Early childhood cryptosporidiosis causes acute disease and mortality, as well as lasting malnutrition and developmental delay. However, there are no safe and effective therapeutics for cryptosporidiosis. Developing such therapeutics will save hundreds and thousands of lives in young children and spare millions of disability-adjusted life years lost (DALYs). This white paper discusses the global public health impact of Cryptosporidium infections, the immediate need for more effective treatment of cryptosporidiosis, and recent advances that are yielding multiple promising leads for therapeutic development. We will discuss the remaining challenges, which is to complete the preclinical and clinical steps to bring these novel therapeutics to children in urgent need of treatment.
Diarrhoeal diseases cause unacceptable loss of life, mainly among infants and children in low-income and middle-income countries (LMICs). The Global Enteric Multicentre Study (GEMS) revealed the pathogens associated with diarrhoea in children in LMICs.1 Of particular prevalence, as cause of severe disease, were rotavirus, Cryptosporidium spp, enterotoxigenic Escherichia coli and Shigella. The parasite Cryptosporidium (C. hominis and C. parvum) remains one of the most lethal pathogens for malnourished infants and children, with a devastating health impact on those under 2 years of age. The GEMS study estimated about 7.5 million cases of Cryptosporidium infection occur every year within this population in Africa and Asia resulting in over 200 000 Cryptosporidium-attributable deaths due to moderate-to-severe diarrhoea, with an excess of 59 000 deaths compared with children with similar symptoms that were Cryptosporidium negative.2
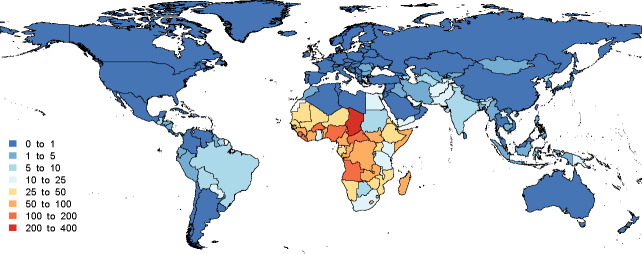
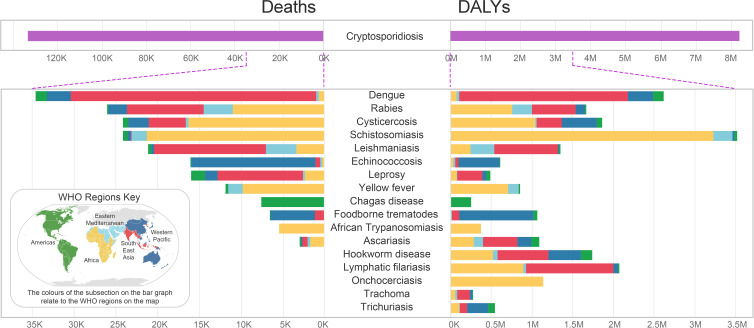
Cryptosporidium infection in these malnourished children is also significantly associated with debilitating stunted growth contributing to excess mortality.3–6 This Cryptosporidium-associated stunting and wasting leads to poor physical and neurological health with poor childhood development, resulting in a lasting effect on population health in LMICs.5 This burden falls disproportionately on children in sub-Saharan Africa, but also in South America and Asia (figure 1). In 2018, Dr Khalil and coworkers at the Institute for Health Metrics and Evaluation reported that acute Cryptosporidium infection was associated with an annual loss of greater than 4.2 million DALYs.3 Each DALY represents the loss of a full year of healthy life. In 2019, the Global Burden of Disease study revised the number of deaths and DALYs attributable to Cryptosporidium to 133 422 deaths and 8.2 million DALYs per year, taking into account both the acute and long-term effects of Cryptosporidium infection.7 To put this in perspective with other diarrhoeal diseases within the same 2019 study, cholera is attributable to less deaths (117 000) and DALYs (7.1 million), and both Shigella and Rotavirus were responsible for only slightly more deaths (148 000 and 235 000, respectively) and DALYs (10 million and 17 million).7 In contrast to cryptosporidiosis, vaccines or treatments are available or in advanced development for these infections. Notably, when comparing Cryptosporidium with WHO recognised neglected tropical diseases (NTDs), it greatly exceeds both the deaths and DALYs associated with essentially all of these diseases (figure 2).8
Figure 1.
