Commentary: This is a concise and well-written review of metatarsal fracture anatomy, pathophysiology and treatment depending on bone injured and displacement. Special attention was paid to the complex 5th metatarsal fracture types and their individual recommended treatment.
Metatarsal fractures account for a significant proportion of foot injuries, representing 35% of all foot fractures and 5% to 6% of all skeletal injuries, with an estimated incidence of 6.7/10 000 people.5,28,41,42 These injuries are more common in females (2:1) in the general population, although in the athletic population, they are seen most commonly in males.28,37,41,42 Patients in their second through fifth decade of life most commonly sustain metatarsal fractures, with a mean age of 42. 28 Most metatarsal fractures occur by low-energy trauma, although they can also occur from penetrating trauma. 28 Anatomically, the metatarsals fall into 3 groups: first, fifth, and central metatarsals. In a population study investigating metatarsal fractures, fifth metatarsal fractures occurred most commonly, followed by middle metatarsals and the first metatarsal. 28
Although most first and fifth metatarsal fractures are isolated fractures, multiple metatarsal fractures often occur in contiguous bones. If a fracture is identified in a single metatarsal, the orthopedist must closely inspect adjacent metatarsals and joints, especially the Lisfranc articulation. 28 Stress fractures can also occur in metatarsals, most commonly in the second metatarsal but also not uncommonly in the third and fifth metatarsal. They are seen typically in women with osteoporosis and athletes with repetitive stress injuries, which includes groups as diverse as ballet dancers and military recruits. 36
The appropriate and successful management of these fractures requires knowledge of the anatomy, pathophysiology, and treatments for each of the metatarsal fracture groups. Unfortunately, outcomes are generally less predictable in patients with risk factors such as obesity and diabetes. 5 This review focuses on acute metatarsal fractures, with only a cursory discussion of stress fractures and Lisfranc injuries.
First and Central Metatarsals
Fractures involving the first and central (second through fourth) metatarsals can vary significantly, including stress and acute traumatic fractures. First metatarsal fractures are not as common as central metatarsal fractures. 28 There is a 60% rate of contiguous fractures when patients sustain fractures involving the central metatarsals. 28
Anatomy
First Metatarsal
The first metatarsal is larger than the lesser 4 metatarsals. Distally, there is the transmetatarsal ligament in the first webspace. The resting position of the first tarso-metatarsal joint is supported by a capsule containing strong, thick ligaments. The first metatarsal base is the site of attachment for 2 powerful muscles, tibialis anterior and peroneus longus. The first metatarsal head overlies the 2 sesamoid bones, which provides 2 of the 6 contact points of the forefoot and allows the first ray to support up to 40% of the forefoot weight. The blood supply is primarily from a single nutrient artery with secondary epiphyseal and metaphyseal arteries.
Central Metatarsals
The central metatarsals have significant ligamentous structures that link each bone to their adjacent neighbors (Figure 1A). The base of each central metatarsal houses 3 ligaments (dorsal, central, plantar) that stabilize and support each respective metatarsal and the neighboring metatarsal, with the only exception being the lack of a connection between the base of the first and second metatarsal bases. Instead, the Lisfranc ligament spans from the second metatarsal to the medial cuneiform to provide stability. These metatarsals are the main sites of origin of dorsal and plantar interossei, which provide metatarsophalangeal stabilization so that the long flexor and extensor can have effect. However, these muscles can also act as a deforming force on metatarsal fractures. There is a cascade of increased motion through the tarso-metatarsal joints culminating in the fourth and fifth tarso-metatarsal joints. The increase in motion in the sagittal plane in these metatarsals allows for significant adaptability to terrain by the metatarsal heads. The second and third tarso-metatarsal joints are relatively resistant to this sagittal motion, and therefore, stress fractures are more common in the second and third metatarsals than they are in the fourth and fifth metatarsals.
Figure 1.
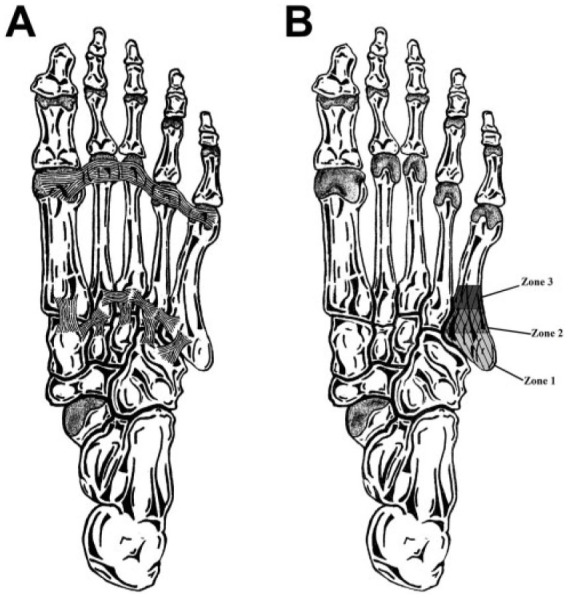
(A) Plantar depiction of the intermetatarsal ligamentous structures that link each bone to their adjacent neighbors. (B) Plantar depiction of the zones of the fifth metatarsal fractures.
