Abstract
Objective: The appearance of the gingival tissue around the teeth is essential in the aesthetics of the anterior maxillary region of the oral cavity. Abnormalities in symmetry and contour can significantly compromise the appearance of the natural or restored dentition, so the outcome is highly relevant to treatment choice. This study evaluated the efficacy of crown lengthening for restoration of maxillary anterior tooth defects. Methods: A total of 80 patients (87 affected teeth) diagnosed with maxillary anterior tooth loss in Ganzhou People’s Hospital between May 2020 and August 2021 were retrospectively enrolled and divided into an experimental group or a reference group according to different treatment methods, with 40 cases in each group. The reference group received a post and core procedure, while the experimental group received crown lengthening plus a post and core procedure. Outcome measures included clinical efficacy, gingival periodontal-related indices, and dental aesthetics indices. Results: Crown lengthening plus post and core procedure was associated with a significantly higher clinical efficacy (95.65%) versus post and core procedure alone (78.05%) (P<0.05). Postoperatively, the levels of probing depth (PD), plaque index (PLI), bleeding index (BI), and gingival index (GI) were lower in patients of the experimental group than those in the reference group (all P<0.05). Crown lengthening plus post and core procedure resulted in more Kay class I and II patients and fewer Kay class III and IV versus the post and core procedure alone (P<0.05). The position of gingival margin (PGM) and gingival recession (GR) of patients in the experimental group were higher than those in the reference group after operation (P<0.05). Logistic regression analysis showed that the morphology of broken ends, plaque control, hygiene habits, and smoking were influencing factors for maxillary anterior tooth defects (all P<0.05). Patients were more satisfied (97.50%) in the experimental group than those in the reference group (80.00%) (P<0.05). Conclusion: Crown lengthening improves the periodontal condition of patients with maxillary anterior tooth loss, reduces gingival sulcus bleeding, and improves dental aesthetics and patient satisfaction. Further clinical studies are required prior to clinical promotion.
Keywords: Maxillary anterior teeth, dental defects, crown lengthening, restorative results
Introduction
The anterior maxillary region is an important area for oral aesthetics, and tooth loss in this region results in serious aesthetic implications [1]. Traumatic fractures and severe dental caries are prone to the loss of maxillary anterior teeth and the formation of vestigial roots and crowns that violate the distance from the bottom of the gingival sulcus to the alveolar ridge, affecting the patient’s masticatory function and appearance [2]. With the increasing aesthetic requirements of the patients in the oral cavity, maxillary anterior tooth defects require appropriate interventions to restore the distance from the base of the gingival sulcus to the alveolar ridge [3,4]. The ideal anterior tooth appearance necessitates healthy and non-inflammatory periodontal tissues. Periodontal tissue must be properly prepared prior to restorative treatment to ensure good morphology, function, aesthetics, and patient comfort of the masticator [5]. As a standard treatment, the post and core procedure is performed after a root canal to salvage existing teeth that have lost a significant amount of the internal structure [6].
Crown lengthening [7] is a periodontal surgical procedure that restores biological width by bone resection and reduction of the alveolar height in patients with maxillary anterior tooth defects. It can expose the root surface of stubs whose sections are subgingival or increase the length of clinical crowns, reducing the irritation of periodontal tissues and improving the restoration of the affected tooth [8,9]. The distance from the bottom of the gingival sulcus to the top of the alveolar ridge is normally constant, including the bonded epithelium and the connective tissue attached to the root surface at the top of the alveolar ridge crown. The biological width of the various components of periodontal tissue (biological width) is an average size of 1.07 mm for connective tissue, 0.97 mm for epithelial attachment, and 0.69 mm for sulcus depth [10]. It is essential to remain within the biological width during crown lengthening, or the gingiva will be inflamed, hyperplastic, or edematous after the restoration, resulting in a recession of the alveolar ridge [11,12]. It was found that the presence of caries or restorations close to the alveolar ridge may lead to inflammation and bone loss due to violation of the biological width, suggesting that the restoration margin is at least 3 mm from the coronal surface of the alveolar ridge, for which crown lengthening is available [13].
