Abstract
Background
Fear of childbirth (FOC) is a prevalent issue among pregnant women and significantly relates to adverse outcomes for the mother and child. However, it is not clear the prevalence and risk factors of FOC among pregnant women in a region with a moderate level of economic development in China. The aim of this study was to investigate the prevalence and risk factors of FOC among pregnant women in the third trimester of pregnancy in Lianyungang city, Eastern China.
Methods
A cross-sectional survey was conducted from December 2022 to February 2023 among pregnant women in the third trimester who met the inclusion criteria and visited Lianyungang Maternal and Child Health Hospital in Jiangsu Province, Eastern China. A structured questionnaire including sociodemographic characteristics, clinical characteristics, FOC, family function, doctor-patient communication, social support, general self-efficacy, anxiety, depression, insomnia symptoms, and quality of life was used to collect data. A multiple linear regression model was used to identify predictors of FOC.
Results
This study included 535 pregnant women in the third trimester. The mean score of FOC was 30.67 ± 10.18, and the median score was 29.00. The prevalence of FOC was 56.64%. Multiple linear regression analysis revealed that pregnant women with electronic screen exposure time more than 5 h per day (β = 2.02, 95%CI: 0.50–3.53, P < 0.05), no history of cesarean section (β = 2.66, 95%CI: 0.61–4.71, P < 0.05), likes sour food or hates greasy food (β = 1.75, 95%CI: 0.00-3.50, P < 0.05), anxiety (β = 0.50, 95%CI: 0.21–0.80, P < 0.05) and depression (β = 0.30, 95%CI: 0.04–0.57, P < 0.05) were more likely to have a greater level of FOC than their counterparts. However, a significantly lower level of FOC was observed in pregnant women who were multipara (β=-1.64, 95%CI: -3.27–0.01, P < 0.05), not worrying about delivery without family members (β=-3.75, 95%CI: -5.26–2.25, P < 0.001), had good family function (β=-0.32, 95%CI: -0.64–0.00, P < 0.05) and doctor-patient communication (β=-0.33, 95%CI: -0.64–0.02, P < 0.05).
Conclusions
The prevalence of FOC was high in Lianyungang city, Eastern China. FOC is influenced by multiple factors. There is an urgent need to develop interventions to reduce the prevalence of FOC in the third trimester of pregnancy, and to pay attention to pregnant women with risk factors for FOC.
Keywords: Fear of childbirth, Pregnant women, Associated factors, China
Background
Childbirth is a natural process, but it is also an unpredictable and painful one that can even cause the death of the mother and baby. During pregnancy, pregnant women experience a range of physical and mental changes, including fear of childbirth [1]. Fear of childbirth (FOC) includes both excessive maternal preoccupation with labor pain during pregnancy [2] and secondary fear of childbirth following normal delivery, miscarriage, and termination of pregnancy [3–5]. The prevalence of FOC varies from country to country and region to region, ranging from 4–82% [6–9], and has shown an increasing trend recently [6], which has gradually attracted great attention from the academic community.
FOC can have adverse outcomes for the mother and child. During pregnancy, FOC may cause changes in the uterine environment, with implications for increased fetal heart rate and reduced intrauterine movement [10], which are associated with the increased risk of postdates, intrauterine growth restriction and fetal distress as signs of fetal hypoxemia [11]. FOC may also increase the risk of adverse neonatal outcomes such as preterm childbirth and low birth weight [12]. Moreover, FOC are associated with prolonged labor, cesarean section, choice of epidural analgesia, prenatal and postpartum depression, and anxiety [13, 14]. In addition, FOC can increase perinatal costs, and the cost of severe FOC pregnant women is significantly higher than that of mild [15]. Therefore, it is necessary to understand the prevalence and risk factors for FOC.
The risk factors for FOC are complex and multifaceted. Previous studies in Europe and the Middle East have reported a number of risk factors for FOC, including nullipara, advanced maternal age, low socioeconomic status, unplanned pregnancy, previous cesarean section, vacuum delivery, perineal tear, shoulder dystocia, pregnancy complications (e.g., gestational diabetes), anxiety, depression, low self-efficacy, low self-esteem, negatively appraising birth, loneliness, fear of pain, disagreement with the birth plan proposed by the obstetrician [16–21]. However, there are differences.
between these regions and China in terms of life background, ethnic religion, and social structure, so the findings from these regions may not be applicable to Chinese populations.
In recent years, Chinese scholars have also started to try to study risk factors for FOC in some cities, such as Xi’an, Chongqing, Changsha and Guangdong, and found that primiparas, advanced maternal age, unplanned pregnancy, few spousal support, few social support, previous cesarean section, low self-efficacy, depression and use of pregnancy-related smartphone applications were the main risk factors [9, 14, 22–24]. However, these cities are national central cities or high developed regions in China, which differ from the middle or less developed areas in terms of their living background, social structure, etc. Therefore, it is necessary to conduct cross-sectional studies to understand the prevalence of FOC and its influencing factors in the middle or less developed areas in China.
In addition to the aforementioned influencing factors, there are also some factors that may potentially increase the occurrence of FOC. For example, certain clinical symptoms (such as abdominal pain and vaginal bleeding) during pregnancy are a painful experience for pregnant women, which makes them fearful when facing a more painful upcoming delivery experience. Therefore, these clinical symptoms may be a potential risk factor for FOC. Environmental pollution increases the risk of adverse fetal/neonatal outcomes [25, 26]. When faced with an impending delivery, pregnant women may experience FOC due to excessive concerns about their child’s health. Maternal disagreement with the birth plan proposed by the obstetrician was a risk factor for severe FOC [18], which might be partly related to doctor-patient communication. Clinical symptoms (e.g., abdominal pain, vaginal bleeding), environmental pollution, and Doctor-patient communication have not received sufficient attention in previous studies on the prevalence of FOC and its influencing factors, which is lacking of analysis of these modules.
Pregnant women had more intense FOC in the third trimester than in the first or second trimester of pregnancy [3]. The third trimester is a period of particular concern. However, few studies have focused on the prevalence of FOC and its influencing factors in the third trimester of pregnancy in China. Therefore, this study was conducted in a cross-sectional study in an middle developed area, with the main objective of understanding the prevalence of FOC and providing an in-depth analysis of the effects of sociodemographic characteristics, clinical characteristics, family function, doctor-patient communication, social support, general self-efficacy, anxiety, depression, insomnia symptoms, and quality of life on FOC in the third trimester of pregnancy, in order to provide a theoretical basis for the development and implementation of targeted interventions.
Methods
Study design and setting
A cross-sectional survey was conducted from December 2022 to February 2023 in Lianyungang Maternal and Child Health Hospital in Jiangsu Province, Eastern China. Lianyungang Maternal and Child Health Hospital is the only tertiary maternal and child health hospital in Lianyungang, which is responsible for providing comprehensive health care services for women and children in the whole city. Lianyungang is located in the middle of China’s coast, in the northeast part of underdeveloped Jiangsu Province, covering an area of about 7,615 square kilometers. In 2021, the city’s permanent population was 4.602 million, the birth population was 31,400, and the per capita gross domestic product (GDP) was 81,015 CNY (the national per capita GDP was 80,976 CNY).
