Abstract
Aim: The dual-antiplatelet therapy (DAPT) score is recommended for predicting the risk of ischemia and bleeding for patients undergoing percutaneous coronary intervention (PCI). This study aimed to investigate the long-term prognostic value of the DAPT score in older PCI patients.
Methods: This study enrolled 10,724 consecutive patients who underwent PCI from January 2013 to December 2013 in Fu Wai hospital, among whom 2,981 (27.8%) were aged ≥ 65 years. The ischemic endpoint was major adverse cardiovascular and cerebrovascular events (MACCE, including myocardial infarction, all-cause death, and stroke). The bleeding endpoint was Bleeding Academic Research Consortium (BARC) 2, 3, or 5 bleeding.
Results: After a 5-year follow-up, 256 (12.0%) MACCEs and 53 (2.5%) BARC 2, 3, or 5 bleeding occurred. The patients were divided into two groups according to the DAPT score: the low-score (<2,n=1,646) and high-score (≥ 2,n=485) group. Multivariate Cox regression revealed that the risk of MACCE was similar between the two groups [hazard ratio (HR): 1.214, 95% confidence interval (CI): 0.916–1.609,P=0.178], whereas the risk of bleeding was significantly higher in the high-score group than in the low-score group (HR: 2.447, 95% CI: 1.407–4.257,P=0.002). The DAPT score did not show prognostic value in MACCE [area under the receiver operating characteristic curve (AUROC), 0.534; 95% CI: 0.496–0.572,P=0.079]; however, it demonstrated a certain prognostic value in BARC 2, 3, or 5 bleeding (AUROC, 0.646; 95% CI: 0.573–0.719,P<0.001).
Conclusion: This study suggested that in older PCI patients, the DAPT score did not show predictive value for MACCE; however, it had a certain predictive value for 5-year BARC 2, 3, or 5 bleeding.
Keywords: DAPT score, older, MACCE, bleeding, PCI
Abbreviations and Acronyms: CHD = coronary heart disease; PCI = percutaneous coronary intervention; DAPT = dual-antiplatelet therapy; MI = myocardial infarction; CHF = congestive heart failure; LVEF = left ventricular ejection fraction; MACCE = major adverse cardiovascular and cerebrovascular events; BARC = Bleeding Academic Research Consortium; HR = hazard ratio; CI = confidence interval; ROC = receiver operating characteristic curve; SYNTAX = Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery; AUROC = area under the receiver operating characteristic curve; ACS = acute coronary syndrome; PES = paclitaxel-eluting stent
Introduction
With the acceleration of population aging, there had been a sharp increase in the prevalence of coronary heart disease (CHD) among older people. Despite receiving percutaneous coronary intervention (PCI) and guideline-recommended intensive dual-antiplatelet and statin therapy, older patients with CHD are more prone to experience ischemic and bleeding events than younger patients 1 - 3) . In the era of global aging, early identification of older patients with high risks of long-term thrombosis and bleeding events who are undergoing PCI remains a challenge; early identification of these patients is important to improve prognosis.
The dual-antiplatelet therapy (DAPT) score is important for predicting the risk of ischemia and bleeding following PCI, which has been recommended by ESC and AHA/ACC guidelines of DAPT in coronary artery disease as a practical tool to guide clinical decision-making 4 , 5) . Several studies have validated that the DAPT score is capable of discriminating between high-score groups who have higher thrombosis risk and low-score groups who have higher bleeding risk 6 - 10) . Nonetheless, the external validation of the DAPT score predictive value is not completely consistent in the real world 11 , 12) . Furthermore, to date, there is no research evaluating the utility of the DAPT score in older patients undergoing PCI.
Aim
This study aimed to investigate the performance of the DAPT score in predicting the 5-year ischemia and bleeding risk in older patients undergoing PCI from a large-sample study in the real world.
Methods
Study Design and Population
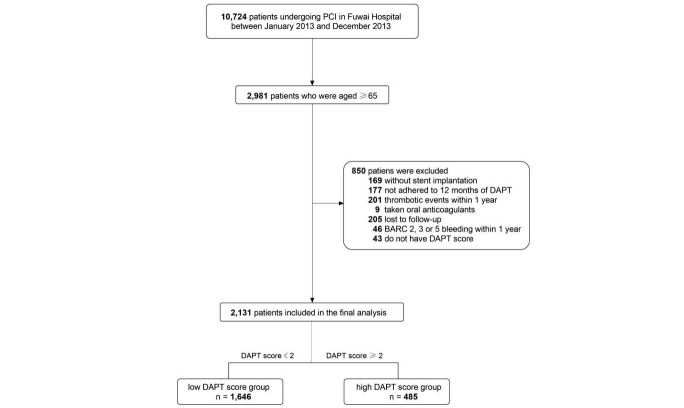
This was a prospective, single-center, observational cohort study. A total of 10,724 consecutive patients who had undergone PCI from January 2013 to December 2013 in Fu Wai hospital (National Center for Cardiovascular Diseases, Beijing, China) were enrolled, and patients aged ≥ 65 years were included in the final analysis. Consistent with the inclusion and exclusion criteria for the DAPT score 13) , we excluded patients who had any of the following conditions: absence of stent implantation, nonadherence to 12-month DAPT, occurrence of thrombotic and bleeding events within 1 year, intake of oral anticoagulants, and lost to follow-up. All the patients were given aspirin and P2Y12 receptor antagonist at baseline. After PCI, they were administered aspirin 100 mg daily indefinitely and clopidogrel 75 mg daily or ticagrelor 90 mg twice daily for at least 1 year. The study was conducted in accordance with the Declaration of Helsinki. The ethics committee of Fu Wai Hospital approved this research protocol. Written informed consent was obtained from all of the patients.