Crown lengthening facilitates the repositioning of the alveolar ridge at a sufficient apical distance to allow space for the reattachment of connective tissue. Combined with a post and core procedure, crown lengthening is considered to achieve higher clinical efficacy and better aesthetic efficacy. However, current clinical studies question the necessity of crown lengthening, arguing that the body will rebuild the invaded biological width over time. To this end, this study was conducted to evaluate the efficacy of crown lengthening for the restoration of maxillary anterior tooth defects.
Materials and methods
Participants
A total of 80 patients (87 affected teeth in total) diagnosed with maxillary anterior tooth loss in Ganzhou People’s Hospital between May 2020 and August 2021 were retrospectively enrolled and divided into an experimental group or a reference group according to different treatment methods. 40 patients with 41 affected teeth in the reference group received the post and core procedure, and the other 40 patients with 46 affected teeth in the experimental group received crown lengthening on the basis of the reference group. The flowchart of the patients’ enrollment is shown in Figure 1.
Figure 1.

The flowchart of the patients enrollment.
Inclusion and exclusion criteria
Inclusion criteria: 1) Subjects with maxillary anterior tooth loss due to various reasons, conforming to the relevant diagnostic criteria of Combined Periodontology, regardless of gender. 2) Subjects with tolerance to surgery and no relevant treatment contraindications. 3) Subjects with sufficient root length of the affected tooth. 4) Subjects with good oral hygiene before surgery.
Exclusion criteria: 1) Subjects with severe oral infection or other serious diseases. 2) Subjects with loose teeth. 3) Subjects with abnormal coagulation function and hematological system diseases.
Treatment method
Reference group
The reference group received a standard dental restoration procedure, the post and core procedure. The typical procedure was as follows. The root canal was dried, and a root canal with 1/2 the length of the root canal was prepared. Paraffin oil was applied to the inner wall of the root canal, and then the post and core and a suitable wax pattern were fabricated and secured. During fabrication and insertion of the restoration, special attention should be paid to the accuracy and tightness of the margins to reduce local plaque buildup and protect gingival health.
Experimental group
The experimental group received crown lengthening plus post and core procedure. Local infiltration anesthesia was performed on the side of the affected tooth using 4% Articaine. An internal oblique incision was made at the tooth defect, a full-thickness palatal mucosal periosteal flap was incised, and a separator was used to turn over the thick flap and fully expose the alveolar periosteum and the broken root of the tooth. The adhesions around the fractured root were scraped away and thoroughly rinsed, followed by hemostasis. The alveolar ridge was completely trimmed with a high-speed ball drill to allow a distance of 3 mm from the cross-section of the root. The cross-section of the root was trimmed and excess gingival tissue was removed with an electric knife to maintain the proper shape, and then adequately rinsed and sutured. The complete surgical wound was filled with a periodontal plugging agent and oral antibiotics were used to prevent infection.
8 weeks postoperatively, patients received the post and core procedure, which was identical to that used in the reference group. The crown margin was located on the tooth tissue approximately 2 mm below the edge of the post and core.
Outcome measures
Primary outcome
In this study, clinical efficacy was set as the primary outcome. The clinical efficacy of all patients was evaluated at 5 months postoperatively. Markedly effective: The patient had healthy gums, comfortable chewing, tight and well-positioned gum and crown margins, and stable restorations. Effective: The patient had mild gingival inflammation, mild chewing discomfort, slightly poor gingival margins and crowns, with grade I teeth loosening but not affecting appearance. Ineffective: The patient had obvious discomfort when chewing, the gingiva and crown did not fit together, gingivitis and periodontitis were obvious, with grade II tooth loosening. Efficiency = (markedly effective + effective)/total number of cases ×100%.
Secondary outcome
In this study, the secondary outcome included plaque index (PLI), gingival index (GI), dental aesthetics, gingival index, tooth exposure and satisfaction. The influencing factors of efficacy were analysed.
