Abstract
Introduction & importance
Atlanto-occipital assimilation is a rare congenital abnormality which can cause atlantoaxial instability. Basilar invagination and instability can lead to cord compression and myelopathy in young individuals.
Case report & discussion
A 37-year-old male presented with gradually worsening axial neck pain for four years duration His deep tendon reflexes are exaggerated in all four limbs but there is no weakness or imbalance. Following radiological evaluation, he was diagnosed to have partial atlantooccipital assimilation causing atlantoaxial instability, basilar invagination and early myelopathy. He was treated with occipital-cervical fusion after the closed reduction of the atlantoaxial joint.
Conclusion
Atlanto-axial assimilation can lead to atlantoaxial instability and subsequently myelopathy. Dynamic radiographs and computed tomography are helpful in the diagnosis. Reducible atlantoaxial instability can be managed with closed reduction and occipitocervical fusion.
Keywords: Atlanto-axial instability, Atlantooccipital assimilation, Occipitocervical fusion, Hypoplasia of the atlas, Cervical myelopathy, Hyperreflexia
Highlights
-
•
Atlanto-occipital assimilation is a rare congenital condition which leads to atlantoaxial instability.
-
•
Dynamic radiographs, computed tomography and MRI helps diagnose this condition.
-
•
Late presentation or missed diagnosis can lead to myelopathy.
-
•
No recommended treatment is available as it is a rare condition
-
•
Occipito-cervical fusion is a safe treatment due to the rudimentary nature of the atlas and the risk of failure of atlantoaxial fusion.
1. Introduction
Atlanto-occipital assimilation (AOA) is a rare congenital craniovertebral anomaly where partial or complete ossification of the atlas with the occiput occurs. Synonyms for these conditions are atlantooccipital fusion and occipital-cervical synostosis. Synostosis occurs in the anterior arch of the atlas and partial synostosis is the commonest. The incidence of AOA varies with a range from 0.14 %-0.75 % of the population and male to female ratio is equal [1,2]. The incidence of this condition is slightly higher in Caucasians (0.5 %–1.0 %) [1].
This congenital fusion leads to hypermobility at the atlantoaxial joints which leads to atlantoaxial instability. Because of the rarity of this congenital condition and its consequence, there are no consensus for treatment is available in the literature.
This is report is about a patient who presented with chronic neck pain and was found to have partial atlantooccipital assimilation with atlantoaxial instability causing early myelopathy in an adult treated with occipitocervical fusion.
2. Case report
This case report has been prepared according to the SCARE guidelines [3].
2.1. Clinical
A 37-year-old male presented to the clinic with axial neck pain. Pain is gradually worsening and becomes prominent on forward flexion of the neck and extension. There is no radiating pain to the upper limbs. The gait and balance were normal. There was hyperreflexia elicited on deep tendon reflex elicitations in all four limbs. However, the rest of the neurological examination was normal. There was no history of childhood trauma to the neck. He denied any history of ear infections or ear surgery in the past. His modified Japanese orthopaedic association score for cervical myelopathy was 18/18 as he has no weaknesses or disability and he is falling into grade II myelopathy according to the Nurick grading system as he has cord signs (hyperreflexia) without difficulty in walking.
2.2. Imaging
Radiographs of the cervical spine revealed a hypoplastic atlas with atlantoaxial subluxation. The subluxation worsened on flexion (Fig. 1).
Fig. 1.
Radiographs of the cervical spine (A, B, C & D) shows hypoplastic atlas with atlanto axial instability. The instability at the atlanto-axial joint demonstrated well on flexion (C)and extension (D) radiographs.
The computer tomography demonstrated the atlantoaxial instability and fused atlantooccipital joint (Fig. 2).
Fig. 2.
Pre-operative sagital & axial computed tomographic images of cervical spine demonstrate atlanto-axial instability.
In images A & B the atlanto-dens interval (X) is 8.9 mm. This distance should be <3 mm in adult and <4.5 mm in children.
In image C clivus-canal angle (CCA) is 149.7-. which is normal as this angle should be 150°. The tangent line drawn along the superior surface of the clivus (Y) is Wackenheim clivus base line. The posterior and superior migration of dense to this line is called basilar invagination. The subject meets the requirement to be labelled as having a basilar invagination.
Image D demonstrated the basion-posterior arch: Opisthion-anterior arch interval is 1.2. This ratio more than one considered abnormal.
Image E shows the Posterior atlanto dens interval (PADI)/space available for the cord (<14 mm considered increased risk of neurology).
Image F shows Occiput-C2 angle (Y is McGregor's line) is guides surgeons to achieve the correct position (Normal value is vary in individuals −5° to 35°).
