Abstract
Nonsurgical management is almost always considered the first-line treatment for the vast majority of foot and ankle pathologies. Foot orthoses, shoe modifications, and therapeutic footwear are considered essential tools for successful conservative management of different foot and ankle disorders. Orthopedic foot and ankle surgeons should have a meticulous understanding of the lower extremity biomechanics as well as the pathoanatomy and the sequelae of diseases affecting the foot and/or ankle. This is essential to the understanding of the desired effects of the different inserts, orthotics, shoe modifications, or braces that may be prescribed for these conditions. In this article, we will summarize the orthoses used for treatment of the most commonly encountered foot and ankle pathologies, with the exclusion of treatment for the diabetic foot because of the unique requirements of that disease process.
Keywords: braces, orthotics, conservative management
Commentary: This report is a review of orthotic treatment of foot and ankle disorders. The fundamental biomechanical abnormalities of common problems are reviewed. The biomechanical basis of brace or orthotic treatments to share load, absorb shock, return energy and reduce areas of high strain are described.
Introduction
Different foot inserts, orthoses, braces, and shoe modifications can be powerful tools for the conservative management of a variety of foot and ankle pathologies that compromise joint function, motor function, sensation/proprioception, and skin integrity and predispose to deformities. Examples include congenital disorders (eg, planovalgus, tarsal coalition), sports-related or overuse disorders (eg, plantar fasciitis, posterior tibial tendinitis), and systemic disorders with foot and ankle involvement (eg, diabetes, rheumatoid arthritis).24,67,69
The goals of treatment using orthotics and footwear modifications are to attempt restoration of normal function as well as to try to prevent further progression of the disease process affecting the foot and/or ankle. This can be achieved by designing orthotics to offload high-pressure areas, minimize shear forces, cushion sites of tenderness, correct flexible deformities, or provide foot control and support. Footwear modifications and braces are particularly beneficial to restrict painful motion, compensate for lost motion, accommodate deformity, provide support, and subsequently improve gait and ambulation. However, these orthotics and footwear modifications are not intended to either permanently prevent or correct the development of structural deformities.24,61,67,69
Biomechanical and Clinical Rationale
A foot orthosis is an externally applied apparatus that can be inserted in a shoe to help support or improve the function of the foot and/or ankle. The goal is either to reduce pressure across a specific region of the foot or ankle by offloading this area, or to accommodate deformities resulting from a disease process. The target effect of the orthotic can be achieved by applying controlled force on the foot to achieve either pressure transfer and redistribution, or motion restriction. The ultimate goal is maintaining neutral or near neutral subtalar joint alignment through the gait cycle.21,24,44,67,70
In general, foot orthoses are readily available in 2 forms, prefabricated off-the-shelf orthoses and custom-molded orthoses manufactured from a model of the patient’s foot. The potential advantages of using a prefabricated orthotic are immediate availability, lower cost, and time conservation for the patient as well as the health care provider. Additionally, in many cases insurance companies do not pay for many of these custom braces or orthotics, which can make starting with off-the-shelf products a good first step; this needs to be explained and discussed with the patient. On the other hand, custom orthoses have the advantages of more intimate fit and the ability to be modified to individual differences if needed; hence custom orthoses are particularly essential for patients with a significant deformity, as well as patients with neuropathic arthropathy with loss of protective sensation who are predisposed to joint collapse, skin breakdown, and ulceration.11,24,67
There are 8 potential objectives of using a foot orthosis24,25:
Shock attenuation and absorption
Provide cushion to tender areas of foot
Relieve areas of abnormal increased plantar pressure (pressure dissipation across the plantar surface)
Provide support, and protection of a healed fracture site total-contact concept
Minimize shear forces
Attempt correction of flexible deformities, or to provide support and stability
Restrict motion of painful joints
Try to accommodate rigid deformities
Custom orthoses can be broadly classified into 3 main forms: accommodative (soft), rigid, and semirigid.
Accommodative (Soft) Foot Orthoses
Soft orthoses are primarily designed to provide cushioning and protection. They offer padding, shock attenuation, and reduction of friction shear forces. They are made of softer and less durable materials, and hence the need for periodic follow-up for possible repairs. The uses of soft orthoses include insensate foot and fixed deformities (especially with bony prominences).24,42,67
Rigid Foot Orthoses
Rigid orthoses are designed to provide excellent arch support and control for flexible deformities, and are often durable. They are used to control or decrease motion, such as in arthritis of the forefoot or midfoot. On the other hand, they offer only minimal cushion, shock absorption, and protection, and hence these orthoses are not suitable for use in neuropathic patients. Although rigid orthoses can be easily fit into fashionable shoes, they are not easily adjustable, and don’t mold or conform to plantar foot prominences, and thus they are not suitable for use in patients with prominent plantar exostoses or plantar fat pad cushion atrophy.24,26,42,67
Semirigid Orthoses
Semirigid orthoses are the most frequently used orthoses. They combine the advantages of accommodative orthoses (cushioning, shock absorption, and protection) with those of rigid orthoses (weight redistribution, and support and control for flexible deformities). 24
This type of orthosis is manufactured with a soft, less-dense upper layer for cushioning, and a more firm core (base) layer for support. The semirigid orthosis is commonly used to offload areas subjected to abnormal high pressure by dissipating and evenly redistributing plantar pressure. This is particularly helpful in neuropathic patients, where the plantar aspect of the heel and forefoot are the areas subjected to the highest pressure.24,25,67
These orthoses are easily adjustable, and can be modified to accommodate minor foot changes. They have greater longevity compared to accommodative orthoses, but they still require follow-up and periodic replacement.24,67
Off-the-Shelf Orthoses
These orthoses can be used in patients with no deformity, neuropathy, or ulcers to provide cushioning and shock attenuation. An example would be the longitudinal metatarsal pad that can be added on a cushioned insert to relieve plantar pain in patients with Morton neuroma or metatarsalgia. Another example is the visco heel pads that are commonly used to treat plantar heel pain. It is important to educate patients on the appropriate way to use and place those off-the-shelf orthoses inside shoes.24,41,67
The keys to successful orthotic prescriptions and to provide patients with the best possible orthoses are a thorough understanding of the lower extremity biomechanics, the identification of areas of high pressure, the use of proper molding technique, as well as proper selection of the manufacturing material to achieve the desired function of the orthosis.
University of California Biomechanics Laboratory Foot Orthoses
The University of California Biomechanics Laboratory (UCBL) (Figure 1) orthosis is designed to control postural flexible deformities by controlling and maintaining the hindfoot in neutral position—hence the importance of maintaining the heel in neutral or near neutral alignment while the orthosis is being molded on the patient’s foot. The biomechanical concept of the UCBL is to stiffen and lock the transverse tarsal joints by keeping the calcaneus in a neutral position and thus limit pronation and forefoot abduction. With excessive valgus, a medial post to the heel and forefoot can be added.8,67
Figure 1.
