Abstract
Background
Surgical site infection (SSI) is a common complication following craniotomy that increases morbidity, mortality, and medical expenses. The objectives of this study were to determine the relevant risk factors associated with SSI after elective craniotomy for brain tumor and analyse the treatments for SSI.
Methods
A retrospective nested case‒control study was conducted using data from patients who underwent craniotomy for brain tumor resection at the Neurosurgical Oncology Department No. 6 of Beijing Tiantan Hospital, Capital Medical University, between January 2019 and December 2021. Risk factors for SSI were determined using multivariate logistic regression analysis. We analyzed microbiological and related treatment data for different SSI types.
Results
Among 2061 patients who underwent craniotomy for brain tumor, 31 had SSI (1.50%). In the multivariate logistic regression analysis, body mass index (BMI) and operative duration were identified as independent risk factors for SSI. The most common microorganism isolated from SSIs was Staphylococcus epidermidis (22.9%), and drug sensitivity results showed that gram-positive bacteria were sensitive to linezolid, vancomycin and tigecycline, whereas gram-negative bacteria were sensitive to meropenem, cefepime and ceftazidime. Six of the seven patients who underwent bone flap removal due to osteomyelitis were infected with gram-negative bacteria.
Conclusions
BMI and operative duration were identified as independent risk factors for SSI. Diabetes mellitus, previous ratio therapy, type of incision, recurrence tumor and other risk factors were not found to be associated with the occurrence of SSI in this study.
Supplementary Information
The online version contains supplementary material available at 10.1186/s41016-023-00336-1.
Keywords: Brain tumor, Elective craniotomy, Neurosurgery, Surgical site infection, Risk factors, Infection control
Background
Surgical site infection (SSI) after elective craniotomy can result in permanent disability, prolonged hospitalization, or unscheduled readmissions, all of which increase health-care expenses [1]. In previous studies, the incidence of SSI after craniotomy ranges from 1.2 to 5.3% [1–16]. Henri et al. reported that SSI after first glioblastoma resection is a severe condition, significantly influencing patient survival [4]. In another study, infection, a surgical complication in neurosurgery, was the most common reason for readmission [17].
To date, only a few studies have particularly focused on the risk factors for SSI after elective craniotomies for brain tumor [18]. We believe it is important to focus on surgical site infections for elective craniotomy for brain tumor. First, the incisions for elective craniotomy are mostly clean incisions compared to cranial trauma surgery and transsphenoidal surgery. Second, compared to patients undergoing cerebrovascular and bypass surgery, brain tumor patients, especially those with malignant brain tumors, have a poorer prognosis based on the disease itself. Therefore, avoiding surgical site infection while pursuing prolonged patient survival is particularly important for elective craniotomy for brain tumor.
Previous studies on SSI after craniotomy have mostly been limited to risk factor analysis, and the identified risk factors include advanced age, diabetes mellitus, malnutrition, preoperative steroid use, preoperative radiation, obesity, the length of surgery, clean-contaminated and contaminated surgery, and a history of recent neurosurgical intervention [13, 19].
The objective of this study was to determine the factors that contribute to the development of SSI after elective craniotomies for brain tumor resection to provide evidence for SSI prevention.
Methods
Baseline characteristics
Patients who underwent craniotomy for brain tumor resection at the neurosurgical oncology department NO. 6, Beijing Tiantan Hospital, Capital Medical University, between January 2019 and December 2021 were retrospectively assessed for this study.
The same operation preparation protocol was followed for all the patients; hair was shaved the day before surgery and skin was prepared preoperatively (using antiseptic iodine and alcohol). Reference Global Guidelines For The Prevention Of Surgical Site Infections (2018) recommendations, while considering the half-life of the antibiotic [20]. All patients (if not allergic) received a single dose of the prophylactic antibiotic intravenous cefuroxime (1.5 g, with a half-life of approximately 80 min) at induction/before skin incision, repeated every 4 h during surgery. Antibiotics are not routinely administered after surgery unless the neurosurgeon suspects, intraoperatively, that the patient is at risk of infection (e.g., mastoid air cells or sinus opening, violation of sterility during surgery, coinfection before surgery).
Definition and classification of SSIs
Researchers have debated the classification and definition of SSIs [4]. Based on the American Centers for Disease Control and Prevention (CDC) criteria for Surgical Site Infection (2017) [21], and in order to make the SSI false-positive rate as low as possible. We defined SSI as a purulent discharge requiring local debridement or osteomyelitis/abscess requiring reoperation, as well as positive cultures from secretion samples or CSF. This is comparable to the definition of SSI used by Sami et al. [12].
We divided SSI into the following three types: SSI-S (superficial infections involving only skin or subcutaneous tissue), SSI-D (deep infections including fascia and/or muscle), and SSI-OS (organ or space infections, such as osteomyelitis, meningitis, ventriculitis, or abscess), for more details on classification criteria, see the Additional Table S1. This is similar to the classification by Stienen et al. [7].
