Abstract
This case report describes the first known successful treatment of exfoliative cheilitis with the interleukin-4 receptor alpha antagonist dupilumab in an adult patient. With no response to topical tacrolimus, hydrocortisone, dapsone, crisaborole or systemic doxycycline, low dose isotretinoin, or methotrexate, she had resolution with off-label dupilumab after 4 months of treatment.
Keywords: Exfoliative cheilitis, cheilitis, atopic dermatitis, dupilumab
Introduction
Exfoliative cheilitis (EC) is a rare and chronic inflammatory condition that affects the cutaneous lip. It is characterized by excessive desquamation of thickened keratin scales.1,2 This causes cyclical and continuous peeling of the lips with associated pain, pruritus, and tingling. Studies show that it typically affects young females; however, a wide age range (20–80 years) has been shown to be affected. 2 Although no cause has been elucidated, between 40 and 87% of cases have been associated with psychiatric disorders (e.g., depression, anxiety, obsessive compulsive disorder,) and habits such as lip licking and lip biting.1–3
EC is a diagnosis of exclusion after ruling out other conditions including actinic cheilitis, atopic cheilitis, and allergic contact cheilitis. Atopic cheilitis is triggered by an allergen and would have positive allergy testing, whereas allergic contact cheilitis is triggered by a hapten and has positive patch testing. 4 Bacterial, fungal, and viral infections should also be excluded.
The approach to treatment is challenging due to limited data and lack of strong evidence to guide therapy. Topical therapies include corticosteroids, tacrolimus, antibacterial and antifungal ointments, keratolytic agents (urea and salicylic acids), cryotherapy, Calendula officinalis, narrowband ultraviolet B phototherapy, excimer laser therapy, and more recently CO2 laser.1,2,5–9 Systemic therapies include oral corticosteroids, antifungals, antivirals, and antidepressants, all with variable response.6,10
The human monoclonal antibody, dupilumab is an antagonist of the interleukin-4 (IL-4) receptor alpha. This inhibits the pro-inflammatory IL-4 and IL-13 pathways. In dermatology, dupilumab has been approved for moderate to severe atopic dermatitis and more recently prurigo nodularis. To our knowledge, this is the first case of EC successfully treated with off-label dupilumab.
Case report
A 35-year-old female with a history of childhood atopic dermatitis presented to our clinic with a 2.5 year history of erythematous and scaly lips. She had multiple flares monthly which would induce pain and pruritis. She had previously been treated by another dermatologist who tried topical corticosteroids, topical tacrolimus, petroleum jelly, and doxycycline (for possible concomitant rosacea). Tacrolimus ointment was useful in preventing flares; however, did not reduce the duration of flares. Other previous investigations, including patch testing, varicella zoster virus polymerase chain reaction (PCR), and herpes simplex virus PCR which were all negative.
When she presented to our clinic, her lips were edematous, scaly with microvesicles, and a few cream-colored pustules (Figure 1(a)). In the consult visit, tacrolimus ointment was prescribed to prevent flares, hydrocortisone valerate 0.2% ointment to be used during flares, prophylactic valacyclovir 500 mg twice daily for 3 months, and Vaseline as a lip barrier. The hydrocortisone worked well during flares, however flares were becoming increasing frequent to once weekly. At follow-up, she still had microvesicles and pustules on the lip (Figure 1(b)). Dapsone 5% gel twice daily was trialed and was ineffective. Crisaborole 2% ointment twice daily worsened the flares. Systemic therapy included isotretinoin 10 mg daily, which triggered retinoid dermatitis on the face, methotrexate was also ineffective. Treatment with alitretinoin 30 mg PO daily was suggested, however this was unaffordable to the patient. Finally, dupilumab with a 600 mg loading dose, followed by 300 mg every 4 weeks was prescribed. After 4 months of treatment, her lips were no longer pruritic or painful. She no longer required topical tacrolimus or corticosteroid. On exam the hyperkeratotic scale had resolved, there were no perioral lesions or scarring (Figure 2). She has not had any flares of EC. She has occasional irritation of the eyelids; however, she is able to manage this with emollients.
Figure 1.
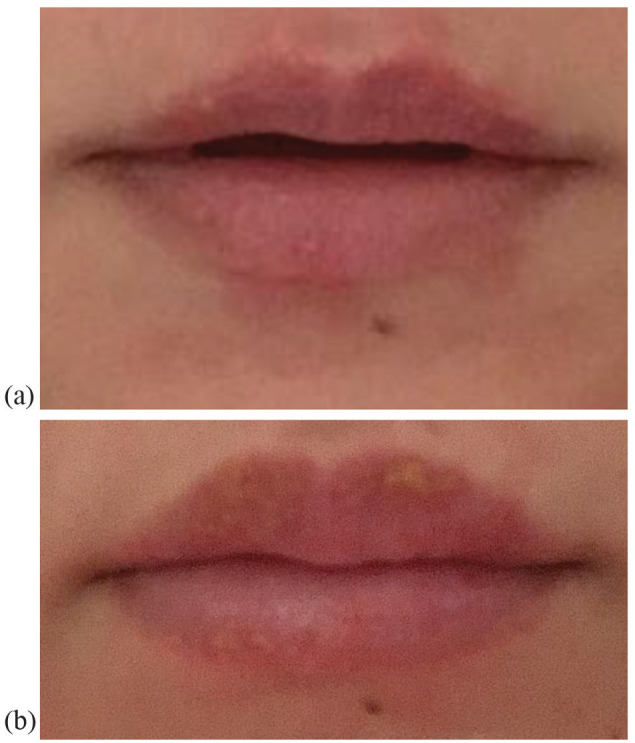
(a) Edematous, scaly cutaneous lip with microvesicles, and a few cream-colored pustules, (b) at follow-up she continued to have microvesicles, pustules, and yellow lamellar scale on the cutaneous lips.
