Lung cancer is the leading cause of cancer mortality worldwide and is often diagnosed in the advanced stages with a reduced likelihood of curative treatment and survival.1 Lung cancer disproportionately affects socioeconomically deprived groups with higher incidence and worse outcomes, partly due to high rates of smoking and occupational exposures.2
The clinical effectiveness of lung cancer screening (LCS) with low-dose CT (LDCT) has been established with improved lung cancer outcomes. A recent meta-analysis reported a pooled relative reduction in lung cancer- specific mortality of 0.84 (95% confidence interval = 0.76 to 0.92).3 Accordingly, in June 2022, the UK National Screening Committee recommended LCS for high-risk adults based on age and smoking history.4
The proposed model of implementation is likely to be informed by the NHS England Targeted Lung Health Check (TLHC) model, which has generated essential evidence regarding the practicalities of delivering LCS.5 TLHCs identify high-risk cohorts based on age and smoking history, inviting them for triage risk assessment. Patients exceeding the risk threshold are invited for an LDCT scan. Unlike breast, bowel, and cervical cancer screening programmes that invite all patients within a particular age range, risk stratification by age and smoking history presents further challenges for LCS implementation.
We present important considerations regarding the potential role of general practice in LCS. Expertise within primary care and the unique position of general practice within communities could address these challenges to facilitate the successful implementation of a new LCS programme and support equitable and informed participation.
CHALLENGES FOR GENERAL PRACTICE
Utilising electronic health records (EHRs) to identify screening-eligible patients
LCS programmes will primarily rely on smoking data held in primary care EHRs to identify the high-risk population (aged 55–74 years, with a history of smoking within 20 years). However, smoking codes within EHRs were not intended for this purpose and vary in validity and completeness.6 Without improving reliability of EHR smoking codes, the programme risks excluding patients who may be eligible for LDCT screening, calling for strategies and tools to improve smoking data quality.7 General practice will play a key role in facilitating equitable and inclusive access to LDCT screening by helping to build accurate smoking EHR data. Self-referral and inviting patients with a missing smoking code to triage risk assessment could potentially supplement strategies to update EHRs, enhance accessibility, and minimise risks associated with patient identification.
Achieving equitable and informed participation in LCS
Participation in LCS is variable, with uptake rates of 16% among eligible US adults and 35%–53% in the UK TLHCs.7,8 In the US, participation is impacted by inconsistent implementation, confusion around eligibility, variable insurance reimbursement, and the delayed endorsement of the American Academy of Family Physicians.8 Additionally, inequalities in LCS participation exist, with lower rates of participation among individuals from low socioeconomic backgrounds with longstanding smoking histories, while emerging evidence signals additional ethnic and regional variation.5
Behavioural influences on LCS non- participation include low awareness of LCS, cancer fear and fatalism, smoking- related stigma, beliefs about eligibility for screening, experiences of poor lung cancer outcomes in social networks, and complex life circumstances.9 Participation may also be adversely affected by the variable quality of information that is often used to support informed decision making and preparation for abnormal LCS results.
Addressing issues of equitable participation may improve the cost-effectiveness and clinical effectiveness of LCS. Behavioural interventions including GP endorsement, pre-screening reminders, and personalised invitations have been shown to increase cancer screening uptake among low socioeconomic groups.11 Careful consideration must be taken to mitigate existing inequalities in accessing LCS, given that this remains a significant issue in other cancer screening programmes. Traditionally, GPs have played a vital role in reducing barriers to screening participation and providing an accessible setting for person-centred care and education. They are therefore in a unique position to support equitable and informed participation in LCS.
Capacity within primary care to support LCS
GP-led initiatives including practice letters, telephone reminders, and counselling appointments would place additional demands on already constrained capacity. For example, should administrative staff be allocated time to call patients and explain the programme? Should practices document and follow up on patients who have declined LCS invitations? Automated reports around eligibility and those who have not participated could facilitate some of this. Practices may need to be incentivised to undertake such work both in terms of staff engagement and backfill for administrative time. Finally, the role of general practice in the follow-up of incidental findings is yet to be established. It is arguably inappropriate for the responsibility for surveillance to fall to general practice, highlighting the need for coordination with secondary care services.
