Abstract
This study aims to compare the outcomes of interlaminar and transforaminal approaches for full-endoscopic discectomy (FED) for treating L4/5 lumbar disc herniation (LDH).
A retrospective study of patients with L4/5 LDH treated with interlaminar endoscopic lumbar discectomy (IELD, n = 19) or transforaminal endoscopic lumbar discectomy (TELD, n = 105) was conducted. Patient background, radiological findings, and operative data were collected. Oswestry Disability Index (ODI) and European Quality of Life-5 Dimension (EQ-5D) scores were recorded preoperatively and 1 and 2 years postoperatively.
Although ODI and EQ-5D scores 1 and 2 years postoperatively improved statistically in the IELD and TELD groups, there were no statistical differences between the groups. IELD was predominantly performed in patients who were taller and heavier. The mean operative times and the frequency of laminectomy for IELD and TELD were 67.2 and 44.6 min and 63.2 and 17.1%, respectively (P < 0.001). The radiological findings showed that the concave configuration of the L4 lamina, interlaminar space width, and foraminal width were statistically different between the groups. There were no complications in either of the groups. Reoperation was required for recurrence in two and five patients in the IELD and TELD groups (P = 0.29), respectively.
Operative outcomes were identical between the two groups. Although the operative time was longer in the IELD group, both approaches were safely and effectively performed. Depending on the patient's physique and preoperative radiological findings, the more suitable approach for L4/5 LDH should be chosen.
Keywords: lumbar disc herniation, full-endoscopic discectomy, minimally invasive, interlaminar approach, transforaminal approach
Introduction
Several strategies are available for the treatment of lumbar disc herniation (LDH). Among them, full-endoscopic discectomy (FED) has attracted attention as a minimally invasive spinal surgery.1-3) There are several different approaches for FED, such as interlaminar, transforaminal, posterolateral, and translaminar, but comparisons between the different approaches have not been well discussed. One reason is that each approach is suitable for a particular LDH type: the posterolateral approach is suitable for foraminal and extraforaminal LDH, whereas the translaminar approach is suitable for highly migrated LDH.4,5) It is reasonable to select a large bone window to insert the endoscope. Therefore, the interlaminar approach [interlaminar endoscopic lumbar discectomy (IELD)] is preferentially selected for patients with a large interlaminar space, such as L5/S1 intracanal LDH.6) Conversely, the transforaminal approach [transforaminal endoscopic lumbar discectomy (TELD)] is preferentially selected for patients with large vertebral foramen such as L1/2, L2/3, and L3/4 intracanal LDH.7)
L4/5 intracanal LDH has intermediate characteristics between those of L5/S1 and L3/4; hence, spine surgeons frequently waver in the selection of IELD or TELD. There are several comparative analyses between IELD and TELD,8-21) but studies limited to L4/5 intracanal LDH are few.12,21) Furthermore, previous studies did not strictly analyze preoperative radiological factors that affect the approach selection. Therefore, in this study, we firstly compared the short- and long-term operative outcomes between IELD and TELD for the treatment of L4/5 intracanal LDH and then tried to identify the factors that affect approach selection.
Materials and Methods
Study design
Retrospective comparative study.
Patient selection
A total of 311 consecutive patients with L4/5 LDH who underwent discectomy using a 4.1-mm working-channel endoscope (RIWOspine GmbH, Knittlingen, Germany) between January 2016 and March 2020 were recruited for the study. All patients had apparent L5 radiculopathy that was resistant to medical treatment, epidural steroids, and/or nerve blocks. All patients underwent discectomy at the L4/5 vertebral level only. Foraminal and extraforaminal LDHs were excluded because FED has a distinct advantage over other posterior approaches (open, microscopic, and microendoscopic) for these types of LDH.4) We also excluded patients for whom we could not distinguish whether the radiculopathy was caused by combined L4/5 lumbar canal stenosis or other diseases (infection, discal cyst, and progressive supranuclear palsy). A total of 132 patients were excluded due to the difficulties in obtaining follow-up data.
The study was conducted in accordance with the ethical standards of the institutional research committee (IRB No: 20200507) and the 1964 Helsinki Declaration. Informed consent was obtained from the patients for the surgical procedure.
