Abstract
Background:
Measuring the health of the population is of great significance to the development of a region. We aimed to estimate the population, probability of death, and quality of life in western China.
Methods:
We calculated the age-specific mortality rate and prevalence rate of diseases and injuries using the Full Population Database and the Home Page of Inpatient Medical Record. We used multiple interpolation methods to insert missing information from the death data and the model of Kannisto to adjust the mortality rate for elderly individuals. The age-specific prevalence rate of diseases and injuries was adjusted according to the standard ratio of age and methods of equal proportional allocation. Life expectancy was calculated by a life table, and the quality of life was estimated using the Sullivan method.
Results:
The total population continued to increase in 2015 to 2019 in the Shaanxi Province, China. The mortality rate of children under five has improved, and the mortality rate of people over 65 is decreasing year by year. Life expectancy increased from 74.66 years in 2015 to 77.19 years in 2019. Even with the total risk of disease and injury, the health-adjusted life expectancy increased by 1.90 years within 5 years, and the number of unhealthy years significantly improved. Health-adjusted life expectancy increased by 1.75 years when only considered the ten major disease systems (tumors; endocrinology, nutrition and metabolism; mental and behavioral disorders; nervous system; sensory diseases; circulatory system; respiratory system; digestive system; genitourinary system; musculoskeletal system and connective tissue), and the number of unhealthy years increased slightly.
Conclusions:
In the past five years, Shaanxi Province has made progress in improving life expectancy and controlling the development of chronic diseases. It is necessary to take specific preventive measures and improve the quality of basic public health services.
Keywords: China, Chronic disease, Life expectancy, Mortality rate, Quality of life
Introduction
Population health is an important indicator of the prosperity and development of a country and region. Life expectancy (LE) is an important indicator for evaluating the health of the population and measures the number of years the population can survive.[1,2] Health-adjusted life expectancy, also called healthy life expectancy, is a measure of the quality of life (QoL) of individuals in a region; the prevalence of diseases and injuries are considered when calculating life expectancy. Measuring QoL is of great significance for evaluating the level of socioeconomic development and health service of a country or region and comprehensively measuring the health of the population.[3]
Shaanxi Province, a capital of ancient China and a province that has developed rapidly even compared with the whole country in modern time in recent years, is located in the western part of China. According to data released by the National Health Commission of China, LE in China increased from 68.55 years in 1990 to 74.85 years in 2010, and the LE in Shaanxi Province grew from 67.40 years to 74.68 years, which is an average level of development status that is comparable to the overall level of China.[4] Most research on QoL states that the population health in Beijing, Shanghai, and Guangzhou has surpassed the average level of the Chinese population; the population may even experience the same QoL as populations in developed countries.[5–8] However, to date, studies that included measurement of QoL in western China are relatively scarce, and the results of healthy life expectancy (HALE) have not been reported.
This study aims to estimate healthy life expectancy in Shaanxi Province and analyze the development of population health based on a cross-sectional study, to provide a reference to Shaanxi for developing health policy and improving population health.
Methods
Source of data
The population and death data of this study were derived from the Full Population Database (FPD) and mantained by Health Commission of Shaanxi Province, a basic database identified by the resident ID card as the main information in a region. Data collection is maintained by the family planning staff at the village (township) and community (town) levels, and the data collection card is used for household collection and input into the system. The frequency of collection and maintenance is at any time. Compared with the population data officially announced by the Shaanxi Provincial Bureau of Statistics, in the original database of the FPD, the coverage rates from 2015 to 2019 were 93.48%, 94.03%, 94.15%, 94.10%, and 94.49%, respectively. The number of births (defined as the 0-year-old population) comes from the Shaanxi Statistical Yearbook 2020 and the National Statistical Yearbook,[9,10] which is an annual statistical publication that comprehensively and systematically reflect economic, social, and technological development of the region. The data for calculating the prevalence came from the Home Page of Inpatient Medical Record (HPIMR) in Shaanxi Province from 2015 to 2019. The HPIMR is a summary of case data formed by medical staff using text and codes to refine and summarize relevant information during the patient's hospitalisation, containing the clinical diagnosis in a specific table.[11] In this study, we used medical records data of HPIMR from all hospitals except for traditional Chinese medicine hospitals. We identified the disease of the patient according to the main diagnosis of the patient, and the admission time was the diagnosis time of the disease. An inpatient entry will be generated for each inpatient visit, so we delete the same patient inpatient entry for the same disease according to the patient ID number and the disease classification of the main diagnosis to ensure that there are no duplicate entries.
