Abstract
Background
The relationship between adverse childhood experiences (ACEs) and adverse adulthood experiences (AAEs) and their association with incident cardiovascular disease (CVD) have not been extensively studied. Considering social support, we evaluated the complex relations of ACEs and AAEs with incident CVD.
Methods
This prospective cohort study used data from the 2014 life course survey and the 2015 and 2018 surveys of the China Health and Retirement Longitudinal Study, a national survey of Chinese adults aged ≥ 45 years from 28 provinces across China. The study population included 5836 individuals (mean [SD] age, 59.59 [8.22] years, 49.7% were males). Information on ACEs, AAEs, young adulthood social support, health behavior factors, health status factors, and demographics was measured. Cox regression models, the difference method to estimate the mediation proportion, and the additive and multiplicative interactions were performed. Subgroup and sensitivity analyses were also conducted.
Results
During follow-up, 789 incident cases of CVD occurred. The fully adjusted model, including demographics, health behaviors, health status factors (e.g., depressive symptoms), and social support as control variables, demonstrated that the overall number of ACEs (Hazard ratio [HR]: 1.11, 95% CI: 1.08 to 1.14) and AAEs (HR: 1.19, 95% CI: 1.16 to 1.22) were associated with an increased risk of incident CVD. A dose–response relationship existed between the number of ACEs or AAEs and incident CVD risk. The overall AAEs were found to mediate 17.7% (95% CI: 8.2 to 34.2%) of the association between ACEs and incident CVD. Moreover, a significant additive interaction between ACEs and AAEs was detected (RERI [95% CI]: 0.32 [0.09 to 0.56]). Compared with adults without exposure to both ACE and AAE, those with exposure to both at least one ACE and one AAE indicator had the highest risk of incident CVD (HR: 1.96, 95% CI: 1.72 to 2.23).
Conclusions
Exposure to ACEs or AAEs was independently associated with an increased risk of incident CVD among Chinese middle-aged and older adults in a dose–response manner, and the overall AAEs partially mediated the association between ACEs and incident CVD. Preventive measures aimed at addressing either ACEs or AAEs alone may not significantly reduce the risk of CVD later in life. The necessity of a comprehensive life-course health strategy targeting the prevention of adversity merits increased attention.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12916-023-03015-1.
Keywords: Adverse childhood experience, Adverse adulthood experience, New-onset cardiovascular disease, Cohort study
Background
Cardiovascular diseases (CVDs) are the leading global cause of mortality and a significant contributor to disability [1]. The World Health Organization defines CVD as a group of disorders of the heart and blood vessels, including stroke, coronary heart disease, and other related conditions [2]. Recent studies have highlighted the association between adverse childhood experiences (ACEs) and a series of cardiovascular risk factors [3, 4] and events later in life [5–7]. ACEs refer to a broad range of potentially stressful experiences during childhood and adolescence [8]. The American Heart Association (AHA) has issued scientific and policy statements recognizing the impact of ACEs on cardiometabolic health throughout the life course [9, 10]. The AHA statement proposes potential pathways that link ACEs and CVD by affecting health behaviors, such as smoking and physical inactivity, pathophysiological factors like the dysregulation of the nervous, immune system, and neuroendocrine systems, and psychological factors [10]. These pathways have been supported by a recent review [5] and several studies [11, 12].
In addition, exposure to ACEs may heighten the risk of encountering adversities and perceived burdensomeness in adulthood [13, 14]; and adverse adulthood experiences (AAEs) may act as triggers in the association between ACEs and adult health [15]. However, critical knowledge gaps remain. First, few studies have concurrently investigated the impacts of ACEs and AAEs on subsequent CVDs. Research on the interaction and joint associations of ACEs and AAEs with cardiovascular health is limited, and results are inconsistent. A recent cross-sectional study revealed that childhood adversity and adulthood stressful life events are significantly and independently linked to cardiovascular health in German adults, without interactions between childhood adversity and adulthood stressful life events [16]. In contrast, a previous longitudinal study using a single variable (i.e., adulthood neighborhood disadvantage) to represent individual-level AAEs found the combined effects of childhood psychosocial adversity and neighborhood disadvantage on incident CVD among Finnish adults [7]. Second, although AAEs may be mediators between ACEs and CVDs, few studies have constructed pathway models linking ACEs, AAEs, and subsequent CVDs, and the extent to which the overall AAEs mediate the association between ACEs and incident CVD remains to be explored. Third, it is unclear whether the findings are consistent across subpopulations of different ages and sex.
According to the social support models proposed by Cohen and Wills, good social support can directly or indirectly mitigate the negative impacts of stressful events through both its structural aspects, such as the existence of relationships, and its functional aspects, which involve perceived supports that address the needs arising from stressful events [17]. Despite this knowledge, the role of social support in mitigating the adverse effects of ACEs or AAEs on cardiometabolic health has not received sufficient attention [18, 19]. Therefore, it is hypothesized that social support may serve as a covariate or modifier in the associations of ACEs and AAEs with incident CVD. Using data from the China Health and Retirement Longitudinal Study (CHARLS) and taking into account the influence of social support, this study has three main objectives: firstly, to investigate the associations of ACEs and AAEs with incident CVD; secondly, to estimate the extent to which the overall AAEs mediate the association between ACEs and incident CVD; and finally, to explore potential interactions or joint relations of ACEs and AAEs on incident CVD.
Methods
Study population
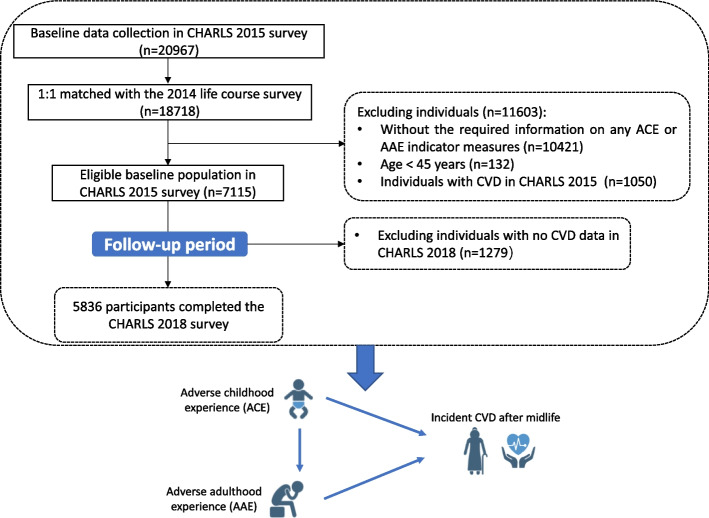
This cohort study was a secondary analysis of the data from the CHARLS, an ongoing nationally representative cohort study among Chinese adults aged ≥ 45 years from 450 villages or resident communities within 28 provinces across China [20]. The study has conducted four main surveys, with the first wave being launched in 2011, and follow-up surveys in 2013, 2015, and 2018. Information on ACEs, AAEs, and young adulthood social support was additionally collected during the 2014 life course survey among all living respondents in the 2011 and 2013 waves surveys. The details of the CHARLS survey have been previously reported [20, 21]. The current study utilized data from the 2014 life course survey and the 2015 and 2018 main surveys of CHARLS. As described in the Additional file 1: Appendix. S1 and Fig. 1, 7115 adults in the 2015 main survey (baseline) have information from the 2014 life course survey. We excluded those without the required information on any ACE or AAE indicator measures (N = 10,421), aged below 45 years or without age information (N = 132), with CVD in the CHARLS 2015 survey (N = 1050), and with no CVD data in the CHARLS 2018 survey (N = 1279); our final cohort comprised 5836 individuals.
Fig. 1.
Flowchart depicting the study design and derivation of the study population
Measures
Adverse childhood and adulthood experiences
In accordance with previous literature about ACE that established their significant implications for health and social outcomes [5, 8, 22, 23], this study extracted ten widely used ACE indicators. Briefly, we defined three domains of ACEs, including the household dysfunction domain (household substance use, household mental illness, domestic violence, criminal behavior in the household, parental separation or divorce, and parental death), neglect and abuse domains (physical neglect, emotional neglect, and physical abuse), and additional ACE domain (exposure to natural disasters). All ACE indicators are defined in Additional file 2: Tab. S1, and responses to each indicator were dichotomized. The ten indicators were summed to generate a cumulative ACE score for each individual, resulting in a cumulative score ranging from 0 to 10. Based on the cumulative numbers of ACE, participants were categorized into five groups: 0, 1, 2, 3, and 4 or more ACEs [5, 23]. Based on previous literature [24], this study extracted five AAE indicators from the CHARLS dataset, including experiencing the death of the child, lifetime discrimination, ever being confined to bed, ever being hospitalized for a month or longer, and ever leaving a job due to health conditions. The details of questions and responses for each factor are outlined in Additional file 2: Tab. S1. Responses to each indicator were dichotomized and summed to generate a cumulative AAE score for each individual, ranging from 0 to 5. Participants were further classified into five groups based on the cumulative numbers of AAE: 0, 1, 2, 3, and 4 or more AAEs. The assessment of ACE or AAE has been extensively employed in previous studies [5, 8, 10, 12, 15, 24–28].