Incidental findings and overdiagnosis
The potential for additional activity arising from abnormal LCS results, including incidental LDCT findings, must be considered. The National Lung Screening Trial (NLST) reported 33.8% of individuals had ‘significant’ incidental findings, which included non-pulmonary masses and many other radiological findings requiring further specialist review.12 Given the extensive understanding we have of the significant incidental findings that can be expected to arise, it is imperative to establish effective pathways to facilitate referrals and prevent delaying patient care, missed diagnoses, and undue GP workload. However, uncertainties regarding the benefits of follow-up for incidental findings (for example, emphysema, coronary artery calcification, interstitial disease, aortic disease, and adrenal masses) should be acknowledged and will require adequate resourcing to support shared decision making with patients. Finally, LCS raises the potential for overdiagnosis. Given that a proportion of LDCT-detected cancers may never progress to symptomatic disease, informed decision making is essential. Discussing the numbers needed to screen and harm using decision support tools (Figure 1) may aid informed decision making.10
Figure 1.
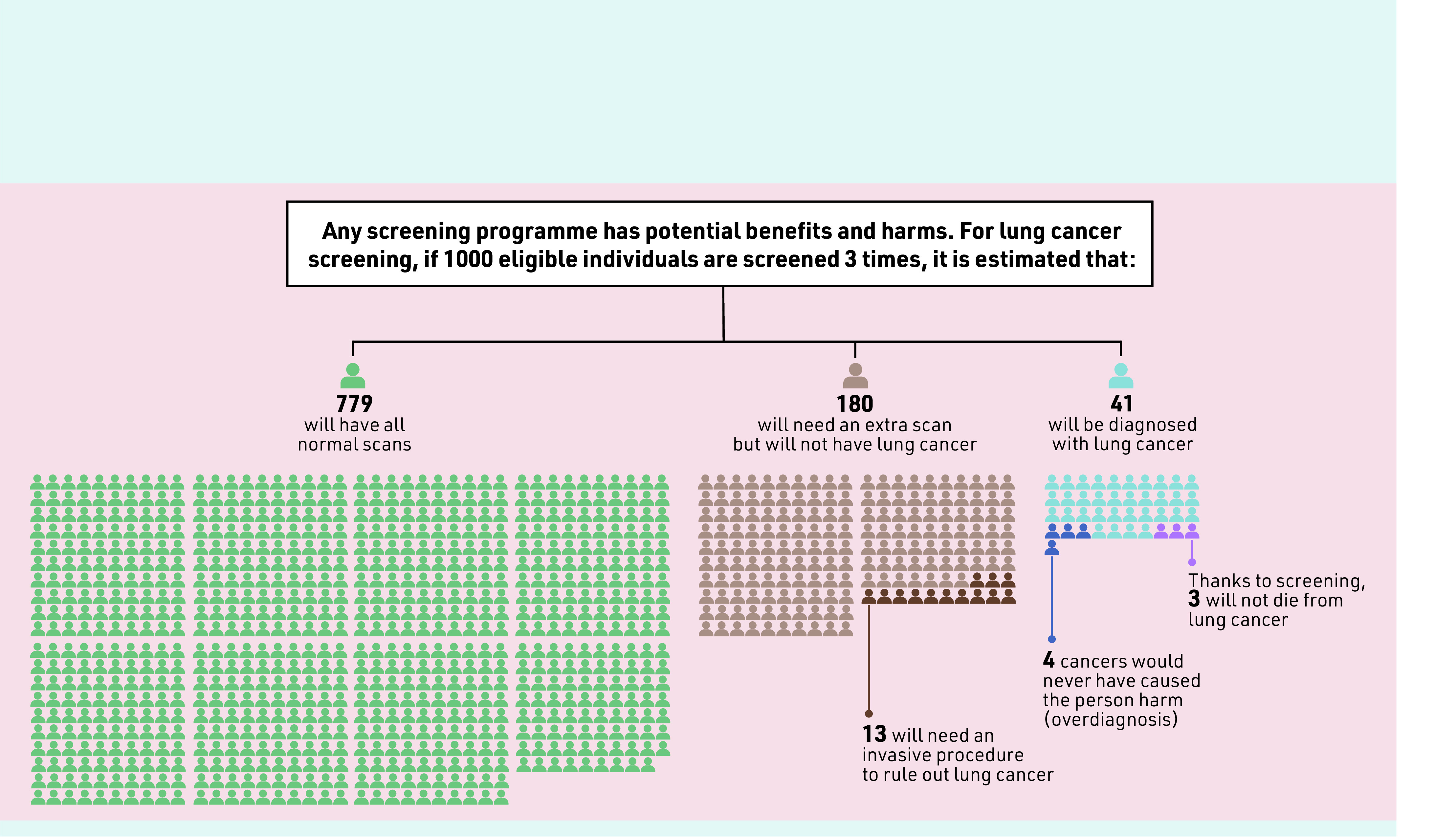
A 1000-person tool for lung cancer screening, based on the National Lung Screening Trial. Numbers needed to treat and harm incorporating other trials are available.10 Reproduced with permission from the World Health Organization International Agency for Research on Cancer.