Data collection
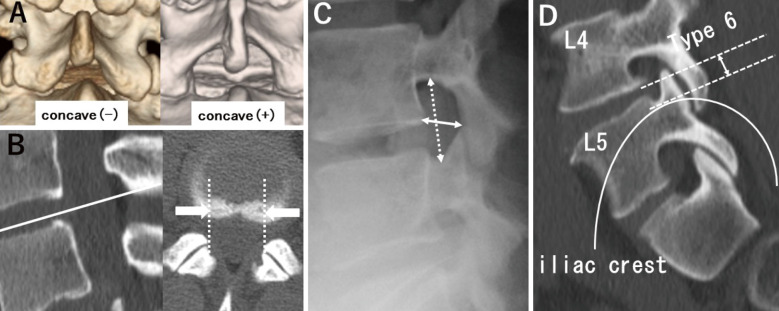
Patient characteristics, including age, sex, height, weight, body mass index (BMI), and radiculopathy side, were collected (Table 1). Preoperative plain radiographs were obtained, and T2-weighted magnetic resonance imaging (MRI) and computed tomography (CT) were performed to determine the characteristics of LDH (type, size, and degree of migration), the vertebral lamina [existence of a concave configuration and width of the interlaminar space (ILS)], the vertebral foramen (height and width), and the position of the iliac crest (Fig. 1). LDH was divided into three types based on axial MRI scans: shoulder/ventral, central, and axillary. Although L5/S1 LDH was divided into four types (shoulder, ventral, central, and axilla) in the original paper,6) it was difficult to distinguish between the ventral and shoulder types in L4/5 LDH due to the narrower spinal canal. Therefore, we considered the shoulder and ventral types as a single entity in this study. The migration extent was consistent with Lee's classification (Supplementary Fig. 1).22) Types 2 and 3 were combined as near-migration, whereas types 1 and 4 were combined as far-migration. The LDH size (anteroposterior size ratio) was evaluated by measuring the height of the protrusion against the anteroposterior diameter of the spinal canal. A concave (−) shape was defined as a straight caudal margin of the upper vertebral laminae (CM-UVL), as evaluated using three-dimensional CT, whereas a concave (+) shape was defined as a CM-UVL with a measurable concavity (Fig. 1A).23) The ILS width was calculated using axial CT and was determined as the widest distance between the bilateral facet joints at the corresponding disc level (Fig. 1B).6) Foraminal height was measured as the maximum distance between the inferior margin of the pedicle of the superior vertebra and the superior margin of the pedicle of the inferior vertebra. The foraminal width was measured as the shortest distance between the superior edge of the superior articular process of the caudal vertebra and the posterior edge of the inferior endplate of the cranial vertebra (Fig. 1C).24) Type 6 is the point between the upper margin of the L5 pedicle and the lower endplate of L4 vertebral body. We divided to types 1-5 and type 6 and defined type 6 as a high iliac crest (Fig. 1D).25)
Table 1.
Demographic data of 124 patients
| Variables | IELD (N = 19) | TELD (N = 105) | p value | |
|---|---|---|---|---|
| Age, mean (SD) | 46.4 (17.0) | 44.8 (14.9) | 0.69 | |
| Sex (male) [n (%) ] | 16 (84.2%) | 69 (65.7%) | 0.18 | |
| Body height (cm), mean (SD) | 173.2 (8.0) | 166.7 (7.4) | <0.001 | |
| Bodyweight (kg), mean (SD) | 72.2 (13.6) | 64.6 (13.5) | 0.03 | |
| BMI | 23.7 (3.3) | 23.1 (3.9) | 0.55 | |
| Radiculopathy side * | 0.80 | |||
| R [n (%) ] | 11 (57.9%) | 55 (52.4%) | ||
| L [n (%) ] | 8 (42.1%) | 50 (47.6%) | ||
| Preoperative NRS, mean (SD) | 6.8 (2.2) | 6.6 (2.3) | 0.75 | |
| Preoperative ODI, mean (SD) | 41.0 (13.6) | 44.6 (18.9) | 0.42 | |
| Preoperative EQ-5D, mean (SD) | 0.53 (0.14) | 0.51 (0.20) | 0.61 |
*When the patients complained of bilateral radiculopathy, we considered the side where the radiculopathy was more severe. BMI, body mass index; IELD, interlaminar endoscopic lumbar discectomy; TELD, transforaminal endoscopic lumbar discectomy; SD, standard deviation; NRS, numerical rating scale; ODI, Oswestry Disability Index; EQ-5D, European Quality of Life-5 Dimensions
Fig. 1.
