Abstract
Background:
Health literacy is a critical health determinant. To implement initiatives aiming at improving health literacy among children, adapted measurement tools are needed.
Objective:
This study aimed to translate, adapt, and test the Health Literacy Survey Child Questionnaire-15 (HLS-Child-Q15) to assess health literacy among French-speaking 8- to 11-year-old pupils.
Methods:
The HLS-Child-Q15 was translated and adapted to the French context to become the HLS-Child-Q15-FR. A cross-sectional survey was carried out using a written, self-reported questionnaire to assess the psychometric properties of the HLS-Child-Q15-FR.
Key Results:
Translation and adaptation of the HLS-Child-Q15 German-French translated versions were cross-referenced. Back-translation led to minor refinements. Qualitative pre-test among children led to simplifications in wording and structure. Validation of the HLS-Child-Q15-FR. Four trained interviewers collected data among 3,107 pupils in 74 elementary schools of the Auvergne-Rhône-Alpes region. HLS-Child-Q15-FR showed good reliability (alpha = 0.83). Exploratory factor analysis showed a two-factor model related to health care and primary prevention. Construct validity analyses suggested removing 3 items. External validity analyses indicated a significant and moderate relationship with perceived self-efficacy.
Conclusion:
This study aimed to address the issue of measuring health literacy among French-speaking 8- to 11-year-old pupils. The HLS-Child-Q15-FR showed a high internal consistency. Statistics suggested a two-dimensional thematic scale. These findings should be further investigated. [HLRP: Health Literacy Research and Practice. 2023;7(3):e144–e153.]
Plain Language Summary:
We translated and adapted the HLS-Child-Q15 to allow the measurement of health literacy, a critical health determinant, among French-speaking 8- to 11-year-old pupils. The HLS-Child-Q15-FR showed good statistical properties with high internal consistency as well as an internal two-factor model related to health care and primary prevention.
Health literacy is acknowledged as a critical determinant of health across the lifespan (Bollweg & Okan, 2019; Paakkari et al., 2019; World Health Organization, 2013). The World Health Organization (2017, p. 4) also acknowledged that health literacy “empowers and drives equity” and “must be an integral part of the skills, and competencies developed over a lifetime, first and foremost through the school curriculum.” However, to implement evidence-based initiatives aiming at improving health literacy among children and school curriculum, relevant, age- and cultural-adapted measurement tools are needed (Bollweg & Okan, 2019).
Bollweg and Okan (2019) identified 17 instruments to measure health literacy among children younger than age 13 years. None of them was available in French. More generally, to our knowledge, only one tool measuring health literacy has been validated in French and it was directed toward adults (Ousseine et al., 2018). However, the development of an age-specific tool is advised as well as children's involvement in the development of such instrument aiming to measure health literacy among children (Bollweg & Okan, 2019).
This study aimed to address this issue by translating, adapting, and testing a short scale developed to assess generic, self-reported, health literacy among French-speaking 8- to 11-year-old children.
With the objective to identify a tool measuring health literacy among pupils between ages 8 and 11 years, a literature review was conducted. The Health Literacy Survey Child Questionnaire-15 (HLS-Child-Q15), measuring self-reported health literacy in children age 9 to 10 year and performing well with 15 items was chosen (Bollweg, Okan, Freţian, et al., 2020). First, the covered age range is similar to our study population of 8- to 11-year-old pupils. Second, the HLS-Child-Q15 was based on the European Health Literacy Survey Questionnaire (HLS-EU-Q). It thus allows the perspective to measure health literacy over a lifetime with comparable tools.
Based on these facts, our work is in line with the assessment of generic health literacy and with the assessment of children's “perceived difficulty in accessing, understanding, appraising, and applying health information in the contexts of healthcare, disease prevention and health promotion” (Bollweg, Okan, Freţian, et al., 2020; Sørensen et al., 2012). This measure of children's health literacy is subjective and not objective like functional literacy based on performance tests. As a matter of fact, how easy or difficult children perceive something related to health care, health prevention, or health promotion might be a determinant of their future health-related conceptions and adopted behaviors.
Methods
As the HLS-Child-Q15 6 matched our selection criteria, we contacted Bollweg, Okan, Freţian, et al. (2020) to express our interest in the developed tool and to discuss the possibility to translate and adapt it to the French context. Following the German team agreement, development of the HLS-Child-Q15-FR (French version) was launched with a similar method to allow cross-cultural comparison.
Translation and Adaptation of the HLS-Child-Q15 for 8- to 11-Year-Old French Pupils
Consistently with guidelines to translate, adapt, and validate scales (Sousa & Rojjanasrirat, 2011) and with studies conducted in the field (Maindal et al., 2016; Ousseine et al., 2018), we adopted a 4-step approach to adapt the HLS-Child-Q15 for French pupils.
First, translation of the HLS-Child-Q15 from German to French was performed by a French native speaker and a translation professional. Then, back-translation from French to German was performed by a German native speaker and a second translation professional. Phrasing of each item was discussed until agreement.
Second, a qualitative pretest was conducted among a small group of a similar age range (8- to 11-year-old children) in a socially disadvantaged community center to ensure accessibility. Individual interviews were conducted. The understanding of the translated scale in general was discussed first, then each item was discussed individually. Information regarding these children was not recorded.
Third, a research-team meeting was held to discuss the translation process, to assess the scale's content and to make the contextual adjustments based on children's feedback.
Finally, a partner research team in educational sciences carried out an external reviewing on the translated and culturally adapted scale (see Acknowledgment section).
This four-step approach led to the development of the HLS-Child-Q15-FR.
Study Design
A cross-sectional survey was conducted using a written, self-reported questionnaire. The HLS-Child-Q15-FR scale was a part of a larger questionnaire, including 80 items overall related to children's well-being in school. This data collection was conducted in the Alliance for health project, a multi-partner intervention research developed to implement a comprehensive approach to health promotion at the school and community levels. Primary schools on four French departments (Cantal, Isère, Loire, Rhône) were randomly selected into the intervention or control group.