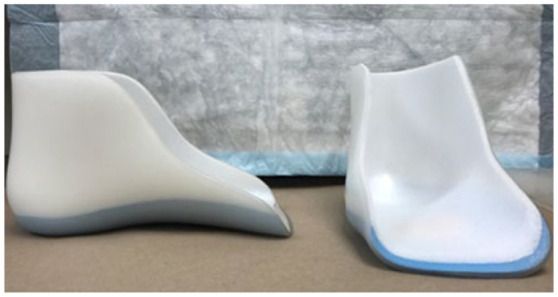
The University of California Biomechanics Laboratory (UCBL) Foot Orthoses with a supramalleolar extension.
Additionally, UCBL orthoses can be used in fixed deformities such as midfoot arthritis to reduce motion and pain. With fixed deformities, particular attention should be paid to any bony prominence, which would require a relief over the prominence and use of a material for padding and pressure absorption in the relief area.18,67
Ankle-Foot Orthoses
There are 2 basic forms of ankle-foot orthoses (AFOs): the double-upright construction attached to the shoe and the molded ankle-foot orthosis (MAFO) (Figure 2). Depending on the pathology, the AFO can be fixed or articulated to permit ankle range of motion. Different adjustments of the AFO orthoses can be made for improved deformity control, and to extend the indications of their use to include flexible as well as rigid deformities.49,55,67
Figure 2.

The molded ankle-foot orthosis (MAFO).
The most commonly used forms of MAFO are the posterior shell that fits inside the shoes, and the Arizona brace (leather lacer) that is described later in more detail. The design of the MAFO is dictated by the pathology being treated and the desired effect of the brace. If the goal is to limit ankle range of motion, the trim lines should extend anteriorly to the level of the midline of the malleoli. However, if intended to only control subtalar or midtarsal motion while maintaining some ankle motion, the trim line should end posterior to the malleoli. For midfoot arthritis, a full-length foot plate should be used to reduce pain during walking.49,55,67
Dynamic Ankle-Foot Orthoses
The dynamic AFO (Figure 3) was originally developed in 1985 to help with gait control and improvement in pediatric patients with neuromuscular disorders. This brace provides proprioceptive feedback from the ground through the dynamic footplate, and may even help strengthen calf muscles. The goal is to provide support, and at the same time allow some normal range of motion. These orthoses are manufactured of carbon graphite. The dynamic AFO can assist ankle dorsiflexion by means of a flex built into the substance of the AFO, and hence can be used to treat patients with drop foot deformity.2,22,52,68
Figure 3.
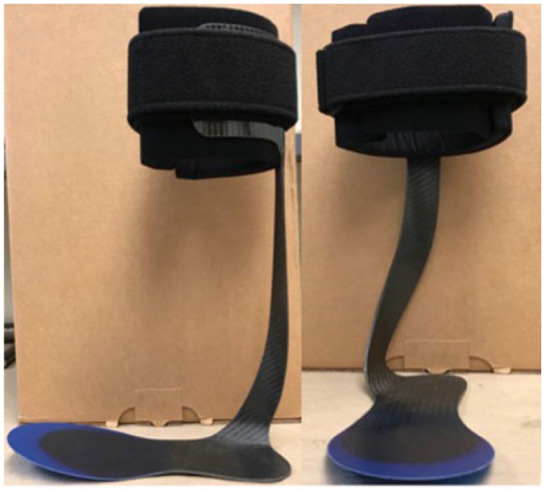
The dynamic ankle-foot orthosis.
Hinged AFO
The hinged AFO can be used in patients with foot drop, where it can provide dorsiflexion assistance dictated by the type of hinge (articulation) used. This type of brace is also known as Dorsiflexion Assist Functional AFO (Figure 4). The medial and lateral hinge joints closely align with the anatomic ankle joint, and the trim lines encompass the sides of the leg as well as the back, thus providing the desired support for those patients featuring foot drop. With more severe foot drop deformity, a Plantar Flexion Stop AFO can be used. When used for severe drop foot deformity, the articulation would permit dorsiflexion while blocking plantarflexion.34,64
Figure 4.

The dorsiflexion assist ankle-foot orthosis.
Source: Picture provided by Dr Douglas Richie.
The Arizona Brace AFO
The Arizona Brace (Ernesto Castro, Custom Footwear Inc, Mesa, AZ) was designed for the conservative management of posterior tibial tendon dysfunction (PTTD) but can also be used to treat other hindfoot conditions. The goal is to maintain the hindfoot in a neutral or near neutral alignment by correcting the acquired hindfoot valgus position as a result of the PTTD. The brace fits into a comfort shoe and stabilizes the ankle, subtalar, and midtarsal joints. The brace provides medial and lateral hindfoot stability and minimizes subfibular impingement that results from the hindfoot valgus.4,67
There are 2 basic forms of the Arizona brace: the lace and the hook-and-loop (Figure 5). The brace provides hindfoot stability by using the concept of 3-point fixation; hence, it is biomechanically similar to a well-molded short leg cast. The main advantage over a standard MAFO is its reduced height, which is generally better accepted by patients.4,67 The possible disadvantages of the Arizona brace are its relative bulkiness and difficulty fitting inside shoes; hence, it cannot be tolerated by some patients. The excellent stability of this brace also allows its use for the nonoperative management of peroneal tendinosis, and ankle and hind-foot arthritis. 67
Figure 5.

The Arizona brace.
Specific Foot and Ankle Disorders
Plantar Fasciitis
Night splints
Night splints are frequently used for the conservative management of plantar fasciitis.6,53,66 Night splints (Figure 6) keep the ankle in a dorsiflexed position and subsequently help to prevent contraction of the plantar fascia during periods of inactivity. This is particularly helpful with the classic start-up heel pain, frequently experienced by patients with the first few steps in the morning. The problems commonly encountered with the use of night splints are patients’ noncompliance, cost, and potential negative impact on sleeping habits.6,53,66,67 The use of night splints has been shown to be an effective tool in the nonoperative management of plantar fasciitis, usually in combination with other treatment modalities.48,66
Figure 6.

Plantar fascia night splint.
