years of age, from a total of 76,357 patient records (NJR, 2019). When considering THA in younger adults, many factors influence clinical advice, including patient activity levels, timing of surgery, fixation method, implant, and bearing-couple choice (Wang et al., 2016). Not only do these factors have an impact on implant longevity but they also influence the ease and likelihood of future revisions (Wang et al., 2016). Surgical attitudes toward THA in younger adults have become more positive throughout the years (Kumar et al., 2017). This could potentially be attributed to the increase in implant survival times and, by extension, reductions in planned revision surgeries enabled by use of new surgical techniques and introduction of modern bearing surfaces and implants (Kamath et al., 2012).
One method of measuring successful outcomes in clinical practice is through Patient Reported Outcome Measures (PROMs) (Larsson et al., 2019), which are completed by the patient to assess symptoms of pain, functional ability, and health status (Wright et al., 2000) and are standardized throughout patient populations to measure the success of interventions from the patient perspective (Larsson et al., 2019; Wright et al., 2000). Extensive attention has been given to research examining PROMs and expectations in older patients (Conner-Spady et al., 2014; Mahomed et al., 2002; Nam et al., 2015; Scott et al., 2019), and PROMS are widely recognized as an effective outcome measurement tool. However, scarce attention has been paid in examining potential differences in PROMs between the rapidly growing younger patient population requiring THA and their older counterparts (Malcolm et al., 2014).
Literature using qualitative research to inform orthopaedic practice is less common but informative (Gooberman-Hill et al., 2011). Through observation and interpretation, qualitative research strives to gain a deeper understanding of the behavior, experience, attitudes, intentions, and motivations of participants (Braun & Clarke, 2013). A qualitative approach is much more effective in exploring patient experiences (Rapport et al., 2013). The need to understand the psychological impact and experience of orthopaedic patients throughout their treatment and recovery was highlighted in previous studies exploring patients with hip fractures (Zidén et al., 2010), where qualitative methods identified many areas of importance to patients that were not evident in the existing outcome measures (Archibald, 2003).
Knowledge of the potentially differing needs of this patient group can support nurses to provide the best quality care possible. Nursing practice requires an individualized, holistic approach toward patients (Van Rooyen & Jordan, 2013). By listening to patients, exploring their experiences, and involving them and their families as healthcare partners, nurses can more effectively support and address the needs of this patient population (Janes & Serrant, 2018).
Objectives
Patient demographics such as age, gender, and preoperative QOL influence patient-reported outcomes (Aalund et al., 2017). Current knowledge and practice are heavily informed by the views of the predominantly older patient population that historically undergoes THA surgery. It is unclear whether outcome priorities and goals important to older patients are as important to younger THA patients or, indeed, if younger THA patients consider other outcome priorities more important than those currently measured using standard PROMs. The purpose of this systematic literature review was to explore young adults' priorities and concerns when undergoing a primary elective THA. The search explored studies focusing on the priorities identified by patients themselves.
Methods
This systematic review was conducted and reported in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) guidelines (Page et al., 2021).
Registration and protocol
This systematic literature review is registered under the PROSPERO international register (Registration No. CRD42021279411).
Inclusion Criteria
Studies were included if they included participants 18–50 years of age who had undergone a primary THA and used qualitative data or free-text reported outcomes. Studies were excluded if they utilized only standard PROMs in reporting outcomes or reported on the operative procedure only. This ensured that the topics assessed in the included studies were not limited to those addressed by the PROMs tool. Only articles published in the English language were included.
Search Strategy
The literature review was based on systematic searches in multiple literature databases. The approach was adopted following a scoping exercise, which resulted in no other systematic review in this subject area.
The search terms were developed using the PIO search strategy (Akobeng, 2005). The PIO search strategy is considered appropriate for exploratory research questions focusing on qualitative research. Key words are divided into three categories: Population, Intervention, and Outcome (Jenson, 2019; Munn et al., 2018). Table 1 demonstrates the PIO search strategy used in this literature review and its relation to the inclusion/exclusion criteria.
Table 1. PIO Framework (EBSCO, 2019) and Inclusion/Exclusion Criteria.
| PIO | Inclusion | Exclusion |
|---|---|---|
| Population | Adult patients between the ages of 18 and 50 years, inclusive, who have undergone or are scheduled to undergo an elective primary THR. | |
| Intervention | Elective primary THR. All potential chronic health conditions resulting in the need for THR will be included. | THR used to treat traumatic fractures or dislocation of the hip joint. Literature exploring implant survivorship and revision surgeries, studies exploring surgical approaches or implant types, studies exploring the hospital inpatient stay and operative procedure only will be excluded. |
| Outcome | Eligible studies will include data gathered from the patient, either by qualitative methods or by free-text questions on standard PROMs. | Research that measures outcomes by exclusively using standard PROMs tools will be excluded. |
| Types | Qualitative, quantitative, and mixed-method studies are included if reporting qualitative data from the patient. | |
| Date range | No limit | |
| Geography | Worldwide | Note will be taken of studies in countries where the health service is comparable with the National Health Service. |
| Language | English text | Non-English text |
Note. PROM = Patient Reported Outcome Measures; THR = total hip replacement.
Systematic searches were conducted using all possible combinations of the three categories of key words; these included words such as “total hip arthroplasty, priorities, expectations,” amongst others. A full list of included words can be found in Table 2. An example of the combinations of words used in the search strategy is demonstrated in Appendix A.
Table 2. Key Words and Categories Used in Database Searches.
| Population | Intervention | Outcome |
|---|---|---|
| Young patient | Total hip replacement | Priorities |
| Young person | Total hip arthroplasty | Expectations |
| Middle age | THR | Importance |
| Less than 50 | THA | Quality of life |
| Hip prothesis | Health priorities | |
| Perceptions OR Views | ||
| Experiences | ||
| Sport OR Exercise | ||
| Sex OR Relationships | ||
| Function OR mobility | ||
| Pain |
Note. THA = total hip arthoplasty; THR = total hip replacement.
The searches were not limited by historical time constraints or geographical limitations. Forward citation searches and the reference lists of key full-text articles included in the review were manually checked by the researcher to identify any potential eligible studies.
Selection Process
An electronic search took place using Cochrane, MEDLINE, AHMED, Emcare, CINAHL, Web of Science, Scopus, BNI, and EMBASE databases by the primary researcher. Studies reported empirical findings on the priorities and goals expressed by young patients (<50 years) when undergoing a THA. The consensus in the literature appears to classify “young patients” undergoing a THA as younger than 50 years (Crowninshield et al., 2006; Malcolm et al., 2014; Ravi et al., 2012). To be consistent with the literature classification, the systematic literature review enforced the upper age limit as 50 years. Primary observational studies with retrospective, cross-sectional, or prospective research design and randomized controlled trials were eligible if qualitative data were reported.
Data Collection Process
Data collection was completed primarily by a single researcher; three separate researchers then reviewed the data collected to ensure all important aspects were included. Data collected in the participants' own words relating to the important aspects of their own recovery were sought and prioritized.
Data Items
Articles selected for the review were analyzed to identify and capture data relating to the following: (1) study features, including study design and year of publication; (2) study population details, including number of participants and participant demographics; (3) data for outcome measures, including results and thematic findings; and (4) limitations, both limitations recorded by the study author and limitations in answering the question posed in this literature review.
Reporting Bias Assessment
All titles and abstracts were manually screened against the eligibility criteria to identify suitable studies. As part of the quality assurance process, 10% of rejected articles were independently reviewed by other members of the research team. Following this, the full text of any studies identified for potential inclusion was retrieved and examined against the eligibility criteria; 10% of the rejected articles at this stage were reviewed by the research team. Any disagreements were managed through discussion with all four members of the team until an overall consensus was reached.
Because of the variation in study designs included, the quality of studies was assessed using a tool developed specifically for conducting quality appraisal of mixed studies, the Mixed Method Appraisal Tool (MMAT; Hong et al., 2018). The MMAT was designed for the appraisal stage of systematic mixed studies reviews, for example, those that include qualitative, quantitative, randomized controlled trials, observational, and mixed-methods studies. This tool appraises transparency, recruitment, method of data collection, and outcome measurements using a “yes,” “no,” or “can't tell” scoring system, thus appraising the quality of the studies as high, moderate, or low. The outcome of this assessment is presented in Appendix B.