Pathophysiology
As in all metatarsal fractures, first and central metatarsal fractures occur with either direct or indirect trauma.21,28 Rarely, crush injuries may cause these fractures and are often associated with soft-tissue and other bony injury.28,31 Stress fractures generally occur with an acute and sustained increase in the intensity of activity and are frequently associated with metabolic or endocrine deficiency.6,13,25 It is paramount with first, second, and third metatarsal fractures to evaluate for intra-articular involvement or concomitant trauma such as Lisfranc injuries. Furthermore, given the relatively limited soft-tissue envelope around the metatarsals, evaluation of possible lacerations or defects communicating with the fracture site is indicated.
Treatment
First Metatarsal
The first metatarsal is important for normal ambulation. Residual shortening or instability of first metatarsal fractures could lead to transfer metatarsalgia and possible lateral metatarsal stress injury. 31 Treatment of first-ray fractures is intended to restore length and alignment to reduce the potential for weight transfer to the lesser metatarsals. As seen on pedographic analyses, shortening or amputation of the first ray leads to alterations in overall weight-bearing (WB) distribution throughout the foot. 1 The high degree of cancellous bone present in the first metatarsal portends a high rate of successful union. 4
Injury location, fracture pattern, degree of displacement, and fracture stability are factors considered when determining treatment. Nondisplaced or minimally displaced first metatarsal fractures can be managed nonoperatively with a variety of foot orthoses to immobilize the surrounding joints and allow protected WB. A variety of immobilization options exist: a short leg plaster splint or fiberglass cast, a postoperative surgical shoe, or a removable fracture boot. Little evidence suggests any superiority between these modalities.3,15,25,37 As pain allows, the choice of immobilization can be transitioned to allow increased mobility. The resumption of physical activity can begin once relatively pain-free range of motion and strength have been achieved. 31
Operative intervention is recommended for fractures that are unstable and displaced. In general, sagittal plane displacement is of prime concern, especially relative dorsiflexion due to the concern for load transfer and subsequent transfer metatarsalgia. Indications for operative intervention include angulation greater than 10°, greater than 3 to 4 mm of displacement, articular involvement, and the presence of a rotational deformity or shortening.5,18,22,35 First metatarsal head and base fractures require restoration of a congruent joint to reduce the risk of posttraumatic arthrosis and subsequent deformities such as hallux valgus or hallux varus.33,44
The choice of operative fixation can vary depending on both fracture location and orientation. Fixation options include percutaneous Kirschner wire (K-wire) placement for diaphyseal fractures amenable to closed reductions or plate osteosynthesis with compression, locking, or bridge plate constructs depending on fracture pattern. 31
Most first metatarsal injuries can be addressed via either a dorsal or medial approach. The dorsal incision is made directly over the shaft of the first metatarsal and extends deep between the extensor hallucis longus and extensor hallucis brevis tendons. A medial approach can be used with an incision along the midaxial aspect of the first metatarsal. 17 With a medial approach, identification and protection of the distal anterior tibialis is necessary. 17 Low-profile implants placed on the tensioned, or plantar aspect, of the first metatarsal are biomechanically advantageous and have a lower risk of tendon irritation. 4 Fixation of intra-articular fractures warrants anatomic reduction with fragment-specific fixation to restore joint congruence and reduce the risk of posttraumatic arthrosis. 21
Authors’ preferred approach
Fractures that are nondisplaced or minimally displaced are treated nonoperatively with the patient non–weight bearing (NWB) in a boot for 4 to 6 weeks (Figure 2), with progressive increases in WB after 6 weeks. The patient is allowed to wean from the boot at 8-10 weeks. Displaced shaft fractures are treated with compression plating for transverse fractures or bridge plating for fractures with any degree of comminution, while articular fractures are treated with fragment specific fixation. Postoperatively, first metatarsal injuries can be NWB in a short leg splint for 2 weeks. The patient is then transitioned to a controlled ankle movement (CAM) boot to maintain NWB for another 4 weeks. WB is allowed in the boot at the 6-week mark, with the patient subsequently weaning out of the boot at the 9-week mark. Rehabilitation can commence at this point to increase mobility and restore baseline gait kinematics.
