Abstract
Triceps tendon avulsion is a rare but debilitating condition and the least frequent of all tendon injuries, but it is receiving increasing attention in the literature. The most common mechanism of injury is resisted extension, which is typically seen in a fall onto an extended hand. Such injuries are easily overlooked and should be considered a differential diagnosis in all patients who describe pain and swelling at the posterior aspect of the elbow following a traumatic event. Non-operative management is the general principle for partial rupture as opposed to a variety of surgical treatments for a complete avulsion. The goal of this meta-analysis is to analyse the current literature on triceps avulsion and provide a detailed overview of the occurrence, diagnosis, treatment options and outcomes, comparison of various repair techniques, and consequences of this injury.
Keywords: isolated rupture, cohort studies, suture techniques, meta-analysis, distal triceps repair, triceps avulsion
Introduction and background
Rupture or avulsion of the triceps tendon was first reported by Partridge in 1868 [1]. This uncommon injury accounted for fewer than 0.8% of all upper limb tendon injuries and 2% of all tendon injuries as reported by Anzel et al. in a study of 1014 tendon and muscle injury cases over nine years [2]. These injuries are more prevalent in those aged 30 to 50 with a mean age of 36 years [3,4]. Triceps avulsion occurs when force is supplied to a contracting muscle in conjunction with deceleration-type impact, overloading the tendon eccentrically [4]. A partial or full rupture can occur as an isolated event or with accompanying fractures. The most frequent site of rupture is the osseo-tendinous insertion of the triceps, but reports of rupture within or in the centre of the musculo-tendinous junction have also been reported [5]. A partial tear is characterised by weakness and reduced extension of the elbow against gravity but not to resistance. This is a result of the anconeus muscle compensating against resistance or secondary to an intact lateral head of the triceps tendon. A complete rupture, on the other hand, usually manifests itself by the inability to extend the elbow against resistance. As a result, a triceps tear diagnosis can be difficult, and a research found that nearly 50% of acute triceps ruptures had been misdiagnosed at the first presentation [4]. Despite being uncommon in clinical practice, blunt trauma that causes triceps tendon rupture has been described in the literature [6]. Complete ruptures or tears involving more than 50% of the tendon are indications requiring surgical intervention [7]. There have been reports of treating triceps tendon avulsion using a variety of surgical techniques, including repair with sutures through the transosseous tunnel or suture anchors. Despite these injuries, the available literature on their treatment and management is sparse and inconsistent in its findings; therefore standard surgical care is yet to be developed. As a result, all available information on these injuries must be gathered and assessed in a meta-analysis to offer a better understanding of the injury and treatment recommendations.
Review
Methodology and search strategy
The Cochrane collaboration standards were followed for this systematic review and meta-analysis report, and the results were reported in accordance with the PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analysis) recommendations [8]. An exhaustive literature search was carried out of the online databases between 1990 and 2022 for isolated triceps tendon avulsion. The search was performed in the English language, and a narrative study design was implemented in this research, as shown in Tables 1, 2.
Table 1. Search design, eligibility criteria, and methodology.
| ITEMS | SPECIFICATION |
| Databases | PubMed, MEDLINE, EMBASE, and Cochrane Library |
| Time frame | 1990-2022 |
| Inclusion criteria | Research that focused on adults isolated triceps tendon avulsions or injuries. Only studies written in English were included in the search. |
| Exclusion criteria | Studies examining the avulsion of tendons in connection with fractures as well as those involving injuries to children, animals, or cadavers were excluded from consideration. The research design did not include letters to the editor or case reports. |
| Selection process | Data from the studies and research design including sample size, patient characteristics, interventions, outcome measures, and outcomes, were independently retrieved by four reviewers. The Newcastle-Ottawa Scale (NOS) [9] was used to evaluate the quality of the included research, and any disagreements were resolved through discussion and consensus. |
| Statistical Methods and Analysis | We used Review Manager (RevMan) version 5.4.1 to perform the meta-analysis. |
Table 2. Strategy for searching the database.
