Introduction and importance:
SCHMID metaphyseal chondrodysplasia is a rare cause of short stature with a good prognosis regarding other types of chondrodysplasia in reason of the normal integrity of the growth plate.
Case presentation:
The authors present a rare case of 4-year-2-month-old boy referred to our Unit for harmonious short stature, he had a waddling gait, subtle micromelia, and hyperlordosis, no special facies.
Clinical discussion:
The skeletal scan made the diagnosis of SCHMID metaphyseal chondrodysplasia. The first laboratory workup showed elevated thyroid stimulating hormone and anti-tissue transglutaminase immunoglobulin A. The duodenal biopsies confirmed the diagnosis of coeliac disease. Treatment of levothyroxine was initiated with a gluten-free diet .6 years later, his re-evaluation showed a low insulin-like growth factor 1 and low growth hormone peaks confirming the diagnosis of growth hormone deficiency, Growth hormone therapy was initiated with an adjusted dose of levothyroxine.
Conclusion:
Other causes of short stature should not be missed when diagnosing chondrodysplasia, and further investigations should be carried out to detect other concomitant disorders since metaphyseal chondrodysplasia is a rare cause for short stature while hypothyroidism and coeliac disease are relatively common.
Keywords: coeliac disease, growth hormone deficiency, hypothyroidism, SCHMID metaphyseal chondrodysplasia
Introduction
Highlights
Metaphyseal chondrodysplasia, schmid type, is a very rare inherited disorder characterized by short stature with abnormally short arms and legs (short-limbed dwarfism) and bowed legs (genu varum).
Hypothyroidism is where your thyroid gland does not produce enough hormones.
Coeliac disease) is a systemic autoimmune disease caused by a lifelong intolerance to gluten. Growth hormone deficiency, also known as dwarfism or pituitary dwarfism, is a condition caused by insufficient amounts of growth hormone in the body.
Short stature is a general term used to describe a condition in which a child or a teen’s height is well below the average height of his or her peers.
Short stature is a common cause for paediatric endocrinologist consultation, it is a general term for children whose height is two SDs or more below the mean height for children of the same sex and age, short stature may indicate pathologic causes like systemic disorders, endocrine conditions and genetic disease.1
Chondrodysplasias are a heterogeneous group of skeletal disorders characterized by short stature and other skeletal malformation.2,3 The incidence as a group is 1 per 4000 birth.3 SCHMID metaphyseal chondrodysplasia )SMCD) is a mild type of chondrodysplasia with a better prognosis.3,4
SMCD is a rare autosomal dominant disorder caused by heterozygous mutations in the gene encoding type X collagen with unknown incidence.5 The main manifestation is short stature, genu varum, and waddling gait during the first years of life. Radiologic findings are enlarged capital femoral epiphyses, metaphyseal abnormalities of the long bones, anterior cupping, sclerosis, and splaying of the ribs, mild hand involvement. No extraskeletal anomalies were reported. Intelligence and life expectancy are preserved.6
Subclinical hypothyroidism (SCH) is a biochemical condition characterized by increased thyroid stimulating hormone with normal levels of thyroid hormone. It is typically asymptomatic. The most common cause of SCH is chronic autoimmune thyroiditis. SCH is a common disorder with an incidence of in children.7
Coeliac disease (CD) is a common systemic autoimmune disease that primarily affects the small intestine caused by gluten intolerance, which causes immunologically mediated inflammatory destruction. There is a remarkable association with the human leucocyte antigen DR3-DQ2 and/or DR4-DQ8. The Clinical presentation is variable and ranges from gastrointestinal symptoms to non-gastrointestinal manifestation with increased risk for some malignancies. The pooled global prevalence is 1.4% but can vary considerably by region.8
Growth hormone deficiency (GHD) is defined as impaired secretion of growth hormone (GH) by the pituitary gland that results in growth failure, this could be congenital or acquired, isolated or combined with other pituitary hormonal deficits.9 The incidence of GHD in children is ~1:4000.9
We report a case of a 4-year-2-month-old male with severe short stature caused by SMCD associated with subclinical hypothyroidism, GHD, and CD.
This case report has been reported in line with the SCARE criteria 2020.10
Case presentation
A 4-year-2-month-old boy (Fig. 1) was referred to our Endocrinology Clinic to evaluate for Severe Short Stature. He was the offspring of consanguineous parents, born at term by normal vaginal delivery. The family medical history was only positive for a familial short stature.