Estimates of mortality rate
We adjusted the age-specific population based on FPD, and we used the number of births in the statistical yearbook as the standard number of 0-year-old people. The number of births in different areas and sexes was adjusted by the total birth rates of the Statistical Yearbook. We divided the population into 19 age groups in total. Under the age of 5 years, the patients were divided into a 0-year-old group and a 4-year-old group (1–4 years old) and then were divided into groups at 5-year intervals up to 85 years old and above (for example, the 5-year-old group was 5 to 9 years old, the 10-year-old group was 10 to 14 years old, and so on). We used multiple imputation (MI) to fill in the missing data of covariates of the number of deaths of the integration of 2018 to 2019, such as sex, areas, and cities (the detailed steps can be found in Supplementary Materials), and then used the total mortality rate of the Statistical Yearbook to adjust the population death, including men and women, urban and rural areas, and prefecture-level cities. Finally, the mortality rate of a specific age group was calculated by death and population. Due to the small number of elderly people (>80 years old), especially individuals >85 years old, we used the Kannisto extrapolation model to correct the mortality rate of the elderly because of the biased death population. The process of the estimation of mortality rate is presented in Supplementary Figure 1.
Estimates of the prevalence
We used the indexnot () function in Stata software (Stata Corp, College Station, TX, USA) to extract keywords to identify diseases. We linked data of inpatients based on the medical records number from the HPIMR and extracted ten major disease systems (referred to as chronic disease systems) according to ICD-10, which are tumors (C00-D48); endocrinology, nutrition and metabolism (E00-E90); mental and behavioral disorders (F00-F99); nervous system (G00-G99); sensory diseases (H00-H95, including diseases of the eyes and appendages, ear and mastoid diseases); circulatory system (I00-I99); respiratory system (J00-J99); digestive system (K00-K93); genitourinary system (N00-N99); musculoskeletal system and connective tissue (M00-M99). Disease observations with other codes are not included in this specific study. At the same time, we also estimated the prevalence of total disease-injury, mainly based on the adjusted proportion of these ten chronic disease systems in the entire HPIMR. The process of the estimation of prevalence is presented in Supplementary Figure 2.
Calculation of LE, HLE, and unhealthy years
We assumed that a generation of people born at the same time in a specific location die sequentially according to their age group specific mortality rate until they are all dead; to calculate the age group death probability, the number of survivors and other indicators, and the final calculated LE is used to illustrate the quality level of the population. Second, we used HALE as an indicator to assess QoL. We added the prevalence of the total disease-injury or the prevalence of ten major disease systems for a specific age group to the life table, and we used the Sullivan method to calculate the healthy life expectancy with total diseases and injuries (HALE-TDIs) and healthy life expectancy with ten system diseases (HALE-TENDs). Unhealthy years were calculated based on the difference between LE and HLE. The process of the area division in Shaanxi Province and the estimation of the results (Supplementary Figure 3). R version 3.6.2 (Ross Ihaka, Robert Gentleman, Oakland, New Zealand), Stata version 15, SAS version 9.4 (North Carolina State University, America), and ArcGis version 10.4 (Esri, America) were used for data analyzing.
Results
Total population changes
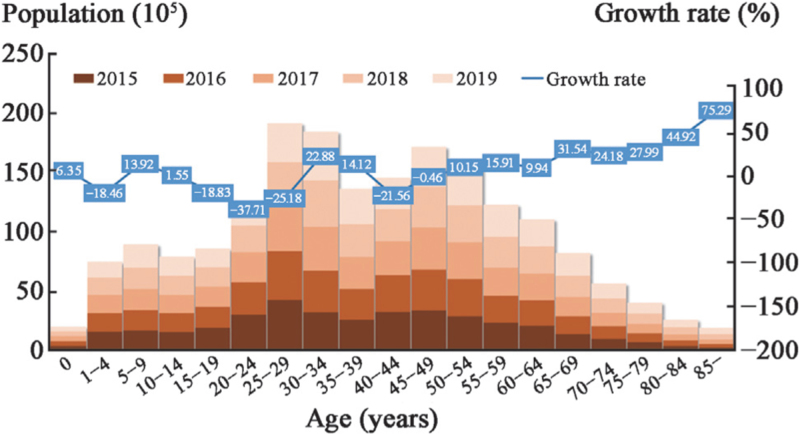
As shown in Figure 1, the population growth rate was approximately 2.17% in 5 years, and the average growth per year was 0.43%. The five-year growth rate of the population of infants under 0 was approximately 6.35%, the growth rate of children aged 1 to 4 years was approximately −18.46%, and the population growth rate of children under 5 was approximately −13.14%. The population of 5- to 14-year-olds continued to grow, while that of 15- to 29-year-olds declines, and the total population growth rate of 5- to 29-year-olds was approximately −17.20%. The population aged 30 to 39 years was increasing year by year, the population aged 40 to 49 years was decreasing, and the population growth rate of the population aged 30 to 49 years was approximately 4.58%. The population had been increasing year by year beginning at the age of 50 years, and the proportion of the elderly over 65 years old increased from 9.45% to 13.62%, with an average growth of 34.35% per year.
Figure 1.
Total population by age from 2015 to 2019 in Shaanxi Province.