FUTURE OF LCS AND GENERAL PRACTICE
With the expansion of the TLHC programme, LCS will soon be available to patients in the UK. GPs have a critical role in contributing to the programme’s success by facilitating inclusive identification and invitation of high-risk patients, and supporting equitable and informed participation. However, the implications for GPs must be reasonable, achievable, and explicitly acknowledged given the current workload crisis in primary care. Moreover, there must be effective communication with primary care and the programmes regarding results, scheduled screens, and participation. Screening promises to contribute to improvements in lung cancer outcomes, but, to ensure those at greatest risk are reached, general practice must be considered as an active partner. This will require envisaging a clear and positive role for general practice in screening along with sincere engagement with the profession on the case for screening and acknowledgement of resulting workload implications.
Acknowledgments
Thanks to Matthew Callister and Matthew Thompson for their helpful comments in drafting this article.
Provenance
Commissioned; peer reviewed.
Competing interests
Stephen H Bradley is a member of the lung screening standards development group for England (Office for Health Improvement and Disparities) and is the clinical lead for cancer for the Leeds office of the West Yorkshire Integrated Care Board. The views expressed are those of the authors and do not necessarily reflect those of employers or affiliated organisations.
REFERENCES
- 1.Knight SB, Crosbie PA, Balata H, et al. Progress and prospects of early detection in lung cancer. Open Biol. 2017;7(9):170070. doi: 10.1098/rsob.170070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vaccarella S, Georges D, Bray F, et al. Socioeconomic inequalities in cancer mortality between and within countries in Europe: a population-based study. Lancet Reg Health Eur. 2022;25:100551. doi: 10.1016/j.lanepe.2022.100551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Field JK, Vulkan D, Davies MPA, et al. Lung cancer mortality reduction by LDCT screening: UKLS randomised trial results and international meta-analysis. Lancet Reg Health Eur. 2021;10:100179. doi: 10.1016/j.lanepe.2021.100179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.UK National Screening Committee . Lung cancer. London: UKNSC; 2022. [Google Scholar]
- 5.Dickson JL, Hall H, Horst C, et al. Uptake of invitations to a lung health check offering low-dose CT lung cancer screening among an ethnically and socioeconomically diverse population at risk of lung cancer in the UK (SUMMIT): a prospective, longitudinal cohort study. Lancet Public Health. 2023;8(2):e130–e140. doi: 10.1016/S2468-2667(22)00258-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dickson JL, Hall H, Horst C, et al. Utilisation of primary care electronic patient records for identification and targeted invitation of individuals to a lung cancer screening programme. Lung Cancer. 2022;173:94–100. doi: 10.1016/j.lungcan.2022.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Dowd EL, Lee RW, Akram AR, et al. Defining the road map to a UK national lung cancer screening programme. Lancet Oncol. 2023;24(5):e207–e218. doi: 10.1016/S1470-2045(23)00104-3. [DOI] [PubMed] [Google Scholar]
- 8.Rivera MP, Katki HA, Tanner NT, et al. Addressing disparities in lung cancer screening eligibility and healthcare access. An official American Thoracic Society statement. Am J Respir Crit Care Med. 2020;202(7):e95–e112. doi: 10.1164/rccm.202008-3053ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Quaife SL, Marlow LAV, McEwen A, et al. Attitudes towards lung cancer screening in socioeconomically deprived and heavy smoking communities: informing screening communication. Health Expect. 2017;20(4):563–573. doi: 10.1111/hex.12481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jonas DE, Reuland DS, Reddy SM, et al. Screening for lung cancer with low-dose computed tomography: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2021;325(10):971–987. doi: 10.1001/jama.2021.0377. [DOI] [PubMed] [Google Scholar]
- 11.Duffy SW, Myles JP, Maroni R, Mohammad A. Rapid review of evaluation of interventions to improve participation in cancer screening services. J Med Screen. 2017;24(3):127–145. doi: 10.1177/0969141316664757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gareen IF, Gutman R, Sicks J, et al. Significant incidental findings in the National Lung Screening Trial. JAMA Intern Med. 2023 doi: 10.1001/jamainternmed.2023.1116.. [DOI] [PMC free article] [PubMed] [Google Scholar]