PLI assessment: The tooth surface was gently scraped with a probe and scored according to the amount and thickness of plaque. 0 points: no plaque on the gingival margin; 1 point: gingival margin tooth surface; 2 points: little plaque; 3 points: a lot of soft scale in the gingival sulcus or gingival margin and adjacent surfaces. GI assessment: 0 points: normal gingiva; 1 point: inflammation, mild discoloration, mild edema and no bleeding on probing; 2 points: moderate inflammation, edema, redness and bleeding on probing; 3 points: marked inflammation, redness and swelling of the gingiva, with ulceration and a tendency to spontaneous bleeding.
Dental aesthetics assessment: The Kay Dental Aesthetic Classification was used to evaluate the dental aesthetics of patients before and after treatment, which was classified into Class I-IV. Class I: complete tooth structure; Class II: slight changes in tooth structure; Class III: 2 or more changes in tooth structure; Class IV: malocclusion.
Gingival index: The gingival index (GI) of all patients before operation and 2, 6 and 3 months after operation was recorded, with a score of 0 points for normal gingiva, 1 point for gingival inflammation, slight discoloration, slight edema, and no bleeding on probing, 2 points for moderate inflammation, edema, red and exploratory bleeding of gingiva, and 3 points for obvious inflammation at gingiva, which was prone to spontaneous bleeding.
Tooth exposure: The tooth defect exposure of all patients before and 2, 6, and 3 months after surgery was recorded, including the position of gingival margin (PGM) and gingival recession (GR).
Patient satisfaction: A self-created patient satisfaction questionnaire of Ganzhou People’s Hospital was used, with a score of 100 points, divided into 4 levels, i.e., highly satisfied (80-100), satisfied (60-79), less satisfied (30-59), and dissatisfied (0-29). The higher the score, the higher the patient satisfaction.
Influencing factors of efficacy: Clinical data of patients were collected, including postoperative residual, depth of broken ends, height of bone removal, depth of crown margin, shape of broken end, plaque control, health habits and smoking status, and then multivariate Logistic regression analysis was performed to analyze the risk factors affecting the repair effect of maxillary anterior tooth defects.
Statistical analysis
GraphPad Prism 8 was used for image processing, and SPSS 26.0 software was used to statistically analyze the data. The measured data were expressed as (mean ± standard deviation) and tested by a t-test. The counted data were expressed as rate (%) and analyzed by chi-square test. P<0.05 indicated that a difference was significant.
Results
Patient characteristics
In the experimental group, there were 40 patients (46 affected teeth), including 22 males and 18 females, aged 18-70 (40.56 ± 13.56) years, with a BMI of 18-24 (21.56 ± 1.14) kg/m2 and duration of disease of 1-180 (73.72 ± 11.23) d. There were 11 cases of dental caries and 29 cases of trauma in terms of the cause of the defects. In the reference group, there were 40 patients (41 affected teeth), including 25 males and 15 females, aged 18-70 (39.88 ± 13.12) years, with a BMI of 18-24 (21.71 ± 1.08) kg/m2 and duration of disease of 1-180 (72.98 ± 11.33) d. There were 13 cases of dental caries and 27 cases of trauma in terms of the cause of the defects. The patient characteristics between the two groups were comparable (all P>0.05) (Table 1).
Table 1.
Patient characteristics
| Experimental | Reference | t/χ2 | P | |
|---|---|---|---|---|
| n | 40 | 40 | ||
| Affected teeth | 46 | 41 | ||
| Gender (Male/Female) | 22/18 | 25/15 | 0.462 | 0.496 |
| Age (x̅ ± s, years) | 40.56 ± 13.56 | 39.88 ± 13.12 | 0.228 | 0.820 |
| BMI (kg/m2) | 21.56 ± 1.14 | 21.71 ± 1.08 | 0.604 | 0.548 |
| Disease duration (d) | 73.72 ± 11.23 | 72.98 ± 11.33 | 0.293 | 0.770 |
| Cause of defect | 0.238 | 0.626 | ||
| Dental caries | 11 | 13 | ||
| Trauma | 29 | 27 |
BMI, body mass index.