This article focuses only on the methods and results associated with the development and validation of the HLS-Child-Q15-FR. Statistical analyses were conducted on baseline data.
Sample and Data Collection
The survey is among 3rd to 5th grades pupils in primary schools drawn to be included in the ALLIANCE project. Discussion with education professionals led to the expectation that pupils in 3rd to 5th grades would be able to participate. Trained interviewers (reading, administration's rhythm, answers to questions related to items understanding, investigator's form) read the questions and answers. This organization ensures accessibility to the questionnaire for all children and limits non-completion because of reading issues.
The overall questionnaire was completed during one hour of school time in the presence of teachers who were invited to respect the confidentiality of pupils' answers.
Measures
Self-reported subjective health literacy was assessed using HLS-Child-Q15-FR encompassing 15 items asking pupils their perceived ease or difficulty in finding, understanding, and applying health-related information. Each item begins with “Is it easy or difficult for you to …?” Pupils answer each question using a 4-point scale from very easy, easy, difficult to very difficult. A mean score is calculated for each pupil. High perceived ease in dealing with health-information matches with a high score of self-reported subjective health literacy.
Perceived self-efficacy was assessed using 3 items consistent with the Bollweg, Okan, Freţian, et al. (2020) method to test the external validity: (1) “When I have a problem in an exercise, I always manage to find the solution”; (2) “Since I am good at school, I can solve all the exercises I am asked to do”; and (3) “If the exercise is very difficult, I still look for a way to manage to figure it out.” These three items were chosen among the French perceived self-efficacy scale developed by Fenouillet et al. (2014). Pupils answered these questions using 5-point scale from strongly disagree, disagree, neither agree nor disagree, agree to strongly agree.
Demographic variables included age, gender, and grade. The family sociodemographic status is assessed using the Family Affluence Scale III (FAS-III) measuring children's access to markers of material wealth such as having their own bedroom, a car, a dishwasher, and leaving home for holidays (Torsheim et al., 2016). As pupils might encounter difficulties identifying their parents or guardians' occupations, this 6-items measure was perceived as the most age-adapted one. A high score matches a high socioeconomic level. To conduct statistical analyses, pupils' scores were divided in three categories showed as relevant in the French context 12: (1) the 20% of pupils with the lowest FAS scores; (2) the 20% of pupils with the highest FAS scores; and (3) the remaining 60% of pupils with intermediate FAS score. As plain scores are calculated, the three categories were constructed with the threshold values allowing to be the closest to 20% of the sample.
Statistical Analysis
As preliminary analyses showed that average health literacy did not vary significantly between schools, municipalities, residential areas or school status, clustering analyses were not considered in this scale validation study.
First, an item analysis was conducted. Answers' distribution between modalities and missing responses were characterized. Items' performance was assessed through item difficulty, which should range from 20% to 80% for high performance (Sørensen et al., 2012). Items with high variance are also expected to perform better. Corrected item-total correlations were used to appraise item discrimination (poor correlation <0.3, a threshold consistent with guidelines in the field) (Costello & Osborne, 2005).
Internal consistency was measured using Cronbach's alpha. The standard cut-offs were considered (alpha ≥0.90 excellent, 0.80–0.90 good, 0.70–0.80 acceptable, 0.60–0.70 questionable, 0.50–0.60 poor, alpha ≤0.50 unacceptable) (Chalghaf et al., 2019; Tavakol & Dennick, 2011). Because alpha is influenced by the sample size and items, Revelle's omega and average split-half reliability were applied to confirm reliability.
Internal validity was appraised though three dimensions (Tavakol et al., 2008). Content validity was assessed through an exploratory factor analysis (EFA) to identify the scale's dimensions and whether any of the items captured information about the latent variable. The principal axis method with oblique rotation was used due to correlation between items. Bartlett's test of sphericity and Kaiser-Meyer-Olkin Criterion (KMO) were calculated to ensure data were adequate to conduct EFA.
Construct validity was assessed through a confirmatory factor analysis to test the formal hypothesis associated with the EFA results. Model fitting was assessed using Chi-squared, comparative fit index (CFI) CFI >0.9), Tucker-Lewis Index (TLI) (TLI >0.90), root mean square error of approximation (RMSEA) (RMSEA <0.05), and standardized root mean squared residual (SRMR) (SRMR <0.05). The best fitting model was identified, and composite reliability measures were computed on associated factors. The average variance extracted to assess convergent validity (>0.5) was measured, so as the composite reliability to assess discriminant validity (>0.7).
The dataset was randomly split (50:50) to perform EFA on one sample and Confirmatory Factors Analysis (CFA) on another.
External validity was assessed by measuring whether our latent construct was significantly correlated to other related external measures—in our case, to the concept of perceived self-efficacy. Thus, a construct gathering the 3 items was regressed on the health literacy scale.
Analyses were conducted with R software version 4.0.3 (2020-10-10). A 0.05 cut-off was chosen for all p values.
Ethical Processes
This study was submitted and approved by the INSERM Ethics Board (N°2019-095). Consistent with French data protection regulations, the survey was submitted to the Data Protection Officer at the University Jean Monnet Saint-Etienne. Information regarding the survey, data collection, storage and utilization was provided to pupils' parents or legal guardians. Both parents and children were informed that all information would be treated anonymously. Participation was voluntary and pupils were told they could stop at any moment. No incentive was used.
Results
Translation and Adaptation of the HLS-Child-Q15 for 8- to 11-Year-Old French Pupils
Translation and back-translation. German-French translated versions were cross-referenced and questions were adapted to remain the closest to the original meaning. French-German back-translation led to minor refinements.
Qualitative pre-test. Six children between ages 8 and 11 years were interviewed. They often associated health-related knowledge and actions to take care of their health to those carried out by their parents. Some sentences used words or grammatical structures too complex for the 8-year-old interviewee.