In one study, night splints (combined with anti-inflammatory medications, viscoelastic heel pads, and a stretching program for the gastrocnemius and soleus muscles) were 89% effective in curing plantar fasciitis. 6
Orthotics
Orthotics are commonly used as a part of multifaceted regimen for treating plantar fasciitis. The goals of using orthotics in plantar fasciitis are to provide medial arch support, and increase the midfoot contact area. This results in greater force redistribution, pressure reduction under the heel, and subsequently reduced strain on the plantar fascia with weight bearing.53,67
Different types of orthotics are available for plantar fasciitis. Some orthotics are intended to reduce pressure at heel strike by using a soft hindfoot insole. 53 Others rely on providing medial arch support, and hindfoot stability to offload the plantar fascia throughout the gait cylce.9,10,58
The types of orthotics frequently used include simple viscoelastic heel pads (Figure 7) without 3-dimensional structure, and the multilayered 3-dimensional orthotics (plantar fascia support insoles) (Figure 8). 65 The use of prefabricated insole has been shown to be equally successful as custom-made inserts.5,33 However, patients with concomitant plantar fasciitis and structural malalignment such as pes planovalgus or pes cavus would require the use of custom-molded orthoses. Additionally, prefabricated insoles represent a more economical alternative.5,33,67
Figure 7.

Viscoelastic heel pads.
Figure 8.

Plantar fascia support insole.
The most important design concept for reducing plantar pressure during ambulation is a conforming profile insert. The insert should closely conform to the shape of the arch of the foot, to reduce flattening and elongation of the foot, and subsequently reduce the strain on the diseased plantar fascia with walking. Conforming insoles should be made from a stiffer material to prevent bottoming out.14,29,67 The use of orthotics was found to be 89% effective in alleviating pain from plantar fasciitis. 53
Tendon Disorders
Orthotics and braces can be a powerful tool for the management of acute and chronic tendon disorders.
Posterior Tibial Tendon Dysfunction
The goals of orthotic management of posterior tibial tendon dysfunction (PTTD) are to attempt restoring the medial arch and to eliminate pronation, which should subsequently reduce the strain across the pathologic tendon. The main factor in determining the type of the brace to be used is whether the deformity is rigid or flexible. This will also dictate the primary function expected from the brace, whether it is corrective or accommodative.17,67
With a flexible deformity (stage II), the brace is aimed at attempting to correct the deformity. Subsequently, the heel must be molded into a subtalar neutral position. On the other hand, with more advanced PTTD with a rigid uncorrectable deformity (stage III), the brace is molded in situ aiming at providing comfort, decreasing pain, and preventing the foot from collapsing into worsening alignment.17,67
Stage I
In the acute stage, immobilization in a short leg cast or a walking boot is often used. After resolution of the acute symptoms, a semirigid orthosis with medial posting is often successful. 23
Stage II
At this stage, while the deformity remains flexible, a UCBL orthosis, a custom articulated AFO, or an over-the-counter ankle-stirrup brace are valid options. The UCBL targets restoration of the medial arch of the foot by maintaining the hindfoot in neutral alignment, and limiting forefoot abduction. This is achieved by building up the lateral border of the foot.3,4,8,45 The use of UCBL orthosis has been shown to be 77% successful for the conservative management of stage II PTTD. 8
The Richie Brace (Figure 9) is an alternative option in stage II PPTD. This brace has a lower profile compared to other custom ankle-foot orthoses. It is designed with open leg front and back for comfort. The brace features a custom well-contoured and balanced footplate, articulated to adjustable semirigid leg uprights, to help control and limit the excessive pronation forces with PTTD. 51 Custom ankle-foot orthoses have been shown to be 67% effective for nonoperative management of stage II PTTD. 8
Figure 9.

The Richie brace.
Source: Picture provided by Dr Douglas Richie.
The Arizona brace, described earlier, represents another powerful tool in conservative management of PTTD. In addition to relieving symptoms, it may allow healing of the tendon and restoration of function when combined with a graduated program of rehabilitation. The use of Arizona brace was reported to be 90% effective in conservative management of stage I, II, and III PTTD. 4
Stage III
Because of the rigid deformity in stage III, the use of braces is not aimed at correction, but rather to accommodate the deformity. A fixed deformity necessitates the use of a more supportive brace. The most commonly used braces are the Arizona brace and the MAFO. The brace cannot reestablish the arch in a fixed deformity, or restore normal kinematics as it holds the foot rigid. The goals are to provide support for the collapsed arch, reduce pain, and subsequently improve function.17,67
Stage IV
In this stage, a rigid deformity with concomitant deltoid failure and ankle arthritis would dictate the use of a nonarticulated brace, such as the solid AFO. An important concept in patients with severe valgus deformities is to avoid attempting to correct the deformity by molding the AFO. This leads to pressure across the hind foot, lateral malleolus, and fifth ray with subsequent pain and possible skin breakdown or ulceration over any bony prominences. 30
Achilles Tendinopathy (Insertional/Noninsertional)
The etiology of Achilles tendinopathy is multifactorial, and the management usually involves a multimodal approach. Nonoperative management is almost always recommended as initial treatment for Achilles tendinopathy, whether insertional or noninsertional. 1
Generally, for insertional Achilles tendinopathy, the concept is to use a heel lift, and open-back shoes and/or Achilles sleeve to avoid rubbing of the tendon against the shoe and subsequent irritation. On the other hand, for noninsertional Achilles tendinopathy, immobilization in the acute phase usually with a CAM (controlled ankle movement) boot can help quiet the acute inflammatory process and reduce the pain.1,36,54,67
Foot orthoses can be helpful in patients with abnormal foot pronation contributing to the pathogenesis of Achilles tendinopathy. The goal is to attempt correcting the excessive foot pronation, and the resultant calcaneal eversion, and subsequently reduce the strain within the pathologic Achilles tendon.12,32,36,40,56 However, the effectiveness of foot orthoses in Achilles tendinopathy is not well documented in literature.
For chronic dysfunction of the Achilles tendon, a custom-molded AFO, or Arizona brace, is commonly used to control the symptoms. 67 Another option is the AirHeel brace (Donjoy Orthopedics, Vista, CA) (Figure 10). The concept of this brace is to improve the Achilles tendon circulation by delivering pulsating compression to the Achilles region by means of 2 interconnected air cells above and below the calcaneus. The AirHeel brace has been shown to be as effective (91% at 1-year follow-up) as eccentric training in the treatment of chronic Achilles tendinopathy. 47
Figure 10.

The AirHeel brace.
Source: Picture provided by DJO Global, Vista, CA.