Ascertainment of incident CVD events
Following previous research utilizing the CHARLS dataset [29, 30], the study outcome was incident CVD events during the follow-up period, and the following standardized questions assessed incident CVD events: “Have you been told by a doctor that you have been diagnosed with a heart attack, angina, coronary heart disease, heart failure, or other heart problems?” or “Have you been told by a doctor that you have been diagnosed with a stroke?”. Participants reporting heart disease or stroke during the follow-up period were defined as having incident CVD. The follow-up time was measured as the time elapsed from the date of the last interview to either the date of CVD diagnosis or the date of the latest interview (March 2019) in which the individual participated.
Other covariates
Demographic and health-related data were collected through face-to-face interviews. Demographic information included age, sex (male or female), residential area (rural or urban), marital status (married or other marital status, including never married, separated, divorced, and widowed), and educational level (no formal education, primary school or below, middle or high school, or college or above). Health behavior factors included smoking and alcohol consumption (never, former, or current) and physical activity. Health status factors consisted of body mass index (BMI), depressive symptoms, self-reported physician-diagnosed health conditions (hypertension, diabetes, dyslipidemia, and chronic kidney disease), and the use of medications or therapies for hypertension, diabetes, and dyslipidemia. Further details on the definitions of these covariates can be found in Additional file 1: Appendix. S1 [31–33].
Young adulthood social support, encompassing economic, noneconomic, and emotional support, was also assessed in the CHARLS dataset through the following questions [34], “when you were a young adult, was there anyone who provided you with financial support for your work?”, “when you were a young adult, was there anyone who provided you with positive nonfinancial support for work?”, and “when you were a young adult, was there anyone who provided you with positive support or mentoring for your interpersonal relationship?”. Responses were dichotomized, and a total score ranging from 0 to 3 was calculated, with higher scores indicating greater social support [34].
A sub-cohort of 4113 individuals underwent assessments of metabolic biomarkers. These included fasting plasma glucose, glycosylated hemoglobin (HbA1c), total cholesterol, triglycerides, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, high-sensitivity C-reactive protein (hs-CRP), and serum creatinine. The estimated glomerular filtration rate (eGFR) was calculated using the 2009 creatinine equation from the Chronic Kidney Disease Epidemiology Collaboration [35].
Statistical analysis
Descriptive statistics are presented as means with standard deviations (SDs) or median with interquartile range (IQR) for continuous variables and frequency with percentage for categorical variables. First, the baseline characteristics were summarized for different levels of ACEs and AAEs, and differences among groups were tested using appropriate statistical tests such as the chi-square test, analysis of variance, or Kruskal–Wallis test.
Second, in this study, 837 of 5836 data items were missing and were imputed using the multiple imputations of chained equations method with baseline characteristics. Ten imputed data sets were created, and the main analyses were applied to these sets [36]. The incidence rates of CVD per 1000 person-years were calculated, and Cox proportional hazard regression models were used to estimate the hazard ratios (HRs) and 95% confidence intervals (CIs) of outcomes associated with ACE and AAE levels. Four models were estimated based on previous literature [29, 37], where model 1 was adjusted for age and sex; model 2 was adjusted for age, sex, residence, marital status, educational level, and health behaviors (physical activity, smoking status, and alcohol consumption); model 3 was adjusted for the variables in model 2 plus health status variables (BMI; history of diabetes, hypertension, dyslipidemia, and chronic kidney disease; use of diabetes medications, hypertension medications, and lipid-lowering therapy; and depressive symptoms); model 4 was adjusted for the variables in model 3 and additionally added young adulthood social support.
Third, to explore the role of AAEs in the ACEs and incident CVD relationship, we employed the difference method to estimate the proportion of mediation by the overall AAEs for the association between ACEs and incident CVD by comparing the estimates from models without and with the hypothesized mediator [38]. Additionally, we calculated the C statistics of the two models to compare the predictions with and without adjusting for the overall AAEs [39].
Fourth, we examined the joint associations of ACEs and AAEs by categorizing ACEs and AAEs levels into two categories: those who did not report any ACE or AAE (0) and those who reported at least one ACE or AAE (≥ 1 indicator). Participants were then divided into four groups based on their combined ACEs and AAEs status. To assess the additive and multiplicative interactions between ACEs and AAEs, we included a product interaction term (ACEs × AAEs) in model 4, and the HR (95% CI) of the product term was used to measure interaction on the multiplicative scale. The relative excess risk due to interaction (RERI) with 95% CI was also calculated as a measure of interaction on the additive scale, using the regression coefficients and covariance matrix [40].
Young adulthood social support, sex, and age were also tested as effect modifiers in models 1 through 3, with a product interaction term (ACEs/ AAEs × young adulthood social support/sex/age) fitted. Moreover, to explore potential variations in different subgroups, we conducted subgroup analyses by sex (males and females) and age groups (< 60 years and ≥ 60 years, defined as elders by the World Health Organization [41]).
Three sensitivity analyses were also performed to test the robustness of the findings: (1) we further adjusted for metabolic biomarkers in the subgroup of 4113 participants who underwent metabolic examinations; (2) we used each ACE or AAE indicator separately instead of the overall accumulation of ACEs or AAEs indicators in the models. This allowed us to determine if the results remained consistent with those of the main analyses and provided additional insights into which specific ACEs or AAEs might have significant impacts on incident CVD; (3) we repeated all analyses using the complete dataset (4996 participants).
All analyses were conducted using SAS (version 9.3, SAS Institute, Cary, NC) and Stata (version 17.0, StataCorp, College Station, TX, USA). Two-sided P < 0.05 was considered statistically significant.
Results
Characteristics of the study population
Table 1 depicts the baseline characteristics of the study population stratified by the number of ACEs, while Additional file 2: Tab. S2 presents the baseline characteristics stratified by the number of AAEs. The study included 5836 participants, with a mean (SD) age of 59.59 (8.22) years, and 49.7% were males. Of the total population, 80.5% had been exposed to at least one ACE indicator, 36.2% had been exposed to at least one AAE indicator, and 30.9% had been exposed to both ACEs and AAEs, shown in Additional file 3: Fig. S1. Participants exposed to one or more ACEs or AAEs indicators were more likely to be older, living in rural areas, unmarried, less educated, current smokers/drinkers, and have higher depressive symptoms scores than those without exposure. We also observed an increasing trend in the prevalence rates of hypertension and chronic kidney disease as the number of ACEs indicators increased.