Total (acute and long-term) Cryptosporidium DALYs per 1000 child-years among children under 5 (GBD estimates and geographic distribution, Ibrahim Khalil). DALYs after accounting for undernutrition-associated DALYs due to cryptosporidiosis.7 DALYs, disability-adjusted life years lost; GBD, Global Burden of Disease.
Figure 2.
Infectious disease deaths and DALYs by WHO region.8 There are estimated to be 133 000 deaths per year and 8200K DALYs due to cryptosporidiosis (pink), which greatly exceed the WHO NTDs, note differences in scales. DALYs, disability-adjusted life years lost; NTDs, neglected tropical diseases.
Effective treatment to mitigate the impact of cryptosporidiosis on child health and survival is woefully lacking. Nitazoxanide is the only US Food and Drug Administration (FDA) approved therapeutic for treating Cryptosporidium infection. It has been shown to be ineffective in immunocompromised individuals and less than 50% effective in malnourished children less than 5 years old.9 Nitazoxanide in vitro does have direct activity against Cryptosporidium, but only at concentrations much higher than those achieved during therapy. Animal models suggest nitazoxanide likely relies on stimulation of the immune system to expel Cryptosporidium. Those most threatened by infection, malnourished children and the immunocompromised cannot mount the immune response required for effective therapy with nitazoxanide.10 11
This unmet medical need inspired a recent surge in Cryptosporidium research that has yielded the modern experimental tools and facile animal models needed to discover antiparasitic compounds and validate their targets.12–23 Most importantly, safe and effective compounds in preclinical models with direct action against Cryptosporidium have emerged.13 15 16 18 24–31 This represents a major advance, significantly expanding the quality and quantity of the portfolio. Multiple drug candidates are now progressing towards preclinical development and clinical trials at an uneven pace (table 1). The initial high-risk research that led to these compounds was conducted by multiple academic and industry groups, often with extensive academic and industry collaboration and with governmental and philanthropic support. Now further investments are needed to capitalise on this rich portfolio and accelerate the development and registration of transformative therapies for this largely unmet medical need.
Table 1.
Examples of compounds in preclinical development
| Inhibitor/compound series | Lead laboratory | Effective in animal models | Stage | References |
| Phosphatidylinositol 4-kinase | Novartis | Yes | Phase 1 human trials | 15 |
| Bumped kinase inhibitors | University of Washington | Yes | Preclinical candidate | 26 |
| Lysyl tRNA synthetase | DDU, University of Dundee | Yes | Late lead profiling | 13 |
| Benzoxaborole | Anacor, University of Vermont | Yes | Late lead profiling | 29 |
| SLU-2633/MMV665917 | St. Louis University, University of Vermont | Yes | Late lead profiling | 31 |
| Phenylalanine tRNA synthetase | BROAD Institute, University of Vermont | Yes | Early lead profiling | 16 |
A vaccine that prevents Cryptosporidium morbidity and mortality would be of great benefit to childhood health in LMICs, and research towards vaccination should be supported. However, natural immunity to Cryptosporidium is non-sterile and requires multiple infections, highlighting the parasite’s potential to evade immunity. Developing vaccines to address parasitic infections, like Cryptosporidium, has been difficult and we are probably at least a decade from having a safe and effective vaccine. Developing a therapeutic will allow us to address child health in LMICs in a much faster time frame. Even after vaccines arrive, there will be a need for drugs because of insufficient protection, lack of coverage and challenges of roll-out and delivery.