Other frequently used tools for Achilles tendinopathy include heel lifts, night splints, and shoe modifications. The use of heel lifts made of shock-absorbing materials can raise the heel away from the back of the shoe, and reduce rubbing and strain on the tendon. It is worth mentioning that the lift should be used bilaterally to avoid creating additional functional problems, as a result of limb-length discrepancy that would occur with unilateral use of heel lift. 21
Ankle joint dorsiflexion night splints represent another option in patients with Achilles tendinopathy. They are often used at night or during periods of inactivity. The goal is to antagonize the natural ankle joint gravity-assisted equinus by maintaining the ankle in a dorsiflexed position, thus preventing additional contracture and reducing the strain within the Achilles tendon over time. 54 The use of night splints alone has not been shown to be effective for Achilles tendinopathy, with greater reduction of pain seen when the night splint was combined with a 12-week eccentric exercise program. 54
Shoe-wear modification can be another useful tool; using shoes that are softer in the back of the heel, with increased heel height and a forefoot rocker can help reduce the irritation of the diseased tendon. Similarly, a silicone Achilles sleeve can help reduce the irritation of the tendon from rubbing against the back of a shoe. 54
Cavus Foot
Orthotics are a useful adjunct in the nonoperative management of cavus foot deformity. Thorough understanding of the deformity and the resultant pressure areas is imperative to select the proper orthotic or brace. With cavus deformity, there is tripod weight bearing, resulting in high contact zones underneath the first and fifth metatarsal heads (metatarsalgia) as well as the heel. The high arch and the lack of flexibility predispose to plantar fasciitis and contribute to high impact on the heel. Furthermore, the varus hindfoot creates excessive stress on the lateral ankle ligaments with subsequent lateral ankle instability and frequent ankle sprains.15,38
The Coleman ‘block test’ can help inform the type of orthotic for cavus deformity. If the hindfoot is supple, the cavus is secondary to a plantarflexed first ray (forefoot driven). Subsequently, the hindfoot will correct with accommodation of the plantarflexed first ray. This can be achieved with an orthotic with a first ray recess (cut-out), a metatarsal bar, and possibly a lateral forefoot post.15,35,38,66 A commonly used OTC reverse orthotic is the Arch Rival (Donjoy Orthopedics, Vista, CA) (Figure 11). The use of reverse orthotics has been shown to be 92% effective for the conservative management of forefoot-driven cavus. 35
Figure 11.

The Arch Rival.
Source: Picture provided by DJO Global, Vista, CA.
In case of a hindfoot-driven cavus, the typical custom orthotic would be a semirigid full-length orthotic with an elevated heel to accommodate gastrocnemius tightness, a lateral hindfoot to midfoot heel wedge (Figure 12), either a lateral forefoot post or first-ray recess, and no medial arch support. With more fixed cavus deformity, patients are usually treated with AFO such as the Arizona brace; however, patients are less likely to tolerate and benefit from orthoses. In neurologic-driven cavus patients with severe muscle weakness and foot drop (Charcot-Marie-Tooth disease), a dorsiflexion assist hinged AFO can be used.15,35,38,67
Figure 12.
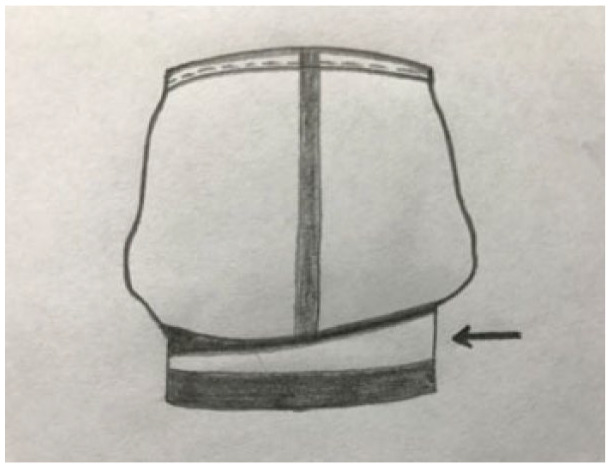
A diagram illustrating the back of a right shoe with a lateral heel wedge (arrow).
Interdigital (Morton) Neuroma
Morton neuromas or interdigital neuroma can be successfully treated with metatarsal pads (Figure 13), custom orthotics, and shoe-wear modification. The rationale of the metatarsal pad is to splay the metatarsals, relieve the metatarsal head pressure, and thus reduce pressure on the affected neuroma. To achieve the desired effect, the pad must be the proper size, as well as appropriately positioned underneath the foot proximal to the level of the lesion; another option is to use an insole with the metatarsal pad built in. The patient must be informed that the goal is not to pad under the lesion, but to redistribute the pressure away from the lesion. A wider and low-heeled shoe with a large toe box can help prevent compression of the metatarsal heads.28,60,67 Shoe modifications are almost always the first line treatment for Morton neuromas, with a reported success rate of 63%. Shoe modifications (metatarsal pad, shoes with wide toe boxes, and low heels) with steroid injections has been shown to give better results (85%) at 6 months in Morton neuromas than shoe modifications alone (63%). 57
Figure 13.
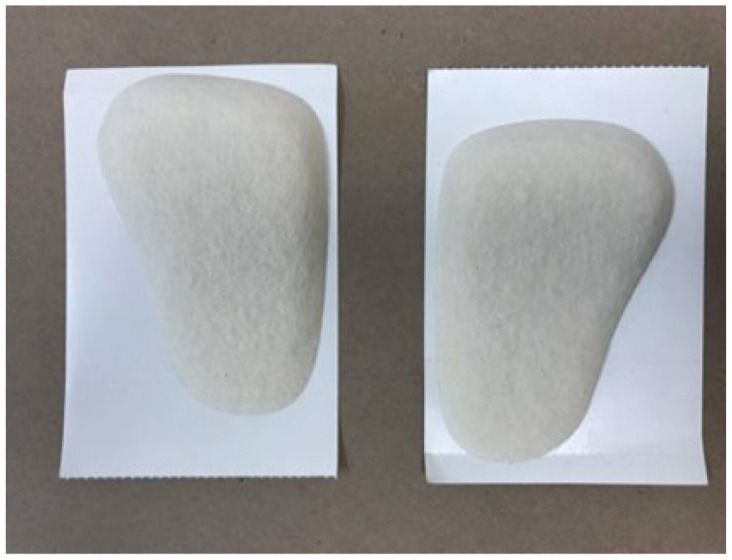
Metatarsal pad.
Arthritis of the Foot and Ankle
Arthritis of the foot and ankle can be a source of considerable pain, dysfunction, and subsequent disability with weight bearing. The goal of orthotics use in arthritic conditions of the foot and ankle is to limit pain, improve function, and to attempt delaying or prevention of operative intervention. The patients should be educated that the use of orthotics is not intended to correct the underlying degenerative joint disease. Orthoses have been shown to result in greater pain relief in comparison to the sole use of nonsteroidal anti-inflammatory drugs for the conservative management of foot and ankle arthritis. 63 The basic principles of conservative treatment of foot and ankle arthritis revolve around limiting motion at the affected joint while preserving function and gait.
