Abstract
Congenital heart defects (CHDs) are birth abnormalities that may drastically alter the structure and functionality of the heart. For 70% of infants with congenital disorders to survive or maintain a better quality of life, surgery is necessary. Over 500 000 of the 1.5 million CHD cases reported annually, or 1% of all live births, occur in Africa, according to the WHO. A surmounted 90% of these patients are from Africa, and as a consequence, 300 000 infants die annually as a result of poor care or difficulty accessing adequate healthcare. However, the high prevalence of CHDs, precipitated by a plethora of aetiologies worldwide, is particularly pronounced in Africa due to maternal infectious diseases like syphilis and rubella amongst the pregnant populace. In low- and middle-income countries, especially in Africa, where foreign missions and organizations care for the majority of complicated cardiac surgical patients, access to secure and affordable cardiac surgical therapy is a substantial issue. Interventions for CHDs are very expensive in Africa as many of the continent’s domiciles possess low expenditures and funding, thereby cannot afford the costs indicated by associated surgical treatments. Access to management and healthcare for CHDs is further hampered by a lack of trained surgical personnel, specialized tools, infrastructure, and diagnostic facilities in Africa.
Keywords: Africa, cardiac surgery, congenital heart defects, infant mortality
Highlights
Africa has a severe shortage of skilled cardiac surgeons and other healthcare professionals necessary for cardiac surgery. Many African nations lack certified cardiac surgeons, and the limited workforce hinders the effectiveness of congenital heart defect (CHD) interventions.
Many African countries lack the necessary resources, specialized equipment, and organizations to provide effective diagnostic and treatment interventions for CHDs. Poor diagnostic and treatment involvement rates among locals contribute to challenges in managing CHDs.
The cost of cardiac surgery is often unaffordable for most African countries due to their low-income status. Lack of cardiac surgical care stakeholders during planning processes leads to a lack of inclusion of cardiac surgical services in national healthcare plans.
To improve access to cardiac surgery in Africa, it is recommended to establish long-lasting and sustainable cardiac surgery programs. This can be achieved through collaborations with international groups, regional training programs, and the development of efficient distribution and procurement systems.
Background
Congenital heart defects (CHDs), also known as congenital heart anomalies, impair the anatomy and functionality of the heart. One of the most frequent is congenital heart disease, which has catastrophic and progressive debilitating symptoms. To ensure survival, CHDs require early and intensive medical and surgical healthcare. Complications that outweigh CHDs comprise pulmonary hypertension, pneumonia, congestive hepatopathy, chronic renal disease, and sudden cardiac death due to arrhythmia. Every 100 newborns are diagnosed with a CHD, and 70% necessitate appropriate interventions to either survive or increase their quality of life1. Over 500 000 of the 1.5 million CHD incidences annually, or 1% of all live births, occur in Africa, according to the WHO2. Despite a 34.5% decrease in CHD mortality globally over the previous decade, CHD is currently the 7th leading etiology of newborn mortality in Africa3. The majority of the population lack access to treatment, where financial hardship are adding factors to the rise in CHD mortality3. Maternal infectious diseases such as syphilis and rubella among the pregnant populace are prominent factors in the occurrence of CHDs in Africa4. These communicable diseases also constitute a major factor in the prevalence of CHD worldwide.
Six billion individuals internationally are now denied access to safe and affordable cardiac surgery, with the majority living in low- and middle-income countries (LMICs)5. In Africa, in particular, the public health sector has placed much emphasis on infectious diseases over the past decade due to their high prevalence and mortality. Other public health issues, such as surgical disease and congenital malformations, have not received critical attention. Till date, most multifaceted cardiac surgical inpatients, including CHDs, are handled by foreign missions due to Africa’s limited capacity for cardiac surgery6,7. In Africa, just one surgeon conducts cardiothoracic surgery for every 4 million patients, which accounts for ~1% of the global capacity. Furthermore, the region has a shockingly small number of cardiac surgery facilities, with sub-Saharan Africa (SSA), excluding South Africa, possessing just one facility for every 38 million individuals8 (Fig. 1). In this article, the constraints of cardiac surgery in Africa are discussed, along with the availability of necessary equipment and professional proficiency. Additionally, it aims to draw attention to potential recommendations for improving healthcare accessibility and lowering the number of CHD-related mortalities that may have been avoided.
Figure 1.