Figure 1.
A 4-year-2-month-old boy with short stature, bowing lower limbs, and micromelia.
His weight was 13 kg (1.74th) percentile his height was 85 cm (0.1) percentile and his head circumference was 47 cm (−3.3 SD)on CDC growth charts. The blood pressure was 100/60 mmHg, the heart rate of 85 bpm, and the respiratory rate of 20 bpm.
On physical Examination, he was conscious, and oriented, with no facial dysmorphia, subtle short upper and lower limbs, bowing of the lower limbs, waddling gait, and hyperlordosis.
The urogenital examination showed micropenis. The rest of his physical examination was normal.
The initial biochemical workup is shown in Table 1.
Table 1.
The results of biochemical workup.
| Test | Result | Normal values | Test | Result | Normal values |
|---|---|---|---|---|---|
| HGB | 11 | 11–14 g/dl | Urea | 17 | 5–18 Mg/dl |
| MCV | 72 | 75–86 fl | Creatinine | 0.4 | 0.2–0.5 Mg/dl |
| Calcium | 9.4 | 8.8–10.8 mg/dl | AST | 64 | 15–50 U\l |
| Phosphorous | 3.8 | 4–7 mg/dl | ALT | 25 | 4–36 U/l |
| ALP | 163 | 65–210 U\L | Glucose | 84 | 70–110 Mg/dl |
ALP, alkaline phosphatase; ALT, alanine transaminase; AST, aspartate aminotransferase; HGB, haemoglobin; MCV, mean corpuscular volume.
The results were unremarkable.
Hormonal workup is shown in Table 2:
Table 2.
The results of hormonal findings.
| Test | Result | Normal values | Test | Result | Normal values |
|---|---|---|---|---|---|
| TSH | 7.8 | 0.3–5 mIU/ul | Anti-TTG-IgA | 145 | 0–3 U/ml |
| FT4 | 1.13 | 0.8–2 ng/dl | IGF1 | 55 | 5–128 ng/dl |
Anti-TTG-IgA, anti-tissue transglutaminase immunoglobulin A; FT4, free thyroxine 4; IGF1, insulin-like growth factor 1; TSH, thyroid stimulator hormone.
Table 2 showed an elevated thyroid stimulating hormone and positive anti-tissue transglutaminase immunoglobulin A.
The child had Duodenal Biopsies confirming CD (Marsh type 3b).
Due to the presence of mild microcephaly, he had a computed tomography-SCAN of the brain which was normal.
A complete skeletal scan showed changes in the bone structure at the terminal parts of the femoral bones and no changes in the pelvis (Fig. 2). there were no remarkable changes in the bone structure of the vertebrae (Fig. 3) which lead to the diagnosis of Metaphyseal chondrodysplasia type SCHMID.
Figure 2.

Pelvis and lower limbs radiograph show bowing femurs, large capital epiphyses, and short femoral necks. Wide growth plate of tubular bones.
Figure 3.

Normal spinal column.
A treatment with levothyroxine 25 mcg per day was initiated, with a gluten-free diet.
Lost to follow up. At the age of 10 years and 4 months, his height was 117 cm (0.1 percentile), and his weight was 26 kg (0.4 percentile) rising concerns about the integrity of his pituitary gland.
His hormonal workup is shown in Table 3.
Table 3.
The results of hormonal workup.
| Test | Result | Normal values | Test | Result | Normal values |
|---|---|---|---|---|---|
| TSH | 6.8 | 0.3–5 mIU/ul | Cortisol 8 AM | 18.67 | 3–21 mcg/dl |
| FT4 | 1.88 | 0.8–2 ng/dl | IGF1 | 39.1 | 5–128 ng/dl |
Table 3 showed a high level of TSH and a low IGF1.
FT4, free thyroxine 4; IGF1, insulin-like growth factor 1; TSH, thyroid stimulator hormone.
The dose of levothyroxine was adjusted to 50 mcg/kg per day.
A GH provocation test (Table 4) with insulin (0.01 unit/kg) showed low peaks.
Table 4.
Growth hormone provocation test.
| Test | Result |
|---|---|
| GH fasting at rest | 0.78 ng/ml |
| GH after ½ h | 1.46 ng/ml |
| GH after 1 h | 0.37 ng/ml |
| GH after 1+1/2 h | 0.02 ng/ml |
GH, growth hormone.