Ankle Arthritis
Ankle arthritis pain occurs secondary to sagittal plane motion at the tibiotalar joint. Conservative treatment of ankle arthritis should focus on limiting the amount of dorsiflexion and plantarflexion of the ankle while maintaining effective gait biomechanics. An MAFO can be effective when the prosthesis is fixed at the ankle and the trim lines extend anterior to the malleoli.63,67 An Arizona brace is another orthosis, which is commonly effective in stabilizing sagittal hindfoot motion as previously described. The Arizona brace may also allow for an improved fit within a shoe, which can improve patient compliance. Both the molded AFO and Arizona brace reduce ankle joint loading at the cost of motion in the sagittal plane. There is currently lack of clinical trials evaluating and comparing the effectiveness of different brace designs for the conservative management of ankle arthritis, with only a biomechanical study showing that a rigid hindfoot orthosis offers selective restriction of ankle-hindfoot motion while permitting sufficient forefoot motion in comparison with the MAFO. 19
These braces can be combined with a rocker-bottom–soled shoe to balance the motion lost at the ankle and allow for effective forward propulsion. 24 Furthermore, a solid ankle cushion heel (SACH) orthosis (Figure 14) has been shown to help with reducing ankle joint motion, while allowing for a smoother transition from heel strike to toe off during the gait cycle.39,71 The concept of a rocker-bottom–soled shoe with a cushioned heel is to decrease impact at heel strike, and thus transferring sagittal plane motion from the ankle joint to the bottom of the shoe.
Figure 14.

SACH (solid ankle cushion heel).
Subtalar Arthritis
Arthritis of the subtalar joint generates pain with both axial loading during heel strike and osteophyte impingement during inversion and eversion. 17 This motion can be especially painful when walking on uneven terrain.27,43 Isolated subtalar arthritis can be treated with a hinged-ankle AFO to control motion in the coronal plane yet allow normal physiologic function at the ankle. A UCBL insert is less rigid yet effective in limiting subtalar inversion and eversion in the treatment of subtalar arthritis. SMO (supramalleolar orthosis) is a modification of the UCBL (Figure 1) in which the orthosis extends proximally above the level of the malleoli to increase constraint and stability of the hindfoot. 67 There is no clinical study evaluating the effectiveness of different brace designs for conservative management of subtalar arthritis. However, a biomechanical study showed superiority of the UCBL over the AFO for patients with subtalar arthritis pain originating from subtalar ROM, the UCBL provided restriction of hindfoot motion while allowing forefoot motion. 20
If the ankle and subtalar joints are both affected by osteoarthritis, a fixed AFO with or without UCBL, or an SMO is most effective in limiting motion in both joints. 67
Midfoot Arthritis
Midfoot arthritis can be treated with stabilization of the transverse tarsal and tarsometatarsal joints while permitting function during weight bearing. Stiff-soled shoes and alternate lacing methods to avoid dorsal pressure are common first line modalities.24,67 A UCBL can be effective by cupping the heel medially and laterally, while the arch of the UCBL supports the midfoot, stabilizing the midtarsal joint and limiting the abduction and adduction of the midfoot. 67 A carbon graphite shank is another option that functions as a stiff plantar support strut and has been shown to reduce plantar pressure along the midfoot. 46 This insert is available in variable lengths and is interchangeable among shoes, which may improve patient compliance. A full-length carbon graphite shank has been shown to be 75% effective for conservative management of midfoot arthritis. 50
More severe cases of midfoot arthritis are best treated with an AFO with an extended footplate to minimize motion within the affected joints. 67 A double rocker-bottom shoe modification may also be beneficial for the patient with midfoot arthritis. 24
The concept of the rocker-bottom–soled shoe is to allow the foot to roll from heel-strike to the toe-off phases of the gait cycle, thereby providing a smooth transition with more controlled joint motion. This can be achieved with the use of a rigid contoured platform, where the site and pitch of the contour can be adjusted and tailored to the pathology.
A double-rocker–soled shoe (Figure 15) has the thinnest portion of the contoured platform at the level of the midfoot. This contour targets the relief of midfoot pressure without increasing forefoot or hindfoot pressure, thus helping the transition from heel strike to toe off without the foot bending. This eliminates painful midfoot dorsiflexion present during the native gait cycle. This can be particularly useful in patients with midfoot arthritis, or Charcot arthropathy with rocker-bottom foot deformity.7,23,24
Figure 15.
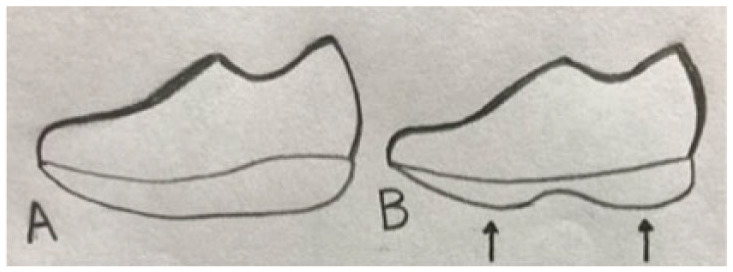
(A) Single-rocker–soled shoe. (B) Double-rocker–soled shoe.
Hallux Disorders
Hallux Rigidus (First Metatarsophalangeal Joint Arthritis)
The first metatarsophalangeal joint is the most common site of forefoot arthritis. With hallux rigidus, high heels and shoes with narrow toe boxes should be avoided, as they increase the dorsiflexion forces on the first metatarsophalangeal joint and worsen the symptoms. 67 For mild hallux rigidus, stiff-soled footwear and figure of 8 taping can be effective in limiting the excursion at the first metatarsophalangeal joint. 59 A Morton extension plate (Figure 16) is another effective option in controlling motion and reducing pain at the first metatarsophalangeal joint.31,67 The shank is typically composed of either steel or carbon graphite and can be either embedded within the layers of the sole or available as an interchangeable orthosis. 42 It acts as an internal splint to reduce the bending moment around the hallux and limit dorsiflexion during gait. Additionally, a rocker-bottom sole can help improve gait biomechanics and further compensate for the limited dorsiflexion. 31 In one study, the success rate of conservative management of hallux rigidus was 55% (428/772 patients with symptomatic hallux rigidus), with 362 (84%) of these 428 patients treated with orthoses including low-heeled shoes, shoes with a stiffer sole, rocker-bottom shoes, metatarsal bar, and Morton extension. 16
Figure 16.

The Morton extension plate.
Hallux Valgus
Hallux valgus is one of the most commonly encountered pathologies in the orthopedic foot and ankle field. Patients should be educated that orthotic devices and custom footwear cannot correct or prevent hallux valgus but may delay progression and control discomfort.13,67 Conservative treatment focuses on reducing discomfort and progression of the deformity through footwear with an especially wide toe box. Narrow footwear and fashionable heels place excess valgus stress on the first metatarsophalangeal joint and should be avoided. 67 Other treatment modalities consist of medial eminence padding, metatarsal offloading pads to reduce pressure on the metatarsal heads, and appropriate correction of any underlying pronation deformity. Severe pronation of the forefoot can place an increased pressure over the first metatarsophalangeal joint medial eminence, and an appropriate orthotic can theoretically reduce this pressure; however, this has not shown to be effective.13,67 Orthotics are not indicated for patients without this component to their pain as most orthotics cannot control the valgus positioning of the hallux. Another nonorthotic treatment option is the bunion night splint; however, this has not been shown to be effective.37,62
Summary
Foot orthoses and shoe modifications represent an essential component of the nonoperative management protocols for a wide variety of acute and chronic disorders of the foot and ankle (Table 1), including congenital deformities, traumatic injuries, inflammatory disorders (RA), arthritis (forefoot, midfoot and hindfoot), neurologic conditions, diabetes, and sports-related injuries.
