Abstract
Telepharmacy is a practical part of telemedicine that refers to providing pharmaceutical services within the scope of the pharmacist's obligations while maintaining a temporal and spatial distance between patients, users of health services, and healthcare professionals. The present study was a cross-sectional study conducted among community pharmacists in Saudi Arabia between March and May 2022 to assess their knowledge, perceptions, and readiness for telepharmacy. The survey was filled out by 404 respondents. The majority of respondents were male (59.90%) and the age of more than half of them was between 30 and 39 years old (54.46%). Most participants worked in urban areas (83.66%), and 42.57% had less than five years of experience in a pharmacy. Most participants agreed that telepharmacy is available in Saudi Arabia (82.67%). Approximately 70% of pharmacists felt that telepharmacy promotes patient medication adherence, and 77.72% agreed that telepharmacy increases patient access to pharmaceuticals in rural areas. More than 72% of pharmacists said they would work on telepharmacy initiatives in rural areas for free, and 74.26% said they would work outside of usual working hours if necessary. In the future, this research could aid in adopting full-fledged telepharmacy pharmaceutical care services in Saudi Arabia. It could also help academic initiatives by allowing telepharmacy practice models to be included as a topic course in the curriculum to prepare future pharmacists to deliver telepharmacy services.
Keywords: Community pharmacists, Knowledge, Perceptions, Readiness, Telepharmacy
1. Introduction
The progress of medical treatments depends on proper and effective connections between healthcare providers and patients (Petropoulou et al., 2005, Rogers et al., 2017). With the growth of information technology and the rapid, easy access to a large quantity of data on the internet in recent decades, a new form of communication between healthcare practitioners and patients has emerged through a variety of technology-based healthcare services (Petropoulou et al., 2005, Rogers et al., 2017). Telemedicine is defined as the use of electronic communication to convey medical information from one location to another and to provide and support clinical care (Rogers et al., 2017, Kane-Gill and Rincon, 2019).
Telepharmacy is a practical part of telemedicine that refers to providing pharmaceutical services within the scope of the pharmacist's obligations while maintaining a temporal and spatial distance between patients, users of health services, and healthcare professionals (Kane-Gill and Rincon, 2019, Poudel and Nissen, 2016). The term “telepharmacy” refers to a type of pharmaceutical care in which pharmacists and patients are not physically present but can communicate via information and communication technologies (Baldoni et al., 2019). Drug selection, order review and distribution, patient counseling and monitoring, and clinical service provision are all examples of telepharmaceutical services (Win, 2017, Le et al., 2020).
Previous research has found that telepharmacy can improve the delivered healthcare. It can improve the quality of healthcare–pharmaceutical services, decrease healthcare–pharmaceutical errors, increase patients' access to healthcare–pharmaceutical services, enable recognition of unknown adverse effects of drugs, increase pharmacist, nurse, and physician satisfaction, reduce healthcare–pharmaceutical service costs, and improve pharmacist education (Gamus and Chodick, 2019, Peterson et al., 2007, Keeys et al., 2014).
Growing evidence suggests that telepharmacy and the implementation of such technology may reduce shortages and inequalities in the provision and delivery of healthcare services for patients living in rural communities or in areas where access to healthcare or pharmaceutical services is difficult (Omboni and Tenti, 2019, Kimber and Peterson, 2006, Margolis and Ypinazar, 2008, Strasser, 2003). It has long been common practice for community pharmacists to give patient care over the phone. However, utilizing Internet teleservices like messaging apps, smartphone apps, and online shopping has just become commonplace in recent years (Jirjees et al., 2022). Pharmacy practices quickly changed to include medication counseling, drug therapy monitoring, COVID-19 explanation and screening, and medicine home delivery for patients. These services have improved patients' lives and made it simpler for patients to contact pharmacists (Jirjees et al., 2022).
In Saudi Arabia, telepharmacy services are regulated by the Ministry of Health, which has issued regulations on the use of telepharmacy, which include requirements for the qualifications of pharmacists providing telepharmacy services, the confidentiality of patient information, and the need for a physical pharmacy location to support the telepharmacy service (2022, MOH). In the community setting, telepharmacy can help improve access to pharmacy services in remote or underserved areas. It can also provide more convenient access to pharmacy services for patients who may have difficulty traveling to a physical pharmacy location. In Saudi Arabia, there is a lack of data about the knowledge, beliefs, and readiness for telepharmacy among community pharmacists. Furthermore, there is a lack of study of the factors that affect their knowledge, beliefs, and readiness. As a result, this study aimed to analyze community pharmacists' knowledge, perceptions, and readiness for telepharmacy services in Saudi Arabia.
2. Methodology
2.1. Study design
This was a cross-sectional study conducted among community pharmacists in Saudi Arabia between March and May 2022 to assess their knowledge, perceptions, and readiness for telepharmacy.
2.2. Study sample
The study included pharmacists who worked in community pharmacies in Saudi Arabia, which was the fast-growing sector in the pharmaceutical industry. It was considered the country's largest employer of pharmacists, which received more attention from the government (Almaghaslah et al., 2018). The study did not include community pharmacists from other countries or pharmacists who worked in different settings. The subjects' participation was purely voluntary, and no monetary compensation was offered.