Death probability of the population
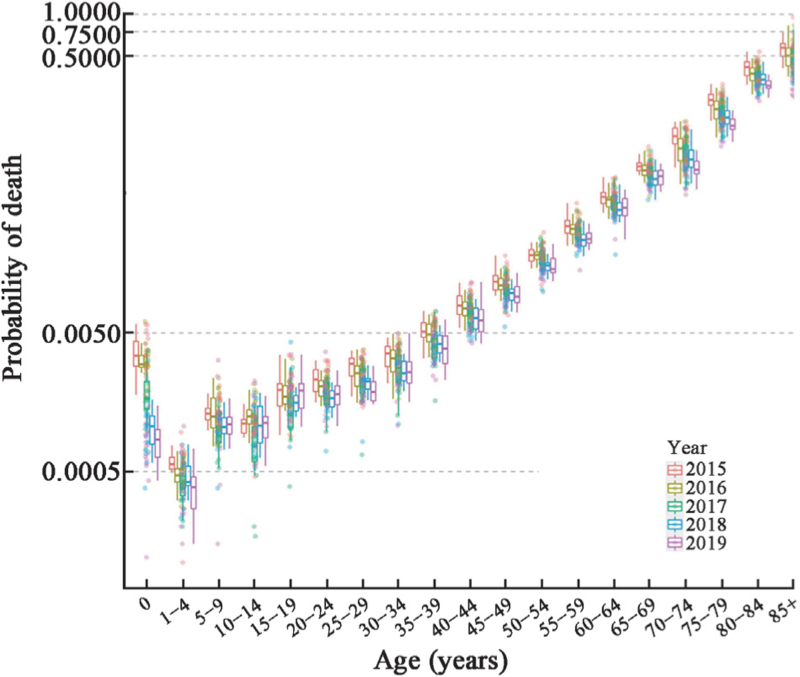
As shown in Figure 2, the average mortality rate of the population of all age groups has improved in the past five years, and it has been declining year by year. From 2015 to 2019, the probability of death of newborns (below 0 year old) was improved, while it was still higher than that in the 4-year-old age group. The difference of the probability of death of children <5 years had increased significantly, showing that the disparities were gradually increasing in improving the mortality rate of children under 5 years in the province. In 2019, the probability of death of the population aged 60 to 69 years fluctuated significantly compared with 2015, and the death situation of the elderly population varied at multiple levels. However, starting from the age of 70 years, the difference of the probability of death in a specific year was reduced, which means that the difference in mortality rate improved and the gap narrowed.
Figure 2.
Death probability distribution by age in Shaanxi Province, 2015–2019. This figure shows the distribution of death probability after the Kannisto extrapolated model by age group from 2015 to 2019. The transverse coordinates represent 19 age groups divided by the full age group, the longitudinal coordinates represent the death probability shown in a natural logarithmic scale, the box represents the upper quartiles and lower quartiles (75th and 25th percentile), the horizontal bars in the box represent the mean level, and the circles of different colors represent the scatter of jitter.
Life expectancy, healthy life expectancy and unhealthy years
Table 1 shows LE, HALE-TDIs, and HALE-TENDs in 2015 and 2019. LE at birth increased from 74.66 years to 77.19 years in 5 years, which was prolonged by approximately 2.54 years, and men (from 74.04 years to 76.61 years) had fewer years of life extension than women (from 75.32 years to 77.83 years). Since 2015, all prefecture-level life expectancies have improved from 2015 to 2019. The overall LE of Guanzhong was higher than that of other areas in Shaanxi, and the overall growth rate of LE in southern Shaanxi was faster than that in northern Shaanxi, with an average annual growth of 0.69 years per year. Xi’an and Tongchuan had a high level of LE in the Guanzhong area and even the whole province. Hanzhong developed rapidly from 73.45 years in 2015 to 77.14 years in 2019. LE in 65-year-old people increased by approximately 1.89 years in five years, and the increase in elderly men was higher than that in women, but LE was lower. LE at 65 years old still increased by approximately 2.83 years in Hanzhong, while the increase in Weinan was relatively slow.
Table 1.
LE, HALE-TDIs, and HALE-TENDs at birth and LE, HALE-TDIs, and HALE-TENDs at 65 years in Shaanxi population.