| Search Terms | Strategy |
| Triceps Tendon Rupture, Triceps tendon Avulsion, Isolated Triceps avulsion rupture, Triceps tendon injury | PubMed, MEDLINE, EMBASE, Cochrane Text availability: Abstract, full text. Article type: Systemic review including meta-analysis, Meta-analysis, Randomized controlled trial, retrospective studies. Publication date: Articles between 1990-2022 |
Results
Study Characteristics and Data Synthesis
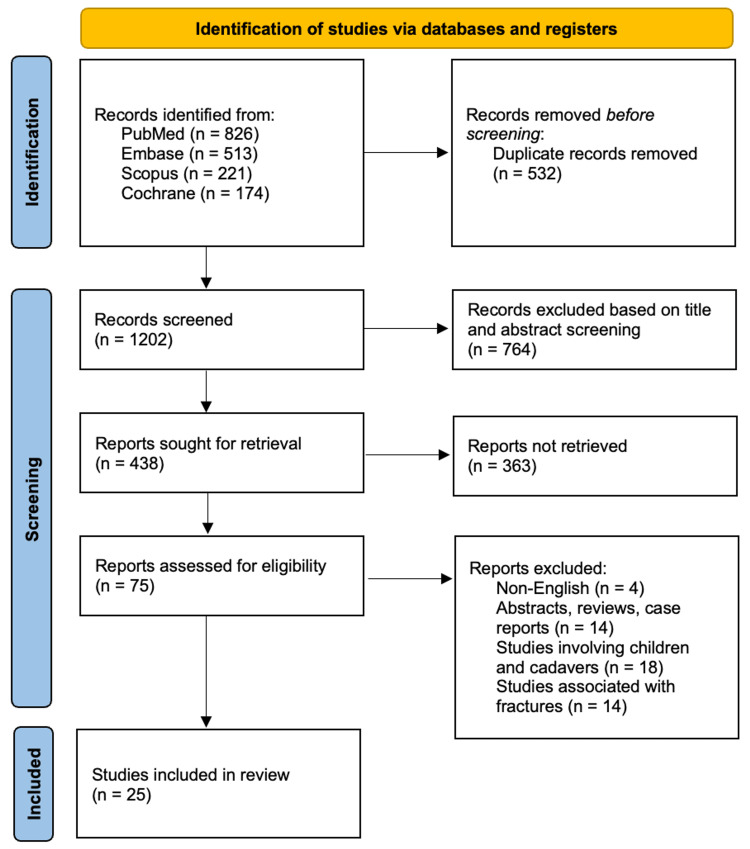
The exhaustive literature search through the above-mentioned database in Table 2 yielded 1734 articles related to the study. A detailed screening process of the 1734 articles led to the exclusion of 532 duplicates. The other 1202 articles then had their titles and abstracts screened, of which only 438 met the screening criteria. Of the remaining 438 articles, 363 were not retrieved, and the other 75 articles were assessed using the eligibility criteria. This assessment led to the inclusion of 25 articles that met the requirements for analysis. The study selection results are presented in the PRISMA flow diagram (Figure 1). Characteristics of included studies are presented below (Table 3).
Table 3. Summary of various studies involved in the analysis, different interventions, and outcomes of interest.
| Study Type | Number of studies included | Sample Size | Mean Age | Most Common Injury Types | Intervention Type |
| Randomized Controlled Trials | 12 | 2,586 | 48 years (18-85 years) | Triceps Tendon Avulsion (n=12 studies), Olecranon Fracture (n=6 studies), Elbow Dislocation (n=5 studies) | Surgical |
| Prospective Cohort Studies | 8 | 2,586 | 48 years (18-85 years) | Triceps Tendon Avulsion (n=8 studies), Olecranon Fracture (n=1 study), Elbow Dislocation (n=1 study) | Surgical |
| Retrospective Cohort Studies | 5 | 2,586 | 48 years (18-85 years) | Triceps Tendon Avulsion (n=5 studies), Olecranon Fracture (n=0 studies), Elbow Dislocation (n=1 study) | Surgical |
Figure 1. PRISMA flow chart for the study selection process.
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses
These 25 studies comprised 12 randomized controlled trials, eight prospective cohort studies, and five retrospective cohort studies, with a combined sample size of 2,586 patients. The mean age of participants across all studies was 48 years, ranging from 18 to 85 years. The most common injury types investigated in these studies were isolated triceps tendon avulsion, olecranon fracture-associated avulsion, and elbow dislocation-associated injury. Most studies (n=20) investigated surgical interventions, while the remaining studies investigated conservative management.