Preoperative radiological findings on the vertebral lamina, vertebral foramen, and iliac crest. (A) A concave (−) shape was defined as a straight caudal margin of the upper vertebral laminae (CM-UVL), as evaluated using three-dimensional CT, whereas a concave (+) shape was defined as a CM-UVL with a measurable concavity. (B) The interlaminar space (ILS) width was calculated using axial CT and determined as the widest distance between the bilateral facet joints at the corresponding disc level (between two white arrows). (C) Foraminal height was measured as the maximum distance between the inferior margin of the pedicle of the superior vertebra and the superior margin of the pedicle of the inferior vertebra (solid line). The foraminal width was measured as the shortest distance between the superior edge of the superior articular process of the caudal vertebra and the posterior edge of the inferior endplate of the cranial vertebra (dotted line). (D) The highest point of the iliac crest was classified using Choi’s classification. Type 6 is the point between the upper margin of the L5 pedicle and the lower endplate of L4 vertebral body. We divided to types 1-5 and type 6 and defined type 6 as high iliac crest.
Data on the operative time, mean volume of the removed nucleus pulposus, performance of laminectomy, intraoperative bleeding, postoperative hospital stay, recurrence, and operative complications were obtained from the medical records (Table 2). Intraoperative bleeding was calculated by subtracting the amount of saline irrigation from the suctioned amount. As 3 mL was the lowest data obtained using this formula, 3 mL was determined as the limit and unmeasurable cases were recorded as 3 mL. Short-term operative outcomes were evaluated using the numerical rating scale (NRS) at hospital admission and discharge. Long-term outcomes were evaluated using the pre- and postoperative Oswestry Disability Index (ODI) scores (ranging from 0 to 100; higher scores indicate back pain-related disability) and the European Quality of Life-5 Dimension (EQ-5D) scores (ranging from 0 to 1; higher scores indicate better quality of life).26,27) Postoperative ODI and EQ-5D scores were obtained at 1 and 2 years postoperatively (Table 2).
Table 2.
Univariate analysis of operative outcomes
| Variables | IELD (N = 19) | TELD (N = 105) | p value | |
|---|---|---|---|---|
| Operative time (min), mean (SD) | 67.2 (21.5) | 44.2 (17.5) | <0.001 | |
| Frequency of laminectomy [n (%) ] | 12 (63.2%) | 18 (17.1%) | <0.001 | |
| Mean volume of removed nucleus pulposus (g), mean (SD) | 0.71 (0.67) | 1.08 (0.85) | 0.07 | |
| Intraoperative bleeding (mL), mean (SD) | 3.7 (2.2) | 6.5 (29.0) | 0.68 | |
| Postoperative hospital stay (days), mean (SD) | 1.5 (0.9) | 1.5 (0.9) | 0.98 | |
| Complications | Dural tear [n (%)] | 0 (0) | 0 (0) | 1 |
| Postoperative
hematoma [n (%)] |
0 (0) | 0 (0) | 1 | |
| Recurrent LDH [n (%) ] | 2 (10.5%) | 5 (4.8%) | 0.29 | |
| NRS at discharge, mean (SD) | 1.5 (1.4) | 1.4 (1.7) | 0.8 | |
| ODI 1 year, mean (SD) | 10.3 (12.4) | 11.4 (10.7) | 0.69 | |
| ODI 2 years, mean (SD) | 13.1 (13.1) | 11.8 (10.1) | 0.68 | |
| EQ-5D 1 year, mean (SD) | 0.87 (0.17) | 0.84 (0.16) | 0.52 | |
| EQ-5D 2 years, mean (SD) | 0.86 (0.15) | 0.84 (0.14) | 0.84 |
IELD, interlaminar endoscopic lumbar discectomy; TELD, transforaminal endoscopic lumbar discectomy; SD, standard deviation; LDH, lumbar disc herniation; NRS, numerical rating scale; ODI, Oswestry Disability Index; EQ-5D, European Quality of Life-5 Dimensions
Statistical analysis
Demographic data and outcome measures were compared between the two groups using a t-test and chi-square test for continuous and categorical variables, respectively. Pre- and postoperative outcome measures were compared using a paired t-test. All analyses were performed using STATA (version 16.0, Stata Corp. LLC, College Station, TX, USA). A two-sided P-value of <0.05 is considered statistically significant.