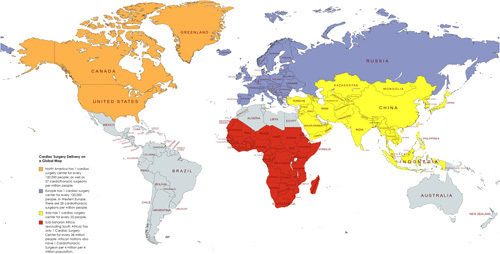
Cardiac surgery delivery representation on a global map (Created with Mapchart.Net)8.
CHD surgical care and limitations in Africa
Governance, cost, and financing
For the governments of the various African nations to have an extremely successful heart surgery program, particularly to aid CHD patients, long-term strategic planning and structures will be warranted. The National Surgical, Obstetric, and Anesthesia Plans (NSOAP) structure has been introduced to healthcare systems globally, but particularly in LMICS, in order to guide and enhance strategy plans9–11. Up until 2021, only six African nations; Zambia, Tanzania, Senegal, Ethiopia, Nigeria, and Rwanda, had developed and hoped to adopt NSOAPs, with several other African nations in the process. However, due to a lack of cardiac surgical care stakeholders during the planning processes, no NSOAP has so far included cardiac surgical services in Africa5.
Cardiac surgery is a complex discipline that requires a significant financial investment. Unfortunately, because most African countries are LMICs, such medical procedures are frequently unaffordable (Fig. 2). The main impediments to expanding surgical intervention in Africa are a lack of administrative capability and poverty4,6. Despite sparsely large government investments in tertiary cardiac surgical centers, there remains a financial burden for the upkeep and expansion of said initiatives. To cut costs, several African countries, including Namibia, Uganda, and Zambia, have implemented co-payment fees for public health services such as cardiac surgery6. However, only 30% of individuals may afford this fee. Also, recent studies in Kenya, Uganda, Tanzania, Cameroon, and Zimbabwe also observed that a substantial proportion of infants necessitating CHD surgery faced cost as the most substantial barrier to their treatment4,12,13. In most African nations, philanthropic groups had to alleviate the expenses for interventions associated with CHD as locals were not able to afford such procedures4,6,12.
Figure 2.
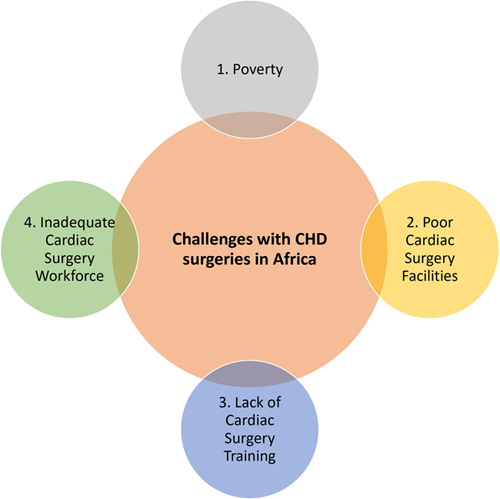
The major obstacles to congenital heart defects surgical delivery in African countries.
The cardiac surgery workforce for CHDs
Particularly in terms of its capacity to perform cardiac surgery, the surgical community in Africa must conform to international standards (Fig. 2). Due to a severe dearth of the interdisciplinary team members necessary for cardiac surgery, such as cardiac surgeons, anesthesiologists, surgical nurses, radiologists, and many others5, the effectiveness of CHD and cardiac surgical intervention is frequently decreased in many African countries. In terms of the number of heart surgeons per million individuals, low-income countries lag far behind high-income countries (HICs)5. In HICs, there are 9.51 pediatric cardiac surgeons and 7.15 adult cardiac surgeons per million individuals, respectively8. Low-income countries, on the contrary, have only 0.04 and 0.07 adult and pediatric cardiac surgeons per 1 million pediatric patients, respectively14.
There are no certified cardiac surgeons in several African nations, notably the Democratic Republic of the Congo (78.7 million individuals) and Ethiopia (102.4 million individuals)8. Additionally, until 2001, no congenital cardiac procedures were performed in Sudan or other underdeveloped African nations, and from 2003 to 2016, only one specialized cardiac physician provided appropriate care15. Another illustration is Zimbabwe, which had just one pediatric cardiothoracic surgeon serving a population of 15.1 million individuals prior to reintroducing the African Pediatric Fellowship Program in 202116. This extreme shortage of skilled surgical workforce to provide appropriate emergency and surgical care has impeded the adoption of better surgical services throughout Africa.