| LE (years) | HALE-TDIs (years) | HALE-TENDs (years) | ||||||||||
| 2015 | 2019 | 2015 | 2019 | 2015 | 2019 | |||||||
| Parameters | At birth | At 65 years | At birth | At 65 years | At birth | At 65 years | At birth | At 65 years | At birth | At 65 years | At birth | At 65 years |
| Total | 74.66 | 16.61 | 77.19 | 18.50 | 67.85 | 9.30 | 69.76 | 10.84 | 70.55 | 12.20 | 72.30 | 13.46 |
| Men | 74.04 | 16.52 | 76.61 | 18.43 | 66.91 | 8.65 | 69.11 | 10.51 | 69.74 | 11.77 | 71.67 | 13.22 |
| Women | 75.32 | 16.71 | 77.83 | 18.59 | 68.80 | 9.90 | 70.43 | 11.14 | 71.39 | 12.60 | 72.97 | 13.69 |
| Rural areas | 74.32 | 16.09 | 76.87 | 18.31 | 67.05 | 8.44 | 67.56 | 8.85 | 69.93 | 11.47 | 70.74 | 12.09 |
| Urban areas | 74.37 | 16.41 | 77.44 | 18.66 | 68.30 | 9.77 | 71.32 | 12.25 | 70.71 | 12.40 | 73.41 | 14.44 |
| Xianyang | 74.63 | 16.32 | 76.79 | 17.83 | 67.71 | 8.97 | 70.07 | 10.96 | 70.45 | 11.89 | 72.37 | 13.31 |
| Shangluo | 72.73 | 16.05 | 76.58 | 18.60 | 67.69 | 10.35 | 70.48 | 12.21 | 69.69 | 12.61 | 72.57 | 14.40 |
| Ankang | 72.67 | 15.46 | 75.42 | 17.50 | 67.25 | 9.49 | 68.26 | 9.98 | 69.40 | 11.86 | 70.71 | 12.55 |
| Baoji | 74.64 | 15.82 | 77.38 | 18.17 | 66.71 | 7.49 | 69.73 | 10.37 | 69.85 | 10.80 | 72.35 | 13.04 |
| Yan’an | 72.61 | 14.77 | 75.50 | 16.54 | 65.09 | 6.55 | 68.03 | 8.80 | 68.07 | 9.81 | 70.59 | 11.45 |
| Yangling | 77.26 | 18.31 | 79.11 | 19.85 | – | – | – | – | – | – | – | – |
| Yulin | 73.51 | 15.75 | 74.96 | 17.65 | 67.27 | 8.99 | 68.90 | 11.19 | 69.74 | 11.67 | 70.98 | 13.40 |
| Hanzhong | 73.45 | 15.73 | 77.14 | 18.57 | 68.02 | 9.89 | 70.25 | 11.48 | 70.17 | 12.21 | 72.61 | 13.91 |
| Weinan | 75.42 | 17.59 | 77.40 | 18.82 | 70.58 | 12.41 | 71.78 | 13.10 | 72.50 | 14.47 | 73.70 | 15.06 |
| Xi Xian | 74.10 | 15.76 | 77.11 | 18.25 | – | – | – | – | – | – | – | – |
| Xi’an | 76.56 | 17.86 | 78.81 | 19.52 | 66.45 | 7.14 | 67.43 | 7.81 | 70.46 | 11.39 | 71.33 | 11.82 |
| Tongchuan | 76.04 | 18.05 | 78.83 | 19.69 | 72.05 | 13.85 | 72.17 | 12.94 | 73.63 | 15.52 | 74.45 | 15.25 |
| Guanzhong | 75.61 | 17.20 | 77.88 | 18.84 | 68.83 | 9.99 | 70.59 | 11.36 | 71.52 | 12.85 | 73.08 | 13.92 |
| Shanbei | 73.18 | 15.39 | 75.22 | 17.25 | 66.49 | 8.12 | 68.71 | 10.38 | 69.14 | 11.00 | 70.94 | 12.73 |
| Shannan | 73.03 | 15.75 | 76.45 | 18.25 | 67.66 | 9.84 | 69.72 | 11.25 | 69.79 | 12.18 | 72.03 | 13.65 |
–: Not available; HALE-TDIs: Healthy life expectancy with total diseases and injuries; HALE-TENDs, Healthy life expectancy with ten system diseases; LE: Life expectancy.
Considering total diseases and injuries, HALE-TDIs at birth increased from 67.85 years in 2015 to 69.75 years in 2019. The HALE-TDIs increased in almost all prefecture-level cities, and Yan’an fluctuated from 2017 to 2018. Tongchuan and Weinan had higher HALE-TDIs. The increase in HALE-TDIs for men (2.20 years) was higher than that for women (1.63 years). However, the growth in urban areas was almost 6 times that in rural areas, where the increment was approximately 0.51. Baoji, Yan’an, and Shangluo have increased their HALE-TDIs at birth by more than 2.5 years. The HALE-TDIs at 65 years have increased from 9.30 years to 10.84 years. The healthy years of people over 65 years old in the same period have improved.
When considering only the ten major disease systems, HALE-TENDs at birth increased by 1.75 years in 5 years from 70.55 years to 72.30 years, which was higher in females than males, and urban areas were higher than rural areas. The HALE-TENDs in Guanzhong were approximately 73.08 years, followed by southern and northern Shaanxi. The HALE-TENDs in Tongchuan in 2019 were approximately 74.45 years, followed by 73.70 years in Weinan. The maximum change in HALE-TENDs over five years in Weinan was approximately 2.88 years. HALE-TENDs at age of 65 years were 13.46 with an increase of 1.26 since 2015, and HALE-TENDs at 65 years increased by 2.04 in urban areas. The increment of HALE-TENDs increased in five years. The increment of HALE-TENDs in prefecture-level cities increased over 5 years, while it declined by 0.27 in Tongchuan.