Data collection
Basic data were collected using an electronic medical record system. Demographic data included sex, age, diabetes mellitus, BMI (body mass index: calculated from the height and weight provided in the admission record), previous radiotherapy (yes or no), recurrence (yes or no) and histological diagnoses. Furthermore, the following parameters were collected regarding the operations: consecutive operation (yes or no), type of incision, operative duration (measured from skin incision to last suture/closure), estimated blood loss, and length of postoperative hospital stay. With reference to a meta-analysis involving 26 studies [22] and the data we have collected above, we chose to examine BMI, diabetes mellitus, previous ratio therapy, recurrence tumor, type of incision, operative duration, and estimated blood loss as potential risk factors for SSI after elective craniotomy for brain tumor in this study. Finally, we collected results from microbiological cultures, drug sensitivity results, and the relevant treatment of SSI.
Statistical analysis
Statistical analysis was performed using SPSS 26.0 and GraphPad Prism 8.3.0. A retrospective nested case‒control study was conducted to determine the possible risk factors for SSI. Each case of SSI was matched with two controls based on the following three criteria: age (± 0), sex, and period of procedure (± 12 months). For all variables, between-group comparisons were made using the t test/Wilcoxon rank-sum for continuous variables or the chi-square test/Fisher’s exact test for categorical variables as appropriate. Multivariate analysis using logistic regression to identify independent risk factors. ROC curves were drawn for independent prognostic factors. The best cut-off value was determined using Youden's Index, which maximizes the sum of sensitivity and specificity-1. The AUC of each independent prognostic factor was compared to determine its prognostic value. For descriptive analysis, microbiological cultures, drug sensitivity results and the relevant treatment of SSI were provided. Odds ratios (ORs) were obtained with corresponding 95% confidence intervals (CIs). Statistical significance was defined as P < 0.05.
Results
Prevalence of SSI and comparison of the baseline data
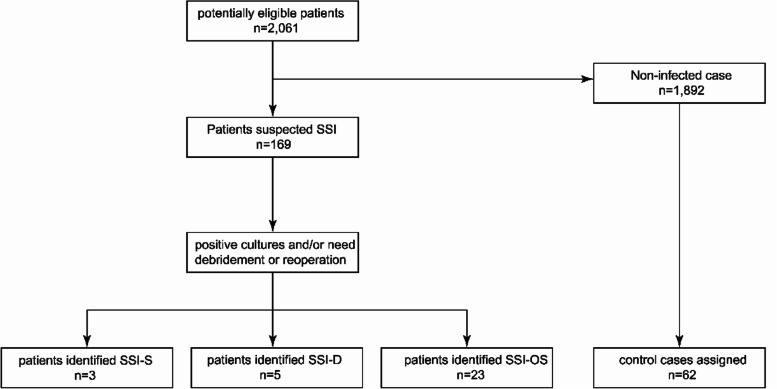
A total of 2061 patients who underwent craniotomy for brain tumor resection between January 2019 and December 2021 met the inclusion criteria. Thirty-one cases of surgical site infections were identified, and 62 matched controls were selected based on three criteria (age, sex, period of procedure) from the remaining cases (Fig. 1). The overall infection rate was 1.50%, which was similar to the SSI rate after craniotomy for brain tumors reported by Laura G. Valentini et al. [16].
Fig. 1.
Summary of patient selection
Table 1 shows a comparison of the basic data of the two groups. Significant differences in BMI (P = 0.007), duration of neurosurgery (p = 0.01), and length of postoperative hospital stay (p < 0.001) were identified in between-group comparisons.
Table 1.