Clinical efficacy
Patients in the experimental group had 21 teeth with markedly effective efficacy, 23 teeth with effective efficacy and 2 teeth with ineffective efficacy, while patients in the reference group had 13 teeth with markedly effective efficacy, 19 teeth with effective efficacy and 9 teeth with ineffective efficacy. Crown lengthening plus post and core procedure was associated with a higher treatment efficacy versus post and core procedure alone (P<0.05) (Table 2).
Table 2.
Clinical efficacy (%)
| Affected teeth | Excellent | Good | Difference | Excellent rate | |
|---|---|---|---|---|---|
| Experimental | 46 | 21 | 23 | 2 | 95.65 |
| Reference | 41 | 13 | 19 | 9 | 78.05 |
| χ2 | 6.082 | ||||
| P | 0.014 |
Gingival periodontal-related indices
There was no significant difference in the levels of gingival periodontal-related indices between the two groups of patients before surgery (P>0.05). After surgery, patients in the experimental group had a PD of 1.35 ± 0.18, PLI of 0.64 ± 0.08, BI of 1.05 ± 0.21, and the patients in the reference group had a PD of 2.13 ± 0.30, PLI of 1.51 ± 0.13, BI of 1.64 ± 0.33. Significantly lower PD, PLI, and BI levels were observed in the patients in the experimental group compared to the reference group (P<0.05) (Figure 2).
Figure 2.
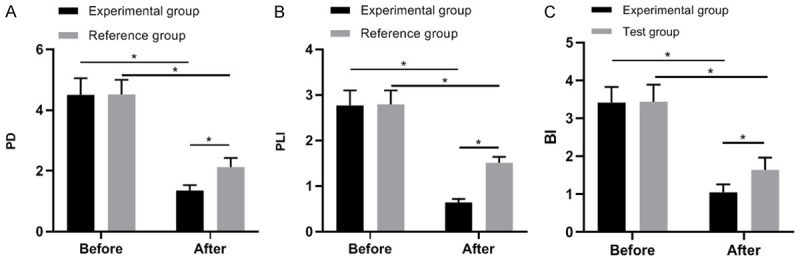
Comparison of PD levels (A), PLI levels (B) and BI levels (C) between patients in experimental group and reference group. Note: * indicates P<0.05 in the comparison between the two groups.
Dental aesthetics
There was no significant difference in the aesthetic class of teeth between the two groups of patients before surgery (P>0.05). After surgery, there were 15 cases of class I, 22 cases of class II, 3 cases of class III and 0 cases of class IV in the experimental group and 9 cases of class I, 12 cases of class II, 14 cases of class III and 5 cases of class IV in the reference group. Crown lengthening plus post and core procedure resulted in more Kay class I and II patients and fewer Kay class III and IV versus the post and core procedure alone (P<0.05) (Table 3).
Table 3.
Kay dental aesthetics (%)
| Experimental (n=40) | Reference (n=40) | χ2 | P | ||
|---|---|---|---|---|---|
| Preoperatively | I | 4 (10.00) | 5 (12.50) | 0.317 | 0.957 |
| II | 15 (37.50) | 14 (35.00) | |||
| III | 17 (42.50) | 18 (45.00) | |||
| IV | 4 (10.00) | 3 (7.50) | |||
| Postoperatively | I | 15 (37.50) | 9 (22.50) | 16.56 | <0.001 |
| II | 22 (55.00) | 12 (30.00) | |||
| III | 3 (7.50) | 14 (35.00) | |||
| IV | 0 (0.00) | 5 (12.50) | |||
Gingival index
There was no significant difference in gingival index between the two groups before operation (P>0.05). The GI of the patients in the experimental group was (1.64 ± 0.51) at 2 weeks after surgery, (1.13 ± 0.21) at 6 weeks after surgery, and (0.91 ± 0.12) at 3 months after surgery. The GI in the reference group was (2.01 ± 0.44) at 2 weeks after surgery, (1.80 ± 0.35) at 6 weeks after surgery, and (1.52 ± 0.18) at 3 months after surgery. The GI level of the patients in the experimental group after surgery was lower than that of the patients in the reference group (P<0.05) (Figure 3).