Table 1.
Baseline characteristics of the study population by the number of adverse childhood experiences (ACEs)
| Characteristics | Total | Number of ACEs indicators (N = 5836) | |||||
|---|---|---|---|---|---|---|---|
| 0 (n = 1137) | 1 (n = 2095) | 2 (n = 1388) | 3 (n = 821) | ≥ 4 (n = 395) | P valuea | ||
| Age, mean (SD), years | 59.6 (8.2) | 56.3 (8.3) | 59.8 (7.9) | 60.7 (8.0) | 60.8 (8.2) | 61.4 (7.9) | < 0.001 |
| Sex, n (%) | |||||||
| Male | 2901 (49.7) | 486 (42.7) | 1080 (51.6) | 723 (52.1) | 414 (50.4) | 198 (50.1) | < 0.001 |
| Female | 2935 (50.3) | 651 (57.3) | 1015 (48.4) | 665 (47.9) | 407 (49.6) | 197 (49.9) | |
| Residential areab, n (%) | |||||||
| Rural | 4799 (82.2) | 879 (77.3) | 1677 (80.0) | 1187 (85.6) | 704 (85.7) | 352 (89.1) | < 0.001 |
| Urban | 1036 (17.8) | 258 (22.7) | 418 (20.0) | 200 (14.4) | 117 (14.3) | 43 (10.9) | |
| Marital status | |||||||
| Married | 4972 (85.2) | 995 (87.5) | 1808 (86.3) | 1166 (84.0) | 681 (82.9) | 322 (81.5) | 0.003 |
| Other marital status | 864 (14.8) | 142 (12.5) | 287 (13.7) | 222 (16.0) | 140 (17.1) | 73 (18.5) | |
| Educational levelb, n (%) | |||||||
| No formal education | 2288 (39.2) | 315 (27.7) | 737 (35.2) | 599 (43.2) | 417 (50.8) | 220 (55.7) | < 0.001e |
| Primary school or below | 1348 (23.1) | 231 (20.3) | 504 (24.1) | 342 (24.7) | 185 (22.5) | 86 (21.8) | |
| Middle or high school | 2079 (35.6) | 548 (48.2) | 804 (38.4) | 429 (30.9) | 213 (25.9) | 85 (21.5) | |
| College or above | 117 (2.0) | 43 (3.8) | 47 (2.2) | 17 (1.2) | 6 (0.7) | 4 (1.0) | |
| Smoking statusb, n (%) | |||||||
| Nonsmoker | 3509 (62.2) | 770 (69.8) | 1229 (60.6) | 792 (59.3) | 484 (60.9) | 234 (61.3) | < 0.001 |
| Former smoker | 398 (7.1) | 60 (5.4) | 142 (7.0) | 107 (8.0) | 58 (7.3) | 31 (8.1) | |
| Current smoker | 1735 (30.8) | 273 (24.8) | 656 (32.4) | 436 (32.7) | 253 (31.8) | 117 (30.6) | |
| Alcohol consumptionb, n (%) | |||||||
| Nondrinker | 3399 (58.7) | 705 (62.7) | 1245 (59.9) | 777 (56.2) | 452 (55.3) | 220 (56.0) | 0.011 |
| Former drinker | 504 (8.7) | 92 (8.2) | 176 (8.5) | 115 (8.3) | 84 (10.3) | 37 (9.4) | |
| Current drinker | 1891 (32.6) | 328 (29.2) | 656 (31.6) | 490 (35.5) | 281 (34.4) | 136 (34.6) | |
| Physical activity (≥ 3 × a week)b, n (%) | |||||||
| Yes | 4939 (84.6) | 973 (85.6) | 1786 (85.3) | 1182 (85.2) | 677 (82.5) | 321 (81.3) | 0.088 |
| No | 897 (15.4) | 164 (14.4) | 309 (14.7) | 206 (14.8) | 144 (17.5) | 74 (18.7) | |
| Health conditions (yes)b, n (%) | |||||||
| Diabetes | 258 (4.5) | 51 (4.6) | 87 (4.2) | 69 (5.1) | 33 (4.1) | 18 (4.6) | 0.787 |
| Hypertension | 1094 (19.0) | 184 (16.4) | 380 (18.4) | 290 (21.1) | 161 (19.8) | 79 (20.3) | 0.038 |
| Dyslipidemia | 407 (7.2) | 83 (7.5) | 149 (7.3) | 92 (6.8) | 48 (6.0) | 35 (9.1) | 0.355 |
| Chronic kidney disease | 333 (5.8) | 40 (3.6) | 99 (4.8) | 97 (7.0) | 58 (7.1) | 39 (9.9) | < 0.001 |
| History of medication use (yes)b, n (%) | |||||||
| Diabetes medications | 181 (3.1) | 30 (2.6) | 64 (3.1) | 45 (3.2) | 25 (3.0) | 17 (4.3) | 0.587 |
| Hypertension medications | 812 (13.9) | 135 (11.9) | 301 (14.4) | 208 (15.0) | 110 (13.4) | 58 (14.7) | 0.198 |
| Lipid-lowering therapy | 213 (3.6) | 38 (3.6) | 79 (4.0) | 49 (3.7) | 29 (3.7) | 18 (4.9) | 0.836 |
| BMIb, kg/m2, mean (SD) | 23.6 (4.2) | 23.9 (3.9) | 23.8 (4.3) | 23.4 (4.2) | 23.3 (4.0) | 22.9 (4.1) | < 0.001 |
| Blood pressureb, mm Hg, mean (SD) | |||||||
| Systolic pressure | 128.1 (21.4) | 125.4 (18.6) | 128.2 (21.3) | 129.1 (21.2) | 128.3 (21.3) | 130.5 (25.7) | 0.002 |
| Diastolic pressure | 75.4 (11.9) | 75.2 (11.6) | 75.5 (11.7) | 75.4 (12.1) | 74.8 (12.1) | 76.0 (12.2) | 0.560 |
| Depressive symptoms scorec, mean (SD) | 7.8 (6.1) | 6.5 (5.6) | 7.1 (5.7) | 8.2 (6.1) | 9.4 (6.7) | 10.61 (6.39) | < 0.001 |
| Adulthood social support, mean (SD) | 0.4 (0.7) | 0.4 (0.7) | 0.3 (0.7) | 0.4 (0.7) | 0.4 (0.7) | 0.4 (0.7) | 0.021 |
| Metabolic biomarkersd | |||||||
| Fasting plasma glucose, mg/dL mean (SD) | 109.1 (34.1) | 108.1 (32.2) | 109.5 (36.9) | 110.3 (33.3) | 107.5 (27.7) | 109.3 (39.2) | 0.474 |
| HbA1c (%), mean (SD) | 14.5 (2.3) | 14.2 (2.1) | 14.5 (2.3) | 14.5 (2.2) | 14.5 (2.5) | 14.7 (2.6) | 0.301 |
| Total Cholesterol, mg/dL, mean (SD), | 192.6 (37.3) | 191.4 (36.4) | 193.0 (37.6) | 193.1 (37.2) | 191.1 (36.7) | 195.9 (39.4) | 0.364 |
| Triglyceride, mg/dL, median (IQR) | 103.6 (77.9) | 100.9 (79.7) | 107.1 (82.3) | 103.5 (71.7) | 100.9 (82.3) | 100.0 (81.4) | 0.142 |
| High-density lipoprotein, mg/dL, mean (SD) | 51.3 (15.3) | 50.8 (15.0) | 50.4 (15.5) | 52.3 (15.6) | 52.0 (15.2) | 51.8 (14.5) | 0.017 |
| Low-density lipoprotein, mg/dL, mean (SD) | 115.8 (34.1) | 115.6 (32.9) | 116.4 (34.5) | 115.4 (33.8) | 114.7 (34.1) | 117.1 (36.9) | 0.802 |
| hs-CRP, mg/L, median (IQR) | 1.0 (1.4) | 0.9 (1.5) | 1.0 (1.4) | 1.0 (1.4) | 1.0 (1.6) | 1.0 (1.4) | 0.195 |
| eGFR, mL/min/1.73 m2, mean (SD) | 94.4 (14.0) | 97.3 (14.5) | 93.8 (13.6) | 93.6 (14.4) | 93.4 (13.3) | 94.5 (13.3) | < 0.001 |
Abbreviations: ACEs Adverse childhood experiences, SD Standard deviation, IQR Interquartile range (75th quartile minus 25th quartile), BMI Body mass index, hs-CRP High-sensitivity C-reactive protein, eGFR Estimated glomerular filtration rate
aP value was based on the chi-square test for categorical data and analysis of variance or the Kruskal–Wallis test for continuous data where appropriate
bMissing data: 1 for the area of residence, 4 for educational level, 194 for smoking, 42 for drinking, 89 for diabetes, 70 for hypertension, 144 for dyslipidemia, 45 for kidney,38 for lipid-lowering therapy, 100 for BMI, 98 for systolic pressure, 91 for diastolic pressure, 69 for depressive symptoms scores
cThe depressive symptoms score was measured by the 10-item Center for Epidemiology Scale for Depression, ranging from 0 to 30, with higher scores indicating a higher level of depressive symptoms severity
dMeasured in the subpopulation of 4113 participants
eUsing Fisher’s exact test in r × c contingency tables
Associations of ACEs and AAEs with incident CVD
A total of 789 participants experienced incident CVD (heart disease, 475 cases; stroke, 369 cases) during the follow-up period. The unadjusted incidence rates of incident CVD were higher among individuals exposed to ACEs or AAEs. After adjusting for covariates in model 4, an increased risk of incident CVD was associated with the overall number of ACEs (HR: 1.11, 95% CI: 1.08 to 1.14) and AAEs (HR: 1.19, 95% CI: 1.16 to 1.22), as shown in Table 2. A dose–response relationship between the number of ACEs or AAEs and incident CVD risk was observed, and the relationship remained significant in the fully adjusted model 4 (e.g., ACE [HR: 1.29, 95% CI:1.17 to 1.42 for one ACE indicator; HR: 1.39, 95% CI: 1.25 to 1.54 for two ACEs indicators; HR: 1.56, 95% CI: 1.40 to 1.75 for three indicators; HR: 1.58, 95% CI: 1.38 to 1.81 for at least four indicators]). For CVD components, even after adjusting for covariates in model 4, the overall number of ACEs and AAEs were associated with an increased risk of incident heart disease (ACE, HR: 1.06, 95% CI: 1.02 to 1.10; AAE, HR: 1.19, 95% CI: 1.15 to 1.24) and incident stroke (ACE, HR: 1.17, 95% CI: 1.13 to 1.20; AAE, HR: 1.17, 95% CI: 1.13 to 1.21). Similar dose–response relationships between the number of AAEs and the risks of incident heart disease or incident stroke were observed (Table 2).
Table 2.