Method of Analysis
In the studies using qualitative design, a three-phase narrative synthesis method was used as explained by Popay et al. (2006). These steps consist of developing the preliminary synthesis, exploring relationships in the data, and assessing the robustness of the synthesis product. The preliminary synthesis of the findings in the included studies occurred during the data extraction stage. The results of the studies were organized by identifying and describing textually, maintaining “text in context” (Sandelowski et al., 2013). This identified the findings and patterns within and throughout the included studies while maintaining context. Heterogeneity was examined by assessing differences and similarities within the context, outcomes, and mechanism of the identified studies (Linden & Hönekopp, 2021). This technique allowed the detection of any emerging themes across the studies in relation to the issues important to young patients when undergoing a THA.
Results
Study selection
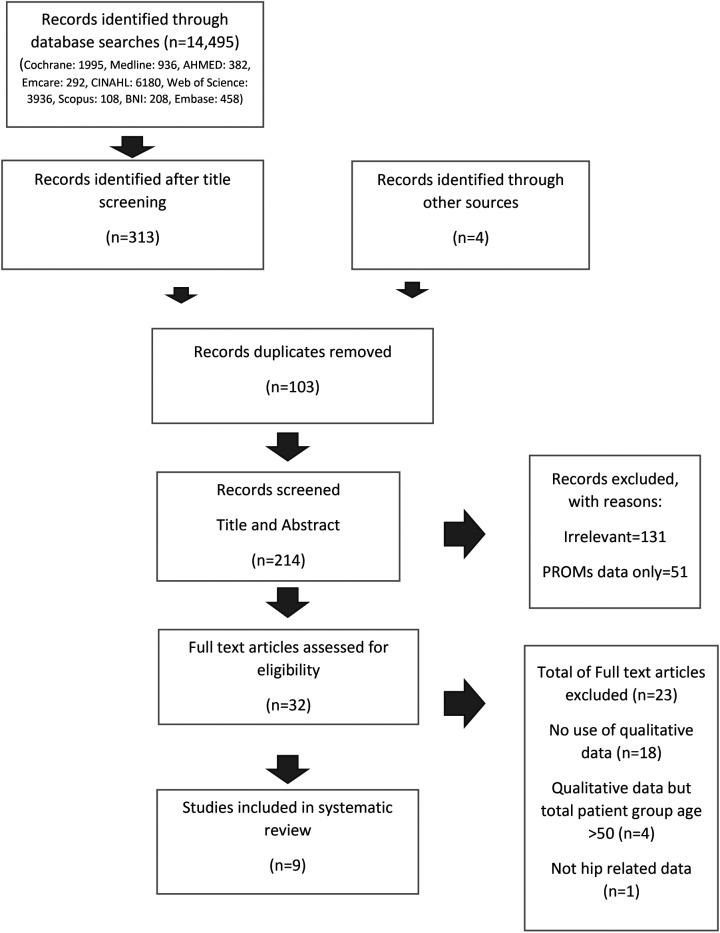
The database searches identified 14,495 records. These record titles and abstract were screened, and 313 records were assessed as being relevant to the review objectives; a further 4 studies were identified through reference lists and forward citations. Records were entered into Endnote, and once duplicates were removed, 214 records remained. In total, 182 records were excluded because of a lack of qualitative data or for relying solely on PROMs data to inform outcomes. Thirty-two full-text articles were screened against the inclusion and exclusion criteria, 18 articles were excluded for reporting no qualitative data, four were excluded for the participant age groups being older than 65 years, and one was excluded for having no hip-related data. The screening process resulted in identification of nine articles that satisfied the inclusion criteria for the final review. Figure 1 details the search and screening process in a PRISMA chart.
Figure 1.
PRISMA chart detailing the search and screening process.
Search results fitting the inclusion and exclusion criteria were limited. All nine articles assessed as meeting the eligibility criteria had limitations in answering the objective of the literature review. The nine studies all involved patients younger than 50 years who had undergone a THA and incorporated qualitative data in the study design. However, each study was designed to answer a specific question and none of these aligned exactly to that posed in this article. No study focused on the outcome priorities of younger THA patients.
Eight studies used qualitative methods in their design, with one study using mixed methods (Lafosse et al., 2008). Lafosse et al. (2008) used postal questionnaires and included space for additional comments by the participant. No additional comments were reported fully within the article, however, nor attributed to specific patient ages.
Seven studies were retrospective in design, and patients were asked to record their data postsurgery (Berg et al., 2019; Fujita et al., 2006; Goodman et al., 2020; Lafosse et al., 2008; Montin et al., 2002; Singh et al., 2020; Sjøoveian & Leegaard, 2017), one study included preoperative interviews (Demierre et al., 2011), and one study covered the early recovery period—9 weeks from the day of operation (Strickland et al., 2017). Six studies used semistructured qualitative interviews at various timepoints through the patient journey (Berg et al., 2019; Fujita et al., 2006; Montin et al., 2002; Sjøoveian & Leegaard, 2017; Strickland et al., 2017), and two studies utilized a nominal group technique (NGT). An NGT employs a highly structured group discussion format to achieve group consensus on a specific topic (Goodman et al., 2020; Singh et al., 2019). Singh et al. (2019) used this method to qualitatively explore patient perspectives on what constitutes hip or knee arthroplasty failure. Forty-two participants were divided into eight nominal groups; two of these groups consisted of participants younger than 45 years. However, the study did not identify how many of these had undergone THA surgery, as operations were recorded as “total knee arthroplasty (TKA) or THA.” The NGT was also used by Goodman et al. (2020) to explore patient perspectives of outcomes after TKA and THA. Goodman et al. (2020) added younger adults to the study after it was noted that the initial participant sample included an insufficient number of younger participants. As a result, two groups of participants younger than 45 years were added to the study. These groups totaled nine participants, with seven of them undergoing a THA.
Only three of the review studies exclusively explored participants undergoing a THA (Fujita et al., 2006; Lafosse et al., 2008; Montin et al., 2002); the other six articles also included patients undergoing a TKA, and in some instances revisions of joint arthroplasties in their Method and Results sections. These studies did not differentiate which joint was operated on within their findings, making it difficult to attribute any themes or findings to THA patient groups. All the studies used methods of thematic analysis when presenting their results. Findings were sometimes linked to individual participants, allowing some clarity on potential priorities for the population of interest in this review.
Results of synthesis
All nine studies included in the report consisted of THA patients. However, six of the nine focused on both THA and TKA patients. The nine studies covered a participant population ranging in age from 22 to 92 years and so were not targeted at the younger THA patient.
The nine articles included within this review contain a total of 14 confirmed THA participants reported as being younger than 50 years. Of the five studies (Berg et al., 2019; Demierre et al., 2011; Fujita et al., 2006; Goodman et al., 2020; Sjøoveian & Leegaard, 2017) that reported the gender of the THA participants, eight participants younger than 50 years were male and six were female.
Four studies did not specify individual participant age and reported mean age and age range only (Demierre et al., 2011; Lafosse et al., 2008; Montin et al., 2002; Strickland et al., 2017). Singh et al. (2020) reported seven participants as younger than 45 years but did not differentiate between patients undergoing THA and TKA. Thus, it was not possible to calculate the average age of the total included participant sample relevant to this systematic review.
Use of the MMAT appraisal tool identified six studies as moderate to high quality and three as poor to moderate quality; however, the data could not be meta-analyzed because of the heterogeneity in outcome measures and study aims. A summary of the quality appraisal of the included studies can be found in Table 3.