Figure 3.

Comparison of GI level at different time points between patients in experimental group and reference group. Note: * indicates P<0.05 in the comparison between the two groups.
Tooth exposure
There was no significant difference in tooth exposure index between the two groups before operation (all P>0.05). At 2 weeks, 6 weeks, 3 months after operation in the experimental group, the PGM was (0.99 ± 0.22), (1.23 ± 0.13) and (1.44 ± 0.32), the GR was (0.72 ± 0.25), (1.05 ± 0.31), and (1.19 ± 0.34), respectively. At 2 weeks, 6 weeks, and 3 months after operation in the reference group, the PGM was (0.81 ± 0.25), (0.99 ± 0.18), and (1.08 ± 0.32), and the GR was (0.64 ± 0.22), (0.87 ± 0.28), and (1.01 ± 0.41). The PGM and GR levels of patients in the experimental group were higher than those in the reference group after surgery (all P<0.05) (Figure 4).
Figure 4.

Comparison of PGM levels (A) and GR levels (B) between patients in experimental group and reference group. Note: * indicates P<0.05 in the comparison between the two groups. Position of gingival margin (PGM) and gingival recession (GR).
Influencing factors of efficacy
The results of multivariate Logistic regression analysis showed that there were no significant differences in postoperative residual, depth of broken end, height of bone removal, or depth of crown margin between the two groups (all P>0.05), while there were significant differences in the shape of broken end, plaque control, hygiene habits and smoking status (all P<0.05) (Figure 5 and Table 4).
Figure 5.

Forest map of factors influencing curative effect.
Table 4.
Logistic regression analysis of factors influencing curative effect
| Factor | β | SE | Wald | OR | 95% CI | P | |
|---|---|---|---|---|---|---|---|
| Broken end morphology | 1.318 | 0.278 | 22.677 | 3.741 | 2.151 | 6.489 | 0.011 |
| plaque control | 2.285 | 0.428 | 17.123 | 4.653 | 2.668 | 8.456 | 0.021 |
| hygiene habits | 1.485 | 0.348 | 40.651 | 3.165 | 2.354 | 6.478 | 0.019 |
| smoking | 0.958 | 0.268 | 19.832 | 2.141 | 1.189 | 3.894 | 0.025 |
Patient satisfaction
In the experimental group, 23 patients were highly satisfied, 26 patients were satisfied, 1 patient was less satisfied, and 0 patients were dissatisfied, while 11 patients in the reference group were highly satisfied, 21 patients were satisfied, 5 patients were less satisfied, and 3 patients were dissatisfied. Patients were more satisfied (97.50%) in the experimental group than in the reference group (80.00%) (P<0.05) (Table 5).
Table 5.
Patient satisfaction (%)
| Patient satisfaction | n | Highly satisfied | Satisfied | Dissatisfied | Satisfaction rate |
|---|---|---|---|---|---|
| Experimental | 40 | 23 | 26 | 1 | 97.5% |
| Reference | 40 | 11 | 21 | 8 | 80% |
| χ2 | 6.132 | ||||
| P | 0.013 |
Discussion
The maxillary anterior is an important aesthetic area of the oral cavity and has a significant impact on the patient’s appearance, mental health, and social life [14]. Maxillary anterior tooth loss is the destruction of tooth defects due to broken crowns, debris, and other diseases, with broken roots extending below the gingiva, seriously compromising the restorative and masticatory function of the tooth [15,16]. Crown lengthening follows the biological width principle to reduce the height of the alveolar ridge and gingival margin for restoration in patients with anterior tooth loss, with the coronal margin positioned without violating the biological width. It is mainly used to expose the subgingival end of traumatically cracked teeth or stub roots, or to ameliorate the aesthetic appearance of short crowns and gingival smiles. Clinical research has shown that the use of crown lengthening to expose the subgingival margin of the residual root better satisfies the requirements of restoration, gingival stability, and health [17].