Definitions and Endpoints
In this study, the DAPT score was determined according to the original DAPT study 13) . The DAPT score calculator used for all patients consisted of nine factors: age, cigarette smoking, diabetes mellitus, myocardial infarction (MI) at presentation, prior PCI or prior MI, paclitaxel-eluting stent (PES), stent diameter <3 mm, congestive heart failure (CHF) or left ventricular ejection fraction (LVEF) <30%, and vein graft stent. The parameters of the DAPT score used the first laboratory results within 24 h of admission. Older patients were defined as those aged ≥ 65 years. The ischemia endpoint was defined as major adverse cardiovascular and cerebrovascular events (MACCEs, a composite of MI, all-cause death, or stroke). MI was diagnosed according to the third universal definition of myocardial infarction 14) . The bleeding endpoint was defined by Bleeding Academic Research Consortium (BARC) type 2, 3, or 5 bleeding 15) . Additional endpoints assessed included components of the above endpoints. The patients were divided into two groups according to the cutoff point of the DAPT score.
Follow-Up
Follow-up by telephone interview or clinical visits was scheduled at 30 days, 6 months, 1 year, 2 years, and 5 years, with a 91.5% follow-up rate at 5 years. If any clinical symptoms occurred or myocardial ischemia was documented, the patients were advised to return for coronary angiography. Time to event was calculated as the period between the date of PCI and the event, or the date of loss to follow-up, whichever came first. All adverse events were adjudicated by two independent cardiologists, and probably disagreement was resolved by consensus.
Statistical Analysis
Continuous variables with normal distribution were expressed as mean±standard deviation and compared using Student’s t-test. Categorical variables were expressed as numbers (%) and compared using the Pearson χ2 test or Fisher’s exact test. According to the risk stratification of the original DAPT score 13) , the patients were divided into the high-score group (score ≥ 2) and low-score group (score <2). Survival curves were generated in each score group by the Kaplan–Meier method, and differences were compared using the log-rank test. Univariate and multivariate Cox regression was used for survival analysis. Gender, body mass index, and other variables, which were statistically significant in the univariate Cox regression, were included in the final multivariate analysis. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated. To evaluate the ability of the DAPT score to predict MACCE and bleeding, receiver operating characteristic (ROC) analysis was conducted. The association between the DAPT score and endpoints in different subgroups was assessed by Cox regression models with tests for interaction. Two-sided P<0.05 was considered to indicate statistical significance. All statistical analyses were conducted using SPSS 25.0 (IBM Corp., Armonk, New York, USA).
Results
Patients’ Characteristics
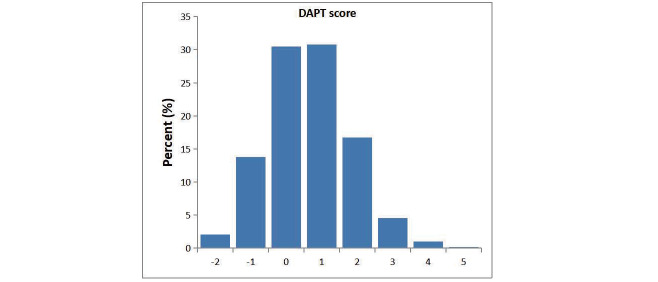
Among 10,724 consecutive patients who underwent PCI throughout 2013 in Fu Wai Hospital, 2,981 aged ≥ 65 years were enrolled. After excluding patients according to the exclusion criteria, 2,131 were finally included in this study ( Supplementary Fig.1 ) . The average age of the patients was 70.3±4.5 years, and 784 (36.8%) of them were female. Most patients took clopidogrel, and only a few (0.2%) took ticagrelor. According to the DAPT cutoff score of 2 recommended by the guidelines, the patients were divided into the high-score group (score ≥ 2, n=485) and the low-score group (score <2, n=1,646). The high-score group had younger patients; had lesser proportion of women; had higher number of patients with history of peripheral vascular disease, stroke, and coronary artery bypass grafting treatments; had higher SYNTAX score; had higher proportion of smokers; had higher number of patients with diabetes; had patients who previously underwent PCI or had MI; had patients with MI at presentation; had patients with CHF or LVEF <30%; and used stent diameter <3 mm, vein graft stent, PES, and had lesser proportion of patients used second- or third-generation stent compared with the low-score group ( Table 1 ) . The distribution of the DAPT score is presented in Fig.1 .
Supplementary Fig.1. Patient flow chart.
PCI, percutaneous coronary intervention; DAPT, dual-antiplatelet therapy; BARC, Bleeding Academic Research Consortium
Table 1. Baseline characteristics of patients.
| Parameters | low DAPT score (score <2, n= 1,646) | high DAPT score (score ≥ 2, n= 485) | P Value |
|---|---|---|---|
| Age, years | 71.0±4.6 | 69.8±3.9 | <0.001*** |
| Female | 671 (40.8) | 113 (23.3) | <0.001*** |
| BMI, kg/m2 | 25.3±3.1 | 25.1±3.2 | 0.381 |
| Hypertension | 1,165 (70.8) | 341 (70.3) | 0.842 |
| Peripheral vascular disease | 51 (3.1) | 30 (6.2) | 0.002*** |
| Previous stroke | 250 (15.2) | 96 (19.8) | 0.016*** |
| Prior CABG | 77 (4.7) | 51 (10.5) | <0.001*** |
| ACS | 983 (59.7) | 309 (63.7) | 0.114 |
| Ccr <60 ml/min | 355 (21.6) | 105 (21.6) | 0.969 |
| SYNTAX score | 11.9±8.5 | 13.3±9.0 | 0.002*** |
| Factors in DAPT score | |||
| Age ≥ 75 | 411 (25.0) | 46 (9.5) | <0.001*** |
| Cigarette smoking | 564 (34.3) | 352 (72.6) | <0.001*** |
| Diabetes | 374 (22.7) | 291 (60.0) | <0.001*** |
| Prior PCI or MI | 411 (25.0) | 331 (68.2) | <0.001*** |
| MI at presentation | 152 (9.2) | 150 (30.9) | <0.001*** |
| CHF or LVEF <30% | 3 (0.2) | 49 (10.1) | <0.001*** |
| Stent diameter <3mm | 801 (48.7) | 398 (82.1) | <0.001*** |
| Vein graft stent | 0 (0) | 7 (1.4) | <0.001*** |
| Paclitaxel-eluting stent | 21 (1.3) | 25 (5.2) | <0.001*** |
| 2nd or 3rd generation stent | 1,254 (76.2) | 333 (68.7) | <0.001*** |
Values are presented as mean±standard deviation, or n (%).