Surgical technique
Patients were carefully logrolled into the prone position. Both IELD and TELD were performed under general anesthesia (total intravenous anesthesia with propofol and remifentanil) with motor-evoked potential monitoring. During the surgery, a fluoroscope was placed across the center of the operating table to ensure appropriate timing. Nine skilled surgeons performed FED using a 4.1-mm working-channel endoscope. They each had more than 5 years of experience in spinal surgery and have received advanced training in FED. An 8-mm skin incision was made 5-10 mm and 80-120 mm lateral to the midline for IELD or TELD, respectively. The basic operative procedure has been previously described.4,6,7)
Results
Table 1 summarizes the patients' demographic data. This retrospective study included 19 and 105 patients with L4/5 LDH in the IELD (16 men and 3 women) and TELD (69 men and 46 women) groups, respectively. The mean age at surgery was 46.4 and 44.8 years in the IELD and TELD groups, respectively. The mean height and weight were 173.2 cm and 72.2 kg in the IELD group and 166.7 cm and 64.6 kg in the TELD group, respectively. The mean BMI was 23.7 and 23.1 in the IELD and TELD groups, respectively. There were statistically significant differences in the heights and weights of the patients between the two groups (Table 1).
The NRS score was used to evaluate the early effects on leg pain. The preoperative NRS score (6.8 ± 2.2) in the IELD group improved significantly postoperatively (1.5 ± 1.4; P < 0.001). The preoperative NRS score (6.6 ± 2.3) in the TELD group also improved significantly postoperatively (1.4 ± 1.7; P < 0.001). However, there was no significant difference in the leg pain evaluation at discharge between the IELD and TELD groups (Table 2).
There was a significant difference in the mean operative time between the IELD and TELD groups (67.2 ± 21.5 min vs. 44.2 ± 17.5 min; P < 0.001), as well as in the frequency of laminectomy (63.2% vs. 17.1%; P < 0.001). There were no significant differences in the mean volume of the removed nucleus pulposus, intraoperative bleeding, and postoperative hospital stay between the IELD and TELD groups. There were no major complications, such as dural tears or postoperative hematoma, in either of the groups. During the first 2 years postoperatively, reoperation for recurrent LDH was performed in two (10.5%) and five (4.8%) patients in the IELD and TELD groups, respectively. However, there were no significant differences in the complications or recurrence between the two groups.
The preoperative ODI scores in the IELD and TELD groups (41.0 ± 13.6 vs. 44.6 ± 18.9) improved significantly postoperatively at the 1-year follow-up (10.3 ± 12.4 vs. 11.4 ± 10.7; P < 0.001) and remained approximately the same at the 2-year follow-up (11.4 ± 10.7 vs. 11.8 ± 10.1). The preoperative EQ-5D scores in the IELD and TELD groups (0.53 ± 0.14 vs. 0.51 ± 0.20) also improved significantly postoperatively at the 1-year follow-up (0.87 ± 0.17 vs. 0.84 ± 0.16; P < 0.001) and remained approximately the same at the 2-year follow-up (0.86 ± 0.15 vs. 0.84 ± 0.14). However, the ODI and EQ-5D scores at each time point were not significantly different between the two groups.