Surgical Technique
Numerous repair types have been documented in the literature, but no consensus on a specific surgical procedure has been found. Table 4 describes some of the research included in this literature. Although the transosseous approach appeared to be more popular, the re-rupture rate was similarly significant. Suture anchor repair was the second most frequently used repair followed by primary suture. Our analysis showed that surgical intervention for the repair of the triceps tendon was associated with significantly better outcomes than conservative management for isolated triceps tendon avulsion (relative risk {RR}=2.32, 95% CI 1.75-3.07). Among the different surgical interventions, repair with suture anchors was associated with the highest rate of successful outcomes for triceps tendon avulsion (RR=2.62, 95% CI 1.64-4.18).
Table 4. Comparison of various repair techniques in different studies.
| Study | Sample Size | Repair Technique | Mean age | Mean follow-up (months) | Rerupture Rate | Distibution of repair technique |
| Waterman et al. [6] | 69 | Bone Tunnels, Suture Repair, or Suture Anchor | 48 years | 48 | 0% across all repair | 43.5% (30) - transosseous repair, 33.3% (23 )- primary suture repair, 18.8% (13) - suture anchor repair |
| Horneff et al. [10] | 56 | Transosseous or Suture Anchor | 52.7 years | 51 | 7.1% (2 transosseous, 2 suture anchor) | 58.9% (33) - transosseous repair, 41.1% (23 ) - suture anchor repair |
| Giannicola et al. [11] | 28 | Transosseous, Suture Anchor, and combination | 45 years | 47.5 | 3.0% (1 suture anchor) | 69% (20) - transosseous repair, 24.1% (7) - suture anchor repair, 6.9% (2) - a combination of both |
| Mirzayan et al. [12] | 184 | Transosseous or Anchor | 49 years | 32 | 3.8 % (7 transosseous repairs) | 57.1% (105) - transosseous repair, 39.6% (73 ) - suture anchor repair, 3.3% (6) - other techniques not documented |
The most prevalent mechanism for injury across all studies was an accidental fall or direct trauma to the elbow, followed by weightlifting training sessions. The functional evaluation was performed using a variety of scoring techniques that differed between studies (Table 5). The majority of the patients with a triceps tendon injury had radiographs taken. A few studies reported further imaging for diagnostic purposes, such as magnetic resonance imaging (MRI) or ultrasound (US). All re-rupture patients underwent examination as well as diagnostic MRI imaging.
Table 5. Studies comparing mechanism of injury, radiological evidence, and overall outcome scores.
KJOC: Kerlan-Jobe Orthopaedic Clinic; MEPS: Mayo Elbow Performance Score; QuickDASH: Quick Disabilities of the Arm, Shoulder and Hand; VAS: visual analog scale; VR-12: Veterans RAND 12-Item Health Survey, m-ASES: Modified American Shoulder and Elbow Surgeons Score, MRI: Magnetic Resonance Imaging, US: Ultrasound
| Study | Mechanism of Injury | Radiological Evidence | Overall Outcome Scores |
| Waterman et al. [6] | Direct elbow trauma (44.9%), extension/lifting exercises (20.3%), overuse (17.4%), and hyperflexion or hyperextension (17.4%) | No mention of radiological evidence | MEPS: 90.7 ± 25; QuickDASH: 9.7 ± 14.8; VAS score: 0.9 ± 1.7 KJOC score: 84.5 ± 20.0; VR-12 score: 0.8 ± 0.1 |
| Horneff et al. [10] | Traumatic/accidental fall | MRI | MEPS: 94 ± 9.5; QuickDASH: 4.8 ± 5.0 |
| Giannicola et al. [11] | Accidental fall - direct trauma - 65.5% weightlifting - 34.%% | X-ray- 100%, US- 31 % MRI- 62% | MEPS: 94 (60 - 100); QuickDASH: 10 (0-52); m-ASES: 94 (58 to 100) |
| Mirzayan et al. [12] | Accidental fall - 56.5% weight lifting and benchpress - 19% High energy trauma - 9.2% | X-ray - 64.1% MRI - 38.5% positive sign | Outcome measured score not used |
Discussion
Triceps tendon injury is often seen in middle-aged or older adults who participate in activities that involve repetitive use of the elbow, such as weightlifting, boxing, professional football, or racket sports players, possibly due to the rigorous training routine [13]. Underlying medical conditions such as diabetes, chronic renal failure, haemodialysis, hyperparathyroidism, and systemic and anabolic steroid use have also been associated with an increased risk of triceps tendon rupture [14-16]. Along with being rarely described, this injury pattern is not only challenging to diagnose but often delayed.
