Abstract
Since ancient times, physicians have been aware of correlations between the carotid artery and consciousness; however, carotid stenosis was only recently identified as the cause of atherothrombotic ischemic stroke. In 1658, Wepfer described the first suggestion of a link between symptoms of cerebral arterial insufficiency and carotid pathology. In 1951, Fisher reported details of the symptoms and pathological findings and emphasized that cervical atheromatous lesions induced cerebral infarction with various symptoms. The beginning of carotid artery surgery was ligation of the carotid artery for neck or head injury, but surgeons were aware that this operation induced cerebral symptoms due to lack of blood supply. Carotid endarterectomy (CEA) was first reported by Eastcott et al. in 1954, and in Japan, Kimoto performed a successful CEA in 1962. In 1979, percutaneous transluminal angioplasty (PTA) was performed for patients with fibromuscular dysplasia, and then, carotid artery stenting (CAS) was first performed in 1989 by Mathias. In Japan, Kuwana et al. were the first to perform carotid PTA, in 1981, whereas Yamashita et al. performed the first CAS in 1997. Yoshimura et al. proposed staged carotid stenting to prevent hyperperfusion syndrome. Some issues in carotid reconstruction are still debated today, which include conventional (standard) CEA versus the eversion technique, CEA versus CAS versus medical therapy, and medical economic problems. In the future, we must continue to develop more effective, safer, and less expensive therapeutic methods to prevent carotid stroke, carrying on the efforts of the ancient peoples who pioneered this research.
Keywords: history, carotid endarterectomy, carotid ligation, surgical treatment
Introduction
Carotid artery reconstruction is one of the most common operations in the neurosurgical field, and carotid endarterectomy (CEA) is the basic operation for carotid reconstruction. In 2015, over 80,000 CEAs were performed in the United States, and over 4,000 were performed in Japan.1,2) Since ancient times, physicians have been aware of correlations between carotid artery and consciousness, but carotid stenosis was only recently identified as the cause of atherothrombotic ischemic stroke.3) Vascular reconstruction for carotid lesions is also a relatively new operation, both worldwide and in Japan. An understanding of the relationship between carotid artery lesions and cerebral infarction and an appreciation of the history of carotid reconstruction are valuable for neurosurgeons. In this report, I review historical papers on carotid stroke and carotid reconstruction globally and in Japan.
Relationships between Carotid Artery Lesions and Cerebral Infarction
The term carotid is derived from the Ancient Greek verb “karos” (κάρος), which means “to stupefy”.4,5) Hippocrates first stated that the sudden-onset of paralysis and aphasia were signs of apoplexy.4,6) Rufus suggested that the word “karos” was used because superficial compression of this artery induced stupefaction.3,5,6) The metope of the Parthenon in Athens portrays a centaur gripping the neck and compressing the carotid artery of a Lapith during the legendary Centauromachy.3,4,7) Galen ascribed the loss of consciousness to compression not of the carotid arteries per se but of “sensitive nerves” located on the vessels and noticed that arterial occlusion was the cause of apoplexy.4,5)
Wepfer, a Swiss pathologist, described the first suggestion of a link between symptoms of cerebral arterial insufficiency and carotid pathology in 1658.4,5,8-10) He postulated that interruption of the blood supply to the brain was the cause of apoplexy.4,5,8-10) In 1664, the clinical importance of the cerebral arterial circle was confirmed by Willis, who reported the cases of two patients with right internal carotid artery (ICA) occlusion that remained asymptomatic due to the presence of collateral supply.4,5,9,11)
In 1754, the hypothesis of emboli arising from the artery was put forward by van Swieten.9,12) In 1765, Petit discovered an aneurysm of the carotid artery bifurcation in a patient and noted total occlusion of the common carotid artery (CCA) 7 years later on autopsy, but the patient had experienced no stroke.4,9,13) In 1856, Virchow published his seminal work, in which he coined the terms “thrombosis,” “ischemia,” and “embolus,” as well as reviving the expression “arteriosclerosis”.14) He also described embolus within the carotid artery as being associated with ipsilateral monocular blindness.4,5,14)
In 1881, Penzoldt published the case of a patient who exhibited sudden-onset blindness of the right eye with delayed contralateral hemiplegia.4,5,15) The autopsy revealed a thrombotically obstructed right CCA.4,5,15) Hultquist reported thromboembolism of the carotid system in approximately 3% of routine autopsies.16,17) In 1905, Chiari developed the thromboembolic hypothesis based on work on ulcerated plaques and surface thrombus.6,16-19) His findings were the first to show the atherosclerotic carotid bifurcation as a prominent source of stroke-inducing cerebral emboli.6,16,17,19) Moreover, in 1914, an examination of autopsy cases by Hunt identified that both occlusion and stenosis of the carotid artery could induce cerebral syndromes.4,5,20) They proposed examining the carotid vessels at autopsy as a cause of stroke,17,20) even though this advice has long been disregarded.17) In 1937, Moniz and colleagues showed cases with occlusion of the cervical portion of the ICA on angiography, along with the clinical details of those cases.4,17,21) In 1951, Jonson and Walker reported 107 cases of carotid thrombosis diagnosed angiographically and emphasized that carotid occlusion was far more common than generally recognized.4,22)
Moreover, in 1951, Fisher described eight cases with occlusive lesions of the carotid artery and reported detailed symptoms and pathological findings. He emphasized that cervical atheromatous lesions induced cerebral infarction with various transient or permanent symptoms.4,5,17,23,24) This landmark article by Fisher brought major attention to the carotid arteries as the pathological substrate for stroke, and the idea of surgical reconstruction of the carotid arteries came into being.4)
After the 1950s, several CEAs had been performed and elucidation of the etiologies of postoperative complications continued to advance. In 1963, Bruetman et al. reported six cases of postoperative intracerebral hemorrhage. Patients consistently showed clinical improvements after CEA; then, hemorrhages suddenly occurred.25) Bland et al. reported intracerebral hemorrhage soon after CEA in patients with postoperative hypertension but did not suggest any etiology for this hemorrhagic complication.26) Sundt et al. in 1981 and Bernstein et al. in 1984 reported hyperperfusion syndrome after CEA.27,28) Both reports mentioned that this phenomenon resembled breakthrough perfusion such as postoperative arteriovenous malformation in patients who had severe postoperative hypertension.27,28) Subsequent to these reports, neurologists and neurosurgeons investigated the mechanisms and frequency of hyperperfusion syndrome.29-31) A great deal of hard work was put into preventing hyperperfusion syndrome, which was a severe postoperative complication.29,32) Table 1 summarizes the historical evolution of ideas on the relationship between carotid artery lesions and cerebral infarction.
Table 1.