We then compared the preoperative plain radiographs, MRI, and CT images between the two groups and attempted to identify the factors that affected the approach selection. Although there were no significant differences in the LDH size and migration and vertebral foramen height (Table 1), there were significant differences in other radiological findings between the IELD and TELD groups. There was a significant difference in the LDH type between the two groups (P = 0.028). TELD was preferentially selected for the central LDH type (47.6%), whereas IELD was preferentially selected for the axilla LDH type (15.8%). There was a significant difference in the L4 vertebral lamina configuration between the two groups (P < 0.001). IELD was preferentially selected for the concave (+) configuration (78.9%), whereas TELD was preferentially selected for the concave (−) configuration (78.1%). There was a significant difference in the ILS width between the two groups (P < 0.001); the mean ILS width was 25.05 ± 3.31 mm and 20.64 ± 3.20 mm in the IELD and TELD groups, respectively. There was a significant difference in the vertebral foramen width between the two groups (P < 0.02); the mean vertebral foramen width was 8.98 ± 2.44 mm and 10.24 ± 2.18 mm in the IELD and TELD groups, respectively (Table 3). There was a significant difference in the iliac crest position between the groups (P = 0.02). IELD was preferentially selected for patients with a high iliac crest (63.2%), whereas TELD was preferentially selected for those without a high iliac crest (66.3%).
Table 3.
Univariate analysis of radiological findings
| Variables | IELD (N = 19) | TELD (N = 105) | p value | |
|---|---|---|---|---|
| LDH type | Central | 4 (21.1%) | 50 (47.6%) | 0.03 |
| Ventral | 12 (63.2%) | 51 (48.6%) | ||
| Axilla | 3 (15.8%) | 4 (3.8%) | ||
| Size of LDH* | Mean | 0.50 | 0.53 | 0.28 |
| SD | 0.12 | 0.15 | ||
| LDH migration | (−) | 1 (5.3%) | 30 (28.6%) | 0.06 |
| Near-migration | Zone 2/3 | 15 (78.9%) | 64 (61.0%) | |
| Far-migration | Zone 1/4 | 3 (15.8%) | 11 (10.5%) | |
| Configuration of L4 vertebral lamina | Concave + | 15 (78.9%) | 23 (21.9%) | <0.001 |
| Concave − | 4 (21.1%) | 82 (78.1%) | ||
| ILS width | Mean (mm) | 25.05 | 20.64 | <0.001 |
| SD | 3.31 | 3.20 | ||
| Vertebral foramen | ||||
| Height | Mean (mm) | 18.11 | 19.26 | 0.07 |
| SD | 2.77 | 2.47 | ||
| Width | Mean (mm) | 8.98 | 10.24 | 0.02 |
| SD | 2.44 | 2.18 | ||
| Iliac crest position | Type 6 | 12 (63.2%) | 35 (33.7%) | 0.02 |
| ≤Type 5 | 7 (36.8%) | 69 (66.3%) |
*Size of LDH was calculated using the anteroposterior size ratio. IELD, interlaminar endoscopic lumbar discectomy; TELD, transforaminal endoscopic lumbar discectomy; LDH, lumbar disc herniation; SD, standard deviation; ILS, interlaminar space
Discussion
Although there are several comparative analyses of IELD and TELD,8-21) studies limited to L4/5 intracanal LDH are very few.12,21) Furthermore, most of the studies do not distinguish between the different vertebral levels and LDH types (e.g., intracanal, foraminal, or extraforaminal). Among these articles, L5/S1 LDH has been the most studied, and findings regarding the operative outcomes and time, complications, and recurrence rates remain controversial. Our study established that the short- and long-term operative outcomes, complications, and recurrence rates were similar in both approaches. However, the operative time was significantly longer in the IELD group than in the TELD group, which differs from the results of the previous studies.12,21) As laminectomy was also more frequently performed in the IELD group, the longer operative time may have been due to the laminectomy. Previous retrospective studies must have a bias in the approach selection, but no study mentions that. The factors that affect a surgeons' decision-making regarding the approach selection have not been previously analyzed. Our study also had a bias in the approach selection, similar to that in the previous studies. Therefore, we analyzed factors that may influence the achievement of similar operative outcomes and complication and recurrence rates.