Table 3. Characteristics of Included Studies.
| Ref | First Author | Year | Place | Aim | Design and Methods | Sample Size | Average Age of Participants | Relevant Sample | Outcomes | MMAT Result |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Lafosse | 2008 | Toulouse, France | To determine the significance of sexual difficulties in patients with chronic hip pain before and after surgery. | Observational study, retrospective postal questionnaires | 135 THAs | Mean age: 51.8 years; age range: 22–65 years | Not specified | 19% considered their sexual difficulties to be severe to extreme prior to surgery. This caused tension and unhappiness in relationships for 7% of participants. | Mixed-methods study assessment 1/5 Low quality (Appendix B) |
| 2 | Sjøveian | 2017 | Norway | What is the patient's experience of pain after discharge? How does the patient manage the rehabilitation process? | Qualitative study, retrospective semistructured interviews | 12 total; 6 THAs | Age range: 45–83 years | 1 THA | Patients experience varying degrees of pain in first 3–5 weeks after discharge. | Qualitative study assessment 5/5 High quality (Appendix B) |
| 3 | Singh | 2020 | New York | To determine the themes that define TJA failure from the patient's perspective. To assess whether these themes confirm the core set domains endorsed by the PROMs OMERACT. | Observational, qualitative, retrospective study, nominal group method | 42 total; 21 THAs | Mean age: 66 years | n = 7, not specified if THA or TKA | When defining a failure of total joint replacement, the themes that ranked highest with participants were as follows: (1) pain; (2) adverse postoperative effects; (3) unable to resume normal activities or return to work; (4) little or no improvement in quality of life; and (5) early revision surgery | Qualitative study assessment 5/5 High quality (Appendix B) |
| 4 | Goodman | 2020 | New York | What results matter the most to a patient undergoing/having a knee or hip arthroplasty? | Observational, qualitative, retrospective study, nominal group method | 45 total; 20 THAs | Mean age: 65 years | 7 THAs | All participant groups ranked the same top three outcomes, though responses varied with age. The younger participant groups rated restored quality of life (including social life) as second in importance and improved function as third. | Qualitative study assessment 5/5 High quality (Appendix B) |
| 5 | Fujita | 2006 | Saga City, Japan | To describe OA patients' experience before and after THA to have a better understanding of patients' perspectives on THA. | Observational, qualitative study, retrospective semistructured interviews | 20 THAs | Age range: 45–91 years | 3 THAs | Participants reported the following: -Life restricted by pain and disability -Inferiority complex relating to disability -Difficulties with daily activities -Distress over body image |
Qualitative study assessment 5/5 High quality (Appendix B) |
| 6 | Strickland | 2017 | Oxford, United Kingdom | To explore patients' perspective of surgery and early recovery when undergoing a lower-limb (hip or knee) arthroplasty. | Qualitative study, perioperative open semistructured interviews | 30 total; 16 THAs | Age range: 45-92 years | Not specified | Reported themes consisted of the following: Improving function and mobility Pain Experiences of healthcare Support from others Involvement and understanding of care decisions Behavior and coping Fatigue and sleeping |
Qualitative study assessment 5/5 High quality (Appendix B) |
| 7 | Demierre | 2011 | Lausanne, Switzerland | To explore the patient illness experience from the moment the decision is made to perform arthroplasty. | Qualitative study, semistructured interviews | 24 total, 12 THAs | Mean age: 57 years | Not specified | Reported themes consisted of the following: Pain consequences generating limitations in functional, psychological, and social aspects. Ambivalence toward pain medication |
Qualitative study assessment 5/5 High quality (Appendix B) |
| 8 | Berg | 2019 | Sweden | To explore patients' perspective and experiences of undergoing THA and TKA surgery within the entire fast track care process. | Qualitative study, retrospective semistructured interviews | 24 total; 13 THAs | Age range: 44–85 years | 1 THR | The importance of person-centered care. Focus on management of daily life, rehabilitation, and recovery. Uncertainty over whether the patient's progress was normal and questions over unfulfilled expectations. |
Qualitative study assessment 3/5 (Appendix B) |
| 9 | Montin | 2002 | Finland | To explore the experience of THA patients of being a patient, care received, and of the healthcare organization. | Qualitative study, retrospective semistructured interviews | 17 THAs | Age range: 22–79 years | Not specified | Reported themes consisted of the following: Pain, rest, and mobility were major physical experiences |
Qualitative study assessment 2/5 (Appendix B) |
Note. OA = osteoarthritis; PROMs = Patient Reported Outcome Measures; THA = total hip arthoplasty; TJA = total joint arthoplasty; TKA = total knee arthoplasty.
Themes
Although unable to attribute specific themes to this review's patient demographic, four topics emerged as common themes in the included studies: (1) pain; (2) mobility and function; (3) relationships; and (4) patient expectations and education.
Pain
The experience of pain is reported as being diverse among participants in eight of the nine studies (Berg et al., 2009; Demierre et al., 2011; Fujita et al., 2006; Goodman et al., 2020; Montin et al., 2002; Singh et al., 2019; Sjøoveian & Leegaard, 2017; Strickland et al., 2017). Differing degrees of pain and methods of coping between participants were a common theme. Pain control medication was reported as both a necessity and a curse. Demierre et al. (2011) stated analgesics were viewed as necessary to maintain an acceptable QOL. Participants' concern with the amount of pain medication they were taking preoperatively was evident; seven of the nine studies (Berg et al., 2009; Demierre et al., 2011; Fujita et al., 2006; Goodman et al., 2020; Singh et al., 2019; Sjøoveian & Leegaard, 2017; Strickland et al., 2017) reported a decrease in required pain medication postsurgery as an important outcome to the participant. Strickland et al. (2017) and Demierre et al. (2011) discovered that participants viewed pain as part of the disease and accepted it as part of the recovery process. A THA participant (40 years old) described his concerns surrounding long-term use of pain medication; he was aware of the negative consequences and potential side effects that regular, long-term use of pharmaceutical analgesics could have.
I do not know if I'll ever be able to stop (taking) medication. I know also that the drugs I take, the pain relievers, are not without any negative consequences on my health either. Well for now, it works for me. But I know I would not take them my whole life. (Demierre et al., 2011; p. 553)
Sjøoveian and Leegaard (2017) used qualitative semistructured interviews to explore THA and TKA patient experiences of pain after discharge from hospital. This study was primarily focused on aspects of pain and rehabilitation in the immediate postoperative period and therefore information regarding priorities and other experience was not addressed. The study included one participant younger than 50 years, and no direct quotations or results were directly linked to this individual in the study reports.
Mobility and Function
Function and mobility were common concerns reported in the included studies, although often merged with other aspects of the participant experience. Fujita et al. (2006) reported the limitations of function and mobility directly influenced participants' ability to fulfill their role, either professionally or socially. This was echoed by Demierre et al. (2011), who reported that the inability to perform usual roles due to restricted function and mobility caused feelings of guilt and resulted in negative implications on participants' psychological well-being. The study stated that participants often attempted to hide their difficulties to avoid feelings of being “handicapped and stigmatized” (Demierre et al., 2011, p. 552). Three articles (Fujita et al., 2006; Demierre et al., 2017; Strickland et al., 2017) reported that an improvement in QOL due to recovery of function and mobility in the joint was a key theme in participants' recovery priorities and expectations. Singh et al. (2020) stated that improving function, mobility, and QOL were reported by participants as one of the chief purposes for undergoing surgery. The younger participants in the studies by Singh et al. (2020) and Goodman et al. (2020) ranked improving QOL (including aspects of social participation) much higher in importance than the older participant groups. Although exercise and sport were not highlighted as a theme from the nine included articles, one 40-year-old male reported missing physical exercise: “It has been since two years that, that I cannot go and run into the forest, what I do like very much, to go and pick mushrooms, or hike into the mountains” (Demierre et al., 2011, p. 553).
Relationships
Sjøoveian and Leegaard (2017) identified that support from family members was crucial in participants' recovery, whether through practical means or as emotional support. Strickland et al. (2017), Demierre et al. (2011), Montin et al. (2002), and Berg et al. (2019) named this support as a key factor; they also identified patient frustration due to the need to rely on others and feeling like a burden to friends and family. The younger groups in Goodman et al. (2020) reported feeling concerned that their friends and family would fail to understand their experience of chronic pain and disability. Lafosse et al. (2008) explored the impact on intimate sexual relationships and found that 19% of study participants reported hip pain having a significant effect on sexual activity, in turn, causing stress and tension in their relationship. Women were affected more than men in this regard and often took longer to commence sexual activity postsurgery than the male participants. A 40-year-old male was quoted: “Even with my wife, it is not easy in bed; I cannot do all these things anymore. So I tell myself, I am still young, I still want to enjoy life” (Demierre et al 2011, p. 553).