Figure 2.

Cutaneous lips without any hyperkeratotic scale, perioral lesions, or scaring, photo was taken 3 months after starting dupilumab.
Discussion
Effective treatment options for EC are limited. To the best of our knowledge, this is the first case report of successful treatment of EC with dupilumab. Dupilumab is a human monoclonal immunoglobulin-G4 (IgG4) antibody that targets the shared IL-4Rα subunit that blocks the IL-4 and IL-13 transduction pathways. 11 This inhibits the aberrant T helper-2 (Th2)-mediated inflammatory pathway to help normalize barrier function. 11 Suppressing IL-4 and IL-13 with dupilumab changes gene expression, which decreases markers of epidermal proliferation and inflammatory mediators. 12 It also acts to increase lipid metabolism proteins, structural, and barrier proteins. 12
EC is a condition affecting the vermilion boarder of the lip characterized by inflammation and desquamation often with thick keratin scale. Histopathology demonstrates parakeratosis, hyperkeratosis, acantholysis, as well as acute and chronic inflammation, including lymphoplasmacytic infiltration in the dermis.2,13 Patients with EC have a predisposition of type I IgE-mediated hypersensitivity. 14 Interestingly, this patient also had a history of childhood atopic dermatitis. It is thus possible that the therapeutic effect of dupilumab blocking the Th2 pathway, downregulating inflammatory mediators and epidermal proliferation contributed to resolution of EC in this patient. This case suggests that dupilumab may be considered in patients with recalcitrant EC, particularly if they have a history of atopic dermatitis.
Acknowledgments
The authors would like to acknowledge the dermatology staff at the University of Ottawa who assisted in the care of this patient.
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: G. Gavigan has received honoraria from Amgen, AbbVie, Bausch, Beiersdorf, Galderma, Lilly, Medexus Pharma, Novartis, L’Oreal Canada, Pfizer, Sanofi, Sun Pharma, UCB, and Valent.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Patient consent: Written informed consent for patient information and images to be published was provided by the patient.
References
- 1. Reade PC, Sim R. Exfoliative cheilitis a factitious disorder? Int J Oral Maxillofac Surg 1986; 15: 313–317. [DOI] [PubMed] [Google Scholar]
- 2. Almazrooa SA, Woo SB, Mawardi H, et al. Characterization and management of exfoliative cheilitis: a single-center experience. Oral Surg Oral Med Oral Pathol Oral Radiol 2013; 116: e485–e489. [DOI] [PubMed] [Google Scholar]
- 3. Crotty CP, Dicken CH. Factitious lip crusting. Arch Dermatol 1981; 117: 338–340. [PubMed] [Google Scholar]
- 4. Schena D, Fantuzzi F, Girolomoni G. Contact allergy in chronic eczematous lip dermatitis. Eur J Dermatol 2008; 18: 688–692. [DOI] [PubMed] [Google Scholar]
- 5. Taniguchi S, Kono T. Exfoliative cheilitis: a case report and review of the literature. Dermatology 1998; 196: 253–255. [DOI] [PubMed] [Google Scholar]
- 6. Daley TD, Gupta AK. Exfoliative cheilitis. J Oral Pathol Med 1995; 24: 177–179. [DOI] [PubMed] [Google Scholar]
- 7. Postlethwaite KR, Hendrickse NM. A case of exfoliative cheilitis. Br Dent J 1988; 165: 23. [DOI] [PubMed] [Google Scholar]
- 8. Park CS, Park JH, Lee J, et al. Chronic exfoliative cheilitis successfully treated by pinhole method using CO2 laser. Ann Dermatol 2019; 31(3): 361–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bhatia BK, Bahr BA, Murase JE. Excimer laser therapy and narrowband ultraviolet B therapy for exfoliative cheilitis. Int J Womens Dermatol 2015; 1(2): 95–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Aydin E, Gokoglu O, Ozcurumez G, et al. Factitious cheilitis: a case report. J Med Case Rep 2008; 2: 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Beck LA, Thaçi D, Hamilton JD, et al. Dupilumab treatment in adults with moderate-to-severe atopic dermatitis. N Engl J Med 2014; 371(2): 130–139. [DOI] [PubMed] [Google Scholar]
- 12. Hamilton JD, Suárez-Fariñas M, Dhingra N, et al. Dupilumab improves the molecular signature in skin of patients with moderate-to-severe atopic dermatitis. J Allergy Clin Immunol 2014; 134(6): 1293–1300. [DOI] [PubMed] [Google Scholar]
- 13. Mani SA, Shareef BT. Exfoliative cheilitis: report of a case. J Can Dent Assoc 2007; 73(7): 629–632. [PubMed] [Google Scholar]
- 14. Cai L, Wei J, Ma D, et al. Predisposition of hypersensitivity in patients with exfoliative cheilitis. J Dent Sci 2022; 17(1): 476–481. [DOI] [PMC free article] [PubMed] [Google Scholar]