Sample Size Calculator by Raosoft, Inc. was used to determine the sample size. A 5% margin of error, 95% level of confidence, and 50% response distribution are used (Raosoft, 2004). The number of pharmacists in our poll should have been at least 377.
2.3. Data collection and analysis
An online survey was used to collect data from participants. The survey was utilized with the author's permission (Elnaem et al., 2022). The survey was available in English. Three pharmacy academics examined the content validity of the questionnaire after considering their experience and understanding of the study topic. Then, in order to eliminate any questions that were pointless or inadequate, we sent the questionnaire to a small group of pharmacists as a pilot test. After the validation, the final survey was reduced from 35 to 32 items (Cronbach's Alpha for the survey was 0.84).
The study survey included questions regarding community pharmacists' telepharmacy knowledge, telepharmacy attitudes, and telepharmacy preparedness, as well as items regarding their sociodemographic and employment statistics. The information was retrieved using an Excel spreadsheet, and the findings were displayed as numbers and percentages.
Regarding the knowledge, the correct answers were given 1 and the incorrect answers were given 0 after that we calculated the average knowledge scores. A knowledge score of less than 50% indicates poor knowledge, a score between 50% and 75% indicates moderate knowledge, and a score of more than 75% indicates good knowledge. Regarding the average perceptions and readiness scores, the responses were divided into two categories: strongly agree and agree, which received a score of 1, and neutral, disagree, and strongly disagree, which received a score of 0, after that, we calculated the average perceptions and readiness scores. A perception score of less than 50% indicates negative perception and a score of more than or equal to 50% indicates positive perception. A readiness score of 50% or more indicates good readiness and a score of less than 50% indicates poor readiness.
Statistical analyses were performed using SPSS Statistics 25. We conducted a Chi-Square test. The level of significance was set at a P value < 0.05. After that, univariate analysis was conducted to show the factors which are significantly and independently associated with the study outcomes. The variables with a P value < 0.2 in the univariate analysis were included in the logistic regression analysis.
3. Results
The survey was sent to 500 pharmacists. It was filled out by 404 respondents (the response rate was 80.8%). The majority of respondents were male (59.90%) and the age of more than half of them was between 30 and 39 years old (54.46%); their highest pharmacy degree was a bachelor's degree (57.18%), and they had completed their latest pharmacy degree or training from Saudi Arabia (82.92%) (Table 1).
Table 1.
Participants' sociodemographic characteristics (N = 404).
| Variable | Category | Number | Percentage |
|---|---|---|---|
| Gender | Male | 242 | 59.90 |
| Female | 162 | 40.10 | |
| Marital status | Married | 204 | 50.50 |
| Divorced | 72 | 17.82 | |
| Widowed | 17 | 4.21 | |
| Single | 111 | 27.47 | |
| Age | 20–29 | 88 | 21.78 |
| 30–39 | 220 | 54.46 | |
| 40–49 | 75 | 18.56 | |
| 50–59 | 21 | 5.20 | |
| Education level | Bachelor | 231 | 57.18 |
| Pharm.D. | 96 | 23.76 | |
| Master | 47 | 11.63 | |
| Doctorate (Ph.D.) | 13 | 3.22 | |
| Other* | 17 | 4.21 | |
| In which country have you earned your latest pharmacy degree or training? | Saudi Arabia | 335 | 82.92 |
| UK | 3 | 0.74 | |
| USA | 8 | 1.98 | |
| Malaysia | 1 | 0.25 | |
| Egypt | 36 | 8.91 | |
| India | 2 | 0.50 | |
| Yemen | 5 | 1.24 | |
| Other | 14 | 3.46 | |
| Nationality | Saudi Arabian | 342 | 84.65 |
| Non-Saudi Arabian | 62 | 15.35 |
Other degrees such as diploma.
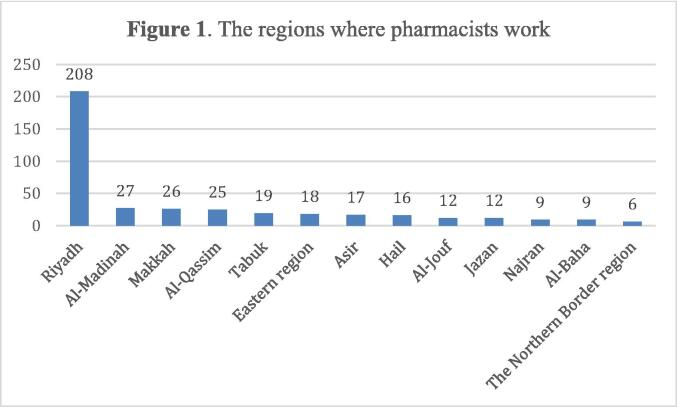
About 51.49% of the pharmacists were working in Riyadh city, 6.68% of them were working in Al-Madina city, and 6.44% of them were working in Makkah city (Fig. 1).