Participants
Pregnant women in the third trimester who met the inclusion criteria and visited Lianyungang Maternal and Child Health Hospital from December 2022 to February 2023 were recruited in this study. The inclusion criteria for pregnant women included the following: (1) gestational age of 28 weeks or more; (2) age greater than or equal to 18 years; (3) no intellectual disability, cognitive impairment or major diseases; (4) able to understand the content of the questionnaire and agree to participate in this study. The exclusion criteria for pregnant women included the following: (1) pregnant women with a clearly diagnosed psychiatric disorder or a history of any psychiatric disorder; (2) unable to communicate normally; (3) do not agree to participate in this study. The recruited pregnant women independently completed a questionnaire distributed by the investigators. To ensure the quality of the data, a fixed team of 5 uniformly trained investigators collected the questionnaires in this study. Single population proportion formula was employed to calculate the minimum sample size required. Because there were no previous studies at the study sites, to get maximize the minimum sample size we used prevalence of FOC as 50% (P = 50%), 95%CI, margin error of 5%, and 20% nonresponse rate. The minimum sample size required was calculated to be 461. A systematic random sampling method was employed to select participants. In order to obtain more reliable conclusions, a total of 550 pregnant women were recruited in this study, of which 15 were excluded due to incomplete questionnaire filling due to time constraints. Therefore, a total of 535 pregnant women were included in the study, with a participation rate of 97.3%.
Data collection
Data were collected using a structured questionnaire designed on the basis of literature review and consultation with experts. To ensure the validity of the questionnaire, a pre-survey was conducted at the study site. The questionnaire was modified and refined according to the pre-survey. The questionnaire was composed of 11 parts: sociodemographic characteristics, clinical characteristics, FOC, family function, doctor-patient communication, social support, general self-efficacy, anxiety, depression, insomnia symptoms and quality of life (QOL). Sociodemographic characteristics included age, education, area of residence, occupation, monthly family income, self-rated stress, perceived poor resistance, daily time of exposure to electronic screens, and environmental pollution around the home. Environmental pollution around the home was measured by asking “Is there any environmental pollution within 100 meters of your home, such as sewer, garbage dump, noise, heating company (fuel), etc.?”. Clinical characteristics mainly focused on parity, history of abortion, history of cesarean section, threatened abortion, complication of pregnancy, hospitalization during pregnancy, clinical symptoms (vomiting, lower abdominal pain, vaginal bleeding, dizziness and fatigue, loss of appetite, likes sour food or hates greasy food) and worrying about delivery without family members. Acid food includes acid fruit, acid dried fruit, yogurt, pickled Chinese cabbage and so on. Greasy food included greasy and fatty meat foods.
FOC was measured using the Chinese version of the Childbirth Attitude Questionnaire (CAQ) validated in Chinese pregnant women [27]. The questionnaire was originally designed by Areskog [28] and developed by Lowe [29] and Tanglakmankhong [30]. It included 16 items, and each answer of the subjects was rated on a 4-point Likert scale (1, “not at all” to 4, “high”). Item scores were summed to the total questionnaire score, which ranged from 16 to 64. Higher scores indicate more severe FOC. Those pregnant women with a score greater than or equal to 28 were considered to have FOC, with 28 to 39 classified as mild, 40 to 51 as moderate, and 52 to 64 as severe [14]. In the current study, the questionnaire had high internal consistency (Cronbach’s α = 0.95).
Family function was measured using Adaptation Partnership Growth and Resolved (APGAR) questionnaire [31]. The questionnaire consisted of 5 items, and each item was scored on a 3-point Likert scale (0, “hardly ever” to 3, “almost always”). The total score was the sum of each item score, ranging from 0 to 10. Higher scores indicated better family function. This questionnaire was widely used in the assessment of family function in pregnant women [32]. In the current study, the questionnaire had excellent internal consistency (Cronbach’s α = 0.92).
Doctor-patient communication was measured using a component derived from the Consumer Assessment of Healthcare Providers and Systems (CAHPS) [33]. This component consisted of 4 items, which related to the way medical staff explain, listen carefully, respect and time spent. The never, sometimes, usually, and always response formats were used for each item and were assigned 1, 2, 3, and 4 points, respectively. The sum of item scores was the total score of the scale, which ranged from 4 to 16. High scores reflected good doctor-patient communication. The scale had good reliability and validity [34]. In the current study, its Cronbach’s α was 0.89.
Social support was measured using the Oslo 3-item social support scale, which was frequently used to assess social support related issues in community settings [35]. The scale dealt with the number of close people on whom serious problems can be relied, the degree to which people care, and the level of ease of getting practical help from neighbors. Total scores ranged from 3 to 14, with higher scores indicating better social support [35]. In the current study, the scale had acceptable internal consistency (Cronbach’s α = 0.60).
General self-efficacy was measured using the General Self-Efficacy Scale (GSES). Self-efficacy refers to an individual’s perception or belief about whether he or she can adopt appropriate behaviors in the face of environmental challenges [36]. The GSES was a self-reported measure consisting of 10 items. Each item was scored using a 4-point Likert scale (1, “not at all true” to 4, “exactly true”). The scores of the 10 items were summed to obtain a total score, which ranged from 10 to 40. A higher total score represented a higher self-efficacy of the study subjects. The scale has been shown to have good internal consistency across different countries [37]. In the current study, its Cronbach’s α was 0.91.
Anxiety was measured using the Generalized Anxiety Disorder-7 (GAD-7) scale suitable for use in the perinatal period [38]. It was a 7-item scale with each item scored on a 4-point Likert scale (0, “not at all” to 3, “almost every day”). The total score ranged from 0 to 21, with higher scores indicating more severe anxiety symptoms. In the current study, the scale had high internal consistency (Cronbach’s α = 0.93).
Depression was measured using the Patient Health Questionnaire-9 (PHQ-9) used to screen for depressive symptoms and assess their severity [39]. The questionnaire consisted of 9 items, each of which was scored using a 4-point Likert scale (0, “not at all” to 3, “almost every day”). Total scores ranged from 0 to 27, with higher scores indicating more severe depressive symptoms. The questionnaire has been widely used in epidemiological surveys and has good reliability and validity [40]. In the current study, the questionnaire had good internal consistency (Cronbach’s α = 0.86).
Insomnia symptoms were measured using the Insomnia Severity Index (ISI), which has been shown to have good reliability and validity [41]. It consisted of 7 items, each of which was scored using a 5-point Likert scale, ranging from 0 to 4. The total score ranges from 0 to 28, with higher scores indicating more severe insomnia symptoms. In the current study, it had high internal consistency (Cronbach’s α = 0.90).
QOL was assessed using the EUROHIS-QOL 8-item index (WHOQOL-8) derived from the WHOQOL-100 and the WHOQOL-BREF [42, 43]. The scale consisted of 8 items including psychological, physical, social and environmental domains. Questions were answered based on a 5-point Likert scale, ranging from 1 to 5. The total score was the sum of 8 item scores, with higher scores indicating better QOL. The scale has been shown to have satisfactory internal consistency across multiple countries [42, 43]. In the current study, its Cronbach’s α was 0.83.
Data analysis
All data analyses were performed using SPSS21.0 (IBM Corporation, Armonk, State of New York) software. Continuous data were described as means and standard deviations (SDs) or medians and interquartile ranges, and categorical data were described as frequencies and percentages. The rank sum test was used to compare FOC of pregnant women in the third trimester among different groups. Mann-Whitney U test was used for comparison between the two groups, and Kruskal-Wallis H test was used for comparison between the three groups. Spearman’s correlation analysis was used to assess correlations between family function, doctor-patient communication, social support, general self-efficacy, anxiety, depression, insomnia symptoms, QOL and FOC. Significant variables from univariate analyses were included in multiple linear regression models to exclude the influence of confounding factors and to identify independent related factors of FOC. All tests were two-sided, and the level of statistical significance was set to P < 0.05.