Patient Expectations and Education
Optimizing patient expectations and education was a common priority across the research. The younger nominal groups in Goodman et al. (2020) considered this topic as a high priority. An important part of holistic and patient-centered care is meaningful participation of patients and their families in decisions regarding their own care (Institute of Medicine, 2001). Strickland et al. (2017), Demierre et al. (2011), and Berg et al. (2019) highlighted the patient's desire to be involved in their own care and included in surgery decision-making. They concluded that shared decision-making between the patient and the clinician is imperative in developing an effective partnership between the surgeon and the patient. Montin et al. (2002) reported that knowing what the patients themselves consider the most important aspects of their care was crucial when supporting patients undergoing a THR, though did not elaborate further on this statement.
A short one-sentence quotation from a 44-year-old woman referring to the decision being made for surgery was featured: “I was terrified. Because just that day I didn't have so much pain. I thought, he won't believe me” (Berg et al 2019, p. 3).
As this is the only quotation or information attributed to this participant, we were left without any further clarification into her experience.
Demierre et al. (2011) found that the lack of control in the logistics of the surgery process—for example, waiting lists, timings, and potential for cancellations—negatively affected participants' psychological and emotional well-being. Four studies (Berg et al., 2019; Demierre et al., 2011; Lafosse et al., 2007; Sjøoveian & Leegaard, 2017) cited insufficient information from healthcare professionals regarding what to expect from recovery, prompting participants to seek information from other sources. Participants in Berg et al. (2019) reported comparing their rate of improvement and rehabilitation with that of others perceived as being in similar situations on social media. Berg et al. (2019) acknowledged that these sources could sometimes provide misleading information, resulting in unrealistic expectations.
Reporting Biases
With the uncertainty that the information available applies to the patient population of interest for this review, it is impossible to definitively address the question in this systematic review. Research utilizing PROMs and clinical and radiological outcome measures are frequently used (dependent on the author's position) as evidence that THA operations either satisfy or do not satisfy patient outcome priorities and needs. This systematic review demonstrates that no study to date has asked younger adults about their THA priorities and goals. Patient voices have become lost behind clinicians' and other healthcare professionals' assumptions of what constitutes a successful outcome; these assessments are too often based on the priorities, goals, and needs of a significantly older patient population undergoing the same intervention.
Only one of the studies included took place within the United Kingdom (Strickland et al., 2017), two studies took place in the United States (Goodman et al., 2020; Singh et al., 2020), one in Japan (Fujita et al., 2006), one in Sweden (Berg et al., 2019), one in Finland (Montin et al., 2002), one in Norway (Sjøoveian & Leegaard, 2017), one in France (LaFosse et al., 2008) and one in Switzerland (Demierre et al., 2011). Each of these countries has a different healthcare system, and this affects participants' experience of their illness and surgery, potentially affecting the data collected. Fujita et al. (2006) acknowledged that the wait for THA in Japan may be much shorter than that in other countries; consequently, the participant population in that study may not be representative of those in other countries, where longer waiting lists mean patients live with their symptoms for a significant period.
The retrospective method used in seven of the studies can also cause limitations on data collected. Retrospective interviews rely on participant memory of the experience, and memories can be unintentionally altered over time (Friedman & Winstanley, 1998); priorities that were important to participants at the time of the experience may not feel significant when retrospective interviews are conducted. Berg et al. (2019) recognized that the single retrospective interview 3 months postsurgery made it difficult for the participants to explore the full experience in depth. It is advisable that future research in this field take place during the diagnosis and treatment journey as opposed to retrospectively.
Notably, the researchers of the nine studies do not address their own bias or preconceptions on the subject. The analysis of qualitative data requires interpretation by the researcher. The concern is that the researcher's interpretation of a subject may be influenced by their experience and opinions, resulting in the introduction of bias (Cresswell & Cresswell, 2018) or, worse yet, invalid findings (Pathak et al., 2013). Qualitative research is sometimes criticized for this perceived lack of subjectivity; however, these criticisms are unwarranted if study weaknesses are adequately addressed and the limitations of the findings identified (Howard & Davis, 2002). The nine studies included in this literature review do not give any insight into the researchers' personal or professional experiences or how they addressed the potential for bias.
Certainty of Evidence
The included studies focused on different aspects of patient experiences with THA. All contained potentially relevant information regarding younger THA patient priorities and experiences; however, a significant constraint to effective evaluation of this information and the studies' findings is the failure of some included studies to attribute findings to specific age categories and/or to differentiate between THA and TKA patients.
Discussion
Although there is an absence of qualitative research on younger THA patient priorities, there is extensive literature available on the patient priorities that clinicians and researchers assume is important to this patient population. These general themes include return to work, sports and leisure activities, sexual activity, and caring responsibilities for young families. These topics are generally considered relevant to this age group (Borg et al., 2017; Kurtz et al., 2009; Malcolm et al., 2014; Tilbury et al., 2014); therefore, it is reasonable to assume they would also apply to the patient group in question.
It is estimated that between 15% and 45% of patients who undergo a THA are of working age (Kuijer et al., 2009; Tilbury et al., 2014). Hip conditions requiring THA are associated with decreased physical function, increased missed workdays, possible loss of employment, and subsequently reduced household income (Li et al., 2006). The annual cost of work-related musculoskeletal disorders is calculated by estimating both financial cost and “human cost” and is difficult to assess (Health and Safety Executive, 2018). Individuals experience the impact of the costs of ill health on their QOL, whereas the employer and society deal with the effects on loss of productivity and an increased need for healthcare, rehabilitation, and compensation (Bhattacharya, 2014; Bieleman et al., 2011; Sharif et al., 2016).
Employment has been shown to be important for both physiological and psychological well-being (Cook et al., 1982; Linn et al., 1985; Ross & Mirowsky, 1995); working has significant benefits on mental, emotional, and physical health, not to mention the financial benefits (Gignac et al., 2004; O'Brien & Feather, 1990; Waddell & Burton, 2006). Loss of employment can create an increased burden on both patients and their families (Tilbury et al., 2015). An early return to work following surgery has potential health benefits in addition to socioeconomic benefits (Baker et al., 2020).
In this synthesis, younger adults identified the negative impact on their social QOL as an important concern. Social isolation and the avoidance of social interaction due to chronic hip conditions are explored throughout the literature but are focused on the older patient (>65 years; Cattan et al., 2005; Iredell et al., 2004; Siviero et al., 2020). The results presented in this article indicate that this is a concern across all age groups and not exclusive to the older individual.
The impact of THA surgery on sexual activity appears to be little considered or understood by clinicians (Coradazzi et al., 2013; Dahm et al., 2004). Research on this topic suggests that THA is known to significantly affect sexual activity, whether through anxiety regarding specific positions or pain (Coradazzi et al., 2013; Klit, 2014). More than half of participants included in studies attributed their sexual difficulties directly to their chronic hip pain and disability (Currey, 1970; Issa et al., 2017; Todd et al., 1973). Total hip arthoplasty has a beneficial effect on sexual activity in younger adults, with this improvement being more frequently reported by women (Baldursson & Brattström, 1979; Lafosse et al., 2008; Meyer et al., 2003; Stern et al., 1991; Todd et al., 1973). The literature overwhelmingly supports clinicians discussing sexuality with hip surgery patients and suggests that education and further information on sexual activity postsurgery may decrease pain and facilitate self-awareness, self-confidence, and improved body image; this, in turn, can promote positive sexual health (Meiri et al., 2014).
Of the themes identified within the nine studies, several findings in this systematic review are also recognized and explored within wider literature on THA; these topics are relevant to all age groups and not exclusively specific to the younger patient and are presented in the following text.
In this synthesis, the effect and experience of pain and the loss of function and mobility emerged as dominant themes within the patient experience. The literature on THA endorses this finding. Indeed, THA was initially designed primarily to address low mobility and symptoms of pain in elderly patients (Charnley, 1961). Surgeons perform THA to address a variety of conditions, such as osteoarthritis, osteonecrosis, inflammatory arthritis, and congenital deformities (Adelani et al., 2013). These conditions and disabilities occur in differing frequencies within all age groups, and the primary symptoms experienced are widely reported as pain and limitation of function (Keeney et al., 2015). Consequently, inclusion of these themes within included studies was expected.