Fig. 1.
The regions where pharmacists work.
Most participants worked in urban areas (83.66%) and 42.57% had less than five years of experience in a pharmacy. Most respondents had previously provided pharmaceutical services through telepharmacy (76.73%). More than 66.34% of the respondents utilized the information from the Ministry of Health website and 53.22% of them used information from social media (Table 2).
Table 2.
Community pharmacist's employment characteristics (N = 404).
| Variable | Category | Number | Percentage |
|---|---|---|---|
| What is your area of Work? | Rural | 66 | 16.34 |
| Urban | 338 | 83.66 | |
| Years of experience in pharmacy | Less than 5 | 172 | 42.57 |
| 5–10 | 116 | 28.71 | |
| 11–15 | 103 | 25.50 | |
| More than 15 | 13 | 3.22 | |
| What is your job position at your community pharmacy? | Staff Pharmacist | 215 | 53.22 |
| Pharmacy supervisor | 91 | 22.52 | |
| Pharmacy Manager | 42 | 10.40 | |
| Other | 56 | 13.86 | |
| Have you previously provided pharmaceutical services through telepharmacy? | Yes | 310 | 76.73 |
| No | 94 | 23.27 | |
| Source of information | Local channels and international channels | 143 | 35.40 |
| Social media | 215 | 53.22 | |
| WHO website and social pages | 183 | 45.30 | |
| Scientific journals | 183 | 45.30 | |
| Ministry of Health (MOH) website | 268 | 66.34 | |
| Colleagues | 101 | 25.00 | |
| Others | 67 | 16.58 |
Participants showed excellent knowledge regarding telepharmacy in Saudi Arabia. Most participants agreed that telepharmacy is available in Saudi Arabia (82.67%), and 85.40% agreed that telepharmacy played a big role during the COVID-19 outbreak around the world. The majority of participants agreed that telepharmacy involved adverse drug reaction monitoring and reporting (83.67%) and that patients from rural areas could have more medication access and information via telepharmacy (80.94%) (Table 3).
Table 3.
Community pharmacist' telepharmacy knowledge (N = 404).
| Item | Response | Number | Percentage |
|---|---|---|---|
| Telepharmacy is available in Saudi Arabia | Yes | 334 | 82.67 |
| No | 20 | 4.95 | |
| Do not know | 50 | 12.38 | |
| Information Communication Technology (ICT) knowledge is important for pharmacists in how to conduct telepharmacy. | Yes | 344 | 85.15 |
| No | 25 | 6.19 | |
| Do not know | 35 | 8.66 | |
| Telepharmacy played a big role during the COVID-19 outbreak around the world. | Yes | 345 | 85.40 |
| No | 22 | 5.44 | |
| Do not know | 37 | 9.16 | |
| Telepharmacy does require a strong internet connection or high-performance technology. | Yes | 276 | 68.32 |
| No | 92 | 22.77 | |
| Do not know | 36 | 8.91 | |
| Telepharmacy provides better counseling in terms of privacy and length of the session. | Yes | 346 | 85.64 |
| No | 25 | 6.19 | |
| Do not know | 33 | 8.17 | |
| Telepharmacy is also involved in Adverse Drug Reaction monitoring and reporting. | Yes | 338 | 83.67 |
| No | 27 | 6.68 | |
| Do not know | 39 | 9.65 | |
| Patients from rural areas can have more medication access and information via telepharmacy. | Yes | 327 | 80.94 |
| No | 38 | 9.41 | |
| Do not know | 39 | 9.65 |
Approximately 70% of pharmacists felt that telepharmacy promotes patient medication adherence, and 77.72% agreed that telepharmacy increases patient access to pharmaceuticals in rural areas. Approximately 84.4% of participants believed that telepharmacy saves patients money and time traveling to healthcare institutions, and 82.43% agreed that patient consultation via telepharmacy is effective. In addition, 83.41% of participants believed that pharmacy schools should include education programs on computers, information technology, and telepharmacy to aid in future telepharmacy use, and 73.76% thought that telepharmacy helps to minimize pharmacists' shortages (Table 4).
Table 4.
Community pharmacist' telepharmacy perceptions (N = 404).