Results
Current status of FOC in pregnant women in the third trimester
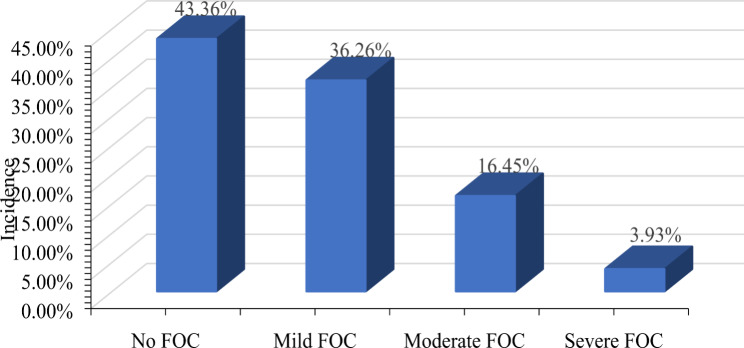
Among 535 pregnant women in the third trimester, the mean score of FOC was 30.67 ± 10.18, and the median score was 29.00. The prevalence of FOC was 56.64%, with mild 36.26%, moderate 16.45% and severe 3.93% (Fig. 1).
Fig. 1.
Current status of FOC in pregnant women in the third trimester. Notes: FOC: fear of childbirth
Sociodemographic characteristics
The pregnant women who participated in the study ranged in age from 18 to 41 years, with a mean age of 29.39 ± 4.47 years, and a small number (12.52%) were 35 years or older. Nearly two-thirds of pregnant women (66.54%) had a college education or above, and nearly one-third (33.27%) lived in rural areas. More than half of pregnant women (53.83%) were currently employed, and the largest number (43.93%) had a family income of 5001 to 10,000 a month. Nearly a quarter (23.93%) of pregnant women self-rated their stress as big, and a smaller proportion (4.86%) perceived that they had a poor resistance. More than half of pregnant women (52.71%) were exposed to electronic screens for more than 5 h per day, and about one in five (19.81%) reported environmental pollution around their homes. The univariate analyses showed that the FOC scores of pregnant women were statistically significant among different age, education, self-rated stress, perceived poor tolerance, time of electronic screen exposure per day and environmental pollution around the home (P < 0.05) (Table 1).
Table 1.
Sociodemographic characteristics and their relationships with fear of childbirth
| Variables | Pregnant women | FOC | P | |||
|---|---|---|---|---|---|---|
| n | % | median | interquartile range | |||
| Age (years) | 0.040 | |||||
| <35 | 468 | 87.48 | 29.50 | 24.00–37.00 | ||
| ≥35 | 67 | 12.52 | 26.00 | 21.00–34.00 | ||
| Education | 0.049 | |||||
| High school or below | 179 | 33.46 | 28.00 | 21.00–36.00 | ||
| College or above | 356 | 66.54 | 30.00 | 24.00-36.75 | ||
| Area of residence | 0.293 | |||||
| Urban | 357 | 66.73 | 30.00 | 24.00–36.00 | ||
| Rural | 178 | 33.27 | 28.00 | 22.00–37.00 | ||
| Employed | 0.713 | |||||
| Yes | 288 | 53.83 | 29.00 | 24.00–35.00 | ||
| No | 247 | 46.17 | 29.00 | 22.00–38.00 | ||
| Family income (RMB/month) | 0.159 | |||||
| ≤5000 | 100 | 18.69 | 27.50 | 22.25-33.00 | ||
| 5001–10,000 | 235 | 43.93 | 30.00 | 23.00–37.00 | ||
| ≥ 10,001 | 200 | 37.38 | 29.00 | 24.00–38.00 | ||
| Self-rated stress | < 0.001 | |||||
| Small | 407 | 76.07 | 28.00 | 23.00–34.00 | ||
| Big | 128 | 23.93 | 33.00 | 27.00-43.75 | ||
| Perceived poor resistance | 0.011 | |||||
| Agree | 26 | 4.86 | 35.50 | 26.50-44.25 | ||
| Disagree | 509 | 95.14 | 29.00 | 23.00–35.00 | ||
| Time of electronic screen exposure per day (hours) | < 0.001 | |||||
| ≤ 5 | 253 | 47.29 | 28.00 | 22.00-33.50 | ||
| >5 | 282 | 52.71 | 31.00 | 25.00–40.00 | ||
| Environmental pollution around the home | < 0.001 | |||||
| Yes | 106 | 19.81 | 32.00 | 26.00–43.00 | ||
| No | 429 | 80.19 | 28.00 | 23.00–34.00 | ||
Notes: FOC: fear of childbirth; Significant values are in bold
Clinical characteristics
Among the respondents, more than half (55.70%) were multiparous and more than one-third (34.39%) had a history of abortion. The number of pregnant women with a history of cesarean Sect. (19.44%) was approximately a quarter of those without. Similarly, the number of pregnant women with threatened abortion (18.88%) were approximately a quarter of those without. More than a quarter of pregnant women (26.36%) experienced pregnancy complications, and a large proportion (78.50%) did not experience hospital admission during pregnancy. Among the recruited pregnant women, 350 (65.42%) had vomiting during pregnancy, 78 (14.58%) had lower abdominal pain, 109 (20.37%) had vaginal bleeding, 151 (28.22%) had dizziness and fatigue, 185 (34.58%) had loss of appetite, and 147 (27.48%) had likes sour food or hates greasy food. Among the participants, nearly half of the pregnant women (45.42%) reported concerns about not having a family member with them during delivery. The univariate analyses indicated that there were statistically significant differences in FOC scores of pregnant women according to parity, history of abortion, history of cesarean section, threatened abortion, lower abdominal pain, vaginal bleeding, dizziness and fatigue, loss of appetite, likes sour food or hates greasy food and worrying about delivery without family members. (P < 0.05) (Table 2).
Table 2.
Clinical characteristics and their relationships with fear of childbirth
| Variables | Pregnant women | FOC | P | ||||
|---|---|---|---|---|---|---|---|
| n | % | median | interquartile range | ||||
| Parity | 0.002 | ||||||
| Nullipara | 237 | 44.30 | 31.00 | 25.00-36.50 | |||
| Multipara | 298 | 55.70 | 28.00 | 21.00-35.25 | |||
| History of abortion | 0.047 | ||||||
| Yes | 184 | 34.39 | 27.00 | 21.00–37.00 | |||
| No | 351 | 65.61 | 30.00 | 25.00–36.00 | |||
| History of cesarean section | < 0.001 | ||||||
| Yes | 104 | 19.44 | 25.50 | 19.00-33.75 | |||
| No | 431 | 80.56 | 30.00 | 25.00–37.00 | |||
| Threatened abortion | 0.009 | ||||||
| Yes | 101 | 18.88 | 32.00 | 25.00-43.50 | |||
| No | 434 | 81.12 | 29.00 | 23.00-34.25 | |||
| Complication of pregnancy | 0.114 | ||||||
| Yes | 141 | 26.36 | 31.00 | 23.50–40.50 | |||
| No | 394 | 73.64 | 29.00 | 23.00–35.00 | |||
| Hospitalization during pregnancy | 0.958 | ||||||
| Yes | 115 | 21.50 | 29.00 | 25.00–35.00 | |||
| No | 420 | 78.50 | 29.00 | 23.00–37.00 | |||
| Vomiting during pregnancy | 0.791 | ||||||
| Yes | 350 | 65.42 | 30.00 | 23.00-37.25 | |||
| No | 185 | 34.58 | 29.00 | 24.00–34.00 | |||
| Lower abdominal pain | < 0.001 | ||||||
| Yes | 78 | 14.58 | 32.00 | 26.75-44.00 | |||
| No | 457 | 85.42 | 29.00 | 23.00–35.00 | |||
| Vaginal bleeding | 0.004 | ||||||
| Yes | 109 | 20.37 | 31.00 | 25.00–42.00 | |||
| No | 426 | 79.63 | 29.00 | 23.00–35.00 | |||
| Dizziness and fatigue | < 0.001 | ||||||
| Yes | 151 | 28.22 | 32.00 | 25.00–40.00 | |||
| No | 384 | 71.78 | 28.00 | 23.00–34.00 | |||
| Loss of appetite | |||||||
| Yes | 185 | 34.58 | 30.00 | 25.00–41.00 | 0.019 | ||
| No | 350 | 65.42 | 29.00 | 23.00–34.00 | |||
| Likes sour food or hates greasy food | < 0.001 | ||||||
| Yes | 147 | 27.48 | 32.00 | 25.00–42.00 | |||
| No | 388 | 72.52 | 28.00 | 22.00–34.00 | |||
| Worrying about delivery without family members | < 0.001 | ||||||
| Yes | 243 | 45.42 | 31.00 | 26.00–41.00 | |||
| No | 292 | 54.58 | 27.00 | 22.00–33.00 | |||
Notes: FOC: fear of childbirth; Significant values are in bold
Correlations analyses
Among the pregnant women interviewed, the median scores of family function, doctor-patient communication, social support and general self-efficacy were 9.00, 13.00, 11.00 and 28.00, respectively. The correlation analyses showed that family function, doctor-patient communication, social support and general self-efficacy were negatively correlated with FOC (r=-0.227, r=-0.132, r=-0.167 and r=-0.107, respectively, P < 0.05). Among participants, the median scores for anxiety, depression, and insomnia symptoms were 2.00, 5.00, and 8.00, respectively. The correlation analyses found that anxiety, depression and insomnia symptoms were positively correlated with FOC (r = 0.479, r = 0.422 and r = 0.294, respectively, P < 0.001). Among the respondents, the mean score of QOL was 29.93 ± 3.89, and the correlation analyses showed that QOL was negatively correlated with FOC (r=-0.251, P < 0.001) (Table 3).