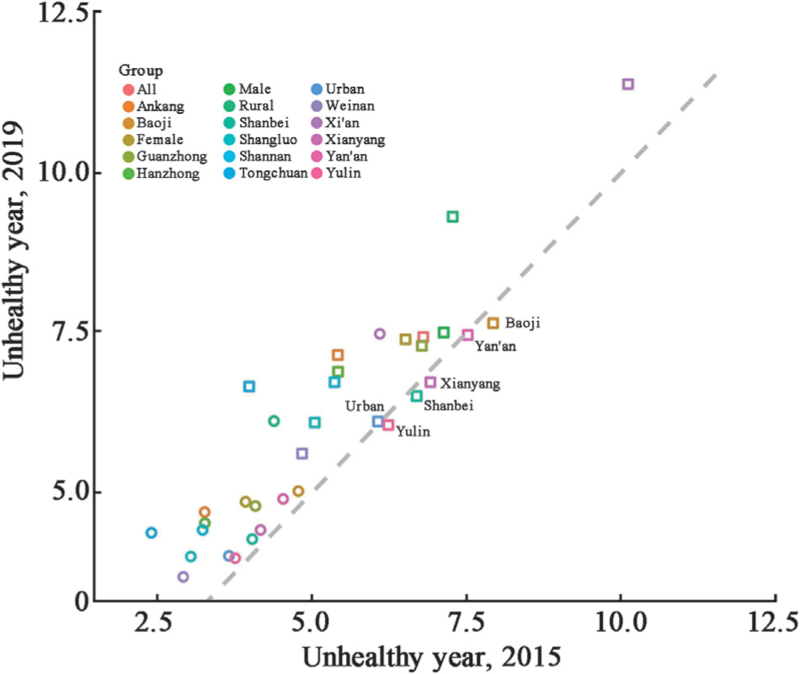
A scatter plot of the number of unhealthy years in various cities in Shaanxi Province in western China is shown in Figure 3. From 2015 to 2019, when considering total diseases and injuries, only four prefecture-level cities (Baoji, Yan’an, Xianyang, and Yulin) experienced a decline in the number of unhealthy years. The number of unhealthy years in urban areas gradually decreased, and the number of unhealthy years in males was higher than that in females. With only ten system diseases considered, despite LE and HALE-TENDs being increased at birth and at 65 years, the number of unhealthy years in all prefecture-level cities was increasing under the influence of the ten system diseases.
Figure 3.
The spatial distribution of LE in 13 prefecture-level cities in Shaanxi Province, 2015–2019. LE: Life expectancy.
Discussion
Using cross-sectional data, this article evaluated the 5-year changes by specific age in population and deaths and comprehensively measured the QoL of the population in Shaanxi Province in China. Our research found that Shaanxi Province has achieved good results in reducing mortality in the past five years, and the population structure has also changed. The reverse growth of the population number in the 0-year-old group and the gradual increase of the elderly population have led to an inverted population pyramid, which will pose challenges for the health and lead to financial changes in the whole province. At the same time, we found that LE and HLE increased almost universally, and LE in women was higher than that in men. HALE under the total diseases and injuries at birth and HALE under the ten major disease systems at birth both improved. Unhealthy years under the total diseases and injuries increased by 0.62 years in 5 years, and it increased by 0.78 years under the 10 major disease systems, and the unhealthy years differed among cities.
The results of this study show that the situation in the Shaanxi Province is not optimistic due to the population aging phenomenon. The number of elderly people >65 years in Shaanxi is increasing, accounting for approximately 13.62% of the total population in 2019. Our results are similar to the seventh national census of China, which found that the population of China in 2020 will increase by 5.38% compared with 2010, with an average annual growth rate of 0.53%. The 65-year-old population in the country accounts for approximately 13.50% of the total population, and the elderly population in the Shaanxi Province accounts for approximately 13.32%.[12] Population aging has become a serious area of concern to China. According to the National Bureau of Statistics, the dependency ratio of the elderly population was 16.8% in 2018 in China, with a year-on-year increase of 40.00% from 2010. Compared with 2010, the dependency ratio of the elderly population in Shaanxi increased by 35.35% year-on-year in 2018.[4] In terms of the mortality rate, it has improved significantly in children under 5 years old in Shaanxi. It is an important global achievement in the past few decades in the improvement in the mortality rate of children under 5 years of age.[6,13] Although the migration of the floating population may be a key factor affecting population structure and size, we must emphasize that this population inversion model will lead to an increase in the dependency ratio in Shaanxi. We should intervene by introducing policies such as raising fertility rates and decreasing the deaths of the birth population.