Multiple recent efforts centred in academia, industry and in joint venture have produced highly promising late preclinical therapeutic leads that are markedly superior to nitazoxanide in preclinical models (table 1). This is a truly transformative advance in both quality and quantity offering a viable path towards treatment. These compounds now require varying degrees of advanced preclinical testing, and clinical trials performed before they can be deployed. The target population is infants, however, for a proof of concept (phase 2a) study, testing in infants is inadvisable due to safety, pharmacokinetic and ethical challenges. Cryptosporidiosis is typically rare in adults living in high transmission areas due to acquired immunity, except in HIV/AIDS patients. Recent advances in the clinical evaluation of novel antimalarials provide critical guidance forward. Human challenge models using healthy volunteers have proven an invaluable tool32 33 providing an insight into efficacy without the risks associated with highly vulnerable populations. Multiple such studies have been conducted with Cryptosporidium in the past and were found to be safe34–36 and the model has recently be updated.37 We support a clinical trial plan proposed in which the proof of concept (phase 2a study) is conducted with volunteers intentionally infected with C. parvum, followed by phase 2b and 3 studies in children in endemic areas.37
Since malaria and Cryptosporidium belong to the same phylum Apicomplexa, they share some conserved drug targets, and thus there is a synergy possibility in research and development of malaria and Cryptosporidium therapeutics. But like malaria, Cryptosporidium may develop resistance to monotherapy, given the high numbers of parasites during infection. Indeed, emergence of resistance has been documented in the newborn calf model of infection for one compound that targets methionyl-tRNA-synthetase.38 Therefore, it is probably necessary to take several compounds through clinical development to provide the possibility of combination treatment (table 1). There are also possibilities for synergy with the animal health market, particularly for dairy cattle, where in some areas nearly 100% of newborn calves acquire C. parvum infection, and Cryptosporidium infection has been shown to lead to lasting weight loss and reduced milk production.39–41
A challenge to be addressed is the clinical usage of an anti-Cryptosporidium drug. Studies indicate that there are multiple causes of diarrhoea; as indicated above, causative organisms include Shigella spp, enterotoxigenic E. coli, Campylobacter jejuni and rotavirus. There is current compelling evidence of unmet therapeutic need for enteric cryptosporidiosis found in three patient groups: (1) young children aged 0–24 months in LMICs; (2) malnourished children under age 5 and (3) immunosuppressed individuals of any age.42 43 A recent publication outlines an effective therapeutic could be used to reduce the large burden of Cryptosporidium in LMICs (table 2).42 Cryptosporidium therapy could be used syndromically, for instance in children less than 2 years old with moderate-to-severe diarrhoea, probably combined with an antibacterial to cover the major treatable causes, E. coli, Shigella spp. and C. jejuni. Treatment could be carried out with a diagnostic, such as a point-of care rapid antigen detection test, or a PCR, similar to that used in SARS-CoV-2 detection. This diagnostic-directed therapy might be especially helpful in malnourished children less than 5 years old, where asymptomatic and mildly symptomatic Cryptosporidium has been shown to be highly associated with poor outcomes, such as stunting, poor physical and mental development and excess deaths from other causes. These diagnostic tools are available now, and the rapid antigen detection test can be done at small village clinics where sick and malnourished children are first seen. In the event that a compound or combination with appropriate safety profile can be developed, mass drug administration could be used, particularly given the high infectivity of the parasite and the fact that many infants are likely to be chronically infected.
Table 2.
Use case scenarios for an anti-Cryptosporidium therapeutic for LMICs adapted from 42
| Target population | Disease burden | Potential treatment sites | Potential treatment strategies | Current applicability: nitazoxanide |
| Young children aged 0–24 months | 7.5 million cases with moderate-to-severe diarrhoea,2 133 000 deaths and 8.2M DALYs annually in LMICs7 | Primary, secondary and tertiary health facilities in LMICs | Diagnosis-based treatment | Not approved in children under 12 months, only ~30% efficacy in malnourished9 |
| Empiric treatment in high-risk populations where diagnostic tools are not available | Insufficient evidence and guidelines | |||
| Community based treatment | Mass drug administration in seasons with high prevalence | Insufficient evidence and guidelines | ||
| Malnourished children | Estimated 50 million wasted children globally.45 Recent studies indicate 10%–20% prevalence of cryptosporidiosis in children with acute malnourishment.9 46–48 | Primary, secondary and tertiary health facilities in LMICs. Malnutrition care centres in clinics and hospitals |
Diagnosis-based treatment | Poorly effective (~30% efficacious)9 |
| Empiric treatment in high-risk populations where diagnostic tools are not available | Insufficient evidence and guidelines. Nitazoxanide poorly effective9 | |||
| Immunocompromised patients | Estimates range from 5% to 50% of PLWHA and up to 30% of solid organ transplant recipients.49–53 | Primary, secondary and tertiary health facilities in LMICs. HIV/AIDS treatment programmes. Transplant centres in any global setting |
Diagnosis-based treatment | Poorly or non-effective for PLWHA9 43 54 |
| Empiric treatment in high-risk populations where diagnostic tools are not available | Insufficient evidence and guidelines Poorly or non-effective for PLWHA9 43 54 |
Adapted from Ashigbie et al. 42
DALYs, disability-adjusted life years lost; LMICs, low-income and middle-income countries; PLWHA, people living with HIV/AIDS.