Relationships between CA lesion and cerebral infarction, and history of CA reconstruction worldwide
| Year | Authors | Relationships between CA lesion and cerebral infarction | History of carotid artery reconstruction worldwide |
|---|---|---|---|
| BC 460-370 | Hippocrates4,5) | Stated that sudden onset of paralysis and aphasia were signs of apoplexy | |
| 100 | Rufus3,5,6) | Suggested that the word “karos” was used because superficial compression of CAs induced stupefaction | |
| 131-201 | Galen4,5) | Noticed that arterial occlusion was the cause of apoplexy | |
| 1552 | Pare9,33) | Performed carotid ligation to control bleeding from an epee wound | |
| 1658 | Wepfer4,5,8-10) | Postulated that interruption of blood supply to the brain was the cause of apoplexy | |
| 1664 | Willis4,5,9,11) | Reported two patients with asymptomatic right ICA occlusion and with collateral supply | |
| 1754 | Swieten9,12) | Reported the hypothesis of emboli arising from the artery | |
| 1765 | Petit4,9,13) | Found asymptomatic complete occlusion of CA by thrombus | |
| 1775 | Warner9,35) | Ligated the CA when removing a massive lipoma | |
| 1793 | Hebenstreit4,5,7,9,36) | Used carotid ligation to control bleeding resulting from operative removal of a scirrhous tumor | |
| 1798 | Abernathy4,5,7,9) | Performed elective CCA ligation for a patient with traumatic injury of the CA in a goring by a cow | |
| 1803 | Fleming4,9,38) | Exposed and ligated the CA proximal to the rupture site in an injury caused by the patient | |
| 1805 | Cooper39,40) | First attempted ligation of a CA for a patient with cervical aneurysm | |
| 1809 | Travers4,9) | Successfully ligated the CA for a patient with carotid-cavernous fistula | |
| 1856 | Virchow4,5,14) | Described embolus within the CA as associated with ipsilateral monocular blindness | |
| 1881 | Penzoldt4,5,15) | Published the case of a patient who exhibited sudden-onset blindness in the right eye with delayed contralateral hemiplegia | |
| 1885 | Horsley4,33,41,42) | Successfully performed CA ligation for a patient with intracranial aneurysm | |
| 1905 | Chiari6,16-19) | Developed the thromboembolic hypothesis based on work on ulcerated plaques and surface thrombus | |
| 1914 | Hunt4,5,20) | Identified that both occlusion and stenosis of the CA could induce cerebral syndromes | |
| 1937 | Moniz4,17,21) | Indicated cases with occlusion of the cervical portion of the ICA on angiography, along with clinical details of cases | |
| 1951 | Fisher4,5,17,23,24) | Emphasized that cervical atheromatous lesions induced cerebral infarction with various temporary or permanent symptoms | |
| 1951 | Carrea4,5,47) | Partially resected the atheromatous portion of the CA, then re-established flow through an ECA-to-distal ICA anastomosis | |
| 1952 | Conley and Pack43) | Reported end-to-end anastomosis after resection of a neoplasm around the CA system | |
| 1953 | Conley4,44) | Reported using an interposition graft to reconstruct a resected cervical artery after tumor surgery using superficial femoral or saphenous vein | |
| 1953 | DeBakey3-5,48) | Performed CEA with primary closure; patient survived 19 years | |
| 1954 | Eastcott4,49,50) | First published report of CEA | |
| 1959 | DeBakey51) | Reported the original eversion technique | |
| 1963 | Bruetman25) | Reported six cases of postoperative intracerebral hemorrhage after CEA | |
| 1979 | Mathias66) | Performed PTA for patients with fibromuscular dysplasia | |
| 1980 | Mullan70) | Reported PTA for web-like ICA stenosis | |
| 1981 | Sundt27) | Reported a mechanism of hyperperfusion syndrome after CEA | |
| 1983 | Bockenheimer and Mathias66,72) | Performed successful PTA for proximal atherosclerotic ICA stenosis | |
| 1983 | Wiggli and Gratzl71) | Performed successful PTA for proximal atherosclerotic ICA stenosis | |
| 1984 | Bernstein28) | Reported the mechanism and histopathology of hyperperfusion syndrome after CEA | |
| 1987 | Theron77,78) | Developed the balloon-type distal protection system | |
| 1989 | Mathias66) | Placed a self-expanding stent in a carotid atherosclerotic lesion as rescue treatment | |
| 1994 | Marks75) | Performed stent placement for ICA dissection | |
| 1996 | Roubin76) | Reported CAS for a total of 210 procedures in 152 CAs | |
| 1996 | Kachel79) | Expressed the new concept of flow reversal in the ICA resulting from blockade of the ECA and CCA | |
| 2000 | Parodi81,82) | Developed a new device and protection system using Kachel’s idea | |
| 2001 | Yaday83) | Demonstrated the concept of the filter protection device | |
| 2004 | Leipzig84) | Developed a clamping device system using flow reversal | |
| 2006 | Alexandrescu89,90) | Reported good outcomes from transcarotid artery revascularization | |
| 2009 | Yoshimura106) | Developed staged angioplasty as a method for preventing postoperative hyperperfusion from CAS |
CA, carotid artery; ICA, internal carotid artery; CEA, carotid endarterectomy; CCA, common carotid artery; ECA, external carotid artery; PTA, percutaneous transluminal angioplasty; CAS, carotid artery stenting
History of Carotid Artery Reconstruction
1) Carotid artery ligation
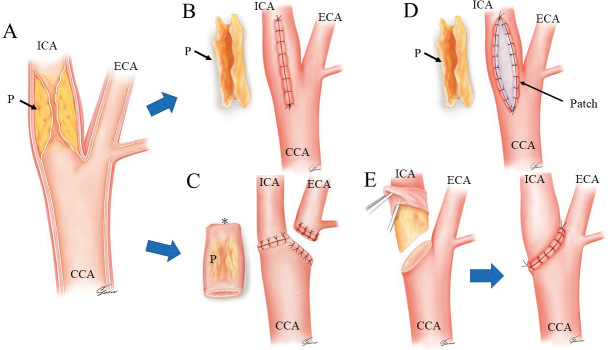
The beginning of carotid artery surgery was ligation of the carotid artery (Fig. 1). Pare performed the first such ligation in 1552,9,33) which was aimed at controlling bleeding from an epee wound to the patient, a soldier; however, aphasia and hemiplegia were seen subsequently.9,33) In those times, vessel ligations were performed using silk or catgut threads.34) Warner ligated the carotid artery when removing a massive lipoma in 1775.9,35) Hebenstreit injured a carotid artery during the operative removal of a scirrhous tumor in 1793 and controlled the resulting bleeding by carotid ligation.4,5,7,9,36) This patient survived for a long time following the operation.4,9,36) In 1798, Abernathy performed elective CCA ligation for a patient with traumatic injury of the carotid artery in a goring by a cow, but the patient died 30 h later.4,5,7,9) By the beginning of the 19th century, several reports had described successful ligation of the carotid artery.4,5,7,9,37) In 1803, Fleming exposed the carotid artery proximal to a rupture site and ligated the carotid artery, which had been injured by the patient himself; his assistant Coley reported this case in 1817.4,9,38)
Fig. 1.
The first surgeries on the carotid artery involved ligation of the carotid artery for patients with head or neck trauma to control massive bleeding.
