Abstract
Background
Critically ill patients have life-threatening conditions requiring immediate vital organ function intervention. But, critical illness in the emergency department (ED) has not been comprehensively described in resource-limited settings. Understanding the characteristics and dynamics of critical illness can help hospitals prepare for and ensure the continuum of care for critically ill patients. This study aimed to describe the pattern and outcomes of critically ill patients at the ED of the National Hospital in Tanzania from 2019 to 2021.
Methodology
This hospital-records-based retrospective cohort study analyzed records of all patients who attended the ED of Muhimbili National Hospital between January 2019 and December 2021. Data extracted from the ED electronic database included clinical and demographic information, diagnoses, and outcome status at the ED. Critical illness in this study was defined as either a severe derangement of one or more vital signs measured at triage or the provision of critical care intervention. Data were analyzed using Stata 17 to examine critical illnesses’ burden, characteristics, first-listed diagnosis, and outcomes at the ED.
Results
Among the 158,445 patients who visited the ED in the study period, 16,893 (10.7%) were critically ill. The burden of critical illness was 6,346 (10.3%) in 2019, 5,148 (10.9%) in 2020, and 5,400 (11.0%) in 2021. Respiratory (18.8%), cardiovascular (12.6%), infectious diseases (10.2%), and trauma (10.2%) were the leading causes of critical illness. Most (81.6%) of the critically ill patients presenting at the ED were admitted or transferred, of which 11% were admitted to the ICUs and 89% to general wards. Of the critically ill, 4.8% died at the ED.
Conclusion
More than one in ten patients attending the Tanzanian National Hospital emergency department was critically ill. The number of critically ill patients did not increase during the pandemic. The majority were admitted to general hospital wards, and about one in twenty died at the ED. This study highlights the burden of critical illness faced by hospitals and the need to ensure the availability and quality of emergency and critical care throughout hospitals.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12873-023-00858-y.
Keywords: Critical illness, Emergency department, Tanzania
Introduction
Critically ill patients have potentially reversible life-threatening conditions requiring immediate vital organ function treatment [1, 2]. Despite the potential of underestimation due to the assumption that critically ill patients are found only in the ICU, critical illness is thought to affect up to 45 million people worldwide in 2010 [3, 4]. This burden is unevenly distributed worldwide, with lower-income countries bearing the biggest brunt [3, 5]. The burden is expected to increase due to the epidemiological transition of diseases coupled with emerging and re-emerging infectious diseases [6, 7].
Critically ill patients usually present to hospitals through emergency departments (ED). At the EDs, patients are triaged according to their severity, resuscitated, and stabilized to prevent death or other complications; and transferred to the respective specialty of care [8]. With the growing field of Emergency medicine globally, low-and-middle-income countries are seeing the development of EDs in different levels of health facilities [1, 7, 9, 10].
Tanzania is no exception. Tanzania’s is a lower-middle income country and its first full-capacity public ED was established in 2010 at Muhimbili National Hospital [11]. The country is continuing to scale-up EDs that are managing an increasing number of patients presenting with diverse conditions, both critically and non-critically ill. However, the burden and characteristics of patients with critical illnesses in Tanzanian EDs have not been systematically documented. The available evidence is from studies conducted over a short period and excluded specific populations, such as children and trauma patients, who also constitute a significant proportion of ED visits [12]. Furthermore, the emergence of the COVID-19 pandemic has resulted in critical illness in about a third of its hospitalized victims, and it has radically changed health-seeking behaviors worldwide [13–15]. Recognizing the vital role of EDs as entry points to the hospitals for all patients, including children and trauma patients, and the need for a comprehensive and updated description of critical illness at the ED in resource-limited settings, especially in the era of COVID-19, this study aimed to describe the burden, trends, characteristics, causes, and outcomes of critically-ill patients at the ED of the National Hospital in Tanzania from 2019 to 2021.
Methods
Study design
This was a hospital-records-based cohort study of critically ill patients who attended the ED of a Tanzanian National Hospital for three years, from January 2019 to December 2021.
Setting
The study was conducted at the Muhimbili National Hospital (MNH) ED in Dar es Salaam, Tanzania. MNH has two campuses; for this study, only data for the Upanga campus has been analyzed. The ED receives acute patients from all hospitals in the country and directly from the community and admits them at MNH or transfers them to the specialized national hospitals of Jakaya Kikwete Cardiac Institute (JKCI) or the Muhimbili Orthopedic Institute (MOI) after being triaged, stabilized and initiated management accordingly. Obstetric emergencies are handled in the obstetric unit. Trauma cases seen at the ED are transferred to MOI or MNH for further management, depending on the nature of their injury. The three hospitals, MNH, JKCI, and MOI, are located within the same campus and have a total bed capacity of 1,982 beds.
At the ED, patients are received, registered, and triaged based on their vital signs and illness severity and then managed accordingly. The goal is for stable patients to leave the ED within two hours and up-to seven hours for severely sick patients. In addition, resuscitation rooms and a mini-ICU at the ED receive severely sick patients that require emergency or critical care. Further description of the ED and the Tanzania’s health system have been described elsewhere [11, 16].
Dar es Salaam is the most populous city in Tanzania. During the COVID-19 pandemic, over 40,000 confirmed cases have been reported in Tanzania, with Dar es Salaam having the highest number of cases [17, 18].
Data source
Data were extracted from the ED electronic information system. Clinicians and triage nurses at the ED enter information about the patients into the electronic system as they are providing care. The extracted data included the time the patient arrived at and was discharged from the ED, demographic information, the presenting complaint, diagnoses at the ED (the first listed diagnosis was used as the main diagnosis), interventions provided, laboratory results, ED outcome status, and the corresponding admission ward at MNH or transfer facility.