Comparison of baseline characteristics
| Characteristic | Case(n = 31) | Controls(n = 62) | P value |
|---|---|---|---|
| Sex | 1.0a | ||
| Male | 20(64.5%) | 40(64.5%) | |
| Female | 11(35.5%) | 22(35.5%) | |
| Age (years) | 1.0b | ||
| Mean (SD) | 45.9(15.1) | 45.9(15.0) | |
| Median (IQR) | 50(33–57) | 50(33–57) | |
| Range | 17–77 | 17–77 | |
| BMI (kg/m2) | 0.007b | ||
| Mean (SD) | 26.0(4.8) | 23.3(2.9) | |
| Median (IQR) | 25.1(22.6–27.7) | 23.4(21.4, 25.5) | |
| Range | 18.7–41.0 | 15.6–28.6 | |
| Diabetes mellitus (yes or no) | 2(6.5%) | 2(3.2%) | 0.598c |
| Previous ratio-therapy (yes or no) | 3(9.7%) | 2(3.2%) | 0.329c |
| Recurrence tumor (yes or no) | 4(12.9%) | 3(4.8%) | 0.217c |
| Histological diagnosis | 0.495a | ||
| High-grade glioma | 14(45.2%) | 17(27.4%) | |
| Low-grade glioma | 4(12.9%) | 11(17.7%) | |
| Meningiomas | 6(19.4%) | 17(27.4%) | |
| Hemangioblastoma | 2(6.5%) | 1(1.6%) | |
| Metastatic tumor | 0(0%) | 4(6.5%) | |
| Schwannomas | 1(3.2%) | 5(6.5%) | |
| Epidermoid cysts | 1(3.2%) | 2(3.2%) | |
| Other tumors | 3(9.7%) | 6(9.7%) | |
| Type of surgical wound* | 0.745a | ||
| I (Clean) | 28(90.3%) | 53(85.5%) | |
| II (Clean/Contaminated) | 3(9.7%) | 9(14.5%) | |
| Operative duration(h) | 0.001b | ||
| Mean(SD) | 4.6(1.1) | 3.8(1.0) | |
| Median (IQR) | 4.5(4.0, 5.5) | 3.9(3.0, 4.4) | |
| Range | 2.8–6.8 | 1.9–7.0 | |
| Estimated blood loss(ml) | 0.137b | ||
| Mean(SD) | 258.1(200.0) | 211.29(101.4) | |
| Median (IQR) | 200(100, 300) | 200(150, 300) | |
| Range | 100–1200 | 50–600 | |
| Length of post-operative hospital stay (days) | < 0.001b | ||
| Mean(SD) | 28.3(16.1) | 9.7(2.9) | |
| Median (IQR) | 23(20, 31) | 9.0(7.8, 11.0) | |
| Range | 14–94 | 6–20 | |
Abbreviations: BMI Body mass index, SD Standard deviation, IQR Interquartile range
*According to the classification criteria for surgical wound created by the Center for Disease Control and Prevention (I, clean; II, clean/contaminated; III, contaminated; and IV, dirty)
achi-square test
bt test
cFisher’s exact
Risk factors and their predictive value
To determine relevant risk factors associated with SSI, BMI, diabetes mellitus, previous ratio therapy, recurrence tumor, type of incision, operative duration, and estimated blood loss were included in the univariate logistic regression analysis. The results showed that BMI and operative duration were associated with a higher risk of SSI. BMI (OR 1.24, 95% CI 1.06–1.44, p = 0.006) and operative duration (OR 2.09, 95% CI 1.31–3.34, p = 0.002) were also independent risk factors for post-craniotomy SSI according to the multivariate logistic regression analysis (Table 2).
Table 2.
Multivariate analysis for the risk for surgical site infection
| Covariate | B | Wals | p value | OR (95% CI) |
|---|---|---|---|---|
| BMI | 0.21 | 7.52 | 0.006 | 1.24(1.06–1.44) |
| Operative duration | 0.74 | 9.48 | 0.002 | 2.09(1.31–3.34) |
| Constant | − 9.05 | 15.26 | < 0.001 | < 0.001 |
CI Confidence interval, OR Odds ratio, BMI Body mass index
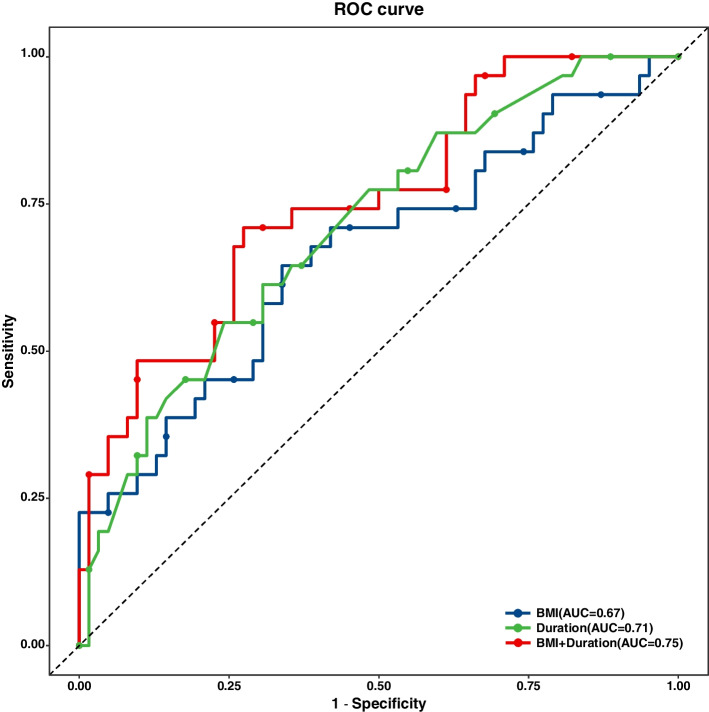
Logistic regression analysis was performed to obtain regression coefficients for independent risk factors, and then ROC analysis of BMI, operative duration, and the combination of the two factors was performed for the predictive evaluation of SSI. The optimal cut-off values of BMI, operative duration, and the combination of the two factors were 24.36 kg/m2, 4.465 h and 30.93, respectively. The AUCs were 0.67, 0.71 and 0.75, respectively. The sensitivity was 64.52%, 54.84%, and 72.58%, respectively. The specificity was 66.13%, 75.81% and 70.97%, respectively (Fig. 2 and Additional Table S2).