Beyond this, the authors believe that Cryptosporidium should be formally recognised as a NTD by the WHO, for its major impact is in LMICs and predominantly affects infants and young children. As noted above, Cryptosporidium has a very significant impact compared with many other NTDs currently listed by the WHO (figure 2). This status will bring the critical medical need of Cryptosporidium treatment to the attention of funding bodies, foundations, international health organisations and pharmaceutical companies. Cryptosporidium should also be on the list of tropical infections eligible for a priority review voucher (PRV) by US FDA.44 The PRV programme has proven to be an important financial incentive to pharmaceutical companies wishing to develop drugs for NTDs.
There are some exciting compounds at a later preclinical or early clinical stage. This calls for more funding to move these leads into clinical trials, to properly evaluate the effect that they will have on millions of people (primarily infants and young children). Going into the clinic will enable us to determine the profile of a drug that can have clinical impact and to establish a way for its use.
Thus, in summary, using either deaths or DALYs as parameters, the unmet medical need for Cryptosporidium infection exceeds that of most NTDs and causes a huge impact on Africa and Asia. The current therapeutic available is inadequate for the vast majority of this unmet medical need. Tenable use case scenarios exist for how more effective therapeutics for Cryptosporidium infection could be deployed to reduce deaths and DALYs. Cryptosporidium should be recognised as a major unmet medical need and designated a NTD by the WHO and as a tropical disease with PRV status by the US FDA. The fastest way to address the unmet need is to close funding gaps in preclinical candidates and clinical trials, and this should lead to an effective Cryptosporidium therapeutic in a few years.
Footnotes
Handling editor: Seye Abimbola
Collaborators: Cryptosporidiosis Therapeutics Advocacy Group: Samuel L M Arnold, PhD, University of Washington School of Pharmacy; Beatriz Baragana, PhD, University of Dundee; Lynn Barrett, University of Washington; Frederick S Buckner, MD, University of Washington; Jeremy D Burrows, Phil, Medicines for Malaria Venture; Maria A Caravedo, MD, University of Texas Medical Branch; Ryan Choi University of Washington; Robert K M Choy, PhD, PATH; Eugenio de Hostos, PhD, Calibr at Scripps Research; Thierry Diagana, PhD, Global Health, Novartis Institutes for BioMedical Research, Inc.; Suzanne Duce, PhD, University of Dundee; Rashidul Haque, MB, PhD, ICDDR, B; Matthew A Hulverson, University of Washington; Christopher D Huston, MD, University of Vermont; Pui-Ying D Iroh Tam, DMed, Malawi-Liverpool Wellcome Programme; Paul Kelly, MD, TROPGAN, University of Zambin; Tom Kennedy, PhD, Eleven Bravo LLC; Ibrahim A Khalil, MPH, University of Washington; Minju Kim, University of Washington Hans Rosling Center Global Health; Poonum Korpe, MD, Johns Hopkins Bloomberg School of Public Health; Benoît Laleu, PhD, Medicines for Malaria Venture; Diana Lalika, University of Washington; Fabrice Laurent, PhD, INRAE, Univ. of Tours; Case W McNamara, PhD, Calibr at Scripps Research; Marvin J Meyers, PhD, St. Louis University; Roberta M O’Connor, PhD, University of Minnesota; Kayode K Ojo, PhD, University of Washington; Philipp Olias, PhD, Justus-Liebig-University Giessen; Richard Omore, PhD, Kenya Research Institute, Center for Global Health Research; Nede Ovbiebo, University of Washington; James Platts-Mills, MD, University of Virginia; Mattie C Pawlowic, PhD, University of Dundee; William A Petri, Jr MD, PhD, University of Virginia; Gladys Queen, MS, University of Washington; Divya Rao, University of Washington; Kevin Reed, PhD, University of Dundee; Michael W Riggs, DVM, University of Arizona; Jennifer L Roxas, PhD, University of Arizona; Adam Sateriale, PhD, The Francis Crick Institute; Deborah A Schaefer, MS University of Arizona; L David Sibley, PhD, Washington University in St. Louis; Jonathan M Spector, MPH, Global Health, Novartis Institutes for BioMedical Research, Inc.; Chris Tonkin, PhD, The Walter and Eliza Hall Institute of Medical Research; Timilehin E Toye, BPHARM, University of Washington; Saul Tzipori, DVM, PhD, Ds, Tufts University; Timothy Wells, PhD, Medicines for Malaria Venture; A Clinton White, MD University of Texas, Medical Branch; Grace S Yang, University of Washington.