To exclude any possibility of an autoimmune polyendocrine syndrome, parathyroid hormone and glycated haemoglobin were within normal limits (Table 5).
Table 5.
Parathyroid hormone and glycated haemoglobin results.
| Test | Result | Normal values | Test | Result | Normal values |
|---|---|---|---|---|---|
| PTH | 40 | 15–65 Pg/ml | Calcium | 9 | 8.8–10.8 mg/dl |
| Glycated haemoglobin | 5 | 4–6.8% | Phosphorous | 4.3 | 4–7 mg/dl |
PTH, parathyroid hormone.
MRI of the brain and pituitary gland was normal (Fig. 4).
Figure 4.
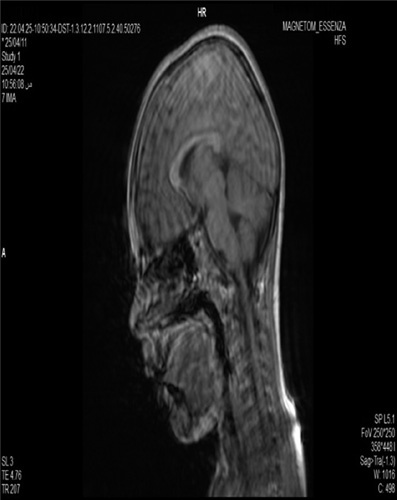
Showed a normal MRI of the brain and the pituitary gland.
The estimation of his bone age based on the Greulich and Pyle atlas was 6 years.
A GH therapy with a dose of 0.24 mg/kg per week was initiated associated with free gluten diet.
Discussion
Chondrodysplasia is a rare cause of short stature which might be easily diagnosed by clinical aspects and skeletal scan. However, SMCD is a subtle type of chondrodysplasia with mild manifestations.1–6
In the present case, the suspicion of SMCD was made by a clinical examination which showed short stature, waddling gait, microcephaly, and subtle micromelia. A skeletal survey showed signs suggesting SMCD, and more investigations showed hypothyroidism and CD. 6 years later, his degraded measurements raise concerns about GHD.
SMCD is rarely associated with other hormonal deficiencies. To the best of our knowledge, this is the first description of an association between SMCD, hypothyroidism, GHD, and CD which might be just an accidental event.
Alenazi et al. 11 .described a case of a Saudi female with GHD and Achondroplasia.
The gold standard for the diagnosis of SMCD is based on genetic testing6, which is not available in our case.
In our case, GH therapy could have double benefits due to the presence of GH deficiency and the normality of the growth plate which is not affected in SMCD, this theory is confirmed by Knawaza et al. 12 who studied 85 Japanese children- with different types of skeletal dysplasia—treated with GH therapy for 1 year. The trial concluded that GH therapy was effective for height gain.
GH therapy is considered an indication of short stature in Turner syndrome patients even in the absence of GHD with promising results due to the integrity of the growth plate, early initiation of GH therapy is important to achieve a reasonable final height in these girls.13
SMCD is a rare cause of short stature but CD and acquired hypothyroidism are relatively common9,11–14 in our region whose early diagnosis and management might improve the height expectancy.
CD is a chronic autoimmune disease caused by gluten ingestion, the clinical manifestations may vary from asymptomatic to severe malabsorption with extraintestinal symptoms such as growth failure, learning disorders, iron deficiency, and high risk of autoimmune diseases.8 In our case, the patient had no specific symptoms and the diagnosis was made accidentally in the context of first-line investigations for short stature.
There is an association between CD and autoimmune hypothyroidism three times higher than the general population,15 thus, at the time of diagnosis one of them, it is important to investigate the other for appropriate management.
At the supposed age of puberty, other investigations regarding the pituitary-gonadal axis should be performed to determine delayed puberty in the context of another hormonal deficiency.
After puberty, another possibility of management as surgical correction and limb lengthening could be helpful for SMCD patients.16,17
Conclusion
SMCD is a mild type of chondrodysplasias characterized by short stature and other subtle skeletal malformation and requires the patient’s growth chart monitoring. In case the growth chart started to deteriorate over time, the possibility of other associated disorders should be considered that could be treatable so the final height expectancy may improve.
Ethical approval
This case report did not require review by the Ethics Committee Tishreen university hospital, Latakia, Syria.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Sources of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution
A.C. contributed in data interpretation, and as a mentor and reviewer for this case report. F.B. contributed in performing an extensive literature review. O.A. contributed as a mentor and reviewer for this case report. Z.A., A.M., and F.K. contributed in writing the paper.