Fig. 2.
The ROC curve of BMI, operative duration, and the combination of BMI and operative duration for predictive evaluation for SSI
Pathogenic microorganism results
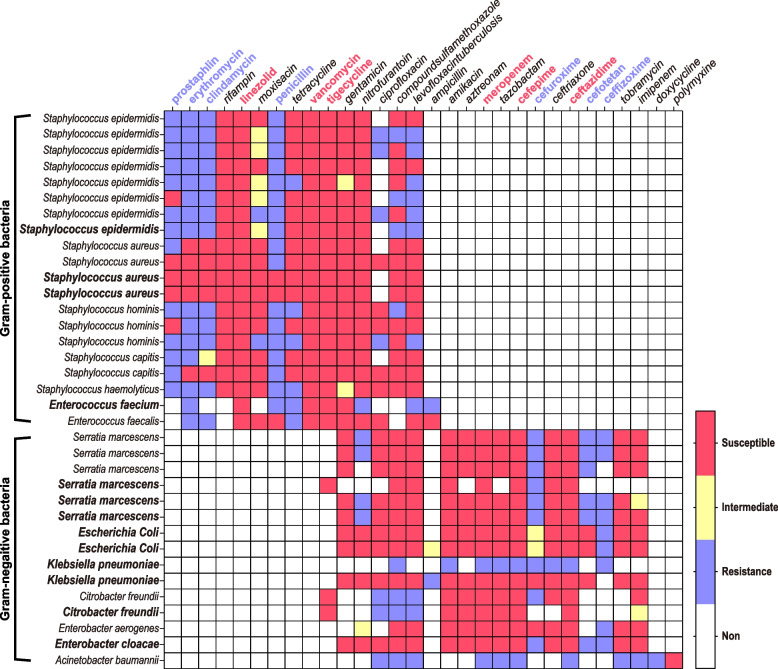
A total of 35 strains of nonrepetitive pathogenic bacteria were collected from the CSF and pyogenic samples, of which 57.1% (20 strains) were gram-positive bacteria and 42.9% (15 strains) were gram-negative bacteria. The most common pathogenic bacteria isolated from SSIs were S. epidermidis (22.9%), followed by Serratia marcescens (17.1%) and Staphylococcus aureus (11.4%). The drug sensitivity results showed that all gram-positive bacteria were sensitive to linezolid, vancomycin, and tigecycline, but most were insensitive to prostaphlin, erythromycin, clindamycin, and penicillin. Except for one strain of Klebsiella and A. baumannii, all gram-negative bacteria were sensitive to meropenem, cefepime and ceftazidime, but most were insensitive to cefuroxime, cefotetan and ceftizoxime (Table 3 and Fig. 3).
Table 3.
Pathogens causing SSI after elective craniotomy for brain tumor
| Specimens resource | |||
|---|---|---|---|
| Pathogenic bacteria | CSF | Pyogenic fluids | Quantity |
| Gram-positive bacteria | 20 (57.1%) | ||
| Staphylococcus epidermidis | 7 | 1 | 8 (22.9%) |
| Staphylococcus aureus | 2 | 2 | 4 (11.4%) |
| Staphylococcus hominis | 3 | 0 | 3 (8.6%) |
| Staphylococcus capitis | 2 | 0 | 2 (5.7%) |
| Staphylococcus hemolyticus | 1 | 0 | 1 (2.9%) |
| Enterococcus faecium | 0 | 1 | 1 (2.9%) |
| Enterococcus faecalis | 1 | 0 | 1 (2.9%) |
| Gram-negative bacteria | 15 (42.9%) | ||
| Serratia marcescens | 3 | 3 | 6 (17.1%) |
| Escherichia Coli | 0 | 2 | 2 (5.7%) |
| Klebsiella pneumoniae | 0 | 2 | 2 (5.7%) |
| Citrobacter freundii | 1 | 1 | 2 (5.7%) |
| Acinetobacter baumannii | 1 | 0 | 1 (2.9%) |
| Enterobacter aerogenes | 1 | 0 | 1 (2.9%) |
| Enterobacter cloacae | 0 | 1 | 1 (2.9%) |
| Total | 22 | 13 | 35 (100%) |
Fig. 3.