The clinical presentation of triceps tendon rupture varies depending on the severity of the injury. Patients typically report sudden pain and weakness in the elbow, which may be accompanied by a popping or tearing sensation. Occasionally, individuals may experience a discernible gap in the triceps tendon and exhibit a positive modified Thompson squeeze test developed to aid the diagnosis as described by Viegas [4].
The diagnosis of triceps tendon rupture is typically made based on the patient's clinical presentation and imaging studies. X-rays may reveal a displaced olecranon or a small avulsion fragment [17,18], commonly known as a "fleck sign" (Figure 2) [16]. Triceps ruptures have the potential to go undetected through X-ray imaging. Consequently, healthcare professionals resort to utilising US and MRI to diagnose both partial and complete tears of the triceps [17,19,20]. Mayo Elbow Performance Score (MEPS) can be used to grade the severity of the avulsion, as shown in Table 6 [21].
Table 6. Mayo Elbow Performance Score (MEPS).
| Function | Definition | Points | Score classification |
| Pain | None | 45 | Excellent > 90 |
| Mild | 30 | ||
| Moderate | 15 | ||
| Severe | 0 | ||
| Motion | Arc > 100 | 20 | Good: 75-89 |
| Arc 50-100 | 15 | ||
| Arc < 50 | 5 | ||
| Stability | Stable | 10 | Fair: 60-74 |
| Moderate Instability | 5 | ||
| Gross instability | 0 | ||
| Function | Comb Hair | 5 | Poor < 60 |
| Feed | 5 | ||
| Hygiene | 5 | ||
| Shirt | 5 | ||
| Shoe | 5 | ||
| Total | 100 |
Figure 2. Lateral X-ray image of the elbow.
The arrow is showing an avulsed fragment - Fleck Sign
Image source: Original X-ray from a patient seen by one of the authors in the Emergency Department.
Suitable treatment for a triceps rupture should consider factors such as the location of the rupture, the strength of elbow extension, the patient's expectations, and the patient's medical condition. Partial tendon ruptures with less than 50% tendon involvement, and triceps muscle ruptures are often treated conservatively. This involves immobilising the elbow until the injury has healed, followed by a period of range of motion exercises and, finally, strengthening exercises [22]. In a case series, Van Riet et al. reported that out of 15 cases of partial triceps ruptures treated conservatively, nine cases did not show any improvement, and six cases required reconstruction [18].
Procedures for the repair of the triceps tendon can primarily be classified into three types: transosseous (TO), suture anchor (SA), and anatomic techniques [23]. Numerous techniques, such as transosseous cruciate repair, transosseous speed bridge repair, a combination of bone tunnels and suture anchors, and allo/autograft, have been reported in the literature [24]. Various repair techniques have been used and have varied results, as shown in Tables 4, 5. Yeh's transosseous cruciate repair method is the most commonly reported technique in the literature [25,26], and the suture anchor technique for tendon repair is gaining more popularity [27].
Numerous studies have demonstrated positive results using various surgical techniques: transosseous bone tunnels, suture repair, and anchor placement. In a retrospective case study of 69 patients who underwent triceps tendon repair, Waterman et al. reported no re-rupture in any patient at the time of final follow-up [6]. There was no statistically significant association found between patient age, the degree of tear, the surgical technique employed, and the presence of perioperative complications. According to Horneff et al., SA repair is associated with higher DASH scores as compared to TO repair [10]. However, no significant difference was found in the risk of re-rupture based on the type of repair (P > 0.99).
