Abstract
Purpose
The purpose of this study was to evaluate practice patterns of a single surgeon with respect to meniscectomy and meniscal repair over a 20-year period at a single institution.
Methods
A cross-sectional descriptive study was carried out by reviewing the surgical data from the past 20 years (2002-2021) of patients who underwent arthroscopic primary meniscal surgery. Age, sex, knee and meniscus affected, morphology of the meniscal tear, meniscal radial location, location on the axial plane, tissue quality, and associated injuries were recorded. An analysis of the evolution of the characteristics of the meniscal lesions was performed according to the presence of degenerative tissue, the repairability of the lesion, and the treatment performed. Categorical data were represented in contingency tables and compared using the χ2 test for significance of differences, which was set at P < .05.
Results
In total, 1,892 cases were included. A decrease in degenerative meniscal tears was found, from 63.2 in 2002 to 2006 to 9.7% in 2017 to 2021 (P < .001), while repairable tears increased from 1.6% to 82.3% P < .001); in the same periods, arthroscopic partial meniscectomy procedures declined from 75.7% to 17.7% (P < .001) while meniscal repair increased from 0.4% to 81.3% (P < .001). All types of tears increased significantly their repairability, although longitudinal tears, root tears, and ramp lesions showed the highest possibilities for repair.
Conclusions
In the present study, a drastic change in the attitude toward meniscal preservation in the past 20 years was observed, with a large increase in the proportion of tears considered repairable found in primary arthroscopic surgery (to 80% of cases) and a decrease in degenerative meniscus tears (to less than 10%).
Clinical Relevance
In the past 2 decades, arthroscopic knee surgery has evolved such that more meniscus tears are deemed repairable, and fewer tears considered degenerative are indicated for arthroscopy.
Meniscal tears can be divided into 2 different types, according to the way they are generated: traumatic tears happen after an accident in which the knee exceeds its limits while degenerative meniscus tears (DMTs) happen insidiously and progressively.1 Although there is a wide variety of different meniscal tears, combining aspects of both traumatic and degenerative types, their treatment has traditionally been surgical in both situations and mainly by performing arthroscopic partial meniscectomy (APM),2 although meniscal repair was already a well-established tool 20 years ago.3
In the past years, the attitude toward the treatment of meniscal tears has shifted to a more conservative approach,4 as the benefits of meniscal repair (MR) are well known5; the concept of meniscal repairability has evolved along the years, and more and more indications for MR are considered nowadays (including root tears, ramp lesions, or older patients, among others), broadening the possibilities for surgical conservation of the menisci.6 Some national data show an increase in such procedures,7 although none of them exceeds 30% of MR indications; for this reason, a more aggressive behavior toward meniscal preservation seems possible and necessary.
The aim of the present study was to evaluate practice patterns of a single surgeon with respect to meniscectomy and meniscal repair over a 20-year period at a single institution; we hypothesized that the proportion of meniscal tears considered repairable (RTs) and repaired has increased over the past 20 years.
Methods
The present work was carried out following the guide principles from the Declaration of Helsinki (last amendment in Fortaleza 2013)8 and the Standards for Good Clinical Practice.9 Personal data were handled according to the Regulation (EU) 2016/679 from the European Parliament and Council from April 27, 2017, relative to the protection of natural persons regarding the treatment of personal data and their free circulation,10 and the Organic law 3/2018, from December 5, 2018, about the protection of personal data and guarantee of digital rights.11 A preprint version of the present study has been previously published on a preprint server.
A cross-sectional descriptive study was carried out by reviewing a database with data obtained from the surgical notes of the past 20 years (2002-2021) from patients who underwent arthroscopic knee surgery in a knee surgery specialized center, by the senior author (A.E.-B.), who has more than 30 years of experience in sports medicine and knee surgery; the data were compiled in a specific model for knee arthroscopy in which all the data from the patients, the meniscal tears and associated injuries (which will be further described), and the treatment performed were recorded and where a demonstrative drawing was added to clarify the lesion and the procedure; this model is similar to the one published by the Meniscal Documentation Committee of the International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine.12 All patients had signed an informed consent prior to surgery allowing the use of their clinical data for scientific purposes.
The patients included in this study were those subjected to primary meniscal surgery. Those with previous surgery on the same knee, whether on the menisci or other intraarticular structure, were excluded.
Several sociodemographic and clinical variables were assessed: age (measured in years and stratified in 4 groups for comparative purposes: 0-15, 16-30, 31-45, and >45 years), sex (male or female), knee (right or left) and meniscus (medial or lateral) affected, morphology of the meniscal tear (longitudinal, horizontal, radial, flap, root avulsion, ramp lesion, or complex), meniscal radial location (zone 1: periphery; zone 2: middle third; zone 3: free edge), and location on the axial plane (anterior horn, middle third, posterior horn, or miscellaneous segments of the meniscus); all the variables described were compiled in a model specifically designed for knee arthroscopy.
Tissue quality (i.e., degenerative or nondegenerative; all DMTs were considered complex, and the presence of degenerative tissue discarded the possibility of repair) was registered, as well as the presence of accompanying injuries. Meniscal tears considered RTs were the longitudinal ones in zones 1 and 2, ramp lesions, root avulsions (except those with very degenerative tissue), and those radial and horizontal that reached zone 1. Bucket handle tears were considered longitudinal tears. Other types of meniscal tears apart from the ones described might have the potential for healing (namely, complex tears in very young patients), so they were only considered RTs when they were repaired. The moment of the surgery was recorded in terms of years and stratified in groups of 5 years (2002-2006, 2007-2011, 2012-2016, 2017-2021) for comparative purposes. The treatment performed in each case was registered as APM, benign neglect, suture, rasping, sealing, reinsertion, and a combination of more than one—namely, suture plus APM, suture plus reinsertion, and reinsertion plus APM. Those treatment options were compiled into 3 groups for comparative purposes: APM alone, MR (including reinsertion and the combinations previously stated), and other conservative surgical procedures (rasping alone, sealing with electrofrequency, and benign neglect).
All the characteristics were extracted from a database built in a Microsoft Excel 2010 spreadsheet, which was anonymized by a person not related with the study (Francisca Balagué Jerez). The review of the data was performed by a single orthopaedic surgeon (A.E.-R.), who is specialized in arthroscopic knee surgery.
Statistical Analysis
A descriptive analysis of the variables described previously was carried out and presented in terms of frequency. Categorical data were represented in contingency tables and compared using the χ2 test for significance of differences. The presence of DMTs was compared according to the moment of the surgery to check the evolution in the past 20 years, as well as the presence of a RT and the treatment performed. The level of statistical significance was set at P < .05. The data analysis was performed using the IBM SPSS statistics application, version 20.0 (SPSS).