Image G shows complete fusion of bilateral facet joints with occipital condyles (arrows).
Magnetic resonance imaging (Fig. 3) showed partial fusion of the atlantooccipital joint, atlantoaxial instability, and no cord signal changes at the level of instability.
Fig. 3.
Sagital and axial MRI images showing atlantoaxial instability, and narrowing of the canal and there are no cord signal changes.
2.3. Procedure
Occipito-cervical posterior fusion from occiput to 4th cervical vertebra (Fig. 4C & D) using pars screws to the axis and lateral mass screws to the rest of the vertebrae with the occipital plate (NuVasive™) was performed following the discussion at the combined multidisciplinary spine meeting.
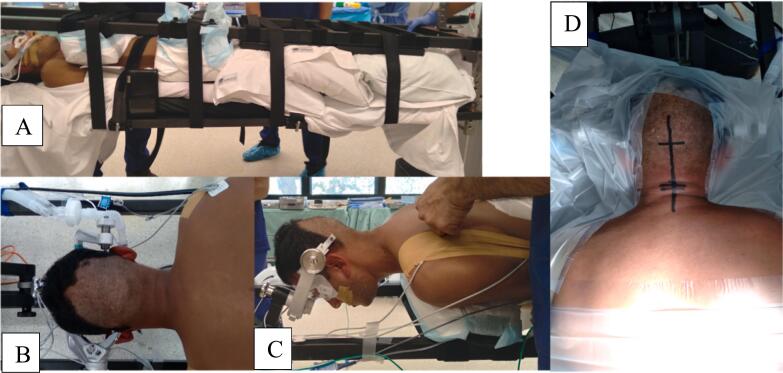
Fig. 4.
Pre-operative positioning of patient before surgery. Initially, patient was positioned supine on Jackson table and the head was stabilized with Mayfield head holder in supine position after general anaesthesia (A). Patient was rolled with the Jackson table to 360° after “sandwich” him with another Jackson table.
The final position of the head and marked incision site are shown in panels B, C & D.
As the assimilated section would strain C1 screw alone and also C1 pedicles being hypoplastic, not only was a single-level atlantoaxial fusion avoided but further C1 was skipped from instrumentation to decrease complications. The screws were guided by stealth station™ surgical navigation (Medtronic). The levels of fusion were made to prevent the early failure of fusion due to the long lever arm. Banked demineralized bone was used as infuse™ is not available anymore in Australia. The recovery was uneventful and the patient was mobilized with a Philadelphia cervical collar for 6 weeks. Initially he was managed with patient controlled analgesia followed by oral analgesia (Fig. 5).
Fig. 5.
Post-reduction and post-operative imaging of craniocervical region.
Radiograph (A) and Computed tomography (B) are pre-operative post-reduction images that confirm the reduction of instability. Fluoroscopic images C & D demonstrate the final position of the construct after fusion.
The patient will be monitored at the clinic for improvements in symptoms, signs and the progression of fusion. At six weeks after surgery patient did not have neck pain and returned to work. His pain and the restriction of motion has been continuously improving which has been evident in his 03 month follow-up. Patient is happy and his pain score became 0/10 (Fig. 6).
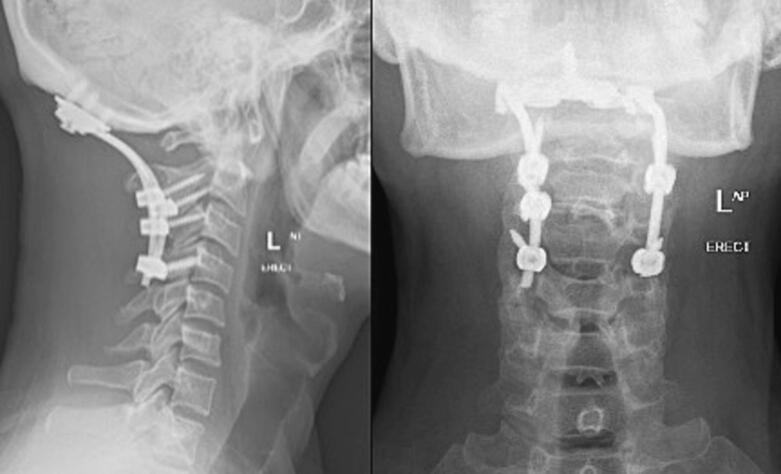
Fig. 6.
Post-operative radiographs of the neck at two week follow up which show good positioning of implants.