Table 3.
Correlation analyses and descriptive statistics of variables
| Variables | Median (P25, P75) | Mean ± SD | Correlation with FOC | |
|---|---|---|---|---|
| Correlation coefficients | P | |||
| Family function | 9.00 (5.00, 10.00) | -0.227 | < 0.001 | |
| Doctor-patient communication | 13.00 (11.00, 16.00) | -0.132 | 0.002 | |
| Social support | 11.00 (10.00, 12.00) | -0.167 | < 0.001 | |
| General self-efficacy | 28.00 (25.00, 30.00) | -0.107 | 0.013 | |
| Anxiety | 2.00 (0.00, 6.00) | 0.479 | < 0.001 | |
| Depression | 5.00 (2.00, 8.00) | 0.422 | < 0.001 | |
| Insomnia symptoms | 8.00 (5.00, 12.00) | 0.294 | < 0.001 | |
| QOL | 29.93 ± 3.89 | -0.251 | < 0.001 | |
Notes: FOC: fear of childbirth; QOL: quality of life; Significant values are in bold
Multiple linear regression for predicting FOC
The multiple linear regression results showed that pregnant women with electronic screen exposure of more than 5 h per day had higher score of FOC than those with no more than 5 h per day (β = 2.02, 95%CI: 0.50–3.53, P < 0.05). Multiparas had lower scores of FOC than nulliparas (β=-1.64, 95%CI: -3.27–0.01, P < 0.05). Pregnant women without a history of cesarean section had higher score of FOC than pregnant women with a history of cesarean section (β = 2.66, 95%CI: 0.61–4.71, P < 0.05). Pregnant women who experienced likes sour food or hates greasy food had higher score of FOC than those who did not (β = 1.75, 95%CI: 0.00-3.50, P < 0.05). Pregnant women who were not worried about not having a family member with them during delivery had lower score of FOC than those who were worried (β=-3.75, 95%CI: -5.26–2.25, P < 0.001). In addition, pregnant women with good family function (β=-0.32, 95%CI: -0.64–0.00, P < 0.05) and doctor-patient communication (β=-0.33, 95%CI: -0.64–0.02, P < 0.05) had lower score of FOC. However, pregnant women with high anxiety (β = 0.50, 95%CI: 0.21–0.80, P < 0.05) and depression (β = 0.30, 95%CI: 0.04–0.57, P < 0.05) had higher score of FOC. Thus, time of electronic screen exposure per day, parity, history of cesarean section, likes sour food or hates greasy food, worrying about delivery without family members, family function, doctor-patient communication, anxiety and depression can be used to predict FOC in pregnant women in the third trimester (Table 4).
Table 4.
Results of Multiple linear regression analysis for predicting FOC
| Variables | Estimate | 95% CI | SE | t | P | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Age (years) (Ref: <35) | ||||||
| ≥ 35 | -0.76 | -3.12 | 1.60 | 1.20 | -0.63 | 0.529 |
| Education (Ref: High school or below) | ||||||
| College or above | 0.47 | -1.20 | 2.15 | 0.85 | 0.56 | 0.579 |
| Self-rated stress (Ref: Big) | ||||||
| Small | -1.35 | -3.31 | 0.61 | 1.00 | -1.35 | 0.177 |
| Perceived poor resistance (Ref: Agree) | ||||||
| Disagree | 1.15 | -2.42 | 4.73 | 1.82 | 0.63 | 0.527 |
| Time of electronic screen exposure per day (hours) (Ref: ≤5) | ||||||
| >5 | 2.02 | 0.50 | 3.53 | 0.77 | 2.62 | 0.009 |
| Environmental pollution around the home (Ref: Yes) | ||||||
| No | -0.70 | -2.64 | 1.23 | 0.99 | -0.71 | 0.476 |
| Parity (Ref: Nullipara) | ||||||
| Multipara | -1.64 | -3.27 | -0.01 | 0.83 | -1.97 | 0.049 |
| History of abortion (Ref: No) | ||||||
| Yes | -0.19 | -1.88 | 1.51 | 0.86 | -0.22 | 0.830 |
| History of cesarean section (Ref: Yes) | ||||||
| No | 2.66 | 0.61 | 4.71 | 1.04 | 2.55 | 0.011 |
| Threatened abortion (Ref: Yes) | ||||||
| No | -1.51 | -3.62 | 0.59 | 1.07 | -1.42 | 0.157 |
| Lower abdominal pain (Ref: No) | ||||||
| Yes | 1.79 | -0.40 | 3.97 | 1.11 | 1.61 | 0.108 |
| Vaginal bleeding (Ref: No) | ||||||
| Yes | 0.65 | -1.36 | 2.66 | 1.02 | 0.64 | 0.525 |
| Dizziness and fatigue (Ref: No) | ||||||
| Yes | 1.33 | -0.39 | 3.05 | 0.88 | 1.52 | 0.130 |
| Loss of appetite (Ref: No) | ||||||
| Yes | 0.50 | -1.17 | 2.16 | 0.85 | 0.58 | 0.560 |
| Likes sour food or hates greasy food (Ref: No) | ||||||
| Yes | 1.75 | 0.00 | 3.50 | 0.89 | 1.97 | 0.049 |
| Worrying about delivery without family members (Ref: Yes) | ||||||
| No | -3.75 | -5.26 | -2.25 | 0.77 | -4.90 | < 0.001 |
| Family function | -0.32 | -0.64 | 0.00 | 0.16 | -1.97 | 0.049 |
| Doctor-patient communication | -0.33 | -0.64 | -0.02 | 0.16 | -2.10 | 0.036 |
| Social support | 0.44 | -0.08 | 0.95 | 0.26 | 1.66 | 0.097 |
| General self-efficacy | 0.08 | -0.10 | 0.26 | 0.09 | 0.84 | 0.403 |
| Anxiety | 0.50 | 0.21 | 0.80 | 0.15 | 3.37 | 0.001 |
| Depression | 0.30 | 0.04 | 0.57 | 0.14 | 2.22 | 0.027 |
| Insomnia symptoms | 0.08 | -0.10 | 0.26 | 0.09 | 0.87 | 0.387 |
| QOL | -0.23 | -0.46 | 0.01 | 0.12 | -1.87 | 0.062 |
| Constant | 34.52 | 21.22 | 47.82 | 6.77 | 5.10 | < 0.001 |
Notes: QOL: quality of life; Ref: reference; Significant values are in bold
Discussion
To the best of our knowledge, this is the first cross-sectional study to understand the prevalence of fear of childbirth and its risk factors in a region of China with an intermediate level of economic development in the third trimester of pregnancy. Moreover, in this study, we performed the first analysis of potential risk factors of FOC, including clinical symptoms (e.g., abdominal pain and vaginal bleeding), environmental pollution, and doctor-patient communication. Our study data showed that the overall prevalence of FOC was 56.64%, with 3.93% severe. The prevalence of FOC in this study was slightly lower than the prevalence in those regions from national central cities or economically developed regions of China (Xi’an, Zhengzhou, Chongqing) (range from 67.1 to 70.3%) using the same detection tool (CAQ), but the prevalence of severe FOC was within the range of those regions (range from 2.2–5.5%) [14, 23, 24]. The prevalence of FOC abroad was reported in some previous studies: 4.5% in Belgium, 3.7% in Finland, 24% in Australia, 27% in the United States, and 13.1% in India [13, 44–47]. The prevalence in those countries is significantly lower than our reported, which may be related to the differences of life contexts, ethnic religions, social structures and measurement methods. Therefore, we may conclude that FOC is highly prevalent in China, which requires sufficient attention from academia and medical institutions.