Study population and eligibility criteria
All patients who presented to the ED within three years, from 1st January 2019 to 31st December 2021, were included in the study. Critical illness was primarily defined as present in any patient who either had a severe derangement of one or more vital signs as measured at triage or received a critical care intervention at the ED. The critical interventions included oxygen therapy, intubation, suction, tracheostomy, cardiopulmonary resuscitation, adrenaline/epinephrine, atropine, and chest tube insertion. The vital signs included systolic blood pressure (SBP), pulse rate (HR), respiratory rate (RR), blood oxygen saturation (SpO2%), and the Glasgow coma scale (GCS). The age-dependent cut-offs for severe derangement of vital signs were based on previous literature (Table 1) [1, 19–22].
Table 1.
Cut-offs for severely deranged vital signs by age
| Vital Sign | Age | Severely Deranged Cut-off |
|---|---|---|
| Respiratory rate per minute | < 1 month | < 20 or > 80 |
| 1 month-<1 year | < 15 or > 60 | |
| 1 year- <5 years | < 10 or > 50 | |
| 5 years- 12 years | < 8 or > 40 | |
| > 12 years | < 8 or > 30 | |
| Saturation (%) | All | < 90% |
| Pulse rate per minute | < 1 month | < 80 or > 200 |
| 1 month- <1 year | < 80 or > 180 | |
| 1 year- <5 years | < 70 or > 170 | |
| 5 years- 12 years | < 60 or > 150 | |
| > 12 years | < 40 or > 130 | |
| Glasgow Coma Scale | All | ≤ 8/15 |
| Systolic Blood Pressure (mmHg) | < 3 months | < 50 |
| 3 months- <1 year | < 70 | |
| 1 year- <4 years | < 75 | |
| 4 years- <12 years | < 80 | |
| ≥ 12 years | < 90 |
Because critical illness is notoriously difficult to define [2, 4], and due to the limitations of our data source, retrospective data collected primarily for clinical purposes, we used two additional, alternative definitions to estimate the burden of critical illness in sensitivity analyses. First, we used a broader definition for critical illness, including patients who received care in the resuscitation room or the mini-ICU in the ED in addition to those in the primary definition. The second alternative definition was more restrictive and included only patients with one or more severely deranged vital signs.
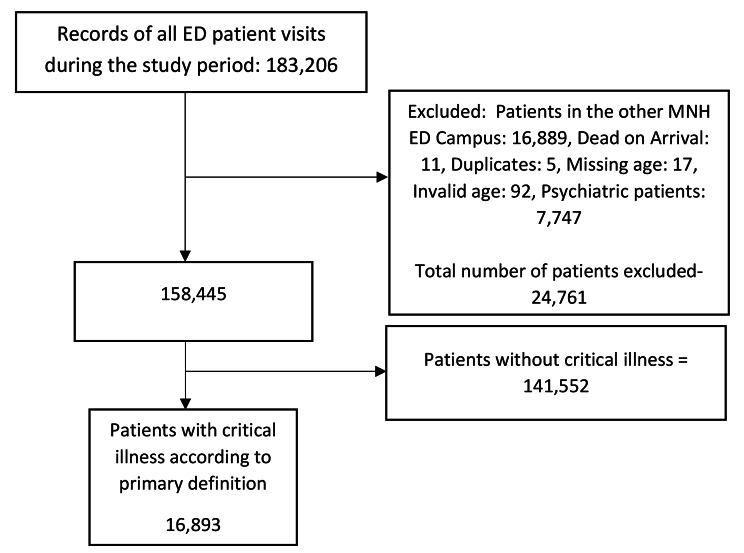
We excluded from this study records of patients who lacked data for their age or were dead at arrival. Psychiatric patients with non-somatic complaints were also excluded, as were those in the electronic information system but had received care in the ED of MNH’s additional campus (Fig. 1).
Fig. 1.
Flowchart of the data extraction for the study participants
Data extraction, management, and analysis
Anonymized data were extracted from the electronic information system in Excel format and were imported into STATA 17 (StataCorp, Texas, USA). Eligible patients were identified, and duplicates were removed. The data were cleaned and checked for their validity and completeness, and outliers were identified and cleaned or removed if not plausible. Descriptive statistics using frequencies, percentages, median and interquartile range (IQR) were used to summarize the patients’ demographic and clinical characteristics.
Missing vital signs were imputed as not being severely deranged. A sensitivity analysis where missing vital signs were imputed as severely deranged was done. Imputation was not done for the Glasgow Coma Scale for all patients and not for systolic blood pressure for children under 15 years, as there was significant non-random missing data.
The burden of critical illness, defined by the primary and alternative definitions and the sensitivity analysis, was calculated and presented. Using the primary definition, the total number and proportion of critically ill patients per year and their mean daily/monthly numbers were calculated. The trend of the monthly proportion of patients who were critically ill was presented with line graphs, together with the number of critically ill, non-critically ill and total number of patients. The proportion of critically ill patients were further disaggregated by the demographic of the patients. The proportion of critical illness by year was done, and the chi-squared test was used to compare the observed proportion of critical illness in 2020 and 2021 to that in the first year, 2019. Diagnoses of critically ill patients were classified according to the first listed diagnosis and grouped using the organ system affected. Outcomes at the ED were presented using pie charts, and admission wards were categorized and presented using bar graphs.