A substantial difference was observed between the TO and A categories based on information gathered from the largest dataset, as described by Mirazayan et al. [12]. The findings of the study reveal a statistically significant difference in the re-rupture rates between the TO and SA groups. A re-rupture rate of 6. 7% was reported among the TO group, whereas no re-rupture was reported in the SA group (P = 0.0244). A significant difference in the overall operation rate was also noticed, with the TO group exhibiting a re-operation rate of 9.5% compared to the SA group's percentage of 1.4% (P = 0.026). The study also discovered that those in the TO group stayed longer in medical care for an average of 4.3 months as opposed to 3.4 months in the SA group (P = 0.0014). The incidence of postoperative infection was significantly higher in the TO group, with a rate of 3.8% compared to 0% in the SA group (P = 0.092).
Overall, the reported cases of re-rupture range from 0% to 25% in high-demand cohorts [28]. Even though direct suture repair is the method that is most frequently utilised [12], there are numerous variants in suture procedures, including how the suture is attached to the distal tendon and how the tendon is then anchored to its insertion point on the olecranon tip.
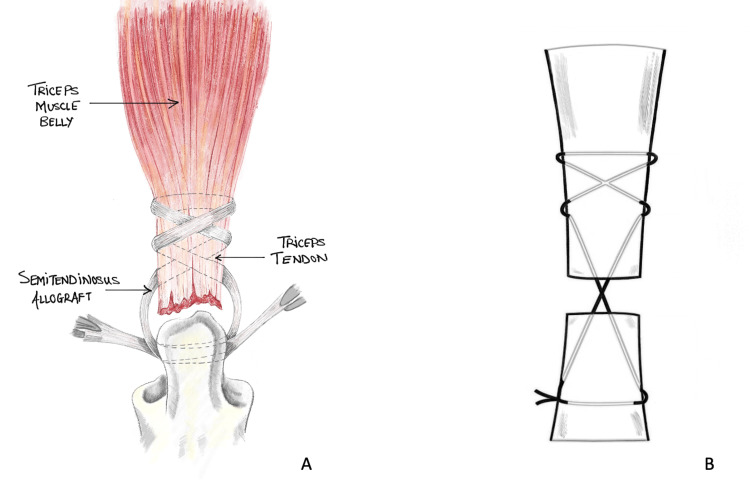
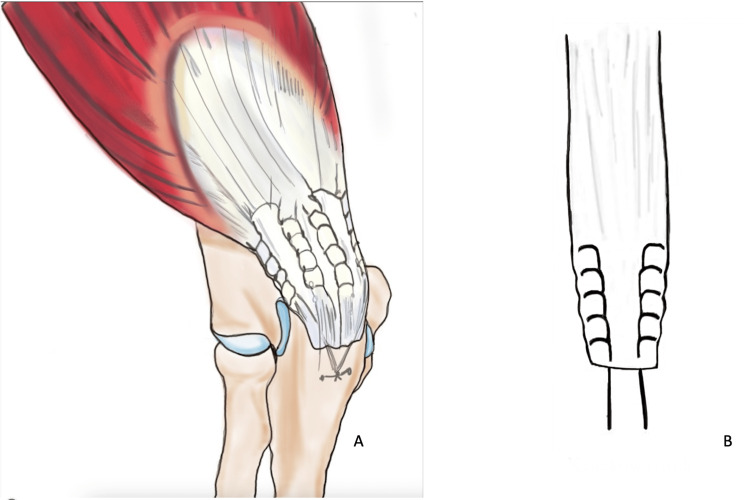
The majority of the latest repair methods involve utilising either the Bunnell (Figure 3) or Krackow (Figure 4) whipstitch technique, which entails threading non-absorbable sutures through the tendon. Suture pullout through the tendon is one of the common reasons for re-rupture described in various literature. The study conducted by Mait et al. on 30 bovine Achilles tendons comparing two vs four-stranded Krackow and the Krackow-Bunnel combination found the two-stranded Krackow technique to be inferior to the other methods [29]. The author also found that the Krackow/Bunnell group showed significantly more deformation before suture failure than the four-stranded Krackow construct (36.2 vs 28.7 mm, p = 0.009). The suture demonstrated a significantly higher resistance to rupture with an increased energy requirement (4635 vs 3346 N/mm; p = 0.016) [29]. Even though this study was conducted on bovine specimen and using Achilles tendons (that are usually subject to higher loads than triceps tendons), it highlights a higher mechanical advantage favoring the Krackow-Bunnel combination than the four-stranded Krackow technique and can be used where suture pullout is a significant concern. However, more thorough research and evaluation are required to reach a definitive conclusion before this technique can be used in clinical settings for patient use.