The Heatmap of drug sensitivity. In the column labels, bolded font indicates secretion pathogenic bacterial culture and regular font indicates a CSF bacterial culture. In the row labels, red font indicates relatively sensitive antibiotics and blue font represents relatively insensitive antibiotics
Treatment and prognosis of SSI
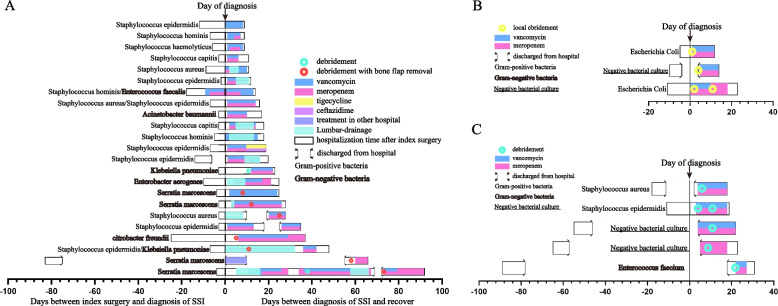
We reviewed and summarized the treatment process of 31 cases of SSI that occurred after elective craniotomy for brain tumors. The treatment process mainly includes antibiotic treatment, lumbar drainage, local anaesthesia for debridement, general anaesthesia for thorough debridement, and bone flap removal due to osteomyelitis. The mean times from operation to SSI-S, SSI-D and SSI-OS were 8.7 days, 47.6 days, and 10.5 days, respectively. The mean times to SSI cure were 16.3 days, 22.6 days, and 25.7 days, respectively. The treatment required for each type of SSI was different. Patients with only positive CSF cultures in SSI-OS require only antibiotics and lumbar drainage. SSI-S requires local anaesthesia for debridement, and SSI-D and brain abscesses in SSI-OS require general anaesthesia for thorough debridement, whereas patients with osteomyelitis even need removal of bone flaps. In addition, it is noteworthy that four of the five SSI-D cases were found to be infected after discharge, and six of the seven patients who had bone flap removal due to osteomyelitis were infected with gram-negative bacteria (Fig. 4 and Additional Table S3).
Fig. 4.
swimming plot. Detailed treatment procedures for different subtypes of SSI. A SSI-OS treatment procedures. B SSI-S treatment procedures. C SSI-D treatment procedures
Discussion
Incidence and classification of SSI
In numerous studies, the rates of SSI after neurosurgery varied due to differences in patient characteristics, operation indication, follow-up time, and SSI criteria [12]. For example, Stienen et al. defined SSI according to CDC standards [7], while Hsiu-Yin et al. defined SSI according to the National Healthcare Safety Network (NHSN) definition of SSI [9]. Consequently, comparing SSI incidence across studies with different criteria and demographics should be done with caution. Defining a universal diagnostic criterion for SSI after craniotomy is both worthwhile and urgent.
Proper classification of SSI is critical because deep or organ/space infections are associated with significantly increased disability and mortality compared with superficial infections. SSI-OS (organ/space infections) accounted for most SSI cases (74.2%) in the current investigation, which is consistent with research by Chiang et al. [9] but different from that reported by Buang et al. [23].
BMI and operative duration
This study shows that the combination of BMI and operative duration has some predictive value but does not yet achieve high accuracy (the AUC of the combination of BMI and duration was 0.75 < 0.90). BMI was identified as an independent risk factor after craniotomy for brain tumor resection in this study. Connor et al. also identified BMI as a significant risk factor for the occurrence of SSI [13]. Adipose tissue has been reported to be insufficiently vascularized, which can make wound healing difficult. Furthermore, macro- and micronutrient deficiencies, which are common in overweight people, can compromise immune system function, thus increasing their risk for SSI [24]. This suggests that during the perioperative period, we should pay attention to overweight patients, as they may be at high risk for SSI.
The operative duration was found to be a significant independent risk factor for neurosurgery in numerous studies [5, 13, 16]. In this study, the operative duration was also found to be a significant independent risk factor for SSI. In a retrospective study of patients who had a craniotomy due to a brain tumor, Hardy et al. discovered that each additional hour spent in surgery resulted in a 43% increase in the odds ratio of developing an SSI [5]. Multiple factors influence the operative duration [16], and the presence of surgical trainees, surgical method and approach, surgeon proficiency, communication and logistics among operative specialists may also be important [1]. More bacteria could enter the incision by several routes, including airborne dissemination, surgical tools, and the patient's skin, as the duration of the operation lengthens [1]. Therefore, neurosurgeons should devise an ideal surgical strategy to efficiently reduce preoperative time.
However, diabetes mellitus, previous ratio therapy, type of incision, recurrence tumor and other risk factors reported in previous studies [19, 25, 26] were not found to be associated with the occurrence of SSI in this study. It is worth noting that diabetes mellitus is a significant predictor in most studies of surgical site infections. Unexpectedly, the results of this study showed that diabetes mellitus was not a risk factor for surgical site infection. We believe this is mainly due to the fact that we have avoided some infections by closely monitoring and strictly controlling the patient's blood glucose in the perioperative period. In addition, the relatively small size of the case group also influenced our findings.