Conflicts of interest disclosure
All of the authors declare that they have no competing interests.
Research registration unique identifying number (UIN)
Not applicable.
Guarantor
Ahmad Chreitah.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 28 June 2023
Contributor Information
Ahmad Chreitah, Email: ahmad.chreitah@tishreen.edu.sy.
Fatima Bress, Email: fatima.bress@tishreen.edu.sy.
Omar Aljanati, Email: Omar.aljanati@tishreen.edu.sy.
Zeina Alkilany, Email: Zeina.alkilany@tishreen.edu.sy.
Aria Mohammed, Email: aria.mohammed@tishreen.edu.sy.
Fatima Kherbek, Email: fatima.kherbek@tishreen.edu.sy.
References
- 1.Richmond E, Rogol J, Alan D, et al. Causes of short stature. UpToDate [pristupljeno 16.6. 2020.]. Dostupno na: https://www. uptodate. com/contents/causes-of-short-stature, 2021
- 2.Bonafe L, Cormier-Daire V, Hall C, et al. Nosology and classification of genetic skeletal disorders: 2015 revision. Am J Med Genet Part A 2015;167A:2869–2892. [DOI] [PubMed] [Google Scholar]
- 3.Patterson SE, Dealy CN. Mechanisms and models of endoplasmic reticulum stress in chondrodysplasia. Dev Dyn. 2014;2437:875–893. [DOI] [PubMed] [Google Scholar]
- 4.Lachman RS, Rimoin DL, Spranger J. Metaphyseal chondrodysplasia, Schmid type. Clinical and radiographic delineation with a review of the literature. Pediatr Radiol 1988;18:93–102. [DOI] [PubMed] [Google Scholar]
- 5.Warman ML, Abbott M, Apte SS, et al. A type X collagen mutation causes Schmid metaphyseal chondrodysplasia. Nat Genet 1993;5:79–82. [DOI] [PubMed] [Google Scholar]
- 6.Richmond CM, Savarirayan R.Schmid Metaphyseal Chondrodysplasia. [Google Scholar]
- 7.Shriraam M, Sridhar M. Subclinical hypothyroidism in children. Indian pediatrics. 2014;51:889–95. [DOI] [PubMed] [Google Scholar]
- 8.Hill ID. Epidemiology, pathogenesis, and clinical manifestations of celiac disease in children. (2020). UpToDate [en línea][consultado el 05/09/2018]. Disponible enwww.uptodate.com/contents/epidemiology-pathogenesis-and-clinical-manifestations-of-celiac-disease-in-children/
- 9.Ranke MB. Short and long-term effects of growth hormone in children and adolescents with GH deficiency. Front Endocrinol 2021;12:720419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agha RA, Franchi T, Sohrabi C, et al. for the SCARE Group. The SCARE 2020 Guideline: Updating Consensus Surgical CAse REport (SCARE) Guidelines. Int J Surg 2020;84:226–230. [DOI] [PubMed] [Google Scholar]
- 11.Alenazi B, AlTamimim F, Albahkali. M. Saudi, growth hormone deficiency in achondroplasia. Eur J Pharm Med Res Case Rep 2017;4:206–208. [Google Scholar]
- 12.Kanazawa H, Tanaka H, Inoue M, et al. Efficacy of growth hormone therapy for patients with skeletal dysplasia. J Bone Miner Metab 2003;21:307–310. [DOI] [PubMed] [Google Scholar]
- 13.Gravholt CH, Viuff MH, Brun S, et al. Turner syndrome: mechanisms and management. Nat Rev Endocrinol 2019;15:601–614. [DOI] [PubMed] [Google Scholar]
- 14.LaFranchi S. Acquired hypothyroidism in childhood and adolescence. (2007). UpToDate (Consultado el 3 de agosto de 2015). [Google Scholar]
- 15.Minelli R, Gaiani F, Kayali S, et al. Thyroid and celiac disease in pediatric age: a literature review. Acta Biomed 2018;89(9-S):11–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Al Kaissi A, Ghachem MB, Nabil NM, et al. Type of Metaphyseal Chondrodysplasia: Diagnosis and Management. Orthop Surg 2018;10:241–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Herzenberg JE, Paley D. Stature lengthening: skeletal dysplasia. In Limb Lengthening and Reconstruction Surgery. CRC Press; 2006:601–622. [Google Scholar]