Figure 3. Bunnel repair technique.
Bunnel suture repair technique (A) using allograft and schematic diagram (B)
Images re-drawn by authors to represent the repair technique
Figure 4. Krackow repair technique.
Four-stranded Krackow repair suture technique (A) and schematic diagram of two-stranded repair (B)
Images re-drawn by authors to represent the repair technique.
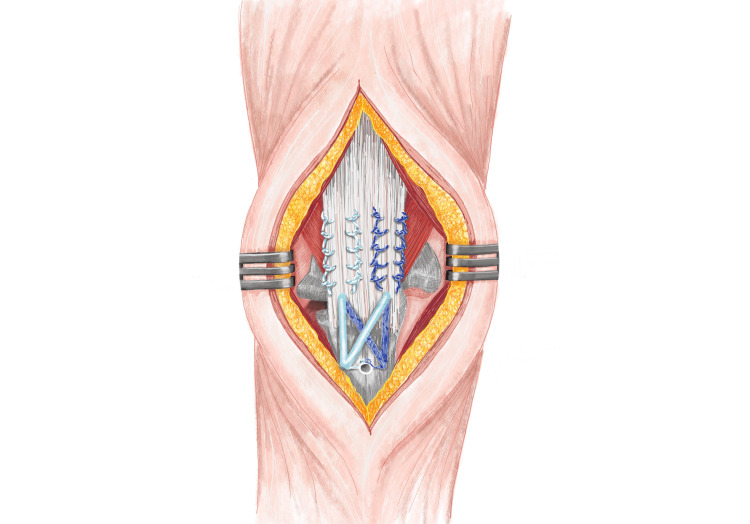
The anatomic repair technique described by Yeh et al. [28] covered 86% of the anatomic footprint as compared to the TO cruciate technique. The displacement of footprint between anatomic repair and TO cruciate repair was even more pronounced after cyclical loading with a significant gap formation, P < 0.05. The knotless suture technique (Figure 5) described in a biochemical study was found to have significantly reduced the risk of iatrogenic injury and had a superior anatomic footprint repair as compared to TO repair in average load to failure (462.9N vs 233.5 N) [30,31].
Figure 5. Knotless suture technique with four-stranded Krackow whipstitch.
Images re-drawn by authors to represent the repair technique
Interpretation of the results and limitations
According to the gathered data, surgical intervention is associated with better outcomes compared to conservative management for the repair of triceps tendon rupture. This data is consistent with the previous research and systematic reviews demonstrating the superiority of surgical intervention. Future research and study design should seek to enhance the understanding of the disease mechanism and develop targeted strategies for prevention and rehabilitation.
Despite the diligent effort, this study has several limitations. We identified three limitations to this study at an individual and meta-analysis level. First, the gathered data had to meet the inclusion and exclusion criteria set by the independent reviewer. Secondly, significant variability was identified based on sample size, follow-up, assessment criteria, and mechanism of sustained injury. Finally, our analysis was limited to studies published in the English language only, which may have introduced publication bias and the likelihood of generalizability of our findings.
Conclusions
Triceps tendon avulsion is a rare injury often associated with falls onto an outstretched hand. The aetiology of triceps tendon avulsion is multifactorial, and several risk factors have been identified. The diagnosis of triceps tendon avulsion is often delayed, but MRI is the gold standard for diagnosis. Treatment options for triceps tendon avulsion include both surgical and non-surgical approaches. Our findings add to our understanding of the relative efficiency of various surgical approaches, with suture anchor repair with or without knotless repair appearing to be the most successful technique for triceps tendon avulsion. Early identification of such tendon injuries and prompt interventions forms the cornerstone of a successful outcome. The application is enormous with the new developing approaches and research comparisons. Additional studies and standard criteria for assessment and follow-up are needed, however, to establish the best surgical procedures for these sorts of injuries and to analyse long-term results such as patient-reported function and quality of life.
Acknowledgments
AH and JG contributed equally to the work and should be considered co-first authors. Both worked on designing the study, methodology, statistical analysis, studies and drafting the manuscript. VB carried out statistical methods and analysis of the data along with performance scoring analysis of various literature study contributed to the manuscript. CA, MA, and KT contributed with the figures and designed the study by independently reviewing the selection process. SA helped in critical analysis of the paper and contributed to the editing of the manuscript. BR and SP helped with the literature study and editing the manuscript. All authors read and approved the final manuscript.