Results
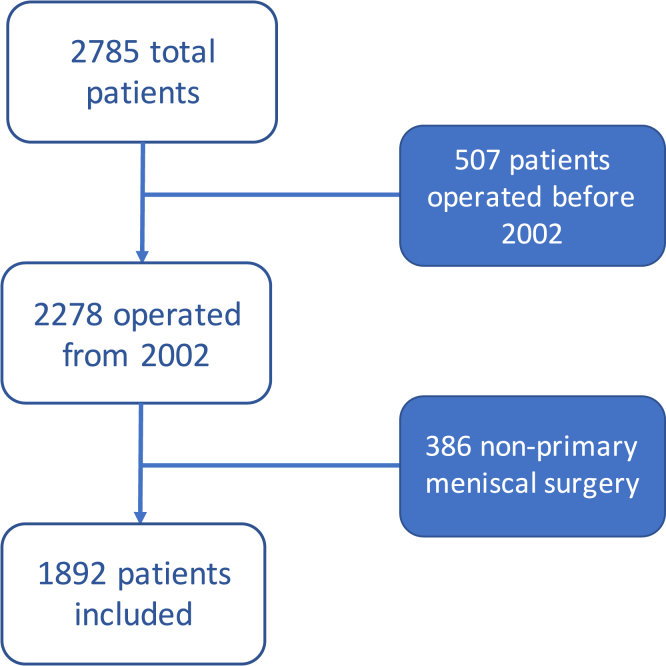
A total of 1,892 patients met the criteria for inclusion in the present study and underwent data analysis (Fig 1). The general demographic and clinical distribution of the patients is shown in Table 1. Mean (SD) age was 36.21 (13.628) years (range, 7-76 years). Surgery in males was more frequent than in females (3:1). The main group of patients operated on was between 31 and 45 years old (40.6%). The right knee (53.9%), the medial meniscus (59.1%), the posterior horn (61.7%), and zone 1 (52.9%) were the most frequent locations for meniscal tears found in the general data. Longitudinal tears (40.2%) were the most prevalent type of tear; the most commonly performed treatment in general was APM (63.6%).
Fig. 1.
Flowchart showing the selection of the patients. A total of 2,785 surgical reports were reviewed: 507 were discarded because they were operated on before 2002, while 386 of the remaining 2,278 were discarded because their surgery did not imply a primary meniscal surgery.
Table 1.
Demographical and Clinical Distribution of Patients
| Characteristic | N | % |
|---|---|---|
| Total | 1,892 | 100 |
| Date of surgery | ||
| 2002-2006 | 247 | 13 |
| 2007-2011 | 548 | 29 |
| 2012-2016 | 583 | 30.8 |
| 2017-2021 | 514 | 27.2 |
| Sex | ||
| Female | 459 | 24.3 |
| Male | 1433 | 75.7 |
| Age, y | ||
| <16 | 60 | 3.2 |
| 16-30 | 629 | 33.2 |
| 31-45 | 769 | 40.6 |
| >45 | 434 | 23 |
| Knee | ||
| Right | 1,019 | 53.9 |
| Left | 873 | 46.1 |
| Meniscus | ||
| Medial | 1118 | 59.1 |
| Lateral | 774 | 40.9 |
| Region | ||
| Anterior horn | 89 | 4.7 |
| Middle third | 176 | 9.3 |
| Posterior horn | 1167 | 61.7 |
| Miscellaneous | 460 | 24.3 |
| Zone | ||
| 1 | 1001 | 52.9 |
| 2 | 664 | 35.1 |
| 3 | 227 | 12 |
| Type of tear | ||
| Complex | 634 | 33.5 |
| Longitudinal (bucket handle) | 761 (178) | 40.2 (9.4) |
| Flap | 147 | 7.8 |
| Radial | 213 | 11.3 |
| Horizontal | 52 | 2.7 |
| Root avulsion | 71 | 3.7 |
| Ramp | 14 | 0.7 |
| Anterior cruciate ligament tear | ||
| Yes | 851 | 45 |
| No | 1,041 | 55 |
Degenerative Tears
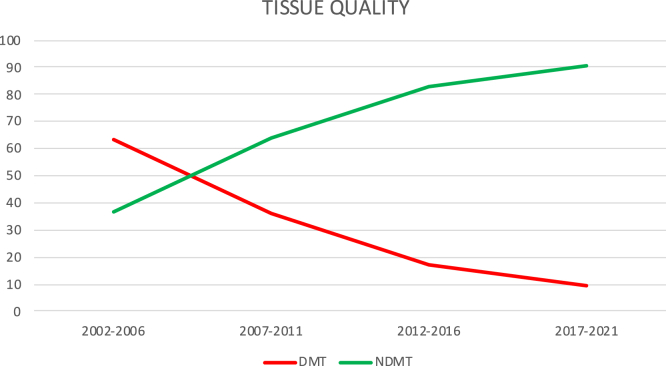
DMTs were present in 26.6% of the cases (Table 2); however, this percentage has significantly evolved through the years (from 63.2% in 2002-2006 to 9.7% in 2017-2021; Fig 2). Regarding sex (Tables 3 and 4), although the figures are lower in males in 2017 to 2021 (7.4 vs 15.9%; P < .05), the decrease was higher in female patients (61.1% vs 51.4%). Patients <30 years old had DMTs in less than 20% at all times. The main drop in DMTs happened in patients >45 years old (from 85.6% in 2002-2006 to 37.1%; P < .001). A just over 50% decrease in DMTs was found in both knees and both menisci. The peripheral zone and the posterior horn of the meniscus experimented the highest drop in DMTs, reaching 5.4% and 7.4%, respectively, in 2017 to 2021, while the anterior horn kept over 30% of DMT (P < .001). The percentage of DMT dropped in all of types of tears, with the longitudinal tears having a stronger decrease.
Table 2.
Evolution of Tissue Quality of Meniscal Tears Through the Past 20 Years
| Date | Tissue Quality, n (%)∗ |
Total, n | |
|---|---|---|---|
| Degenerative | Nondegenerative | ||
| 2002-2006 | 156 (63.2) | 91 (36.8) | 247 |
| 2007-2011 | 197 (35.9) | 351 (64.1) | 548 |
| 2012-2016 | 101 (17.3) | 482 (82.7) | 583 |
| 2017-2021 | 50 (9.7) | 464 (90.3) | 514 |
| Total | 504 (26.6) | 1,388 (73.4) | 1,892 |
Significant difference: P < .001.
Fig. 2.
General evolution of arthroscopic findings according to the quality of meniscal tissue. Diagram showing the evolution of meniscal tears in the past 20 years according to the presence of degenerative tissue. DMT, degenerative meniscus tear; NDMT, nondegenerative meniscus tear.
Table 3.