Previous studies found that exposure to electronic screens for more than 5 h per day in pregnant women was a risk factor for depressive symptoms [48]. Moreover, increased exposure to electronic screens was associated with higher depressive symptomatology [49]. Of note, high FOC was associated with using pregnancy-related smartphone applications [24]. Our data showed that electronic screen exposure of more than 5 h per day for pregnant women was a risk factor for FOC. This might be related to pregnant women accessing negative childbirth information on the Internet [50, 51]. Therefore, closer collaboration among media experts, health professionals and policy makers are needed to guide pregnant women to obtain positive childbirth information. We found that high FOC was associated with environmental pollution near the home in the univariate analysis, but further large-sample, multicenter studies are needed to clarify the correlation between environmental pollution and FOC.
In this study, we found that high FOC was associated with nullipara, consistent with several previous studies [9, 14, 52, 53]. It might be due to the lack of experience and information about the childbirth process for nulliparous women [54]. However, some other studies stated that multiparous women experienced FOC with a lower level [13, 55], in which case multiparous women usually experienced traumatic or negative childbirth previously [7]. Notably, in this study, we also found higher FOC scores in pregnant women without history of cesarean section, which is inconsistent with previous findings [13, 56, 57]. This may be related to the fact that the vast majority of young Chinese women who experienced caesarean section previously only consider having a second child if they have a strong desire to have children and are optimistic about childbirth currently. Interestingly, our data showed that pregnant women who like sour food or hate greasy food were more likely to develop FOC. Previous studies showed that pregnant women often experienced altered taste sensations during pregnancy, such as a preference for acidic foods or an aversion to fatty foods [58, 59], which might cause insufficient food diversity. Inadequate food diversity could lead to fetal nutritional abnormalities, and nutritional abnormalities could lead to pregnancy complications and adverse pregnancy outcomes [60, 61]. When faced the upcoming delivery, pregnant women might suffer from FOC due to fear of unhealthiness for themselves and their children. In order to have adequate nutrition for themselves and their fetus, some pregnant women might have to eat foods they didn’t like, adding to the negative emotions that could also be a significant cause of FOC. Therefore, nutrition experts should take measures to ensure a balanced nutritional balance for mother and fetus by reasonably matching foods with full consideration of the pregnant woman’s tastebuds. In addition, our study found that worrying about delivery without family members was a risk factor for FOC. Previous studies showed that the presence and encouragement of family members during childbirth could increase a pregnant woman’s confidence and help her get through the painful process [62, 63]. It is noteworthy that this study took place after the adoption of “Category B” control measures for novel coronavirus infection in China (no more centralized nucleic acid testing, judged close contacts, restrictions on access to public places, centralized isolation, and so on). Pregnant women fear that family members would be infected and need to isolate themselves at home, unable to accompany themselves through the painful process of childbirth or to receive adequate care. Therefore, health care providers need to take into account the concerns of pregnant women and provide timely counseling and quality services.
Our study found that family function was associated with FOC. This finding is similar to the results of several previous studies where inadequate family support was a risk factor for FOC [64, 65]. A possible explanation for this finding might be that family support including information and experiences of childbirth can help pregnant women stay positive about the upcoming childbirth during pregnancy [66]. Previous studies showed that classes for pregnant women taught by midwives, which provide important information on prenatal care and preparation for delivery, can be effective in reducing the prevalence of FOC. However, pregnant women who lack family support may have difficulty accessing such classes, and this may also be an important reason for FOC. Therefore, social workers should communicate with pregnant women’s family members to ensure adequate family support for pregnant women. Our findings suggest that doctor-patient communication was associated with FOC. Previous studies showed that good doctor-patient communication increases patient satisfaction and compliance [67], and that disagreement with the birth plan proposed by the obstetrician was a risk factor for FOC [18]. When a pregnant woman faces a doctor-patient communication dilemma, she may choose not to carry out the doctor’s orders, which may be a potentially important reason for FOC. Therefore, health care facilities need to strengthen training in medical and nursing communication skills to give pregnant women a better health care experience. We also found that anxiety was a risk factor for FOC, which was consistent with previous literature [64, 68]. Since FOC is considered a form of anxiety disorder or a phobic fear [12], it was not surprising that anxiety disorders are associated with higher levels of FOC. In addition, our study also found that depression was a risk factor for FOC, which was consistent with previously literature [13, 23]. Depression, characterized by low mood, lack of pleasure and despair, may lead to negative feelings about childbirth and low self-efficacy, which have been identified as potential causes of fear of childbirth [22, 24, 69]. Therefore, health care providers should focus on counseling for anxious and depressed pregnant women to reduce the prevalence of FOC.
Our study shows that the prevalence of FOC is high and mainly mild. Therefore, effective intervention measures to reduce FOC should be developed. When making the intervention measures, more attention should be paid to the pregnant women who have first birth, no history of caesarean section, and experienced liking sour food or hating greasy food. In addition, reducing electronic screen exposure time, anxiety and depression, and improving family function and doctor-patient communication can also reduce the occurrence of FOC.
There are some limitations of this study that need to be elaborated. First, as a cross-sectional study, causal relationships between variables could not be obtained, and Longitudinal studies are needed in the future. Second, this study was conducted only in a region with a moderate level of economic development in eastern China, which may differ from western, southern, and northern China in terms of life background, ethnic religion, and social structure, and further multicenter studies are needed. Third, FOC, family function, doctor-patient communication, social support, general self-efficacy, anxiety, depression, insomnia symptoms, and quality of life in this study were measured through subjective assessment scales, and lacked objective evaluation indicators, which might cause some bias. Finally, this study only included pregnant women in the third trimester of pregnancy, and pregnant women in the first and second trimester of pregnancy were not included. Further research should be conducted to expand the population in the future.