In 1805, Cooper first attempted ligation of a carotid artery for a patient with a cervical aneurysm, but the patient died 21 days postoperatively.39) After that unsuccessful case, he successfully ligated the carotid artery to treat a cervical aneurysm in 1808.40)
In 1809, Travers diagnosed and successfully ligated the carotid artery for a patient with carotid-cavernous fistula.4,9) Horsley successfully performed carotid artery ligation for a patient with an intracranial aneurysm in 1885.4,33,41,42) Following that report, surgeons continued to perform carotid ligation for patients with intracranial aneurysm until the advent of direct surgery for this pathology.42) In 1868, Pilz identified 600 descriptions of carotid ligations for cervical aneurysm or hemorrhage, although the mortality rate after surgery was 43%.4,5)
2) Anastomosis of the carotid artery
In 1952, Conley and Pack reported end-to-end anastomosis after resection of a neoplasm around the carotid artery system.43) They concluded that such anastomosis was safe and useful in the resection of the carotid artery.43) The following year, Conley reported the interposition graft to reconstruct a resected cervical artery after tumor surgery using superficial femoral or saphenous vein.4,44)
3) Carotid endarterectomy
Des Santos performed thromboendarterectomy in a peripheral artery before CEA in 1946,45) whereas Wylie removed atherosclerotic plaque from the aortoiliac artery before CEA.46)
After Fisher's landmark articles,17,23,24) the mood regarding carotid artery reconstruction was positive. There is no dispute that the first successful carotid artery reconstruction for occlusive disease occurred in Buenos Aires in 1951.3-5,47) The neurosurgeon Carrea and his colleagues diagnosed left ICA stenosis angiographically, partially resected the atheromatous portion of the artery, and then re-established flow through an external carotid artery-to-distal ICA anastomosis.4,5) Nevertheless, the report of this surgery was not published until 4 years later.47) The first successful CEA was performed by DeBakey in 1953, using a primary closure.3-5) Although the patient survived 19 years without neurological events, the case was not reported until 1975.48) In that paper, DeBakey described that the artery was sutured using silk.48)
The first published report of CEA was made by Eastcott et al. in 1954.4,49) They resected an atheromatous region of the ICA and performed end-to-end reconstruction of the ICA and CCA under hypothermic general anesthesia.4,49,50) Since that report, several methods for resecting carotid atherosclerotic plaque and anastomosing carotid vessels have been described. DeBakey et al. reported the original eversion technique,51) whereas Etheredge and Raithel et al. developed further eversion techniques,52,53) although conventional CEA is still considered to be the standard operation.2,4,6) In terms of historical changes in the suture materials applied to CEA, silk was used first, with monofilament, nonabsorbable polypropylene entering commonly used subsequently.54) Additionally, polytetrafluoroethylene and hexafluoropropylene-VDF are currently in use, as is monofilament, absorbable suture material.55)
CEA has been reported for the prevention of fatal and disabling strokes, but the indications for CEA remain to be debated. DeBakey proposed an international co-operative study of CEA efficacy, leading to a joint study. The results of that randomized study, which included 2400 operations, were published in 1968 and 1969,56,57) with an overall surgical mortality rate of 4%.57) After those reports, the use of CEA exploded in North America.58,59) Further randomized studies performed in the 1990s statistically confirmed the effectiveness of CEA.60,61)
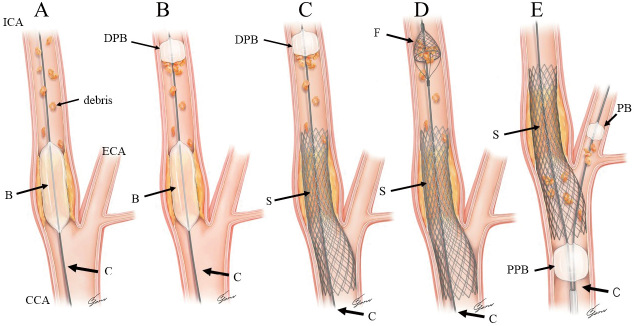
Table 1 summarizes the history of carotid artery reconstructions worldwide, and Fig. 2 depicts the historical transitions of surgical reconstructions for the carotid artery.
Fig. 2.
Historical transitions in surgical reconstruction of the carotid artery.
A: Illustration of carotid artery stenosis due to atherosclerotic plaque.
B: DeBakey et al. performed carotid endarterectomy with a primary closure.
C: Eastcott et al. resected an atheromatous lesion in the internal carotid artery (ICA) and performed end-to-end reconstruction of the ICA and common carotid artery.
D: Patch angioplasty as initially performed using the saphenous vein and then later using an artificial vascular membrane.
E: The original eversion technique as first described by DeBakey et al., which involved cutting the carotid bifurcation and resecting the plaque.
CCA: common carotid artery; ICA: internal carotid artery; ECA: external carotid artery; P: plaque. *Resected an atheromatous region of ICA.
4) Carotid artery reconstruction by endovascular surgery
In 1964, Dotter and Judkins first reported percutaneous transluminal angioplasty (PTA) for patients with stenosis of the superficial femoral artery.62) Gruntzig and Hopt introduced the balloon dilatation catheter as a PTA tool in 1974.63) After these two reports, angioplasty started to be performed for peripheral vessels or other brachiocephalic branches in addition to the coronary arteries.64-66) In cases of ICA stenosis among patients with fibromuscular dysplasia, PTA was performed by Mathias in 1979,66) Hasso et al. in 1981,67) and Garrido and Montaya in 1981.68) In 1980, Kerber et al. performed PTA for proximal stenosis of the CCA during distal CEA,66,69) and Mullan et al. reported PTA for web-like ICA stenosis that same year.70) In 1983, Bockenheimer and Mathias and another group of Wiggli and Gratzl performed the first successful PTAs for proximal atherosclerotic ICA stenosis.66,71,72) After these reports, PTA for CCA or ICA stenosis increased during the 1980s.72-74)
In 1989, Mathias placed a self-expanding stent (Wallstent for the iliac artery; Schneider, Minneapolis, MN, USA) in a carotid atherosclerotic lesion. In that case, PTA was performed first, but dissection occurred at the lesion so the stent was placed as a rescue treatment.66) In 1994, stent placement for the ICA was performed by Marks et al. in two patients with ICA dissection.75) They used Palmaz stents (Johnson & Johnson, Warren, NJ, USA), and the lesions were successfully resolved.75) In 1996, Roubin et al. reported carotid artery stenting (CAS) for a total of 210 procedures in 152 carotid arteries.76) After these initial reports, the application of CAS increased with the development of new stent devices, such as the Palomaz stent, Wallstent, Precise stent (Cordis, Santa Clara, CA, USA), and closed cell stent. Finer closed stents are currently being developed.
In the endovascular treatment of carotid artery lesions, protection against distal embolism is a crucial issue. In 1981, Mathias developed a mesh-type protection device, but commercial manufacture was never achieved.66) In 1987, Theron et al. developed a balloon-type distal protection system that later evolved into the triaxial system.77,78) This idea was later commercialized as the “PercuSurge” device (Bait, Montmorency, France).79,80) In 1996, Kachel expressed the new concept of flow reversal in the ICA resulting from the blockade of the external carotid artery and CCA.79) In 2000, Parodi et al. developed a new device and protection system using the ideas expressed by Kachel.81,82) Yaday described the concept of filter protection devices and Jaeger et al. reported results for filter-protected CAS in 2001.83) In 2004, the Leipzig group developed a clamping device (INVATEC s.r.1., Roncadelle, Italy) system by applying the principles of flow reversal.84)
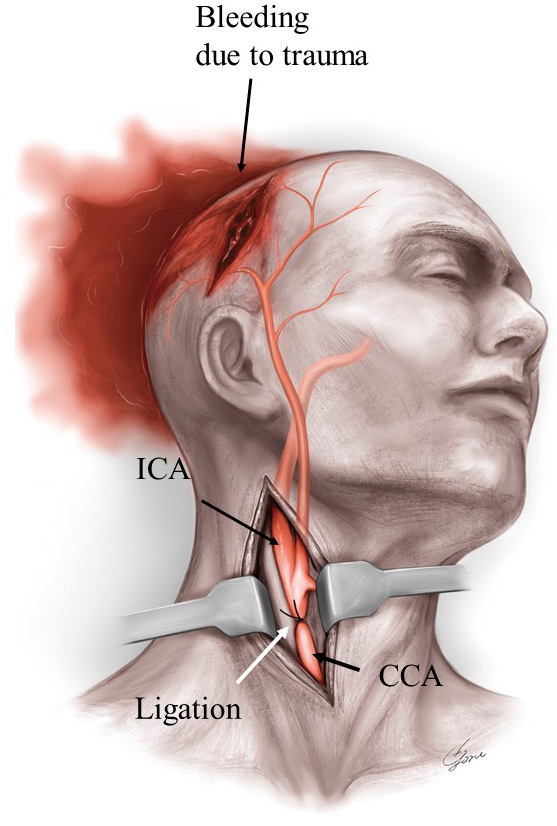
As another problem associated with embolic complications, the access route itself affects the risk of embolism.85) Passing the aortic arch is dangerous in elderly patients undergoing transfemoral procedures during CAS,85) so transbrachial artery or transcarotid (cervical) artery access was chosen in patients with a dangerous aortic arch.86-88) Recently, transcarotid artery revascularization using flow reversal was proposed and showed good outcomes in elderly patients with carotid artery stenosis.89,90) Fig. 3 demonstrates the historical transitions in endovascular reconstructions of the carotid artery.
Fig. 3.
Historical transitions in the endovascular reconstruction of the carotid artery.
A: Percutaneous transluminal angioplasty for patients with atherosclerotic carotid artery stenosis, initially without distal protection against embolism.