Evolution of Arthroscopic Findings According to the Quality of Meniscal Tissue Analyzed by Sex, Age, and Knee Affected
| Date | TQ | Sex, n (%) |
Age, n (%) |
Knee, n (%) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | P Value | <16 | 16-30 | 31-45 | >45 | P Value | Right | Left | P Value | ||
| 2002-2006 | NDMT | 77 (41.4) | 14 (23) | .01 | 4 (100) | 15 (68.2) | 56 (50.9) | 16 (14.4) | <.001 | 49 (38.9) | 42 (34.7) | .496 |
| DMT | 109 (58.6) | 47 (77) | 0 (0) | 7 (31.8) | 54 (49.1) | 95 (85.6) | 77 (61.1) | 79 (65.3) | ||||
| 2007-2011 | NDMT | 276 (68.1) | 75 (52.4) | .001 | 9 (81.8) | 140 (97.2) | 141 (63.8) | 61 (35.5) | <.001 | 176 (63.3) | 175 (64.8) | .713 |
| DMT | 129 (31.9) | 68 (47.6) | 2 (18.2) | 4 (2.8) | 80 (36.2) | 111 (64.5) | 102 (36.7) | 95 (35.2) | ||||
| 2012-2016 | NDMT | 381 (82.6) | 97 (82.9) | .941 | 21 (100) | 230 (88.8) | 203 (84.2) | 28 (45.2) | <.001 | 260 (83.6) | 222 (81.6) | .528 |
| DMT | 81 (17.4) | 20 (17.1) | 0 (0) | 29 (11.2) | 38 (15.8) | 34 (54.8) | 51 (16.4) | 50 (18.4) | ||||
| 2017-2021 | NDMT | 348 (92.6) | 116 (84.1) | .004 | 22 (91.7) | 200 (98) | 186 (94.4) | 56 (62.9) | <.001 | 274 (90.1) | 190 (90.5) | .897 |
| DMT | 28 (7.4) | 22 (15.9) | 2 (8.3) | 4 (2) | 11 (5.6) | 33 (37.1) | 30 (9.9) | 20 (9.5) | ||||
DMT, degenerative meniscus tear; NDMT, nondegenerative meniscus tear; TQ, tissue quality.
Table 4.
Evolution of Arthroscopic Findings According to the Quality of Meniscal Tissue Analyzed by Meniscus Affected, Zone and Region of the Lesion, and Type of Tear
| Date | TQ | Meniscus, n (%) |
Zone, n (%) |
Region, n (%) |
Type of Tear, n (%) |
P Value | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MED. | LAT. | P Value | 1 | 2 | 3 | P Value | MISC. | AH | MT | PH | P Value | COMP. | LONG. | FLAP | RADIAL | HORIZ. | ROOT | RAMP | |||
| 2002-2006 | NDMT | 57 (33.9) | 34 (43) | .166 | 24 (34.3) | 47 (36.4) | 20 (41.7) | .710 | 18 (30) | 4 (30.8) | 21 (60) | 48 (34.5) | .020 | 40 (26.5) | 5 (33.3) | 28 (66.7) | 14 (46.7) | 4 (44.4) | <.001 | ||
| DMT | 111 (66.1) | 45 (57) | 46 (65.7) | 82 (63.6) | 28 (58.3) | 42 (70) | 9 (69.2) | 14 (40) | 91 (65.5) | 111 (73.5) | 10 (66.7) | 14 (33.3) | 16 (53.3) | 5 (55.6) | |||||||
| 2007-2011 | NDMT | 216 (61.7) | 135 (68.2) | .130 | 217 (76.1) | 105 (54.7) | 29 (40.8) | <.001 | 123 (66.8) | 15 (50) | 25 (58.1) | 188 (64.6) | .274 | 50 (25.8) | 206 (93.6) | 24 (57.1) | 57 (79.2) | 11 (78.6) | 3 (50) | <.001 | |
| DMT | 134 (38.3) | 63 (31.8) | 68 (23.9) | 87 (45.3) | 42 (59.2) | 61 (33.2) | 15 (50) | 18 (41.9) | 103 (35.4) | 144 (74.2) | 14 (6.4) | 18 (42.9) | 15 (20.8) | 3 (21.4) | 3 (50) | ||||||
| 2012-2016 | NDMT | 237 (86.5) | 245 (79.3) | .022 | 241 (88.3) | 180 (82.9) | 61 (65.6) | <.001 | 119 (80.4) | 15 (50) | 58 (81.7) | 290 (86.8) | <.001 | 102 (54.5) | 224 (96.1) | 46 (100) | 80 (95.2) | 18 (90) | 11 (91.7) | 1 (100) | <.001 |
| DMT | 37 (13.5) | 64 (20.7) | 32 (11.7) | 37 (17.1) | 32 (34.4) | 29 (19.6) | 15 (50) | 13 (18.3) | 44 (13.2) | 85 (45.5) | 9 (3.9) | 0 (0) | 4 (4.8) | 2 (10) | 1 (8.3) | 0 (0) | |||||
| 2017-2021 | NDMT | 300 (92) | 164 (87.2) | .078 | 353 (94.6) | 98 (77.8) | 13 (86.7) | <.001 | 56 (82.4) | 11 (68.8) | 24 (88.9) | 373 (92.6) | .001 | 69 (67.6) | 284 (96.9) | 14 (82.4) | 25 (92.6) | 9 (100) | 50 (94.3) | 13 (100) | <.001 |
| DMT | 26 (8) | 24 (12.8) | 20 (5.4) | 28 (22.2) | 2 (13.3) | 12 (17.6) | 5 (31.3) | 3 (11.1) | 30 (7.4) | 33 (32.4) | 9 (3.1) | 3 (17.6) | 2 (7.4) | 0 (0) | 3 (5.7) | 0 (0) | |||||
AH, anterior horn; COMP., complex; DMT, degenerative meniscus tear; HORIZ., horizontal. LAT., lateral; LONG., longitudinal; MED., medial; MISC., miscellaneous regions affected; MT, middle third; NDMT, nondegenerative meniscus tear; PH, posterior horn; TQ, tissue quality.
Repairable Tears
RTs represented 49.2% of the cases (Table 5), but they evolved from 1.6% in 2002 to 2006 to 82.3% in 2017 to 2021 (P < .001). Males and females experienced an increase >80% in RTs (Tables 6 and 7), which rose >90% in the group between 16 and 30 years old and reached 50% in the group >45 years old in 2017 to 2021. No statistical differences were found between both legs and both menisci (except in 2012-2016, when the RTs of the lateral meniscus declined). An increment of RTs of almost 90% was found in zone 1 while an 86.4% increase was found in the posterior horn, which were the most common locations for RTs (P < .001). Longitudinal and horizontal tears, root avulsions, and ramp lesions were the most repairable ones in 2017 to 2021. Complex tears underwent a rise in RTs of almost 40%, and flap tears showed their first RTs in the same period.
Table 5.