Research-team meeting. Wording and structure too complex were simplified. For instance, how easy or difficult is it for you to was changed for is it easy or difficult for you to. Examples were added to illustrate the 5th question as the following “for instance, in the morning, at noon or in the evening, with water or by eating?” Like the German version, “for you” was kept to limit, if possible, the bias emerging from references to adults' knowledge and actions.
External reviewing. Researchers in educational sciences proposed a few rewordings to ensure the understandability by 8- to 11-year-old pupils.
Validation of the Translated and Adapted HLS-Child-Q15 for 8- to 11-Year-Old French Pupils
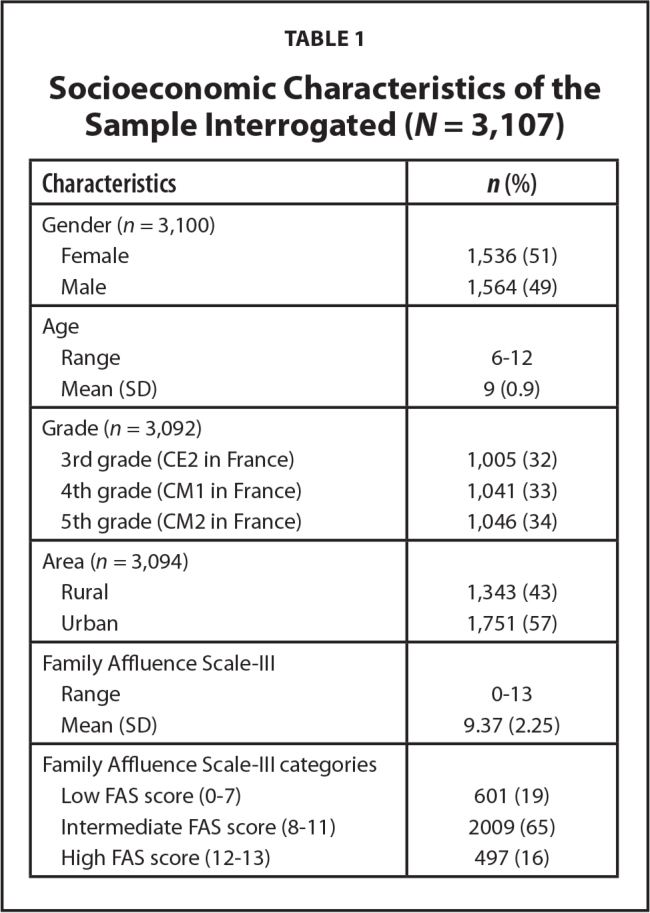
Sample and data collection. Four trained interviewers collected data among 3,107 pupils enrolled in 74 elementary schools between October 2019 and March 2020. The whole questionnaire took around 1 hour to be completed. Five minutes were necessary to read the HLS-Child-Q15-FR and allowing pupils to choose their answers.
Table 1 summarizes the sample characteristics.
Table 1.
Socioeconomic Characteristics of the Sample Interrogated (N = 3,107)
| Characteristics | n (%) |
|---|---|
|
| |
| Gender (n = 3,100) | |
| Female | 1,536 (51) |
| Male | 1,564 (49) |
|
| |
| Age | |
| Range | 6–12 |
| Mean (SD) | 9 (0.9) |
|
| |
| Grade (n = 3,092) | |
| 3rd grade (CE2 in France) | 1,005 (32) |
| 4th grade (CM1 in France) | 1,041 (33) |
| 5th grade (CM2 in France) | 1,046 (34) |
|
| |
| Area (n = 3,094) | |
| Rural | 1,343 (43) |
| Urban | 1,751 (57) |
|
| |
| Family Affluence Scale-III | |
| Range | 0–13 |
| Mean (SD) | 9.37 (2.25) |
|
| |
| Family Affluence Scale-III categories | |
| Low FAS score (0–7) | 601 (19) |
| Intermediate FAS score (8–11) | 2009 (65) |
| High FAS score (12–13) | 497 (16) |
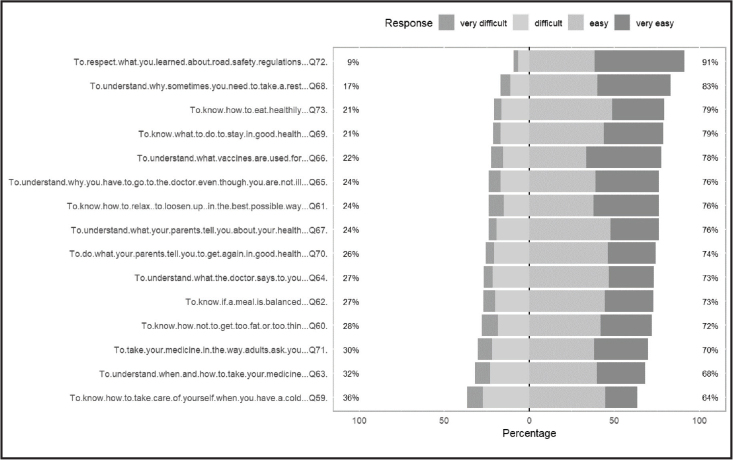
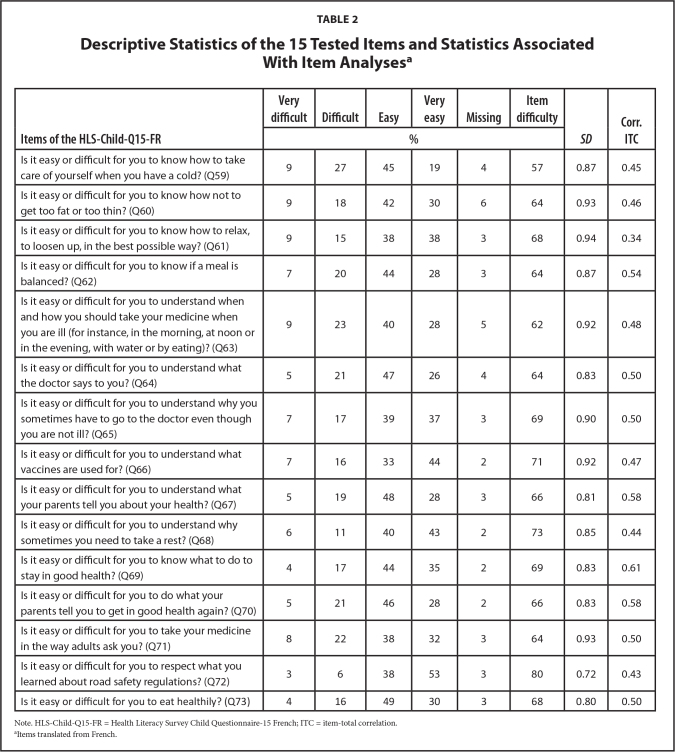
Item analyses. Missing answers ranged from 2% to 6%. The critical threshold of 10% was not reached. The item difficulty parameter ranged between 57% for Q59 to 80% for Q72. The item difficulty parameter was comprised between 20% and 80% showing high performance for the 15 items. Nevertheless, the item response distribution showed a skewness toward easy and very easy answers as illustrated in Figure 1.