| Items |
Frequency n (%) |
||||
|---|---|---|---|---|---|
| Strongly Disagree | Disagree | Unsure | Agree | Strongly Agree | |
| Telepharmacy improves patient's adherence to the medication | 16 (3.96) |
27 (6.68) |
80 (19.80) |
268 (66.34) |
13 (3.22) |
| Telepharmacy has a higher error rate for medication dispensing and filling compared to traditional pharmacy | 18 (4.45) |
133 (32.92) |
93 (23.02) |
149 (36.88) |
11 (2.72) |
| Telepharmacy enhances patient's access to medications in rural areas | 8 (1.98) |
20 (4.95) |
62 (15.35) |
296 (73.27) |
18 (4.45) |
| Telepharmacy provides a complete privacy setting during the consultation period | 8 (1.98) |
19 (4.70) |
53 (13.12) |
293 (72.52) |
31 (7.67) |
| Telepharmacy increases pharmacist's workload and commitment | 10 (2.48) |
78 (19.31) |
73 (18.07) |
220 (54.45) |
23 (5.69) |
| Telepharmacy helps patients save their money and travel time to reach the healthcare facilities | 7 (1.73) |
11 (2.72) |
45 (11.14) |
307 (75.99) |
34 (8.41) |
| I am willing to share my personal information on the online database when using telepharmacy services | 6 (1.49) |
22 (5.44) |
84 (20.79) |
274 (67.82) |
18 (4.45) |
| Telepharmacy minimizes the cost to establish a pharmaceutical business in comparison to the regular pharmacy | 9 (2.23) |
12 (2.97) |
68 (16.83) |
295 (73.02) |
20 (4.95) |
| Patient consultation via telepharmacy is effective | 7 (1.73) |
15 (3.71) |
49 (12.13) |
305 (75.50) |
28 (6.93) |
| Pharmacy schools should provide education programs on computers, IT, and telepharmacy to assist in the future utilization of telepharmacy | 5 (1.24) |
10 (2.48) |
52 (12.87) |
303 (75.00) |
34 (8.41) |
| Therapeutic drug monitoring via telepharmacy in rural areas is easily monitored | 5 (1.24) |
19 (4.70) |
84 (20.79) |
278 (68.81) |
18 (4.45) |
| Security is a greater concern in a remote site telepharmacy than in a traditional community pharmacy | 6 (1.49) |
36 (8.91) |
58 (14.36) |
277 (68.56) |
27 (6.68) |
| telepharmacy helps to minimize the shortage of pharmacists | 14 (3.46) |
25 (6.19) |
67 (16.58) |
282 (69.80) |
16 (3.96) |
More than 72% of pharmacists stated that they are willing to work on telepharmacy projects in remote regions even if they are not paid, and 74.26% said that they are willing to work outside of normal working hours if necessary. Approximately 79% of pharmacists agreed that they are prepared to provide medication counseling via two-way video consultation, such as phone calls, text messages, or voice calls using mobile devices. Furthermore, 81.68% of pharmacists claimed that they are prepared to tackle telepharmacy deployment in community pharmacies. About 83.17% of pharmacists indicated that they are ready to use telepharmacy to improve and reduce the risk of medication errors among patients, and 83.17% said that they are ready to use telepharmacy to conduct medication reconciliation (Table 5).
Table 5.
Telepharmacy readiness among pharmacists (n = 404).
| Items |
Frequency n (%) |
||||
|---|---|---|---|---|---|
| Strongly Disagree | Disagree | Unsure | Agree | Strongly Agree | |
| I am ready to work on telepharmacy projects in rural areas, even without an incentive. | 9 (2.23) |
20 (4.95) |
84 (20.79) |
276 (68.32) |
15 (3.71) |
| I am ready to work after office hours if needed. | 12 (2.97) |
32 (7.92) |
60 (14.85) |
284 (70.30) |
16 (3.96) |
| I am ready to conduct drug counseling via two-way video consultations such as telephone calls, text messages, or voice calls through mobile applications. | 6 (1.49) |
16 (3.96) |
63 (15.59) |
301 (74.50) |
18 (4.45) |
| I am ready to teach patients how to use their drug delivery device (e.g., inhaler, insulin pen) properly through video consultation. | 6 (1.49) |
13 (3.22) |
48 (11.88) |
314 (77.72) |
23 (5.69) |
| I am ready to undergo training in ethics and legal issues related to telepharmacy | 2 (0.50) |
9 (2.23) |
49 (12.13) |
314 (77.72) |
30 (7.42) |
| I am ready to face the implementation of telepharmacy in community pharmacies | 8 (1.98) |
12 (2.97) |
54 (13.37) |
305 (75.49) |
25 (6.19) |
| I am ready to conduct Home Medication Review through telepharmacy | 4 (0.99) |
12 (2.97) |
55 (13.61) |
306 (75.74) |
27 (6.68) |
| I am ready to improve and reduce the risk of medication errors among patients through telepharmacy. | 5 (1.24) |
16 (3.96) |
47 (11.63) |
308 (76.24) |
28 (6.93) |
| I am ready to carry the increment of workload when conducting telepharmacy. | 2 (0.50) |
16 (3.96) |
53 (13.12) |
310 (76.73) |
23 (5.69) |
| I am ready to conduct medication reconciliation via telepharmacy services. | 5 (1.24) |
17 (4.20) |
46 (11.39) |
315 (77.97) |
21 (5.20) |
| I am ready to perform remote prescription checking before dispensing drugs from an automated medication dispensing cabinet. | 4 (0.99) |
15 (3.71) |
53 (13.12) |
313 (77.48) |
19 (4.70) |
| I am ready to use mobile applications and the Internet to receive refill orders from patients and transfer prescriptions. | 7 (1.73) |
15 (3.71) |
60 (14.85) |
307 (75.99) |
15 (3.71) |
The association between pharmacists' knowledge scores and their personal data is shown in Table 6. Univariate analysis was conducted to show the factors which are significantly and independently associated with the study outcomes. The variables with a P value < 0.2 in the univariate analysis including experience, gender, age, education level, and area of work were entered in the logistic regression analysis. The analysis showed that female gender (P value 0.003) and having a bachelor’s degree (P value 0.046) were linked with higher knowledge scores.