Figure 2.
Anteroposterior and lateral foot radiographs of a 47-year-old woman who fell and sustained an ankle fracture and first metatarsal fracture, which was treated nonoperatively in a controlled ankle movement boot. Nondisplaced first metatarsal fractures are treated non–weight bearing (NWB) for 4 to 6 weeks in the same fashion that ankle fractures after open reduction and internal fixation are made NWB for 4 to 6 weeks; thus, the weight-bearing status was not affected in this case.
Central Metatarsals
The central metatarsals have increased relative stability as a result of the surrounding soft-tissue attachments such that nondisplaced or minimally displaced fractures are often managed nonoperatively.5,33 Deformity in the sagittal plane can be associated with pain upon loading of the foot, while transverse displacement can result in irritation of the intermetarsal nerve bundles.3,5 Nondisplaced or minimally displaced fractures can be managed with the same WB and immobilization strategies as first metatarsal fractures. 3 There is little evidence to suggest long-term differences in outcomes with the use of rigid or soft splinting of central metatarsal fractures. 43 A randomized study comparing cast immobilization with elastic, compressive support found both cohorts to have achieved radiographic healing at an average of 3 months’ follow-up, with the elastic bandage group reporting higher American Orthopaedic Foot & Ankle Society midfoot scores and less pain over the course of treatment. 43
The principle concern with these central metatarsal fractures is any displacement in the sagittal plane. If the metatarsal head is translated inferiorly by 4 mm or greater, whereby it might focally increase WB stress in a given area, then operative intervention is indicated. By the same token, if the fracture has dorsal displacement of the capital fragment, whereby the risk of transfer metatarsalgia may be increased, then surgery may be indicated. While there is concern about displacement of multiple metatarsal fractures, the inherent stability provided by surrounding soft-tissue structures limits this displacement. This stabilization remains intact even in the presence of multiple concomitant metatarsal fractures as they often displace in unison and maintain their respective anatomic relationships, thus resulting in a decreased risk of subsequent symptoms. 3
Surgical management of central metatarsal fractures involves intramedullary fixation with either antegrade or retrograde K-wires. The approach to fixation depends on the degree of dorsal displacement of the distal metatarsal fracture fragment, although perhaps as much on surgeon preference.3,43 Advantages of K-wire fixation include minimal insult to the surrounding soft tissues, although the ability to obtain sufficient fracture reduction is limited and increases the risk of fixation failure. Another disadvantage of K-wires is the inherent risk of pin site infection. As in many long-bone fractures, the ideal candidate for intramedullary fixation is a transverse, diaphyseal fracture. Open reduction and plate osteosynthesis is an option for fixation; however, the anatomy of the central metatarsals can be a limiting factor. 4 Exposure of central metatarsal fractures involves 1 or 2 parallel longitudinal incisions placed either directly dorsal for isolated fractures or in the intermetatarsal spaces if multiple rays are involved. 17 The close proximity of adjacent metatarsals can limit lag screw placement in certain fracture patterns. Despite this limitation, open reduction and plate fixation avoids the risk of pin site complications and can reduce the risk of metatarsophalangeal stiffness from K-wire placement within adjacent joints. 3
Compared with fifth metatarsal fractures, there is a paucity of data on the outcomes of first and central metatarsal fractures. However, in our experience, these nonoperatively managed fractures have relatively benign outcomes.
Author’s preferred approach
Central metatarsal fractures can often be managed successfully with nonoperative treatment. The authors’ preferred method is similar to that described above for first metatarsal fractures with a period of NWB and then WB in a boot (Figure 3). Operative indications include: significant sagittal displacement, open injuries, and multiple metatarsal fractures. However, most multiple metatarsal fractures are stable, and the authors have successfully treated many of these injuries nonoperatively with a protocol f similar to that used for the treatment of isolated metatarsal fractures. The authors’ preferred method for open reduction and internal fixation (ORIF) is compression or bridge plating with a similar postoperative course to first metatarsal fractures.
Figure 3.
The anteroposterior (AP) and lateral radiographs on the left depict fractures of the second, third, and fourth metatarsals in a 17-year-old boy. These were treated nonoperatively with non–weight bearing in a controlled ankle movement (CAM) boot for 6 weeks. The corresponding radiographs on the right (AP) and bottom (lateral) depict well-healing fractures 4 weeks after immobilization in a CAM boot.