Figure 1.
Graphical representation of the distribution of items responses where 1 = very difficult, 2 = difficult, 3 = easy, and 4 = very easy.
Standard deviation ranged from 0.72 for Q72 to 0.94 for Q61. Variance of all 15 items appeared suitable.
Corrected item-total correlations ranged from 0.34 for Q61 to 0.61 for Q69. The mean corrected item-total correlation was 0.492. No item showed poor correlation, even if Q61 showed a corrected item-total correlation (ITC) lower than the 0.4 validity threshold. Four items had a corrected ITC greater than 0.5 (Q62, Q67, Q69, Q70).
Table 2 summarizes the 15 tested items and their associated statistics.
Table 2.
Descriptive Statistics of the 15 Tested Items and Statistics Associated With Item Analysesa
| Items of the HLS-Child-Q15-FR | Very difficult | Difficult | Easy | Very easy | Missing | Item difficulty | SD | Corr. ITC |
|---|---|---|---|---|---|---|---|---|
| % | ||||||||
| Is it easy or difficult for you to know how to take care of yourself when you have a cold? (Q59) | 9 | 27 | 45 | 19 | 4 | 57 | 0.87 | 0.45 |
| Is it easy or difficult for you to know how not to get too fat or too thin? (Q60) | 9 | 18 | 42 | 30 | 6 | 64 | 0.93 | 0.46 |
| Is it easy or difficult for you to know how to relax, to loosen up, in the best possible way? (Q61) | 9 | 15 | 38 | 38 | 3 | 68 | 0.94 | 0.34 |
| Is it easy or difficult for you to know if a meal is balanced? (Q62) | 7 | 20 | 44 | 28 | 3 | 64 | 0.87 | 0.54 |
| Is it easy or difficult for you to understand when and how you should take your medicine when you are ill (for instance, in the morning, at noon or in the evening, with water or by eating)? (Q63) | 9 | 23 | 40 | 28 | 5 | 62 | 0.92 | 0.48 |
| Is it easy or difficult for you to understand what the doctor says to you? (Q64) | 5 | 21 | 47 | 26 | 4 | 64 | 0.83 | 0.50 |
| Is it easy or difficult for you to understand why you sometimes have to go to the doctor even though you are not ill? (Q65) | 7 | 17 | 39 | 37 | 3 | 69 | 0.90 | 0.50 |
| Is it easy or difficult for you to understand what vaccines are used for? (Q66) | 7 | 16 | 33 | 44 | 2 | 71 | 0.92 | 0.47 |
| Is it easy or difficult for you to understand what your parents tell you about your health? (Q67) | 5 | 19 | 48 | 28 | 3 | 66 | 0.81 | 0.58 |
| Is it easy or difficult for you to understand why sometimes you need to take a rest? (Q68) | 6 | 11 | 40 | 43 | 2 | 73 | 0.85 | 0.44 |
| Is it easy or difficult for you to know what to do to stay in good health? (Q69) | 4 | 17 | 44 | 35 | 2 | 69 | 0.83 | 0.61 |
| Is it easy or difficult for you to do what your parents tell you to get in good health again? (Q70) | 5 | 21 | 46 | 28 | 2 | 66 | 0.83 | 0.58 |
| Is it easy or difficult for you to take your medicine in the way adults ask you? (Q71) | 8 | 22 | 38 | 32 | 3 | 64 | 0.93 | 0.50 |
| Is it easy or difficult for you to respect what you learned about road safety regulations? (Q72) | 3 | 6 | 38 | 53 | 3 | 80 | 0.72 | 0.43 |
| Is it easy or difficult for you to eat healthily? (Q73) | 4 | 16 | 49 | 30 | 3 | 68 | 0.80 | 0.50 |
Note. HLS-Child-Q15-FR = Health Literacy Survey Child Questionnaire-15 French; ITC = item-total correlation.
Items translated from French.
HLS-Child-Q15-FR showed a Cronbach's alpha of 0.83 indicating good reliability. Revelle's omega (0.85) and average split-half reliability (0.83) supported the scale's reliability.
Internal validity. Bartlett's test of sphericity indicated significant correlations between variables (χ2(105) = 6996.3, p < .001) while the KMO Criterion (0.91) indicated that the data are largely sufficient to conduct factor analysis. A screen plot suggested the possibility of a 3-factor model and ideally a 2-factor model to keep eigenvalue strictly greater than 1. Two factors were extracted and accounted for 28% of the variance. Factors 1 and 2 had eigenvalues of 2.45 and 1.79, respectively, and explained 58% and 42%, respectively, of the variance.