To identify such factors, we focused on L4/5 intracanal LDH (the most common LDH type in which operators occasionally waver in approach selection) and compared the preoperative radiological findings between the IELD and TELD groups. Before comparing the outcomes, we compared the patients' background data between the two groups. The surgeons preferentially selected IELD for taller and heavier patients, but not for those with high BMI. This indicates that surgeons might select IELD for patients who have a good physique, but not simple obesity. As the ILS size is partly dependent on the patient's physical status, this bias may account for selecting patients with a large ILS for IELD.
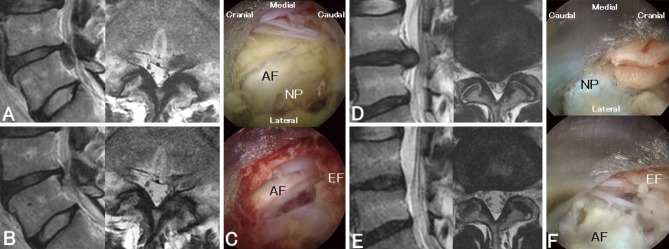
We found significant differences in some radiological findings between the IELD and TELD groups and considered the following possible reasons: (1) Differences in the LDH type (P = 0.03): TELD was preferentially selected for central LDH, whereas IELD was preferentially selected for axilla LDH (Fig. 2). To remove central LDH via IELD, it is necessary to retract the nerve root and dural sac. To remove axilla LDH via TELD, it is necessary to remove part of the lower pedicle and use curved forceps. To avoid these invasive, sophisticated techniques and risks, surgeons might select an alternative approach. We could not find a statistical difference in the extent of LDH migration (P = 0.06); however, IELD was selected for more migrated LDHs. This finding might be similar to that for LDH types because the axilla type migrates more caudally than the central type. Zhao et al. reported a similar advantage of IELD for highly migrated or axilla LDHs.21) (2) Differences in the L4 vertebral lamina configuration (P < 0.001): IELD was preferentially selected for the concave (+) configuration, whereas TELD was preferentially selected for the concave (−) configuration. If there is a concave (+) configuration, surgeons can easily access the ILS, reducing the area of laminectomy required than that with the concave (−) configuration.6,23) Hence, IELD was preferentially selected for the concave (+) configuration. (3) Differences in the ILS width (P < 0.001): The mean ILS width was 25.05 ± 3.31 mm and 20.64 ± 3.20 mm in the IELD and TELD groups, respectively. Similar to the L4 vertebral lamina configuration, this difference indicated that the surgeons preferentially selected IELD for patients with an accessible interlaminar window.28) (4) Differences in the vertebral foramen width (P < 0.02): The mean vertebral foramen width was 8.98 ± 2.44 mm and 10.24 ± 2.18 mm in the IELD and TELD groups, respectively. We could not find a statistical difference in the vertebral foramen height (P = 0.07); the height tended to be more in the TELD group than in the IELD group. This difference indicated that surgeons preferentially select TELD for patients with an accessible vertebral foramen. However, the vertebral foramen width was more important than the height. (5) Differences in the iliac crest position (P = 0.02): IELD was preferentially selected for those with a high iliac crest (63.2%); surgeons avoided TELD in patients with a high iliac crest due to inaccessibility.
Fig. 2.
Representative cases treated by left IELD (A, B, C) and right TELD (D, E, F). (A, B, D, E) Pre-(A, D) and postoperative (B, E) sagittal (left) and axial (right) T2-weighted MR images are shown. (C, F) Intraoperative photographs before (upper) and after (lower) removal of the herniated nucleus pulposus (NP) are shown. After removal of NP, the spaces are created at caudal site of annulus fibrosus (AF) by IELD and between AF and epidural fat tissue by TELD.
This study had several limitations. Primarily, it was not a prospective, multi-institutional, or completely matched comparative study. Furthermore, we lost more than a hundred patients to follow-up. However, we showed similar operative outcomes between IELD and TELD in both short- and long-term follow-ups. In addition, by analyzing the preoperative radiological findings, we were able to identify several factors that affect a surgeons' decision-making regarding approach selection.