B: Percutaneous transluminal angioplasty for patients with atherosclerotic carotid artery stenosis with a distal protection balloon to prevent embolism.
C: Carotid artery stenting for patients with atherosclerotic carotid artery stenosis with distal protection balloon for the embolus.
D: Carotid artery stent for patients with atherosclerotic carotid artery stenosis with distal filter protection device to protect against embolism.
E: Carotid artery stenting for patients with atherosclerotic carotid artery stenosis using flow reversal methods with proximal common carotid and external carotid artery balloons.
CCA: common carotid artery; ICA: internal carotid artery; ECA: external carotid artery; B: balloon; C: catheter; S: stent; DPB: distal protective balloon; F: distal filter protection device; PPB: proximal protection balloon; PB: protection balloon at the external carotid artery
History of Carotid Surgery in Japan
The first successful performance of CEA in Japan appears to have been in 1962, by Professor Kimoto and colleagues in the Department of Surgery at Tokyo University.91) They performed CEA for a patient with symptomatic left ICA stenosis using a vein patch. During ICA clamping, they used an external shunt.91) The next CEA in Japan was by Ogata et al. in 1964, for a patient with left ICA stenosis.92) They resected the affected region and performed reconstruction using a Tetoron graft.92) Kageyama et al. performed CEA for a patient with left ICA occlusion in 1965,93) then, in 1969, Takaku et al. reported four cases of CEA with resection of sympathetic nerves around the carotid artery. They used hypothermic anesthesia during CEA and warfarin after CEA.94) Following these operations, energetic Japanese neurosurgeons performed CEA in various institutes: Ono at Nagasaki University,95) Ueda at Tokushima University,96) and Professor Endo at Toyama University.97) However, the number of CEAs was quite small compared to the situation in North America. Professor Mori from Nagasaki University examined the number of CEAs performed in Japan using a questionnaire survey and estimated the total number of CEA performed in 1987 as approximately 500.98) This represented an annual rate of CEA for the Japanese population less than 1% of that of the United States.98) The author undertook a questionnaire survey of the number of CEAs performed in Japan in 1993, identifying 531 CEAs in 260 institutes.99) Professor Endo et al. found that 395 institutes performed 1336 CEAs in 2000 and 1427 CEAs in 2001.100) However, in those days, the number of CEAs performed by a single institute was very small.98-100) Since the beginning of 2000, the use of CEA has gradually increased, but with the widespread use of carotid stenting at the same time, the number of CEAs performed increased only slightly and has remained around 4,000 for the last 4-5 years.2)
Endovascular reconstruction of the carotid artery began slightly later in Japan than in Europe. In 1981, Kuwana et al. performed PTA for a patient with extracranial ICA stenosis, with the case reported in Japanese in 1985.101) At the beginning of 1990, PTA for extracranial ICA stenosis was established in Japan, and several reports of PTA for extracranial ICA stenosis have been published, with balloon protection used in a few cases during PTA.102,103)
After reports of CAS by Marks et al. and other endovascular surgeons,75,76) Yamashita et al. reported CAS as a rescue therapy for a patient with iatrogenic ICA dissection in 1997.104) After that report, CAS for extracranial ICA stenosis started to be performed more frequently in Japan from the late 1990s and the beginning of the 2000s.105) Nowadays, almost 10,000 patients undergo CAS in Japan each year.2)
As mentioned above, hyperperfusion after carotid artery reconstruction is a crucial complication. Thus, endovascular neurosurgeons should prevent this complication. In 2009, Yoshimura et al. developed staged angioplasty as a method for preventing postoperative hyperperfusion from CAS.106) The effectiveness of this method was confirmed in subsequent studies.107,108)
Problems and Future Issues in Carotid Reconstruction
Discussions of which methods are superior for carotid revascularization are still ongoing, including 1) conventional (standard) CEA versus eversion technique;109,110) 2) primary closure versus patch angioplasty,2,111-113) 3) general anesthesia versus local anesthesia,114,115) and 4) non-shunting versus selective shunting versus routine shunting.2,116) We have described and discussed these issues previously.2,116-118) Additionally, the superiority of treatments for carotid artery lesions must be discussed in terms of CEA versus CAS versus medical therapy.119-121) Table 2 summarizes randomized studies on the treatment of carotid artery lesions, including medical treatments.56,57,60,61,122-130) Long-term follow-up results of randomized controlled trials as secondary analyses have now been published.131-133) New information on the treatment of carotid artery lesions becomes available on an almost daily basis.
Table 2.
Randomized studies of the treatment of carotid artery lesions, including medical treatments
| Year | Study | Results |
|---|---|---|
| 1968 | Joint study of extracranial arterial occlusion56,57) | Although surgical mortality was 4%, outcomes of CEA in TIA patients with more than 50% stenosis were better than those of medical therapy |
| 1991 | North American Symptomatic Carotid Endarterectomy Trial Collaborators (NASCET)60) | In symptomatic patients with more than 70% stenosis, CEA showed absolute benefit compared to medical treatment |
| 1995 | Asymptomatic Carotid Atherosclerosis Study: endarterectomy for asymptomatic carotid artery stenosis (ACAS)61) | In asymptomatic patients with more than 60% stenosis, CEA showed absolute benefit compared to medical treatment |
| 1998 | MRC European Carotid Surgery Trial (ECST)122) | In symptomatic patients with more than 70% stenosis, CEA showed absolute benefit compared to medical treatment |
| 2001 | Endovascular versus surgical treatment in patients with carotid stenosis in the Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS)123) | Endovascular treatment showed similar major risks and effectiveness in prevention of stroke during 3 years compared with carotid surgery |
| 2004 | Stenting and Angioplasty with Protection in Patients at High Risk for Endarterectomy trial (SAPPHIRE)124) | Among patients with severe carotid artery stenosis (more than 50%) and coexisting conditions, CAS was not inferior to CEA |
| 2004 | Asymptomatic Carotid Surgery Trial (ACST)125) | In asymptomatic patients with more than 60% stenosis, CEA showed absolute benefit compared to medical treatment |
| 2006 | Endarterectomy Versus Angioplasty in Patients With Symptomatic Severe Carotid Stenosis (EVA-3S)126) | In symptomatic patients with more than 60% stenosis, rates of death and stroke at 1 and 6 months were lower with CEA than with CAS |
| 2006 | Stent-Supported Percutaneous Angioplasty of the Carotid Artery versus Endarterectomy trial (SPACE)127) | This study failed to prove non-interiority of CAS compared with CEA in symptomatic patients with more than 50% stenosis |
| 2010 | Carotid artery stenting compared with endarterectomy in patients with symptomatic carotid stenosis (ICSS)128) | In symptomatic patients with more than 50% stenosis, CEA was safer than CAS |
| 2010 | Carotid Revascularization Endarterectomy versus Stenting Trial (CREST)129) | In symptomatic or asymptomatic patients with more than 50% stenosis, outcomes did not differ significantly between CAS and CEA |
| 2016 | Asymptomatic Carotid Trial (ACT) I130) | In asymptomatic patients with more than 70% stenosis who were not at high risk of surgical complications, CAS was noninferior to CEA |
| 2016 | Long-term results of stenting versus endarterectomy for carotid-artery stenosis (CREST)131) | In symptomatic or asymptomatic patients with more than 50% stenosis, outcomes did not differ significantly between CAS and CEA over 10 years of follow-up |
| 2021 | Second Asymptomatic Carotid Surgery Trial (ACST-2)132) | In asymptomatic patients with more than 60% stenosis, protective effects of CAS and CEA were similar for at least the first few years |
| 2022 | Carotid endarterectomy or stenting or best medical treatment alone for moderate-to-severe asymptomatic carotid artery stenosis (SPACE-2)133) | In symptomatic patients with more than 50% stenosis, CEA plus BMT or CAS plus BMT were not found to be superior to BMT alone |
TIA, transient ischemic attack; CEA, carotid endarterectomy; CAS, carotid artery stenting; BMT, best medical treatment
Complication and recurrence rates have not reached zero, irrespective of the maneuvers or pharmacotherapies. Although randomized studies and meta-analyses have been conducted as described above, conclusive results have not been established. Furthermore, as techniques for carotid reconstruction by endovascular surgery become more complicated and as new medicines are developed, medical costs will continue to increase.1,134) Indications for carotid reconstruction in super-aging patients remain controversial worldwide and in Japan.135)
In the future, we must develop more effective, safer, and less expensive therapeutic methods for preventing carotid stroke, which will repay the efforts of our great antecedents.