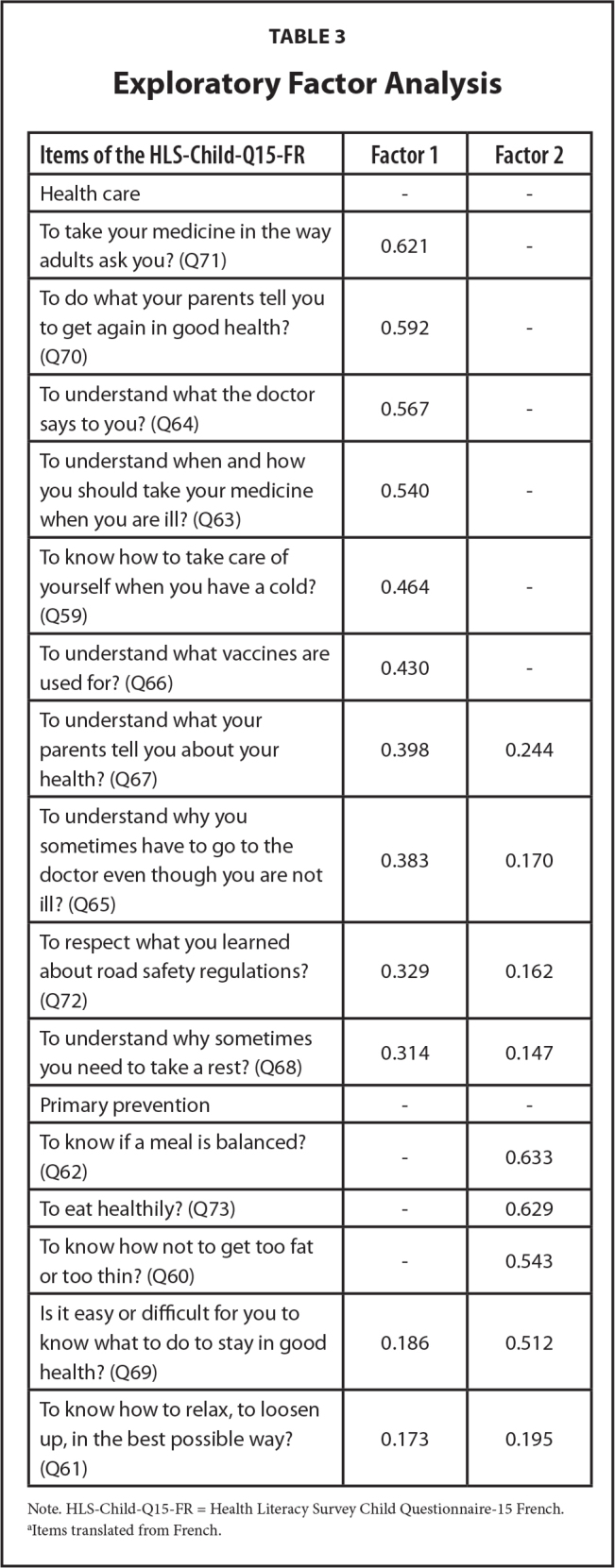
Eight of 15 items (Q59, Q63, Q64, Q65, Q66, Q67, Q70, Q71) loaded on factor 1 with factor loadings greater than 0.38; they referred to medication and being back in good health. Four items (Q60, Q62, Q69, Q73) loaded on factor 2 with factor loadings greater than 0.5; these items referred to diet and general health. Three items (Q61, Q68, Q72) with factor loadings less than 0.33 loaded neither in factor 1 nor in factor 2 (see Table 3).
Table 3.
Exploratory Factor Analysis
| Items of the HLS-Child-Q15-FR | Factor 1 | Factor 2 |
|---|---|---|
| Health care | - | - |
| To take your medicine in the way adults ask you? (Q71) | 0.621 | - |
| To do what your parents tell you to get again in good health? (Q70) | 0.592 | - |
| To understand what the doctor says to you? (Q64) | 0.567 | - |
| To understand when and how you should take your medicine when you are ill? (Q63) | 0.540 | - |
| To know how to take care of yourself when you have a cold? (Q59) | 0.464 | - |
| To understand what vaccines are used for? (Q66) | 0.430 | - |
| To understand what your parents tell you about your health? (Q67) | 0.398 | 0.244 |
| To understand why you sometimes have to go to the doctor even though you are not ill? (Q65) | 0.383 | 0.170 |
| To respect what you learned about road safety regulations? (Q72) | 0.329 | 0.162 |
| To understand why sometimes you need to take a rest? (Q68) | 0.314 | 0.147 |
| Primary prevention | - | - |
| To know if a meal is balanced? (Q62) | - | 0.633 |
| To eat healthily? (Q73) | - | 0.629 |
| To know how not to get too fat or too thin? (Q60) | - | 0.543 |
| Is it easy or difficult for you to know what to do to stay in good health? (Q69) | 0.186 | 0.512 |
| To know how to relax, to loosen up, in the best possible way? (Q61) | 0.173 | 0.195 |
Note. HLS-Child-Q15-FR = Health Literacy Survey Child Questionnaire-15 French.
Items translated from French.
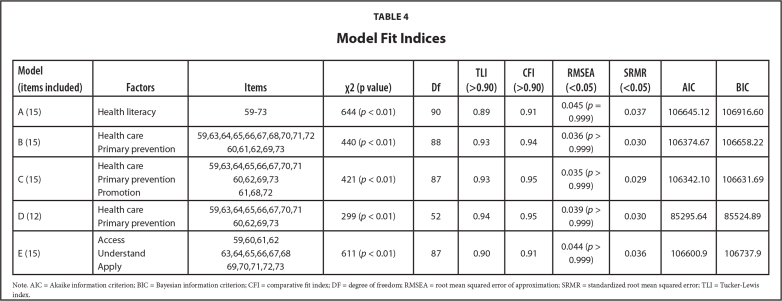
Construct validity. A contextual 3-factor model (model C) was computed in accordance with our EFA findings with factor 1 related to health care, factor 2 related to primary prevention, and factor 3 related to health promotion. A contextual 2-factor model (model D in Table 4) was assessed with the 12 items showing good factor loadings with factor 1 and factor 2 in our EFA. Finally, the conceptual framework of the HLS-EU-Q was tested. Three factors were accounted to assess the perceived difficulty of accessing (Q59 to 62), understanding (Q63 to 68), and applying (Q69 to 73) health information (model E in Table 4).