DAPT, dual-antiplatelet therapy; BMI, body mass index; MI, myocardial infarction; PCI, percutaneous coronary intervention; CABG, coronary artery bypass grafting; ACS, acute coronary syndrome; Ccr, creatinine clearance rate; SYNTAX, Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery; CHF, congestive heart failure; LVEF, left ventricular ejection fraction
***P values indicating statistical significance
Fig.1. Distribution of the DAPT score among older PCI patients.
DAPT, dual-antiplatelet therapy; PCI, percutaneous coronary intervention
5-year Incidence Rates between the High- and Low-Score DAPT Groups
After a 5-year follow-up, 256 (12.0%) patients experienced MACCE [among them, 69 (3.2%) experienced MI, 109 (5.1%) all-cause death, and 93 (4.4%) stroke], whereas 53 (2.5%) experienced BARC 2, 3, or 5 bleeding. No significant differences were observed in the incidence rates of MACCE (14.2% vs. 11.4%) and its component [including MI (3.3% vs. 3.2%), all-cause death (6.6% vs. 4.7%), and stroke (4.9% vs. 4.2%)] between the high- and low-score groups. However, for BARC 2, 3, or 5 bleeding, the event rate was significantly higher in the high-score than in the low-score group (4.7% vs. 1.8%, P<0.001) ( Supplementary Table 1 ) . BARC 3 or 5 bleeding is presented in Supplementary Table 1 .
Supplementary Table 1. 5-year incidence rates of high vs. low DAPT score.
| low DAPT score (score <2, n= 1,646) | high DAPT score (score ≥ 2, n= 485) | P Value | |
|---|---|---|---|
| MACCE | 187 (11.4%) | 69 (14.2%) | 0.088 |
| BARC 2, 3 or 5 bleeding | 30 (1.8%) | 23 (4.7%) | <0.001*** |
| MI | 53 (3.2%) | 16 (3.3%) | 0.931 |
| All-cause death | 77 (4.7%) | 32 (6.6%) | 0.092 |
| Stroke | 69 (4.2%) | 24 (4.9%) | 0.474 |
| BARC 3 or 5 bleeding | 9 (0.5%) | 7 (1.3%) | 0.044*** |
DAPT, dual-antiplatelet; MACCE, major adverse cardiovascular and cerebrovascular events; BARC, Bleeding Academic Research Consortium; MI, myocardial infarction
***P values indicating statistical significance
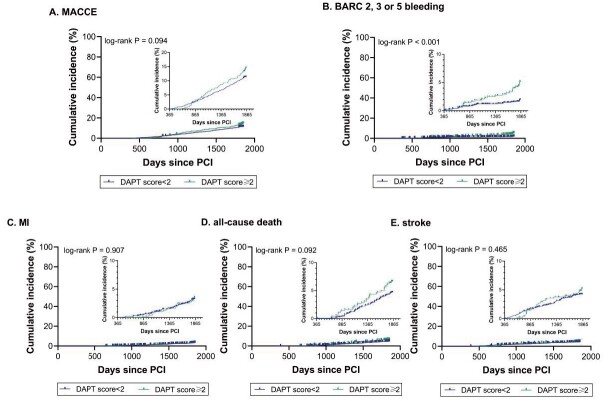
Kaplan–Meier Survival Curve Analysis between the High- and Low-Score Groups
Kaplan–Meier survival curve analysis revealed that the cumulative 5-year incidence rate of MACCE was similar between the two groups (P=0.094). However, patients with high scores had higher cumulative 5-year incidence of BARC 2, 3, or 5 bleeding than those with low scores (P<0.001). Further analysis revealed that the cumulative incidences of MI, all-cause death, and stroke were similar between the two groups ( Fig.2 ) .
Fig.2. Kaplan–Meier curve analysis of clinical outcomes according to the different DAPT score groups.
DAPT, dual-antiplatelet therapy; MACCE, major adverse cardiovascular and cerebrovascular events; BARC, Bleeding Academic Research Consortium; MI, myocardial infarction; PCI, percutaneous coronary intervention
Cox Regression Analysis
After multivariate adjustment, the risk of MACCE (HR: 1.214, 95% CI: 0.916–1.609) was similar between the two groups, whereas the risk of BARC 2, 3, or 5 bleeding in patients with high scores was 2.447 times higher than those in patients with low scores (HR: 2.447, 95% CI: 1.407–4.257). For further analysis, the risks of MI (HR: 0.891, 95% CI: 0.501–1.585), all-cause death (HR: 1.346, 95% CI: 0.883–2.052), and stroke (HR: 1.232, 95% CI: 0.769–1.972) were still similar between the two groups ( Table 2 ) . The associations between each component in the DAPT score and MACCE as well as BARC 2, 3, or 5 bleeding are presented in Supplementary Table 2 .