Conclusion
In this report, I have reviewed both the evolution of the concept of how carotid artery lesions affect cerebral infarction and the history of carotid artery reconstructions worldwide and in Japan.
Conflicts of Interest Disclosure
The author has no conflicts of interest to declare regarding this study or its findings.
References
- 1). Cole TS, Mezher AW, Catapano JS, et al. : Nationwide trends in carotid endarterectomy and carotid artery stenting in the post-CREST era. Stroke 51: 579-587, 2020 [DOI] [PubMed] [Google Scholar]
- 2). Uno M, Takai H, Yagi K, Matsubara S: Surgical technique for carotid endarterectomy: current methods and problems. Neurol Med Chir (Tokyo) 60: 419-428, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3). Munster AB, Thapar A, Davies AH: History of carotid stroke. Stroke 47: e66-e69, 2016 [DOI] [PubMed] [Google Scholar]
- 4). Thompson JE: The evolution of surgery for the treatment and prevention of stroke. The Willis Lecture. Stroke 27: 1427-1434, 1996 [DOI] [PubMed] [Google Scholar]
- 5). Min WD, Loftus CM: History of carotid surgery. Neurosurg Clin N Am 12: 167-172, 2001 [PubMed] [Google Scholar]
- 6). Thompson JE: The development of carotid artery surgery. Arch Surg 107: 643-648, 1973 [DOI] [PubMed] [Google Scholar]
- 7). Thompson JE: Carotid surgery: the past is prologue. The John Homans lecture. J Vasc Surg 25: 131-140, 1997 [DOI] [PubMed] [Google Scholar]
- 8). Wepfer JJ: Obsevartiones anatomicae ex cadaveribus eorum, quossustudit apoplexia cum exercitatione de eius loco agffecto. Schaffhausen, Waldkirch Alexandri Riedingii. 1658: 670 [Google Scholar]
- 9). Pearce JM: Historical note on carotid disease and ligation. Eur Neurol 72: 26-29, 2014 [DOI] [PubMed] [Google Scholar]
- 10). Gurdjian ES, Gurdjian ES: History of occlusive cerebrovascular disease I. from Wepfer to Moniz. Arch Neurol 36: 340-343, 1979 [DOI] [PubMed] [Google Scholar]
- 11). Willis T: Cerebri Anatome: cui Accessit Nervorum Descriptio et Usus, in Flesher, Martyn and Allestry. London, 1664 [Google Scholar]
- 12). van Swieten G: Of the Apoplexy, Palsy and Epilepsy. Commentaries on the Aphorisms of Dr Herman Boerhaave, ed 6. John & Paul Knapton, London, 1754 [Google Scholar]
- 13). Cutter I: Ligation of the common carotid artery. Amos Twitchell Surg Gynecol Obstet (Int Obstet Surg) 48: 1-3, 1920 [Google Scholar]
- 14). Virchow R: Thrombose und Embolie. Gefassen Zundung und Septische Infektion in Gesammelte Abhandlungen zur Wissen Schaftlichen Medicin Frankfurt: AM Meidinger. 1856: 219-732 [Google Scholar]
- 15). Penzoldt F: Uber thrombose (autochtone oder embolische) der carotis. Dtsch Arch Klin Med 28: 80-93, 1881 [Google Scholar]
- 16). Hultquist GT: Uber Thrombose und Embolie der Arteria Carotis und Hierbei Vorkommende. Gehirnstorungen, Jene Gustav Fisher, 1942 [Google Scholar]
- 17). Fishier M: Occlusion of the internal carotid artery. AMA Arch Neurol Psychiatry 65: 346-377, 1951 [DOI] [PubMed] [Google Scholar]
- 18). Tallarita T, Gerbino M, Gurrieri C, Lanzino G: History of carotid surgery: from ancient Greeks to the modern era. Perspect Vasc Surg Endovasc Ther 25: 57-64, 2013 [DOI] [PubMed] [Google Scholar]
- 19). Chiari H: Ueber das Verhalten des teilungswinkels der carotis communis bei der endarteritis chronica deformans. Verh Dtsch Pathol G.E.S 9: 326-330, 1905 [Google Scholar]
- 20). Hunt JR: The role of the carotid arteries, in the causation of vascular lesions of the brain, with remarks on certain special features of the symptomatology. Am J M Ac 147: 704, 1914 [DOI] [PubMed] [Google Scholar]
- 21). Moniz E, Lima A, de Lacerda R: Hemiplegies par thorombose de la carotide interne. Presse Med 45: 977-980, 1937 [Google Scholar]
- 22). Johnson HC, Walker AE: The angiographic diagnosis of spontaneous thrombosis of the internal and common carotid arteries. J Neurosurg 8: 631-659, 1951 [DOI] [PubMed] [Google Scholar]
- 23). Fisher M, Adams RD: Observations on brain embolism with special reference to the mechanism of hemorrhagic infarction. J Neuropathol Exp Neurol 10: 92-94, 1951 [PubMed] [Google Scholar]
- 24). Fisher M: Occlusion of the carotid arteries: further experiences. A.M.A. Arch Neurol Psychiatry 72: 187-204, 1954 [DOI] [PubMed] [Google Scholar]
- 25). Bruetman ME, Fields WS, Crawford ES, Debakey ME: Cerebral hemorrhage in carotid artery surgery. Arch Neurol 9: 458-467, 1963 [DOI] [PubMed] [Google Scholar]
- 26). Bland JE, Chapman RD, Wylie EJ: Neurological complications of carotid artery surgery. Ann Surg 171: 459-464, 1970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27). Sundt TM Jr., Sharbrough FW, Piepgras DG, Kearns TP, Messick JM Jr., O'Fallon WM: Correlation of cerebral blood flow and electroencephalographic changes during carotid endarterectomy: with results of surgery and hemodynamics of cerebral ischemia. Mayo Clin Proc 56: 533-543, 1981 [PubMed] [Google Scholar]
- 28). Bernstein M, Fleming JF, Deck JH: Cerebral hyperperfusion after carotid endarterectomy: a cause of cerebral hemorrhage. Neurosurgery 15: 50-56, 1984 [DOI] [PubMed] [Google Scholar]
- 29). Piepgras DG, Morgan MK, Sundt TM Jr., Yanagihara T, Mussman LM: Intracerebral hemorrhage after carotid endarterectomy. J Neurosurg 68: 532-536, 1988 [DOI] [PubMed] [Google Scholar]
- 30). Hosoda K, Kawaguchi T, Ishii K, et al. : Prediction of hyperperfusion after carotid endarterectomy by brain SPECT analysis with semiquantitative statistical mapping method. Stroke 34: 1187-1193, 2003 [DOI] [PubMed] [Google Scholar]
- 31). Ogasawara K, Sakai N, Kuroiwa T, et al. : Intracranial hemorrhage associated with cerebral hyperperfusion syndrome following carotid endarterectomy and carotid artery stenting: retrospective review of 4494 patients. J Neurosurg 107: 1130-1136, 2007 [DOI] [PubMed] [Google Scholar]
- 32). Kawamata T, Okada Y, Kawashima A, et al. : Postcarotid endarterectomy cerebral hyperperfusion can be prevented by minimizing intraoperative cerebral ischemia and strict postoperative blood pressure control under continuous sedation. Neurosurgery 64: 447-453; discussion 453, 2009 [DOI] [PubMed] [Google Scholar]
- 33). Robicsek F: The medical history of extracranial cerebrovascular disease, in Robicsek F (ed): Extracranial Cerebrovascular Disease. New York, Macmillan, 1986, pp 5-18 [Google Scholar]
- 34). Mele GJ: The early history of the ligature. S Afr Med J 1: 290-292, 1934 [Google Scholar]
- 35). Warner J: Cases in Surgery; With Introductions, Operations and Remarks. ed 4. Johnson, London, 1784: 41-42 [Google Scholar]
- 36). Hebenstreit EBG: Zusätze zu Benjamin Bells Abhandlung von Den Geschwüren and Deren Behandlung. Weidmann, Leipzig, 1793 [Google Scholar]
- 37). Abernethy J: Observations on Injuries of the Head and on Miscellaneous Subjects. Dobson, Philadelphia, 1811 [Google Scholar]