Table 4.
Model Fit Indices
| Model (items included) | Factors | Items | χ2 (p value) | Df | TLI (>0.90) | CFI (>0.90) | RMSEA (<0.05) | SRMR (<0.05) | AIC | BIC |
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| A (15) | Health literacy | 59–73 | 644 (p < 0.01) | 90 | 0.89 | 0.91 | 0.045 (p = 0.999) | 0.037 | 106645.12 | 106916.60 |
|
| ||||||||||
| B (15) | Health care | 59,63,64,65,66,67,68,70,71,72 | 440 (p < 0.01) | 88 | 0.93 | 0.94 | 0.036 (p > 0.999) | 0.030 | 106374.67 | 106658.22 |
| Primary prevention | 60,61,62,69,73 | |||||||||
|
| ||||||||||
| C (15) | Health care | 59,63,64,65,66,67,70,71 | 421 (p < 0.01) | 87 | 0.93 | 0.95 | 0.035 (p > 0.999) | 0.029 | 106342.10 | 106631.69 |
| Primary prevention | 60,62,69,73 | |||||||||
| Promotion | 61,68,72 | |||||||||
|
| ||||||||||
| D (12) | Health care | 59,63,64,65,66,67,70,71 | 299 (p < 0.01) | 52 | 0.94 | 0.95 | 0.039 (p > 0.999) | 0.030 | 85295.64 | 85524.89 |
| Primary prevention | 60,62,69,73 | |||||||||
|
| ||||||||||
| E (15) | Access | 59,60,61,62 | 611 (p < 0.01) | 87 | 0.90 | 0.91 | 0.044 (p > 0.999) | 0.036 | 106600.9 | 106737.9 |
| Understand | 63,64,65,66,67,68 | |||||||||
| Apply | 69,70,71,72,73 | |||||||||
Note. AIC = Akaike information criterion; BIC = Bayesian information criterion; CFI = comparative fit index; DF = degree of freedom; RMSEA = root mean squared error of approximation; SRMR = standardized root mean squared error; TLI = Tucker-Lewis index.
Except for model A, all models showed satisfactory Tucker-Lewis Index. All models showed significant Chi-squared, satisfactory CFI, SRMR and RMSEA with significant p values. The model showing the best indices and having the lowest degree of freedom, Akaike information criterion (AIC), Bayesian information criterion (BIC), and Chi-squared statistics is model D identifying health care and primary prevention areas.
Composite reliability measures alpha and omega were acceptable for the two factors health care (alpha = 0.75; omega = 0.75) and primary prevention (alpha = 0.69; omega = 0.68), but were not acceptable for the third factor health prevention (alpha = 0.43; omega = 0.42). On another hand, the average variance extracted (AVE) is lower than the 0.5 threshold for the three factors with the lowest AVE for the promotion factor.
External validity. The perceived self-efficacy (PSE) construct gathering 3 items was regressed on the 12-item health literacy scale. Standard estimates ranged from 0.47 to 0.59 for health care factor's items, from 0.52 to 0.56 for primary prevention factor's items, and from 0.50 to 0.59 for PSE-related items. Covariances' estimations with perceived self-efficacy reached 0.42 for the entire 12-item scale, 0.36 for the Healthcare factor and 0.38 for the Primary prevention factor. All p values were significant (p < .01). These data indicate a significant and moderate statistical relationship between health literacy and perceived self-efficacy.
Relationships with Sociodemographic Variables
Analyses of FAS-III score showed a non-significant increase of the mean health literacy score among the intermediate FAS score group compared to the low FAS score group (p = .12). There is, however, a significant increase of the mean health literacy score between the high FAS score group and the low FAS score group (p < .01).
No significant differences in mean health literacy scores were found between schools in urban vs. rural areas or between public vs. private schools.
A significant higher health literacy score (p < .01) was found among boys (mean = 2.55, standard deviation [SD] = 0.16) vs. girls (mean = 2.46, SD = 0.18). A significant increase of the health literacy score (p = .02) was also found regarding an increase in age (0.05 per year).
Discussion
This study aimed to address the issue of measuring health literacy among French-speaking 8- to 11-year-old pupils by translating, adapting, and testing a 15-item scale developed by Bollweg, Okan, Freţian, et al. (2020) to assess generic, self-reported, health literacy among primary school pupils. It is the first study to measure health literacy among a large sample of young French pupils, a population that has not yet received much attention in the field of health literacy's assessment despite the associated crucial issues.
Our findings suggest a two-dimensional thematic scale, not in a conceptual way (access, understand, and apply), but in a thematic one (information related to health care and primary prevention). Statistics showed a high internal consistency.
Translation and Adaptation of the HLS-Child-Q15 for 8- to 11-Year-Old French Pupils
As no major changes were needed, the first step of our work showed that the HLS-Child-Q15 scale was easily transferable in the French context. This finding supports the use of this scale across different countries. First, the costs of translation and cultural adaptation in similar developed countries are limited thanks to similar general lifestyle conditions. Second, it can allow cross-cultural comparison of studies among children as it is already done for the HLS-EU-Q. Third, as this scale was translated and adapted from previous research conducted in the field (Bollweg, Okan, Pinheiro, et al., 2020), it may allow comparison with studies conducted among pupils or even adults, for instance, from a lifetime perspective.