Evolution of Meniscal Tears Through the Past 20 Years According to the Possibility of Repair and According to the Treatment Performed
| Date | Possibility to Repair, n (%)∗ |
Treatment, n (%)∗ |
Total | |||
|---|---|---|---|---|---|---|
| Repairable | Nonrepairable | Meniscectomy | Meniscal Repair | Other | ||
| 2002-2006 | 4 (1.6) | 243 (98.4) | 187 (75.7) | 1 (0.4) | 59 (23.9) | 247 |
| 2007-2011 | 248 (45.3) | 300 (54.7) | 501 (91.4) | 16 (2.9) | 31 (5.7) | 548 |
| 2012-2016 | 255 (43.7) | 328 (56.3) | 425 (72.9) | 108 (18.5) | 50 (8.6) | 583 |
| 2017-2021 | 423 (82.3) | 91 (17.7) | 91 (17.7) | 418 (81.3) | 5 (1) | 514 |
| Total | 930 (49.2) | 962 (50.8) | 1,204 (63.6) | 543 (28.7) | 145 (7.7) | 1,892 |
Significant difference: P < .001.
Table 6.
Evolution of Arthroscopic Findings According to the Repairability of the Meniscal Tear Analyzed by Sex, Age, and Knee Affected
| Date | Repairability | Sex, n (%) |
Age, n (%) |
Knee, n (%) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | P Value | <16 | 16-30 | 31-45 | >45 | P Value | Right | Left | P Value | ||
| 2002-2006 | RT | 4 (2.2) | 0 (0) | .248 | 1 (25) | 1 (4.5) | 2 (1.8) | 0 (0) | .001 | 2 (1.6) | 2 (1.7) | .967 |
| NRT | 182 (97.8) | 61 (100) | 3 (75) | 21 (95.5) | 108 (98.2) | 111 (100) | 124 (98.4) | 119 (98.3) | ||||
| 2007-2011 | RT | 202 (49.9) | 46 (32.2) | <.001 | 6 (54.5) | 114 (79.2) | 86 (38.9) | 42 (24.4) | <.001 | 123 (44.2) | 125 (46.3) | .630 |
| NRT | 203 (50.1) | 97 (67.8) | 5 (45.5) | 30 (20.8) | 135 (61.1) | 130 (75.6) | 155 (55.8) | 145 (53.7) | ||||
| 2012-2016 | RT | 190 (40.8) | 65 (55.6) | .004 | 13 (61.9) | 135 (52.1) | 94 (39) | 13 (21) | <.001 | 138 (44.4) | 117 (43) | .742 |
| NRT | 276 (59.2) | 52 (44.4) | 8 (38.1) | 124 (47.9) | 147 (61) | 49 (79) | 173 (55.6) | 155 (57) | ||||
| 2017-2021 | RT | 311 (82.7) | 112 (81.2) | .683 | 23 (95.8) | 195 (95.6) | 160 (81.2) | 45 (50.6) | <.001 | 244 (80.3) | 179 (85.2) | .146 |
| NRT | 65 (17.3) | 26 (18.8) | 1 (4.2) | 9 (4.4) | 37 (18.8) | 44 (49.4) | 60 (19.7) | 31 (14.8) | ||||
NRT, nonrepairable meniscus tear; RT, repairable meniscus tear.
Table 7.
Evolution of Arthroscopic Findings According to the Repairability of the Meniscal Tear Analyzed by Meniscus Affected, Zone and Region of the Lesion and Type of Tear
| Date | Repairability | Meniscus, n (%) |
Zone, n (%) |
Region, n (%) |
Type of Tear, n (%) |
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MED. | LAT. | P Value | 1 | 2 | 3 | P Value | MISC. | AH | MT | PH | P Value | COMP. | LONG. | FLAP | RADIAL | HORIZ. | ROOT | RAMP | P Value | ||
| 2002-2006 | RT | 3 (1.8) | 1 (1.3) | .763 | 3 (4.3) | 1 (0.8) | 0 (0) | <.001 | 0 (0) | 0 (0) | 4 (11.4) | 0 (0) | <.106 | 0 (0) | 2 (13.3) | 0 (0) | 2 (6.7) | 0 (0) | <.001 | ||
| NRT | 165 (98.2) | 78 (98.7) | 67 (95.7) | 128 (99.2) | 48 (100) | 60 (100) | 13 (100) | 31 (88.6) | 139 (100) | 151 (100) | 13 (86.7) | 42 (100) | 28 (93.3) | 9 (100) | |||||||
| 2007-2011 | RT | 165 (47.1) | 83 (41.9) | .238 | 197 (69.1) | 51 (25.6) | 0 (0) | <.001 | 104 (56.5) | 11 (36.7) | 6 (14) | 127 (43.6) | <.001 | 5 (2.6) | 201 (91.4) | 0 (0) | 29 (40.3) | 10 (71.4) | 3 (50) | <.001 | |
| NRT | 185 (52.9) | 115 (58.1) | 88 (30.9) | 141 (74.4) | 71 (100) | 80 (43.5) | 19 (63.3) | 37 (86) | 164 (56.4) | 189 (97.4) | 19 (8.6) | 42 (100) | 43 (59.7) | 4 (28.6) | 3 (50) | ||||||
| 2012-2016 | RT | 171 (62.4) | 84 (27.2) | .<.001 | 172 (63) | 82 (37.8) | 1 (1.1) | <.001 | 76 (51.4) | 8 (26.7) | 7 (9.9) | 164 (49.1) | <.001 | 7 (3.7) | 219 (94) | 0 (0) | 13 (15.5) | 8 (40) | 7 (58.3) | 1 (100) | <.001 |
| NRT | 103 (37.6) | 225 (72.8) | 101 (37) | 135 (62.2) | 92 (98.9) | 72 (48.6) | 22 (73.3) | 64 (90.1) | 170 (50.9) | 180 (96.3) | 14 (6) | 46 (100) | 71 (84.5) | 12 (60) | 5 (41.7) | 0 (0) | |||||
| 2017-2021 | RT | 271 (83.1) | 152 (80.9) | .515 | 351 (94.1) | 71 (56.3) | 1 (6.7) | <.001 | 55 (80.9) | 7 (43.8) | 13 (48.1) | 348 (86.4) | <.001 | 43 (42.2) | 288 (98.3) | 2 (11.8) | 19 (70.4) | 9 (100) | 52 (98.1) | 13 (100) | <.001 |
| NRT | 55 (16.9) | 36 (19.1) | 22 (5.9) | 55 (43.7) | 14 (93.3) | 13 (19.1) | 9 (56.3) | 14 (51.9) | 55 (13.6) | 59 (57.8) | 5 (1.7) | 15 (88.2) | 8 (29.6) | 0 (0) | 1 (1.9) | 0 (0) | |||||
AH, anterior horn; COMP., complex; HORIZ., horizontal; LAT., lateral; LONG., longitudinal; MED., medial; MISC., miscellaneous regions affected; MT, middle third; NRT, nonrepairable meniscus tear; PH, posterior horn; RT, repairable meniscus tear.
