Abstract
Background:
First metatarsophalangeal (MTP) joint arthrodesis can be fixed using either a dorsal plate or crossed screws. However, there is considerable difference in the cost of these implants, and it is not known if there is sufficient difference in outcome that might justify this cost difference. Our aim was to compare the functional results and patient satisfaction rates after first MTP joint arthrodesis in a group of patients using the same surgical technique except for the fixation devices.
Methods:
A prospective cohort of 27 patients who underwent first MTP joint fusion by the same surgeon using 2 crossed screws or a single screw with a dorsal plate was recruited over a 3-year period. Demographic information, patient satisfaction rates, complications, and union rates were evaluated. American Orthopaedic Foot & Ankle Society (AOFAS) and visual analog scale (VAS) scoring systems were used pre- and postoperatively to compare the functional outcomes. Thirty consecutive procedures (screws, n = 15; plate, n = 15) were performed. Age (55.8 ± 11.1 vs 63.3 ± 12.4 years for screws and plate respectively; P = .091) and female gender percentages (80% and 73%, P = .666) were similar between groups.
Results:
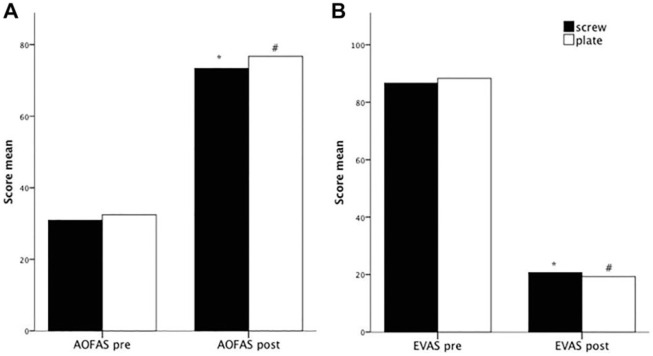
The overall union rate was 93% with no differences between groups. AOFAS and VAS scores improved significantly postoperatively for each technique, and no differences were found between the two in the improvement in AOFAS (42.4 ± 8.0 vs 44.3 ± 8.2, screws and plate respectively; P = .520) and VAS scores (66.0 ± 5.4 vs 69.0 ± 6.9;P = .195). The implant cost for screws was $40 and for dorsal plate, $328.
Conclusions:
First MTP joint fusion using either screws or plate fixation results in an improvement in AOFAS and VAS scores. Functional improvement and patient satisfaction did not differ between the 2 techniques, despite a considerable difference in cost between the two methods of fixation.
Level of Evidence:
Level III, prospective comparative study.
Keywords: first MTP arthrodesis, fixation technique, cost effectiveness
Commentary: In this Level III prospective comparative study two approaches to first metatarsophalangeal fusion are evaluated: Plates and screws vs. screws alone were used in 2 cohorts of 15 patients. Other than expense of implant, no differences in outcome were found. The power of the findings are limited by sample size.
Introduction
The efficacy and predictability of first MTP joint arthrodesis has been established with high patient satisfaction in addition to reliable pain relief, lasting correction of the deformity, and ability to resume most activities of daily living.5,8,11,14 For internal fixation, a stable construct is necessary and several methods have been advocated: lag screw, dorsal plate,4,5 wire loop,7,27 Kirschner wire (K-wire),7,9,23 cat gut suture, 24 Steinmann pin fixation, staples, 15 and an external fixator. 3 Among these, the use of a compression lag screw with a dorsal neutralization plate is the most biomechanically stable construct. 20 Nonetheless, the use of 2 crossed screws, a combination of screw and K-wire, or bone clamps for concentric arthritis of the MTP joint and good bone quality have been shown to be successful techniques and significantly less expensive.17,26
A central concern in medicine is to maintain quality while minimizing cost. The purpose of our study was to compare the functional results and patient satisfaction rates after first MTP joint fusion done at a single institution by one surgeon using the same surgical technique with different types of fixation that differ in cost.
Material and Methods
Patients
Our institutional review board approved this study, and patients gave informed consent for participation in the study. A total of 27 patients (30 MTP joints) who had MTP joint arthrodesis performed by a single surgeon at one institution between January 2012 and December 2015 were prospectively enrolled in the study. Patient demographic variables and pathology were recorded (Table 1).
Table 1.