Validation of the Translated and Adapted HLS-Child-Q15 for 8- to 11-Year-Old French Pupils
Item analyses. We observed only a few percentages of missing answers. The data collection circumstances may explain this low rate as questions were read by trained interviewers in school hours with the teachers present. Interviewers' training was based on actual experience of data collection in primary schools from the involved researchers ensuring relevant instructions and contextual preparations.
Even if item 72 reached 80% of item difficulty, no items were too easy or too difficult. However, we can observe that answers are skewed toward the easy response spectrum. This finding is consistent with previous studies conducted in the field (Bollweg, Okan, Freţian, et al., 2020) underlining a perceived ease of dealing with health-related information. As health literacy is positively and significantly correlated with perceived health-efficacy, it might also reflect a social desirability bias of producing good results. Studies conducted among adults also showed this skewness toward easy and very easy answers (Duong et al., 2017; Lorini et al., 2017).
All corrected item-total correlations were higher than the 0.3 threshold. These indicators are satisfactory but also question whether the scale is unidimensional. The unidimensional aspect is also questioned by the not satisfactory TLI associated with model A.
Internal consistency and construct validity. The Cronbach's alpha, the Revelle's Omega, and the average split-half reliability coefficient all indicate high internal consistency. ITC coefficients, the screen plot, the EFA, and CFA all suggest a bi-dimensional scale.
Three items appeared to perform less than the 12 others: to respect what you learned about road safety regulations? (Q72), to understand why sometimes you need to take a rest? (Q68) and to know how to relax, to loosen up, in the best possible way? (Q61). These three items appeared more related to health promotion, but they did not appear to be related enough to each other to constitute a factor.
Results from statistical analyses suggest the most performing model to be D (highest TLI, higher CFI, lowest AIC and lowest BIC): two-factor solution with 12 items, health care, and primary prevention. This finding is consistent with Bollweg, Okan, Freţian, et al. (2020) who also found through their EFA a factor structure related to health topics. The other models with satisfactory indicators but higher AIC and BIC, such as model B, model C, and model E are, however, also consistent with conceptual frameworks relevant in the field. Future research should investigate further the existence of these latent factors and their associations with the conceptual framework of health literacy in childhood.
External validity. Correlation between HLS-Child-Q15-FR and perceived self-efficacy items were significant and moderate. Perceived self-efficacy was found associated with health literacy in previous studies conducted among children (Bollweg, Okan, Freţian, et al., 2020). According to Bollweg, Okan, Freţian, et al. (2020) this might be due to the notion of perceived difficulty inherent with the concept of health literacy.
In this study, we did not assess functional health literacy. This might be a limit as we were not able to relate with objective measure of competencies among pupils. However, perceived self-efficacy was found to be associated more with subjective health literacy than functional health literacy (Bollweg, Okan, Freţian, et al., 2020). Future research could analyze further relationships between these concepts and whether mediated effects exist.
Study Limitations
First, pupils did not have the possibility to answer I don't know. Although willingness not to answer and don't know responses are not distinguishable, it may also encourage children to choose an answer relevant for them. Our low rate of missing answers may illustrate that.
Second, our qualitative study was conducted on a small sample of pupils. Although it allowed us to test the translation and cultural adaptation of the scale, a wider sample could allow going further in analyzing children's answers, knowledge, and understanding of questions.
Third, consistently with all surveys, social desirability could have influenced children's answers. To lower this effect, the anonymity of answers was carefully explained to pupils, and it was reminded that, if they wanted, they could not answer questions that would make them feel uncomfortable.
Fourth, as mentioned previously, this measure of children's health literacy is subjective and self-reported. Although it has its drawbacks, it allows assessing pupils' perceptions with a tool already used in other countries and adapted from a widely used one among adults.
Finally, we also did not conduct the final step for testing a scale validity—test-retest reliability—because of limited human and financial resources. Testing the retest reliability of this promising tool could be an interesting perspective in future research.
Conclusion
This study aimed to address the issue of measuring health literacy among French-speaking 8- to 11-year-old pupils by translating, adapting, and testing the HLS-Child-Q15 developed by Bollweg, Okan, Freţian, et al. (2020). Statistics showed a high internal consistency. The exploratory factor analysis suggested a two-dimensional thematic scale related to health care and primary prevention. Several indicators also suggested that the scale could be reduced to 12 items. These findings should be confirmed by other studies or a confirmatory analysis among another sample of pupils.
Despite its few limitations, this study contributes to the growing field of research on health literacy among children and its associated crucial issues.
Acknowledgments
The authors thank Julie Pironom, Carine Simar, and Didier Jourdan, researchers from the Clermont-Auvergne University ACTé team who are a part of the Alliance research project management and who participated in the data collection; Torsten Bollweg and Orkan Okan for consultation and for use of the Health Literacy Survey Child Questionnaire-15 (HLS-Child-Q15); and all the teachers and pupils who supported the survey and completed the questionnaire.
Funding Statement
Grant: This research was funded by the Regional Health Agency of the Auvergne-Rhône-Alps region grant (2019-PPS-463) and the MILDECA (Mission Interministérielle de Lutte contre les Drogues Et les Conduites Addictives).