Results
There were 158,445 patient visits to the ED between January 2019 and December 2021. On average, 4,401 patient visits were made per month – 144.6 per day. The median age (IQR) of patients who attended the ED was 34.6 (21.0- 54.1) years. About 60% of all patients were below 45 years of age, and over half (55%) were men. Most of the patients (80.9%) who attended the ED came from Dar es Salaam and the neighboring regions in the Eastern zone. Less than half of the patients (46.8%) had health insurance coverage, and 14.9% of the patients were brought in using an ambulance (Table 2).
Table 2.
Demographic characteristics of patients who attended the MNH ED 2019–2021
| Variable | 2019 (61,815) | 2020 (47,361) | 2021 (49,269) | Overall (158,445) |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | N (%) | |
| Age group | ||||
| 0- <15 years | 11,993 (19.4) | 9452 (20.0) | 9645 (19.6) | 31,090 (19.6) |
| 15- <30 years | 14,628 (23.7) | 10,295 (21.7) | 10,319 (20.9) | 35,242 (22.2) |
| 30- <45 years | 13,441 (21.7) | 10,544 (22.3) | 11,077 (22.5) | 35,062 (22.1) |
| 45- <60 years | 10,761 (17.4) | 8161 (17.2) | 8734 (17.7) | 27,656 (17.5) |
| 60- <75 years | 8008 (13.0) | 6487 (13.7) | 6919 (14.0) | 21,414 (13.5) |
| 75-<90 years | 2735 (4.4) | 2189 (4.6) | 2356 (4.8) | 7280 (4.6) |
| >=90 years | 249 (0.4) | 233 (0.5) | 219 (0.4) | 701 (0.4) |
| Sex | ||||
| Male | 33,801 (54.7) | 25,968 (54.8) | 27,331 (55.5) | 87,100 (55.0) |
| Female | 28,014 (45.3) | 21,393 (45.2) | 21,938 (44.5) | 71,345 (45.0) |
| Zones | ||||
| Dar Es Salaam & Eastern Zone | 49,852 (80.6) | 38,033 (80.3) | 40,279 (81.8) | 128,164 (80.9) |
| Elsewhere | 11,963 (19.4) | 9328 (19.7) | 8990 (18.2) | 30,281 (19.1) |
| Mode of Arrival | ||||
| Ambulance | 8662 (14.0) | 7300 (15.4) | 7665 (15.6) | 23,627 (14.9) |
| Public transport | 24,893 (40.3) | 18,115 (38.3) | 17,412 (35.3) | 60,420 (38.1) |
| Private car/ Taxi | 18,745 (30.3) | 15,856 (33.5) | 16,716 (33.9) | 51,317 (32.4) |
| Walked | 3592 (5.8) | 2496 (5.3) | 2258 (4.6) | 8346 (5.3) |
| Others* | 498 (0.8) | 594 (1.3) | 311 (0.6) | 1403 (0.9) |
| Missing | 5425 (8.8) | 3000 (6.3) | 4906 (10.0) | 13,331 (8.4) |
| Payment Mode | ||||
| Public/ Cost sharing | 26,896 (43.5) | 22,122 (46.7) | 22,948 (46.6) | 71,966 (45.4) |
| Health Insurance | 30,456 (49.3) | 21,194 (44.7) | 22,527 (45.7) | 74,177 (46.8) |
| Private Payment | 2614 (4.2) | 2375 (5.0) | 2269 (4.6) | 7258 (4.6) |
| Others** | 162 (0.3) | 102 (0.2) | 249 (0.5) | 513 (0.3) |
| Missing | 1687 (2.7) | 1568 (3.3) | 1276 (2.6) | 4531 (2.9) |
* stretchers, carried by good samaritans
** Exemption, foreigners
The burden of critical illness
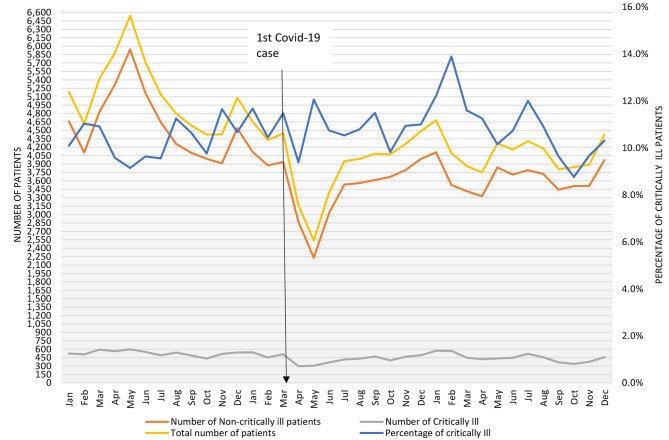
According to the primary definition, 16,893 (10.7%) patients were critically ill. These include 5475 patients (3.5%) classified as critically ill as they received critical care interventions and 13,893 patients (8.8%) classified as critically ill as they had one or more severely deranged vital signs (Table 3). The number and proportion of patients at the ED who were critically ill were 6,345 (10.3%) for 2019, 5,148 (10.9%) for 2020 (X2 p-value = 0.001), and 5,400 (11.0%) for 2021 (X2 p-value < 0.001) (Fig. 2). The mean number of critically ill patients seen per month at the ED was 481 (ranging from 297 to 598, mean per day = 15.4).
Table 3.