Fifth Metatarsal
Fifth metatarsal fractures are the most common of the metatarsal fractures. The management of these fractures depends on the zone of injury. Zone 1 metatarsal base (avulsion) fractures and distal diaphyseal (dancer’s) fractures have excellent healing potential and are routinely treated nonoperatively. In contrast, zone 2 and 3 metatarsal base fractures have less consistent results with nonoperative treatment. There is a lack of randomized controlled trials investigating treatment options. 39
Fifth metatarsal fractures are broadly divided into 2 groups: proximal base fractures and distal fractures (Figure 1B). For proximal fractures, Dameron 8 was the first to differentiate tuberosity fractures from proximal diaphyseal fractures, noting a clear difference in healing capacity between the two. Proximal fifth metatarsal fractures were subsequently stratified by Torg et al based on healing potential. These were described as either involving the tuberosity or the proximal diaphysis distal to the tuberosity, with the distal group referred to as the Jones type.7,32,40 However, as Torg’s descriptions were more consistent with stress fractures, the more common classification used today is that introduced by Lawrence and Botte. 20 This classification describes zone 1 injuries as being avulsion fractures of the tuberosity, zone 2 fractures involving the metaphyseal-diaphyseal junction (ie, Jones fracture), and zone 3 representing the proximal 1.5 cm of the diaphysis, or proximal diaphyseal stress fractures, often in the setting of a cavovarus foot. 9 Zone 1 injuries account for 93% of proximal fifth metatarsal injuries, zone 2 are 4%, and zone 3 are 3%.5,26 O’Malley and Hamilton 27 described distal diaphyseal fractures in high performance dancers leading to these injuries being colloquially termed dancer’s fractures.
Anatomy
The fifth metatarsal is distinguished from the other lesser metatarsals in that it has tendon insertions at its base, the peroneus brevis inserts dorsally on the proximal tubercle, and the peroneus tertius inserts on the dorsal proximal metadiaphyseal junction. In addition, the plantar fascia also has a strong attachment to the plantar aspect of the tubercle. 11 An os vesalianum, an accessory ossicle of the foot that is rarely symptomatic, may be confused for a fracture (Figure 4).
Figure 4.
Oblique foot radiograph depicting an os vesalianum, often confused for a fracture.
The blood supply to the fifth metatarsal was investigated in a cadaver model, identifying 3 sources, including the nutrient artery, metaphyseal perforators, and periosteal arteries. 38 The nutrient artery enters the medial cortex at the junction of the proximal and middle third of the diaphysis and supplies the shaft. The secondary epiphyseal and metaphyseal arteries supply the base and tuberosity. Between the nutrient artery and the metaphyseal perforators is a watershed area in which poor vascularity may potentially limit fracture healing.
Pathophysiology
Patients presenting with fifth metatarsal fractures usually report acute trauma. 12 The mechanism for zone 1 fractures involves forefoot supination with plantarflexion, resulting in a transverse to slightly oblique fracture primarily from the pull of the lateral band of the plantar fascia. 5 Similarly, zone 2 injuries result from a plantarflexed forefoot with an adduction force applied. 12 Zone 3 injuries typically result from chronic repetitive trauma, often in the setting of a cavovarus foot. The presence of a cavovarus foot has been noted to potentially predispose to both Jones-type fractures and stress fractures of the fifth metatarsal. One study noted that 18/21 acute Jones fractures presented with radiographic hindfoot varus. 34 Since zone 2 and 3 injuries can behave in a similar way clinically, some authors have suggested that it is unnecessary to differentiate them.5,27 Distal diaphyseal fractures generally occur when a person is standing in plantarflexion (ie, on one’s “tip-toes”) and sustains an inversion injury. In dancers, this injury occurs when a ballet dancer is in the demipointe position and falls “over the top” or sustains an inversion injury with the ankle fully plantarflexed.
Treatment
The treatment of the fifth metatarsal fractures depends on the specific injury and various patient factors as well as the goals of the patient. When nonoperative management is selected for zone 1 fractures, the patient will be allowed to bear weight in either a CAM boot or an orthopaedic postoperative shoe. These devices ultimately are for patient comfort and can be discontinued once the patient’s pain subsides to a significant enough degree. Operative management not commonly indicated in these injuries. In contrast, zone 2 and 3 fractures may require surgical management. For the purposes of this discussion of treatment, zone 2 and 3 fractures will be discussed together while zone 1 injuries and distal diaphyseal fractures will be discussed separately.