Demographic Data. a
| Screws | Plate | P | |
|---|---|---|---|
| Age, mean ± SD | 55.8 ± 11.1 | 63.3 ± 12.4 | .91 |
| Female gender | 12 (80) | 11 (73) | .666 |
| RA | 3 (20) | 1 (7) | .283 |
| Smoke tobacco | 3 (20) | 4 (27) | .666 |
| DM | 1 (7) | 1 (7) | 1.0 |
| Diagnosis | .828 | ||
| Hallux rigidus | 11 (73) | 12 (80) | |
| Severe bunion | 2 (13) | 1 (7) | |
| Hallux varus | 2 (13) | 2 (13) |
Abbreviations: DM, diabetes mellitus; RA, rheumatoid arthritis.
Values are n% unless otherwise noted.
Included in the study were patients with first MTP joint arthrodesis with the use of either 2 solid crossed compression steel screws (3.5-mm small fragment screw, DePuy Synthes, Inc, Raynham, MA; $19.91 each) (Figure 1) or a single solid oblique compression steel screw (2.7-mm small fragment screw; DePuy Synthes; $54.40) with a dorsal T shaped 2×3-hole nonlocking steel plate (2.7-mm small fragment plate, DePuy Synthes; $48.48) stabilized with 4 or 5 solid compression steel screws (2.7-mm small fragment screw; DePuy Synthes; $45.03 each) (Figure 2). Patients were alternately assigned to the 2 treatment groups. There was no variation from this protocol at any time during the study.
Figure 1.
(A) Preoperative and (B) 1-year postoperative lateral and anteroposterior radiographs of a first MTP joint fusion performed with 2 crossed screws. MTP, metatarsophalangeal.
Figure 2.
(A) Preoperative and (B) 1-year postoperative lateral and anteroposterior radiographs of a first MTP joint fusion performed with a dorsal plate. MTP, metatarsophalangeal.
Surgery
A dorsal incision was made over the first MTP joint, the extensor hallucis tendon (EHL) was retracted medially and the caspule opened longitudinally. The joint was prepared with spherical reamers and completed with K-wire fenestration into the subchondral bone. The toe was then positioned both clinically and radiologically such that the tip of the toe rested on a flat metal surface and there was 0 to 8 degrees of valgus and 20 to 30 degrees of dorsiflexion at the MTP joint. In none of the patients was simultaneous bilateral surgery performed. Surgical time taken for each procedure was registered, and global surgical costs were calculated, considering that the operation theater (OT) rental cost is $400 per hour at our hospital.
Following surgery, a soft dressing was applied. Patients were kept nonweightbearing for 3 weeks after surgery. At the 3-week postoperative visit, the stiches were removed and the patients were allowed to fully weightbear using a postoperative shoe.12,17 Patients were followed clinically until radiographic fusion was evident.
Functional Evaluation
All patients were assessed clinically and radiographically by the treating surgeon 1 week, 3 weeks, 2 months, and 6 months after surgery. Symptoms were evaluated preoperatively and at 1 year after surgery using the American Orthopaedic Foot & Ankle Society (AOFAS) score 13 and the visual analog scale (VAS) score for pain during daily activities. Patient satisfaction rate, complications, and union rates were recorded.
Statistics
Categorical data (sex, rheumatoid arthritis, tobacco smoking, diabetes mellitus, diagnosis of main pathology, complications, willingness to do surgery again, and patient satisfaction) were expressed as the absolute number (%) and continuous variables (age and AOFAS and VAS scores) as mean ± SD.
Pre- and postoperative AOFAS and VAS scores were compared using a paired sample t test. Continuous variables between treatment groups were compared using Student t test. Categorical data were compared using chi-square.
Power analysis considering the mean AOFAS and VAS scores and type I and II errors of 0.05 and 80%, respectively, was performed using the results from our study. A P value of less than .05 was considered statistically significant. Finding a significant difference in functional outcome between the 2 techniques would require 278 patients per group.
Results
The overall union rate was 93%. Two patients (1 in each group) developed nonunion. Both patients were smokers and required revision.
Complications included 2 patients who developed nonunion, 2 patients who required hardware removal (1 in each group), 1 malunion (plate group), 1 dorsal dysesthesia (plate group), and 1 superficial infection (screw group).