Incidence of cardiovascular disease (CVD) and hazard ratios for associations of adverse childhood experiences (ACEs) and adverse adulthood experiences (AAEs) with incident CVD
| Case, No | Incidence rate, per 1000 person-years | HR (95% CI) | ||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |||
| Cardiovascular disease | ||||||
| ACEs indicatorsa (1-unit per increasing) | NA | NA | 1.12 (1.09–1.14) | 1.14 (1.11–1.17) | 1.12 (1.05–1.20) | 1.11 (1.08–1.14) |
| No. of ACEs indicators | ||||||
| 0 | 109 | 24.41 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 1 | 272 | 33.14 | 1.24 (1.13–1.35) | 1.27 (1.16–1.39) | 1.29 (1.17–1.42) | 1.29 (1.17–1.42) |
| 2 | 204 | 37.78 | 1.37 (1.25–1.51) | 1.45 (1.32–1.60) | 1.39 (1.25–1.54) | 1.39 (1.25–1.54) |
| 3 | 137 | 42.91 | 1.54 (1.39–1.71) | 1.64 (1.48–1.82) | 1.56 (1.39–1.74) | 1.56 (1.40–1.75) |
| ≥ 4 | 67 | 43.93 | 1.55 (1.37–1.76) | 1.70 (1.50–1.93) | 1.57 (1.37–1.80) | 1.58 (1.38–1.81) |
| AAEs indicatorsa (1-unit per increasing) | NA | NA | 1.21 (1.18–1.24) | 1.22 (1.19–1.25) | 1.18 (1.15–1.22) | 1.19 (1.16–1.22) |
| No. of AAEs indicators | ||||||
| 0 | 427 | 29.31 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 1 | 163 | 36.57 | 1.11 (1.03–1.19) | 1.16 (1.07–1.25) | 1.10 (1.01–1.19) | 1.10 (1.01–1.19) |
| 2 | 96 | 48.07 | 1.48 (1.35–1.62) | 1.52 (1.38–1.66) | 1.42 (1.29–1.56) | 1.42 (1.29–1.56) |
| 3 | 74 | 57.19 | 1.90 (1.71–2.10) | 1.94 (1.75–2.15) | 1.66 (1.49–1.85) | 1.67 (1.50–1.86) |
| ≥ 4 | 29 | 60.80 | 2.00 (1.71–2.33) | 2.07 (1.77–2.42) | 1.99 (1.70–2.34) | 2.00 (1.70–2.35) |
| Heart disease | ||||||
| ACEs indicatorsa (1-unit per increasing) | NA | NA | 1.08 (1.04–1.11) | 1.10 (1.06–1.14) | 1.06 (1.02–1.10) | 1.06 (1.02–1.10) |
| No. of ACEs indicators | ||||||
| 0 | 62 | 13.88 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 1 | 156 | 19.01 | 1.25 (1.10–1.43) | 1.30 (1.14–1.48) | 1.33 (1.15–1.54) | 1.33 (1.15–1.54) |
| 2 | 129 | 23.89 | 1.24 (1.08–1.43) | 1.31 (1.14–1.51) | 1.25 (1.07–1.46) | 1.25 (1.07–1.46) |
| 3 | 85 | 26.62 | 1.39 (1.20–1.62) | 1.49 (1.28–1.74) | 1.42 (1.20–1.68) | 1.42 (1.20–1.67) |
| ≥ 4 | 43 | 28.20 | 1.41 (1.17–1.70) | 1.55 (1.29–1.87) | 1.37 (1.12–1.68) | 1.37 (1.12–1.68) |
| AAEs indicatorsa (1-unit per increasing) | NA | NA | 1.23 (1.19–1.28) | 1.24 (1.20–1.29) | 1.19 (1.15–1.24) | 1.19 (1.15–1.24) |
| No. of AAEs indicators | ||||||
| 0 | 265 | 18.19 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 1 | 96 | 21.54 | 1.20 (1.08–1.34) | 1.25 (1.12–1.40) | 1.17 (1.04–1.32) | 1.17 (1.04–1.32) |
| 2 | 53 | 26.54 | 1.60 (1.40–1.82) | 1.63 (1.43–1.86) | 1.57 (1.36–1.80) | 1.57 (1.36–1.80) |
| 3 | 42 | 32.46 | 1.91 (1.65–2.22) | 1.96 (1.69–2.28) | 1.55 (1.32–1.83) | 1.55 (1.31–1.83) |
| ≥ 4 | 19 | 39.83 | 2.13 (1.71–2.66) | 2.19 (1.75–2.74) | 2.04 (1.61–2.59) | 2.04 (1.61–2.58) |
| Stroke | ||||||
| ACEs indicatorsa (1-unit per increasing) | NA | NA | 1.16 (1.13–1.19) | 1.18 (1.15–1.22) | 1.16 (1.13–1.20) | 1.17 (1.13–1.20) |
| No. of ACEs indicators | ||||||
| 0 | 52 | 11.86 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 1 | 135 | 16.83 | 1.27 (1.13–1.44) | 1.31 (1.16–1.48) | 1.32 (1.16–1.50) | 1.32 (1.16–1.50) |
| 2 | 91 | 17.26 | 1.56 (1.38–1.77) | 1.66 (1.46–1.89) | 1.60 (1.40–1.83) | 1.60 (1.40–1.83) |
| 3 | 61 | 19.70 | 1.72 (1.50–1.97) | 1.84 (1.60–2.11) | 1.76 (1.52–2.04) | 1.76 (1.53–2.04) |
| ≥ 4 | 30 | 20.30 | 1.79 (1.53–2.10) | 1.98 (1.68–2.33) | 1.86 (1.57–2.21) | 1.87 (1.58–2.22) |
| AAEs indicatorsa (1-unit per increasing) | NA | NA | 1.19 (1.15–1.23) | 1.20 (1.16–1.24) | 1.17 (1.13–1.21) | 1.17 (1.13–1.21) |
| No. of AAEs indicators | ||||||
| 0 | 192 | 13.45 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 1 | 81 | 18.59 | 1.06 (0.97–1.17) | 1.12 (1.01–1.23) | 1.06 (0.95–1.17) | 1.06 (0.95–1.17) |
| 2 | 48 | 24.64 | 1.34 (1.18–1.51) | 1.37 (1.21–1.55) | 1.25 (1.10–1.42) | 1.25 (1.10–1.42) |
| 3 | 34 | 27.35 | 1.74 (1.53–1.99) | 1.79 (1.57–2.05) | 1.62 (1.41–1.87) | 1.63 (1.42–1.88) |
| ≥ 4 | 14 | 30.70 | 2.11 (1.74–2.55) | 2.22 (1.83–2.69) | 2.17 (1.78–2.64) | 2.17 (1.78–2.65) |
Model 1 was adjusted for age and sex
Model 2 was adjusted for age, sex, residence, educational level, marital status, physical activity, smoking status, and alcohol consumption
Model 3 was adjusted as Model 2 plus body mass index; history of diabetes, hypertension, dyslipidemia, and chronic kidney disease; use of diabetes medications, hypertension medications, and lipid-lowering therapy; and depressive symptoms score
Model 4 was adjusted as Model 3 plus young adulthood social support
Abbreviations: ACEs Adverse childhood experiences, AAEs Adverse adulthood experiences, No. Number, HR Hazard ratio, 95% CI, 95% confidence interval, NA Not available or not applicable
aContinuous variable
Mediation analysis of AAEs on associations between ACEs and incident CVD
After adjusting for AAEs and other covariates, each additional ACE indicator was associated with a 9% (95% CI: 3 to 16%) higher risk of incident CVD, and the hazard ratios were larger without adjusting for AAEs. The overall AAEs were found to mediate 17.7% (95% CI: 8.2 to 34.2%) of the association between ACEs and incident CVD (Table 3). In addition, after adjusting for covariates other than AAEs, the adjusted HRs for incident CVD in individuals exposed to at least one ACE indicator were 1.38 (95 CI: 1.10 to 1.68) compared to those not exposed. However, after adjusting for AAEs and other covariates, the above associations decreased slightly to 1.36 (1.10 to 1.68), with the mediation proportion attributed to AAEs being 4.6% (95% CI: 1.3 to 15.4%) of the relationship (Table 3). Furthermore, the additional inclusion of AAEs did not enhance the predictive power of ACEs for incident CVD, shown in Additional file 2: Tab. S3.
Table 3.
Associations of adverse childhood experiences (ACEs) with incident cardiovascular disease (CVD) and mediation proportion of the associations attributed to adverse adulthood experiences (AAEs)
| HR (95% CI)a | Mediation proportion (%) (95% CI) | ||
|---|---|---|---|
| Unadjusted for AAEs | Adjusted for AAEs | ||
| Cardiovascular disease | |||
| ACEs indicatorsb (1-unit per increasing) | 1.11 (1.08–1.14) | 1.09 (1.03–1.16) | 17.7 (8.2–34.2) |
| No. of ACEs indicators | |||
| 0 | 1.00 (reference) | 1.00 (reference) | - |
| ≥ 1 | 1.38 (1.12–1.70) | 1.36 (1.10–1.68) | 4.6 (1.3–15.4) |
| Heart disease | |||
| ACEs indicatorsb (1-unit per increasing) | 1.06 (1.02–1.10) | 1.04 (0.98–1.08) | 36.7 (4.0–89.0) |
| No. of ACEs indicators | |||
| 0 | 1.00 (reference) | 1.00 (reference) | - |
| ≥ 1 | 1.32 (1.16–1.51) | 1.30 (1.14–1.49) | 5.6 (1.0–26.1) |
| Stroke | |||
| ACEs indicatorsb (1-unit per increasing) | 1.17 (1.13–1.20) | 1.15 (1.11–1.18) | 10.9 (4.5–24.0) |
| No. of ACEs indicators | |||
| 0 | 1.00 (reference) | 1.00 (reference) | - |
| ≥ 1 | 1.51 (1.34–1.70) | 1.49 (1.32–1.68) | 3.3 (0.9–11.9) |
Abbreviations: ACEs Adverse childhood experiences, AAEs Adverse adulthood experiences, HR Hazard ratio, 95% CI, 95% confidence interval
aModels were adjusted for age, sex, residence, marital status, educational level, health behaviors (physical activity, smoking status, and alcohol consumption), health status variables (BMI; history of diabetes, hypertension, dyslipidemia, and chronic kidney disease; use of diabetes medications, hypertension medications, and lipid-lowering therapy; and depressive symptoms), and young adulthood social support
bContinuous variable
For CVD components, after adjusting for AAEs and other covariates, the associations of the number of ACE indicators with incident heart disease and incident stroke were slightly decreasing compared to the observed associations from the models without adjusting for AAEs. The mediation proportion attributed to AAEs was 36.7% (95% CI: 4.0 to 89.0%) for the associations between the overall ACEs and incident heart disease and 10.9% (95% CI: 4.5 to 24.0%) for the associations for incident stroke, respectively (Table 3). Moreover, the additional inclusion of AAEs did not enhance the predictive power of ACEs for incident heart disease or incident stroke, shown in Additional file 2: Tab. S3.