Current literature generally accepts that younger adults may engage or wish to engage in high activity levels postoperatively (Clohisy et al., 2008; Kinkel et al., 2009; Malcolm et al., 2014), although it is important to acknowledge that this generalization has varying levels of applicability to specific medical conditions (Keeney et al., 2015). Participation in exercise and sport is reported to be one of the least fulfilled expected outcomes after THA (Jourdan et al., 2012; Malcolm et al., 2014; Nilsdotter et al., 2003) and one of the more common reasons for dissatisfaction with a prosthetic joint (Mannion et al., 2020). Yet, it is one of the higher rated expectations in younger adults (Jourdan et al., 2012; Mancuso et al., 2009). A large number of younger adults return to recreational or impact sport after THA (Keeney et al., 2015; Prokopetz et al., 2012). It is not unreasonable to conclude that a younger person may aspire to higher functional outcomes than older patients, who may be willing to accept lower attained functional scores (Judge et al., 2012).
It is acknowledged that patients' concerns after THA differ significantly from the views of the clinician and that patients often feel their needs and views are underappreciated (Jourdan et al., 2012; Kinnaman & Mabrey, 2006). Our results indicate that shared decision-making between the patient and the clinician, and the active involvement of the patient in their care, can avoid this misalignment and enhance the therapeutic relationship between the surgeon and the patient.
Conclusion
This systematic review highlights the absence of quality qualitative data relating to the priorities and expectations of young adults when undergoing a THA. The necessity of further qualitative research in this field is evident. Without exploring these patients' own perceptions of their experience and priorities, we cannot be confident that the literature is not just presenting what clinicians and researchers assume is important to this patient population. As a result, orthopaedic nurses and other healthcare professionals may be uncertain that they are addressing patient needs and providing holistic, individualized, and patient-centered care. Further research is essential to identify what outcomes and expectations are important to young adults when undergoing a THA and how best to meet their priorities.
Acknowledgments
This literature review was supported by Milton Keynes University Hospital and Bournemouth University. Neither Milton Keynes University Hospital nor Bournemouth University had any involvement in the study design; in the collection, analysis, and interpretation of data; in writing of the manuscript; and in the decision to submit the manuscript for publication. Publication was sponsored by Milton Keynes University Hospital.
Appendix A. Search Strategy
| Details an example of searches that will be used: MEDLINE advanced search October 3, 2021 | |
|---|---|
| 1 | MH “Hip Prothesis” |
| 2 | MH “Arthroplasty, Replacement, Hip” |
| 3 | MH “Health Priorities” |
| 4 | MH “Quality of Life” |
| 5 | TI (Prior* OR Expectation* OR Importan* OR Goal* OR sport* OR exercise* OR sex OR pain OR function OR mobility OR relationship* OR perception* OR experience* OR view*) and AB (Prior* OR Expectation* OR Importan* OR Goal* OR sport* OR exercise* OR sex OR pain OR function OR mobility OR relationship* OR perception* OR experience* OR view*) |
| 6 | TI (middle age*) AND AB (middle age*) OR TI (less than 50) AND AB (less than 50) |
| 7 | TI (young patient*) AND AB (young patient*) |
| 8 | TI (qualitative OR phenomenolog*) AND AB (qualitative OR phenomenolog*)) |
| 9 | S1 OR S2 |
| 10 | S6 OR S7 |
| 11 | S3 OR S4 |
| 12 | S5 AND S9 |
| 13 | S5 AND S9 AND S10 |
| 14 | S8 AND S13 |
| 15 | S8 AND S12 |
| 16 | S5 AND S8 AND S9 |
| 17 | S9 AND S10 AND S11 |
Note. AB = word in abstract; MH = Medical Subject Heading; TI = word in title.
Appendix B. MMAT Assessment Tool: Screening Questions
| Ref | First Author | Year | Citation | SQ 1. Are There Clear Research Questions? | SQ 2. Do the Collected Data Allow to Address the Research Questions? | Mixed Methods/Qualitative |
|---|---|---|---|---|---|---|
| 1 | Lafosse | 2008 | Sexual function before and after primary total hip arthroplasty | Yes | Yes | Mixed methods |
| 2 | Sjøoveian | 2017 | Hip and knee arthroplasty—Patients' experiences of pain and rehabilitation after discharge from hospital | Yes | Yes | Qualitative |
| 3 | Singh | 2020 | When has a knee or hip replacement failed? A patient perspective | Yes | Yes | Qualitative |
| 4 | Goodman | 2020 | Patients' perspectives of outcomes after total knee and total hip arthroplasty: A nominal group study | Yes | Yes | Qualitative |
| 5 | Fujita | 2020 | Qualitative study of osteoarthritis patients' experience before and after total hip arthroplasty in Japan | Yes | Yes | Qualitative |
| 6 | Strickland | 2017 | Early recovery following lower limb arthroplasty: Qualitative interviewing with patients undergoing elective hip and knee replacement surgery. Initial phase in the development of a patient-reported outcome measure | Yes | Yes | Qualitative |
| 7 | Demierre | 2011 | The long and painful path towards arthroplasty: A qualitative study | Yes | Yes | Qualitative |
| 8 | Berg | 2019 | Fast-track program of elective joint replacement in hip and knee—Patients' experiences of the clinical pathway and care process | Yes | Yes | Qualitative |
| 9 | Montin | 2002 | The experiences of patients undergoing total hip replacement | Yes | Yes | Qualitative |
Mixed-Methods Assessment.
| Ref | First Author | Year | 5.1. Is There an Adequate Rationale for Using a Mixed Methods-Design to Address the Research Question? | 5.2. Are the Different Components of the Study Effectively Integrated to Answer the Research Question? | 5.3. Are the Outputs of the Integration of Qualitative and Quantitative Components Adequately Interpreted? | 5.4. Are Divergences and Inconsistencies Between Quantitative and Qualitative Results Adequately Addressed? | 5.5. Do the Different Components of the Study Adhere to the Quality Criteria of Each Tradition of the Methods Involved? | Comments |
|---|---|---|---|---|---|---|---|---|
| 1 | Lafosse | 2008 | Yes | No | No | No | No | Unsolicited comments not reported or attributed to particular patients |
Qualitative Methods Assessment.
| Ref | First Author | Year | 1.1. Is the Qualitative Approach Appropriate to Answer the Research Question? | 1.2. Are the Qualitative Data Collection Methods Adequate to Address the Research Question? | 1.3. Are the Findings Adequately Derived From the Data? | 1.4. Is the Interpretation of Results Sufficiently Substantiated by Data? | 1.5. Is There Coherence Between Qualitative Data Sources, Collection, Analysis, and Interpretation? | Comments |
|---|---|---|---|---|---|---|---|---|
| 2 | Sjøoveian | 2017 | Yes | Yes | Yes | Yes | Yes | Study focused on pain and rehabilitation retrospectively and little focus was accorded to priorities and goals moving forward. |
| 3 | Singh | 2020 | Yes | Yes | Yes | Yes | Yes | No separation between THA and TKA in nominal groups, so not clear if there was a difference between responses based on joint. |
| 4 | Goodman | 2020 | Yes | Yes | Yes | Yes | Yes | Not clear on what participants had TKA or THA, no separation of results, so unclear if any differences between the procedures. |
| 5 | Fujita | 2006 | Yes | Yes | Yes | Yes | Yes | Eligibility criteria excludes other diagnosis—Not representative of all patients undergoing a THA. |
| 6 | Strickland | 2017 | Yes | Yes | Yes | Yes | Yes | Age range is from 45 years upwards, unknown how many participants were younger than 50 years, or if those younger than 50 years were hip or knee operations. Age not identified as being a specific factor in certain themes. Quotations from participants not linked to their age or surgery site (i.e., hip or knee). |
| 7 | Demierre | 2011 | Yes | Yes | Yes | Yes | Yes | Small sample size did not differentiate between pathology and diagnosis; revision surgeries included in sample size. THA and TKA included in the sample. |
| 8 | Berg | 2019 | Yes | Can't tell | Can't tell | Yes | Yes | One quotation attributed to THR patient younger than 50 years. No other themes sorted by specific age group or surgery site. |
| 9 | Montin | 2002 | Yes | Yes | Can't tell | No | No | Limited reports of raw data, no reports of participant ages. No recognition of researchers own bias and assumptions in limitations. |
Note. THA = total hip arthoplasty; THR = total hip replacement; TKA = total knee arthoplasty.
Footnotes
Ethics Approval and Consent to Participate: HRA approval was not required for this study due to no identifiable or personal details being collected. This was confirmed by both the Health Research Authority and Milton Keynes Research and Development Department.