Zone 1 fractures
In view of their excellent healing potential, nondisplaced zone 1 fractures of the fifth metatarsal may be managed nonoperatively. Good outcomes have been described in these patients, with nonunion rates as low as 0.5% to 1% reported.19,34 Furthermore, the specific nonoperative modality selected appears to matter little, as a meta-analysis of 187 tuberosity fractures in 2011 showed no difference in union and refracture rates when different conservative treatment modalities were compared. 38 As for WB status, patients may bear full weight as tolerated. Early full WB provides better functional outcome and earlier return to work when compared with NWB treatment.14,19
Operative intervention is rarely indicated for zone 1 fractures. The most common indication for operative intervention in this zone is significant displacement (ie, greater than 3 mm). 19 Some have suggested that fractures with more than 2 mm of articular displacement should undergo ORIF, as the risk of secondary displacement approaches 45% and there is some concern for posttraumatic arthritis. 23
Authors’ preferred approach
A conservative approach is almost always warranted in the treatment of these fractures, as the clinical results of nonoperative treatment, even for displaced and comminuted fractures, are quite good. The patient is placed into a CAM walker boot and allowed to bear weight as tolerated. The boot is ultimately for the patient’s comfort, and so the patient is allowed to come out of the boot once his or her pain sufficiently subsides, although many patients will stay in the boot for 4 to 6 weeks.
Zone 2 and 3 fractures
Most of the controversy in the management of fifth metatarsal fractures lies within zone 2. In this zone, nonoperative management may be considered in nondisplaced fractures. The patient should be managed initially in any modality that provides full immobilization and allows NWB, ideally for 6 to 8 weeks. 24 The highly active patient (ie, athlete) may wish to avoid a lengthy period of NWB, and so those patients may prefer operative treatment. One of the first studies to evaluate operative treatment of these injuries assessed 25 patients in a military population that were treated nonoperatively in a short leg NWB cast for 8 weeks. Eighteen fractures healed at mean of 21.2 weeks, while 7 went on to surgery at a mean of 25 weeks, for a nonunion rate of 28%. However, the results of this study may not be generalizable to the population as a whole as the patients in this study were young and healthy with theoretically higher healing capacity Furthermore, those patients who did ultimately heal were limited in their ability to ambulate pain free for over 5 months. 7 Thus, some surgeons are more aggressive with these injuries in young active patients and in athletes.
While there is a lack of consensus on the appropriate treatment for acute nondisplaced zone 2 fractures, there is less debate about the treatment of displaced fractures in this zone, with most of these injuries requiring operative management. When compared with nonoperative management with NWB in a short leg cast, early intramedullary screw fixation and WB within 14 days of injury resulted in a faster clinical union by almost 50%. 24 Multiple studies have also supported the use of early intramedullary screw fixation for this pattern in the active patient population, as results demonstrated a faster return to sport (mean 7.5 weeks) and shorter time to clinical union in competitive athletes.24,29
Percutaneous fixation with an intramedullary screw is the preferred approach for the treatment of zone 2 fractures as it allows for minimal stripping at the fracture site and can achieve adequate compression (Figure 5).10,29 Many authors have assessed what type (cannulated vs noncannulated), size, and length of screw is most appropriate, with screw sizes anywhere from 4.5 mm to 6.5 mm. In general, noncannulated screws are preferred with an attempt to get the largest core diameter screw that can adequately fit the canal. 30 In one study evaluating the fifth metatarsal radiographically, the average straight-length segment of the metatarsal was noted to be 68% of the total length of the metatarsal, as there is often a lateral bend to the metatarsal for which a straight screw cannot account. Moreover, 75% of the 119 patients assessed in their study had an inner coronal diameter of the fifth metatarsal greater than 4.5 mm, suggesting that screws should likely be at least 4.5 mm in most patients. 30
Figure 5.

Anteroposterior and lateral foot radiographs of a 16-year-old high-level soccer player with a zone 2 fifth metatarsal fracture in the setting of a mild to moderate cavovarus foot, which was treated with an intramedullary screw.
Decision making regarding zone 2 fractures, whether nonoperative or operative, must consider the position of the hindfoot. The incidence of hindfoot varus in patients with zone 2 injuries is much higher than in the general population, and this must be identified and corrected concurrently as its presence can predispose to refracture following fracture fixation. 30 There is little guidance in the literature as to when surgical correction of hindfoot varus should be considered. Many surgeons are reticent to perform such a surgery in young, healthy, active people, especially those who may be athletically gifted. In these cases, orthotics (lateral heel wedge with forefoot post and/or cutout underneath the first metatarsal) may be considered.