Interaction and joint analysis of ACEs and AAEs on incident CVD
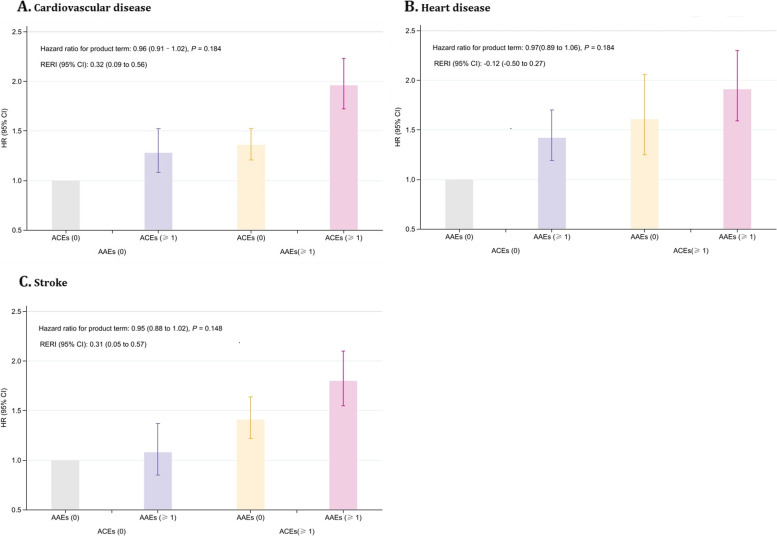
In the fully adjusted model, no significant multiplicative interaction was observed between ACEs and AAEs on incident CVD (P = 0.184, Fig. 2A), but a significant additive interaction was detected (RERI [95% CI]: 0.32 [0.09 to 0.56], Fig. 2A). The joint analysis of ACEs and AAEs on incident CVD revealed that compared to those not exposed to either, the adjusted HR for adults exposed to at least one ACE and one AAE indicator was highest at 1.96 (95% CI: 1.72 to 2.23) (Fig, 2A).
Fig. 2.
Interaction and joint analysis of adverse childhood experiences and adverse adulthood experiences with incident cardiovascular disease
For CVD components, in the fully adjusted model, no significant multiplicative interaction was observed between ACEs and AAEs on incident heart disease (P = 0.184, Fig. 2B) and incident stroke (P = 0.148, Fig. 2C), but a significant additive interaction was observed for incident stroke (RERI [95% CI]: 0.31 [0.05 to 0.57], Fig. 2C). The joint analysis for incident heart disease or incident stroke demonstrated that exposure to at least one ACE and one AAE indicator was associated with the highest magnitude of both incident heart disease (HR: 1.91, 95% CI: 1.59 to 2.30) and incident stroke (HR: 1.80, 95% CI: 1.55 to 2.10) (Fig. 2B and C).
Modifying roles of social support, biological sex, and age
As shown in Additional file 2: Tab. S4, young adulthood social support was a significant modifier in the associations of ACEs or AAEs with incident CVD (ACEs × social support: β [95% CI], − 0.05 [− 0.09 to − 0.02]; AAEs × social support: β [95% CI], − 0.04 [− 0.08 to − 0.01]) in the age- and sex-adjusted model (model 1). However, after adjusting for other covariates, these significant associations disappeared in models 2 and 3. The role of biological sex as a modifier in the associations of ACEs or AAEs with incident CVD was not significant, regardless of whether covariates were included or not. On the other hand, age was found to be a significant modifier in the associations of ACEs or AAEs with incident CVD in model 3 (ACEs × age: β [95% CI], − 0.01 [− 0.01 to − 0.01]; AAEs × age: β [95% CI], 0.003 [0.001 to 0.01]).
Regarding CVD components, the modifying role of social support during young adulthood was observed in the association between AAEs and incident heart disease (AAEs × social support: β [95% CI], − 0.08 [− 0.13 to − 0.02]). Additionally, the modifying roles of biological sex and age were observed in the association between ACEs and incident heart disease (ACEs × sex: β [95% CI], 0.09 [0.01 to 0.17]); ACEs × age: β [95% CI], − 0.01 [− 0.01 to − 0.01]). Furthermore, age was found to be a significant modifier in the associations of both ACEs and AAEs with incident stroke (ACEs × age: β [95% CI], − 0.01 [− 0.01 to − 0.01]; AAEs × age: β [95% CI], 0.01 [0.001 to 0.01]), even adjusting for covariates in model 3.
Subgroup analyses
The results stratified by sex and age group are presented in Additional file 2: Tab. S5–Tab. S6 and Additional file 3: Fig. S2–Fig. S3. After adjusting for covariates, the associations of ACEs or AAEs with incident CVD did not differ significantly between males and females, but the negative association between young adulthood social support and incident CVD was statistically significant only in females. The associations of ACEs with incident CVD were significant only in adults under 60 years old, while the associations of AAEs with incident CVD were stronger in older compared to younger adults, shown in Additional file 2: Tab. S5. The proportions that AAEs mediated in the association between ACEs and incident CVD were similar to the main findings in both males and females and younger adults. However, AAEs did not mediate the association between ACEs and incident CVD among older adults, shown in Additional file 2: Tab. S6. The results of the joint analyses of ACEs and AAEs with incident CVD were consistent with the primary findings, except for significant multiplicative and additive interactions between ACEs and AAEs on incident CVD observed among adults aged < 60 years, shown in Additional file 3: Fig. S3.
Sensitivity analyses
The associations of ACEs or AAEs with incident CVD did not significantly change after further adjusting for fasting plasma glucose, glycosylated hemoglobin, total cholesterol, triglyceride, high-density lipoprotein, low-density lipoprotein, hs-CRP, and eGFR, shown in Additional file 2: Tab. S7. Similar findings were obtained from complete data analyses, shown in Additional file 2: Tab. S8–Tab. S9, except for the absence of a significant additive interaction, shown in Additional file 3: Fig. S4. The fully adjusted models revealed that six types of ACEs indicators (including childhood physical neglect, childhood domestic violence, childhood parental death, childhood physical abuse, childhood household mental illness, and childhood exposure to natural disasters) and three types of AAEs indicators (including ever being confined to bed in adulthood, ever being hospitalized for a month or longer, and ever leaving a job due to health conditions) were significantly associated with incident CVD. Moreover, childhood domestic violence, childhood exposure to natural disasters, and childhood physical abuse were the 3 most prominent ACEs associated with incident CVD, shown in Additional file 2: Tab. S10. The mediation proportion by the overall AAEs for the associations between each ACE indicator and incident CVD showed similar patterns, shown in Additional file 2: Tab. S11.
Discussion
In this cohort study of middle-aged or older adults in China, exposure to ACEs or AAEs was independently associated with an increased risk of incident CVD, and the risk of incident CVD was found to increase with an increasing number of ACE or AAE indicators. Furthermore, the association between ACEs and incident CVD was partially explained by AAEs. An additive interaction was observed between ACEs and AAEs on incident CVD, with the highest risks seen in adults exposed to at least one ACE and one AAE indicator.
Despite consistent reports linking ACEs with CVD in various cultural contexts [5–7], there is limited research investigating the impacts of both ACEs and AAEs on incident CVD, while also considering a series of covariates, including social support. Moreover, previous studies have shown associations between ACEs and CVD risk factors such as smoking, alcohol consumption [8, 42], and depression [11, 12], but there has been a lack of focus on their confounding influences in the associations between ACEs and CVD events. After adjusting for several potential confounding variables, including CVD risk factors and social support, this study still found positive associations of ACEs and AAEs with incident CVD, with a dose–response relationship between the number of ACEs or AAEs and increased risks for both males and females. Similar positive relationships were observed between the number of ACEs or AAEs and the risks of incident heart disease and incident stroke, which are components of the investigated CVD events. These findings align with a previous retrospective cohort study using the UK biobank, which demonstrated a dose–response relationship between the number of childhood maltreatment types and incident CVD [11]. A cross-sectional study in German adults also supports these results, revealing a significant and independent association between adulthood stressful life events and cardiovascular health [16]. The present study expands on previous research by demonstrating the associations of both ACEs and AAEs with incident CVD and its subgroups (i.e., heart disease and stroke) while controlling for potential CVD risk factors and young adulthood social support. Although the potential use of interventions focused on ACE or AAE for cardiovascular health has not been tested in large randomized clinical trials, the potential reversibility of ACE or AAE consequences in adults has received attention [5]. Our findings may provide insight into the early identification of vulnerable groups and the prioritization of prevention and intervention efforts for individuals with ACE or AAE exposure to safeguard their cardiovascular health. Among the individual ACEs examined, childhood domestic violence exhibited the strongest association with incident CVD, followed by childhood exposure to natural disasters and childhood physical abuse. These specific ACEs appear to be crucial aspects that need to be considered in ACE prevention strategies.