Contributors: WCVV made the first draft, modified each draft. IG revised the first draft and led the writing group of the other authors. All the other authors revised the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Contributor Information
Cryptosporidiosis Therapeutics Advocacy CTAG:
Samuel L M Arnold, Beatriz Baragana, Lynn Barrett, Frederick S Buckner, Jeremy D Burrows, Maria A Caravedo, Ryan Choi, Robert K M Choy, Eugenio de Hostos, Thierry Diagana, Suzanne Duce, Rashidul Haque, Matthew A Hulverson, Christopher D Huston, Pui-Ying Iroh Tam, Paul Kelly, Tom Kennedy, Ibrahim A Khalil, Minju Kim, Poonum Korpe, Benoît Laleu, Diana Lalika, Fabrice Laurent, Case W McNamara, Marvin J Meyers, Roberta M O’Connor, Kayode K Ojo, Philipp Olias, Richard Omore, Nede Ovbiebo, James Platts-Mills, Mattie C Pawlowic, William A Petri, Gladys Queen, Divya Rao, Kevin Reed, Michael W Riggs, Jennifer L Roxas, Adam Sateriale, Deborah A Schaefer, L David Sibley, Jonathan M Spector, Chris Tonkin, Timilehin E Toye, Saul Tzipori, Timothy Wells, A Clinton White, and Grace S Yang
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Not required.
References
- 1. Kotloff KL, Nataro JP, Blackwelder WC, et al. Burden and Aetiology of Diarrhoeal disease in infants and young children in developing countries (the global Enteric multicenter study, GEMS): a prospective, case-control study. Lancet 2013;382:209–22. 10.1016/S0140-6736(13)60844-2 [DOI] [PubMed] [Google Scholar]
- 2. Samba O S, Khitam M, Dilruba N, et al. The burden of Cryptosporidium Diarrheal disease among children < 24 months of age in moderate/high mortality regions of sub-Saharan Africa and South Asia, utilizing data from the global Enteric multicenter study (GEMS). PLoS Negl Trop Dis 2016. 10.1371/journal.pntd.0004729.eCollection [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Khalil IA, Troeger C, Rao PC, et al. Morbidity, mortality, and long-term consequences associated with diarrhoea from Cryptosporidium infection in children younger than 5 years: a meta-analyses study. Lancet Glob Health 2018;6:e758–68. 10.1016/S2214-109X(18)30283-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Checkley W, Epstein LD, Gilman RH, et al. Effects of Cryptosporidium Parvum infection in Peruvian children: growth faltering and subsequent catch-up growth. Am J Epidemiol 1998;148:497–506. 10.1093/oxfordjournals.aje.a009675 [DOI] [PubMed] [Google Scholar]
- 5. Checkley W, White AC, Jaganath D, et al. A review of the global burden, novel diagnostics, Therapeutics, and vaccine targets for Cryptosporidium. Lancet Infect Dis 2015;15:85–94. 10.1016/S1473-3099(14)70772-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Korpe PS, Valencia C, Haque R, et al. Epidemiology and risk factors for Cryptosporidiosis in children from 8 low-income sites: results from the MAL-ED study. Clin Infect Dis 2018;67:1660–9. 10.1093/cid/ciy355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. IHME . Global burden of disease study. 2019. Available: https://vizhub.healthdata.org/gbd-results/
- 8. De Rycker M, Baragaña B, Duce SL, et al. Challenges and recent progress in drug discovery for tropical diseases. Nature 2018;559:498–506. 10.1038/s41586-018-0327-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Amadi B, Mwiya M, Musuku J, et al. Effect of Nitazoxanide on morbidity and mortality in Zambian children with Cryptosporidiosis: a randomised controlled trial. Lancet 2002;360:1375–80. 10.1016/S0140-6736(02)11401-2 [DOI] [PubMed] [Google Scholar]