Fifth metatarsal nonunions or delayed unions typically require surgery to achieve union. Prior to undertaking revision surgery, factors that may have predisposed to nonunion should be evaluated, including mechanical (ie, hindfoot varus) and biologic (eg, hypovitaminosis D) factors. The goals of surgical treatment are to improve stability and the local biology, either with excision of the nonunion and bone grafting or with percutaneous injection of platelet-rich plasma or bone marrow aspirate concentrate.16,26
Authors’ preferred approach
The authors have successfully treated many of these patients nonoperatively with 6 weeks of NWB and then progressive WB in a boot, discontinuing the boot at approximately 9 weeks. The authors consider surgery more seriously in athletes and in patients with an established nonunion or delayed union. A discussion is had with the patient about the risks and benefits of surgery as well as the potential success of nonoperative treatment, with counseling that it will likely be 4 to 6 months before the athlete returns to sport. The advantages of surgery include a potentially decreased risk of nonunion, earlier WB, and earlier return to sport. 26 In patients who elect for surgery, an attempt is made to supplement both the stability and the biology of the fracture. The authors prefer an intramedullary screw and percutaneous injection of a concentrated aspiration of bone marrow in all cases (acute fracture, stress fracture, nonunion).16,26 Postoperatively, the patient is NWB for 4 weeks and then WB as tolerated in a CAM boot for another 2 to 4 weeks, at which time the patient discontinues use of the boot and initiates rehabilitation. For operative cases, the total immobilization time is about the same as in nonoperative cases, with the goal of a shorter time to union in operative cases. In athletes, a specific rehabilitation protocol is made based on the patient’s sport and his or her specific timeline.
The presence of a cavovarus foot is very relevant, and, in the majority of these patients, strong consideration should be given to surgical correction of the cavovarus foot. In young high level athletes (ie, high level high school, college, or professional), the authors are hesitant to correct the cavovarus, as it adds to the surgery and is less predictable in terms of recovery, especially as it relates to high level athletic ability/ achievement. In these patients, an orthotic can be often considered. In the majority of patients with a nonunion or delayed union, the authors are more aggressive in correcting the cavovarus foot.
Distal diaphyseal (dancer’s) fractures
Distal diaphyseal fractures of the fifth metatarsal are treated nonoperatively, with excellent functional outcomes reported in large cohort studies. 2 One study reported a 1.4% rate of failure of nonoperative treatment in these injuries, with only 2 of 141 patients requiring surgery for nonunion. 2 Because of the healing capacity of these injuries, an attempt at nonoperative treatment is made for even displaced fractures, as the fifth ray is very mobile and can accommodate a lot of deformity.
Authors’ preferred approach
These fractures are uniformly treated nonoperatively with high union rates. Patients are allowed to WB as tolerated in a CAM boot as pain allows after the injury. The patient weans out of the boot as tolerated typically by 4 to 6 weeks. Formal rehabilitation is typically not necessary.
Conclusion
Metatarsal fractures are generally broken down into first metatarsal, central metatarsal, and fifth metatarsal fractures. Isolated first metatarsal fractures are somewhat rare; nondisplaced fractures are typically treated nonoperatively, while operative treatment is generally reserved for displaced fractures. Central metatarsal fractures are more common and can often be treated nonoperatively, although severe displacement of an isolated fracture or multiple metatarsal fractures may warrant operative intervention. Fifth metatarsal fractures are most commonly encountered. The treatment is specific to the type of injury, with Jones fractures and proximal diaphyseal fractures most warranting consideration of operative treatment. Metatarsal fractures, as a group, are common injuries that can often be successfully treated nonoperatively, with certain injuries potentially needing more aggressive treatment.
Footnotes
This article was originally published as: Sarpong NO, Swindell HW, Trupia EP, Vosseller JT. Metatarsal fractures. Foot Ankle Orthop. 2018 Aug 10;3(3):2473011418775094. doi:10.1177/2473011418775094.