References
- Bollweg , T. M. , & Okan , O . ( 2019. ). Measuring children's health literacy: Current approaches and challenges . In Okan O. & Ullrich B. (Eds.), International handbook of health literacy: research, practice and policy across the life-span (pp. 83 – 98 ). Policy Press; . 10.51952/9781447344520.ch006 [DOI] [Google Scholar]
- Bollweg , T. M. , Okan , O. , Freţian , A. M. , Bröder , J. , Domanska , O. M. , Jordan , S. , Bruland , D. , Pinheiro , P. , & Bauer , U. ( 2020. ). Adapting the European Health Literacy Survey Questionnaire for fourth-grade students in Germany: Validation and psychometric analysis . HLRP: Health Literacy Research and Practice , 4 ( 3 ), e144 – e159 . 10.3928/24748307-20200428-01 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollweg , T. M. , Okan , O. , Pinheiro , P. , Bröder , J. , Bruland , D. , Freţian , A. M. , Domanska , O. M. , Jordan , S. , & Bauer , U. ( 2020. ). Adapting the European Health Literacy survey for fourth-grade students in Germany: Questionnaire development and qualitative pretest . HLRP: Health Literacy Research and Practice , 4 ( 2 ), e119 – e128 . 10.3928/24748307-20200326-01 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalghaf , N. , Guelmami , N. , Re , T. S. , Maldonado Briegas , J. J. , Garbarino , S. , Azaiez , F. , & Bragazzi , N. L. ( 2019. ). Trans-cultural adaptation and validation of the “teacher job satisfaction scale” in Arabic language among sports and physical education teachers (“Teacher of Physical Education Job Satisfaction Inventory”-TPEJSI): Insights for sports, educational, and occupational psychology . Frontiers in Psychology , 10 , 2234 doi: 10.3389/fpsyg.2019.02234 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello , A. B. , & Osborne , J . ( 2005. ). Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis . Practical Assessment, Research, and Evaluation , 10 ( 7 ). 10.7275/JYJ1-4868 [DOI] [Google Scholar]
- Duong , T. V. , Aringazina , A. , Baisunova , G. , Nurjanah, Pham T. V. , Pham K. M. , Truong T. Q. , Nguyen K. T. , Oo W. M. , Mohamad E. , Su T. T. , Huang H. L. , Sørensen K. , Pelikan J. M. , Van den Broucke S. , & Chang , P. W. ( 2017. ). Measuring health literacy in Asia: Validation of the HLS-EU-Q47 survey tool in six Asian countries . Journal of Epidemiology , 27 ( 2 ), 80 – 86 . 10.1016/j.je.2016.09.005 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenouillet , F. , Heutte , J. , Martin-Krumm , C. , & Boniwell , I. ( 2014. ). Validation française de l'échelle multidimensionnelle de satisfaction de vie chez l'élève (Multidimensional Students' Life Satisfaction Scale) . Canadian Journal of Behavioural Science/Revue canadienne des sciences du comportement , 47 ( 1 ), 83 – 90 . 10.1037/a0037624 [DOI] [Google Scholar]
- Lorini , C. , Santomauro , F. , Grazzini , M. , Mantwill , S. , Vettori , V. , Lastrucci , V. , Bechini , A. , Boccalini , S. , Bussotti , A. , & Bonaccorsi , G. ( 2017. ). Health literacy in Italy: A cross-sectional study protocol to assess the health literacy level in a population-based sample, and to validate health literacy measures in the Italian language . BMJ Open , 7 ( 11 ), e017812 10.1136/bmjopen-2017-017812 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maindal , H. T. , Kayser , L. , Norgaard , O. , Bo , A. , Elsworth , G. R. , & Osborne , R. H. ( 2016. ). Cultural adaptation and validation of the Health Literacy Questionnaire (HLQ): Robust nine-dimension Danish language confirmatory factor model . SpringerPlus , 5 ( 1 ), 1232 10.1186/s40064-016-2887-9 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ousseine , Y. M. , Rouquette , A. , Bouhnik , A.-D. , Rigal , L. , Ringa , V. , Smith , A. , & Mancini , J. ( 2017. ). Validation of the French version of the Functional, Communicative and Critical Health Literacy scale (FCCHL) . Journal of Patient-Reported Outcomes , 2 ( 1 ), 3 10.1186/s41687-018-0027-8 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paakkari , L. T. , Torppa , M. P. , Paakkari , O. P. , Välimaa , R. S. , Ojala , K. S. A. , & Tynjälä , J. A. ( 2019. ). Does health literacy explain the link between structural stratifiers and adolescent health? European Journal of Public Health , 29 , 919 – 924 . Advance online publication. 10.1093/eurpub/ckz011 PMID: [DOI] [PubMed] [Google Scholar]
- Sousa , V. D. , & Rojjanasrirat , W. ( 2011. ). Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: A clear and user-friendly guideline . Journal of Evaluation in Clinical Practice , 17 ( 2 ), 268 – 274 . 10.1111/j.1365-2753.2010.01434.x PMID: [DOI] [PubMed] [Google Scholar]
- Sørensen , K. , Van den Broucke , S. , Fullam , J. , Doyle , G. , Pelikan , J. , Slonska , Z. , Brand , H. , & the (HLS-EU) Consortium Health Literacy Project European . ( 2012. ). Health literacy and public health: A systematic review and integration of definitions and models . BMC Public Health , 12 ( 1 ), 80 10.1186/1471-2458-12-80 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torsheim , T. , Cavallo , F. , Levin , K. A. , Schnohr , C. , Mazur , J. , Niclasen , B. , Currie , C. , & the FAS Development Study Group . ( 2016. ). Psychometric validation of the revised family affluence scale: A latent variable approach . Child Indicators Research , 9 , 771 – 784 . 10.1007/s12187-015-9339-x PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tavakol , M. , Mohagheghi , M. A. , & Dennick , R. ( 2008. ). Assessing the skills of surgical residents using simulation . Journal of Surgical Education , 65 ( 2 ), 77 – 83 . 10.1016/j.jsurg.2007.11.003 PMID: [DOI] [PubMed] [Google Scholar]
- Tavakol , M. , & Dennick , R. ( 2011. ). Making sense of Cronbach's alpha . International Journal of Medical Education , 2 , 53 – 55 . 10.5116/ijme.4dfb.8dfd PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . ( 2013. ). Health literacy: The solid facts . https://apps.who.int/iris/bitstream/handle/10665/128703/e96854.pdf [Google Scholar]
- World Health Organization . ( 2017. ). Shanghai declaration on promoting health in the 2030 Agenda for Sustainable Development . Health Promotion International , 32 ( 1 ), 7 – 8 . 10.1093/heapro/daw103 PMID: [DOI] [PubMed] [Google Scholar]