- 38). Coley RW, Fleming D: Case of rupture of the carotid artery, and wounds of several of its branches, successfully treated by tying the common trunk of the carotid itself. Med Chir J Rev 3: 1-4, 1817 [PMC free article] [PubMed] [Google Scholar]
- 39). Cooper A: A case of aneurism of the carotid artery. Med Chir Trans 1: 1-12, 1809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40). Cooper A: Second case of carotid aneurism. Med Chir. Translator 1: 224-235, 1809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41). Travers B: A case of aneurysm of anastomosis in the orbit by ligation of the common carotid artery. Med Clin Transact 2: 1-16, 1811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42). Dandy WE: Results following bands and ligatures on the human internal carotid artery. Ann Surg 123: 384-396, 1946 [PubMed] [Google Scholar]
- 43). Conley JJ, Pack GT: Surgical procedure for lessening the hazard of carotid bulb excision. Surgery 31: 845-858, 1952 [PubMed] [Google Scholar]
- 44). Conley JJ: Free autogenous vein graft to the internal and common carotid arteries in the treatment of tumors of the neck. Ann Surg 137: 205-214, 1953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45). Dos Santos JC: Leriche memorial lecture. From embolectomy to endarterectomy or the fall of a myth. J Cardiovasc Surg (Torino) 17: 113-128, 1976 [PubMed] [Google Scholar]
- 46). Wylie EJ, Kerr E, Davies O: Experimental and clinical experiences with the use of fascia lata applied as a graft about major arteries after thrombo-endarteriectomy and aneurysmorrhaphy. Surg Gynecol Obstet 93: 257-272, 1951 [PubMed] [Google Scholar]
- 47). Carrea R, Molins M, Murphy G: Surgery of spontaneous thrombosis of the internal carotid in the neck; carotido-carotid anastomosis; case report and analysis of the literature on surgical cases. Med (B Aires) 15: 20-29, 1955 [PubMed] [Google Scholar]
- 48). DeBakey ME: Successful carotid endarterectomy for cerebrovascular insufficiency. Nineteen-year follow-up. JAMA 233: 1083-1085, 1975 [PubMed] [Google Scholar]
- 49). Eastcott HH, Pickering GW, Rob CG: Reconstruction of internal carotid artery in a patient with intermittent attacks of hemiplegia. Lancet 267: 994-996, 1954 [DOI] [PubMed] [Google Scholar]
- 50). Friedman SG: The first carotid endarterectomy. J Vasc Surg 60: 1703-8.e1, 2014 [DOI] [PubMed] [Google Scholar]
- 51). De Bakey ME, Crawford ES, Cooley DA, Morris GC Jr.: Surgical considerations of occlusive disease of innominate, carotid, subclavian, and vertebral arteries. Ann Surg 149: 690-710, 1959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52). Etheredge SN: A simple technic for carotid endarterectomy. Am J Surg 120: 275-278, 1970 [DOI] [PubMed] [Google Scholar]
- 53). Raithel D: Carotid eversion endarterectomy: a better technique than the standard operation? Cardiovasc Surg 5: 471-472, 1997 [DOI] [PubMed] [Google Scholar]
- 54). Loftus CM: Technical aspects of carotid endarterectomy with Hemashield patch graft. Neurol Med Chir (Tokyo) 37: 805-818, 1997 [DOI] [PubMed] [Google Scholar]
- 55). Aleksic M, Uedelhoven J, Matoussevitch V, et al. : Results of an observational study in carotid surgery using absorbable suture material. World J Surg 33: 145-149, 2009 [DOI] [PubMed] [Google Scholar]
- 56). Fields WS, North RR, Hass WK, et al. : Joint study of extracranial arterial occlusion as a cause of stroke. I. Organization of study and survey of patient population. JAMA 203: 955-960, 1968 [PubMed] [Google Scholar]
- 57). Blaisdell WF, Clauss RH, Galbraith JG, Imparato AM, Wylie EJ: Joint study of extracranial arterial occlusion. IV. A review of surgical considerations. JAMA 209: 1889-1895, 1969 [PubMed] [Google Scholar]
- 58). Dyken ML, Pokras R: The performance of endarterectomy for disease of the extracranial arteries of the head. Stroke 15: 948-950, 1984 [DOI] [PubMed] [Google Scholar]
- 59). Pokras R, Dyken ML: Dramatic changes in the performance of endarterectomy for diseases of the extracranial arteries of the head. Stroke 19: 1289-1290, 1988 [DOI] [PubMed] [Google Scholar]
- 60). Barnett HJM, Taylor DW, Eliasziw M, et al. : Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med 325: 445-453, 1991 [DOI] [PubMed] [Google Scholar]
- 61). Executive Committee for the Asymptomatic Carotid Atherosclerosis: Endarterectomy for asymptomatic carotid artery stenosis. Executive committee for the asymptomatic carotid atherosclerosis study. JAMA 273: 1421-1428, 1995 [PubMed] [Google Scholar]
- 62). Dotter CT, Judkins MP: Transluminal treatment of arteriosclerotic obstruction. Description of a new technic and a preliminary report of its application. Circulation 30: 654-670, 1964 [DOI] [PubMed] [Google Scholar]
- 63). Grüntzig A, Hopff H: Percutaneous recanalization after chronic arterial occlusion with a new dilator-catheter (modification of the Dotter technique) (author's transl). Dtsch Med Wochenschr 99: 2502-2510, 1974 [DOI] [PubMed] [Google Scholar]
- 64). Mathias K, Heiss HW, Gospos C: Subclavian steal syndrome-operation or dilation? Langenbecks Arch Chir 356: 279-283, 1982 [DOI] [PubMed] [Google Scholar]
- 65). Motarjeme A, Keifer JW, Zuska AJ: Percutaneous transluminal angioplasty of the brachiocephalic arteries. A.J.R. Am J Roentgenol 138: 457-462, 1982 [DOI] [PubMed] [Google Scholar]
- 66). Roffi M, Mathias K: History of carotid artery stenting. J Cardiovasc Surg (Torino) 54: 1-10, 2013 [PubMed] [Google Scholar]
- 67). Hasso AN, Bird CR, Zinke DE, Thompson JR: Fibromuscular dysplasia of the internal carotid artery: percutaneous transluminal angioplasty. A.J.R. Am J Roentgenol 136: 955-960, 1981 [DOI] [PubMed] [Google Scholar]
- 68). Garrido E, Montoya J: Transluminal dilatation of internal carotid artery in fibromuscular dysplasia: a preliminary report. Surg Neurol 16: 469-471, 1981 [DOI] [PubMed] [Google Scholar]
- 69). Kerber CW, Cromwell LD, Loehden OL: Catheter dilatation of proximal carotid stenosis during distal bifurcation endarterectomy. A.J.N.R. Am J Neuroradiol 1: 348-349, 1980 [PMC free article] [PubMed] [Google Scholar]
- 70). Mullan S, Duda EE, Patronas NJ: Some examples of balloon technology in neurosurgery. J Neurosurg 52: 321-329, 1980 [DOI] [PubMed] [Google Scholar]
- 71). Wiggli U, Gratzl O: Transluminal angioplasty of stenotic carotid arteries: case reports and protocol. A.J.N.R. Am J Neuroradiol 4: 793-795, 1983 [PMC free article] [PubMed] [Google Scholar]
- 72). Bockenheimer SA, Mathias K: Percutaneous transluminal angioplasty in arteriosclerotic internal carotid artery stenosis. A.J.N.R. Am J Neuroradiol 4: 791-792, 1983 [PMC free article] [PubMed] [Google Scholar]
- 73). Tsai FY, Matovich V, Hieshima G, et al. : Percutaneous transluminal angioplasty of the carotid artery. A.J.N.R. Am J Neuroradiol 7: 349-358, 1986 [PMC free article] [PubMed] [Google Scholar]