- 10. Schneider A, Wendt S, Lübbert C, et al. Current Pharmacotherapy of Cryptosporidiosis: an update of the state-of-the-art. Expert Opin Pharmacother 2021;22:2337–42. 10.1080/14656566.2021.1957097 [DOI] [PubMed] [Google Scholar]
- 11. Sparks H, Nair G, Castellanos-Gonzalez A, et al. Treatment of Cryptosporidium: what we know, gaps, and the way forward. Curr Trop Med Rep 2015;2:181–7. 10.1007/s40475-015-0056-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Vinayak S, Pawlowic MC, Sateriale A, et al. Genetic modification of the Diarrhoeal pathogen Cryptosporidium Parvum. Nature 2015;523:477–80. 10.1038/nature14651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Baragaña B, Forte B, Choi R, et al. Lysyl-tRNA synthetase as a drug target in malaria and Cryptosporidiosis. Proc Natl Acad Sci U S A 2019;116:7015–20. 10.1073/pnas.1814685116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hulverson MA, Vinayak S, Choi R, et al. Bumped-kinase inhibitors for Cryptosporidiosis therapy. J Infect Dis 2017;215:1275–84. 10.1093/infdis/jix120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Manjunatha UH, Vinayak S, Zambriski JA, et al. A Cryptosporidium PI(4)K inhibitor is a drug candidate for Cryptosporidiosis. Nature 2017;546:376–80. 10.1038/nature22337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Vinayak S, Jumani RS, Miller P, et al. Bicyclic Azetidines kill the Diarrheal pathogen Cryptosporidium in mice by inhibiting parasite Phenylalanyl-tRNA synthetase. Sci Transl Med 2020;12:eaba8412. 10.1126/scitranslmed.aba8412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wilke G, Funkhouser-Jones LJ, Wang Y, et al. A stem-cell-derived platform enables complete Cryptosporidium development in vitro and genetic Tractability. Cell Host Microbe 2019;26:123–34. 10.1016/j.chom.2019.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bellini V, Swale C, Brenier-Pinchart M-P, et al. Target identification of an Antimalarial Oxaborole identifies An13762 as an alternative Chemotype for targeting Cpsf3 in Apicomplexan parasites. iScience 2020;23:101871. 10.1016/j.isci.2020.101871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Swale C, Bougdour A, Gnahoui-David A, et al. Metal-captured inhibition of pre-mRNA processing activity by Cpsf3 controls Cryptosporidium infection. Sci Transl Med 2019;11:eaax7161. 10.1126/scitranslmed.aax7161 [DOI] [PubMed] [Google Scholar]
- 20. Arnold SLM, Choi R, Hulverson MA, et al. Necessity of bumped kinase inhibitor gastrointestinal exposure in treating Cryptosporidium infection. J Infect Dis 2017;216:55–63. 10.1093/infdis/jix247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jumani RS, Hasan MM, Stebbins EE, et al. A suite of Phenotypic assays to ensure pipeline diversity when Prioritizing drug-like Cryptosporidium growth inhibitors. Nat Commun 2019;10:1862. 10.1038/s41467-019-09880-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Funkhouser-Jones LJ, Ravindran S, Sibley LD. Defining stage-specific activity of potent new inhibitors of Cryptosporidium Parvum growth in vitro mBio 2020;11:e00052-20. 10.1128/mBio.00052-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Choudhary HH, Nava MG, Gartlan BE, et al. A conditional protein degradation system to study essential gene function in Cryptosporidium Parvum. mBio 2020;11:e01231-20. 10.1128/mBio.01231-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Love MS, Choy RKM. Emerging treatment options for Cryptosporidiosis. Curr Opin Infect Dis 2021;34:455–62. 10.1097/QCO.0000000000000761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wang B, Castellanos-Gonzalez A, White AC. Novel drug targets for treatment of Cryptosporidiosis. Expert Opin Ther Targets 2020;24:915–22. 10.1080/14728222.2020.1785432 [DOI] [PubMed] [Google Scholar]