The results of the present study showed that crown lengthening resulted in significantly higher treatment efficiency and lower PD, PLI, BI, and GI levels in patients versus the post and core procedure. PGM, and GR levels were higher than those in the reference group on average. PD is the distance from the gingival margin to the bottom of the pocket, reflecting the position and shape of the periodontal pocket on the tooth surface. PLI reflects the thickness of plaque and is used to monitor oral hygiene condition. BI reflects the bleeding condition. GI can monitor the condition of the gums, checking the color of the gums and reflecting bleeding. Intraoperative bone resection is the key to crown lengthening. Preoperative precise measurement of alveolar bone height and accurate calculation of the root-to-crown ratio of the affected tooth are more conducive to providing residual bone to support the affected tooth, thereby effectively avoiding dental restoration loosening. Related studies found that the post and core procedure in conjunction with crown lengthening significantly improved the condition of periodontal tissues in affected teeth and that during the restoration of dental defects, the use of crown lengthening combined with post and core procedure in patients with subgingival residual roots and crowns significantly improved the status of periodontal tissues and enhanced the treatment outcome [18], which was in line with the results in the present study. This is because the post and core procedure requires the use of allogeneic substances that inevitably affect periodontal tissues during the restoration process, leading to changes in the microecology of periodontal tissues, causing gingival bleeding, gingivitis, periodontal pocket probing, and ultimately periodontal restoration. Crown lengthening allows for effective intraoperative removal of the alveolar bone so that the alveolar ridge is parallel to the alveolar bone, or the alveolar bone is slightly below the root defect surface, promoting mutual migration of the alveolar bone and alveolar bone to the residual surface of the root defect and exposing the subgingival margin. The residual root margin can obtain sufficient clinical crown length and normal biological width to facilitate the restoration to further obtain sufficient clamping force and create conditions for the fixation of the restoration while aiding soft tissue healing and reducing inflammation, which contributes more to the restoration of periodontal tissue and the adjustment of periodontal index levels [19].
Furthermore, crown lengthening resulted in more Kay class I and II patients and fewer Kay class III and IV versus the post and core procedure, and patients were more satisfied (97.50%) with crown lengthening than with the post and core procedure (80.00%), suggesting that crown lengthening produces excellent overall treatment results and a high level of satisfaction for patients with maxillary anterior tooth defects. To achieve optimal treatment outcomes in the oral region, it is essential to allow wound healing to be completed after crown lengthening surgery, and any interruption in the wound healing may lead to adverse outcomes [20,21]. Thus, the present study performed the post and core procedure at 8 weeks postoperatively to allow for complete healing of the wound before the final crown preparation and insertion, and the results demonstrated a favorable treatment efficiency.
In addition, logistic regression analysis was conducted on the factors affecting the therapeutic effect, and the results showed that there were no statistically significant differences in postoperative residual, depth of broken end, height of bone removal and depth of crown edge between the two groups (P>0.05), while there were statistically significant differences in the shape of broken end, plaque control, hygiene habits and smoking status (P<0.05). Analysis showed that patients with a step-shaped broken end had more tooth tissue removal, and it was difficult to obtain good coronal displacement through root surface modification, which would easily affect the repair effect of patients. Patients with poor plaque control suffer from a higher degree of oral inflammation and poor oral health, which compromises the surgical efficacy and repair effect. Patients with bad oral hygiene habits have poor oral health cognition, leading to poor oral hygiene, which predisposes to a higher risk of oral bacterial breeding, aggravates the condition of patients, and compromises the repair effect. Smoking can significantly increase the contents of albumin, aspartate aminotransferase, and lactoferrin in the saliva of patients, which can easily affect the immune response of patients, foster the breeding of bacteria in the oral cavity of patients, affect the surgical effect, and lead to poor repair effects in patients.
It is worth mentioning that all surgical operations and examinations in this study were performed by the same two senior clinicians, but this may lead to risks of bias. In addition, due to the limitations of this study such as the small sample size, the results of this study should be further evaluated in future investigations.
Conclusion
Crown lengthening improves the periodontal condition of patients with maxillary anterior tooth loss, reduces gingival sulcus bleeding, and improves dental aesthetics and patient satisfaction. Further clinical studies are required prior to clinical promotion.