- 74). Freitag G, Freitag J, Koch RD, Wagemann W: Percutaneous angioplasty of carotid artery stenoses. Neuroradiology 28: 126-127, 1986 [DOI] [PubMed] [Google Scholar]
- 75). Marks MP, Dake MD, Steinberg GK, Norbash AM, Lane B: Stent placement for arterial and venous cerebrovascular disease: preliminary experience. Radiology 191: 441-446, 1994 [DOI] [PubMed] [Google Scholar]
- 76). Roubin GS, Yadav S, Iyer SS, Vitek J: Carotid stent-supported angioplasty: a neurovascular intervention to prevent stroke. Am J Cardiol 78: 8-12, 1996 [DOI] [PubMed] [Google Scholar]
- 77). Théron J, Raymond J, Casasco A, Courtheoux F: Percutaneous angioplasty of atherosclerotic and postsurgical stenosis of carotid arteries. A.J.N.R. Am J Neuroradiol 8: 495-500, 1987 [PMC free article] [PubMed] [Google Scholar]
- 78). Theron J, Courtheoux P, Alachkar F, Bouvard G, Maiza D: New triple coaxial catheter system for carotid angioplasty with cerebral protection. A.J.N.R. Am J Neuroradiol 11: 869-874; discussion 875, 1990 [PMC free article] [PubMed] [Google Scholar]
- 79). Theron JG, Payelle GG, Coskun O, Huet HF, Guimaraens L: Carotid artery stenosis: treatment with protected balloon angioplasty and stent placement. Radiology 201: 627-636, 1996 [DOI] [PubMed] [Google Scholar]
- 80). Henry M, Amor M, Henry I, et al. : Carotid stenting with cerebral protection: first clinical experience using the PercuSurge GuardWire system. J Endovasc Surg 6: 321-331, 1999 [DOI] [PubMed] [Google Scholar]
- 81). Parodi JC, La Mura R, Ferreira LM, et al. : Initial evaluation of carotid angioplasty and stenting with three different cerebral protection devices. J Vasc Surg 32: 1127-1136, 2000 [DOI] [PubMed] [Google Scholar]
- 82). Parodi J, Bates MC, Ohki T, Schönholz C: The history of proximal carotid protection and flow reversal to prevent stent angioplasty embolization. Semin Vasc Surg 31: 9-14, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83). Jaeger H, Mathias K, Drescher R, et al. : Clinical results of cerebral protection with a filter device during stent implantation of the carotid artery. Cardiovasc Interv Radiol 24: 249-256, 2001 [DOI] [PubMed] [Google Scholar]
- 84). Diederich KW, Scheinert D, Schmidt A, et al. : First clinical experiences with an endovascular clamping system for neuroprotection during carotid stenting. Eur J Vasc Endovasc Surg 28: 629-633, 2004 [DOI] [PubMed] [Google Scholar]
- 85). Jones DW, Brott TG, Schermerhorn ML: Trials and frontiers in carotid endarterectomy and stenting. Stroke 49: 1776-1783, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86). Alexandrescu V, Ngongang C, Proumen J, et al. : Filter-protected carotid stenting via a minimal cervical access with transitory aspirated reversed flow during initial passage of the target lesion. J Endovasc Ther 13: 196-204, 2006 [DOI] [PubMed] [Google Scholar]
- 87). Sfyroeras GS, Moulakakis KG, Markatis F, et al. : Results of carotid artery stenting with transcervical access. J Vasc Surg 58: 1402-1407, 2013 [DOI] [PubMed] [Google Scholar]
- 88). Kwolek CJ, Jaff MR, Leal JI, et al. : Results of the roadster multicenter trial of transcarotid stenting with dynamic flow reversal. J Vasc Surg 62: 1227-1234, 2015 [DOI] [PubMed] [Google Scholar]
- 89). Schermerhorn ML, Liang P, Eldrup-Jorgensen J, et al. : Association of transcarotid artery revascularization vs transfemoral carotid artery stenting with stroke or death among patients with carotid artery stenosis. JAMA 322: 2313-2322, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90). Ghamraoui AK, Ricotta JJ 2nd: Outcomes of transcarotid artery revascularization (TCAR) in octogenarians and older. Ann Vasc Surg 68: 151-158, 2020 [DOI] [PubMed] [Google Scholar]
- 91). Kimoto S, Wada T, Ueno A, Hishida Y, Murakami K, Sato T: Surgical treatment on the carotid artery occlusion. A case of Apoplexy successfully surgically treated. J Clin Surg 17: 1109-1114, 1962(Japanese) [Google Scholar]
- 92). Ogata M, Yamashita T, Ono T, et al. : Experience in clinical application of blood vessel substitute in the parietal internal carotid artery occlusion. Brain Nerve 16: 516-522, 1964(Japanese) [PubMed] [Google Scholar]
- 93). Kageyama N, Nakajima S, Takeda A, Shirabane M: Carotid artery occlusion. -A successful operation case-. J Jpn. Surg Soc 27: 688-692, 1965(Japanese) [Google Scholar]
- 94). Takaku A, Suzuki J, Suzuki S: Neurosurgical aspects of carotid artery surgery in the neck. No To Shinkei 21: 1215-1224, 1969(Japanese) [PubMed] [Google Scholar]
- 95). Ono H: Carotid stenosis. Japanisch-Dtsch Med Ber 21: 69-97, 1976(Japanese) [Google Scholar]
- 96). Ueda S: Surgical procedures for the cervical carotid revascularization. Japanisch-Dtsch Ber 29: 310-335, 1984(Japanese) [Google Scholar]
- 97). Endo S, Kamiyama K, Iwai R, Oka N, Takaku A, Tsukamoto E: Carotid endarterectomy without internal shunt under mannitol administration. Analysis of 35 cases. Neurol Med Chir (Tokyo) 23: 198-202, 1983(Japanese) [DOI] [PubMed] [Google Scholar]
- 98). Mori K: Carotid endarterectomy (CEA). Jpn J Stroke 10: 481-490, 1988(Japanese) [Google Scholar]
- 99). Uno M, Nishitani K, Ueda S, Matsumoto K, Waga S: National questionnaire about the current situation of the carotid endarterectomy in Japanese neurosurgical facilities. Jpn J Stroke 17: 590, 1995(Japanese) [Google Scholar]
- 100). Endo T, Hayashi N, Kuwayama N, Hirashima Y: The existing state of carotid endarterectomy. -Part I: Number of cases and surgical indications. Jpn J Stroke 24: 421-424, 2002(Japanese) [Google Scholar]
- 101). Kuwana N, Mochimatsu Y, Fujino H, Saito A, Mashimo N: Percutaneous transluminal angioplasty for cervical carotid artery stenosis. -A preliminary report-. Jpn J Stroke 7: 142-149, 1985(Japanese) [Google Scholar]
- 102). Nakahara I, Taki W, Tanaka M, Matsumoto K, Kikuchi H: Protective balloon in percutaneous transluminal angioplasty for brachiocephalic arteries. Jpn J Stroke 16: 256-264, 1994(Japanese) [Google Scholar]
- 103). Miyagi O, Fujimaki H, Asakura K, et al. : Percutaneous transluminal angioplasty for arteriosclerotic stenosis of cervical supra-aortic arteries. Surg Cereb Stroke 21: 141-147, 1993 [Google Scholar]
- 104). Yamashita K, Okamoto S, Kim C, Nakatsu S, Miyasaki A, Hojo M: Emergent treatment of iatrogenic dissection of the internal carotid artery with the Palmaz-Schatz stent--case report. Neurol Med Chir (Tokyo) 37: 336-339, 1997 [DOI] [PubMed] [Google Scholar]
- 105). Yoshimura S, Kaku Y, Hayashi K, Ueda T, Sugimoto S, Sakai N: Stenting for stenosis of cervical internal carotid artery. Surg Cereb Stroke 28: 130-136, 2000(Japanese) [Google Scholar]
- 106). Yoshimura S, Kitajima H, Enomoto Y, Yamada K, Iwama T: Staged angioplasty for carotid artery stenosis to prevent postoperative hyperperfusion. Neurosurgery 64: ons122-ons128; discussion ons128, 2009 [DOI] [PubMed] [Google Scholar]