No differences were seen between the preoperative VAS (86.7 ± 7.48 vs 88.3 ± 7.7 in the screws and plate groups, respectively; P = .553) and AOFAS (30.9 ± 6.9 vs 32.4 ± 8.8 in the screws and plate groups, respectively; P = .614) scores nor in the postoperative VAS (20.7 ± 9.6 vs 19.3 ± 9.4; P = .704) and AOFAS (73.3 ± 8.3 vs 76.7 ± 6.3; P = .215) scores among the treatment groups. For both treatment groups, the VAS and AOFAS scores improved significantly in the postoperative evaluation compared with the preoperative status (Figure 3).
Figure 3.
Preoperative (pre) and postoperative (post) functional evaluation using (A) AOFAS and (B) VAS scores. In black are patients who received screw and in white, patients who received plate treatment. *P < .05 pre vs post for screw technique; #P < .05 pre vs post for plate technique. AOFAS, American Orthopaedic Foot & Ankle Society; VAS, visual analog scale.
When patients were asked if they would undergo this surgery again, 25 answered positively. The overall satisfaction rate of 93.4% was similar between the 2 groups. Two patients were unsatisfied with the surgery (1 in each treatment arm). One of these patients developed a nonunion (screw group) and the other one required a revision due to malunion (plate group). The change in AOFAS and VAS scores was similar in both groups (Table 2).
Table 2.
Postoperative Evaluation. a
| Screws n = 15 | Plate n = 15 | P | |
|---|---|---|---|
| Complications | 3 (20) | 4 (27) | .690 |
| Will do surgery again | 14 (93) | 13 (87) | .543 |
| Satisfaction | .931 | ||
| Unsatisfied | 1 (6.7) | 1 (6.7) | |
| Moderately satisfied | 7 (46.7) | 6 (40) | |
| Satisfied | 7 (46.7) | 8 (53.3) | |
| Change in AOFAS score, mean ± SD | 42.4 ± 8.0 | 44.3 ± 8.2 | .520 |
| Change in VAS score, mean ± SD | 66.0 ± 5.4 | 69.0 ± 6.9 | .195 |
Abbreviations: AOFAS, American Orthopaedic Foot & Ankle Society; VAS, visual analog scale.
Values are n % unless otherwise noted.
Taking into account the cost of each device described previously, we calculated the total cost for each technique. The cost for two 3.5-mm solid crossed compression steel screws is $40. The cost of a construct consisting of a single 2.7-mm solid oblique compression steel screw with a dorsal 2.7-mm T-shaped nonlocking steel plate stabilized with five 2.7-mm solid oblique compression steel screws is $328. Therefore, the use of a dorsal plate is 8 times more expensive than the use of the 2 screws in the other technique. The mean operating time for the crossed screw group was 48 ± 14 minutes vs 58 ± 22 minutes for the plate group (P = .53). The OT cost was $400 per hour. The total cost for the cross screw cohort was $480 ± 40 and for the plate cohort $950 ± 40 (P < .05).
Discussion
The present study compares the functional outcomes of 2 different fixation techniques that differ in their cost. Because comparing the outcomes and costs of all the various types of plates and screws would be burdensome, we focused on the most conventional and commonly used devices in our country.
Our results show that both fixation techniques for the first MTP joint arthrodesis have similar functional results, complication rates, and satisfaction level. Given the already high and rising costs of health care, we should therefore consider using the less expensive technique for the treatment of hallux rigidus with first MTP arthrodesis.
High fusion rates are found regardless of the type of fixation used.1,2,6,12,14,16,25 Our fusion rate was 93%, similar to that in various reports.8,10,22 Therefore, it is difficult to make a recommendation on certain constructs over others based solely on fusion rates. 19 Taking into account the most frequent complications, a review of 2818 feet from 37 studies found a nonunion rate of 5.4%, a malunion rate of 6.1%, and the need for hardware removal in 8.5%. 21
Similarly, in our study, we found a nonunion rate of 7%, a malunion rate of 3.3%, and a need for hardware removal in 7%. The patient satisfaction rate is reported to range from 73% to 100%. 18 We obtained an overall satisfaction rate of 93.4%.