Treatment
MR raised from 0.4% to 81.3% (Table 5; Fig 3) in 2017 to 2021, matching the figures of RT (82.3%; .001). No significant differences were found in terms of sex and knee treated; other treatments, which accounted 21.5% for the period 2002 to 2006, almost disappeared in 2017 to 2021 (Tables 8 and 9). MR surpassed 95% in 2017 to 2021 in patients <30 years old (P < .001), while APM was slightly over 50% in patients >45 years old. The treatment performed on both menisci was different before 2017 to 2021 (more APMs on the medial meniscus [1.4:1], more conservative treatments different from MR on the lateral one [2.5:1]; P < .001); in 2017 to 2021, the figures for both menisci matched due especially to the increase in MR. APM in zone 3 dropped from 20.1% of the cases in 2002 to 2006 to 2.9% (only 15 cases) in 2017 to 2021; on the other hand, MR increased from 0% to 93% (P < .001) in zone 1, while the proportion of tears in this zone increased from 28.3% in 2002 to 2006 to 72.6% in 2017 to 2021. All zones rose for MR, surpassing 80% on the posterior horn and when several regions were affected (P < .001). All kinds of tears expanded their rates of MR from 2002 to 2006 and 2017 to 2021; the main case was longitudinal tears, which reached 98%, as well as root tears. APM declined in radial and horizontal tears from 66.7% to 37% and 22.2%, respectively (P < .001).
Fig. 3.
General evolution of repairable meniscal tears and meniscal repairs performed. Diagram showing the general evolution of repairable meniscal tears (RTs) found during knee arthroscopy during the past 20 years and the evolution of the meniscal repairs performed (MRs).
Table 8.
Evolution of Arthroscopic Findings According to the Treatment Performed on Meniscal Tears Analyzed by Sex, Age, and Knee Affected
| Date | Treatment | Sex, n (%) |
Age, n (%) |
Knee, n (%) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | P Value | <16 | 16-30 | 31-45 | >45 | P Value | Right | Left | P Value | ||
| 2002-2006 | APM | 147 (79) | 40 (65.6) | .074 | 3 (75) | 14 (63.6) | 92 (83.6) | 78 (70.3) | <.001 | 100 (79.4) | 87 (71.9) | .204 |
| MR | 1 (0.5) | 0 (0) | 1 (25) | 0 (0) | 0 (0) | 0 (0) | 1 (0.8) | 0 (0) | ||||
| Other | 38 (20.5) | 21 (34.4) | 0 (0) | 8 (36.4) | 18 (16.4) | 33 (29.7) | 25 (19.8) | 34 (28.1) | ||||
| 2007-2011 | APM | 373 (92.1) | 128 (89.5) | .443 | 7 (63.6) | 126 (87.5) | 208 (94.1) | 160 (93) | <.001 | 254 (91.4) | 247 (91.5) | .768 |
| MR | 11 (2.7) | 5 (3.5) | 3 (27.3) | 6 (4.2) | 3 (1.4) | 4 (2.3) | 11 (3.9) | 5 (1.8) | ||||
| Other | 21 (5.2) | 10 (7) | 1 (9.1) | 12 (8.3) | 10 (4.5) | 8 (4.7) | 13 (4.7) | 18 (6.7) | ||||
| 2012-2016 | APM | 349 (74.9) | 76 (65) | .136 | 9 (42.9) | 172 (66.4) | 187 (77.6) | 57 (91.9) | <.001 | 216 (69.5) | 209 (76.8) | .300 |
| MR | 78 (16.7) | 30 (25.6) | 10 (47.6) | 68 (26.3) | 29 (12) | 1 (1.6) | 63 (20.3) | 45 (16.6) | ||||
| Other | 39 (8.4) | 11 (9.4) | 2 (9.5) | 19 (7.3) | 21 (10.4) | 4 (6.5) | 32 (10.2) | 18 (6.6) | ||||
| 2017-2021 | APM | 64 (17) | 27 (19.6) | .830 | 1 (4.2) | 8 (3.9) | 36 (18.3) | 46 (51.7) | <.001 | 60 (19.7) | 31 (14.8) | .215 |
| MR | 307 (81.7) | 111 (80.4) | 23 (95.8) | 194 (95.1) | 158 (80.2) | 43 (48.3) | 241 (79.3) | 177 (84.3) | ||||
| Other | 5 (1.3) | 0 (0) | 0 (0) | 2 (1) | 2 (1.5) | 0 (0) | 3 (1) | 2 (0.9) | ||||
APM, arthroscopic partial meniscectomy; MR, meniscal repair; Other, other conservative treatments different from repair.
Table 9.
Evolution of Arthroscopic Findings According to the Treatment Performed on Meniscal Tears Analyzed by Meniscus Affected, Zone and Region of the Lesion, and Type of Tear
| Date | Treatment | Meniscus, n (%) |
Zone, n (%) |
Region, n (%) |
Type of Tear, n (%) |
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MED. | LAT. | P Value | 1 | 2 | 3 | P Value | MISC. | AH | MT | PH | P Value | COMP. | LONG. | FLAP | RADIAL | HORIZ. | ROOT | RAMP | P Value | ||
| 2002-2006 | APM | 140 (83.3) | 47 (59.5) | <.001 | 61 (87.1) | 107 (82.9) | 19 (39.6) | <.001 | 44 (73.3) | 7 (53.8) | 21 (60) | 115 (82.7) | .009 | 111 (73.5) | 10 (66.7) | 40 (95.2) | 20 (66.7) | 6 (66.7) | .001 | ||
| MR | 1 (0.6) | 0 (0) | 0 (0) | 1 (0.8) | 0 (0) | 0 (0) | 0 (0) | 1 (2.9) | 0 (0) | 0 (0) | 1 (6.7) | 0 (0) | 0 (0) | 0 (0) | |||||||
| Other | 27 (16.1) | 32 (40.5) | 9 (12.9) | 21 (16.3) | 29 (60.4) | 16 (26.7) | 6 (46.2) | 13 (37.1) | 24 (17.3) | 40 (26.5) | 4 (26.7) | 2 (4.8) | 10 (33.3) | 3 (33.3) | |||||||
| 2007-2011 | APM | 337 (96.3) | 164 (82.8) | <.001 | 260 (91.2) | 187 (97.4) | 54 (76.1) | <.001 | 175 (95.1) | 15 (50) | 35 (81.4) | 276 (94.8) | <.001 | 172 (88.7) | 207 (94.1) | 42 (100) | 65 (90.3) | 14 (100) | 1 (16.7) | <.001 | |
| MR | 2 (0.6) | 14 (7.1) | 14 (4.9) | 2 (1) | 0 (0) | 0 (0) | 11 (36.7) | 5 (11.6) | 0 (0) | 5 (2.6) | 4 (1.8) | 0 (0) | 4 (5.6) | 0 (0) | 3 (50) | ||||||
| Other | 11 (3.1) | 20 (10.1) | 11 (3.9) | 3 (1.6) | 17 (23.9) | 9 (4.9) | 4 (13.3) | 3 (7) | 15 (5.2) | 17 (8.7) | 9 (4.1) | 0 (0) | 3 (4.2) | 0 (0) | 2 (33.3) | ||||||
| 2012-2016 | APM | 180 (65.7) | 245 (79.3) | <.001 | 169 (61.9) | 179 (82.5) | 77 (82.8) | <.001 | 128 (86.5) | 20 (66.7) | 57 (80.3) | 220 (65.9) | <.001 | 169 (90.4) | 121 (51.9) | 46 (100) | 69 (82.1) | 19 (95) | 1 (8.3) | 0 (0) | <.001 |
| MR | 83 (30.3) | 25 (8) | 87 (31.9) | 20 (9.2) | 1 (1.1) | 16 (10.8) | 7 (23.3) | 4 (5.7) | 81 (24.2) | 7 (3.7) | 91 (39.1) | 0 (0) | 2 (2.4) | 0 (0) | 7 (58.3) | 1 (100) | |||||
| Other | 11 (4) | 39 (12.7) | 17 (6.2) | 18 (8.3) | 15 (16.1) | 4 (2.7) | 3 (10) | 10 (14) | 33 (9.9) | 11 (5.9) | 21 (9) | 0 (0) | 13 (15.5) | 1 (5) | 4 (33.4) | 0 (0) | |||||
| 2017-2021 | APM | 57 (17.5) | 34 (18.1) | <.001 | 23 (6.2) | 55 (43.7) | 13 (86.6) | <.001 | 13 (19.1) | 9 (56.3) | 15 (55.6) | 54 (13.4) | <.001 | 58 (56.9) | 4 (1.4) | 15 (88.2) | 10 (37) | 2 (22.2) | 1 (1.9) | 0 (0) | <.001 |
| MR | 267 (81.9) | 151 (80.3) | 346 (93) | 71 (56.3) | 1 (6.7) | 55 (80.9) | 7 (43.8) | 12 (44.4) | 344 (85.4) | 43 (42.1) | 287 (98) | 2 (11.8) | 17 (63) | 7 (87.8) | 52 (98.1) | 10 (76.9) | |||||
| Other | 2 (0.6) | 3 (1.6) | 4 (1.1) | 0 (0) | 1 (6.7) | 0 (0) | 0 (0) | 0 (0) | 5 (1.2) | 1 (1) | 2 (0.6) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 3 (23.1) | |||||
AH, anterior horn; APM, arthroscopic partial meniscectomy; COMP., complex; HORIZ., horizontal; LAT., lateral; LONG., longitudinal; MED., medial; MISC., miscellaneous regions affected; MR, meniscal repair; MT, middle third; Other, other conservative treatments different from repair; PH, posterior horn.