The authors declare they have no competing interests.
Contributor Information
Louise Mew, Email: Louise.mew@MKUH.NHS.UK.
Vanessa Heaslip, Email: v.a.heaslip@salford.ac.uk.
Tikki Immins, Email: timmins@bournemouth.ac.uk.
Thomas Wainwright, Email: twainwright@bournemouth.ac.uk.
REFERENCES
- Aalund P. K., Glassou E. N., Hansen T. B. (2017). The impact of age and preoperative health-related quality of life on patient-reported improvements after total hip arthroplasty. Clinical Interventions in Aging, 12, 1951–1956. 10.2147/CIA.S149493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adelani M., Keeney J., Palisch A., Fowler S., Clohisy J. (2013). Has total hip arthroplasty in patients 30 years and younger improved? A systematic review. Clinical Orthopaedics and Related Research, 471(8), 2595–2601. 10.1007/s11999-013-2975-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akobeng A. K. (2005). Principles of evidence-based medicine. Archives of Disease in Childhood, 90, 837–840. 10.1136/adc.2005.071761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Archibald G. (2003). Patients' experiences of hip fracture. Journal of Advanced Nursing, 44, 385–392. 10.1046/j.0309-2402.2003.02817.x [DOI] [PubMed] [Google Scholar]
- Baker P., Coole C., Drummond A., Khan S., McDaid C., Hewitt C., Kottam L., Ronaldson S., Coleman E., McDonald D. A., Nouri F., Narayanasamy M., McNamara I., Fitch J., Thomson L., Richardson G., Rangan A. (2020). Occupational advice to help people return to work following lower limb arthroplasty: The OPAL Intervention Mapping Study. Health Technology Assessment, 24(45), 1–408. 10.3310/hta24450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldursson H., Brattström H. (1979). Sexual difficulties and total hip replacement in rheumatoid arthritis. Scandinavian Journal of Rheumatology, 8(4), 214–216. 10.3109/03009747909114625 [DOI] [PubMed] [Google Scholar]
- Ben-Shlomo Y., Blom A., Boulton C., Brittain R., Clark E., Craig R., Dawson-Bowling S., Deere K., Esler C., Espinoza O., Goldberg A., Gregson C., Howard P., Hunt L., Jameson S., Jennison T., Judge A., Lawrence S., Lenguerrand E., Young E. (2020). The National Joint Registry 17th annual report 2020. National Joint Registry. [PubMed] [Google Scholar]
- Berg U., Berg M., Rolfson O., Erichsen-Andersson A. (2019). Fast-track program of elective joint replacement in hip and knee—Patients' experiences of the clinical pathway and care process. Journal of Orthopaedic Surgery and Research, 14(1), 186. 10.1186/s13018-019-1232-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bieleman H. J., Bierma-Zeinstra S. M., Oosterveld F. G., Reneman M. F., Verhagen A. P., Groothoff J. W. (2011). The effect of osteoarthritis of the hip or knee on work participation. Journal of Rheumatology, 38(9), 1835–1843. 10.3899/jrheum.101210 [DOI] [PubMed] [Google Scholar]
- Bhattacharya A. (2014). Costs of occupational musculoskeletal disorders (MSDs) in the United States. International Journal of Industrial Ergonomics, 44, 448–454. 10.1016/j.ergon.2014.01.008 [DOI] [Google Scholar]
- Borg I., Hertal G., Hermann D. (2017). Age and personal values: Similar value circles with shifting priorities. Psychology and Aging, 32(7), 636–641. 10.1037/pag0000196 [DOI] [PubMed] [Google Scholar]
- Braun V., Clarke V. (2013). Successful qualitative research: A practical guide for beginners. Sage. [Google Scholar]
- Cattan M., White M., Bond J., Learmouth A. (2005). Preventing social isolation and loneliness among older people: A systematic review of health promotion interventions. Ageing and Society, 25(1), 41–67. 10.1017/S0144686X04002594 [DOI] [PubMed] [Google Scholar]
- Charnley J. (1961). Arthroplasty of the hip: A new operation. The Lancet, 277(7187), 1129–1132. 10.1016/s0140-6736(61)92063-3 [DOI] [PubMed] [Google Scholar]
- Clohisy J., Carlisle J., Millis M. (2008). A systematic approach to the plain radiographic evaluation of the young adult hip. The Journal of Bone & Joint Surgery, American Volume, 90(Suppl. 4), 47–66. 10.2106/JBJS.H.00756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conner-Spady B. L., Marshall D. A., Hawker G. A., Bohm E., Dunbar M. J., Frank C., Noseworthy T. W. (2014). You'll know when you're ready: A qualitative study exploring how patients decide when the time is right for joint replacement surgery. BMC Health Services Research, 14, 454. 10.1186/1472-6963-14-454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook D. G., Cummins R. O., Bartley M. J., Shaper A. G. (1982). Health of unemployed middle-aged men in Great Britain. The Lancet, 1(8284), 1290–1294. 10.1016/s0140-6736(82)92852-5 [DOI] [PubMed] [Google Scholar]
- Coradazzi C., Bassini F., Tartali C. (2013). Hip replacement in the young: Return to sexuality, pregnancy and childbirth. Scienza Riabilitativa, 15(2). 36–45. https://doi.org/A331080128/HRCA?u [Google Scholar]
- Cresswell J. W., Cresswell J. D. (2018). Research design: Qualitative, quantitative, and mixed methods approaches. Sage. [Google Scholar]
- Crowninshield R. D., Rosenberg A. G., Sporer S. M. (2006). Changing demographics of patients with total joint replacement. Clinical Orthopaedics and Related Research, 443, 266–272. 10.1097/01.blo.0000188066.01833.4f [DOI] [PubMed] [Google Scholar]
- Currey H. L. (1970). Osteoarthrosis of the hip joint and sexual activity. Annals of the Rheumatic Diseases, 29(5), 488. 10.1136/ard.29.5.488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahm D. L., Jacofsky D., Lewallen D. G. (2004). Surgeons rarely discuss sexual activity with patients after THA: A survey of members of the American Association of Hip and Knee Surgeons. Clinical Orthopaedics and Related Research (1976–2007), 428, 237–240. [PubMed] [Google Scholar]
- Demierre M., Castelao E., Piot-Ziegler C. (2011). The long and painful path towards arthroplasty: A qualitative study. Journal of Health Psychology, 16(4), 549–560. 10.1177/1359105310385365 [DOI] [PubMed] [Google Scholar]
- EBSCO. (2019). CINAHL Plus: The CINAHL Index Plus Additional Nursing and Allied Health Literature and Resources. Retrieved September 2, 2021, from https://www.ebscohost.com/nursing/products/cinahl-databases/cinahl-plus [Google Scholar]
- Friedman and Winstanley. (1998), Changes in subjective properties of autobiographical memories with the passage of time. Memory, 6(4), 367–381. 10.1080/741942606 [DOI] [PubMed] [Google Scholar]
- Fujita K., Makimoto K., Hotokebuchi T. (2006). Qualitative study of osteoarthritis patients' experience before and after total hip arthroplasty in Japan. Nursing and Health Sciences, 8, 81–87. 10.1111/j.1442-2018.2006.00253.x [DOI] [PubMed] [Google Scholar]
- Gignac M. A., Badley E. M., Lacaille D., Cott C. C., Adam P., Anis A. H. (2004). Managing arthritis and employment: Making arthritis-related work changes as a means of adaptation. Arthritis and Rheumatology, 51, 909–916. 10.1002/art.20822 [DOI] [PubMed] [Google Scholar]
- Gooberman-Hill R., Fox R., Chesser T. J. S. (2011). What can qualitative approaches bring to trauma outcome research? Injury, International Journal of Care of the Injured, 42, 321–323. 10.1016/j.injury.2011.01.021 [DOI] [PubMed] [Google Scholar]
- Goodman S., Mehta B., Mirza S., Figgie M., Alexiadas M., Rodriguez J., Sculco P., Parks M., Singh J. (2020). Patients' perspectives of outcomes after total knee and total hip arthroplasty: A nominal group study. BMC Rheumatology, 4, 3. 10.1186/s41927-019-0101-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health and Safety Executive. (2018). Costs to Great Britain of workplace injuries and new cases of work-related ill health—2016/17. Retrieved February 24, 2022, from www.hse.gov.uk/statistics/cost.htm [Google Scholar]