Table 1.
Table Summarizing the Most Commonly Used Off-the-Shelf and Prescription Orthotics, Braces, and Shoe Modifications.
| Foot/Ankle Disorder | Prescription Orthotic, Brace, or Shoe Modification |
|---|---|
| Plantar fasciitis | • Viscoelastic heel pad • Dorsiflexion night splint • Plantar fascia support insole |
| Flexible flatfoot (stages I-II PTTD) | • Semirigid orthotic with arch support or medial heel post • UCBL |
| Rigid flatfoot ± ankle involvement (stages III, IV PTTD) | Solid AFO (Arizona brace) |
| Achilles tendinopathy (insertional/noninsertional) | • MAFO • AirHeel brace • Heel lift • Night splint |
| Subtle cavus (forefoot-driven) | An orthotic with a first ray recess (cut-out), a metatarsal bar and possibly a lateral forefoot post (Arch Rival) |
| Flexible cavovarus (hindfoot-driven) | Semirigid full-length orthotic with an elevated heel, a lateral hindfoot to midfoot heel wedge, either a lateral forefoot post or first-ray recess and no medial arch support. |
| Rigid cavus | Solid AFO (Arizona brace) |
| Interdigital (Morton neuroma) | Metatarsal pad |
| Ankle arthritis | • Arizona brace • MAFO • Rocker-bottom–soled shoe • SACH |
| Midfoot arthritis | • UCBL • Carbon graphite shank • AFO with extended foot plate • Double rocker soled shoe |
| Hallux rigidus | Carbon fiber plate with Morton extension |
Abbreviations: AFO, ankle-foot orthosis; UCBL, University of California Biomechanics Laboratory; MAFO, molded ankle-foot orthosis; PTTD, posterior tibial tendon dysfunction; SACH, solid ankle cushion heel.
The orthopedic foot and ankle surgeon should understand the biomechanics and normal function of the foot and ankle, as well as the sequelae of the disease affecting the foot and/or ankle. The practitioner should be familiar with off-the-shelf inserts, braces, and orthotics as well as the prescription ones. Furthermore, it is becoming increasingly important for the practicing foot and ankle surgeon to find and communicate with a local orthotist and establish a partnership with him or her. This partnership will become an essential part of successful foot and ankle practice for both the conservative and postoperative management of foot and ankle disorders using off-the-shelf and customs orthotics and braces.
Footnotes
This article was originally published as: Elattar O, Smith T, Ferguson A, Farber D, Wapner K. Uses of braces and orthotics for conservative management of foot and ankle disorders. Foot Ankle Orthop. 2018 Aug 5;3(3):2473011418780700. doi:10.1177/2473011418780700.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Alfredson H, Cook J. A treatment algorithm for managing Achilles tendinopathy: new treatment options. Br J Sports Med. 2007;41(4):211-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Alimusaj M, Knie I, Wolf S, et al. Functional impact of carbon fiber springs in ankle foot orthoses [in German]. Orthopade. 2007;36(8):752-756. [DOI] [PubMed] [Google Scholar]
- 3. Alvarez RG, Marini A, Schmitt C, Saltzman CL. Stage I and II posterior tibial tendon dysfunction treated by a structured nonoperative management protocol: an orthosis and exercise program. Foot Ankle Int. 2006;27(1):2-8. [DOI] [PubMed] [Google Scholar]
- 4. Augustin JF, Lin SS, Berberian WS, Johnson JE. Nonoperative treatment of adult acquired flat foot with the Arizona brace. Foot Ankle Clin. 2003;8(3):491-502. [DOI] [PubMed] [Google Scholar]
- 5. Baldassin V, Gomes CR, Beraldo PS. Effectiveness of prefabricated and customized foot orthoses made from low-cost foam for noncomplicated plantar fasciitis: a randomized controlled trial. Arch Phys Med Rehabil. 2009;90(4):701-706. [DOI] [PubMed] [Google Scholar]
- 6. Batt ME, Tanji JL, Skattum N. Plantar fasciitis: a prospective randomized clinical trial of the tension night splint. Clin J Sport Med. 1996;6(3):158-162. [PubMed] [Google Scholar]
- 7. Brown D, Wertsch JJ, Harris GF, Klein J, Janisse D. Effect of rocker soles on plantar pressures. Arch Phys Med Rehabil. 2004;85(1):81-86. [DOI] [PubMed] [Google Scholar]
- 8. Chao W, Wapner KL, Lee TH, Adams J, Hecht PJ. Nonoperative management of posterior tibial tendon dysfunction. Foot Ankle Int. 1996;17(12):736-741. [DOI] [PubMed] [Google Scholar]
- 9. Chia KK, Suresh S, Kuah A, Ong JL, Phua JM, Seah AL. Comparative trial of the foot pressure patterns between corrective orthotics, formthotics, bone spur pads and flat insoles in patients with chronic plantar fasciitis. Ann Acad Med Singapore. 2009;38(10):869-875. [PubMed] [Google Scholar]
- 10. Cullen NP, Singh D. Plantar fasciitis: a review. Br J Hosp Med (Lond). 2006;67(2):72-76. [DOI] [PubMed] [Google Scholar]
- 11. Dahmen R, Haspels R, Koomen B, Hoeksma AF. Therapeutic footwear for the neuropathic foot: an algorithm. Diabetes Care. 2001;24(4):705-709. [DOI] [PubMed] [Google Scholar]
- 12. Donoghue OA, Harrison AJ, Laxton P, et al. Orthotic control of rear foot and lower limb motion during running in participants with chronic Achilles tendon injury. Sport Biomech. 2008;7(2):194-205. [DOI] [PubMed] [Google Scholar]
- 13. Easley ME, Trnka HJ. Current concepts review: hallux valgus part 1: pathomechanics, clinical assessment, and nonoperative management. Foot Ankle Int. 2007;28(5):654-659. [DOI] [PubMed] [Google Scholar]
- 14. Goske S, Erdemir A, Petre M, Budhabhatti S, Cavanagh PR. Reduction of plantar heel pressures: insole design using finite element analysis. J Biomech. 2006;39(13):2363-2370. [DOI] [PubMed] [Google Scholar]