The exact mechanism underlying the associations of ACEs or AAEs with incident CVD remains poorly understood. Dysregulation of the hypothalamic–pituitary–adrenal (HPA) axis, chronic inflammatory processes, increased cardiac electrical instability, myocardial ischemia, and functional changes in the central nervous system have been suggested as potential pathophysiological effects of adverse experiences in childhood or adulthood on the development and progression of CVD events [42, 43]. In addition to the mechanisms mentioned above, previous evidence also suggests that ACEs or AAEs may predispose individuals to poor mental health and an unhealthy lifestyle, including hypertension, high serum cholesterol levels, diabetes, smoking, and obesity, which in turn, predispose individuals to CVD [5, 11, 12]. Therefore, our findings regarding the associations of ACEs or AAEs with incident CVD are physiologically plausible. Nevertheless, further evidence is needed to elucidate the underlying mechanism fully.
Prior evidence suggests AAEs may play a crucial role as a disease trigger in the relationship between ACEs and adult health [15]. The present study builds upon these findings by demonstrating the mediating role of AAEs in the association between ACEs and incident CVD. Our results indicate that the association between ACEs and incident CVD was partly explained by AAEs, highlighting the importance of this pathway in the etiology of CVD. The stress generation model may explain the mediating role of AAEs [44]. Specifically, early life stress may increase the likelihood of encountering more significant stressors in adulthood, with subsequent exposure largely responsible for any variance linked to ACEs [14, 44]. Notably, ACEs, such as neglect and abuse, may inculcate cognitive biases toward the threat, thereby fostering a heightened sense of danger, even in ambiguous circumstances [45]. These negative perceptions may increase anxiety and stress levels over the lifespan. Stressful experiences in adulthood, such as job strain and discrimination, have been linked to poorer overall health and a higher prevalence of conditions such as hypertension and stroke [16]. Importantly, our findings also provide evidence of the significance of avoiding AAEs, which may help mitigate the association between ACEs and incident CVD.
Furthermore, this study observed a significant additive interaction effect between ACEs and AAEs on incident CVD. Notably, the risk associations of AAEs with incident CVD were stronger among those exposed to at least one ACE indicator, highlighting the critical importance of preventing adversity experiences for adults, particularly among those who are more vulnerable to AAEs due to prior exposure to ACEs. These results align with a longitudinal analysis in the Finnish Public Sector, which revealed that the combined effects of childhood psychosocial adversity and adult neighborhood disadvantage increased the risk of CVD [7]. However, a separate longitudinal study in the USA found that ACEs and recent life events were independently associated with a higher level of inflammation at midlife, with no evidence of synergistic effects. Notably, elevated inflammation levels have been shown to be related to CVD [15]. Therefore, given the mixed results, these findings offer valuable insights, but definitive conclusions about the interaction effects between ACEs and AAEs on CVD cannot be drawn. Further research is needed to fully elucidate the complex relations between ACEs and AAEs on the development of CVD.
Previous evidence suggests that early life social support may facilitate the development of effective coping and emotion regulation strategies to mitigate the impact of childhood and adulthood stress, as well as reduce CVD risk factors associated with ACEs or AAEs [19]. However, our study only revealed mild buffering effects of social support during young adulthood on the negative consequences of ACEs or AAEs for CVD. Further research is needed to investigate the role of social support across different age groups, including the influence of additional forms of support such as family and friend support. It is also important to explore additional significant factors that can modify the association between ACEs or AAEs and CVD. Our findings also demonstrated that age could significantly modify the relationship between ACEs or AAEs and incident CVD. Regarding CVD components, biological sex, and age may act as modifiers in the association between ACEs and incident heart disease, while age may play a modifying role in the associations between AAEs and incident stroke. Further subgroup analysis revealed that the associations of ACEs or AAEs with incident CVD did not significantly differ between males and females. However, the associations of ACEs with incident CVD were significant only in adults under 60 years old, whereas the associations of AAEs with incident CVD were stronger in older adults compared to younger ones. Among older adults (> 60 years old), the mediating role of AAEs disappeared in the association between ACEs and incident CVD, suggesting the existence of alternative pathways linking ACEs to later health outcomes [15] and the impact of ACEs on stress reactivity may diminish with age. However, this finding could also be attributed to the fact that individuals with cardiovascular events resulting from ACEs or AAEs may have already passed away by the age of 60. Nevertheless, these findings emphasize the need for further investigation into the modifying roles of biological sex and age.
The strengths of our study include the cohort design and large sample size, which provided ample statistical power to explore the associations of ACEs and AAEs with incident CVD, while enabling mediation and subgroup analyses. Furthermore, this study comprehensively estimated the impacts of both ACEs and AAEs on subsequent CVD events, with consideration of a series of covariates including young adulthood social support. However, several limitations are worth noting. First, the information on ACEs and AAEs relied on retrospective self-reports, which may have been vulnerable to reporting and recall bias. Nevertheless, previous research has demonstrated good test–retest reliability of retrospective measurements of ACEs [25]. Second, the main analysis only summed up the cumulative numbers of ACEs or AAEs, which assumes that different types of ACEs or AAEs have equivalent effects on CVD, possibly disregarding unique information. Nonetheless, this study conducted sensitivity analyses utilizing each ACE or AAE indicator, yielding similar mediation proportion patterns. Third, the study used self-reported doctors’ diagnoses, which may have underestimated the occurrence of CVD events. Moreover, the specific data on categories of heart disease, such as heart attack and coronary heart disease, were not available for our analyses. Fourth, residual confounding remains possible despite controlling for multidimensional covariates, including demographic characteristics, health behavior factors, health status factors, young adulthood social support, and metabolic biomarkers, and causal relationships cannot be confirmed. Fifth, the study findings need to be validated by other cohort studies and randomized control trials. Sixth, although previous studies using the CHARLS dataset reported slightly lower values about the number of CVD cases/total sample size than the present study [3, 18], the low number of CVD cases/total sample size may be a concern. Seventh, it is important to note that the CHARLS dataset only provides data on young adulthood social support. However, social support across other age groups and other forms of support, such as family support and friend support, may also play a role in the associations between ACEs and AAEs with incident CVD. Eighth, in this study, the difference method was used instead of structural equation modeling to estimate the proportion of mediation by the overall AAEs in the association between ACEs and incident CVD. However, conducting specific mediation/path analysis using structural equation modeling could examine direct and indirect estimates. Moreover, the confidence intervals for the mediations have wide ranges, and further research is necessary to validate the study results regarding the mediation of AAEs on the associations between ACEs and incident CVD.
Conclusions
In summary, exposure to ACEs or AAEs could be associated with an increased risk of CVD among middle-aged and older adults in a dose–response manner. We also observed a modest mediation of AAEs on the association between ACEs and incident CVD. Notably, we found a significant additive interaction effect between ACEs and AAEs on the risk of incident CVD, with individuals exposed to both stressors exhibiting the highest risk. Accordingly, the findings suggest that preventing ACEs alone might not substantially reduce the risk of incident CVD later in life, and other strategies for tackling AAEs may also be needed. Therefore, a comprehensive life-course health strategy targeting the prevention of both childhood and adulthood stressors may have potential value in mitigating the risks of incident CVD. However, future randomized clinical trials are needed to confirm these conclusions.
Supplementary Information
Additional file 1: Appendix. S1. Study population and definition of covariates in detail.
Additional file 2: Table S1. Question items and responses for variables included in the adverse childhood and adulthood experiences; Table S2. Baseline characteristics of the study population by the number of adverse adulthood experiences (AAEs); Table S3. C-statistics of models without and with adverse adulthood experiences (AAEs); Table S4. Young adulthood social support, sex, and age as effect modifiers for the associations of adverse childhood experiences (ACEs) and adverse adulthood experiences (AAEs) with incident cardiovascular disease (CVD); Table S5. Hazard ratios for associations of adverse childhood experiences (ACEs), adverse adulthood experience (AAEs), and young adulthood social support with incident cardiovascular disease (CVD): subgroup analyses; Table S6. Associations of adverse childhood experiences (ACEs) with incident cardiovascular disease (CVD) and mediation proportion of the associations attributed to adverse adulthood experience (AAEs): subgroup analyses; Table S7. Associations of adverse childhood experience (ACEs) and adverse adulthood experiences (AAEs) with incident cardiovascular disease (CVD) in the subpopulation of 4113 participants with metabolic biomarkers measurements; Table S8. Hazard ratios for associations of adverse childhood experiences (ACEs), adverse adulthood experiences (AAEs), and young adulthood social support with incident cardiovascular disease (CVD) using the complete dataset; Table S9. Associations of adverse childhood experiences (ACEs) with incident cardiovascular disease (CVD) and mediation proportion of the associations attributed to adverse adulthood experiences (AAEs): using the complete dataset; Table S10. Hazard ratios for associations of each indicator of adverse childhood experiences (ACEs) and adverse adulthood experiences (AAEs) with incident cardiovascular disease (CVD); Table S11. Associations of each indicator of adverse childhood experiences (ACEs) with incident cardiovascular disease (CVD) and mediation proportion of the associations attributed to adverse adulthood experiences (AAEs).