Clinical characteristics of patients who attended the MNH ED 2019–2021
| Variable | 2019 (61,815) | 2020 (47,361) | 2021 (49,269) | Overall (158,445)* |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | N (%) | |
| Severely Deranged SBP | ||||
| No | 47,023 (76.1) | 36,617 (77.3) | 38,574 (78.3) | 122,214 (77.1) |
| Yes | 1052 (1.7) | 716 (1.5) | 760 (1.5) | 2528 (1.6) |
| Missing | 13,740 (22.2) | 10,028 (21.2) | 9935 (20.2) | 33,703 (21.3) |
| Severely Deranged RR | ||||
| No | 54,390 (88.0) | 42,407 (89.5) | 42,504 (86.3) | 139,301 (87.9) |
| Yes | 981 (1.6) | 977 (2.1) | 825 (1.7) | 2783 (1.8) |
| Missing | 6444 (10.4) | 3977 (8.4) | 5940 (12.1) | 16,361 (10.3) |
| Severely Deranged HR | ||||
| No | 53,636 (86.8) | 42,049 (88.8) | 42,148 (85.5) | 137,833 (87.0) |
| Yes | 2498 (4.0) | 1963 (4.1) | 1869 (3.8) | 6330 (4.0) |
| Missing | 5681 (9.2) | 3349 (7.1) | 5252 (10.7) | 14,282 (9.0) |
| Severely Deranged SpO2 | ||||
| No | 54,832 (88.7) | 42,870 (90.5) | 42,757 (86.8) | 140,459 (88.6) |
| Yes | 1396 (2.3) | 1245 (2.6) | 1384 (2.8) | 4025 (2.5) |
| Missing | 5587 (9.0) | 3246 (6.9) | 5128 (10.4) | 13,961 (8.8) |
| Severely Deranged GCS | ||||
| No | 8259 (13.4) | 7754 (16.4) | 7759 (15.7) | 23,772 (15.0) |
| Yes | 311 (0.5) | 232 (0.5) | 238 (0.5) | 781 (0.5) |
| Missing | 53,245 (86.1) | 39,375 (83.1) | 41,272 (83.8) | 133,892 (84.5) |
| Received Critical Care Intervention | ||||
| No | 55,786 (90.2) | 42,673 (90.1) | 42,109 (85.5) | 140,568 (88.7) |
| Yes | 1966 (3.2) | 1648 (3.5) | 1861 (3.8) | 5475 (3.5) |
| Missing | 4063 (6.6) | 3040 (6.4) | 5299 (10.8) | 12,402 (7.8) |
SBP- Systolic Blood Pressure, RR- Respiratory rate, HR- Heart rate, GCS- Glasgow Coma Scale, SpO2- Oxygen Saturation
* The sum of severely deranged individual vital signs is more than the total number of critically ill patients as patients could have more than one severely deranged vital sign
Fig. 2.
Monthly trend of critical illness in the MNH ED from January 2019 to December 2021. Includes the proportion of patients who were critically ill and the absolute numbers of critically ill, non-critically ill, and total patients who attended the ED each month since January 2019
Using the alternative definitions, the burden of critically-ill patients was 8.8% for those with severely deranged vitals alone and 30.8% when patients who received care in the resuscitation rooms or the mini ICUs were also included. When patients with missing vitals were imputed as critically ill, the estimated burden was 21.0%.
The burden of critical illness by socio-demographic characteristics
The median age (IQR) of critically ill patients was 36 (15.1–57.9) years. Males comprised slightly over half (54.4%) of the critically ill patients, and about a quarter (24.8%) were children under the age of 15 years. About a third (34.3%) of critically ill patients had health insurance, and over a third (37.1%) of them were brought to the ED by ambulance.
The proportion critically ill patients among male and female patients attending the MNH ED was 10.6% and 10.8%, respectively. The proportion of critically ill patients was highest among patients attending the ED who were older than 90 years (17.4%), those 75–90 years (13.8%), and children under 15 years (13.5%). About one in ten patients from other regions (11.9%) were critically ill, similarly for patients coming from Dar es Salaam and the Eastern zone (10.4%). The proportion of critical illness was highest among patients who were paying out-of-pocket (10.9%) and on public/cost-sharing plans (13.7%) and was lowest among patients with health insurance (7.8%). About one in four patients, (26.6%), brought by an ambulance were critically ill —Table 4.
Table 4.