3. Discussion
During the development of the cranio-cervical region, the caudal half of the last occipital sclerotome and the rostral half of the first cervical sclerotome unite to form the base of the skull. Abnormalities in this process are leads to the assimilation of atlantooccipital bones [4].
This congenital anomaly at the spino-medullary region can give rise to atlantoaxial instability, basilar invagination, sandwich fusion (atlantooccipital fusion and fusion of axis and third cervical vertebra fusion), Klippel-feil syndrome. Atlanto-axial instability may give rise to fibrous tissue formation (in rheumatoid arthritis and nodal polyarthritis) and amyloid deposition (in patients on dialysis, infection, neoplasia & herniation of the intervertebral disc) [1,5]. Instability, basilar invagination and additional tissue or protein deposition contribute to causing cord compression [4].
Symptoms of this condition may vary from neck pain like this patient and headache to neurological weakness. It is very difficult to identify this condition with standard radiographs and computed tomography will help to identify it. MRI provides information on cord compression and additional details about the tissue or protein deposition in the atlanto-dens interval.
Treatment modalities for this condition vary from conservative management to occipital-cervical fusion and there is no consensus for this rare condition. Asymptomatic and patients with mild symptoms can be managed conservatively with a hard cervical collar [2]. Patients with symptoms, weaknesses and evidence of myelopathy can be treated surgically. The surgical option is posterior decompression and occipito-cervical fusion if the atlantoaxial joint is reducible on pre-operative images. The fusion levels are varied from the occiput to the 4th cervical vertebra according to the stability of the construct. If the atlantoaxial instability is not reducible, the transoral atlantoaxial release has been proposed in a case series [5]. In a case report, laminectomy of the axis and atlantoaxial fusion has been performed and there are no follow-up details of that patient [4]. We performed occipito-cervical fusion to the 4th cervical vertebra using pars screws to the axis and lateral mass screws to the rest of the vertebrae. The initial discussion was about the occipito-cervical fusion, which has been changed over to occipito-cervical fusion due to the long lever arm effect of the partial assimilation of atlanto-occipital joint. There was no literature support of effectiveness of the treatment.
4. Conclusion
Reducible atlantoaxial instability caused by partial atlantooccipital assimilation can lead to myelopathy even without any evidence of cord compression in the imaging. Reducible atlantoaxial instability can be treated by closed reduction and occipito-cervical fusion which will produce a good clinical outcome.
Consent
Informed written consent has been obtained from the patient for the publication of the case report and the accompanying images. Written consent is available for review at the request of the editor of this journal.
Ethical approval
There was no deviation in the standard of management was practised to manage this case report. The ethical approval exempted as it is a case report by the institution (University of NSW). The request number is HC210096.
Funding
No institutional or third-party funding for this work was obtained. KP1 is supported by an educational and training grant by Globus Medical.
Author contribution
All authors of this case report are involved in patient management, collection of data, and writing of this article. The Clinical lead supervised the management and was involved in the correction and editing of the article.
Guarantor
Dr. Ashish Diwan.
Research registration
Not applicable.
Declaration of competing interest
All authors have declared any conflicting financial or personal interests which could have inappropriately influenced their work.
References
- 1.Al-Motabagani M.A., Surendra M. Total occipitalization of the atlas. Anat. Sci. Int. Sep 2006;81(3):173–180. doi: 10.1111/j.1447-073X.2006.00129.x. [DOI] [PubMed] [Google Scholar]
- 2.Electricwala A.J., Harsule A., Chavan V., Electricwala J.T. Complete atlantooccipital assimilation with basilar invagination and atlantoaxial subluxation treated non-surgically: a case report. Cureus. Jun 9 2017;9(6):e1327. doi: 10.7759/cureus.1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Thoma A., et al. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. [Internet]. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. https://www.sciencedirect.com/science/article/pii/S1743919120307718 Available from: [DOI] [PubMed] [Google Scholar]
- 4.Martellacci S., Ben Salem D., Méjean N., Sautreaux J.L., Krausé D. A case of foramen magnum syndrome caused by atlanto-occipital assimilation with intracanal fibrosis. Surg. Radiol. Anat. Mar 2008;30(2):149–152. doi: 10.1007/s00276-007-0288-z. [DOI] [PubMed] [Google Scholar]
- 5.Tian Y., Xu N., Yan M., Passias P.G., Segreto F.A., Wang S. Atlantoaxial dislocation with congenital “sandwich fusion” in the craniovertebral junction: a retrospective case series of 70 patients. BMC Musculoskelet. Disord. Dec 1 2020;21(1) doi: 10.1186/s12891-020-03852-8. [DOI] [PMC free article] [PubMed] [Google Scholar]