Specialized diagnostics and treatment availability and centers
Unfortunately, most African countries lack the resources, specialized equipment, and organizations mandated to provide effective surgical intervention for CHDs. This is especially noticeable in Nigeria, which has the highest population density in Africa (215 million individuals), where only 13 institutions perform congenital heart surgery, with each facility treating an average of 21 patients annually17.
When deciding on a CHD management strategy, early screening and diagnosis are critical considerations. Access to cardiovascular imaging may be limited in Africa, posing challenges for CHD diagnosis and management. However, particularly in richer African countries, technological and organizational advancements have made it feasible to utilize cardiac catheterization and echocardiography for subsequent diagnosis and treatment. In an Egyptian study, fetal echocardiography was demonstrated to be a highly effective diagnostic tool for detecting and managing CHDs, with a 100% accuracy rate for complex lesions, common atrio-ventricular canals, cono-truncal anomalies, cardiac masses, and fetal arrhythmias18. However, fetal echocardiography and screening programs are not widely available in the majority of these low-income African countries, particularly those in SSA, resulting in a delayed CHD diagnosis. According to one study, the rate of antenatal diagnosis in Sudan was only 1%, while rates in HICs ranged between 10 and 15%19.
In Africa, poor diagnostic and treatment involvement rates among locals have been a substantial issue for decades; this is likely due to a variety of factors, such as low public health awareness and high illiteracy rates. According to a recent study, only a very small percentage of CHD patients in the 27 LMICs attended treatment during relief missions20. The low attendance could indicate that not enough outreach efforts are being made to educate the public regarding the risks associated with CHD and to emphasize the serious consequences if these defects are not rectified.
Surgery may not be the only treatment option for CHDs in Africa. In cases where surgical intervention is deemed infeasible, conservative management has shown promising patient outcomes. For example, optimizing hemoglobin levels, enhancing nutritional status, and prescribing medications have been found an effective management for symptom control alongside improving exercise capacity21,22. Furthermore, interventional therapy, such as cardiac catheterization and device closure, has gained popularity in recent years both globally and in Africa due to its less invasive nature and potential to reduce the financial burden on patients when compared to surgery4. Thus, efforts are being made to address the lack of resources and specialized facilities for CHD diagnosis and treatment in Africa. Increased public health awareness and access to cardiovascular imaging are still vital in enabling earlier CHD diagnosis and management. Further research is warranted to explore alternative management options and ensure patients accessing optimal care.
The state of cardiac surgical education and research capacities
Recently, African nations have turned their attention to developing regionally resilient cardiac programmes. The pediatric cardiac program at Kenya’s Moi Teaching and Referral Hospital is one of many specialized centers and training programmes for cardiac healthcare professionals that have been established with the ultimate goal of establishing a cardiothoracic fellowship and empowering local healthcare providers to make this a foundational program23. Another notable example is Ghana’s National Cardiothoracic Center at the Korle Bu Teaching Hospital, constructed through Ghanaian and German collaboration, to provide formal training for senior cardiothoracic fellows in Ghana and West Africa24. However, many African countries have not widely implemented these training strategies. The lack of a clearly defined cardiothoracic surgical specialty alongside training facilities, and insufficient funding for training programs on the African continent, all pose challenges to cardiac surgical training capacity25 (See Fig. 2). In contrast to Europe and North America, where the need for specialized care was first acknowledged in 197326, Africa requires a more similar response. This could be accomplished by developing comprehensive and intensive training programmes. Aside from the CHD training center in Cairo, Egypt, there is no information on particular CHD facilities in other African countries24.
A needs assessment of three healthcare institutions in SSA revealed that several cardiac surgeons and cardiologists had returned to their home countries to mentor new colleagues after completing their training abroad6. However, on arrival home, only a small number of committed cardiac surgery residents were available for formal training. Numerous factors, including a dearth of funding, mentoring, and approval for postgraduate cardiac surgery training, may contribute to this problem6.
The significant information deficit concerning CHDs and other issues relating to cardiac surgery serves as a warning of the continent’s limited research capacity. The precise scope of the issue cannot be ascertained, where more data on CHD surgery outcomes are warranted. The projections of its frequency and effects on the African continent in the literature may be inaccurate because of underreporting, a lack of relevant research data, and later diagnoses. Our study elucidates that the majority of papers on the continent’s capacity for cardiac surgery and CHD cases are written by nonAfricans. To narrow this gap, more African citizens must be trained to conduct ongoing research into these serious global health cases.