Distribution and prevalence of critically ill patients by demographic characteristics
| Variable | 2019 (N = 6345) |
2020 (N = 5148) |
2021 (N = 5400) |
Overall (N = 16,893) | Proportion of critically ill (%) |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | ||
| Median age in years (IQR) | 34.7 (14.0, 56.0) | 36.6 (15.4, 58.5) | 39 (16.5, 59.2) | 36.47 (15.1, 58) | |
| Age groups | |||||
| 0–15 years | 1628 (25.7) | 1264 (24.6) | 1295 (24.0) | 4187 (24.8) | 13.5 |
| 15- <30 years | 1146 (18.1) | 865 (16.8) | 832 (15.4) | 2843 (16.8) | 8.1 |
| 30- <45 years | 1196 (18.8) | 938 (18.2) | 964 (17.9) | 3098 (18.3) | 8.8 |
| 45- <60 years | 1037 (16.3) | 878 (17.1) | 997 (18.5) | 2912 (17.2) | 10.5 |
| 60- <75 years | 926 (14.6) | 858 (16.7) | 939 (17.4) | 2723 (16.1) | 12.7 |
| 75-<90 years | 364 (5.7) | 308 (6.0) | 336 (6.2) | 1008 (6.0) | 13.8 |
| >=90 years | 48 (0.8) | 37 (0.7) | 37 (0.7) | 122 (0.7) | 17.4 |
| Sex | |||||
| Male | 3470 (54.7) | 2754 (53.5) | 2971 (55.0) | 9195 (54.4) | 10.6 |
| Female | 2875 (45.3) | 2394 (46.5) | 2429 (44.9) | 7698 (45.6) | 10.8 |
| Zone | |||||
| Dar Es Salaam & Eastern zone | 4996 (78.7) | 4050 (78.7) | 4344 (80.4) | 13,390(79.3) | 10.4 |
| Elsewhere | 1349 (21.3) | 1098 (21.3) | 1056 (19.6) | 3503 (20.7) | 11.6 |
| Payment Mode | |||||
| Public/ Cost sharing | 2298 (36.2) | 1915 (37.2) | 2062 (38.2) | 6275 (37.1) | 13.7 |
| Health Insurance | 1579 (24.9) | 1224 (23.8) | 1160 (21.5) | 3963 (23.5) | 7.8 |
| Private Payment | 2221 (35.0) | 1867 (36.3) | 2058 (38.1) | 6146 (36.4) | 10.9 |
| Others | 154 (2.4) | 74 (1.4) | 76 (1.4) | 304 (1.8) | 9.7 |
| Missing | 63 (1.0) | 67 (1.3) | 38 (0.7) | 168 (1.0) | 9.4 |
| Mode of arrival | 30 (0.5) | 1 (< 1) | 6 (0.1) | 37 (0.2) | |
| Ambulance | 26.6 | ||||
| Public transport | 3688 (58.1) | 3093 (60.1) | 3048 (56.4) | 9829 (58.2) | 7.1 |
| Private car/ Tax | 2226 (35.1) | 1649 (32.0) | 1917 (35.5) | 5792 (34.3) | 11.9 |
| Walked | 263 (4.1) | 250 (4.9) | 281 (5.2) | 794 (4.7) | 3.6 |
| others | 15 (0.2) | 11 (0.2) | 24 (0.4) | 50 (0.3) | 10.5 |
| Missing | 153 (2.4) | 145 (2.8) | 130 (2.4) | 428 (2.5) | 0.3 |
Underlying first-listed diagnoses among critically ill patients
The five-leading diagnoses among patients with critical illness were respiratory diseases (18.8%), cardiovascular diseases (12.6%), infectious diseases and trauma contributing each 10.2%, and malignancies (8.7%) —Table 5. The list of diseases in each categories can be found in Supplement 1.
Table 5.
Disease categories of the first-listed diagnoses of patients attended at the ED
| Diseases Categories | Frequency | Percent (%) |
|---|---|---|
| Respiratory Diseases | 3,172 | 18.8 |
| Cardiovascular Diseases | 2,128 | 12.6 |
| Infectious diseases | 1,720 | 10.2 |
| Injury & Trauma | 1,719 | 10.2 |
| Cancers/ Malignancies | 1,462 | 8.7 |
| Neurological Diseases | 1,291 | 7.6 |
| Gastrointestinal Diseases | 1,160 | 6.9 |
| Renal Diseases | 787 | 4.7 |
| Hematological Diseases | 708 | 4.2 |
| Endocrine Diseases | 308 | 1.8 |
| Urinary tract Diseases | 256 | 1.5 |
| Others | 2,066 | 12.2 |
| Missing | 116 | 0.7 |
Outcomes of critically ill patients at the ED
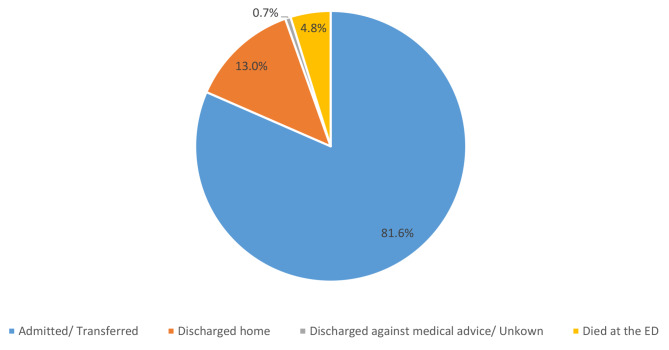
Most, 13,777 (81.6%), of the critically ill patients presenting at the ED were admitted, and 809 (4.8%) died at the ED. About 13% of the critically ill patients were discharged after treatment at the ED (Fig. 3). The proportion of critically ill patients who died in the ED was 4.2% in 2019 and 4.3% in 2020 (X2 = 0.744), and 5.9% in 2021 (X2 < 0.001).
Fig. 3.
Outcome of critically ill patients at the ED (N = 16,893)
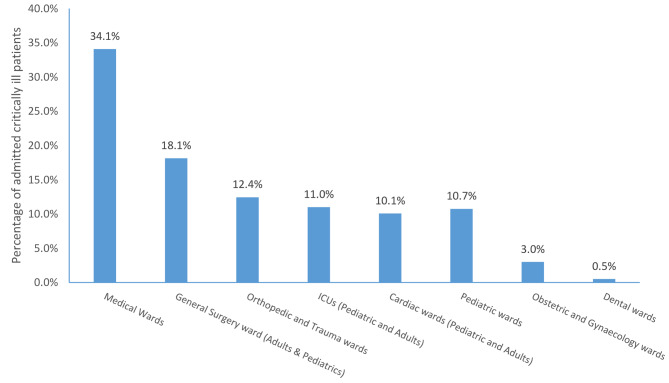
Among those admitted, 11% of critically ill patients were admitted to the ICUs (Pediatric ICU, neonatal ICU, or adult ICU), and 89% were admitted to general wards (Fig. 4).
Fig. 4.