Additional file 3: Figure S1. Overlapping exposure to adverse childhood experiences (ACEs) and adverse adulthood experiences (AAEs); Figure 2. Interaction and joint analysis of adverse childhood experiences (ACEs) and adverse adulthood experience (AAEs) with incident cardiovascular disease (CVD): subgroup analysis by sex; Figure S3. Interaction and joint analysis of adverse childhood experiences (ACEs) and adverse adulthood experience (AAEs) with incident cardiovascular disease (CVD): subgroup analyses: subgroup analysis by age; Figure S4. Interaction and joint analysis of adverse childhood experiences (ACEs) and adverse adulthood experience (AAEs) with incident CVD: using the complete dataset.
Acknowledgements
We appreciate all adults participating in the China Health and Retirement Longitudinal Study. We thank the CHARLS team for sharing the datasets.
Abbreviations
- AAEs
Adverse adulthood experiences
- ACEs
Adverse childhood experiences
- AHA
American Heart Association
- BMI
Body mass index
- CHARLS
China Health and Retirement Longitudinal Study
- CVD
Cardiovascular disease
- eGFR
Estimated glomerular filtration rate
- HbA1c
Glycosylated hemoglobin
- Hs-CRP
High-sensitivity C-reactive protein
Authors’ contributions
LG contributed to the conception and design of the work. WXW, YFL, YWY, and LG performed the analysis. WXW, YFL, YWY, WQJ, YYN, XH, CYL, and LG contributed to the interpretation of data. LG, WXW, and YFL accessed and verified the underlying data reported. WXW and YFL wrote the initial draft of the manuscript. WXW, YFL, YWY, WQJ, YYN, XH, CYL, and LG critically revised the manuscript. WXW, YFL, YWY, WQJ, YYN, XH, CYL, and LG had full access to all the data in the study and had final responsibility for the decision to submit for publication. All authors read and approved the final manuscript.
Funding
This research was supported by a grant from the Natural Science Foundation of Guangdong Province (Dr. Guo, 2022A1515012333; Dr. Wang, 2021A1515111184) and the Science and Technology Planning Project of Guangzhou (Dr. Guo, 202102020136).
Availability of data and materials
The data that support the findings of the study are available through the website of CHARLS: http://charls.pku.edu.cn/index/en.html. To access and use the day for research purpose, approval should be obtained from the CHARLS team at Peking University.
Declarations
Ethics approval and consent to participate
All methods were performed in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants. The CHARLS study was approved by the Biomedical Ethics Review Committee of Peking University (IRB00001052-11015), and ethics approval for the use of CHARLS data was obtained from the University of Newcastle Human Research Ethics Committee. This study was conducted following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Wanxin Wang and Yifeng Liu contributed equally to this work.
References
- 1.Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the Gbd 2019 Study. J Am Coll Cardiol. 2020;76(25):2982–3021. doi: 10.1016/j.jacc.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization (WHO) Cardiovascular Diseases (Cvds) 2021. [Google Scholar]
- 3.Wooldridge JS, Tynan M, Rossi FS, Gasperi M, McLean CL, Bosch J, Trivedi RB, Herbert MS, Afari N. Patterns of Adverse Childhood Experiences and Cardiovascular Risk Factors in U.S. Adults. Stress Health. 2022. 10.1002/smi.3167. [DOI] [PMC free article] [PubMed]
- 4.Aguayo L, Chirinos DA, Heard-Garris N, Wong M, Davis MM, Merkin SS, Seeman T, Kershaw KN. Association of Exposure to Abuse, Nurture, and Household Organization in Childhood with 4 Cardiovascular Disease Risks Factors Among Participants in the Cardia Study. J Am Heart Assoc. 2022;11(9):e23244. doi: 10.1161/JAHA.121.023244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Godoy LC, Frankfurter C, Cooper M, Lay C, Maunder R, Farkouh ME. Association of Adverse Childhood Experiences with Cardiovascular Disease Later in Life: A Review. JAMA Cardiol. 2021;6(2):228–235. doi: 10.1001/jamacardio.2020.6050. [DOI] [PubMed] [Google Scholar]
- 6.Pierce JB, Kershaw KN, Kiefe CI, Jacobs DJ, Sidney S, Merkin SS, Feinglass J. Association of Childhood Psychosocial Environment with 30-Year Cardiovascular Disease Incidence and Mortality in Middle Age. J Am Heart Assoc. 2020;9(9):e15326. doi: 10.1161/JAHA.119.015326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Halonen JI, Stenholm S, Pentti J, Kawachi I, Subramanian SV, Kivimaki M, Vahtera J. Childhood Psychosocial Adversity and Adult Neighborhood Disadvantage as Predictors of Cardiovascular Disease: A Cohort Study. Circulation. 2015;132(5):371–379. doi: 10.1161/CIRCULATIONAHA.115.015392. [DOI] [PubMed] [Google Scholar]
- 8.Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, Jones L, Dunne MP. The Effect of Multiple Adverse Childhood Experiences On Health: A Systematic Review and Meta-Analysis. Lancet Public Health. 2017;2(8):e356–e366. doi: 10.1016/S2468-2667(17)30118-4. [DOI] [PubMed] [Google Scholar]
- 9.American Heart Association. The relationship between adverse childhood experiences (Aces) and health: factors that influence individuals with or at risk of Cvd. In. 2019. https://www.heart.org/-/media/Files/About-Us/Policy-Research/Policy-Positions/Social-Determinants-of-Health/ACEs-Policy-Statement.pdf.
- 10.Suglia SF, Koenen KC, Boynton-Jarrett R, Chan PS, Clark CJ, Danese A, Faith MS, Goldstein BI, Hayman LL, Isasi CR, et al. Childhood and Adolescent Adversity and Cardiometabolic Outcomes: A Scientific Statement From the American Heart Association. Circulation. 2018;137(5):e15–e28. doi: 10.1161/CIR.0000000000000536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ho FK, Celis-Morales C, Gray SR, Petermann-Rocha F, Lyall D, Mackay D, Sattar N, Minnis H, Pell JP. Child Maltreatment and Cardiovascular Disease: Quantifying Mediation Pathways Using Uk Biobank. BMC Med. 2020;18(1). 10.1186/s12916-020-01603-z. [DOI] [PMC free article] [PubMed]
- 12.Deschenes SS, Kivimaki M, Schmitz N. Adverse Childhood Experiences and the Risk of Coronary Heart Disease in Adulthood: Examining Potential Psychological, Biological, and Behavioral Mediators in the Whitehall Ii Cohort Study. J Am Heart Assoc. 2021;10(10):e19013. doi: 10.1161/JAHA.120.019013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Korkeila J, Vahtera J, Nabi H, Kivimaki M, Korkeila K, Sumanen M, Koskenvuo K, Koskenvuo M. Childhood Adversities, Adulthood Life Events and Depression. J Affect Disorders. 2010;127(1–3):130–138. doi: 10.1016/j.jad.2010.04.031. [DOI] [PubMed] [Google Scholar]
- 14.Crielaard L, Nicolaou M, Sawyer A, Quax R, Stronks K. Understanding the Impact of Exposure to Adverse Socioeconomic Conditions On Chronic Stress From a Complexity Science Perspective. BMC Med. 2021;19(1):242. doi: 10.1186/s12916-021-02106-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hostinar CE, Lachman ME, Mroczek DK, Seeman TE, Miller GE. Additive Contributions of Childhood Adversity and Recent Stressors to Inflammation at Midlife: Findings From the Midus Study. Dev Psychol. 2015;51(11):1630–1644. doi: 10.1037/dev0000049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clemens V, Burgin D, Huber-Lang M, Plener PL, Brahler E, Fegert JM. The Interplay Between Child Maltreatment and Stressful Life Events During Adulthood and Cardiovascular Problems-a Representative Study. J Clin Med. 2021;10(17). 10.3390/jcm10173937. [DOI] [PMC free article] [PubMed]
- 17.Cohen S, Wills TA. Stress, Social Support, and the Buffering Hypothesis. Psychol Bull. 1985;98(2):310–357. doi: 10.1037/0033-2909.98.2.310. [DOI] [PubMed] [Google Scholar]
- 18.Traub F, Boynton-Jarrett R. Modifiable Resilience Factors to Childhood Adversity for Clinical Pediatric Practice. Pediatrics. 2017;139(5). 10.1542/peds.2016-2569. [DOI] [PubMed]
- 19.Appleton AA, Buka SL, Loucks EB, Rimm EB, Martin LT, Kubzansky LD. A Prospective Study of Positive Early-Life Psychosocial Factors and Favorable Cardiovascular Risk in Adulthood. Circulation. 2013;127(8):905–912. doi: 10.1161/CIRCULATIONAHA.112.115782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort Profile: The China Health and Retirement Longitudinal Study (Charls) Int J Epidemiol. 2014;43(1):61–68. doi: 10.1093/ije/dys203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cao X, Ma C, Zheng Z, He L, Hao M, Chen X, Crimmins EM, Gill TM, Levine ME, Liu Z. Contribution of Life Course Circumstances to the Acceleration of Phenotypic and Functional Aging: A Retrospective Study. Eclinicalmedicine. 2022;51:101548. doi: 10.1016/j.eclinm.2022.101548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Björkenstam E, Kosidou K, Björkenstam C. Childhood Household Dysfunction and Risk of Self-Harm: A Cohort Study of 107 518 Young Adults in Stockholm County. Int J Epidemiol. 2016;45(2):501–511. doi: 10.1093/ije/dyw012. [DOI] [PubMed] [Google Scholar]