In recent years, various provinces in China have gradually conducted research on the calculation of LE and HLE. A study using the monitoring data of death in Hubei Province established a life table to estimate LE in Hubei Province in 2018 of 79.16 years.[14] A study in Shanghai used the disability weights of the Global Burden of Disease Study to estimate that the LE of Shanghai in 2016 and it was 83.18 years, and the HLE was 69.46 years.[15] The LE of adults >20 years old estimated by the death cause monitoring and underreporting data in Zhejiang Province is approximately 59.08 years, and the HLE is approximately 55.80 years.[16] Although the LE of all provinces in China has generally increased, there are still large differences between regions. Compared with the central and eastern regions in China, LE in Shaanxi Province is relatively low, and the differences approximately about 3 to 6 years old in LE and HLE, respectively.
Our results show that women have a higher LE (at birth and at 65 years old) and a higher HLE than men, whether considering all disease injuries or only 10 system diseases, but the unhealthy number of years for men is slightly higher. However, we found that the difference in unhealthy years in 5 years between women and men gradually decreased. Although HALE has improved year by year, the QoL of women is becoming increasingly unhealthy, and this difference is gradually diminishing compared with the status of men. The Global Burden of Disease (GBD) shows that there are differences in health between sexes. The smaller male–female gap of HALE has decreased over time, which is due to lifestyle behaviors such as smoking or drinking becoming indistinguishable between men and women.[17] The differences in health between the sexes can be divided into physiological gender differences and social gender differences (such as gender differences in health behaviors) are gradually shrinking according to the world health statistics 2019.[18] While this study did not explore the health effects of education, income, and lifestyle, such as smoking, drinking, and physical exercise, other studies have found that social impact factors and lifestyle have had an increasing impact on population health; moreover, this influence also differs by genders and areas.[19–23]
The results of the study show that the Shaanxi population has improved their QoL by decreasing the number of unhealthy years. Our results show that one-third of the prefecture-level cities in Shaanxi Province of western China have a downwards trend in the number of unhealthy years when we considered all diseases and injuries in 5 years. This shows that the QoL of the residents improved during the extended life years. When only considering the 10 system diseases, the unhealthy years of population have an increasing trend. LE continued to be prolonged due to improved living conditions, education, and medical levels.[24] According to the statistical analysis of the GBD 2019, LE has increased from 50.40 years to 73.5 years globally from 1950 to 2019, and the development speed of LE in various countries is obviously different. LE in China has grown rapidly from 49.3 years to 77.6 years, a nearly 28.3-year increase since 1950.[25] However, this extended average lifespan has not led to people being healthier as they age.[26–30] Non-infectious chronic diseases (NCDs) are the main cause of the loss of QoL. The results of a report on the nutrition and chronic disease status of Chinese residents showed that cardiovascular and cerebrovascular diseases, cancer, chronic respiratory diseases, and diabetes became the main chronic diseases affecting the health of the Chinese population in 2019. The premature death rate still reached 16.5%, although the disease-caused premature deaths of residents decreased by 2 percentage compared with 2015 in the whole country. The national public health service project, a project to promote the equalization of public health services for population health, was launched in 2009. Since then, the health of the population has improved significantly in Shaanxi province, and the quality of basic public health services has improved within 5 years, such as the construction of health information platforms and other new media means to carry out public health and medical innovation.[31,32] We showed that the growth rate of the number of unhealthy years caused by NCDs has slowed down, but the growth rate of HLE is slower than LE, which is largely due to the impact of NCDs, which is similar to many studies.[17,33–36] In the extended lives of residents in China, the impact of NCDs on the QoL of the population is gradually increasing. The government needs to continue to pay attention to the harm of NCDs to the health of the population. At the same time, for the improvement of the quality of basic public health services, some key measures, such as increasing policy publicity and informatization, could be strengthened to highlight. Key projects, such as health management for patients with NCDs, child vaccination, health management for elderly individuals, and psychological and behavioral interventions, should continue to be carried out to reduce the burden of disease caused by NCDs.
This study revealed the changes in population and death, as well as the QoL in the Shaanxi province of China, which is of great significance for understanding the development of population health. However, there are also some limitations. First, because the death data from 2015 to 2017 are not fully integrated, which results in the estimation of the mortality rate being relatively high, thus LE for 2015–2017 is relatively low. Second, the lack of prevalence data has led to bias in our estimation of HALE. The definition of healthy in this study is based on exsitence of clinical symptoms. If a person becomes ill without any clinical symptom or hospitalization, then we define the loss of life of this patients as being negligible. Therefore, in addition to inpatients, there are some disease-related data we are unable to obtain. Unfortunately, we realize that if we calculate the specific impairment of a disease to the lifespan, this will largely underestimate the loss of the lifespan of the population. At the same time, the existence of comorbidities can also lead to deviations in calculations. We believe that the main diagnosis is the disease that currently causes the most serious loss of life if a person suffers from a disease and requires hospitalization. Our results with outcomes including total diseases and injuries and the ten main NCDs, were adjusted for equal proportions, which may weaken the influence of the neglected loss, although it will lead to deviation to some extent.