Conclusion
In summary, the results revealed that the overall prevalence of FOC was 56.64%, with mild 36.26%, moderate 16.45% and severe 3.93%. It is identified that exposure to electronic screens for more than 5 h per day, Nullipara, History of cesarean section, like sour food or hate greasy food, worrying about delivery without family members, family function, doctor-patient communication, anxiety and depression were significant risk factors in FOC. Considering the high prevalence of FOC, there is an urgent need to develop interventions to reduce the prevalence of FOC in the third trimester of pregnancy, and to pay attention to pregnant women with risk factors for FOC.
Acknowledgements
We would like to thank the data collectors for their efforts and support and assistance for this study. In addition, we would also express our thanks to the study participants.
Abbreviations
- FOC
fear of childbirth
- GDP
gross domestic product
- QOL
quality of life
- CAQ
Childbirth Attitude Questionnaire
- APGAR
Adaptation Partnership Growth and Resolved
- CAHPS
Consumer Assessment of Healthcare Providers and Systems
- GSES
General Self-Efficacy Scale
- GAD-7
Generalized Anxiety Disorder-7
- PHQ-9
Patient Health Questionnaire-9
- ISI
Insomnia Severity Index
- SD
standard deviation
- CI
confidence interval
- SE
standard error
Authors’ contributions
TZ, MLL and XC provided the research design and advanced the whole study. XC and TZ analysed the data and drafted the manuscript. All authors read, revised and approved the final manuscript and agreed to take responsibility for all aspects of the work.
Funding
This study had no funding support.
Data availability
The datasets generated and/or analysed during the current study are not publicly available for ethical reasons but are available from the corresponding author on reasonable request.
Declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All methods in our study were conducted in accordance with the Declaration of Helsinki. The study was approved by the Ethics Committee of Lianyungang Maternal and Child Health Hospital (approval no.: LW2023005). All participants were informed of the purpose of the study and provided written informed consent before participating in the study.
Consent for publication
Not applicable.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Teng Zhang and Meilin Liu are Co-first Authors.
References
- 1.Fisher C, Hauck Y, Fenwick J. How social context impacts on women’s fears of childbirth: a Western Australian example. Social science & medicine (1982) 2006, 63(1):64–75. [DOI] [PubMed]
- 2.Richens Y, Smith DM, Lavender DT. Fear of birth in clinical practice: a structured review of current measurement tools. Sex reproductive healthcare: official J Swed Association Midwives. 2018;16:98–112. doi: 10.1016/j.srhc.2018.02.010. [DOI] [PubMed] [Google Scholar]
- 3.Hofberg K, Ward MR. Fear of childbirth, tocophobia, and mental health in mothers: the obstetric-psychiatric interface. Clin Obstet Gynecol. 2004;47(3):527–34. doi: 10.1097/01.grf.0000132527.62504.ca. [DOI] [PubMed] [Google Scholar]
- 4.Hofberg K, Brockington I. Tokophobia: an unreasoning dread of childbirth. A series of 26 cases. Br J psychiatry: J mental Sci. 2000;176:83–5. doi: 10.1192/bjp.176.1.83. [DOI] [PubMed] [Google Scholar]
- 5.Bhatia MS, Jhanjee A. Tokophobia: a dread of pregnancy. Industrial psychiatry journal. 2012;21(2):158–9. doi: 10.4103/0972-6748.119649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Connell MA, Leahy-Warren P, Khashan AS, Kenny LC, O’Neill SM. Worldwide prevalence of tocophobia in pregnant women: systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2017;96(8):907–20. doi: 10.1111/aogs.13138. [DOI] [PubMed] [Google Scholar]
- 7.Nilsson C, Hessman E, Sjöblom H, Dencker A, Jangsten E, Mollberg M, Patel H, Sparud-Lundin C, Wigert H, Begley C. Definitions, measurements and prevalence of fear of childbirth: a systematic review. BMC Pregnancy Childbirth. 2018;18(1):28. doi: 10.1186/s12884-018-1659-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koc AE, Colak S, Colak GV, Pusuroglu M, Hocaoglu C. Investigating fear of childbirth in pregnant women and its relationship between anxiety sensitivity and somatosensory amplification. J Obstet gynaecology: J Inst Obstet Gynecol. 2021;41(2):217–23. doi: 10.1080/01443615.2020.1732894. [DOI] [PubMed] [Google Scholar]
- 9.Huang J, Huang J, Li Y, Liao B. The prevalence and predictors of fear of childbirth among pregnant chinese women: a hierarchical regression analysis. BMC Pregnancy Childbirth. 2021;21(1):643. doi: 10.1186/s12884-021-04123-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Van den Bergh BR, Mulder EJ, Mennes M, Glover V. Antenatal maternal anxiety and stress and the neurobehavioural development of the fetus and child: links and possible mechanisms. A review. Neurosci Biobehav Rev. 2005;29(2):237–58. doi: 10.1016/j.neubiorev.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 11.Schifrin BS, Artenos J, Lyseight N. Late-onset fetal cardiac decelerations associated with fetal breathing movements. J maternal-fetal neonatal medicine: official J Eur Association Perinat Med Federation Asia Ocean Perinat Soc Int Soc Perinat Obstet. 2002;12(4):253–9. doi: 10.1080/jmf.12.4.253.259. [DOI] [PubMed] [Google Scholar]
- 12.Vaajala M, Liukkonen R, Ponkilainen V, Mattila VM, Kekki M, Kuitunen I. Birth rate among women with fear of childbirth: a nationwide register-based cohort study in Finland. Ann Epidemiol. 2023;79:44–8. doi: 10.1016/j.annepidem.2023.01.011. [DOI] [PubMed] [Google Scholar]
- 13.Räisänen S, Lehto SM, Nielsen HS, Gissler M, Kramer MR, Heinonen S. Fear of childbirth in nulliparous and multiparous women: a population-based analysis of all singleton births in Finland in 1997–2010. BJOG: an international journal of obstetrics and gynaecology. 2014;121(8):965–70. doi: 10.1111/1471-0528.12599. [DOI] [PubMed] [Google Scholar]
- 14.Han L, Bai H, Lun B, Li Y, Wang Y, Ni Q. The prevalence of fear of Childbirth and its Association with intolerance of uncertainty and coping Styles among pregnant chinese women during the COVID-19 pandemic. Front Psychiatry. 2022;13:935760. doi: 10.3389/fpsyt.2022.935760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nieminen K, Wijma K, Johansson S, Kinberger EK, Ryding EL, Andersson G, Bernfort L, Wijma B. Severe fear of childbirth indicates high perinatal costs for swedish women giving birth to their first child. Acta Obstet Gynecol Scand. 2017;96(4):438–46. doi: 10.1111/aogs.13091. [DOI] [PubMed] [Google Scholar]