Political climate impact affecting CHD and cardiac surgery care
The influence of sociocultural and political variables frequently hinders the effectiveness of cardiac surgery projects in Africa27,28. The sustainability of such projects is seriously threatened, especially in SSA nations, by widespread corruption, a lack of political will, and unanticipated societal tensions27–29. These issues have been made even more difficult by the region’s protracted, ongoing hostilities, having severe consequences on local healthcare systems causing numerous humanitarian crises. Overcrowding and damage to medical facilities, medical supply disruption, and mass exodus of healthcare personnel due to safety concerns are all becoming more prevalent27,28.
Cameroon provides a clear example of the detrimental impact of conflict on healthcare, particularly for cardiac centers. According to research conducted by Mve et al. 27, the cardiac center located in Shisong faced a plethora of challenges due to its location, poor accessibility, security concerns, and medical material supply disruption peri-conflict. The absence of a practical private-public network alongside financial burden have precipitated the leave of staff from centers. Additionally, the war has had an impact on hospital operations due to a decrease in patient admissions and a scarcity of vital supplies like oil and power. These challenges persist and continue to hinder the development and expansion of healthcare services in the region27,28.
Likewise, similar provocations remain present in a number of African nations29,30. For instance, efforts to develop cardiac surgery programs in Kenya and Sudan have been impeded by a number of pressing issues, such as enduring civil wars and terrorist threats31.
Implications and outcomes of poor CHD and other cardiac surgical challenges on the population
Poor cardiac surgery delivery has a significant negative impact on adequate CHD therapy. CHD is a leading cause of infant heart failure (HF) in some African countries. For example, in a cohort of 58 children in southwestern Uganda, 35% of HF cases were attributable to CHD32.
Many infants are placed on lengthy waiting lists for surgical programmes due to a lack of access, and in some dire circumstances, forced to travel to other foreign countries for effective care4,13. For instance, only 12 of the 158 CHD patients in a cardiac center in Cameroon who were on the waiting list between 2002 and 2008 received local surgery13. Unfortunately, 25 individuals died as a result of their CHD. Long treatment delay times have high fatality rates32. The three main aetiologies of adolescent and early adult mortality in African youths with CHD are cyanosis, pulmonary hypertension, and HF32.
High CHD mortality rates and perioperative outcomes need to be addressed, though these findings are extremely scarce in the literature. A study on the perioperative outcomes of CHD patients, for example, was conducted in a hospital in southeast Nigeria. The study included 20 patients who received CHD surgery at a single facility over a 3.5-year period. The findings of the study elucidated that these patients had a 25% overall mortality rate, with a significant portion of those mortalities occurring within the first 30 postoperative days33. According to the survey, the majority of patients were underprivileged and had delayed access to medical care.
Due to limited data accessibility and underreporting, the true effects of subpar cardiac surgery care provided for CHDs in Africa have been grossly underrated.
Rural Africa is almost completely neglected
It is estimated that 60% of Africans reside in rural areas. For CHD patients, there is a discrepancy in cardiac surgery centers in those areas. Surgery, which has been proven to be a routine life-saving intervention for complex diseases like CHDs34, is only available to urban communities, where only one doctor for every 2.5 million individuals is in remote Africa. Lack of access to healthcare in these areas is a serious issue for many remote communities as no local medical apparatus or expertise for diagnosing and managing CHDs are present4,6,35.
Most rural areas in Africa lack the funding and purchasing power necessary to cover even the most basic medical expenses, let alone the possible cost of CHD procedures. Government funding for healthcare is, for the most part, the only source for these poor and neglected areas13,35. Failure to pay for surgical and medical treatment is one of many factors facilitating the late clinical presentation of CHDs in rural regions4,13,35. It is challenging to provide appropriate therapy due to the high frequency of late presentations.
The massive role of international cooperations
The important efforts made by the international community to prevent CHDs in Africa cannot be overstated. Due to humanitarian contributions from Western countries, such as establishing new open heart surgery programs in Africa, congenital heart surgery is becoming more readily accessible in SSA36. Local teams in South Africa, Côte d’Ivoire, and Ghana have completed these procedures with early fatality rates of less than 4%36. With early mortality rates following CHD surgery in children as low as 3.2%, studies demonstrate that these nations’ outcomes are comparable to those of wealthier nations36. The success of managing more than 1000 patients in SSA and the low mortality rate demonstrate the value of humanitarian aid in improving the well-being of African children with CHD36.