- 107). Uchida K, Yoshimura S, Shirakawa M, et al. : Experience of staged angioplasty to avoid hyperperfusion syndrome for carotid artery stenosis. Neurol Med Chir (Tokyo) 55: 824-829, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108). Hayakawa M, Sugiu K, Yoshimura S, et al. : Effectiveness of staged angioplasty for avoidance of cerebral hyperperfusion syndrome after carotid revascularization. J Neurosurg 18: 1-11, 2019 [DOI] [PubMed] [Google Scholar]
- 109). Veraldi GF, Scorsone L, Mastrorilli D, et al. : Carotid endarterectomy with modified eversion technique: results of a Single Center. Ann Vasc Surg 72: 627-636, 2021 [DOI] [PubMed] [Google Scholar]
- 110). Demirel S, Goossen K, Bruijnen H, Probst P, Böckler D: Systematic review and meta-analysis of postcarotid endarterectomy hypertension after eversion versus conventional carotid endarterectomy. J Vasc Surg 65: 868-882, 2017 [DOI] [PubMed] [Google Scholar]
- 111). Marsman MS, Wetterslev J, Jahrome AK, et al. : Carotid endarterectomy with patch angioplasty versus primary closure in patients with symptomatic and significant stenosis: a systematic review with meta-analyses and trial sequential analysis of randomized clinical trials. Syst Rev 10: 139, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112). Orrapin S, Benyakorn T, Siribumrungwong B, Rerkasem K: Patch angioplasty versus primary closure for carotid endarterectomy. Cochrane Database Syst Rev 8: CD000160, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113). AbuRahma AF, Darling RC 3rd: Literature review of primary versus patching versus eversion as carotid endarterectomy closure. J Vasc Surg 74: 666-675, 2021 [DOI] [PubMed] [Google Scholar]
- 114). Harky A, Chan JSK, Kot TKM, et al. : General anesthesia versus local anesthesia in carotid endarterectomy: a systematic review and meta-analysis. J Cardiothorac Vasc Anesth 34: 219-234, 2020 [DOI] [PubMed] [Google Scholar]
- 115). Marsman MS, Wetterslev J, Keus F, et al. : Plexus anesthesia versus general anesthesia for carotid endarterectomy: a systematic review with meta-analyses. Ann Med Surg (Lond) 65: 102327, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116). Uno M, Yagi K, Takai H, et al. : Comparison of single and dual monitoring during carotid endarterectomy. Neurol Med Chir (Tokyo) 61: 124-133, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117). Uno M, Nishi K, Shinno K, Nagahiro S: Carotid endarterectomy with external shunt: a new device and indication for use: technical note. Neurosurgery 48: 1174-1177, 2001 [DOI] [PubMed] [Google Scholar]
- 118). Uno M, Suzue A, Nishi K, Nagahiro S: Hemodynamic cerebral ischemia during carotid endarterectomy evaluated by intraoperative monitoring and post-operative diffusion-weighted imaging. Neurol Res 29: 70-77, 2007 [DOI] [PubMed] [Google Scholar]
- 119). Müller MD, Lyrer P, Brown MM, Bonati LH: Carotid artery stenting versus endarterectomy for treatment of carotid artery stenosis. Cochrane Database Syst Rev 2: CD000515, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120). Keyhani S, Cheng EM, Hoggatt KJ, et al. : Comparative effectiveness of carotid endarterectomy vs initial medical therapy in patients with asymptomatic carotid stenosis. JAMA Neurol 77: 1110-1121, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121). Keyhani S, Cheng EM, Hoggatt K, et al. : Comparative effectiveness of carotid stenting to medical therapy among patients with asymptomatic carotid stenosis. Stroke 53: 1157-1166, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122). European Carotid Surgery Trialists' Collaborative Group: Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet 351: 1379-1387, 1998 [PubMed] [Google Scholar]
- 123). Brown MM, Rogers J, Bland JM: Endovascular versus surgical treatment in patients with carotid stenosis in the Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS): a randomised trial. Lancet 357: 1729-1737, 2001 [PubMed] [Google Scholar]
- 124). Yadav JS, Wholey MH, Kuntz RE, et al. : Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med 351: 1493-1501, 2004 [DOI] [PubMed] [Google Scholar]
- 125). Halliday A, Mansfield A, Marro J, et al. : Prevention of disabling and fatal strokes by successful carotid endarterectomy in patients without recent neurological symptoms: randomised controlled trial. Lancet 363: 1491-1502, 2004 [DOI] [PubMed] [Google Scholar]
- 126). Mas JL, Chatellier G, Beyssen B, et al. : Endarterectomy versus stenting in patients with symptomatic severe carotid stenosis. N Engl J Med 355: 1660-1671, 2006 [DOI] [PubMed] [Google Scholar]
- 127). SPACE Collaborative Group, Ringleb PA, Allenberg J, et al. : 30 day results from the SPACE trial of stent-protected angioplasty versus carotid endarterectomy in symptomatic patients: a randomised non-inferiority trial. Lancet 368: 1239-1247, 2006 [DOI] [PubMed] [Google Scholar]
- 128). International Carotid Stenting Study investigators, Ederle J, Dobson J, et al. : Carotid artery stenting compared with endarterectomy in patients with symptomatic carotid stenosis (International Carotid stenting Study): an interim analysis of a randomised controlled trial. Lancet 375: 985-997, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129). Brott TG, Hobson RW 2nd, Howard G, et al. : Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med 363: 11-23, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130). Rosenfield K, Matsumura JS, Chaturvedi S, et al. : Randomized trial of stent versus surgery for asymptomatic carotid stenosis. N Engl J Med 374: 1011-1020, 2016 [DOI] [PubMed] [Google Scholar]
- 131). Brott TG, Howard G, Roubin GS, et al. : Long-term results of stenting versus endarterectomy for carotid-artery stenosis. N Engl J Med 374: 1021-1031, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132). Halliday A, Bulbulia R, Bonati LH, et al. : Second asymptomatic carotid surgery trial (ACST-2): a randomised comparison of carotid artery stenting versus carotid endarterectomy. Lancet 398: 1065-1073, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133). Reiff T, Eckstein HH, Mansmann U, et al. : Carotid endarterectomy or stenting or best medical treatment alone for moderate-to-severe asymptomatic carotid artery stenosis: 5-year results of a multicentre, randomised controlled trial. Lancet Neurol 21: 877-888, 2022 [DOI] [PubMed] [Google Scholar]
- 134). Kanitra JJ, Graham IA, Hayward RD, Granger DK, Berg RA, Haouilou JC: Estimated cost of transcarotid arterial revascularization compared with carotid endarterectomy and transfemoral carotid stenting. Cureus 14: e23539, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135). Kibrik P, Stonko DP, Alsheekh A, et al. : Association of carotid revascularization approach with perioperative outcomes based on symptom status and degree of stenosis among octogenarians. J Vasc Surg 76: 769-777.e2, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]