- 16.Vaajala M, Liukkonen R, Kuitunen I, Ponkilainen V, Mattila VM, Kekki M. Factors associated with fear of childbirth in a subsequent pregnancy: a nationwide case-control analysis in Finland. BMC Womens Health. 2023;23(1):34. doi: 10.1186/s12905-023-02185-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mortazavi F, Mehrabadi M. Predictors of fear of childbirth and normal vaginal birth among iranian postpartum women: a cross-sectional study. BMC Pregnancy Childbirth. 2021;21(1):316. doi: 10.1186/s12884-021-03790-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ilska M, Brandt-Salmeri A, Kołodziej-Zaleska A, Banaś E, Gelner H, Cnota W. Factors associated with fear of childbirth among polish pregnant women. Sci Rep. 2021;11(1):4397. doi: 10.1038/s41598-021-83915-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Preis H, Benyamini Y, Eberhard-Gran M, Garthus-Niegel S. Childbirth preferences and related fears - comparison between Norway and Israel. BMC Pregnancy Childbirth. 2018;18(1):362. doi: 10.1186/s12884-018-1997-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Räisänen S, Lehto SM, Nielsen HS, Gissler M, Kramer MR, Heinonen S. Risk factors for and perinatal outcomes of major depression during pregnancy: a population-based analysis during 2002–2010 in Finland. BMJ open. 2014;4(11):e004883. doi: 10.1136/bmjopen-2014-004883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jokić-Begić N, Zigić L, Nakić Radoš S. Anxiety and anxiety sensitivity as predictors of fear of childbirth: different patterns for nulliparous and parous women. J Psychosom Obstet Gynaecol. 2014;35(1):22–8. doi: 10.3109/0167482X.2013.866647. [DOI] [PubMed] [Google Scholar]
- 22.Hou Y, Zhou X, Yao M, Liu S. Fear of childbirth and its predictors in re-pregnant women after cesarean section: a cross-sectional multicenter study in China. BMC Pregnancy Childbirth. 2022;22(1):393. doi: 10.1186/s12884-022-04721-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhou X, Liu H, Li X, Zhang S. Fear of Childbirth and Associated Risk factors in healthy pregnant women in Northwest of China: a cross-sectional study. Psychol Res Behav Manage. 2021;14:731–41. doi: 10.2147/PRBM.S309889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Qiu L, Sun N, Shi X, Zhao Y, Feng L, Gong Y, Yin X. Fear of childbirth in nulliparous women: a cross-sectional multicentre study in China. Women and birth: journal of the Australian College of Midwives. 2020;33(2):e136–41. doi: 10.1016/j.wombi.2019.04.005. [DOI] [PubMed] [Google Scholar]
- 25.Soares RD, Dos Santos M, de Moura FR, Muccillo-Baisch AL, Baisch PRM, Soares MCF. da Silva Júnior FMR: gestational and neonatal outcomes in cities in the largest coal Mining Region in Brazil. Int J Environ Res Public Health 2022, 19(19). [DOI] [PMC free article] [PubMed]
- 26.Graafland N, Essers E, Posthumus A, Gootjes D, Ambrós A, Steegers E, Guxens M. Exposure to outdoor residential noise during pregnancy, embryonic size, fetal growth, and birth outcomes. Environ Int. 2023;171:107730. doi: 10.1016/j.envint.2023.107730. [DOI] [PubMed] [Google Scholar]
- 27.Gao LL, Liu XJ, Fu BL, Xie W. Predictors of childbirth fear among pregnant chinese women: a cross-sectional questionnaire survey. Midwifery. 2015;31(9):865–70. doi: 10.1016/j.midw.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 28.Areskog B, Kjessler B, Uddenberg N. Identification of women with significant fear of childbirth during late pregnancy. Gynecol Obstet Invest. 1982;13(2):98–107. doi: 10.1159/000299490. [DOI] [PubMed] [Google Scholar]
- 29.Lowe NK. Self-efficacy for labor and childbirth fears in nulliparous pregnant women. J Psychosom Obstet Gynaecol. 2000;21(4):219–24. doi: 10.3109/01674820009085591. [DOI] [PubMed] [Google Scholar]
- 30.Tanglakmankhong K, Perrin NA, Lowe NK. Childbirth Self-Efficacy Inventory and Childbirth Attitudes Questionnaire: psychometric properties of thai language versions. J Adv Nurs. 2011;67(1):193–203. doi: 10.1111/j.1365-2648.2010.05479.x. [DOI] [PubMed] [Google Scholar]
- 31.Smilkstein G, Ashworth C, Montano D. Validity and reliability of the family APGAR as a test of family function. J Fam Pract. 1982;15(2):303–11. [PubMed] [Google Scholar]
- 32.Wu F, Zhou L, Chen C, Lin W, Liu P, Huang W, Zhong C, Zhang M, Li Q, Chen Q, et al. Association between intimate partner violence and prenatal anxiety and depression in pregnant women: a cross-sectional survey during the COVID-19 epidemic in Shenzhen, China. BMJ open. 2022;12(5):e055333. doi: 10.1136/bmjopen-2021-055333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hays RD, Chawla N, Kent EE, Arora NK. Measurement equivalence of the Consumer Assessment of Healthcare Providers and Systems (CAHPS(®)) Medicare survey items between Whites and Asians. Qual life research: Int J Qual life aspects Treat care rehabilitation. 2017;26(2):311–8. doi: 10.1007/s11136-016-1383-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Morales LS, Elliott MN, Weech-Maldonado R, Spritzer KL, Hays RD. Differences in CAHPS adult survey reports and ratings by race and ethnicity: an analysis of the National CAHPS benchmarking data 1.0. Health Serv Res. 2001;36(3):595–617. [PMC free article] [PubMed] [Google Scholar]
- 35.Dalgard OS, Dowrick C, Lehtinen V, Vazquez-Barquero JL, Casey P, Wilkinson G, Ayuso-Mateos JL, Page H, Dunn G. Negative life events, social support and gender difference in depression: a multinational community survey with data from the ODIN study. Soc Psychiatry Psychiatr Epidemiol. 2006;41(6):444–51. doi: 10.1007/s00127-006-0051-5. [DOI] [PubMed] [Google Scholar]
- 36.Hammersland MH, Aarsand AK, Sandberg S, Andersen J. Self-efficacy and self-management strategies in acute intermittent porphyria. BMC Health Serv Res. 2019;19(1):444. doi: 10.1186/s12913-019-4285-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Arima M, Takamiya Y, Furuta A, Siriratsivawong K, Tsuchiya S, Izumi M. Factors associated with the mental health status of medical students during the COVID-19 pandemic: a cross-sectional study in Japan. BMJ open. 2020;10(12):e043728. doi: 10.1136/bmjopen-2020-043728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mateus V, Cruz S, Costa R, Mesquita A, Christoforou A, Wilson CA, Vousoura E, Dikmen-Yildiz P, Bina R, Dominguez-Salas S, et al. Rates of depressive and anxiety symptoms in the perinatal period during the COVID-19 pandemic: comparisons between countries and with pre-pandemic data. J Affect Disord. 2022;316:245–53. doi: 10.1016/j.jad.2022.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of Mental Disorders. Patient Health Questionnaire Jama. 1999;282(18):1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 40.Sidebottom AC, Harrison PA, Godecker A, Kim H. Validation of the Patient Health Questionnaire (PHQ)-9 for prenatal depression screening. Arch Women Ment Health. 2012;15(5):367–74. doi: 10.1007/s00737-012-0295-x. [DOI] [PubMed] [Google Scholar]
- 41.Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 42.Pires AC, Fleck MP, Power M, da Rocha NS. Psychometric properties of the EUROHIS-QOL 8-item index (WHOQOL-8) in a brazilian sample. Revista brasileira de psiquiatria (Sao Paulo Brazil: 1999) 2018;40(3):249–55. doi: 10.1590/1516-4446-2017-2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schmidt S, Mühlan H, Power M. The EUROHIS-QOL 8-item index: psychometric results of a cross-cultural field study. Eur J Pub Health. 2006;16(4):420–8. doi: 10.1093/eurpub/cki155. [DOI] [PubMed] [Google Scholar]