Table 2. Cox regression of high vs. low DAPT score.
| low DAPT score (score <2) | high DAPT score (score ≥ 2) | P Value | |
|---|---|---|---|
| MACCE | |||
| Univariate Cox regression [HR, (95%CI)] | Reference | 1.266 (0.960-1.668) | 0.094 |
| Multivariate Cox regression [HR, (95%CI)] | Reference | 1.214 (0.916–1.609) | 0.178§ |
| BARC 2, 3 or 5 bleeding | |||
| Univariate Cox regression [HR, (95%CI)] | Reference | 2.631 (1.528-4.529) | <0.001*** |
| Multivariate Cox regression [HR, (95%CI)] | Reference | 2.447 (1.407-4.257) | 0.002***§ |
| MI | |||
| Univariate Cox regression [HR, (95%CI)] | Reference | 1.034 (0.591-1.809) | 0.906 |
| Multivariate Cox regression [HR, (95%CI)] | Reference | 0.891 (0.501-1.585) | 0.695§ |
| All-cause death | |||
| Univariate Cox regression [HR, (95%CI)] | Reference | 1.423 (0.942-2.148) | 0.094 |
| Multivariate Cox regression [HR, (95%CI)] | Reference | 1.346 (0.883-2.052) | 0.167§ |
| Stroke | |||
| Univariate Cox regression [HR, (95%CI)] | Reference | 1.189 (0.747-1.891) | 0.466 |
| Multivariate Cox regression [HR, (95%CI)] | Reference | 1.232 (0.769-1.972) | 0.386§ |
DAPT, dual-antiplatelet therapy; MACCE, major adverse cardiovascular and cerebrovascular events; BARC, Bleeding Academic Research Consortium; MI, myocardial infarction; HR, Hazard ratio; CI, confidence interval
***P values indicating statistical significance
§Multivariate Cox regression was adjusted for gender, body mass index and other significant variables in the univariate model
Supplementary Table 2. Univariate and multivariate Cox regression of each risk factors with clinical outcomes.
| Factors | MACCE | BARC 2, 3 or 5 bleeding | ||||||
|---|---|---|---|---|---|---|---|---|
| Crude HR | P value | Adjusted HR§ | P value | Crude HR | P value | Adjusted HR§ | P value | |
| Female | 0.980 (0.759–1.264) | 0.875 | 1.258 (0.930–1.702) | 0.136 | 0.675 (0.372–1.228) | 0.198 | 0.957 (0.476–1.926) | 0.902 |
| BMI | 1.003 (0.965–1.043) | 0.877 | 0.995 (0.957–1.035) | 0.807 | 1.001 (0.919–1.091) | 0.976 | 0.997 (0.913–1.088) | 0.944 |
| Hypertension | 1.450 (1.082–1.943) | 0.013*** | 1.466 (1.089–1.972) | 0.012*** | 1.816 (0.913–3.614) | 0.089 | ||
| Peripheral vascular disease | 1.639 (0.973–2.761) | 0.063 | 1.012 (0.246–4.157) | 0.987 | ||||
| Previous stroke | 1.173 (0.855–1.609) | 0.324 | 1.857 (1.008–3.420) | 0.047 | 1.833 (0.993–3.382) | 0.053 | ||
| Prior CABG | 1.887 (1.258–2.831) | 0.002*** | 1.818 (1.209–2.734) | 0.004*** | 2.083 (0.891–4.873) | 0.091 | ||
| Risk factors in DAPT score | ||||||||
| Age ≥ 75 | 1.312 (0.991–1.736) | 0.058 | 1.110 (0.583–2.112) | 0.751 | ||||
| Cigarette smoking | 1.440 (1.127–1.840) | 0.004*** | 1.607 (1.203–2.146) | 0.001*** | 1.749 (1.016–3.012) | 0.044*** | 1.630 (0.867–3.066) | 0.129 |
| Diabetes | 0.190 (0.920–1.539) | 0.185 | 1.705 (0.990–2.935) | 0.054 | ||||
| Prior PCI or MI | 1.262 (0.982–1.620) | 0.069 | 2.125 (1.239–3.644) | 0.006*** | 2.029 (1.178–3.496) | 0.011*** | ||
| MI at presentation | 0.789 (0.539–1.155) | 0.223 | 1.586 (0.817–3.080) | 0.173 | ||||
| CHF or LVEF <30% | 1.973 (1.069–3.610) | 0.027*** | 2.083 (1.136–3.817) | 0.018*** | 2.614 (0.815–8.383) | 0.106 | ||
| Stent diameter <3mm | 0.976 (0.762–1.249) | 0.845 | 1.279 (0.734–2.228) | 0.386 | ||||
| Vein graft stent | 2.627 (0.654–10.563) | 0.174 | 0.050 (0.000–1083.117) | 0.784 | ||||
| Paclitaxel-eluting stent | 1.507 (0.745–3.047) | 0.254 | 0.048 (0.000–157.125) | 0.462 | ||||
DAPT, dual-antiplatelet; BMI, body mass index; CABG, coronary artery bypass grafting; MI, myocardial infarction; PCI, percutaneous coronary intervention; CHF, congestive heart failure; LVEF, left ventricular ejection fraction; HR, hazard ratio; CI, confidence interval; MACCE, major adverse cardiovascular and cerebrovascular events; BARC, Bleeding Academic Research Consortium; MI, myocardial infarction
***P values indicating statistical significance
§Gender, BMI and other variables which were statistically significant in univariate Cox regression were included in the multivariate analysis
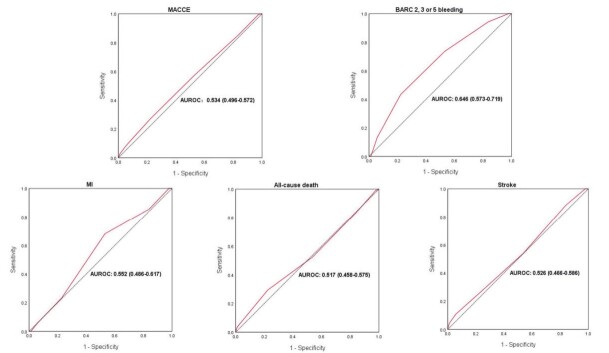
Predictive Value of the DAPT Score
When MACCE was used as the endpoint, the DAPT score did not exhibit a predictive value for ischemic events with an AUROC of 0.534 (95% CI 0.496-0.572, P=0.079). But when BARC 2, 3, or 5 bleeding was used as the endpoint, the DAPT score had a certain prognostic value in bleeding events with an AUROC of 0.646 (95% CI: 0.573–0.719, P<0.001). In further analysis, when MI, all-cause death, and stroke were used as the endpoint, the DAPT score did not exhibit significant predictive values in MI with an AUROC of 0.552 (95% CI: 0.486–0.617, P=0.144), all-cause death with an AUROC of 0.517 (95% CI: 0.458–0.575, P=0.560), and stroke with an AUROC of 0.526 (95% CI: 0.466–0.586, P=0.398) ( Fig.3 ) .