- 23.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults. The Adverse Childhood Experiences (Ace) Study. Am J Prev Med. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 24.Cao X, Ma C, Zheng Z, He L, Hao M, Chen X, Crimmins EM, Gill TM, Levine ME, Liu Z. Contribution of Life Course Circumstances to the Acceleration of Phenotypic and Functional Aging: A Retrospective Study. Eclinicalmedicine. 2022;51:101548. doi: 10.1016/j.eclinm.2022.101548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dube SR, Williamson DF, Thompson T, Felitti VJ, Anda RF. Assessing the Reliability of Retrospective Reports of Adverse Childhood Experiences Among Adult Hmo Members Attending a Primary Care Clinic. Child Abuse Neglect. 2004;28(7):729–737. doi: 10.1016/j.chiabu.2003.08.009. [DOI] [PubMed] [Google Scholar]
- 26.Lin L, Cao B, Chen W, Li J, Zhang Y, Guo VY. Association of Adverse Childhood Experiences and Social Isolation with Later-Life Cognitive Function Among Adults in China. JAMA Netw Open. 2022;5(11):e2241714. doi: 10.1001/jamanetworkopen.2022.41714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lin L, Wang HH, Lu C, Chen W, Guo VY. Adverse Childhood Experiences and Subsequent Chronic Diseases Among Middle-Aged Or Older Adults in China and Associations with Demographic and Socioeconomic Characteristics. JAMA Netw Open. 2021;4(10):e2130143. doi: 10.1001/jamanetworkopen.2021.30143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anda RF, Butchart A, Felitti VJ, Brown DW. Building a Framework for Global Surveillance of the Public Health Implications of Adverse Childhood Experiences. Am J Prev Med. 2010;39(1):93–98. doi: 10.1016/j.amepre.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 29.Li H, Zheng D, Li Z, Wu Z, Feng W, Cao X, Wang J, Gao Q, Li X, Wang W, et al. Association of Depressive Symptoms with Incident Cardiovascular Diseases in Middle-Aged and Older Chinese Adults. JAMA NETW OPEN. 2019;2(12):e1916591. doi: 10.1001/jamanetworkopen.2019.16591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gao K, Cao LF, Ma WZ, Gao YJ, Luo MS, Zhu J, Li T, Zhou D. Association Between Sarcopenia and Cardiovascular Disease Among Middle-Aged and Older Adults: Findings From the China Health and Retirement Longitudinal Study. Eclinicalmedicine. 2022;44:101264. doi: 10.1016/j.eclinm.2021.101264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Soh Y, Tiemeier H, Kawachi I, Berkman LF, Kubzansky LD. Eight-Year Depressive Symptom Trajectories and Incident Stroke: A 10-Year Follow-Up of the Hrs (Health and Retirement Study) Stroke. 2022;53(8):2569–2576. doi: 10.1161/STROKEAHA.121.037768. [DOI] [PubMed] [Google Scholar]
- 32.Boey KW. Cross-Validation of a Short Form of the Ces-D in Chinese Elderly. Int J Geriatr Psych. 1999;14(8):608–617. doi: 10.1002/(sici)1099-1166(199908)14:8<608::aid-gps991>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 33.Chen H, Mui AC. Factorial Validity of the Center for Epidemiologic Studies Depression Scale Short Form in Older Population in China. Int Psychogeriatr. 2014;26(1):49–57. doi: 10.1017/S1041610213001701. [DOI] [PubMed] [Google Scholar]
- 34.Shen Y, Yeatts DE. Social Support and Life Satisfaction Among Older Adults in China: Family-Based Support Versus Community-Based Support. Int J Aging Human Dev. 2013;77(3):189–209. doi: 10.2190/AG.77.3.b. [DOI] [PubMed] [Google Scholar]
- 35.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AR, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, et al. A New Equation to Estimate Glomerular Filtration Rate. Ann Intern Med. 2009;150(9):604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lu K. Number of Imputations Needed to Stabilize Estimated Treatment Difference in Longitudinal Data Analysis. Stat Methods Med Res. 2017;26(2):674–690. doi: 10.1177/0962280214554439. [DOI] [PubMed] [Google Scholar]
- 37.Zhang Y, Chen C, Pan X, Guo J, Li Y, Franco OH, Liu G, Pan A. Associations of Healthy Lifestyle and Socioeconomic Status with Mortality and Incident Cardiovascular Disease: Two Prospective Cohort Studies. BMJ-Brit Med J. 2021:n604. 10.1136/bmj.n604. [DOI] [PMC free article] [PubMed]
- 38.Nevo D, Liao X, Spiegelman D. Estimation and Inference for the Mediation Proportion. Int J Biostat. 2017;13(2). 10.1515/ijb-2017-0006. [DOI] [PMC free article] [PubMed]
- 39.Yan RH, Li W, Gu HQ, Wang Y. Calculation of C Statistics for the Cox Proportional Hazards Regression Models and its Implementation in Sas. Chin J Dis Control Prevent. 2016;20(9):953–956. doi: 10.16462/j.cnki.zhjbkz.2016.09.023. [DOI] [Google Scholar]
- 40.Hosmer DW, Lemeshow S. Confidence Interval Estimation of Interaction. Epidemiology. 1992;3(5):452–456. doi: 10.1097/00001648-199209000-00012. [DOI] [PubMed] [Google Scholar]
- 41.World Health Organization (WHO) Geneva. 2020. Decade of Healthy Ageing Baseline Report. [Google Scholar]
- 42.Su S, Jimenez MP, Roberts CTF, Loucks EB. The Role of Adverse Childhood Experiences in Cardiovascular Disease Risk: A Review with Emphasis On Plausible Mechanisms. Curr Cardiol Rep. 2015;17(10):88. doi: 10.1007/s11886-015-0645-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kivimäki M, Steptoe A. Effects of Stress On the Development and Progression of Cardiovascular Disease. Nat Rev Cardiol. 2018;15(4):215–229. doi: 10.1038/nrcardio.2017.189. [DOI] [PubMed] [Google Scholar]
- 44.Hammen C. Generation of Stress in the Course of Unipolar Depression. Am Psychol Assoc. 1991;100:555–561. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- 45.Banihashemi L, Peng CW, Rangarajan A, Karim HT, Wallace ML, Sibbach BM, Singh J, Stinley MM, Germain A, Aizenstein HJ. Childhood threat is associated with lower resting-state connectivity within a central visceral network. Front Psychol. 2022;13:805049. 10.3389/fpsyg.2022.805049. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Appendix. S1. Study population and definition of covariates in detail.
Additional file 2: Table S1. Question items and responses for variables included in the adverse childhood and adulthood experiences; Table S2. Baseline characteristics of the study population by the number of adverse adulthood experiences (AAEs); Table S3. C-statistics of models without and with adverse adulthood experiences (AAEs); Table S4. Young adulthood social support, sex, and age as effect modifiers for the associations of adverse childhood experiences (ACEs) and adverse adulthood experiences (AAEs) with incident cardiovascular disease (CVD); Table S5. Hazard ratios for associations of adverse childhood experiences (ACEs), adverse adulthood experience (AAEs), and young adulthood social support with incident cardiovascular disease (CVD): subgroup analyses; Table S6. Associations of adverse childhood experiences (ACEs) with incident cardiovascular disease (CVD) and mediation proportion of the associations attributed to adverse adulthood experience (AAEs): subgroup analyses; Table S7. Associations of adverse childhood experience (ACEs) and adverse adulthood experiences (AAEs) with incident cardiovascular disease (CVD) in the subpopulation of 4113 participants with metabolic biomarkers measurements; Table S8. Hazard ratios for associations of adverse childhood experiences (ACEs), adverse adulthood experiences (AAEs), and young adulthood social support with incident cardiovascular disease (CVD) using the complete dataset; Table S9. Associations of adverse childhood experiences (ACEs) with incident cardiovascular disease (CVD) and mediation proportion of the associations attributed to adverse adulthood experiences (AAEs): using the complete dataset; Table S10. Hazard ratios for associations of each indicator of adverse childhood experiences (ACEs) and adverse adulthood experiences (AAEs) with incident cardiovascular disease (CVD); Table S11. Associations of each indicator of adverse childhood experiences (ACEs) with incident cardiovascular disease (CVD) and mediation proportion of the associations attributed to adverse adulthood experiences (AAEs).
Additional file 3: Figure S1. Overlapping exposure to adverse childhood experiences (ACEs) and adverse adulthood experiences (AAEs); Figure 2. Interaction and joint analysis of adverse childhood experiences (ACEs) and adverse adulthood experience (AAEs) with incident cardiovascular disease (CVD): subgroup analysis by sex; Figure S3. Interaction and joint analysis of adverse childhood experiences (ACEs) and adverse adulthood experience (AAEs) with incident cardiovascular disease (CVD): subgroup analyses: subgroup analysis by age; Figure S4. Interaction and joint analysis of adverse childhood experiences (ACEs) and adverse adulthood experience (AAEs) with incident CVD: using the complete dataset.
Data Availability Statement
The data that support the findings of the study are available through the website of CHARLS: http://charls.pku.edu.cn/index/en.html. To access and use the day for research purpose, approval should be obtained from the CHARLS team at Peking University.