Another noteworthy project is the extensive work of the Italian nongovernmental organization (NGO) Associazione Bambini Cardiopatici nel Mondo, which has constructed more than two pediatric tertiary cardiac centers in Africa and trained local experts in collaboration with the UK-based NGO Chain of Hope7. Through twinning agreements and short-term staff exchanges, Children’s Heartlink, a distinct nonprofit organization headquartered in the USA, has also worked with various African cardiac hospitals to train staff and specialists7. Additionally, a partnership between Uganda and the Children’s National Medical Center in Washington, DC, has allowed for the resolution of many congenital cases6. All these efforts have helped save thousands of lives and improve treatment outcomes for CHDs on the African continent.
Future perspectives
Addressing the shortage of skilled cardiac surgeons and training programs in Africa
A number of measures used to address the lack of trained cardiac surgeons in Africa may be implemented. One strategy is to offer incentives, such as greater compensation, opportunities for professional advancement, and better working conditions, to draw and retain experienced cardiac surgeons in Africa (Fig. 3). This will provide the continent more access to highly qualified specialists who can manage cardiac patients effectively.
Figure 3.

Recommendations and Strategies to Improve Congenital Heart Disese Care in Africa.
Establishing public-private partnerships that offer financial and technical support for the training of cardiac surgeons is another crucial stratagem. To provide the resources required to train more cardiac surgeons, cooperating with the commercial sector is paramount. The retention of qualified workers must also be a priority of high intention. In recent years, physician migration from Africa to more industrialized countries has significantly increased due to improved employment opportunities and living circumstances. To address this issue, cardiac staffing and healthcare workforce planning need to be generally improved (Fig. 3). This comprises increased staff training investment and redistribution to areas of need, as well as financial incentives for healthcare staff retention, similar to the successful actions accomplished in Ethiopia37.
Furthermore, the lack of cardiac surgeons in Africa may be resolved by collaborating with networks and professional groups to recruit qualified cardiac surgeons from the African diaspora. It is necessary to facilitate efforts to develop international partnerships that concentrate on staff training at specialized institutions in Africa to enhance the number of exchange programs and fellowships accessible. Profound examples include initiatives from Duke University that concentrate on educating physicians to develop long-lasting, comprehensive cardiac and cardiovascular care programs in Kenya38.
Moreover, it is essential to address the dearth of specialists who have the education and experience needed to handle the complexities of CHDs, thereby effectively encouraging international cooperation that focuses on staff development at African specialist institutions.
Improving access to cardiac surgery services
Improving access to cardiac services is critical when combating CHD in Africa. Continual improvement and expansion of healthcare systems is one of the primary methodologies when achieving this objective. The Cape Town Declaration, aiming to improve cardiac surgical access in developing countries, identified the establishment of specialized cardiac surgery units as a promising strategy. Programs like these have been successful in countries like South Africa39.
In addition, developing and strengthening referral networks is crucial when ensuring prompt, timely referrals to cardiac surgery centers for patients with CHDs. Linking primary care facilities, referral hospitals, and cardiac surgery centers may facilitate the process.
Telemedicine is another effective tool to ameliorate access to cardiac surgery services. Remote consultations between cardiac surgeons and healthcare providers in more rural areas may aid in reducing the need for patients to travel long distances to access care (Fig. 3). By implementing these strategies, the accessibility of cardiac surgery services in Africa may be improved, allowing more individuals to receive the necessary care to combat cardiac disease.
Developing sustainable cardiac surgery programs
To provide high-quality CHD interventions in Africa, it is essential to establish long-lasting cardiac surgery initiatives that are sustainable over time without requiring external financing. A multitude of strategies might be employed to achieve this. Initially, dynamic collaboration with international groups may aid in the creation and upkeep of initiatives for cardiac surgery via the provision of both financial and technical assistance. This may include training local cardiac surgeons in developed nations to increase capability in Africa. Partners from other domiciles may also provide the equipment, materials, and expertise needed to support the cardiac care facilities in Africa.
Furthermore, it is important to create regional training programs for healthcare professionals and surgeons to maintain a self-sufficient, high-quality cardiac care system. These programs should be specialized for CHDs in pediatric populations as are often diagnosed in childhood (Fig. 3). Additionally, it is paramount for healthcare professionals to stay up-to-date with the latest advancements in cardiac surgery through continuing medical education and training programs.
Lastly, a functional distribution and procurement system must be established to ensure patient safety with cardiac disease in Africa having access to the required care. Depending on the unique requirements of each nation, either a centralized or decentralized system may be employed. The objective is to ensure that medical supplies and equipment are available in a timely and efficient manner to improve access to care for those with CHDs.