The proportion of admitted critically ill patients by specialty of care (N = 13,777)
Discussion
Critically ill patients make up about 10% of all patients attended at the ED of a national hospital in Tanzania. The COVID-19 pandemic did not lead to an increase in patient numbers – in fact the overall number of patients who attended the ED and the number of critically ill patients in 2020 and 2021 was lower than that in 2019. The major diagnoses leading to critical illness were respiratory, cardiovascular, and infectious diseases as well as trauma, and the majority of the critically ill were admitted to the hospital’s general wards.
Although the proportion of critically ill at the ED increased slightly in the years under review, the number of ED visits declined. Hence, the observed increase in the proportion of critical illness is driven by a sharper decline of non-critically ill patients than of critically ill patients. Although COVID-19 has been reported to cause critical illness in up to 30% of patients, it is striking that the start of the pandemic in Tanzania in April 2020 coincides with a decrease in patients coming to the ED. This may be due to public health responses, changes in health system policies, or changed community practices of attending the national hospital during the pandemic. Similar findings have been observed in other settings globally [13, 23, 24]. It should be noted that although Tanzania did not implement strict lockdown measures, several preventive measures were implemented in the first wave in 2020[25]. The decreasing number of critically ill patients may also be due to a decline in other conditions, such as road traffic trauma during the pandemic [26].
The proportion of critical illness observed in this study is higher than that reported in a study done previously at the same facility, describing critical illness among adults (6.9%) [12]. Their criteria for critical illness included a triage category and an early warning score cut-off which is more restrictive than in our study. Using more generous individual deranged vital signs as criteria in our study avoids missing an important proportion of patients with a higher risk of death [21].
Critically ill patients had higher ED mortality (4.8%) compared to the ED mortality of all the patients (0.6%) and much higher than non-critically ill (0.06%). The derangement of at least one physiologic parameter has been associated with higher mortality, but early recognition of the derangement and interventions has shown evidence to reduce mortality for some conditions of critically ill patients [27, 28]. The ED mortality among critically ill patients was higher in 2021 than in 2019 or 2020. The reasons for this observation are still unclear, and further investigation is warranted.
The underlying causes of critical illness were diverse. Both infectious and non-communicable diseases are prevalent in Tanzania and cause substantial burdens of critical illness [29]. Indeed, critical illness can be due to a large variety of underlying diseases and can be found in all medical specialties. Specialty or disease-based programs may find it challenging to provide quality care for critically ill patients, and thus all wards and areas of health facilities require the capacity to provide care for critically ill patients. We found that only 11% of critically ill patients were admitted to ICU, while 89% were admitted to general wards. Using ICU-treated patients as the indicator of the burden of critical illness, as has been done previously, can significantly underestimate the burden of critical illness, even in tertiary hospitals [4]. Studies have shown that there is a lack of resources for the provision of emergency and critical care in LMICs [9, 10, 30]. To increase resources and improve care, especially ward-based care for critical illness, the approach described as essential emergency and critical care (EECC) should be implemented [7, 19, 31]. EECC is defined as “the effective lifesaving care of low- cost and low- complexity that all critically ill patients should receive in all wards in all hospitals in the world”. It focuses on early identification of critical illness, timely provision of life-saving care and that is of low cost and low complexity [7, 31]. Because critically ill patients comprises a heterogeneous group of patients, EECC should be a critical part in every specialty in a health facilities, as it improves the care given to critically ill patients and substantially reduce preventable deaths [19, 28].
Strengths and limitations of the study
This study used a single parameters rather than compound scores such as early warning scores because single parameters are easy and less time consuming when resources are limited, and avoid calculation errors. Moreover, single parameters indicate the action that could be taken (such as give oxygen if low saturation) which compound scores don’t [32]. Another strength is that this large study over three years includes a population of over 150,000 patients presenting to the hospital and almost 17,000 critically ill patients. This enables precise estimates of the burden and disaggregation of estimates. However, the study is from a single national center which is not necessarily representative of other settings in the country. Another limitation of this study is the use of hospital record data, where some vital signs data were missing and were treated as not severely deranged. As a result there is a possibility that the burden of critical illness due to deranged vital signs is underestimated. However, we also presented the estimates of the burden where missing values were imputed as severely deranged, which may overestimate the burden. Also, although the analysis of the underlying diagnoses using the clinicians’ recorded first-listed diagnosis has provided useful information, it is imperfect as it relies on the assumption that the first listed diagnosis is the most important and that diagnoses are correct – both assumptions may not hold.
Conclusions
More than one in ten patients attending the emergency department of a Tanzanian National Hospital had a critical illness. The number of critically ill patients did not increase during the pandemic. The majority were admitted to general hospital wards, and about one in twenty died at the ED. This study highlights the burden of critical illness faced by hospitals and the need to ensure the availability and quality of emergency and critical care throughout hospitals.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We thank the patients, their families, and medical personnel at the Muhimbili National Hospital Emergency Department. We also thank the administration and personnel of the Muhimbili national hospitals, the National Institute for Medical Research, and the Muhimbili University of Health and Allied Sciences, particularly the Directorate of Research and Publications.