- 15. Gould JS, Ford D. Orthoses and insert management of common foot and ankle problems. In: Baxter DE, Porter DA, Schon L. eds. Baxter’s The Foot and Ankle in Sport. Chap. 27. Philadelphia, PA: Elsevier; 2008:587-593. [Google Scholar]
- 16. Grady JF, Axe TM, Zager EJ, Sheldon LA. A retrospective analysis of 772 patients with hallux limitus. J Am Podiatr Med Assoc. 2002;92(2):102-108. [DOI] [PubMed] [Google Scholar]
- 17. Haddad SL, Deland JT. Pes planus. In: Coughlin MJ, Saltzman CL, Anderson RB. eds. Mann’s Surgery of the Foot and Ankle. 9th ed. Philadelphia, PA: Elsevier; 2014:1292-1360. [Google Scholar]
- 18. Hu P. Pedorthic care of the arthritic foot. In: Peng Y, Weng X, eds. 7th Asian-Pacific Conference on Medical and Biological Engineering. IFMBE Proceedings, vol 19. Berlin: Springer; 2008. [Google Scholar]
- 19. Huang YC, Harbst K, Kotajarvi B, et al. Effects of ankle-foot orthoses on ankle and foot kinematics in patients with ankle osteoarthritis. Arch Phys Med Rehabil. 2006;87:710-716. [DOI] [PubMed] [Google Scholar]
- 20. Huang YC, Harbst K, Kotajarvi B, et al. Effects of ankle-foot orthoses on ankle and foot kinematics in patients with subtalar osteoarthritis. Arch Phys Med Rehabil. 2006;87(8):1131-1136. [DOI] [PubMed] [Google Scholar]
- 21. Humble RN. Custom foot orthotic management in Achilles tendinopathy. In: Maffulli N, Almekinders LC, eds. The Achilles Tendon. Dordrecht: Springer; 2007:70. [Google Scholar]
- 22. Hylton NM. Postural and functional impact of dynamic AFOs and FOs in a pediatric population. J Prosthet Orthot. 1989;2(1):40-53. [Google Scholar]
- 23. Janisse D, Wertsch JJ, Del Toro DR. Foot orthoses and prescription shoes. In: Redford JB, Basmajian Trautman P, eds. Orthotics–Clinical Practice and Rehabilitation Technology. New York: Churchill Livingstone Inc; 1995. [Google Scholar]
- 24. Janisse DJ, Janisse E. Shoe modification and the use of orthoses in the treatment of foot and ankle pathology. J Am Acad Orthop Surg. 2008;16(3):152-158. [DOI] [PubMed] [Google Scholar]
- 25. Janisse DJ. A scientific approach to insole design for the diabetic foot. Foot. 1993;3(3):105-108. [Google Scholar]
- 26. Janisse DJ. Pedorthic care of the diabetic foot. Diabetic Foot. 1993;5:549-576. [Google Scholar]
- 27. Kile TA, Bouchard M. Degenerative Joint Disease of the Ankle and Hindfoot. Philadelphia, PA: Lippincott Williams & Wilkins; 2004. [Google Scholar]
- 28. Kilmartin TE, Wallace WA. Effect of pronation and supination orthosis on Morton’s neuroma and lower extremity function. Foot Ankle Int. 1994;15(5):256-262. [DOI] [PubMed] [Google Scholar]
- 29. Kogler GF, Solomonidis SE, Paul JP. Biomechanics of longitudinal arch support mechanisms in foot orthoses and their effect on plantar aponeurosis strain. Clin Biomech (Bristol, Avon). 1996;11(5):243-252. [DOI] [PubMed] [Google Scholar]
- 30. Krause F, Bosshard A, Lehmann O, Weber M. Shell brace for stage II posterior tibial tendon insufficiency. Foot Ankle Int. 2008;29(11):1095-1100. [DOI] [PubMed] [Google Scholar]
- 31. Kunnasegaran R, Thevendran G. Hallux rigidus: nonoperative treatment and orthotics. Foot Ankle Clin. 2015;20(3):401-412. [DOI] [PubMed] [Google Scholar]
- 32. Kvist M. Achilles tendon injuries in athletes. Sports Med. 1994;18(3):173-201. [DOI] [PubMed] [Google Scholar]
- 33. Landorf KB, Keenan AM, Herbert RD. Effectiveness of foot orthoses to treat plantar fasciitis: a randomized trial. Arch Intern Med. 2006;166(12):1305-1310. [DOI] [PubMed] [Google Scholar]
- 34. Leung J, Moseley A. Impact of ankle-foot orthoses on gait and leg muscle activity in adults with hemiplegia: systematic literature review. Physiotherapy. 2003;89(1):39-55. [Google Scholar]
- 35. LoPiccolo M, Chilvers M, Graham B. Effectiveness of the cavus foot orthosis. J Surg Orthop Adv. 2010;19(3):166-9 [PubMed] [Google Scholar]
- 36. Maffulli N, Kader D. Tendinopathy of the tendo Achilles. J Bone Joint Surg. 2002;84(1):1-8. [DOI] [PubMed] [Google Scholar]
- 37. Mann RA, Coughlin MJ. Hallux valgus-etiology, anatomy, treatment and surgical considerations. Clin Orthop Relat Res. 1981;157:31-41. [PubMed] [Google Scholar]
- 38. Manoli A, Graham B. The subtle cavus foot, “the underpronator,” a review. Foot Ankle Int. 2005;26(3):256-263. [DOI] [PubMed] [Google Scholar]
- 39. Martin RL, Stewart GW, Conti SF. Posttraumatic ankle arthritis: an update on conservative and surgical management. J Orthop Sports Phys Ther. 2007;37(5):253-259. [DOI] [PubMed] [Google Scholar]
- 40. Mayer F, Hirschmuller A, Muller S, et al. Effects of short-term treatment strategies over 4 weeks in Achilles tendinopathy. Br J Sports Med. 2007;41(7):e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Michael JW. Lower limb orthoses. In: Hsu JD, Michael JW, Fisk JR; American Academy of Orthopaedic Surgeons, eds. AAOS Atlas of Orthoses and Assistive Devices. Philadelphia, PA: Mosby Elsevier; 2008:343-355. [Google Scholar]
- 42. Michaud TC. Foot Orthoses and Other Forms of Conservative Foot Care. Baltimore, MD: Williams & Wilkins; 1993. [Google Scholar]
- 43. Michelson J, Fasler M, Wigley F, Hellman D. Foot and ankle problems in rheumatoid arthritis. Foot Ankle Int. 1994;15(11):608-613. [DOI] [PubMed] [Google Scholar]
- 44. Nawoczenski DA, Cook TM, Saltzman CL. The effect of foot orthotics on three-dimensional kinematics of the leg and rearfoot during running. J Sports Phys Ther. 1995;21(6):317-327. [DOI] [PubMed] [Google Scholar]