Conclusions
This retrospective study with a 2-year follow-up showed that the long-term operative outcomes of IELD and TELD (using a 4.1-mm working channel) for L4/5 intracanal LDH treatment were the same. If the appropriate approach is selected, it is possible to achieve similar, good, operative outcomes irrespective of the selected approach.
Conflicts of Interest Disclosure
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplementary Material
Lee's classification of migrated disc herniations Zone 1, far-upward; Zone 2, near-upward; Zone 3, near-downward; Zone 4, fardownward; VB, vertebral body
References
- 1). Yamaya S, Tezuka F, Sugiura K, et al. : Risk factor for additional intravenous medication during transforaminal full-endoscopic lumbar discectomy under local anesthesia. Neurol Med Chir (Tokyo) 61: 236-242, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2). Lee DY, Lee SH: Learning curve for percutaneous endoscopic lumbar discectomy. Neurol Med Chir (Tokyo) 48: 383-388; discussion 8-9, 2008 [DOI] [PubMed] [Google Scholar]
- 3). Hirano Y, Mizuno J, Takeda M, Itoh Y, Matsuoka H, Watanabe K: Percutaneous endoscopic lumbar discectomy - early clinical experience. Neurol Med Chir (Tokyo) 52: 625-630, 2012 [DOI] [PubMed] [Google Scholar]
- 4). Yokosuka J, Oshima Y, Kaneko T, Takano Y, Inanami H, Koga H: Advantages and disadvantages of posterolateral approach for percutaneous endoscopic lumbar discectomy. J Spine Surg 2: 158-166, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5). Dezawa A, Mikami H, Sairyo K: Percutaneous endoscopic translaminar approach for herniated nucleus pulposus in the hidden zone of the lumbar spine. Asian J Endosc Surg 5: 200-203, 2012 [DOI] [PubMed] [Google Scholar]
- 6). Tonosu J, Oshima Y, Shiboi R, et al. : Consideration of proper operative route for interlaminar approach for percutaneous endoscopic lumbar discectomy. J Spine Surg 2: 281-288, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7). Kondo M, Oshima Y, Inoue H, Takano Y, Inanami H, Koga H: Significance and pitfalls of percutaneous endoscopic lumbar discectomy for large central lumbar disc herniation. J Spine Surg 4: 79-85, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8). Chen J, Jing X, Li C, Jiang Y, Cheng S, Ma J: Percutaneous endoscopic lumbar discectomy for L5S1 lumbar disc herniation using a transforaminal approach versus an interlaminar approach: a systematic review and meta-analysis. World Neurosurg 116: 412-420. e2, 2018 [DOI] [PubMed] [Google Scholar]
- 9). Cheng YP, Cheng XK, Wu H: A comparative study of percutaneous endoscopic interlaminar discectomy and transforaminal discectomy for L5-S1 calcified lumbar disc herniation. BMC Musculoskelet Disord 23: 244, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10). He DW, Xu YJ, Chen WC, et al. : Meta-analysis of the operative treatment of lumbar disc herniation via transforaminal percutaneous endoscopic discectomy versus interlaminar percutaneous endoscopic discectomy in randomized trials. Medicine (Baltimore) 100: e23193, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11). Hua W, Zhang Y, Wu X, et al. : Outcomes of discectomy by using full-endoscopic visualization technique via the interlaminar and transforaminal approaches in the treatment of L5-S1 disc herniation: an observational study. Medicine (Baltimore) 97: e13456, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12). Huang K, Chen G, Lu S, et al. : Early clinical outcomes of percutaneous endoscopic lumbar discectomy for L4-5 highly down-migrated disc herniation: interlaminar approach versus transforaminal approach. World Neurosurg 146: e413-e418, 2021 [DOI] [PubMed] [Google Scholar]
- 13). Huang Y, Yin J, Sun Z, et al. : Percutaneous endoscopic lumbar discectomy for LDH via a transforaminal approach versus an interlaminar approach: a meta-analysis. Orthopade 49: 338-349, 2020 [DOI] [PubMed] [Google Scholar]