Table 6.
Logistic regression analysis of pharmacists' knowledge scores and personal data.
| Variable | Category | Knowledge average score | P value |
|---|---|---|---|
| Years of experience | Less than 5 | 0.76 | 0.300 |
| 5–10 | 0.89 | ||
| 11–15 | 0.84 | ||
| More than 15 | 0.76 | ||
| Gender | Male | 0.81 | 0.003 |
| Female | 0.83 | ||
| Age | 20–29 | 0.76 | 0.565 |
| 30–39 | 0.82 | ||
| 40–49 | 0.88 | ||
| 50–59 | 0.84 | ||
| Education level | Bachelor | 0.83 | 0.046 |
| Pharm.D. | 0.81 | ||
| Master | 0.77 | ||
| Doctorate (Ph.D.) | 0.80 | ||
| Other | 0.87 | ||
| Area of work | Rural | 0.76 | 0.557 |
| Urban | 0.83 |
The association between pharmacists' perception scores and their personal data is shown in Table 7. The variables with a P value < 0.2 in the univariate analysis including experience, gender, age, education level, and area of work were entered in the logistic regression analysis. Female gender (P value 0.000) and increased age (P value 0.03) were linked to higher perception scores.
Table 7.
Logistic regression analysis of pharmacists' perception scores and personal data.
| Variable | Category | Perceptions average score | P value |
|---|---|---|---|
| Years of experience | Less than 5 | 0.69 | 0.512 |
| 5–10 | 0.75 | ||
| 11–15 | 0.77 | ||
| More than 15 | 0.73 | ||
| Gender | Male | 0.69 | 0.000 |
| Female | 0.79 | ||
| Age | 20–29 | 0.68 | 0.030 |
| 30–39 | 0.72 | ||
| 40–49 | 0.79 | ||
| 50–59 | 0.82 | ||
| Education level | Bachelor | 0.72 | 0.538 |
| Pharm.D. | 0.70 | ||
| Master | 0.75 | ||
| Doctorate (Ph.D.) | 0.82 | ||
| Other* | 0.86 | ||
| Job position | Staff pharmacist | 0.74 | 0.330 |
| Pharmacy supervisor | 0.67 | ||
| Pharmacy Manager | 0.67 | ||
| Other | 0.82 |
The association between pharmacists' readiness scores and their personal data is shown in Table 8. The variables with a P value < 0.2 in the univariate analysis including experience, gender, education level, and area of work were entered in the logistic regression analysis. Female gender (P value 0.003) and having a bachelor’s degree (P value 0.046) were linked to higher readiness scores.
Table 8.
Logistic regression analysis of pharmacists' readiness scores and personal data.
| Variable | Category | Readiness average score | P value |
|---|---|---|---|
| Years of experience | Less than 5 | 0.76 | 0.300 |
| 5–10 | 0.86 | ||
| 11–15 | 0.83 | ||
| More than 15 | 0.76 | ||
| Gender | Male | 0.77 | 0.003 |
| Female | 0.86 | ||
| Education level | Bachelor | 0.84 | 0.046 |
| Pharm.D. | 0.73 | ||
| Master | 0.77 | ||
| Doctorate (Ph.D.) | 0.77 | ||
| Other* | 0.91 | ||
| Job position | Staff pharmacist | 0.83 | 0.676 |
| Pharmacy supervisor | 0.75 | ||
| Pharmacy Manager | 0.74 | ||
| Other | 0.85 |
4. Discussion
The present study showed that community pharmacists in Saudi Arabia had a very good knowledge about telepharmacy. Most pharmacists believed that telepharmacy played a significant role during the COVID-19 outbreak and agreed that telepharmacy is available in Saudi Arabia. In contrast, Elnaem et al. reported that there was some variation and uncertainty in responses about the availability of telepharmacy in Malaysia, which could be explained by the fact that it has not yet been fully developed and made widely available (Elnaem et al., 2022).
According to the majority of pharmacists in this study, telepharmacy can provide patients in remote areas with greater drug access and information. Indeed, many healthcare practitioners use telepharmacy services to increase patient access to pharmaceutical care services such as medication counseling, especially during the COVID-19 time (Ibrahim et al., 2023). Similar to the results of the present study, Poudel and Nissen reported that most pharmacists believed that telepharmacy delivers clinical benefits for those in rural regions (Poudel and Nissen, 2016).