Pathogens causing SSI
Our statistics show that Staphylococcus species were the predominant microorganisms found in surgical site infections, similar to previous studies [6]. This demonstrated that the skin flora is the major source of infection. The results of our study suggest that single-shot antibiotic prophylaxis before surgery and routine dressing change after surgery at an appropriate frequency are of great importance.
It should be noted that although gram-negative bacteria are less common than gram-positive bacteria, they cause heavier infections. For example, six of the seven cases of osteomyelitis were infected by Gram-negative bacteria, suggesting a predisposition to cranial osteomyelitis when Gram-negative bacteria are infected. Therefore, to prevent the occurrence of osteomyelitis, radical treatment with early application of high-level antibiotics or thorough debridement should be undertaken when Gram-negative infection is suspected or confirmed.
In addition, analysis of the tumor composition of SSI patients revealed that there was no metastatic tumor in SSI cases. A recent study by Aikun Fu et al. found that intracellular bacteria in breast cancer tissues play a key role in the process of tumor metastasis [27], which suggests that intracellular bacteria no longer have a propensity for infection, but based on the small sample size of this study, evidence supporting this view is limited.
Treatment of SSI
Due to additional treatment for SSI, the length of postoperative hospital stay and readmission rates can increase significantly. In this study, the mean length of postoperative hospital stay (28.3 ± 16.1) of patients with SSI was significantly longer than that of the control group (9.7 ± 2.9), and the maximum length of hospitalization for SSI treatment was 92 days. Ten out of 31 patients were readmitted for SSI treatment. Seven SSI patients underwent bone flap removal due to osteomyelitis, and some of them later underwent costly cranioplasty surgery. All these findings illustrate the high health care cost of SSI and the decreased well-being of the patient. It is therefore particularly crucial to identify patients at high risk of SSI for prevention.
In addition, it is important to know that the different subtypes are not independent of each other; SSI-S (superficial infection) may progress to SSI-D (deep infection), and deep infection may continue to progress to osteomyelitis or abscess in SSI-OS, so early diagnosis and treatment are extremely important. Based on the drug sensitivity results, it is certain that vancomycin combined with meropenem can treat almost all SSI-associated pathogens, and when vancomycin or meropenem allergies exist, we can use tigecycline and ceftazidime to replace these medications, respectively.
Limitation
There are a few limitations in our study. First, only patients requiring local debridement or reoperation due to suspected infection or those with positive bacterial culture results were examined. Consequently, superficial infections that heal spontaneously or require only simple treatment in outpatient clinics are procedurally neglected. This means that the rate of SSI in our study was lower than the actual value, mainly because of the losses from SSI-S. Second, there were 45.2% of high-grade gliomas in the infected cases compared to 27.4% of controls, which may be due to reasons such as post-operative radiotherapy or their own poorer status. But based on the clinical data that could be collected so far, we do not have sufficient evidence to explain why there were more glioma patients in the infected cases, which requires further clinical research. Thirdly, this study was a single canter study and focused on surgical site infections following elective craniotomy for brain tumor. Therefore, the sample size is limited and the results are only applicable to elective craniotomy. Future multicenter studies on surgical site infections for brain tumor after elective craniotomy are expected to be conducted.
Conclusions
There are few reports on the risk factors for SSI after elective craniotomy for brain tumor resection. This study provides some basis for neurosurgeons to prospectively identify high-risk groups and to better understand the required treatment for SSI.
In the current study, BMI and operative duration were identified as independent risk factors for SSI, and the combination of BMI and operative duration has some predictive value for SSI. The most common pathogenic bacteria isolated from SSIs were S. epidermidis, followed by S. marcescens and S. aureus. Gram-negative bacterial infections in SSI-OS are prone to complicate osteomyelitis. The drug sensitivity results show that empirical application of vancomycin combined with meropenem can treat almost all SSI-associated pathogens. The treatment required for each type of SSI is different, and early diagnosis and treatment are extremely important.
Supplementary Information
Additional file 1: Additional Table S1. Surgical site infection criteria. Additional Table S2. Predictive value of BMI, duration of surgery and the combination of them for SSI. Additional Table S3. Treatment of Surgical site infection.
Acknowledgements
We are very grateful to the nursing team in the operating room and neurosurgical oncology department No. 6 of Beijing Tiantan Hospital for their efforts in controlling infection. We are very grateful to the Department of Infection of Beijing Tiantan Hospital for their support of this study.