- 14). Jitpakdee K, Liu Y, Kotheeranurak V, Kim JS: Transforaminal versus interlaminar endoscopic lumbar discectomy for lumbar disc herniation: a systematic review and meta-analysis. Global Spine J 13: 575-587, 2023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15). Mo X, Shen J, Jiang W, et al. : Percutaneous endoscopic lumbar diskectomy for axillar herniation at L5-S1 via the transforaminal approach versus the interlaminar approach: a prospective clinical trial. World Neurosurg 125: e508-e514, 2019 [DOI] [PubMed] [Google Scholar]
- 16). Pruttikul P, Chobchai W, Pluemvitayaporn T, Kunakornsawat S, Piyaskulkaew C, Kittithamvongs P: Comparison of post-operative wound pain between interlaminar and transforaminal endoscopic spine surgery: which is superior? Eur J Orthop Surg Traumatol 32: 909-914, 2022 [DOI] [PubMed] [Google Scholar]
- 17). Wang D, Xie W, Cao W, He S, Fan G, Zhang H: A cost-utility analysis of percutaneous endoscopic lumbar discectomy for L5-S1 lumbar disc herniation: transforaminal versus interlaminar. Spine (Phila Pa 1976) 44: 563-570, 2019 [DOI] [PubMed] [Google Scholar]
- 18). Yan Y, Zhu M, Cao X, et al. : Different approaches to percutaneous endoscopic lumbar discectomy for L5/S1 lumbar disc herniation: a retrospective study. Br J Neurosurg 9: 1-7, 2020 [DOI] [PubMed] [Google Scholar]
- 19). Yin J, Jiang Y, Nong L: Transforaminal approach versus interlaminar approach: a meta-analysis of operative complication of percutaneous endoscopic lumbar discectomy. Medicine (Baltimore) 99: e20709, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20). Zelenkov P, Nazarov VV, Kisaryev S, et al. : Learning curve and early results of interlaminar and transforaminal full-endoscopic resection of lumbar disc herniations. Cureus 12: e7157, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21). Zhao Q, Xiao L, Wu Z, Liu C, Zhang Y: Comparison of the efficacy of fully endoscopic spine surgery using transforaminal and interlaminar approaches in the treatment of prolapsed lumbar 4/5 disc herniation. J Orthop Surg Res 17: 391, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22). Lee S, Kim SK, Lee SH, et al. : Percutaneous endoscopic lumbar discectomy for migrated disc herniation: classification of disc migration and surgical approaches. Eur Spine J 16: 431-437, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23). Koga H, Inanami H: Minimal laminectomy using the interlaminar approach for percutaneous endoscopic lumbar discectomy. Mini-invasive Surg 1: 56-62, 2017 [Google Scholar]
- 24). Korovessis PG, Stamatakis MV, Baikousis AG: Reciprocal angulation of vertebral bodies in the sagittal plane in an asymptomatic Greek population. Spine (Phila Pa 1976) 23: 700-704; discussion 4-5, 1998 [DOI] [PubMed] [Google Scholar]
- 25). Choi KC, Park CK: Percutaneous endoscopic lumbar discectomy for L5-S1 disc herniation: consideration of the relation between the iliac crest and L5-S1 disc. Pain Phys 19: E301-E308, 2016 [PubMed] [Google Scholar]
- 26). EuroQol Group: EuroQol--a new facility for the measurement of health-related quality of life. Health Policy 16: 199-208, 1990 [DOI] [PubMed] [Google Scholar]
- 27). Fairbank JC, Pynsent PB: The Oswestry disability index. Spine (Phila Pa 1976) 25: 2940-2952; discussion 52, 2000 [DOI] [PubMed] [Google Scholar]
- 28). Sakçı Z, Önen MR, Fidan E, Yaşar Y, Uluğ H, Naderi S: Radiologic anatomy of the lumbar interlaminar window and surgical considerations for lumbar interlaminar endoscopic and microsurgical disc surgery. World Neurosurg 115: e22-e26, 2018 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Lee's classification of migrated disc herniations Zone 1, far-upward; Zone 2, near-upward; Zone 3, near-downward; Zone 4, fardownward; VB, vertebral body