Considering the cost of surgical supplies, one group 26 found that AO screws had the lowest average cost and were the most cost-effective device for the procedure. Other authors 12 compared the cost of crossed-screw constructs with dorsal plating constructs. They found that 2 crossed screws were significantly less expensive than dorsal plating and that, clinically, both systems had similar results. The use of nonlocking semitubular plates and precontoured locking plates for MTP joint arthrodesis have been compared, concluding that precontoured locking plates (which are more expensive) should not be routinely used unless in the presence of inflammatory arthropathy. 17 At our health care system, the cost for 2 cross screws is $40; for a dorsal T plate it is $328. The use of 2 crossed screws is, thus, 88% cheaper.
The plate surgical technique took on average 10 minutes longer than the cross screw technique. Taking into consideration the OT cost ($400/h) and that no surgery exceeded 2 hours, both techniques had the same OT cost, differing only in the implant expenses. It must be said that this is a very simplistic way of accounting for OT costs, which in reality are complex and multivariable in a way that this evaluation does not take into account.
Taking into account our data, the sample size required to show any difference in functional outcome between the 2 techniques is 278 patients per group. The small number of patients in our sample is a limitation of our results. Therefore, it is difficult to make solid comparisons among the variants of surgical techniques for first MTP joint arthrodesis. Future appropriately powered controlled and randomized studies are necessary. 18
Based on our results, we strongly believe that a correct surgical technique and postoperative follow-up is the most important factor to achieve high fusion rates when performing first MTP joint arthrodesis. Using implants 8 times more expensive does not lead to better clinical results.
Conclusions
First MTP joint arthrodesis using either crossed screws or plate fixation results in an improvement in AOFAS and VAS scores. We failed to show a difference in functional outcome between both techniques.
Footnotes
This article was originally published as: Filomeno P, López J. First metatarsophalangeal joint arthrodesis: functional outcomes using 2 different fixation techniques. is more expensive better? Foot Ankle Orthop. 2018 Aug 7;3(3):2473011417752674. doi:10.1177/2473011417752674.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Bennett GL, Sabetta J. First metatarsalphalangeal joint arthrodesis: evaluation of plate and screw fixation. Foot Ankle Int. 2009;30(8):752-757. [DOI] [PubMed] [Google Scholar]
- 2. Brodsky JW, Passmore RN, Pollo FE, Shabat S. Functional outcome of arthrodesis of the first metatarsophalangeal joint using parallel screw fixation. Foot Ankle Int. 2005;26(2):140-146. [DOI] [PubMed] [Google Scholar]
- 3. Calderone DR, Wertheimer SJ. First metatarsophalangeal joint arthrodesis utilizing a mini-Hoffman external fixator. J Foot Ankle Surg. 1993;32(5):517-525. [PubMed] [Google Scholar]
- 4. Coughlin MJ. Arthrodesis of the first metatarsophalangeal joint with mini-fragment plate fixation. Orthopedics. 1990;13(9):1037-1044. [DOI] [PubMed] [Google Scholar]
- 5. Coughlin MJ, Grebing BR, Jones CP. Arthrodesis of the first metatarsophalangeal joint for idiopathic hallux valgus: intermediate results. Foot Ankle Int. 2005;26(10):783-792. [DOI] [PubMed] [Google Scholar]
- 6. Ellington JK, Jones CP, Cohen BE, Davis WH, Nickisch F, Anderson RB. Review of 107 hallux MTP joint arthrodesis using dome-shaped reamers and a stainless-steel dorsal plate. Foot Ankle Int. 2010;31(5):385-390. [DOI] [PubMed] [Google Scholar]
- 7. Fitzgerald JA. A review of long-term results of arthrodesis of the first metatarso-phalangeal joint. J Bone Joint Surg Br. 1969;51(3):488-493. [PubMed] [Google Scholar]