Abbreviations
- SSI
Surgical site infections
- SSI-S
Superficial infections of SSI
- SSI-D
Deep infections of SSI
- SSI-OS
Organ or space infections of SSI
- BMI
Body mass index
- CSF
Cerebro-spinal fluid
- SD
Standard deviation
- IQR
Interquartile range
- CI
Confidence interval
- OR
Odds ratio
Authors’ contributions
YL: investigation, formal analysis, visualization, writing—original draft. XM: conceptualization, writing—review and editing. YD: formal analysis, visualization. LY: JC, and NJ: validation, formal analysis. SH: conceptualization supervision, writing—reviewing and editing. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This research study was conducted retrospectively from data obtained for clinical purposes and was approved by the Ethics Committee of Beijing Tiantan Hospital (KY2014-021–02).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Cassir N, De La Rosa S, Melot A, Touta A, Troude L, Loundou A, Richet H, Roche PH. Risk factors for surgical site infections after neurosurgery: a focus on the postoperative period. Am J Infect Control. 2015;43(12):1288–1291. doi: 10.1016/j.ajic.2015.07.005. [DOI] [PubMed] [Google Scholar]
- 2.Schipmann S, Akalin E, Doods J, Ewelt C, Stummer W, Suero Molina E. When the infection hits the wound: matched case-control study in a neurosurgical patient collective including systematic literature review and risk factors analysis. World neurosurgery. 2016;95:178–189. doi: 10.1016/j.wneu.2016.07.093. [DOI] [PubMed] [Google Scholar]
- 3.Schipmann S, Brix T, Varghese J, Warneke N, Schwake M, Brokinkel B, Ewelt C, Dugas M, Stummer W. Adverse events in brain tumor surgery: incidence, type, and impact on current quality metrics. Acta Neurochir (Wien) 2019;161(2):287–306. doi: 10.1007/s00701-018-03790-4. [DOI] [PubMed] [Google Scholar]
- 4.Salle H, Deluche E, Couve-Deacon E, Beaujeux AC, Pallud J, Roux A, Dagain A, de Barros A, Voirin J, Seizeur R, et al. Surgical site infections after glioblastoma surgery: results of a multicentric retrospective study. Infection. 2021;49(2):267–275. doi: 10.1007/s15010-020-01534-0. [DOI] [PubMed] [Google Scholar]
- 5.Hardy SJ, Nowacki AS, Bertin M, Weil RJ. Absence of an association between glucose levels and surgical site infections in patients undergoing craniotomies for brain tumors. J Neurosurg. 2010;113(2):161–166. doi: 10.3171/2010.2.JNS09950. [DOI] [PubMed] [Google Scholar]
- 6.Davies BM, Jones A, Patel HC. Implementation of a care bundle and evaluation of risk factors for surgical site infection in cranial neurosurgery. Clin Neurol Neurosurg. 2016;144:121–125. doi: 10.1016/j.clineuro.2016.03.025. [DOI] [PubMed] [Google Scholar]
- 7.Stienen MN, Moser N, Krauss P, Regli L, Sarnthein J. Incidence, depth, and severity of surgical site infections after neurosurgical interventions. Acta Neurochir (Wien) 2019;161(1):17–24. doi: 10.1007/s00701-018-3745-z. [DOI] [PubMed] [Google Scholar]
- 8.Bekelis K, Coy S, Simmons N. Operative duration and risk of surgical site infection in neurosurgery. World neurosurgery. 2016;94:551–555. doi: 10.1016/j.wneu.2016.07.077. [DOI] [PubMed] [Google Scholar]
- 9.Chiang HY, Kamath AS, Pottinger JM, Greenlee JD, Howard MA, 3rd, Cavanaugh JE, Herwaldt LA. Risk factors and outcomes associated with surgical site infections after craniotomy or craniectomy. J Neurosurg. 2014;120(2):509–521. doi: 10.3171/2013.9.JNS13843. [DOI] [PubMed] [Google Scholar]
- 10.Patel S, Thompson D, Innocent S, Narbad V, Selway R, Barkas K. Risk factors for surgical site infections in neurosurgery. Ann R Coll Surg Engl. 2019;101(3):220–225. doi: 10.1308/rcsann.2019.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Uzuka T, Takahashi H, Nakasu Y, Okuda T, Mitsuya K, Hayashi N, Hirose T, Kurai H. Surgical site infection after malignant brain tumor resection: a multicenter study for induction of a basic care bundle. Neurol Med Chir (Tokyo) 2017;57(10):542–547. doi: 10.2176/nmc.oa.2017-0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abu Hamdeh S, Lytsy B, Ronne-Engstrom E. Surgical site infections in standard neurosurgery procedures- a study of incidence, impact and potential risk factors. Br J Neurosurg. 2014;28(2):270–275. doi: 10.3109/02688697.2013.835376. [DOI] [PubMed] [Google Scholar]