Discussion
The most important finding of the present study was that a shift toward meniscal preservation has been established in the authors’ practice for the past 20 years, confirming our hypothesis; an increase in the amount of RT found in primary arthroscopic surgery from 1.6% from 2002 to 2006 to 82.3% in 2017 to 2021 was shown, matching the figures for conservative surgery (including MR and other conservative options). Furthermore, meniscal surgery on DMTs decreased from 63.2% in the 2002 to 2006 period to 9.7% between 2017 and 2021 (6.5:1).
APM has been the most frequent surgical treatment in meniscal tears for many years,13 becoming almost a part of the popular knowledge, so changing such practice is difficult,14,15 probably because it means not only a shift in scientific evidence but also a cultural change in surgeons’ and patients’ minds. However, although still too mild, some green sprouts in the decrease of APM can be seen in literature,16 especially in patients older than 50 years, similar to the data published in the present study.
APM on DMTs has shown not to improve outcomes from conservative treatment,17 or from sham surgery,18,19 so it has been proposed that it should not be performed as a first-line treatment, but only after failure of nonsurgical procedures.17,20 Subsequently, the goal when treating DMTs should be to decrease the incidence of surgical treatment and, furthermore, taking into account that DMTs are less likely to be repaired because of their lower healing potential and the technical complexity. Such change could be seen in the present study and since 2002 to 2006, but it has increased in the past 10 years, enhanced by the emerging works19, 20, 21 that provided scientific evidence that guides physicians and patients to treat degenerative tears nonoperatively.
On the other hand, a decrease in the proportion of arthroscopic surgery in DMTs would increase the percentage of RTs treated, as seen in this study. The general percentage of RTs (49.2%) is higher than previously published data,6,22 probably because in the present article, only the cases operated on during the past 20 years were included; however, the most interesting aspect found is the growing proportion of RTs through the years. Such rise in the presence of RTs during meniscal surgery has a diverse origin: while age may have previously been used as a hard contraindication to meniscal repair, the indications have continued to expand and evolve for middle-aged patients with nondegenerative tears23; it is very stimulating to check that more than 95% of the tears in patients under 30 years old were considered repairable in 2017 to 2021, while it occurred in more than 50% in patients over 45 years old: such proportions are very high in both cases, compared to Espejo-Reina et al.6 and Fetzer et al.,22 although the latter figures may be improvable in the future, also fueled by the improvements in MR technology.
Another reason for the rise in RTs is their location: tears in zone 1 increased their incidence from 28.3% to 72.6%, while treatment shifted from 87.1% of APM in that zone to 93% of MR; such change in the percentage of tears in zone 1 depends mainly on the change of indications for surgical treatment, which caused a great decrease in tears in zones 2 and 3 (usually more degenerative). Also, the improvement and availability of meniscal suture devices must have influenced the shift of the very poor 87% of APM in 2002 to 2006 to the 93% of MR in 2017 to 2021. Tears in zone 2 reached 56.3% of MR while tears in zone 3 almost disappeared (2.9%). According to the type of tear, longitudinal tears became almost repairable per se through the years, reaching 98% of the cases; bucket handle tears (9.4% of all longitudinal tears) were included as longitudinal tears in the present study because, although having less healing potential than those, their repair is justified.24,25
Root tears and ramp lesions, which have been “discovered” in the past 10 years, added new indications for MR26, 27, 28: in the present study, both of them were considered repairable in >98% of the cases and were not subjected to APM in the same proportion. Furthermore, the indications of MR in radial29 and horizontal30 tears have also risen due to the new evidence that justifies such a procedure; development of the knowledge of the benefits of MR has also allowed surgeons to explore its limits, and complex (42.2%) and flap (11.8%) tears also increased their repairability, more because they were repaired than due to the currently established indications. These limits were pushed especially in very young patients, who have a better healing potential and in whom the consequences of meniscectomy are more deleterious than in middle-aged or older patients: further studies on the outcomes of MR in those kinds of tears are warranted in the future.
MR has widely shown improved clinical outcomes compared to APM, with less progression to osteoarthritis24,31; furthermore, it has also proven higher cost-effectiveness32,33: Feeley et al.34 stated that a 10% decline in APM in favor of MR would result in $43 million savings per year. These data should encourage surgeons to perform less APMs and more MRs: a recent article7 studied the trends in meniscal surgical procedures in 4 different countries, confirming this tendency, with decreases in the proportion of APM between 16% and 30%, but the change still seems too mild. A survey in the same study demonstrated that 50% of the respondents repair less than 25% of the cases of root tears, a clear niche where MR indications can be risen, as shown here. The present study, although showing a low rate of MR in the first period, has demonstrated a similar trend but with a much more aggressive change toward the increase of MR (81.3% in the last period) and the decrease of APM (only a 17.7%). Moreover, in the last period, the figures for MR matched the ones for RTs, which would be the ideal situation. Other conservative treatments, like rasping or sealing, were frequent in 2002 to 2006 (23.9%); however, they almost disappeared through the years with the increase in MR, due to its great evolution and the improvement and availability of the technology necessary to perform it, as well as the drop in the surgical treatment of DMTs.