Making cardiac surgery more affordable
Improving access to cardiac surgery for individuals with CHDs in Africa requires reducing the cost of care. Governments and NGOs may provide financial assistance to families in need, including grants, loans, and subsidies, to help cover the cost of hospital admissions, surgical procedures, and postoperative care.
In addition, negotiating the pricing of medical equipment and supplies can also reduce the cost of heart surgery. Governments and healthcare organizations can work directly with suppliers or use bulk purchase agreements to negotiate lower costs. By decreasing the overall cost of cardiac surgery, interventions may become more accessible to those who need it.
Furthermore, there are less expensive alternatives to surgery for the management of cardiac disease. These approaches might nevertheless be a useful substitute for those who cannot afford more expensive medical treatment, despite being less effective than their more expensive counterparts. By facilitating these strategies, the cost of cardiac surgery may be reduced, allowing for patients with CHDs in Africa more affordable and accessible healthcare.
Mitigating the impact of the political climate on cardiac surgery care provision and capacity in African countries
As previously addressed and elucidated, one of the significant obstacles to the sustainability of these projects is the prevalence of corruption and a lack of political will. Thus, governments should take action to address political corruption alongside aid anticorruption agencies and regulations.
To improve resilience to ongoing hostilities and humanitarian crises in local healthcare systems, investments in upgrading facility infrastructure, a steady supply of necessary medications and supplies, and public-private partnerships, are crucial. Political stability is also essential for the long-term growth of healthcare systems. Efforts should be undertaken to advance political stability by effective leadership, dispute resolution, and the strengthening of democratic institutions. In conflict-affected domiciles, establishing and strengthening private-public partnerships may help develop sustainable and resilient healthcare systems. Accessibility to healthcare services may be increased by establishing mobile clinics, and other innovative approaches to healthcare delivery that can reach patients who are unable to travel to healthcare facilities.
Furthermore, healthcare organizations and governments should prioritize the training and retention of healthcare professionals in conflict-affected regions (Fig. 3). Targeted training programs, incentives for healthcare professionals, and the provision of adequate resources and support may help healthcare professionals perform their duties more effectively. Finally, it is critical to address the root causes of violence and instability in these regions to provide a more secure and stable environment for the delivery of healthcare. Diplomatic efforts, attempts for conflict resolution, and monetary expenditures in socioeconomic development may all be utilized to address the core aetiologies of violence and instability.
By implementing these recommendations, we can ensure that healthcare services, including cardiac surgery programs, are accessible and sustainable even in politically unstable regions of Africa.
Conclusion
Africa’s cardiac surgery capacity to manage CHDs remains a significant challenge. The limited access to quality healthcare, inadequate funding, and lack of sufficient medical expertise continue to hinder the provision of appropriate care for CHD patients in Africa. Furthermore, the high mortality rates associated with CHD procedures in Africa highlight the need for more investment in cardiac surgery infrastructure and training programs. However, efforts made by the international community in providing humanitarian aid and establishing cardiac surgery programs in Africa have improved the prognosis and outcomes for CHD patients profoundly. Nonetheless, there is still much to be done in addressing the systemic issues that perpetuate subpar healthcare delivery for CHDs in Africa. Further research is warranted to better comprehend the implications of poor cardiac surgery on the African population and to develop effective solutions to improve regional cardiac surgery capacity. With appropriate investments and partnerships, it is possible to overcome these challenges and provide better care to CHD patients in Africa, thus improving their quality of life and reducing preventable deaths.
Ethical approval
Not applicable.
Consent
Not applicable.
Source of funding
The authors did not receive any financial support for this work.
Author contribution
W.A.A.: conceptualized the ideas; W.A.A., F.T.A., J.W., S.G., P.O.T., P.N.M.M., T.A.- R., S.M., A.S., and M.P.: reviewed and edited the manuscript. All authors were involved in the initial draft.
Conflicts of interest disclosure
The authors declare that there is no conflict of interest.
Research registration unique identifying number (UIN)
Name of the registry: not applicable.
Unique Identifying number or registration ID: not applicable.
Hyperlink to your specific registration (must be publicly accessible and will be checked): not applicable.
Guarantor
Favor tope Adebusoye.
Data availability statement
No data available.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 8 July 2023
Contributor Information
Wireko A. Awuah, Email: andyvans36@yahoo.com.
Favour T. Adebusoye, Email: Favouradebusoye@gmail.com.