- 26. Hulverson MA, Choi R, Arnold SLM, et al. Advances in bumped kinase inhibitors for human and animal therapy for Cryptosporidiosis. Int J Parasitol 2017;47:753–63. 10.1016/j.ijpara.2017.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hulverson MA, Choi R, McCloskey MC, et al. Repurposing infectious disease hits as anti-Cryptosporidium leads. ACS Infect Dis 2021;7:1275–82. 10.1021/acsinfecdis.1c00076 [DOI] [PubMed] [Google Scholar]
- 28. Buckner FS, Ranade RM, Gillespie JR, et al. Optimization of methionyl tRNA-synthetase inhibitors for treatment of Cryptosporidium infection. Antimicrob Agents Chemother 2019;63:e02061-18. 10.1128/AAC.02061-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lunde CS, Stebbins EE, Jumani RS, et al. Identification of a potent Benzoxaborole drug candidate for treating Cryptosporidiosis. Nat Commun 2019;10:2816. 10.1038/s41467-019-10687-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Guo F, Zhang H, McNair NN, et al. The existing drug Vorinostat as a new lead against Cryptosporidiosis by targeting the parasite Histone Deacetylases. J Infect Dis 2018;217:1110–7. 10.1093/infdis/jix689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Oboh E, Schubert TJ, Teixeira JE, et al. Optimization of the urea Linker of Triazolopyridazine Mmv665917 results in a new Anticryptosporidial lead with improved potency and predicted hERG safety margin. J Med Chem 2021;64:11729–45. 10.1021/acs.jmedchem.1c01136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Roestenberg M, Hoogerwerf M-A, Ferreira DM, et al. Experimental infection of human volunteers. Lancet Infect Dis 2018;18:e312–22. 10.1016/S1473-3099(18)30177-4 [DOI] [PubMed] [Google Scholar]
- 33. McCarthy JS, Rückle T, Djeriou E, et al. A phase II pilot trial to evaluate safety and efficacy of Ferroquine against early Plasmodium Falciparum in an induced blood-stage malaria infection study. Malar J 2016;15:469. 10.1186/s12936-016-1511-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. DuPont HL, Chappell CL, Sterling CR, et al. The infectivity of Cryptosporidium Parvum in healthy volunteers. N Engl J Med 1995;332:855–9. 10.1056/NEJM199503303321304 [DOI] [PubMed] [Google Scholar]
- 35. Chappell CL, Okhuysen PC, Sterling CR, et al. Infectivity of Cryptosporidium Parvum in healthy adults with pre-existing anti-C. Parvum serum immunoglobulin G. Am J Trop Med Hyg 1999;60:157–64. 10.4269/ajtmh.1999.60.157 [DOI] [PubMed] [Google Scholar]
- 36. Chappell CL, Okhuysen PC, Langer-Curry R, et al. Cryptosporidium Hominis: experimental challenge of healthy adults. Am J Trop Med Hyg 2006;75:851–7. [PubMed] [Google Scholar]
- 37. Jumani RS, Blais J, Tillmann H-C, et al. Opportunities and challenges in developing a Cryptosporidium controlled human infection model for testing Antiparasitic agents. ACS Infect Dis 2021;7:959–68. 10.1021/acsinfecdis.1c00057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hasan MM, Stebbins EE, Choy RKM, et al. Spontaneous selection of Cryptosporidium drug resistance in a calf model of infection. Antimicrob Agents Chemother 2021;65:e00023-21. 10.1128/AAC.00023-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Shaw H, ed. A reduction in weight gain in beef calves with clinical Cryptosporidiosis. In: Apicowplexa. La Escorial, Spain, 2017. [Google Scholar]