Abbreviations
- ED
Emergency department
- EECC
Essential Emergency and Critical Care
- GCS
Glasgow Coma Scale
- HR
Pulse rate
- ICU
Intensive Care Unit
- IQR
Inter Quartile Range
- JKCI
Jakaya Kikwete Cardiac Institute
- MNH
Muhimbili National Hospital
- MOI
Muhimbili Orthopedic Institute
- MUHAS
Muhimbili University of Health and Allied Sciences
- RR
Respiratory rate
- SBP
Systolic Blood Pressure
- SpO2
Oxygen Saturation
Author contributions
EAM- conceptualization, data extraction and curation, formal analysis, validation, writing and revising original manuscript. HPN- conceptualization, data extraction and curation, validation, review and editing the manuscript. DEA- conceptualization, review and editing the manuscript. PN- conceptualization, data validation, review and editing the manuscript. VM- Review and editing the manuscript. HB- Review and editing the manuscript. RM- data extraction, validation, review and editing the manuscript. RH- conceptualization, review and editing the manuscript. AB- conceptualization, review and editing the manuscript. JM- conceptualization, supervision, review and editing the manuscript. BS- conceptualization, supervision, review and editing the manuscript. HS- conceptualization, supervision, review and editing the manuscript. TB- conceptualization, supervision, data extraction and curation, formal analysis, validation, writing and revising original manuscript. supervision, review and editing the manuscript.
Funding
This study was supported by the African critical care registry network for pandemic surveillance, clinical management and research (MRC/UKRI MR/V030884/1), and by the Laerdal Foundation (2021-0097) and the Wellcome Trust [220211].
The funders had no role in study design, data collection/extraction and analysis, decision to publish, or manuscript preparation.
Data Availability
The data that support the findings of this study are available from the Muhimbili National Hospital but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. However, upon request and following national policies for data sharing, data may be accessed to researchers requesting and fulfilling requirements as per the Tanzanian National Health Research Ethics guidelines. Contact information: National Health Research Ethics Review Committee Contact email: jikingura@nimr.or.tz Postal address: National Institute for Medical Research P.O. Box 9653 Dar es Salaam, Tanzania.
Declarations
Ethics approval and consent to participate
Ethical approval to conduct this study was obtained from the Muhimbili University of Health and Allied Sciences Research and Ethics Committee (MUHAS-REC-4-2020-217) and the National Health Research and Ethics Committee (NIMR/HQ/R.8a/Vol. IX/3752). Permission to extract patient data was obtained from Muhimbili National Hospital (MNH/TRCU/IRB/Perm/2021/082). Since the study involved anonymized secondary data analysis, informed consent was also waived by the above committees. All the methods were performed in accordance to the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
All other authors have declared no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Baker T. Critical care in Low Resources Settings. Stockholm: Karolinska Institutet; 2015. p. 68. [Google Scholar]
- 2.Kayambankadzanja RK, Schell CO, Wärnberg MG, Tamras T, Mollazadegan H. Towards definitions of critical illness and critical care using concept analysis. BMJ Open. 2022;12(e060972):1–11. doi: 10.1136/bmjopen-2022-060972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adhikari NKJ, Fowler RA, Bhagwanjee S, Rubenfeld GD. Critical care and the global burden of critical illness in adults. Lancet. 2010;376(9749):1339–46. doi: 10.1016/S0140-6736(10)60446-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baker T, Schultz MJ, Dünser MW. Critical illness in developing countries: Dying in the dark. Lancet. 2011;377(9775):1405. Available from: 10.1016/S0140-6736(11)60572-2. [DOI] [PubMed]
- 5.Vincent J, Marshall JC, Ñamendys-silva SA, François B, Martin-loeches I, Lipman J et al. Assessment of the worldwide burden of critical illness: the Intensive Care Over Nations (ICON) audit. Lancet Respir Med. 2014;2(May). [DOI] [PubMed]
- 6.Ruggiero RM. Author ’ s Accepted Manuscript. Am J Med Sci. 2017; Available from: 10.1016/j.amjms.2017.07.001.
- 7.Schell CO, Gerdin Wärnberg M, Hvarfner A, Höög A, Baker U, Castegren M, et al. The global need for essential emergency and critical care. Crit Care. 2018;22(1):1–5. doi: 10.1186/s13054-018-2219-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sultan M, Mengistu G, Debebe F, Azazh A, Trehan I. The burden on emergency centres to provide care for critically ill patients in Addis Ababa, Ethiopia. African J Emerg Med. 2018;8(4):150–4. Available from: 10.1016/j.afjem.2018.07.006. [DOI] [PMC free article] [PubMed]
- 9.Kayambankadzanja RK, Likaka A, Mndolo SK, Chatsika M, Umar E, Baker T. Emergency and critical care services in Malawi: findings from a nationwide survey. of health facilities. 2020;32(March):19–23. doi: 10.4314/mmj.v32i1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baker T, Lugazia E, Eriksen J, Mwafongo V, Irestedt L, Konrad D. Emergency and critical care services in Tanzania: a survey of ten hospitals. BMC Health Serv Res. 2013;13(140):1–9. Available from: http://www.biomedcentral.com/1472-6963/13/140. [DOI] [PMC free article] [PubMed]
- 11.Sawe HR, Mfinanga JA, Mwafongo V, Reynolds TA, Runyon MS. Trends in mortality associated with opening of a full-capacity public emergency department at the main tertiary-level hospital in Tanzania. Int J Emerg Med. 2015;8(24):4–9. Available from: 10.1186/s12245-015-0073-4. [DOI] [PMC free article] [PubMed]
- 12.Kiremeji MK, Kilindimo S, Sawe HR, Kitapondya D, Edward U. Clinical Profile and Outcome of critically ill adult patient ’ s presenting to an urban Emergency Department in sub Saharan Africa: a prospective cohort study in Tanzania. 2020;1–6.