- 13.Wathen C, Kshettry VR, Krishnaney A, Gordon SM, Fraser T, Benzel EC, Modic MT, Butler S, Machado AG. The association between operating room personnel and turnover with surgical site infection in more than 12 000 neurosurgical cases. Neurosurgery. 2016;79(6):889–894. doi: 10.1227/NEU.0000000000001357. [DOI] [PubMed] [Google Scholar]
- 14.Chen C, Zhang B, Yu S, Sun F, Ruan Q, Zhang W, Shao L, Chen S. The incidence and risk factors of meningitis after major craniotomy in China: a retrospective cohort study. PLoS ONE. 2014;9(7):e101961. doi: 10.1371/journal.pone.0101961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grundy TJ, Davies BM, Patel HC. When should we measure surgical site infection in patients undergoing a craniotomy? A consideration of the current practice. Br J Neurosurg. 2020;34(6):621–625. doi: 10.1080/02688697.2019.1645298. [DOI] [PubMed] [Google Scholar]
- 16.Valentini LG, Casali C, Chatenoud L, Chiaffarino F, Uberti-Foppa C, Broggi G. Surgical site infections after elective neurosurgery: a survey of 1747 patients. Neurosurgery. 2008;62(1):88–95. doi: 10.1227/01.NEU.0000311065.95496.C5. [DOI] [PubMed] [Google Scholar]
- 17.Buchanan CC, Hernandez EA, Anderson JM, Dye JA, Leung M, Buxey F, Bergsneider M, Afsar-Manesh N, Pouratian N, Martin NA. Analysis of 30-day readmissions among neurosurgical patients: surgical complication avoidance as key to quality improvement. J Neurosurg. 2014;121(1):170–175. doi: 10.3171/2014.4.JNS13944. [DOI] [PubMed] [Google Scholar]
- 18.Nair SK, Botros D, Chakravarti S, Mao Y, Wu E, Lu B, Liu S, Elshareif M, Jackson CM, Gallia GL, et al. Predictors of surgical site infection in glioblastoma patients undergoing craniotomy for tumor resection. J Neurosurg. 2022:138(5):1227-34. [DOI] [PubMed]
- 19.Korinek AM. Risk factors for neurosurgical site infections after craniotomy: a prospective multicenter study of 2944 patients. The French Study Group of Neurosurgical Infections, the SEHP, and the C-CLIN Paris-Nord. Service Epidémiologie Hygiène et Prévention. Neurosurgery. 1997;41(5):1073–1079. doi: 10.1097/00006123-199711000-00010. [DOI] [PubMed] [Google Scholar]
- 20.WHO . Global guidelines for the prevention of surgical site infection. 2. Geneva: World Health Organization; 2018. [PubMed] [Google Scholar]
- 21.O'Hara LM, Thom KA, Preas MA. Update to the centers for disease control and prevention and the healthcare infection control practices advisory committee guideline for the prevention of surgical site infection (2017): a summary, review, and strategies for implementation. Am J Infect Control. 2018;46(6):602–609. doi: 10.1016/j.ajic.2018.01.018. [DOI] [PubMed] [Google Scholar]
- 22.Fang C, Zhu T, Zhang P, Xia L, Sun C. Risk factors of neurosurgical site infection after craniotomy: a systematic review and meta-analysis. Am J Infect Control. 2017;45(11):e123–e134. doi: 10.1016/j.ajic.2017.06.009. [DOI] [PubMed] [Google Scholar]
- 23.Buang SS, Haspani MS. Risk factors for neurosurgical site infections after a neurosurgical procedure: a prospective observational study at Hospital Kuala Lumpur. Med J Malaysia. 2012;67(4):393–398. [PubMed] [Google Scholar]
- 24.Pierpont YN, Dinh TP, Salas RE, Johnson EL, Wright TG, Robson MC, Payne WG. Obesity and surgical wound healing: a current review. ISRN Obes. 2014;2014:638936. doi: 10.1155/2014/638936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Korinek AM, Golmard JL, Elcheick A, Bismuth R, van Effenterre R, Coriat P, Puybasset L. Risk factors for neurosurgical site infections after craniotomy: a critical reappraisal of antibiotic prophylaxis on 4,578 patients. Br J Neurosurg. 2005;19(2):155–162. doi: 10.1080/02688690500145639. [DOI] [PubMed] [Google Scholar]
- 26.Kourbeti IS, Jacobs AV, Koslow M, Karabetsos D, Holzman RS. Risk factors associated with postcraniotomy meningitis. Neurosurgery. 2007;60(2):317–325. doi: 10.1227/01.NEU.0000249266.26322.25. [DOI] [PubMed] [Google Scholar]
- 27.Fu A, Yao B, Dong T, Chen Y, Yao J, Liu Y, Li H, Bai H, Liu X, Zhang Y, et al. Tumor-resident intracellular microbiota promotes metastatic colonization in breast cancer. Cell. 2022;185(8):1356–1372.e1326. doi: 10.1016/j.cell.2022.02.027. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Additional Table S1. Surgical site infection criteria. Additional Table S2. Predictive value of BMI, duration of surgery and the combination of them for SSI. Additional Table S3. Treatment of Surgical site infection.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.