In conclusion, Shaanxi has made progress to reduce the mortality rate of the population at birth, increasing the lifespan of the population, and controlling the impact of chronic diseases on the overall health of the population from 2015 to 2019. However, measures should still be taken against the growing population size. At the same time, our results show that the QoL of people in Shaanxi Province has improved, but there is still a slow increase in the years of unhealthy survival. Although good progress has been made in the control of chronic diseases, it is still necessary to minimize impact of risk factors and continuously improve the quality of basic public health services.
Funding
This work was supported by a grant from the Project of Standardized test point of telemedicine information system.
Conflicts of interest
None.
Supplementary Material
Footnotes
How to cite this article: Miao X, Chen J, Wu Q, Meng W, Ren L, Wu Z, Guo X, Zhang X, Meng Q. Estimation of the population, death, and quality of life in Shaanxi Province, western China: a cross-sectional study. Chin Med J 2023;136:1832–1838. doi: 10.1097/CM9.0000000000002524
Supplemental digital content is available for this article.
References
- 1.Chen H, Chen G, Zheng X, Guo Y. Contribution of specific diseases and injuries to changes in health adjusted life expectancy in 187 countries from 1990 to 2013: retrospective observational study. BMJ 2019; 364:l969.doi: 10.1136/bmj.l969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.NHC. Healthy China Action, 2019–2030. Avaliable from: https://baike.baidu.com/item/%E5%81%A5%E5%BA%B7%E4%B8%AD%E5%9B%BD%E8%A1%8C%E5%8A%A8%EF%BC%882019%E2%80%942030%E5%B9%B4%EF%BC%89/23543779?fr=aladdin.[Last accessed on 2022-01-10]. [Google Scholar]
- 3.Xilei M, Rongshou Z, Yue C, et al. Measurement and application of health life expectancy (in Chinese). J Environ Occup Med 2019; 36:277–281. 286. doi:10.13213/j.cnki.jeom.2019.18551. [Google Scholar]
- 4.NHC. National Health Statistics Yearbook 2020. Beijing: Peking Union Medical University Press, 2020. [Google Scholar]
- 5.Du J, Li G, Gao YL, Wei ZH, Wang J, Su JT, et al. Influencing factors on healthy life expectancy in adults in Beijing (in Chinese). Chin J Epidemol 2016; 37:1087–1090. doi: 10.3760/cma.j.issn.0254-6450.2016.08.006. [DOI] [PubMed] [Google Scholar]
- 6.Tian X, Tang Z, Jiang J, Fang X, Wu X, Han W, et al. Effects of smoking and smoking cessation on life expectancy in an elderly population in Beijing, China, 1992–2000: an 8-year follow-up study. J Epidemiol 2011; 21:376–384. doi: 10.2188/jea.JE20110001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen R, Xu P, Song P, Wang M, He J. China has faster pace than Japan in population aging in next 25 years. Biosci Trends 2019; 13:287–291. doi: 10.5582/bst.2019.01213. [DOI] [PubMed] [Google Scholar]
- 8.Wang P, Liu Q, Li G, et al. Calculation and analysis of adult healthy life expectancy in Beijing in 2012 (in Chinese). China Health Stat 2016; 75–77. 80. [Google Scholar]
- 9.Shaanxi Statistic Yearbook. Available from: http://tjj.shaanxi.gov.cn/upload/2021/zl/2020/zk/indexch.htm. [Last accessed on Jan 11th, 2022]. [Google Scholar]
- 10.National Bureau of Statistics. Available from: http://data.stats.gov.cn/english/easyquery.htm?cn=C01. [Last accessed on Jan 11th, 2022]. [Google Scholar]
- 11.Xiao X, Zhou D, Sun Y. Big data analysis and application of medical record homepage. Beijing: People's Medical Publishing House; 2021. [Google Scholar]
- 12.Bulletin of the Seventh National Census (No. 2). Available from: http://www.stats.gov.cn/tjsj/tjgb/rkpcgb/qgrkpcgb/202106/t20210628_1818821.html.[Last accessed on Jan 10, 2022]. [Google Scholar]
- 13.Lau RS, Johnson S, Kamalanabhan TJ. Healthy life expectancy in the context of population health and ageing in India. Asia Pac J Public Health 2012; 24:195.doi: 10.1177/1010539510376663. [DOI] [PubMed] [Google Scholar]
- 14.Cheng S, Pan J, He T, et al. Adult healthy life expectancy in hubei Province, 2018 (in Chinese). Mod Prev Med 2021; 48:2457–2460. [Google Scholar]
- 15.Yu HT, Xia T, Wang CF, Fang B, Cai RZ, Chen L, et al. Analysis on the difference between life expectancy and healthy life expectancy in Shanghai (in Chinese). Chin J Epidemol 2021; 42:1018–1023. doi: 10.3760/cma.j.cn112338-20200417-00591. [DOI] [PubMed] [Google Scholar]
- 16.Fei F, Hu R, Zhong J, et al. An analysis on health life expectancy of adult residents in Zhejiang Province (in Chinese). Prev Med 2017; 29:973–977. 982. doi: 10.19485/j.cnki.issn1007-0931.2017.10.001. [Google Scholar]