Fig.3. The AUROC of the DAPT score for predicting MACCE; BARC 2, 3, or 5 bleeding; MI; all-cause death; and stroke.
AUROC, area under the receiver operating characteristic curve; DAPT, dual-antiplatelet therapy; MACCE, major adverse cardiovascular and cerebrovascular events; BARC, Bleeding Academic Research Consortium; MI, myocardial infarction
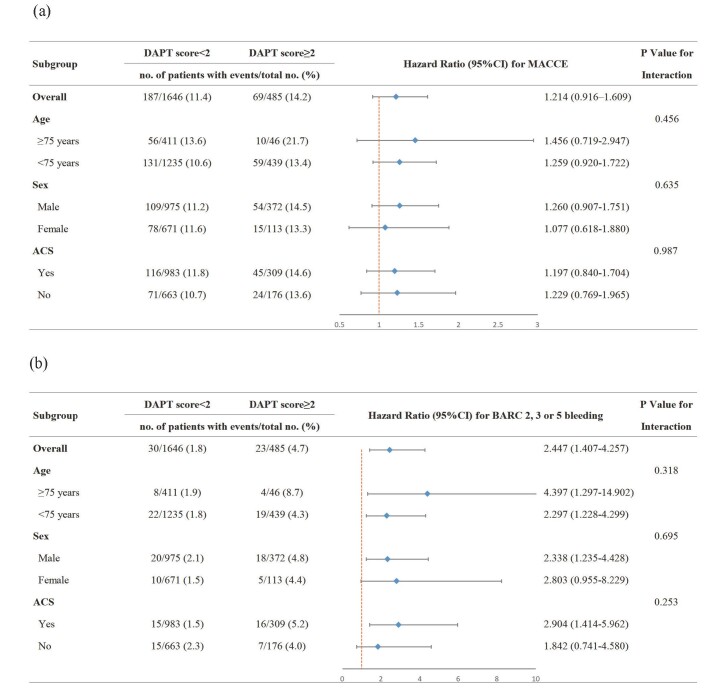
Subgroup Analysis
In the total population, no significant difference was observed in MACCE between the high- and low-score groups. This result was consistent in different subgroups, regardless of age, sex, and acute coronary syndrome (ACS) ( Fig.4a ) . Furthermore, the association between the DAPT score and BARC 2, 3, or 5 bleeding showed no significant interaction with age, sex, and ACS (P value for interaction >0.05) ( Fig.4b ) .
Fig.4. Subgroup analysis of the association between DAPT score and endpoints.
Hazard ratios (HRs) and 95% confidence intervals (CIs) are shown for the MACCE (a) and BARC 2, 3, or 5 bleeding (b). P represents the interaction test between the variable and the DAPT score. DAPT, dual-antiplatelet therapy; MACCE, major adverse cardiovascular and cerebrovascular events; ACS, acute coronary syndrome; BARC, Bleeding Academic Research Consortium
Discussion
DAPT score is an important clinical decision tool recommended by the guidelines for predicting the risk of ischemia and bleeding following PCI to identify patients who could benefit from DAPT treatment beyond 1 year 13) . In this real world large-sample study, we firstly evaluated the predictive performance of the DAPT score for 5-year MACCE and BARC 2, 3, or 5 bleeding risk in older PCI patients. The main findings were as follows: (1) the DAPT score did not exhibit predictive value for 5-year MACCE in older PCI patients; (2) however, the DAPT score had a certain predictive value for 5-year BARC 2, 3, or 5 bleeding in older PCI patients.
Predictive Value for MACCE
Our study found that the DAPT score was not predictive of long-term MACCE in older PCI patients. Several studies evaluating the validity of the DAPT score have been conducted as it was recommended by guidelines 4) . Surprisingly, the results were inconsistent in the external validations. In the original DAPT study 13) , the DAPT score exhibited moderate predictive value for 12 to 30 months of ischemic events following PCI (C-statistic=0.70). Another study by Brener et al. 6) reported that the DAPT score exhibited predictive value for the composite of MI or stent thrombosis with a C-statistic of 0.71. However, an analysis from the ISAR-SAFE trial 16) revealed that the risk of ischemia was similar between the high-score (>2) and low-score (≤ 2) groups (P=0.11). These inconsistent results may be related to different clinical endpoints, study populations, and follow-up durations.
It is worth noting that compared with the above research, our study focused on older PCI patients and did not show the predictive value of DAPT score for ischemic events at a long-term follow-up. The possible reasons were as follows: (1) Older patients usually have characteristics of frequent comorbidities, altered pharmacokinetics and pharmacodynamics, and hemostatic factor plasma level disorders 17) and have high ischemia and bleeding risks 18 , 19) . Our findings suggested that the DAPT score is inappropriate for the prediction of ischemic events in this population. (2) The discrepancy may stem from different clinical endpoints. This study had a follow-up duration of 5 years and used the hard endpoint MACCE (composite of myocardial infarction, all-cause death, or stroke), which is often used in clinical practice. (3) The different stent types may explain part of the negative result. The proportion of patients using PES was significantly lower (2.2% vs 22.9%) in this study than in the original DAPT study 13) . In fact, the original DAPT study also performed a subgroup of patients with second-generation everolimus-eluting stent and found that the treatment effect for ischemic and bleeding events between the high- and low-score groups was not significant. Meanwhile, the PRODIGY study demonstrated that the effect of the difference by DAPT score for the ischemic outcome also disappeared after excluding patients treated with PES 10) . These findings indicated that the influence of different stent types needs to be examined when considering the predictive value of the DAPT score. In summary, we found that the DAPT score could not show predictive value for MACCE. In the future, a more suitable risk score for predicting ischemia for the older Chinese population needs to be established.