Telepharmacy enables patients to avoid driving long distances, losing time at work, and waiting in a clinic with other sick people while getting themselves and their families well (Ahmed et al., 2023). Most pharmacists in the current study stated that telepharmacy saves patients money and time by eliminating the need for them to visit healthcare facilities. Previous research has demonstrated that telepharmacy reduces travel expenses and saves time and facilitates access to healthcare services (Poudel and Nissen, 2016, Win, 2017, Traynor, 2013). More than 91% of the pharmacists who took part in Alanazi et al.'s study believed that employing a telepharmacy system may save time and money (Alanazi et al., 2021). Elnaem et al. reported that the beneficial effect of telepharmacy in saving patients' resources was regarded positively by study participants, with 91% agreement (Elnaem et al., 2022). Nevertheless, the population in Elnaem et al study is pharmacy students, not healthcare professionals.
The present study showed that community pharmacists in Saudi Arabia had positive attitudes toward telepharmacy. Because of the small number of pharmacies in rural areas, and fewer clinical pharmacy services, it is more challenging for people to fill prescriptions, get access to other essential services, and there is an increased risk of prescription errors in such areas (Ahmed et al., 2023). According to the current survey, most community pharmacists believe that telepharmacy helps reduce pharmacist shortages. Previous research has shown that telepharmacy can help alleviate shortages in healthcare services provision and delivery for patients living in rural areas or in locations where access to healthcare or pharmaceutical services is difficult for any reason (Kimber and Peterson, 2006, Margolis and Ypinazar, 2008, Strasser, 2003). Telepharmacy, according to Baldoni et al., is a solution to the pharmacy manpower deficit in which pharmaceutical services are delivered remotely (Baldoni et al., 2019). Furthermore, 75% of the respondents in Elnaem et al.'s study agreed that telepharmacy might help reduce the current shortage of pharmacists (Elnaem et al. 2022).
The present study showed that community pharmacists in Saudi Arabia demonstrated readiness to implement telepharmacy services in their future pharmacy practice. Most pharmacists in the current study responded that they would be willing to work on telepharmacy projects in remote areas even if they were not paid and that they would work outside of regular working hours if necessary. One such motivation is a desire to aid those in need who live in areas with inadequate access to medical services. Additionally, they may seek for tough and varied job environments because they provide opportunities to learn and grow. In contrast, Elnaem et al. stated that the lack of incentives and an excessive workload related to poorer readiness among participants regarding telepharmacy readiness (Elnaem et al. 2022). Ameri et al. stated that payment and reimbursement concerns and a lack of access to information technology infrastructure were among the most significant impediments (Ameri et al., 2020). According to Omran et al., the main challenges to telepharmacy practice include a lack of professional training, ethical issues, and a formal practice framework (Omran et al., 2021).
The present study showed that female gender was linked with higher knowledge scores. This may be because females tend to be more receptive to new technologies and are more likely to embrace change. In contrast to that, Tegegne et al reported that being male was found to be significantly associated with knowledge of telepharamcy but the population in their study is pharmacy students, not healthcare professionals (Tegegne et al., 2023). The present study showed also that having a bachelor’s degree was associated with higher knowledge scores. Tjiptoatmadja and Alfian have reported a significant association between education and knowledge of participants about telepharmacy services (Tjiptoatmadja and Alfian, 2023). Furthermore, Alboraie et al stated that highly qualified individuals have more awareness of telemedicine services (Alboraie et al., 2021). Nonetheless, the population in Alboraie et al study and Tjiptoatmadja and Alfian's study are the general public.
The present study showed that female gender and increased age were linked to higher perception scores. This may be because older pharmacists and women tend to have more experience in the field and have witnessed the evolution of pharmacy practice over time. In contrast to that, Alnajrani et al. stated that there was no association between demographic characteristics (such as age, gender, and education) and the participants' perception of telepharmacy services (Alnajrani et al., 2022), but the sample population in their study is the general public not healthcare professionals.
The present study showed that female gender and having a bachelor’s degree were linked to higher readiness scores. Having a bachelor's degree may indicate that these pharmacists have had more formal education and training, which could increase their readiness to adopt new technologies like telepharmacy. Females may also be more likely to seek out educational opportunities and stay updated with new technologies. A previous study looked into how community pharmacists feel about electronic prescriptions revealed that demographic factors like age and gender played a large role in shaping their perspectives and eventual adoption of the practice. Male pharmacists were shown to have more favorable attitudes towards and more uptake of e-prescribing than their female counterparts. Younger pharmacists, on the other hand, were more open to and quick to accept this technology (Clauson et al., 2011).
Both community and hospital pharmacists can benefit from telepharmacy readiness as it allows them to provide more efficient and effective patient care. The pharmacists who worked in community pharmacies lack professional training and lack access to information technology infrastructure in comparison with pharmacists who worked in hospital pharmacies. Dat et al reported that the readiness of hospital pharmacists was more than the readiness of community pharmacists (91.7% vs 82.7%, P value 0.006) (Dat et al., 2022). Community pharmacies should provide pharmacists with the required workshops and provide them with comprehensive training materials. Continuing professional education is an effective way to broaden knowledge and foster a favorable attitude toward community telepharmacy.