- 44.Lukasse M, Schei B, Ryding EL. Prevalence and associated factors of fear of childbirth in six european countries. Sex reproductive healthcare: official J Swed Association Midwives. 2014;5(3):99–106. doi: 10.1016/j.srhc.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 45.Toohill J, Creedy DK, Gamble J, Fenwick J. A cross-sectional study to determine utility of childbirth fear screening in maternity practice - an australian perspective. Women and birth: journal of the Australian College of Midwives. 2015;28(4):310–6. doi: 10.1016/j.wombi.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 46.Stoll K, Edmonds JK, Hall WA. Fear of Childbirth and Preference for Cesarean Delivery among Young American Women before Childbirth: a Survey Study. Birth (Berkeley Calif) 2015;42(3):270–6. doi: 10.1111/birt.12178. [DOI] [PubMed] [Google Scholar]
- 47.Jha P, Larsson M, Christensson K, Svanberg AS. Fear of childbirth and depressive symptoms among postnatal women: a cross-sectional survey from Chhattisgarh, India. Women and birth: journal of the Australian College of Midwives. 2018;31(2):e122–33. doi: 10.1016/j.wombi.2017.07.003. [DOI] [PubMed] [Google Scholar]
- 48.Wang L, Yang N, Zhou H, Mao X, Zhou Y. Pregnant women’s anxiety and depression symptoms and influence factors in the COVID-19 pandemic in Changzhou, China. Front Psychol. 2022;13:855545. doi: 10.3389/fpsyg.2022.855545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Majumdar P, Biswas A, Sahu S. COVID-19 pandemic and lockdown: cause of sleep disruption, depression, somatic pain, and increased screen exposure of office workers and students of India. Chronobiol Int. 2020;37(8):1191–200. doi: 10.1080/07420528.2020.1786107. [DOI] [PubMed] [Google Scholar]
- 50.Kizilirmak A, Calpbinici P. Investigation of the effect of pregnant women’s childbirth-related internet use on fear of childbirth. J Obstet gynaecology: J Inst Obstet Gynecol. 2022;42(7):3007–13. doi: 10.1080/01443615.2022.2125297. [DOI] [PubMed] [Google Scholar]
- 51.Bjelke M, Martinsson AK, Lendahls L, Oscarsson M. Using the internet as a source of information during pregnancy - A descriptive cross-sectional study in Sweden. Midwifery. 2016;40:187–91. doi: 10.1016/j.midw.2016.06.020. [DOI] [PubMed] [Google Scholar]
- 52.Mandar O, Idrees MB, Ahmed A, Hassan NAL, Adam B. I: Prevalence and associated factors of fear for childbirth among pregnant women in eastern Sudan. J reproductive infant Psychol 2021:1–11. [DOI] [PubMed]
- 53.O’Connell MA, Leahy-Warren P, Kenny LC, O’Neill SM, Khashan AS. The prevalence and risk factors of fear of childbirth among pregnant women: a cross-sectional study in Ireland. Acta Obstet Gynecol Scand. 2019;98(8):1014–23. doi: 10.1111/aogs.13599. [DOI] [PubMed] [Google Scholar]
- 54.Soltani F, Eskandari Z, Khodakarami B, Parsa P, Roshanaei G. Factors contributing to fear of childbirth among pregnant women in Hamadan (Iran) in 2016. Electron physician 2017, 9(7):4725–31. [DOI] [PMC free article] [PubMed]
- 55.Vaajala M, Liukkonen R, Kuitunen I, Ponkilainen V, Mattila VM, Kekki M. Trends in the epidemiology of fear of childbirth and association with intended mode of delivery: a nationwide register-based cohort study in Finland. Acta Obstet Gynecol Scand. 2023;102(4):430–7. doi: 10.1111/aogs.14521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Soh YX, Razak N, Cheng LJ, Lau Y. Determinants of childbirth self-efficacy among multi-ethnic pregnant women in Singapore: a structural equation modelling approach. Midwifery. 2020;87:102716. doi: 10.1016/j.midw.2020.102716. [DOI] [PubMed] [Google Scholar]
- 57.Rouhe H, Salmela-Aro K, Halmesmäki E, Saisto T. Fear of childbirth according to parity, gestational age, and obstetric history. BJOG: an international journal of obstetrics and gynaecology. 2009;116(1):67–73. doi: 10.1111/j.1471-0528.2008.02002.x. [DOI] [PubMed] [Google Scholar]
- 58.Nyaruhucha CN. Food cravings, aversions and pica among pregnant women in Dar es Salaam, Tanzania. Tanzan J health Res. 2009;11(1):29–34. [PubMed] [Google Scholar]
- 59.Ochsenbein-Kölble N, von Mering R, Zimmermann R, Hummel T. Changes in gustatory function during the course of pregnancy and postpartum. BJOG: an international journal of obstetrics and gynaecology. 2005;112(12):1636–40. doi: 10.1111/j.1471-0528.2005.00783.x. [DOI] [PubMed] [Google Scholar]
- 60.Atlaw D, Sahiledengle B, Assefa T, Negash W, Tahir A, Regasa T, Tekalegn Y, Mamo A, Enegeda ZT, Solomon D, et al. Incidence and risk factors of gestational diabetes mellitus in Goba town, Southeast Ethiopia: a prospective cohort study. BMJ open. 2022;12(9):e060694. doi: 10.1136/bmjopen-2021-060694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tilahun AG, Kebede AM. Maternal minimum dietary diversity and associated factors among pregnant women. Southwest Ethiopia 2021 BMC nutrition. 2021;7(1):66. doi: 10.1186/s40795-021-00474-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fathi Najafi T, Latifnejad Roudsari R, Ebrahimipour H. The best encouraging persons in labor: a content analysis of iranian mothers’ experiences of labor support. PLoS ONE. 2017;12(7):e0179702. doi: 10.1371/journal.pone.0179702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liu Y, Li T, Guo N, Jiang H, Li Y, Xu C, Yao X. Women’s experience and satisfaction with midwife-led maternity care: a cross-sectional survey in China. BMC Pregnancy Childbirth. 2021;21(1):151. doi: 10.1186/s12884-021-03638-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hendrix Y, Baas MAM, Vanhommerig JW, de Jongh A, Van Pampus MG. Fear of Childbirth in Nulliparous Women. Front Psychol. 2022;13:923819. doi: 10.3389/fpsyg.2022.923819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Takegata M, Haruna M, Morikawa M, Yonezawa K, Komada M, Severinsson E. Qualitative exploration of fear of childbirth and preferences for mode of birth among japanese primiparas. Nurs Health Sci. 2018;20(3):338–45. doi: 10.1111/nhs.12571. [DOI] [PubMed] [Google Scholar]
- 66.Doaltabadi Z, Amiri-Farahani L, Hasanpoor-Azghady SB, Haghani S. The effect of face-to-face and virtual prenatal care training of spouses on the pregnancy experience and fear of childbirth of primiparous women: a controlled quasi-experimental study. J Telemed Telecare 2021:1357633x211024101. [DOI] [PubMed]
- 67.Barrier PA, Li JT, Jensen NM. Two words to improve physician-patient communication: what else? Mayo Clin Proc. 2003;78(2):211–4. doi: 10.4065/78.2.211. [DOI] [PubMed] [Google Scholar]
- 68.Muñoz-Vela FJ, Rodríguez-Díaz L, Gómez-Salgado J, Fernández-Carrasco FJ, Allande-Cussó R, Vázquez-Lara JM, Fagundo-Rivera J. Fear and anxiety in pregnant women during the COVID-19 pandemic: a systematic review. Int J public health. 2023;68:1605587. doi: 10.3389/ijph.2023.1605587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Çıtak Bilgin N, Coşkun H, Coşkuner Potur D, İbar Aydın E, Uca E. Psychosocial predictors of the fear of childbirth in turkish pregnant women. J Psychosom Obstet Gynaecol. 2021;42(2):123–31. doi: 10.1080/0167482X.2020.1734791. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available for ethical reasons but are available from the corresponding author on reasonable request.