Predictive value for bleeding
We initially reported that the DAPT score had a predictive value for long-term BARC 2, 3, or 5 bleeding in older PCI patients. The original DAPT study demonstrated a predictive value for 12–30 months of moderate and severe bleeding following PCI (C-statistic 0.68) 13) . However, external validation studies have shown poor predictive value of DAPT score for bleeding. Chichareon et al. 20) reported that the DAPT score could not predict BARC 3 or 5 bleeding (0.44% of patients experienced bleeding), and Ueda et al. 21) showed that the DAPT score had poor predictive value for fatal or major bleeding (0.66% of patients experienced bleeding). The different bleeding endpoints and follow-up days could be the possible reasons. Meanwhile, the low bleeding rates may influence the risk prediction performance of the DAPT score 22) . In our study, BARC 2, 3, or 5 bleeding was defined as the bleeding endpoint, and we followed up for 5 years, which had a relatively high cumulative bleeding rate (2.5%) than previous studies 20 , 21) and thus could show predictive value for bleeding.
Interestingly, the original DAPT study 13) demonstrated that lower score was associated with a higher risk of bleeding; however, our study found that a higher DAPT score was associated with a higher bleeding risk. There were some potential explanations for the contradicting results. First, the original DAPT study showed that older age was a significant risk factor for bleeding (1 point for 65–75 years old, 2 points for age ≥ 75 years) 13) ; in this study, all patients enrolled were aged ≥ 65 years, corresponding to those who were at high bleeding risk in the DAPT score. Therefore, the distribution of DAPT score in older population has changed and this may have an impact on the result. Of note, our study also analyzed the association between age and bleeding in the Cox regression model. We found that age ≥ 75 years was not an effective cutoff point for bleeding event prediction in older PCI patients. Second, prior PCI or MI was a significant risk factor for BARC 2, 3, or 5 bleeding in the older patients in the present study, whereas it was considered as a risk factor for ischemia risk in the original DAPT study. A previous randomized clinical trial of 9,013 PCI patients with a median follow-up of 5 years found that PCI or MI at follow-up was a risk factor for BARC 3 or 5 bleeding 23) . In addition, the CREDO-Kyoto trial 24) showed that prior MI was a significant risk factor for bleeding and ultimately included this factor in the bleeding prediction score. These two studies and our results both showed that prior PCI or MI, an ischemia risk variable in the original DAPT study, was an important risk factor for bleeding events, resulting in high DAPT score in older patients with higher bleeding risk. For older PCI patients, our study provided an important view that the higher the DAPT score, the higher the bleeding risk. Notably, there may be ethnic disparities in thrombosis and bleeding tendency between Asians and Caucasians according to “East Asia paradox,” 25) which could have an influence on the utility of the DAPT score. Therefore, the prognostic value of the DAPT score in older patients from different races needs to be further evaluated in the future.
In conclusion, the predictive value of the DAPT score in older PCI patients differs from that in the original DAPT study. Older patients are usually at a high risk of both ischemia and bleeding, which may influence the performance of the DAPT score. This study not only pointed out the limitations of the DAPT score in predicting ischemic events in older PCI patients but also supplemented a new perspective for the DAPT score in predicting BARC 2, 3, or 5 bleeding. Therefore, clinicians should consider individual differences and use comprehensive risk assessment tools to better guide health management in older PCI patients.
Limitations
This study had some limitations that need to be acknowledged. First, this was a single-center study, which may potentially limit the generalizability of our findings. Second, in this study, most patients took clopidogrel. Further studies are warranted to evaluate the efficacy of this score for new antiplatelet drugs and their association. Third, the incidence rate of BARC 3 or 5 bleeding in this study was too low to produce powerful statistical results. Therefore, more large-scale studies should be conducted to further investigate the utility of the DAPT score in older PCI patients according to the BARC 3 or 5 bleeding endpoint. Fourth, because this was an observational cohort study, there may have been some confounding factors. Lastly, this study mainly focused on the older population, and research is required in the future to compare the utility of the DAPT score between younger and older PCI patients.
Conclusion
The present study evaluated the prognostic value of the DAPT score in older patients after PCI at a 5-year follow-up in the real world. The results indicated that the DAPT score could not discriminate the MACCE events in the older PCI patients; however, it had a certain predictive value for BARC 2, 3, or 5 bleeding in long-term follow-up, providing new insights into the application of the DAPT score in older PCI patients in the future.
Acknowledgements
We thank all staff contributing to this study.
Conflicts of Interest Statement
The authors have no conflicts of interest to declare.
Sources of Funding
This work was supported by the CAMS Innovation Fund for Medical Sciences (CIFMS) [2020-I2M-C&T-B-052]; the National Clinical Research Center for Cardiovascular Diseases, Fuwai Hospital, Chinese Academy of Medical Sciences (Grant No.NCRC2020013); Young and middle-aged talents in the XPCC Science and Technology Project (2020CB012); CS Optimizing Antithrombotic Research Fund (BJUHFCSOARF201801-06).
Data Availability Statement
Due to ethical restrictions related to the consent given by subjects at the time of study commencement, our datasets are available from the corresponding author upon reasonable request after permission of the Institutional Review Board of State Key Laboratory of Cardiovascular Disease, Fu Wai Hospital, National Center for Cardiovascular Diseases.