- 13.Butt AA, Azad AM, Kartha A, Masoodi NA, Bertollini R, Samra-Abou A-B, VOLUME AND ACUITY OF EMERGENCY DEPARTMENT VISITS PRIOR TO AND AFTER COVID-19 J Emerg Med. 2020;59(5):730–4. doi: 10.1016/j.jemermed.2020.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Naderi-Azad S, Manion R, Alhusayen R. Impact of COVID-19 on Access to Care: A National Patient Survey. J Cutan Med Surg. 2021;25(4):453–5. doi: 10.1177/12034754211013035. [DOI] [PubMed] [Google Scholar]
- 15.Miyah Y, Benjelloun M, Lairini S, Lahrichi A. COVID-19 Impact on Public Health, Environment, Human Psychology, Global Socioeconomy, and Education. 2022;2022. [DOI] [PMC free article] [PubMed]
- 16.Kwesigabo G, Mwangu MA, Kakoko DC, Warriner I, Mkony CA, Killewo J et al. Tanzania ’ s health system and workforce crisis. J Public Health Policy. 2012;33(2012):35–44. [DOI] [PubMed]
- 17.MOHCDGEC, COVID-19 SITUATION, REPORT. : NO 18 From 08th to 14th January, 2022. MINISTRY OF HEALTH, COMMUNITY DEVELOPMENT, GENDER, ELDERLY AND CHILDREN. 2022. p. 6. Available from: https://www.moh.go.tz/report.
- 18.WHO. WHO Coronavirus (COVID-19) Dashboard. 2023 [cited 2023 Feb 20]. Available from: https://covid19.who.int/.
- 19.Schell CO, Castegren M, Lugazia E, Blixt J, Mulungu M, Konrad D, et al. Severely deranged vital signs as triggers for acute treatment modifications on an intensive care unit in a low-income country Health Services Research. BMC Res Notes. 2015;8(1):1–7. doi: 10.1186/s13104-015-1275-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ngwalangwa F, Phiri CHA, Dube Q, Langton J, Hildenwall H, Baker T. Risk factors for mortality in severely Ill Children admitted to a Tertiary Referral Hospital in Malawi. Am J Trop Med Hyg. 2019;101(3):670–5. doi: 10.4269/ajtmh.19-0127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bell MB, Konrad D, Granath F, Ekbom A, Martling C. Prevalence and sensitivity of MET-criteria in a Scandinavian University Hospital à¬. Resuscitation. 2006;70:66–73. doi: 10.1016/j.resuscitation.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 22.WHO. Pocket book of hospital care for children: guidelines for the management of common childhood illnesses, 2nd edition. 2nd editio. Geneva: World Health Organization. ; 2013. 438 p. [PubMed]
- 23.Sierra NB, Bossuyt N, Braeye T, Leroy M, Moyersoen I, Peeters I et al. All-cause mortality supports the COVID-19 mortality in Belgium and comparison with major fatal events of the last century. 2020;1–8. [DOI] [PMC free article] [PubMed]
- 24.Jennifer M. Characteristics of and important Lessons from the Coronavirus Disease 2019 (COVID-19) outbreak in China Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. 2020;323(13). [DOI] [PubMed]
- 25.Mfinanga SG, Mnyambwa NP, Minja DT, Ntinginya NE, Ngadaya E, Makani J et al. Tanzania ’ s position on the COVID-19 pandemic Global health and its discontents. Lancet. 2021;397(10284):1542–3. Available from: 10.1016/S0140-6736(21)00678-4. [DOI] [PMC free article] [PubMed]
- 26.Butt AA, Kartha A, Asaad N, Azad AM, Bertollini R, Badi A et al. Impact of COVID – 19 upon changes in emergency room visits with chest pain of possible cardiac origin. BMC Res Notes. 2020;1–4. Available from: 10.1186/s13104-020-05381-y. [DOI] [PMC free article] [PubMed]
- 27.Baker T, Blixt J, Lugazia E, Schell CO, Mulungu M, Milton A, et al. Single deranged physiologic parameters are Associated with Mortality in a low-income country. Crit Care Med. 2015;43(10):2171–9. doi: 10.1097/CCM.0000000000001194. [DOI] [PubMed] [Google Scholar]
- 28.Baker T, Schell CO, Lugazia E, Blixt J, Mulungu M, Castegren M, et al. Vital Signs directed therapy: improving care in an intensive care unit in a low-income country. PLoS ONE. 2015;10(12):1–15. doi: 10.1371/journal.pone.0144801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Akaninyene O, Okpa H, Effa E. The Pattern of Respiratory Disease Morbidity and Mortality in a Tertiary Hospital in Southern-Eastern Nigeria. Pulm Med. 2013. [DOI] [PMC free article] [PubMed]
- 30.Coyle RM, Harrison HL. Emergency care capacity in Freetown, Sierra Leone: A service evaluation. BMC Emerg Med. 2015;15(1):1–9. doi: 10.1186/s12873-015-0027-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schell CO, Khalid K, Wharton A, Sanga A, Oliwa J, Sawe HR, et al. Essential emergency and critical care: a consensus among global clinical experts. BMJ Glob Heal. 2021;6(e006585):1–12. doi: 10.1136/bmjgh-2021-006585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baker T, Gerdin M. The clinical usefulness of prognostic prediction models in critical illness. Eur J Intern Med. 2017;45:37–40. Available from: 10.1016/j.ejim.2017.09.012. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the Muhimbili National Hospital but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. However, upon request and following national policies for data sharing, data may be accessed to researchers requesting and fulfilling requirements as per the Tanzanian National Health Research Ethics guidelines. Contact information: National Health Research Ethics Review Committee Contact email: jikingura@nimr.or.tz Postal address: National Institute for Medical Research P.O. Box 9653 Dar es Salaam, Tanzania.