Other previous studies have also revealed a decrease in APM and an increase in meniscal repairs35,36 like in the present study; however, the changes presented seem low according to the current standards6 in general (<25% probability of repair). On the other hand, the trends presented by Wassenburger et al.35 are stronger in sports medicine–trained surgeons: the absence of official fellowship programs could explain that the trends seen in countries like France,37 Japan,38 or the United States39 are not reproduced in other countries.40
Limitations
This study is not without limitations. The data regarding ligament injuries, especially anterior cruciate ligament tears, were not completely available, so the authors decided not to use them for comparative purposes to avoid bias. Ramp lesions and root tears were only recorded during the last periods, so previous data were not available; however, the authors believed that such differentiation should be made in order to provide a complete view of the evolution of the kinds of tears found during knee arthroscopy. Moreover, further analysis on the specific types of root tears could be of interest. Since the study was conducted at 1 center, the results may not be generalizable to other populations. The study design of the present work does not allow for outcome assessment.
Conclusions
In the present study, a drastic change in the attitude toward meniscal preservation in the past 20 years was observed, with a large increase in the proportion of tears considered repairable found in primary arthroscopic surgery (to 80% of cases) and a decrease in DMTs (to <10%).
Acknowledgments
The authors thank Francisca Rius Díaz, associate professor from Universidad de Málaga, for her technical support in the field of statistics.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: This study was partially funded by the following: A.E.-B. and A.E.-R. receive personal fees as consultants from Stryker Iberia, independent from the present study.
All patients had signed an informed consent prior to surgery allowing the use of their clinical data for scientific purposes.
Supplementary Data
References
- 1.Beaufils P., Becker R., Kopf S., Matthieu O., Pujol N. The knee meniscus: Management of traumatic tears and degenerative lesions. EFORT Open Rev. 2017;2(5):195–203. doi: 10.1302/2058-5241.2.160056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abram S.G.F., Judge A., Beard D.J., Wilson H.A., Price A.J. Temporal trends and regional variation in the rate of arthroscopic knee surgery in England: Analysis of over 1.7 million procedures between 1997 and 2017. Has practice changed in response to new evidence? Br J Sports Med. 2019;53(24):1533–1538. doi: 10.1136/bjsports-2018-099414. [DOI] [PubMed] [Google Scholar]
- 3.McCarty E.C., Marx R.G., DeHaven K.E. Meniscus repair: Considerations in treatment and update of clinical results. Clin Orthop Relat Res. 2002;(402):122–134. [PubMed] [Google Scholar]
- 4.Parker B.R., Hurwitz S., Spang J., Creighton R., Kamath G. Surgical trends in the treatment of meniscal tears: Analysis of data from the American Board of Orthopaedic Surgery Certification Examination Database. Am J Sports Med. 2016;44(7):1717–1723. doi: 10.1177/0363546516638082. [DOI] [PubMed] [Google Scholar]
- 5.Totlis T., Haunschild E.D., Otountzidis N., et al. Return-to-sport rate and activity level are high following arthroscopic all-inside meniscal repair with and without concomitant anterior cruciate ligament reconstruction: A systematic review. Arthroscopy. 2021;37(7):2351–2360. doi: 10.1016/j.arthro.2021.02.046. [DOI] [PubMed] [Google Scholar]
- 6.Espejo-Reina A., Aguilera J., Espejo-Reina M.J., Espejo-Reina M.P., Espejo-Baena A. One-third of meniscal tears are repairable: An epidemiological study evaluating meniscal tear patterns in stable and unstable knees. Arthroscopy. 2019;35(3):857–863. doi: 10.1016/j.arthro.2018.08.051. [DOI] [PubMed] [Google Scholar]
- 7.Jacquet C., Mouton C., Becker R., et al. Does practice of meniscus surgery change over time? A report of the 2021 ‘THE MENISCUS’ Webinar. J Exp Orthop. 2021;8(1):46. doi: 10.1186/s40634-021-00365-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Medical Association World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 9.European Medicines Agency. Guideline for good clinical practice E6 (R2). European Medicines Agency. www.ema.europa.eu/en/ich-e6-r2-good-clinical-practice-scientific-guideline. Accessed September 14, 2022.
- 10.European Parliament, Council of the European Union Regulation (EU) 2016/679 of the European Parliament and of the council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC (General Data Protection Regulation) https://eur-lex.europa.eu/legal-content/ES/TXT/?uri=CELEX%3A32016R0679&qid=1611231121319
- 11.Spain. Ley Orgánica 3/2018, de 5 de diciembre, de Protección de Datos Personales y garantía de los derechos digitales. www.boe.es/eli/es/lo/2018/12/05/3
- 12.Anderson A.F., Irrgang J.J., Dunn W., et al. Interobserver reliability of the International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine (ISAKOS) classification of meniscal tears. Am J Sports Med. 2011;39(5):926–932. doi: 10.1177/0363546511400533. [DOI] [PubMed] [Google Scholar]
- 13.Abrams G.D., Frank R.M., Gupta A.K., Harris J.D., McCormick F.M., Cole B.J. Trends in meniscus repair and meniscectomy in the United States, 2005-2011. Am J Sports Med. 2013;41(10):2333–2339. doi: 10.1177/0363546513495641. [DOI] [PubMed] [Google Scholar]
- 14.Chan E.W., Chaulk R.C., Cheng Y., Shin J. No decrease in incidence of arthroscopic meniscectomy in a Canadian province. Knee Surg Sports Traumatol Arthrosc. 2021;29(12):4223–4231. doi: 10.1007/s00167-021-06534-7. [DOI] [PubMed] [Google Scholar]
- 15.Rongen J.J., van Tienen T.G., Buma P., Hannink G. Meniscus surgery is still widely performed in the treatment of degenerative meniscus tears in The Netherlands. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1123–1129. doi: 10.1007/s00167-017-4473-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Essilfie A., Kang H.P., Mayer E.N., Trasolini N.A., Alluri R.K., Weber A.E. Are orthopaedic surgeons performing fewer arthroscopic partial meniscectomies in patients greater than 50 years old? A national database study. Arthroscopy. 2019;35(4):1152–1159.e1. doi: 10.1016/j.arthro.2018.10.152. [DOI] [PubMed] [Google Scholar]