Jack Wellington, Email: wellingtonj1@cardiff.ac.uk.
Shankhaneel Ghosh, Email: shankhaneelghosh1234@gmail.com.
Pearl O. Tenkorang, Email: pearltenkorang3@gmail.com.
Paciencia N.M. Machai, Email: macselemp@gmail.com.
Toufik Abdul-Rahman, Email: Drakelin24@gmail.com.
Shyamal Mani, Email: shyamalmani645@gmail.com.
Abdus Salam, Email: salam.elum@gmail.com.
Marios Papadakis, Email: marios_papadakis@yahoo.gr.
References
- 1.Zheleva B, Atwood JB. The invisible child: childhood heart disease in global health. Lancet 2017;389:16–18. [DOI] [PubMed] [Google Scholar]
- 2.GBD 2017 Congenital Heart Disease Collaborators. Global, regional, and national burden of congenital heart disease, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Child Adolesc Health 2020;4:185–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rossouw B. Congenital heart disease in Africa threatens sustainable development goals. South Afr J Crit Care 2021;37:8–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jivanji SGM, Lubega S, Reel B, et al. Congenital heart disease in East Africa. Front Pediatr 2019;7:250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vervoort D, Swain JD, Pezzella AT, et al. Cardiac surgery in low- and middle-income countries: a state-of-the-art review. Ann Thorac Surg 2021;111:1394–1400. [DOI] [PubMed] [Google Scholar]
- 6.Forcillo J, Watkins DA, Brooks A, et al. Making cardiac surgery feasible in African countries: experience from Namibia, Uganda, and Zambia. J Thorac Cardiovasc Surg 2019;158:1384–93. [DOI] [PubMed] [Google Scholar]
- 7.Hewitson J, Zilla P. Children’s heart disease in sub-Saharan Africa: challenging the burden of disease: children’s heart disease. Sa Heart 2010;7:18–29. [Google Scholar]
- 8.Vervoort D, Meuris B, Meyns B, et al. Global cardiac surgery: access to cardiac surgical care around the world. J Thorac Cardiovasc Surg 2020;159:987–996.e6. [DOI] [PubMed] [Google Scholar]
- 9.Peters AW, Roa L, Rwamasirabo E, et al. National surgical, obstetric, and anesthesia plans supporting the vision of universal health coverage. Glob Health Sci Pract 2020;8:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Albutt K, Sonderman K, Citron I, et al. Healthcare leaders develop strategies for expanding national surgical, obstetric, and anaesthesia plans in WHO AFRO and EMRO regions. World J Surg 2019;43:360–367. [DOI] [PubMed] [Google Scholar]
- 11.Sonderman KA, Citron I, Mukhopadhyay S, et al. Framework for developing a national surgical, obstetric and anaesthesia plan. BJS Open 2019;3:722–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Raphael DM, Roos L, Myovela V, et al. Heart diseases and echocardiography in rural Tanzania: Occurrence, characteristics, and etiologies of underappreciated cardiac pathologies. PloS One 2018;13:e0208931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tantchou Tchoumi JC, Butera G, Giamberti A, et al. Occurrence and pattern of congenital heart diseases in a rural area of sub-Saharan Africa: cardiovascular topics. Cardiovasc J Afr 2011;22:63–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vervoort D, Ma X, Luc JG. Addressing the cardiovascular disease burden in China—is it possible without surgery? JAMA Cardiol 2019;4:952–953. [DOI] [PubMed] [Google Scholar]
- 15.Aliku TO, Lubega S, Lwabi P, et al. Outcome of patients undergoing open heart surgery at the Uganda heart institute, Mulago hospital complex. Afr Health Sci 2014;14:946–953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoosen EG, Cilliers AM, Brown S, et al. Improving access to pediatric cardiac care in the developing world: the South African perspective. Curr Treatm Opt Ped 2022;8:141–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Su Z, Zou Z, Hay SI, et al. Global, regional, and national time trends in mortality for congenital heart disease, 1990-2019: An age-period-cohort analysis for the Global Burden of Disease 2019 study. EClinMed 2022;43:101249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Fahham MM, Gad NA, Ramy AR, et al. Clinical utility of fetal echocardiography: an Egyptian center experience. Egypt Heart J 2021;73:1–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elshazali Osama H, Abdullahi H, Hes O. Assessment of quality of counselling for down syndrome in Sudan. J Ped Neonatal Care 2018;8:232–234. [Google Scholar]