Author Disclosures: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Ademoglu Y, Ada S, Kaplan I. Should the amputations of the great toe be replanted? Foot and Ankle Int. 2000;21(8):673-679. [DOI] [PubMed] [Google Scholar]
- 2. Aynardi M, Pedowitz DI, Saffel H, Piper C, Raikin SM. Outcome of nonoperative management of displaced oblique spiral fractures of the fifth metatarsal shaft. Foot Ankle Int. 2013;34(12):1619-1623. [DOI] [PubMed] [Google Scholar]
- 3. Browner BD, Jupiter JB, Krettek C, Anderson PA. Skeletal Trauma: Basic Science, Management, and Reconstruction. 5th ed. Philadelphia, PA: Saunders; 2014. [Google Scholar]
- 4. Buddecke DE, Polk MA, Barp EA. Metatarsal fractures. Clin Podiatr Med Surg. 2010;27(4):601-624. [DOI] [PubMed] [Google Scholar]
- 5. Cakir H, Van Vliet-Koppert ST, Van Lieshout EMM, De Vries MR, Van Der Elst M, Schepers T. Demographics and outcome of metatarsal fractures. Arch Orthop Trauma Surg. 2011;131(2):241-245. [DOI] [PubMed] [Google Scholar]
- 6. Chuckpaiwong B, Queen RM, Easley ME, Nunley JA. Distinguishing Jones and proximal diaphyseal fractures of the fifth metatarsal. Clin Orthop Relat Res. 2008;466(8):1966-1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Clapper MF, O’Brien TJ, Lyons PM. Fractures of the fifth metatarsal: analysis of a fracture registry. Clin Orthop Relat Res. 1995;(315):238-241. [PubMed] [Google Scholar]
- 8. Dameron TB. Fractures and anatomical variations of the proximal portion of the fifth metatarsal. J Bone Joint Surg 1975;57(6):788-792. [PubMed] [Google Scholar]
- 9. Dean BJF, Kothari A, Uppal H, Kankate R. The Jones fracture classification, management, outcome, and complications: a systematic review. Foot Ankle Spec. 2012;5(4):256-259. [DOI] [PubMed] [Google Scholar]
- 10. DeSandis B, Murphy C, Rosenbaum A, et al. Multiplanar CT analysis of fifth metatarsal morphology: implications for operative management of zone II fractures. Foot Ankle Int. 2016;37(5):528-536. [DOI] [PubMed] [Google Scholar]
- 11. DeVries JG, Taefi E, Bussewitz BW, Hyer CF, Lee TH. The fifth metatarsal base: anatomic evaluation regarding fracture mechanism and treatment algorithms. J Foot Ankle Surg. 2015;54(1):94-98. [DOI] [PubMed] [Google Scholar]
- 12. Egol K, Walsh M, Rosenblatt K, Capla E, Koval KJ. Avulsion fractures of the fifth metatarsal base: a prospective outcome study. Foot Ankle Int. 2007;28(5):581-583. [DOI] [PubMed] [Google Scholar]
- 13. Geyer M, Sander-Beuermann A, Wegner U, Wirth CJ. Stress reactions and stress fractures in the high performance athlete: causes, diagnosis and therapy [in German]. Unfallchirurg. 1993;96(2):66-74. [PubMed] [Google Scholar]
- 14. Gray AC, Rooney BP, Ingram R. A prospective comparison of two treatment options for tuberosity fractures of the proximal fifth metatarsal. Foot (Edinb). 2008;18(3):156-158. [DOI] [PubMed] [Google Scholar]
- 15. Hansis M, Meeder PJ, Weller S. Treatment tactics in fractures of the midfoot [in German]. Aktuelle Traumatol. 1986;16(5):190-195. [PubMed] [Google Scholar]
- 16. Harford JS, Dekker TJ, Adams SB. Bone marrow aspirate concentrate for bone healing in foot and ankle surgery. Foot Ankle Clin. 2016;21(4):839-845. [DOI] [PubMed] [Google Scholar]
- 17. Hoppenfeld S, de Boer P, Buckley R. Surgical Exposures in Orthopaedics: The Anatomical Approach. 5th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2016. [Google Scholar]
- 18. Johnson V. Foot Science. Philadelphia, PA: WB Saunders; 1976. [Google Scholar]
- 19. Konkel KF, Menger AG, Retzlaff SA. Nonoperative treatment of fifth metatarsal fractures in an orthopaedic suburban private multispeciality practice. Foot Ankle Int. 2005;26(9):704-707. [DOI] [PubMed] [Google Scholar]
- 20. Lawrence SJ, Botte MJ. Jones’ fractures and related fractures of the proximal fifth metatarsal. Foot Ankle. 1993;14(6):358-365. [DOI] [PubMed] [Google Scholar]
- 21. Lee DK, Mulder GD, Schwartz AK. Hallux, sesamoid, and first metatarsal injuries. Clin Podiatr Med Surg. 2011;28(1):43-56. [DOI] [PubMed] [Google Scholar]
- 22. Lee EW, Donatto KC. Fractures of the midfoot and forefoot. Curr Opin Orthop. 1999;10(3):224-230. [Google Scholar]