- 45. Neville C, Lemley FR. Effect of ankle-foot orthotic devices on foot kinematics in stage II posterior tibial tendon dysfunction. Foot Ankle Int. 2012;33(5):406-414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Patel A, Rao S, Nawoczenski D, Flemister AS, DiGiovanni B, Baumhauer JF. Midfoot arthritis. J Am Acad Orthop Surg. 2010;18(7):417-425. [DOI] [PubMed] [Google Scholar]
- 47. Petersen W, Welp R, Rosenbaum D. Chronic Achilles tendinopathy: a prospective randomized study comparing the therapeutic effect of eccentric training, the AirHeel brace, and a combination of both. Am J Sports Med. 2007;35(10):1659-1667. [DOI] [PubMed] [Google Scholar]
- 48. Powell M, Post WR, Keener J, Wearden S. Effective treatment of chronic plantar fasciitis with dorsiflexion night splints: a crossover prospective randomized outcome study. Foot Ankle Int. 1998;19(1):10-18. [DOI] [PubMed] [Google Scholar]
- 49. Raikin SM, Parks BG, Noll KH, Schon LC. Biomechanical evaluation of the ability of casts and braces to immobilize the ankle and hindfoot. Foot Ankle Int. 2001;22(3):214-219. [DOI] [PubMed] [Google Scholar]
- 50. Rao S, Baumhauer JF, Becica L, Nawoczenski DA. Shoe inserts alter plantar loading and function in patients with midfoot arthritis. J Orthop Sports Phys Ther. 2009;39(7):522-531. [DOI] [PubMed] [Google Scholar]
- 51. Richie DH. Orthotics. In: DiGiovanni CW, Greisgerg J. eds. Foot and Ankle: Core Knowledge in Orthopedics. Philadelphia, PA: Elsevier-Mosby; 2007:16-38. [Google Scholar]
- 52. Rogozinski BM, Davids JR, Davis RB, III, Jameson GG, Blackhurst DW. The efficacy of the floor-reaction ankle-foot orthosis in children with cerebral palsy. J Bone Joint Surg Am. 2009;91(10):2440-2447. [DOI] [PubMed] [Google Scholar]
- 53. Roos E, Engström M, Söderberg B. Foot orthoses for the treatment of plantar fasciitis. Foot Ankle Int. 2006;27(8):606-611. [DOI] [PubMed] [Google Scholar]
- 54. Roos EM, Engstrom M, Lagerquist A, et al. Clinical improvement after 6 weeks of eccentric exercise in patients with midportion Achilles tendinopathy: a randomized trial with 1-year follow-up. Scand J Med Sci Sports. 2004;14(5):286-295. [DOI] [PubMed] [Google Scholar]
- 55. Rosenbloom KB. Pathology-designed custom molded foot orthoses. Clin Podiatr Med Surg. 2011;28(1):171-187. [DOI] [PubMed] [Google Scholar]
- 56. Ryan M, Grau S, Krauss I, et al. Kinematic analysis of runners with Achilles mid-portion tendinopathy. Foot Ankle Int. 2009;30(12):1190-1195. [DOI] [PubMed] [Google Scholar]
- 57. Saygi B, Yildirim Y, Saygi EK, Kara H, Esemenli T. Morton neuroma: comparative results of two conservative methods. Foot Ankle Int. 2005;26(7):556-559. [DOI] [PubMed] [Google Scholar]
- 58. Seligman DA, Dawson DR. Customized heel pads and soft orthotics to treat heel pain and plantar fasciitis. Arch Phys Med Rehabil. 2003;84(10):1564-1567. [DOI] [PubMed] [Google Scholar]
- 59. Shurnas PS. Hallux rigidus: etiology, biomechanics, and nonoperative treatment. Foot Ankle Clin. 2009;14(1):1-8. [DOI] [PubMed] [Google Scholar]
- 60. Singh SK, Ioli JP, Chiodo CP. The surgical treatment of Morton’s neuroma. Curr Orthop. 2005;19(5):379-384. [Google Scholar]
- 61. Tang SF, Chen CP, Hong WH, Chen HT, Chu NK, Leong CP. Improvement of gait by using orthotic insoles in patients with heel injury who received reconstructive flap operations. Am J Phys Med Rehabil. 2003;82(5):350-356. [DOI] [PubMed] [Google Scholar]
- 62. Tehraninasr A, Saeedi H, Forogh B, Bahramizadeh M, Keyhani MR. Effects of insole with toe-separator and night splint on patients with painful hallux valgus: a comparative study. Prosthet Orthot Int. 2008;32(1):79-83. [DOI] [PubMed] [Google Scholar]
- 63. Thompson JA, Jennings MB, Hodge W, et al. Orthotic therapy in the management of osteoarthritis. J Am Podiatr Med Assoc. 1992;82(3):136-139. [DOI] [PubMed] [Google Scholar]
- 64. Tyson SF, Thornton HA. The effect of a hinged ankle foot orthosis on hemiplegic gait: objective measures and users’ opinions. Clin Rehabil. 2001;15(1):53-58. [DOI] [PubMed] [Google Scholar]
- 65. Walther M, Kratschmer B, Verschl J, et al. Effect of different orthotic concepts as first line treatment of plantar fasciitis. Foot Ankle Surg. 2013;19(2):103-107. [DOI] [PubMed] [Google Scholar]
- 66. Wapner KL, Sharkey PF. The use of night splints for treatment of recalcitrant plantar fasciitis. Foot Ankle. 1991;12(3):135-137. [DOI] [PubMed] [Google Scholar]
- 67. Wapner KL. Conservative treatment of the foot. In: Surgery of the Foot and Ankle. St Louis, MO: CV Mosby, 1999:115-130. [Google Scholar]
- 68. Wolf SI, Alimusaj M, Rettig O, Doderlein L. Dynamic assist by carbon fiber spring AFOs for patients with myelomeningocele. Gait Posture. 2008;28(1):175-177. [DOI] [PubMed] [Google Scholar]
- 69. Woodburn J, Barker S, Helliwell PS. A randomized controlled trial of foot orthoses in rheumatoid arthritis. J Rheumatol. 2002;29(7):1377-1383. [PubMed] [Google Scholar]
- 70. Wu KK. Foot orthoses. In: Goldberg B, Hsue JD. eds. Atlas of Orthoses and Assistive Devices. St. Louis, MO: American Academy of Orthopaedic Surgeons. Mosby-Year Book: 1997:463-476. [Google Scholar]
- 71. Wu WL, Rosenbaum D, Su FC. The effects of rocker sole and SACH heel on kinematics in gait. Med Eng Phys. 2004;26(8):639-646. [DOI] [PubMed] [Google Scholar]