5. Limitations
The study's main limitation is the small sample size with few representations of pharmacists from rural areas; therefore, the findings' generalizability is uncertain. The use of an online survey further raises the possibility of selection bias in the research. Nonetheless, this research offers vital information on pharmacists' knowledge, preparedness, and perceptions of telepharmacy, which is presently not fully explored among community pharmacists in Saudi Arabia. Hence, results may help in designing and implementing telepharmacy services in such setting.
6. Conclusion
The study's results showed that telepharmacy services are well accepted and ready to be used in the community setting. However, it is necessary to develop training programs to improve pharmacists' knowledge and proficiency in telepharmacy among community pharmacists. Future research in this area may help to advance our understanding of the telepharmacy functions that are appropriate for community pharmacy practice and, in turn, direct the creation of efficient ways to integrate telepharmacy services into routine care delivery.
Ethical approval
The study was approved by the Research Ethics Committee/Health and Science Disciplines at Prince Sattam bin Abdulaziz University with an approval number REC-HSD-134-2022.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
This study is supported via funding from Prince Sattam bin Abdulaziz University project number (PSAU/2023/R/1444).
Footnotes
Peer review under responsibility of King Saud University.
References
- Ahmed N.J., Almalki Z.S., Alsawadi A.H., Alturki A.A., Bakarman A.H., Almuaddi A.M., Alshahrani S.M., Alanazi M.B., Alshehri A.M., Albassam A.A., Alahmari A.K., Alem G.M., Aldosari S.A., Alamer A.A. Knowledge, perceptions, and readiness of telepharmacy among hospital pharmacists in Saudi Arabia. Healthcare. 2023;11:1087. doi: 10.3390/healthcare11081087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alanazi A., Albarrak A., Alanazi A., Muawad R. 5PSQ-184 Knowledge and attitude assessment of pharmacists toward telepharmacy in Riyadh City, Saudi Arabia. Eur. J. Hosp. Pharm. 2021;28:A146. doi: 10.1136/ejhpharm-2021-eahpconf.303. [DOI] [Google Scholar]
- Alboraie M., Allam M.A., Youssef N., Abdalgaber M., El-Raey F., Abdeen N., Mahdy R.E., Elshaarawy O., Elgebaly A., Haydara T., Abd-Elsalam S., Nassar Y.A., Shabana H., Zaky S. Knowledge, applicability, and barriers of telemedicine in Egypt: a national survey. Int. J. Telemed. Appl. 2021;2021:5565652. doi: 10.1155/2021/5565652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almaghaslah D., Alsayari A., Asiri R., Albugami N. Pharmacy workforce in Saudi Arabia: challenges and opportunities: a cross-sectional study. Int. J. Health. Plann. Manage. 2018;34:e583–e593. doi: 10.1002/hpm.2674. [DOI] [PubMed] [Google Scholar]
- Alnajrani R.H., Alnajrani N.R., Aldakheel F.S., Alhmoud F.Y., Al-Makenzi H.A., Zahrani H.Y., Lubbad H.A., Alajami H.N. An assessment of the knowledge, perception, and willingness to use telepharmacy services among the general public in the Kingdom of Saudi Arabia. Cureus. 2022;14:e31769. doi: 10.7759/cureus.31769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ameri A., Salmanizadeh F., Keshvardoost S., Bahaadinbeigy K. Investigating pharmacists’ views on telepharmacy: prioritizing key relationships, barriers, and benefits. J. Pharm. Technol. 2020;36:171–178. doi: 10.1177/8755122520931442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldoni S., Amenta F., Ricci G. Telepharmacy services: present status and future perspectives: a review. Medicina. 2019;55:327. doi: 10.3390/medicina55070327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clauson K.A., Alkhateeb F.M., Lugo K.D., Khanfar N.M. E-prescribing: attitudes and perceptions of community pharmacists in Puerto Rico. Int. J. Electronic Healthcare. 2011;6:34–46. doi: 10.1111/ijcp.14209. [DOI] [PubMed] [Google Scholar]
- Dat T.V., Tran T.D., My N.T., Nguyen T.T.H., Quang N.N.A., Tra Vo Nguyen M., Hong Ngoc Vo P., Ho T.T., Manh Nguyen C., Thi Ngoc Nguyen T., Lac-Thuy N.H. Pharmacists’ perspectives on the use of telepharmacy in response to COVID-19 pandemic in ho chi Minh city, Vietnam. J. Pharm. Technol. 2022;38:106–114. doi: 10.1177/87551225221076327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elnaem M.H., Akkawi M.E., Al-Shami A.K., Elkalmi R. Telepharmacy knowledge, perceptions, and readiness among future malaysian pharmacists amid the COVID-19 pandemic. Indian. J. Pharm. Educ. Res. 2022;56:9–16. [Google Scholar]