- Hong Q. N., Fàbregues S., Bartlett G., Boardman F., Cargo M., Dagenais P., Gagnon M. P., Griffiths F., Nicolau B., O'Cathain A., Rousseau M. C., Vedel I., Pluye P. (2018). The Mixed Methods Appraisal Tool (MMAT) Version 2018 for information professionals and researchers. Education for Information, 34(4), 285–291. 10.3233/EFI-180221 [DOI] [Google Scholar]
- Howard D., Davis P. (2002). The use of qualitative research methodology in orthopaedics—Tell it as it is. Journal of Orthopaedic Nursing, 6, 135–139. 10.1016/S1361-3111(02)00051-1 [DOI] [Google Scholar]
- Institute of Medicine. (2001). Crossing the quality chasm: A new health system for the 21st century. National Academies Press. [PubMed] [Google Scholar]
- Iredell H., Grenade L., Nedwetzky A., Collins J., Howat P. (2004). Reducing social isolation amongst older people—Implications for health professionals. Geriaction, 22(1), 13–20. [Google Scholar]
- Issa K., Pierce T., Brothers A., Festa A., Scillia A., Mont M. (2017). Sexual activity after total hip arthroplasty: A systematic review of the outcomes. The Journal of Arthroplasty, 32(1), 336–340. 10.1016/j.arth.2016.07.052 [DOI] [PubMed] [Google Scholar]
- Janes G., Serrant L. (2018). Fragility hip fracture in the under 60s: A qualitative study of recovery experiences and the implications for nursing. International Journal of Orthopaedic and Trauma Nursing, 2(1), 3. Retrieved July 29, 2022, from https://www.imedpub.com/articles-pdfs/fragility-hip-fracture-in-the-under-60s-a-qualitative-study-of-recovery-experiences-and-the-implications-for-nursing.pdf [Google Scholar]
- Jenson K. (2019). 7 Steps to the perfect PICO search. Evidence Based Nursing Practice. Retrieved August 2, 2022, from 7-Steps-to-the-Perfect-PICO-Search-White-Paper_0.pdf [Google Scholar]
- Jourdan C., Poiraudeau S., Descamps S., Nizard R., Hamadouche M., Anract P., Boisgard S., Galvin M., Ravaud P. (2012). Comparison of patient and surgeon expectations of total hip arthroplasty. PLoS One, 7(1), e30195. 10.1371/journal.pone.0030195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Judge A., Arden N., Kiran A., Price A., Javaid M. K., Beard D., Murray D., Field R. E. (2012). Interpretation of patient-reported outcomes for hip and knee replacement surgery. Identification of thresholds associated with satisfaction with surgery. The Journal of Bone & Joint Surgery, British Volume, 94(3), 412–418. 10.1302/0301-620X.94B3.27425 [DOI] [PubMed] [Google Scholar]
- Kamath A. F., Sheth N., Holsakar H., Babatunde O., Lee G., Nelson C. (2012). Modern total hip arthroplasty in patients younger than 21 years. The Journal of Arthroplasty, 27(3), 402–408. 10.1016/j.arth.2011.04.042 [DOI] [PubMed] [Google Scholar]
- Keeney J., Nunley R., Baca G., Clohisy J. (2015). Are younger patients undergoing THA appropriately characterized as active? Clinical Orthopaedics and Related Research, 473(3), 1083–1092. 10.1007/s11999-014-3952-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinkel S., Wollmerstedt N., Kleihans J., Hendrich C., Heisel C. (2009). Patient activity after total hip arthroplasty declines with advancing age. Clinical Orthopaedics and Related Research, 467(8), 2053–2058. 10.1007/s11999-009-0756-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinnaman K., Mabrey J. D. (2006). Arthroscopy of the hip joint. Orthopaedic Nursing, 25(2), 93–97. 10.1097/00006416-200603000-00003 [DOI] [PubMed] [Google Scholar]
- Klit J. (2014). Results of total joint arthroplasty and joint preserving surgery in younger patients evaluated by alternative outcome measures. Danish Medical Journal, 61(4), B4836. [PubMed] [Google Scholar]
- Knight S. R., Aujla R., Biswas S. P. (2011). Total hip arthroplasty—Over 100 years of operative history. Orthopedic Reviews, 3(2), e16. 10.4081/or.2011.e16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuijer P. P., de Beer M. J., Houdijk J. H., Frings-Dresen M. H. (2009). Beneficial and limiting factors affecting return to work after total knee and hip arthroplasty: A systematic review. Journal of Occupational Rehabilitation, 19(4), 375–381. 10.1007/s10926-009-9192-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar A., Bloch B., Esler C. (2017). Trends in total hip arthroplasty in young patients—Results from a regional register. HIP International, 27(5), 443–448. 10.5301/hipint.5000485 [DOI] [PubMed] [Google Scholar]
- Kurtz S. M., Lau E., Ong K., Zhao K., Kelly M., Bozic K. J. (2009). Future young patient demand for primary and revision joint replacement: National projections from 2010 to 2030. Clinical Orthopaedics and Related Research, 467(10), 2606–2612. 10.1007/s11999-009-0834-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lafosse J. M., Tricore J. L., Chiron P., Puget J. (2008). Sexual function before and after primary total hip arthroplasty. Joint Bone Spine, 75(2), 189–194. 10.1016/j.jbspin.2007.05.006 [DOI] [PubMed] [Google Scholar]
- Larsson A., Rolfson O., Kärrholm J. (2019). Evaluation of forgotten joint score in total hip arthroplasty with Oxford Hip Score as reference standard. Acta Orthopaedica, 90(3), 253–257. 10.1080/17453674.2019.1599252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Gignac M. A., Anis A. H. (2006). The indirect costs of arthritis resulting from unemployment, reduced performance, and occupational changes while at work. Medical Care, 44(4), 304–310. 10.1097/01.mlr.0000204257.25875.04 [DOI] [PubMed] [Google Scholar]
- Linden A. H., Hönekopp J. (2021). Heterogeneity of research results: A new perspective from which to assess and promote progress in psychological science. Perspectives on Psychological Science, 16(2), 358–376. 10.1177/1745691620964193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linn M. W., Sandifer R., Stein S. (1985). Effects of unemployment on mental and physical health. American Journal of Public Health, 75(5), 502–506. 10.2105/ajph.75.5.502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahomed N. N., Liang M. H., Cook E. F. (2002). The importance of patient expectations in predicting functional outcomes after total joint arthroplasty. Journal of Rheumatology, 29(6), 1273–1279. [PubMed] [Google Scholar]
- Malcolm T. L., Szubski C. R., Nowacki A. S., Klika A. K., Iannotti J. P., Barsoum W. K. (2014). Activity levels and functional outcomes of young patients undergoing total hip arthroplasty. Orthopedics, 37(11), e983–e992. 10.3928/01477447-20141023-55 [DOI] [PubMed] [Google Scholar]
- Mancuso C., Jout J., Salvati E., Sculco T. (2009). Fulfilment of patients' expectations for total hip arthroplasty. The Journal of Bone & Joint Surgery, American Volume, 91(9), 2073–2078. 10.2106/JBJS.H.01802 [DOI] [PubMed] [Google Scholar]
- Mannion A., Nauer S., Arsoy D., Impellizzeri F., Leunig M. (2020). The association between comorbidity and the risks and early benefits of total hip arthroplasty for hip osteoarthritis. The Journal of Arthroplasty, 35(9), 2480–2487. 10.1016/j.arth.2020.04.090 [DOI] [PubMed] [Google Scholar]
- Markatos K., Savvidou O. D., Foteinou A., Kosmadaki S., Trikoupis I., Goumenos S. D., Papagelopoulos P. J. (2020). Hallmarks in the history and development of total hip arthroplasty. Surgical Innovation, 27(6), 691–694. 10.1177/1553350620947209 [DOI] [PubMed] [Google Scholar]
- Meiri R., Rosenbaum T. Y., Kalichman L. (2014). Sexual function before and after total hip replacement: Narrative review. Sexual Medicine, 2(4), 159–167. 10.1002/sm2.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer H., Stern R., Fusetti C., Salsano F., Campana A., Hoffmeyer P. (2003). Sexual quality-of-life after hip surgery. Journal of Orthopaedics and Traumatology, 4(1), 21–25. 10.1007/s101950300003 [DOI] [Google Scholar]