- 17.GBD 2017 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018; 392:1859–1922. doi: 10.1016/S0140-6736(18)32335-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.WHO. World health statistics 2019: monitoring health for the SDGs, sustainable development goals. Available from: https://www.who.int/publications/i/item/9789241565707. 2019-05-21. [Last accessed on Jan 10, 2022]. [Google Scholar]
- 19.Gakidou E, Cowling K, Lozano R, Murray CJ. Increased educational attainment and its effect on child mortality in 175 countries between 1970 and 2009: a systematic analysis. Lancet 2010; 376:959–974. doi: 10.1016/S0140-6736(10)61257-3. [DOI] [PubMed] [Google Scholar]
- 20.Cutler DM, Lleras-Muney A. Understanding differences in health behaviors by education. J Health Econ 2010; 29:1–28. doi: 10.1016/j.jhealeco.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Conti G, Hansman C. Personality and the education-health gradient: a note on “understanding differences in health behaviors by education”. J Health Econ 2013; 32:480–485. doi: 10.1016/j.jhealeco.2012.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reynolds MM, Avendano M. Social policy expenditures and life expectancy in high-income countries. Am J Prev Med 2018; 54:72–79. doi: 10.1016/j.amepre.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019; 394:1145–1158. doi: 10.1016/S0140-6736(19)30427-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sen W. Life expectancy decomposition and it's influencing factors analysis: based on provincial panel data (in Chinese). Northwest Population 2014; 35:37–42. doi:10.15884/j.cnki.issn.1007-0672.2014.03.007. [Google Scholar]
- 25.GBD 2019 Demographics Collaborators. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet 2020; 396:1160–1203. doi: 10.1016/S0140-6736(20)30977-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xia X, Cai Y, Cui X, Wu R, Liu F, Huang K, et al. Temporal trend in mortality of cardiovascular diseases and its contribution to life expectancy increase in China, 2013 to 2018. Chin Med J 2022; 135:2066–2075. doi: 10.1097/CM9.0000000000002082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li Y, Schoufour J, Wang DD, Dhana K, Pan A, Liu X, et al. Healthy lifestyle and life expectancy free of cancer, cardiovascular disease, and type 2 diabetes: prospective cohort study. BMJ 2020; 368:l6669.doi: 10.1136/bmj.l6669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Meyer AC, Drefahl S, Ahlbom A, Lambe M, Modig K. Trends in life expectancy: did the gap between the healthy and the ill widen or close? BMC Med 2020; 18:41.doi: 10.1186/s12916-020-01514-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hoogendijk EO, van der Noordt M, Onwuteaka-Philipsen BD, Deeg DJH, Huisman M, Enroth L, et al. Sex differences in healthy life expectancy among nonagenarians: a multistate survival model using data from the Vitality 90+ study. Exp Gerontol 2019; 116:80–85. doi: 10.1016/j.exger.2018.12.015. [DOI] [PubMed] [Google Scholar]
- 30.Sepanlou SG, Parsaeian M, Krohn KJ, Afshin A, Farzadfar F, Roshandel G, et al. Disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE) in Iran and its neighboring countries, 1990-2015: findings from Global Burden of Disease Study 2015. Arch Iran Med 2017; 20:403–418. [PubMed] [Google Scholar]
- 31.Significant achievements in basic public health services in Xianyang. Available from: http://sxwjw.shaanxi.gov.cn/sy/sxdt/202104/t20210401_2158419.html.[Last accessed on 2022-01-13]. [Google Scholar]
- 32.Huayin City Holds 2021 National Basic Public Health Service Project and Regional Health Information: Platform Application Training Conference. Available from: http://sxwjw.shaanxi.gov.cn/sy/sxdt/202107/t20210719_2183545.html.[Last accessed on 2022-01-13]. [Google Scholar]
- 33.Safiri S, Kolahi AA, Hoy D, Smith E, Bettampadi D, Mansournia MA, et al. Global, regional and national burden of rheumatoid arthritis 1990–2017: a systematic analysis of the Global Burden of Disease study 2017. Ann Rheum Dis 2019; 78:1463–1471. doi: 10.1136/annrheumdis-2019-215920. [DOI] [PubMed] [Google Scholar]
- 34.GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018; 392:1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fitzmaurice C, Abate D, Abbasi N, Abbastabar H, Abd-Allah F, et al. Global Burden of Disease Cancer Collaboration. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2017: a systematic analysis for the Global Burden of Disease Study. JAMA Oncol 2019; 5:1749–1768. doi: 10.1001/jamaoncol.2019.2996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016; 388:1545–1602. doi: 10.1016/S0140-6736 (16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.