The authors have declared that no competing interests exist.
References
- 1.Bilateral partial rupture of triceps tendon: case report and quantitative assessment of recovery. Harris PC, Atkinson D, Moorehead JD. Am J Sports Med. 2004;32:787–792. doi: 10.1177/0363546503258903. [DOI] [PubMed] [Google Scholar]
- 2.Disruptions of muscles and tendons: an analysis of 1,041 cases. Anzel SH, Covey KW, Weiner AD, et al. https://cir.nii.ac.jp/crid/1571417125669557504. Surgery. 1959;45:406–414. [PubMed] [Google Scholar]
- 3.Avulsion of the triceps tendon. Viegas SF. https://europepmc.org/article/med/2367146. Orthop Rev. 1990;19:533–536. [PubMed] [Google Scholar]
- 4.Triceps tendon rupture: the knowledge acquired from the anatomy to the surgical repair. Celli A. Musculoskelet Surg. 2015;99 Suppl 1:0–66. doi: 10.1007/s12306-015-0359-y. [DOI] [PubMed] [Google Scholar]
- 5.Triceps rupture. A case report and literature review. Bach BR Jr, Warren RF, Wickiewicz TL. Am J Sports Med. 1987;15:285–289. doi: 10.1177/036354658701500319. [DOI] [PubMed] [Google Scholar]
- 6.Surgical repair of distal triceps tendon injuries: short-term to midterm clinical outcomes and risk factors for perioperative complications. Waterman BR, Dean RS, Veera S, et al. Orthop J Sports Med. 2019;7:2325967119839998. doi: 10.1177/2325967119839998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Traumatic rupture of the distal triceps tendon (a series of 7 cases) Neumann H, Schulz AP, Breer S, Faschingbauer M, Kienast B. Open Orthop J. 2015;9:536–541. doi: 10.2174/1874325001509010536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Page MJ, McKenzie JE, Bossuyt PM, et al. BMJ. 2021;372:0. doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Newcastle-Ottawa Scale: comparing reviewers' to authors' assessments. Lo CK, Mertz D, Loeb M. BMC Med Res Methodol. 2014;14:45. doi: 10.1186/1471-2288-14-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Functional outcomes of distal triceps tendon repair comparing transosseous bone tunnels with suture anchor constructs. Horneff JG 3rd, Aleem A, Nicholson T, et al. J Shoulder Elbow Surg. 2017;26:2213–2219. doi: 10.1016/j.jse.2017.08.006. [DOI] [PubMed] [Google Scholar]
- 11.Results of primary repair of distal triceps tendon ruptures in a general population: a multicentre study. Giannicola G, Bullitta G, Rotini R, et al. Bone Joint J. 2018;100-B:610–616. doi: 10.1302/0301-620X.100B5.BJJ-2017-1057.R2. [DOI] [PubMed] [Google Scholar]
- 12.Operative Management of Acute Triceps Tendon Ruptures: Review of 184 Cases. Mirzayan R, Acevedo DC, Sodl JF, Yian EH, Navarro RA, Anakwenze O, Singh A. Am J Sports Med. 2018;46:1451–1458. doi: 10.1177/0363546518757426. [DOI] [PubMed] [Google Scholar]
- 13.Avulsion of the triceps tendon. Pantazopoulos T, Exarchou E, Stavrou Z, Hartofilakidis-Garofalidis G. J Trauma. 1975;15:827–829. doi: 10.1097/00005373-197509000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Rupture of the triceps tendon with olecranon bursitis. A case report with a new method of repair. Clayton ML, Thirupathi RG. https://journals.lww.com/corr/Abstract/1984/04000/Rupture_of_the_Triceps_Tendon_with_Olecranon.30.aspx. Clin Orthop Relat Res. 1984;183:5. [PubMed] [Google Scholar]
- 15.Bilateral rupture of the quadriceps tendon associated with anabolic steroids. Liow RY, Tavares S. Br J Sports Med. 1995;29:77–79. doi: 10.1136/bjsm.29.2.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hyperparathyroidism with avulsion of three major tendons. Report of a case. PR FS, AD A. N Engl J Med. 1962;266:968–971. doi: 10.1056/NEJM196205102661903. [DOI] [PubMed] [Google Scholar]