- 20.Cardarelli M, Polivenok I, Chadikovski V, et al. Prevalence of critical congenital heart disease during surgical mission trips to low-middle income countries. What to expect. J Humanit Cardiovasc Med 2022;1:14. [Google Scholar]
- 21.Woldesenbet R, Murugan R, Mulugeta F, et al. Nutritional status and associated factors among children with congenital heart disease in selected governmental hospitals and cardiac center, Addis Ababa Ethiopia. BMC Pediatr 2021;21:538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Doumbia AK, Koné O, Dembélé A, et al. Congenital heart disease in newborns: epidemiological and clinical particularities in a neonatology department in Mali. Open J Pediatr 2022;12:857–66. [Google Scholar]
- 23.Grant Enables Expansion of Cardiac Surgery at MTRH. AMPATH Kenya 2022. Accessed 3 April 2023. https://www.ampathkenya.org/news-blog-feed/2022/5/21/grant-enables-expansion-of-cardiac-surgery-at-mtrh
- 24.Edwin F, Entsua-Mensah K, Sereboe LA, et al. Conotruncal heart defect repair in Sub-Saharan Africa: remarkable outcomes despite poor access to treatment. World J Pediatr Congenit Heart Surg 2016;7:592–599. [DOI] [PubMed] [Google Scholar]
- 25.Edwin F, Zühlke L, Farouk H, et al. Status and challenges of care in Africa for adults with congenital heart defects. World J Pediatr Congenit Heart Surg 2017;8:495–501. [DOI] [PubMed] [Google Scholar]
- 26.Perloff JK. Pediatric congenital cardiac becomes a postoperative adult. The changing population of congenital heart disease. Circulation 1973;47:606–619. [DOI] [PubMed] [Google Scholar]
- 27.Mve Mvondo C, Giamberti A, Ngowe Ngowe M, et al. Cardiac surgery development in cameroon: unexpected challenges from a socio-political crisis. Front Cardiovasc Med 2022;9:253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Djankou TL, Albonico V. Emergency relocation of a cardio-surgical health facility due to war. Glob Clin Eng J 2020;2:39–49. [Google Scholar]
- 29.Nwiloh J, Smit F, Mestres C, et al. Challenges to providing open heart surgery for 186 million Nigerians. Niger J Cardiovasc Thorac Surg 2018;3:8–13. [Google Scholar]
- 30.Cristiano S, Ulgiati S, Gonella F. Systemic sustainability and resilience assessment of health systems, addressing global societal priorities: learnings from a top nonprofit hospital in a bioclimatic building in Africa. Renewab Sustain Energy Rev 2021;141:110765. [Google Scholar]
- 31.Nwafor IA, Eze JC, Anyanwu CH, et al. The scope of cardiac surgery at a national cardiothoracic center of excellence (NCTCE) in Nigeria: a 3 year review. J Vasc Med Surg 2017;5:2. [Google Scholar]
- 32.Zühlke L, Mirabel M, Marijon E. Congenital heart disease and rheumatic heart disease in Africa: recent advances and current priorities. Heart 2013;99:1554–1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nwafor IA, Eze JC. Status of congenital heart defects in Nigeria: the role of cardiac surgery.. World J Cardiovas Surg 2019;9:63–72. [Google Scholar]
- 34.Scaling up Safe Surgery for District and Rural Populations in Africa. [Accessed 3 April 2023] https://cordis.europa.eu/project/id/733391
- 35.Mazhani T, Steenhoff AP, Tefera E, et al. Clinical spectrum and prevalence of congenital heart disease in children in Botswana. Cardiovasc J Afr 2020;31:257–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yangni-Angate KH, Meneas C, Diby F, et al. Cardiac surgery in Africa: a thirty-five year experience on open heart surgery in Cote d’Ivoire. Cardiovasc Diagn Ther 2016;6(suppl 1):S44–S63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Derbew M, Laytin AD, Dicker RA. The surgical workforce shortage and successes in retaining surgical trainees in Ethiopia: a professional survey. Hum Resour Health 2016;14:105–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Partner Spotlight: Cardiac Care Unit Addressing Dire Need in Kenya. (2015). Accessed 15 May 2023 https://globalhealth.duke.edu/news/partner-spotlight-cardiac-care-unit-addressing-dire-need-kenya.
- 39.Zilla P, Bolman RM, Yacoub MH, et al. The Cape Town Declaration on access to cardiac surgery in the developing world. Cardiovasc J Afr 2018;29:256–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data available.