- Montin L. Suominen T. Leino-Kilpi H. (2002). The experiences of patients undergoing total hip replacement. Journal of Orthopaedic Nursing, 6(1), 23–29. [Google Scholar]
- Munn Z., Stern C., Aromataris E., Lockwood C., Jordan Z. (2018). What kind of systematic review should I conduct? A proposed typology and guidance for systematic reviewers in the medical and health sciences. BMC Medical Research Methodology, 18(1), 5. 10.1186/s12874-017-0468-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nam D., Nunley R. M., Sauber T. J., Johnson S. R., Brooks P. J., Barrack R. L. (2015). Incidence and Location of pain in young, active patients following hip arthroplasty. The Journal of Arthroplasty, 30(11), 1971–1975. 10.1016/j.arth.2015.05.030 [DOI] [PubMed] [Google Scholar]
- National Joint Registry (NJR). (2019). National Joint Registry: 16th annual report. Retrieved November 20, 2021, from www.NJRcentre.org.uk [Google Scholar]
- Nilsdotter A., Petersson F., Roos E., Lohmander L. (2003). Predictors of patient relevant outcomes after total hip replacement for osteoarthritis; A prospective study. Annals of the Rheumatic Diseases, 62(10), 923–930. 10.1136/ard.62.10.923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Brien G. E., Feather N. T. (1990). The relative effects of unemployment and quality of employment on the affect, work values and personal control of adolescents. Journal of Occupational Psychology, 63, 151–165. 10.1111/j.2044-8325.1990.tb00517.x [DOI] [Google Scholar]
- Page M. J., McKenzie J. E., Bossuyt P. M., Boutron I., Hoffmann T. C., Mulrow C. D., Shamseer L., Tetzlaff J. M., Akl E. A., Brennan S. E., Chou R., Glanville J., Grimshaw J. M., Hróbjartsson A., Lalu M. M., Li T., Loder E. W., Mayo-Wilson E., McDonald S., Moher D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pathak V., Jana B., Kaira S. (2013). Qualitative research. Perspectives in Clinical Research, 4(3), 192. 10.4103/2229-3485.115389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popay J., Roberts H., Sowden A., Petticrew M., Arai L., Rodgers M., Britten N., Roen K., Duffy S., (2006). Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC Methods Programme (Version 1, p. b92). Lancaster University. [Google Scholar]
- Prokopetz J., Losina E., Bliss R., Wright J., Baron J., Katz J. (2012). Risk factors for revision of primary total hip arthroplasty: A systematic review. BMC Musculoskeletal Disorders, 13, 251. 10.1186/1471-2474-13-251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapport F., Storey M., Porter A., Snooks H., Jones K., Peconi J., Sanchez A., Siebert S., Thorne K., Clement C., Russell I. (2013). Qualitative research within trials: Developing a standard operating procedure for a clinical trials unit. Trials, 14, 54. 10.1186/1745-6215-14-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravi B., Croxford R., Reichmann W. M., Losina E., Katz J. N., Hawker G. A. (2012). The changing demographics of total joint arthroplasty recipients in the United States and Ontario from 2001 to 2007. Best Practice and Research in Clinical Rheumatology, 26(5), 637–647. 10.1016/j.berh.2012.07.014 [DOI] [PubMed] [Google Scholar]
- Ross C. E., Mirowsky J. (1995). Does employment affect health? Journal of Health and Social Behavior, 1, 230–243. 10.2307/2137340 [DOI] [PubMed] [Google Scholar]
- Sandelowski M., Leeman J., Knafl K., Crandell J. L. (2013). Text-in-context: A method for extracting findings in mixed-methods mixed research synthesis studies. Journal of Advanced Nursing, 69(6), 1428–1437. 10.1111/jan.12000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott C. E. H., MacDonald D. J., Howie C. R. (2019). “Worse than death” and waiting for a joint arthroplasty. The Bone & Joint Journal, 101-B(8), 941–950. 10.1302/0301-620x.101b8.bjj-2019-0116.r1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharif B., Garner R., Sanmartin C., Flanagan W. M., Hennessy D., Marshall D. A. (2016). Risk of work loss due to illness or disability in patients with osteoarthritis: A population-based cohort study. Rheumatology, 55(5), 861–868. 10.1093/rheumatology/kev428 [DOI] [PubMed] [Google Scholar]
- Singh J., Mehta B., Mirza S., Figgie M., Sculco P., Parks M., Goodman S. (2020). When has a hip or knee replacement failed? A patient perspective. The Journal of Rheumatology, 48(3), 447–453. 10.3899/jrheum.191024 [DOI] [PubMed] [Google Scholar]
- Siviero P., Veronese N., Smith T., Stubbs B., Limongi F., Zambon S., Dennison E. M., Edwards M., Cooper C., Timmermans E. J., van Schoor N. M., van der Pas S., Schaap L. A., Denkinger M. D., Peter R., Herbolsheimer F., Otero Á., Castell M. V., Pedersen N. L., ... EPOSA Research Group. (2020). Association between osteoarthritis and social isolation: Data from the EPOSA study. Journal of the American Geriatrics Society, 68(1), 87–95. 10.1111/jgs.16159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sjøveian A., Leegaard M. (2017). Hip and knee arthroplasty—Patient's experiences of pain and rehabilitation after discharge from hospital. International Journal of Orthopaedic and Trauma Nursing, 27, 28–35. 10.1016/j.ijotn.2017.07.001 [DOI] [PubMed] [Google Scholar]
- Stern S. H., Fuchs M. D., Ganz S. B., Classi P., Sculco T. P., Salvati E. A. (1991). Sexual function after total hip arthroplasty. Clinical Orthopaedics and Related Research, (269), 228–235. [PubMed] [Google Scholar]
- Strickland L., Kelly L., Hamilton T., Murray D., Pandit H., Jenkinson C. (2017). Early recovery following lower limb arthroplasty: Qualitative interviews with patients undergoing elective hip and knee replacement surgery. Initial phase in the development of a patient-reported outcome measure. Journal of Clinical Nursing, 27(13–14), 2598–2608. 10.1111/jocn.14086 [DOI] [PubMed] [Google Scholar]
- Tilbury C., Leichtenberg C. S., Tordoir R. L., Holtslag M. J., Verdegaal S. H., Kroon H. M. (2015). Return to work after total hip and knee arthroplasty: Results from a clinical study. Rheumatology International, 35, 2059–2067. 10.1007/s00296-015-3311-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tilbury C., Schaasberg W., Plevier J. W., Fiocco M., Nelissen R., Vliet Vlieland T. (2014). Return to work after total hip and knee arthroplasty: A systematic review, Rheumatology, 53(3), 512–525. 10.1093/rheumatology/ket389 [DOI] [PubMed] [Google Scholar]
- Todd R. C., Lightowler C. D. R., Harris J. (1973). Low friction arthroplasty of the hip joint and sexual activity. Acta Orthopaedica Scandinavica, 44(6), 690–693. 10.3109/17453677308989108 [DOI] [PubMed] [Google Scholar]
- Van Rooyen D., Jordan P. (2013). Foundations of nursing practice: Fundamentals of holistic care. Elsevier. [Google Scholar]
- Waddell G., Burton K. A. (2006). Is work good for your health and well-being? The Stationery Office. [Google Scholar]
- Wang T., Sun J. Y., Zhao X. J., Yin H. (2016). Ceramic-on-ceramic bearings total hip arthroplasty in young patients. Arthroplasty Today, 2(4), 205–209. 10.1016/j.artd.2016.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright J. G., Young N. L., Waddell J. P. (2000). The reliability and validity of the self-reported patient-specific index for total hip arthroplasty. The Journal of Bone & Joint Surgery, American Volume, 82(6), 829–837. 10.2106/00004623-200006000-00009 [DOI] [PubMed] [Google Scholar]
- Zidén L., Scherman M. H., Wenestam C. G. (2010). The break remains—Elderly peoples experiences of a hip fracture 1 year after discharge. Disability and Rehabilitation, 32(2), 103–113. 10.3109/09638280903009263 [DOI] [PubMed] [Google Scholar]