- 17.Triceps tears in athletes: different injury patterns and surgical treatment. Lempainen L, Sarimo J, Rawlins M, Heikkilä J, Orava S. Arch Orthop Trauma Surg. 2011;131:1413–1417. doi: 10.1007/s00402-011-1319-0. [DOI] [PubMed] [Google Scholar]
- 18.Surgical treatment of distal triceps ruptures. van Riet RP, Morrey BF, Ho E, O'Driscoll SW. J Bone Joint Surg Am. 2003;85:1961–1967. doi: 10.2106/00004623-200310000-00015. [DOI] [PubMed] [Google Scholar]
- 19.Distal triceps tendon rupture and repair in an otherwise healthy pediatric patient: a case report and review of the literature. Kibuule LK, Fehringer EV. J Shoulder Elbow Surg. 2007;16:0–3. doi: 10.1016/j.jse.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 20.Chronic tendonopathy as a unique cause of non traumatic triceps tendon rupture in a (risk factors free) bodybuilder: a case report. Mangano T, Cerruti P, Repetto I, Trentini R, Giovale M, Franchin F. J Orthop Case Rep. 2015;5:58–61. doi: 10.13107/jocr.2250-0685.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morrey BF, An KN. Morrey's The Elbow and Its Disorders (Fourth Edition) Philadelphia: W.B. Saunders; 2009. Functional Evaluation of the Elbow; pp. 80–91. [Google Scholar]
- 22.Distal triceps ruptures. Demirhan M, Ersen A. EFORT Open Rev. 2016;1:255–259. doi: 10.1302/2058-5241.1.000038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Triceps tendon anatomic repair utilizing the "suture bridge" technique. Edelman D, Ilyas AM. J Hand Microsurg. 2018;10:166–171. doi: 10.1055/s-0038-1636729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Distal triceps rupture repair: the triceps pulley-pullover technique. Dimock RA, Kontoghiorghe C, Consigliere P, Salamat S, Imam MA, Narvani AA. Arthrosc Tech. 2019;8:0–91. doi: 10.1016/j.eats.2018.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Distal triceps injuries (including snapping triceps): a systematic review of the literature. Shuttlewood K, Beazley J, Smith CD. World J Orthop. 2017;8:507–513. doi: 10.5312/wjo.v8.i6.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Distal triceps rupture. Yeh PC, Dodds SD, Smart LR, Mazzocca AD, Sethi PM. J Am Acad Orthop Surg. 2010;18:31–40. doi: 10.5435/00124635-201001000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Triceps tendon ruptures in professional football players. Mair SD, Isbell WM, Gill TJ, Schlegel TF, Hawkins RJ. Am J Sports Med. 2004;32:431–434. doi: 10.1177/0095399703258707. [DOI] [PubMed] [Google Scholar]
- 28.The distal triceps tendon footprint and a biomechanical analysis of 3 repair techniques. Yeh PC, Stephens KT, Solovyova O, Obopilwe E, Smart LR, Mazzocca AD, Sethi PM. Am J Sports Med. 2010;38:1025–1033. doi: 10.1177/0363546509358319. [DOI] [PubMed] [Google Scholar]
- 29.A biomechanical comparison of different tendon repair techniques. Mait JE, Hayes WT, Blum CL, et al. J Long Term Eff Med Implants. 2016;26:167–171. doi: 10.1615/JLongTermEffMedImplants.2016016536. [DOI] [PubMed] [Google Scholar]
- 30.Distal triceps knotless anatomic footprint repair: a new technique. Paci JM, Clark J, Rizzi A. Arthrosc Tech. 2014;3:0–6. doi: 10.1016/j.eats.2014.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Distal triceps knotless anatomic footprint repair is superior to transosseous cruciate repair: a biomechanical comparison. Clark J, Obopilwe E, Rizzi A, Komatsu DE, Singh H, Mazzocca AD, Paci JM. Arthroscopy. 2014;30:1254–1260. doi: 10.1016/j.arthro.2014.07.005. [DOI] [PubMed] [Google Scholar]