References
- 1).Zeymer U, Hochadel M, Karcher AK, Thiele H, Darius H, Behrens S, Schumacher B, Ince H, Hoffmeister HM, Werner N, Zahn R. Procedural Success Rates and Mortality in Elderly Patients With Percutaneous Coronary Intervention for Cardiogenic Shock. JACC Cardiovasc Interv, 2019; 12: 1853-1859 [DOI] [PubMed] [Google Scholar]
- 2).Rich MW, Chyun DA, Skolnick AH, Alexander KP, Forman DE, Kitzman DW, Maurer MS, McClurken JB, Resnick BM, Shen WK, Tirschwell DL. Knowledge Gaps in Cardiovascular Care of Older Adults: A Scientific Statement from the American Heart Association, American College of Cardiology, and American Geriatrics Society: Executive Summary. J Am Geriatr Soc, 2016; 64: 2185-2192 [DOI] [PubMed] [Google Scholar]
- 3).Li L, Geraghty OC, Mehta Z, Rothwell PM. Age-specific risks, severity, time course, and outcome of bleeding on long-term antiplatelet treatment after vascular events: a population-based cohort study. Lancet, 2017; 390: 490-499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4).Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, Granger CB, Lange RA, Mack MJ, Mauri L, Mehran R, Mukherjee D, Newby LK, O’Gara PT, Sabatine MS, Smith PK, Smith SC, Jr. 2016 ACC/AHA Guideline Focused Update on Duration of Dual Antiplatelet Therapy in Patients With Coronary Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol, 2016; 68: 1082-1115 [DOI] [PubMed] [Google Scholar]
- 5).Valgimigli M, Bueno H, Byrne RA, Collet JP, Costa F, Jeppsson A, Jüni P, Kastrati A, Kolh P, Mauri L, Montalescot G, Neumann FJ, Petricevic M, Roffi M, Steg PG, Windecker S, Zamorano JL, Levine GN. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J, 2018; 39: 213-260 [Google Scholar]
- 6).Brener SJ, Kirtane AJ, Rinaldi MJ, Stuckey TD, Witzenbichler B, Weisz G, Neumann FJ, Metzger DC, Henry TD, Cox DA, Duffy PL, Mazzaferri EL, Jr., Gurbel PA, Brodie BR, Mehran R, McAndrew T, Stone GW. Prediction of Ischemic and Bleeding Events Using the Dual Antiplatelet Therapy Score in an Unrestricted Percutaneous Coronary Intervention Population. Circ Cardiovasc Interv, 2018; 11: e006853 [DOI] [PubMed] [Google Scholar]
- 7).Veron-Esquivel D, Batiz-Armenta F, Cazares-Diazleal AC, Oviedo-Moguel S, Jarvio-Fernandez SM, Arce-Gonzalez JM, Ivey-Miranda JB. Validation of DAPT score for prolonged dual antiplatelet therapy in patients with acute myocardial infarction. Hellenic J Cardiol, 2019; 60: 296-302 [DOI] [PubMed] [Google Scholar]
- 8).Mauri L, Kereiakes DJ, Yeh RW, Driscoll-Shempp P, Cutlip DE, Steg PG, Normand SL, Braunwald E, Wiviott SD, Cohen DJ, Holmes DR, Jr., Krucoff MW, Hermiller J, Dauerman HL, Simon DI, Kandzari DE, Garratt KN, Lee DP, Pow TK, Ver Lee P, Rinaldi MJ, Massaro JM. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N Engl J Med, 2014; 371: 2155-2166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9).Yoshikawa Y, Shiomi H, Watanabe H, Natsuaki M, Kondo H, Tamura T, Nakagawa Y, Morimoto T, Kimura T. Validating Utility of Dual Antiplatelet Therapy Score in a Large Pooled Cohort From 3 Japanese Percutaneous Coronary Intervention Studies. Circulation, 2018; 137: 551-562 [DOI] [PubMed] [Google Scholar]
- 10).Piccolo R, Gargiulo G, Franzone A, Santucci A, Ariotti S, Baldo A, Tumscitz C, Moschovitis A, Windecker S, Valgimigli M. Use of the Dual-Antiplatelet Therapy Score to Guide Treatment Duration After Percutaneous Coronary Intervention. Ann Intern Med, 2017; 167: 17-25 [DOI] [PubMed] [Google Scholar]
- 11).Bittl JA. A Swing and a Miss for the DAPT Score. J Am Coll Cardiol, 2018; 72: 1079-1080 [DOI] [PubMed] [Google Scholar]
- 12).Yeh RW, Mihatov N. The DAPT Score Uncouples Bleeding and Ischemic Risk…Again. JACC: Cardiovascular Interventions, 2020; 13: 647-650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13).Yeh RW, Secemsky EA, Kereiakes DJ, Normand SL, Gershlick AH, Cohen DJ, Spertus JA, Steg PG, Cutlip DE, Rinaldi MJ, Camenzind E, Wijns W, Apruzzese PK, Song Y, Massaro JM, Mauri L. Development and Validation of a Prediction Rule for Benefit and Harm of Dual Antiplatelet Therapy Beyond 1 Year After Percutaneous Coronary Intervention. Jama, 2016; 315: 1735-1749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14).Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Thygesen K, Alpert JS, White HD, Jaffe AS, Katus HA, Apple FS, Lindahl B, Morrow DA, Chaitman BR, Clemmensen PM, Johanson P, Hod H, Underwood R, Bax JJ, Bonow JJ, Pinto F, Gibbons RJ, Fox KA, Atar D, Newby LK, Galvani M, Hamm CW, Uretsky BF, Steg PG, Wijns W, Bassand JP, Menasche P, Ravkilde J, Ohman EM, Antman EM, Wallentin LC, Armstrong PW, Simoons ML, Januzzi JL, Nieminen MS, Gheorghiade M, Filippatos G, Luepker RV, Fortmann SP, Rosamond WD, Levy D, Wood D, Smith SC, Hu D, Lopez-Sendon JL, Robertson RM, Weaver D, Tendera M, Bove AA, Parkhomenko AN, Vasilieva EJ, Mendis S, Bax JJ, Baumgartner H, Ceconi C, Dean V, Deaton C, Fagard R, Funck-Brentano C, Hasdai D, Hoes A, Kirchhof P, Knuuti J, Kolh P, McDonagh T, Moulin C, Popescu BA, Reiner Z, Sechtem U, Sirnes PA, Tendera M, Torbicki A, Vahanian A, Windecker S, Morais J, Aguiar C, Almahmeed W, Arnar DO, Barili F, Bloch KD, Bolger AF, Botker HE, Bozkurt B, Bugiardini R, Cannon C, de Lemos J, Eberli FR, Escobar E, Hlatky M, James S, Kern KB, Moliterno DJ, Mueller C, Neskovic AN, Pieske BM, Schulman SP, Storey RF, Taubert KA, Vranckx P, Wagner DR. Third universal definition of myocardial infarction. J Am Coll Cardiol, 2012; 60: 1581-1598 [Google Scholar]