- Gamus A., Chodick G. Costs and benefits of telemedicine compared to face-to-face treatment in patients with lower extremity ulcers. Adv. Wound. Care. 2019;8:291–297. doi: 10.1089/wound.2018.0906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibrahim O.M., Ibrahim R.M., Al Meslamani A.Z., Al Mazrouei N. Role of telepharmacy in pharmacist counselling to coronavirus disease 2019 patients and medication dispensing errors. J. Telemed. Telecare. 2023;29:18–27. doi: 10.1177/1357633X20964347. [DOI] [PubMed] [Google Scholar]
- Jirjees F., Odeh M., Aloum L., Kharaba Z., Alzoubi K.H., Obaidi H.A. The rise of telepharmacy services during the COVID-19 pandemic: a comprehensive assessment of services in the United Arab Emirates. Pharm Pract. 2022;20:2634. doi: 10.18549/PharmPract.2022.2.2634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane-Gill S.L., Rincon F. Expansion of telemedicine services: telepharmacy, telestroke, teledialysis, tele-emergency medicine. Crit. Care. Clin. 2019;35:519–533. doi: 10.1016/j.ccc.2019.02.007. [DOI] [PubMed] [Google Scholar]
- Keeys C., Kalejaiye B., Skinner M., Eimen M., Neufer J., Sidbury G., Buster N., Vincent J. Pharmacist-managed inpatient discharge medication reconciliation: a combined onsite and telepharmacy model. Am. J. Hosp. Pharm. 2014;71:2159–2166. doi: 10.2146/ajhp130650. [DOI] [PubMed] [Google Scholar]
- Kimber M.B., Peterson G.M. Telepharmacy—enabling technology to provide quality pharmacy services in rural and remote communities. J. Pharm. Pract. Res. 2006;36:128–133. [Google Scholar]
- Le T., Toscani M., Colaizzi J. Telepharmacy: a new paradigm for our profession. J. Pharm. Pract. 2020;33:176–182. doi: 10.1177/0897190018791060. [DOI] [PubMed] [Google Scholar]
- Margolis S.A., Ypinazar V.A. Tele-pharmacy in remote medical practice: the Royal Flying Doctor Service Medical Chest Program. Rural. Remote. Heal. 2008;8:937. (PMID: 18489239) [PubMed] [Google Scholar]
- Omboni S., Tenti M. Telepharmacy for the management of cardiovascular patients in the community. Trends. Cardiovasc. Med. 2019;29:109–117. doi: 10.1016/j.tcm.2018.07.002. [DOI] [PubMed] [Google Scholar]
- Omran S., Elnaem M.H., Ellabany N. Telepharmacy knowledge, attitude and practice among egyptian pharmacists amid the COVID-19 pandemic. J. Am. Coll. Clin. Pharm. 2021;4:1643. [Google Scholar]
- Peterson C.D., Rathke A., Skwiera J., Anderson H.C., Jr. Hospital telepharmacy network: delivering pharmacy services to rural hospitals. J. Pharm. Technol. 2007;23:58–165. doi: 10.1177/875512250702300305. [DOI] [Google Scholar]
- Petropoulou, S.G., Bekakos, M.P., Gravvanis, G.A., 2005. E-prescribing— telepharmacy. In: Paper presented at: 7th Hellenic European Conference on Computers; Athens, Greece.
- Poudel A., Nissen L.M. Tele-pharmacy: a pharmacist’s perspective on the clinical benefits and challenges. Integr. Pharm. Res. Pract. 2016;5:75–82. doi: 10.2147/IPRP.S101685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raosoft, 2004. Raosoft Sample Size Calculator. Raosoft, Inc., Seattle. Available at: http://www.raosoft.com/samplesize.html
- Rogers H., Madathil K.C., Agnisarman S., Narasimha S., Ashok A., Nair A., Welch B.M., McElligott J.T. A systematic review of the implementation challenges of telemedicine systems in ambulances. Telemed. J. E. Health. 2017;23:707–717. doi: 10.1089/tmj.2016.0248. [DOI] [PubMed] [Google Scholar]
- Strasser R. Rural health around the world: challenges and solutions. Fam. Pract. 2003;20:457–463. doi: 10.1093/fampra/cmg422. [DOI] [PubMed] [Google Scholar]
- Tegegne M.D., Wubante S.M., Melaku M.S., Mengiste N.D., Fentahun A., Zemene W., Zeleke T., Walle A.D., Lakew G.T., Tareke Y.T., Abdi M.S., Alemayehu H.M., Girma E.M., Tilahun G.G., Demsash A.W., Dessie H.S. Tele-pharmacy perception, knowledge and associated factors among pharmacy students in northwest Ethiopia: an input for implementers. BMC Med Educ. 2023;23:130. doi: 10.1186/s12909-023-04111-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tjiptoatmadja N.N., Alfian S.D. Knowledge, perception, and willingness to use telepharmacy among the general population in Indonesia. Front Public Health. 2023;10(825554):2022. doi: 10.3389/fpubh.2022.825554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Traynor K. Telepharmacy services bring new patient care opportunities. Am. J. Health. Syst. Pharm. 2013;70:565–566. doi: 10.2146/news130025. [DOI] [PubMed] [Google Scholar]
- Win A.Z. Telepharmacy: time to pick up the line. Res. Social. Adm. Pharm. 2017;13:882–883. doi: 10.1016/j.sapharm.2015.06.002. [DOI] [PubMed] [Google Scholar]