- 23. Mehlhorn AT, Zwingmann J, Hirschmüller A, Südkamp NP, Schmal H. Radiographic classification for fractures of the fifth metatarsal base. Skeletal Radiol. 2014;43(4):467-474. [DOI] [PubMed] [Google Scholar]
- 24. Mologne TS, Lundeen JM, Clapper MF, O’Brien TJ. Early screw fixation versus casting in the treatment of acute Jones fractures. Am J Sports Med. 2005;33(7):970-975. [DOI] [PubMed] [Google Scholar]
- 25. Morrisey EJ. Metatarsal fractures. J Bone Joint Surg Am. 1946;28:594-602. [PubMed] [Google Scholar]
- 26. O’Malley M, DeSandis B, Allen A, Levitsky M, O’Malley Q, Williams R. Operative treatment of fifth metatarsal jones fractures (zone II and III) in the NBA. Foot Ankle Int. 2016;37(5):488-500 [DOI] [PubMed] [Google Scholar]
- 27. O’Malley MJ, Hamilton WG, Munyak J. Fractures of the distal shaft of the fifth metatarsal. Am J Sports Med. 1996;24(2):240-243. [DOI] [PubMed] [Google Scholar]
- 28. Petrisor BA, Ekrol I, Court-Brown C. The epidemiology of metatarsal fractures. Foot Ankle Int. 2006;27(3):172-174. [DOI] [PubMed] [Google Scholar]
- 29. Porter DA, Duncan M, Meyer SJF. Fifth metatarsal Jones fracture fixation with a 4.5-mm cannulated stainless steel screw in the competitive and recreational athlete: a clinical and radiographic evaluation. Am J Sports Med. 2005;33(5):726-733. [DOI] [PubMed] [Google Scholar]
- 30. Raikin SM, Slenker N, Ratigan B. The association of a varus hindfoot and fracture of the fifth metatarsal metaphyseal-diaphyseal junction: the Jones fracture. Am J Sports Med. 2008;36(7):1367-1372. [DOI] [PubMed] [Google Scholar]
- 31. Rammelt S, Heineck J, Zwipp H. Metatarsal fractures. Injury. 2004;35(2):77-86. [DOI] [PubMed] [Google Scholar]
- 32. Roche AJ, Calder JDF. Treatment and return to sport following a Jones fracture of the fifth metatarsal: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2013;21(6):1307-1315. [DOI] [PubMed] [Google Scholar]
- 33. Schenck H. Fractures and dislocations of the forefoot: operative and nonoperative treatment. J Am Acad Orthop Surg. 1995;3(2):70-78. [DOI] [PubMed] [Google Scholar]
- 34. Shahid MK, Punwar S, Boulind C, Bannister G. Aircast walking boot and below-knee walking cast for avulsion fractures of the base of the fifth metatarsal: a comparative cohort study. Foot Ankle Int. 2013;34(1):75-79. [DOI] [PubMed] [Google Scholar]
- 35. Shereff MJ. Fractures of the forefoot. Instr Course Lect. 1990;39:133-140. [PubMed] [Google Scholar]
- 36. Shindle MK, Endo Y, Warren RF, et al. Stress fractures about the tibia, foot, and ankle. J Am Acad Orthop Surg. 2012;20(3):167-176. [DOI] [PubMed] [Google Scholar]
- 37. Shuen WMV, Boulton C, Batt ME, Moran C. Metatarsal fractures and sports. Surgeon. 2009;7(2):86-88. [DOI] [PubMed] [Google Scholar]
- 38. Smith JW, Arnoczky SP, Hersh A. The intraosseous blood supply of the fifth metatarsal: implications for proximal fracture healing. Foot Ankle. 1992;13(3):143-152. [DOI] [PubMed] [Google Scholar]
- 39. Smith TO, Clark A, Hing CB. Interventions for treating proximal fifth metatarsal fractures in adults: a meta-analysis of the current evidence-base. Foot Ankle Surg. 2011;17(4):300-307. [DOI] [PubMed] [Google Scholar]
- 40. Torg JS, Balduini FC, Zelko RR, Pavlov H, Peff TC, Das M. Fractures of the base of the fifth metatarsal distal to the tuberosity: classification and guidelines for non-surgical and surgical management. J Bone Joint Surg Am. 1984;66(2):209-214. [PubMed] [Google Scholar]
- 41. Urteaga AJ, Lynch M. Fractures of the central metatarsals. Clin Podiatr Med Surg. 1995;12(4):759-772. [PubMed] [Google Scholar]
- 42. Vuori JP, Aro HT. Lisfranc joint injuries: trauma mechanisms and associated injuries. J Trauma. 1993;35(1):40-45. [DOI] [PubMed] [Google Scholar]
- 43. Zenios M, Kim WY, Sampath J, Muddu BN. Functional treatment of acute metatarsal fractures: a prospective randomised comparison of management in a cast versus elasticated support bandage. Injury. 2005;36(7):832-835. [DOI] [PubMed] [Google Scholar]
- 44. Zwipp H, Rammelt S. Posttraumatic deformity correction at the foot [in German]. Zentralbl Chir. 2003;128(3):218-226. [DOI] [PubMed] [Google Scholar]