- 15).Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, Kaul S, Wiviott SD, Menon V, Nikolsky E, Serebruany V, Valgimigli M, Vranckx P, Taggart D, Sabik JF, Cutlip DE, Krucoff MW, Ohman EM, Steg PG, White H. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation, 2011; 123: 2736-2747 [DOI] [PubMed] [Google Scholar]
- 16).Harada Y, Michel J, Lohaus R, Mayer K, Emmer R, Lahmann AL, Colleran R, Giacoppo D, Wolk A, Ten Berg JM, Neumann FJ, Han Y, Adriaenssens T, Tolg R, Seyfarth M, Maeng M, Zrenner B, Jacobshagen C, Wohrle J, Kufner S, Morath T, Ibrahim T, Bernlochner I, Fischer M, Schunkert H, Laugwitz KL, Mehilli J, Byrne RA, Kastrati A, Schulz-Schupke S. Validation of the DAPT score in patients randomized to 6 or 12 months clopidogrel after predominantly second-generation drug-eluting stents. Thromb Haemost, 2017; 117: 1989-1999 [DOI] [PubMed] [Google Scholar]
- 17).Andreotti F, Rocca B, Husted S, Ajjan RA, ten Berg J, Cattaneo M, Collet JP, De Caterina R, Fox KA, Halvorsen S, Huber K, Hylek EM, Lip GY, Montalescot G, Morais J, Patrono C, Verheugt FW, Wallentin L, Weiss TW, Storey RF. Antithrombotic therapy in the elderly: expert position paper of the European Society of Cardiology Working Group on Thrombosis. Eur Heart J, 2015; 36: 3238-3249 [DOI] [PubMed] [Google Scholar]
- 18).De Luca G, Dirksen MT, Spaulding C, Kelbæk H, Schalij M, Thuesen L, van der Hoeven B, Vink MA, Kaiser C, Musto C, Chechi T, Spaziani G, Diaz de la Llera LS, Pasceri V, Di Lorenzo E, Violini R, Suryapranata H, Stone GW. Impact of age on long-term outcome after primary angioplasty with bare-metal or drug-eluting stent (from the DESERT cooperation). Am J Cardiol, 2013; 112: 181-186 [DOI] [PubMed] [Google Scholar]
- 19).Lattuca B, Cayla G, Silvain J, Cuisset T, Leclercq F, Manzo-Silberman S, Saint-Etienne C, Delarche N, El Mahmoud R, Carrié D, Souteyrand G, Kerneis M, Hauguel-Moreau M, Zeitouni M, Guedeney P, Diallo A, Collet JP, Vicaut E, Montalescot G. Bleeding in the Elderly: Risk Factors and Impact on Clinical Outcomes After an Acute Coronary Syndrome, a Sub-study of the Randomized ANTARCTIC Trial. Am J Cardiovasc Drugs, 2021; 21: 681-691 [DOI] [PubMed] [Google Scholar]
- 20).Chichareon P, Modolo R, Kawashima H, Takahashi K, Kogame N, Chang CC, Tomaniak M, Ono M, Walsh S, Suryapranata H, Cotton J, Koning R, Akin I, Kukreja N, Wykrzykowska J, Piek JJ, Garg S, Hamm C, Steg PG, Juni P, Vranckx P, Valgimigli M, Windecker S, Onuma Y, Serruys PW. DAPT Score and the Impact of Ticagrelor Monotherapy During the Second Year After PCI. JACC Cardiovasc Interv, 2020; 13: 634-646 [DOI] [PubMed] [Google Scholar]
- 21).Ueda P, Jernberg T, James S, Alfredsson J, Erlinge D, Omerovic E, Persson J, Ravn-Fischer A, Tornvall P, Svennblad B, Varenhorst C. External Validation of the DAPT Score in a Nationwide Population. J Am Coll Cardiol, 2018; 72: 1069-1078 [DOI] [PubMed] [Google Scholar]
- 22).Van Calster B, Vickers AJ. Calibration of risk prediction models: impact on decision-analytic performance. Med Decis Making, 2015; 35: 162-169 [DOI] [PubMed] [Google Scholar]
- 23).Samuelsen PJ, Eggen AE, Steigen T, Wilsgaard T, Kristensen A, Skogsholm A, Holme E, van den Heuvel C, Nordrehaug JE, Bendz B, Nilsen DWT, Bønaa KH. Incidence and risk factors for major bleeding among patients undergoing percutaneous coronary intervention: Findings from the Norwegian Coronary Stent Trial (NORSTENT). PLoS One, 2021; 16: e0247358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24).Natsuaki M, Morimoto T, Yamaji K, Watanabe H, Yoshikawa Y, Shiomi H, Nakagawa Y, Furukawa Y, Kadota K, Ando K, Akasaka T, Hanaoka KI, Kozuma K, Tanabe K, Morino Y, Muramatsu T, Kimura T. Prediction of Thrombotic and Bleeding Events After Percutaneous Coronary Intervention: CREDO-Kyoto Thrombotic and Bleeding Risk Scores. J Am Heart Assoc, 2018; 7: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25).Levine GN, Jeong YH, Goto S, Anderson JL, Huo Y, Mega JL, Taubert K, Smith SC, Jr. Expert consensus document: World Heart Federation expert consensus statement on antiplatelet therapy in East Asian patients with ACS or undergoing PCI. Nat Rev Cardiol, 2014; 11: 597-606 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to ethical restrictions related to the consent given by subjects at the time of study commencement, our datasets are available from the corresponding author upon reasonable request after permission of the Institutional Review Board of State Key Laboratory of Cardiovascular Disease, Fu Wai Hospital, National Center for Cardiovascular Diseases.