- 40. Shaw HJ, Innes EA, Morrison LJ, et al. Long-term production effects of clinical Cryptosporidiosis in neonatal calves. Int J Parasitol 2020;50:371–6. 10.1016/j.ijpara.2020.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Santin M. Cryptosporidium and Giardia in ruminants. Vet Clin North Am Food Anim Pract 2020;36:223–38. 10.1016/j.cvfa.2019.11.005 [DOI] [PubMed] [Google Scholar]
- 42. Ashigbie PG, Shepherd S, Steiner KL, et al. Use-case scenarios for an anti-Cryptosporidium therapeutic. PLoS Negl Trop Dis 2021;15:e0009057. 10.1371/journal.pntd.0009057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Amadi B, Mwiya M, Sianongo S, et al. High dose prolonged treatment with Nitazoxanide is not effective for Cryptosporidiosis in HIV positive Zambian children: a randomised controlled trial. BMC Infect Dis 2009;9:195. 10.1186/1471-2334-9-195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Choy RKM, Huston CD. Cryptosporidiosis should be designated as a tropical disease by the US food and Drug Administration. PLoS Negl Trop Dis 2020;14:e0008252. 10.1371/journal.pntd.0008252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Webb P, Stordalen GA, Singh S, et al. Hunger and malnutrition in the 21st century. BMJ 2018;361:k2238. 10.1136/bmj.k2238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Bitilinyu-Bangoh J, Voskuijl W, Thitiri J, et al. Performance of three rapid diagnostic tests for the detection of Cryptosporidium Spp. and Giardia Duodenalis in children with severe acute malnutrition and diarrhoea. Infect Dis Poverty 2019;8:96. 10.1186/s40249-019-0609-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Jain A, Shah D, Das S, et al. Aetiology and outcome of acute diarrhoea in children with severe acute malnutrition: a comparative study. Public Health Nutr 2020;23:1563–8. 10.1017/S1368980019003069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Opintan JA, Newman MJ, Ayeh-Kumi PF, et al. Pediatric diarrhea in Southern Ghana: etiology and association with intestinal inflammation and malnutrition. Am J Trop Med Hyg 2010;83:936–43. 10.4269/ajtmh.2010.09-0792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Amoo JK, Akindele AA, Amoo AOJ, et al. Prevalence of Enteric parasitic infections among people living with HIV in Abeokuta, Nigeria. Pan Afr Med J 2018;30:66. 10.11604/pamj.2018.30.66.13160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Costa D, Razakandrainibe R, Sautour M, et al. Human Cryptosporidiosis in immunodeficient patients in France (2015-2017). Exp Parasitol 2018;192:108–12. 10.1016/j.exppara.2018.08.001 [DOI] [PubMed] [Google Scholar]
- 51. Sepahvand F, Mamaghani AJ, Ezatpour B, et al. Gastrointestinal parasites in immunocompromised patients; A comparative cross-sectional study. Acta Trop 2022;231:106464. 10.1016/j.actatropica.2022.106464 [DOI] [PubMed] [Google Scholar]
- 52. Wanyiri JW, Kanyi H, Maina S, et al. Cryptosporidiosis in HIV/AIDS patients in Kenya: clinical features, epidemiology, molecular characterization and antibody responses. Am J Trop Med Hyg 2014;91:319–28. 10.4269/ajtmh.13-0254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Wang Z-D, Liu Q, Liu H-H, et al. Prevalence of Cryptosporidium, Microsporidia and Isospora infection in HIV-infected people: a global systematic review and meta-analysis. Parasit Vectors 2018;11:28. 10.1186/s13071-017-2558-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Abubakar I, Aliyu SH, Arumugam C, et al. Treatment of Cryptosporidiosis in immunocompromised individuals: systematic review and meta-analysis. Br J Clin Pharmacol 2007;63:387–93. 10.1111/j.1365-2125.2007.02873.x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data are available.