- 8. Flavin R, Stephens MM. Arthrodesis of the first metatarsophalangeal joint using a dorsal titanium contoured plate. Foot Ankle Int. 2004;25(11):783-787. [DOI] [PubMed] [Google Scholar]
- 9. Gimple K, Amspacher JC, Kopta JA. Metatarsophalangeal joint fusion of the great toe. Orthopedics. 1978;1(6):462-467. [DOI] [PubMed] [Google Scholar]
- 10. Goucher NR, Coughlin MJ. Hallux metatarsophalangeal joint arthrodesis using dome-shaped reamers and dorsal plate fixation: a prospective study. Foot Ankle Int. 2006;27(11):869-876. [DOI] [PubMed] [Google Scholar]
- 11. Hunt KJ, Ellington JK, Anderson RB, Cohen BE, Davis WH, Jones CP. Locked versus nonlocked plate fixation for hallux MTP arthrodesis. Foot Ankle Int. 2011;32(7):704-709. [DOI] [PubMed] [Google Scholar]
- 12. Hyer CF, Glover JP, Berlet GC, Lee TH. Cost comparison of crossed screws versus dorsal plate construct for first metatarsophalangeal joint arthrodesis. J Foot Ankle Surg. 2008;47(1):13-18. [DOI] [PubMed] [Google Scholar]
- 13. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15(7):349-353. [DOI] [PubMed] [Google Scholar]
- 14. Kumar S, Pradhan R, Rosenfeld PF. First metatarsophalangeal arthrodesis using a dorsal plate and a compression screw. Foot Ankle Int. 2010;31(9):797-801. [DOI] [PubMed] [Google Scholar]
- 15. Mann RA, Coughlin MJ. The rheumatoid foot: review of literature and method of treatment. Orthop Rev. 1979;8(8):105-112. [Google Scholar]
- 16. Mann RA, Oates JC. Arthrodesis of the first metatarsophalangeal joint. Foot Ankle. 1980;1(3):159-166. [DOI] [PubMed] [Google Scholar]
- 17. Mayer SA, Zelenski NA, DeOrio JK, Easley ME, Nunley JA, 2nd. A comparison of nonlocking semitubular plates and precontoured locking plates for first metatarsophalangeal joint arthrodesis. Foot Ankle Int. 2014;35(5):438-444. [DOI] [PubMed] [Google Scholar]
- 18. McNeil DS, Baumhauer JF, Glazebrook MA. Evidence-based analysis of the efficacy for operative treatment of hallux rigidus. Foot Ankle Int. 2013;34(1):15-32. [DOI] [PubMed] [Google Scholar]
- 19. Moon JL, McGlamry MC. First metatarsophalangeal joint arthrodesis: current fixation options. Clin Podiatr Med Surg. 2011/4;28(2):405-419. [DOI] [PubMed] [Google Scholar]
- 20. Politi J, John H, Njus G, Bennett GL, Kay DB. First metatarsal-phalangeal joint arthrodesis: a biomechanical assessment of stability. Foot Ankle Int. 2003;24(4):332-337. [DOI] [PubMed] [Google Scholar]
- 21. Roukis TS. Nonunion after arthrodesis of the first metatarsal-phalangeal joint: a systematic review. J Foot Ankle Surg. 2011;50(6):710-713. [DOI] [PubMed] [Google Scholar]
- 22. Sharma H, Bhagat S, DeLeeuw J, Denolf F. In vivo comparison of screw versus plate and screw fixation for first metatarsophalangeal arthrodesis: does augmentation of internal compression screw fixation using a semi-tubular plate shorten time to clinical and radiologic fusion of the first metatarsophalangeal joint (MTPJ)? J Foot Ankle Surg. 2008;47(1):2-7. [DOI] [PubMed] [Google Scholar]
- 23. Smith RW, Joanis TL, Maxwell PD. Great toe metatarsophalangeal joint arthrodesis: a user-friendly technique. Foot Ankle. 1992;13(7):367-377. [DOI] [PubMed] [Google Scholar]
- 24. Turan I, Lindgren U. Compression-screw arthrodesis of the first metatarsophalangeal joint of the foot. Clin Orthop Relat Res. 1987;(221):292-295. [PubMed] [Google Scholar]
- 25. Wassink S, van den Oever M. Arthrodesis of the first metatarsophalangeal joint using a single screw: retrospective analysis of 109 feet. J Foot Ankle Surg. 2009;48(6):653-661. [DOI] [PubMed] [Google Scholar]
- 26. Watson AD, Kelikian AS. Cost-effectiveness comparison of three methods of internal fixation for arthrodesis of the first metatarsophalangeal joint. Foot Ankle Int. 1998;19(5):304-310. [DOI] [PubMed] [Google Scholar]
- 27. Wilson JN. Cone arthrodesis of the first metatarso-phalangeal joint. J Bone Joint Surg Br. 1967;49(1):98-101. [PubMed] [Google Scholar]