- 17.Rotini M., Papalia G., Setaro N., et al. Arthroscopic surgery or exercise therapy for degenerative meniscal lesions: A systematic review of systematic reviews. Musculoskelet Surg. 2023;107(2):127–141. doi: 10.1007/s12306-022-00760-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sihvonen R., Paavola M., Malmivaara A., et al. Arthroscopic partial meniscectomy versus placebo surgery for a degenerative meniscus tear: A 2-year follow-up of the randomised controlled trial. Ann Rheum Dis. 2018;77(2):188–195. doi: 10.1136/annrheumdis-2017-211172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sihvonen R., Paavola M., Malmivaara A., et al. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013;369(25):2515–2524. doi: 10.1056/NEJMoa1305189. [DOI] [PubMed] [Google Scholar]
- 20.Beaufils P., Becker R., Kopf S., et al. Surgical management of degenerative meniscus lesions: The 2016 ESSKA meniscus consensus. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):335–346. doi: 10.1007/s00167-016-4407-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Katz J.N., Brophy R.H., Chaisson C.E., De Chaves L., Cole B.J. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engl J Med. 2013;368(18):1675–1684. doi: 10.1056/NEJMoa1301408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fetzer G., Spindler K.P., Amendola A., et al. Potential market for new meniscus repair strategies: Evaluation of the MOON Cohort. J Knee Surg. 2009;22(3):180–186. doi: 10.1055/s-0030-1247746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Poland S., Everhart J.S., Kim W., Axcell K., Magnussen R.A., Flanigan D.C. Age of 40 years or older does not affect meniscal repair failure risk at 5 years. Arthroscopy. 2019;35(5):1527–1532. doi: 10.1016/j.arthro.2018.11.061. [DOI] [PubMed] [Google Scholar]
- 24.Kalifis G., Raoulis V., Panteliadou F., Liantsis A., D’Ambrosi R., Hantes M. Long-term follow-up of bucket-handle meniscal repairs: Chondroprotective effect outweighs high failure risk. Knee Surg Sports Traumatol Arthrosc. 2022;30(7):2209–2214. doi: 10.1007/s00167-021-06787-2. [DOI] [PubMed] [Google Scholar]
- 25.Costa G.G., Grassi A., Zocco G., et al. What is the failure rate after arthroscopic repair of bucket-handle meniscal tears? A systematic review and meta-analysis. Am J Sports Med. 2022;50(6):1742–1752. doi: 10.1177/03635465211015425. [DOI] [PubMed] [Google Scholar]
- 26.Bhatia S., Laprade C.M., Ellman M.B., Laprade R.F. Meniscal root tears: Significance, diagnosis, and treatment. Am J Sports Med. 2014;42(12):3016–3030. doi: 10.1177/0363546514524162. [DOI] [PubMed] [Google Scholar]
- 27.Chahla J., Dean C.S., Moatshe G., et al. Meniscal ramp lesions: Anatomy, incidence, diagnosis, and treatment. Orthop J Sport Med. 2016;4(7) doi: 10.1177/2325967116657815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Magosch A., Mouton C., Nührenbörger C., Seil R. Medial meniscus ramp and lateral meniscus posterior root lesions are present in more than a third of primary and revision ACL reconstructions. Knee Surg Sports Traumatol Arthrosc. 2021;29(9):3059–3067. doi: 10.1007/s00167-020-06352-3. [DOI] [PubMed] [Google Scholar]
- 29.Milliron E.M., Magnussen R.A., Cavendish P.A., Quinn J.P., DiBartola A.C., Flanigan D.C. Repair of radial meniscus tears results in improved patient-reported outcome scores: A systematic review. Arthrosc Sports Med Rehabil. 2021;3(3):e967–e980. doi: 10.1016/j.asmr.2021.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morris J.H., Magnussen R.A., DiBartola A.C., et al. Patient outcomes after horizontal cleavage tear repair: A systematic review. Arthroscopy. 2020;36(8):2316–2331. doi: 10.1016/j.arthro.2020.04.027. [DOI] [PubMed] [Google Scholar]
- 31.Petersen W., Karpinski K., Bierke S., Müller Rath R., Häner M. A systematic review about long-term results after meniscus repair. Arch Orthop Trauma Surg. 2021;142(5):835–844. doi: 10.1007/s00402-021-03906-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lester J.D., Gorbaty J.D., Odum S.M., Rogers M.E., Fleischli J.E. The cost-effectiveness of meniscal repair versus partial meniscectomy in the setting of anterior cruciate ligament reconstruction. Arthroscopy. 2018;34(9):2614–2620. doi: 10.1016/j.arthro.2018.06.046. [DOI] [PubMed] [Google Scholar]
- 33.Rogers M., Dart S., Odum S., Fleischli J. A cost-effectiveness analysis of isolated meniscal repair versus partial meniscectomy for red-red zone, vertical meniscal tears in the young adult. Arthroscopy. 2019;35(12):3280–3286. doi: 10.1016/j.arthro.2019.06.026. [DOI] [PubMed] [Google Scholar]
- 34.Feeley B.T., Liu S., Garner A.M., Zhang A.L., Pietzsch J.B. The cost-effectiveness of meniscal repair versus partial meniscectomy: A model-based projection for the United States. Knee. 2016;23(4):674–680. doi: 10.1016/j.knee.2016.03.006. [DOI] [PubMed] [Google Scholar]
- 35.Wasserburger J.N., Shultz C.L., Hankins D.A., et al. Long-term national trends of arthroscopic meniscal repair and debridement. Am J Sports Med. 2021;49(6):1530–1537. doi: 10.1177/0363546521999419. [DOI] [PubMed] [Google Scholar]
- 36.Lundberg M., Søndergaard J., Viberg B., Lohmander L.S., Thorlund J.B. Declining trends in arthroscopic meniscus surgery and other arthroscopic knee procedures in Denmark: A nationwide register-based study. Acta Orthop. 2022;93:783–793. doi: 10.2340/17453674.2022.4803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jacquet C., Pujol N., Pauly V., Beaufils P., Ollivier M. Analysis of the trends in arthroscopic meniscectomy and meniscus repair procedures in France from 2005 to 2017. Orthop Traumatol Surg Res. 2019;105(4):677–682. doi: 10.1016/j.otsr.2019.01.024. [DOI] [PubMed] [Google Scholar]
- 38.Katano H., Koga H., Ozeki N., et al. Trends in isolated meniscus repair and meniscectomy in Japan, 2011-2016. J Orthop Sci. 2018;23(4):676–681. doi: 10.1016/j.jos.2018.04.003. [DOI] [PubMed] [Google Scholar]
- 39.Partan M.J., Iturriaga C.R., Cohn R.M. Recent trends in concomitant meniscal procedures during anterior cruciate ligament reconstruction. Orthop J Sports Med. 2018;9(2) doi: 10.1177/2325967120984138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.López-Vega M., Doménech-Fernández J., Peiró S., Ridao-López M. Has arthroscopic meniscectomy use changed in response to the evidence? A large-database study from Spain. Clin Orthop Relat Res. 2023;481(1):7–16. doi: 10.1097/CORR.0000000000002421. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.