Disclosure of conflict of interest
None.
References
- 1.Marcantonio C, Nícoli LG, Pigossi SC, Araújo RFSB, Boeck EM, Junior EM. Use of alveolar distraction osteogenesis for anterior maxillary defect reconstruction. J Indian Soc Periodontol. 2019;23:381–386. doi: 10.4103/jisp.jisp_549_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zachrisson BU, Stenvik A, Haanaes HR. Management of missing maxillary anterior teeth with emphasis on autotransplantation. Am J Orthod Dentofacial Orthop. 2004;126:284–288. doi: 10.1016/S0889540604005244. [DOI] [PubMed] [Google Scholar]
- 3.Silva I, Suska F, Cardemil C, Rasmusson L. Stability after maxillary segmentation for correction of anterior open bite: a cohort study of 33 cases. J Craniomaxillofac Surg. 2013;41:e154–e158. doi: 10.1016/j.jcms.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 4.Pini NP, De-Marchi LM, Gribel BF, Pascotto RC. Digital analysis of anterior dental esthetic parameters in patients with bilateral maxillary lateral incisor agenesis. J Esthet Restor Dent. 2013;25:189–200. doi: 10.1111/jerd.12014. [DOI] [PubMed] [Google Scholar]
- 5.Spear FM, Kokich VG, Matthews DP. The esthetic management of a severe isolated periodontal defect in the maxillary anterior. Compend Contin Educ Dent. 2008;29:280–2. 284–87. [PubMed] [Google Scholar]
- 6.Marzadori M, Stefanini M, Sangiorgi M, Mounssif I, Monaco C, Zucchelli G. Crown lengthening and restorative procedures in the esthetic zone. Periodontol 2000. 2018;77:84–92. doi: 10.1111/prd.12208. [DOI] [PubMed] [Google Scholar]
- 7.Planciunas L, Puriene A, Mackeviciene G. Surgical lengthening of the clinical tooth crown. Stomatologija. 2006;8:88–95. [PubMed] [Google Scholar]
- 8.Wang C, Jia XT, Zhen M, Hu WJ, Zhang H, Chung KH. Success rate of fractured teeth receiving modified crown lengthening surgery and restorations. BMC Oral Health. 2022;22:99. doi: 10.1186/s12903-022-02143-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Creagh J, Bohner L, Sesma N, Coachman C. Digital approaches to facially guided orthodontic and periodontal rehabilitation in the anterior esthetic zone: a case report. J Esthet Restor Dent. 2022;34:226–234. doi: 10.1111/jerd.12860. [DOI] [PubMed] [Google Scholar]
- 10.Aroni MAT, Pigossi SC, Pichotano EC, de Oliveira GJPL, Marcantonio RAC. Esthetic crown lengthening in the treatment of gummy smile. Int J Esthet Dent. 2019;14:370–382. [PubMed] [Google Scholar]
- 11.Kalsi HJ, Bomfim DI, Hussain Z, Rodriguez JM, Darbar U. Crown lengthening surgery: an overview. Prim Dent J. 2020;8:48–53. doi: 10.1308/205016820828463870. [DOI] [PubMed] [Google Scholar]
- 12.Pilalas I, Tsalikis L, Tatakis DN. Pre-restorative crown lengthening surgery outcomes: a systematic review. J Clin Periodontol. 2016;43:1094–1108. doi: 10.1111/jcpe.12617. [DOI] [PubMed] [Google Scholar]
- 13.Hempton TJ, Dominici JT. Contemporary crown-lengthening therapy: a review. J Am Dent Assoc. 2010;141:647–655. doi: 10.14219/jada.archive.2010.0252. [DOI] [PubMed] [Google Scholar]
- 14.Silva Cunha JL, Barboza Santana AV, Alves da Mota Santana L, Meneses Santos D, de Souza Amorim K, Maciel de Almeida Souza L, Ferreira de Sousa S, de Albuquerque-Júnior RLC. Regional odontodysplasia affecting the maxilla. Head Neck Pathol. 2020;14:224–229. doi: 10.1007/s12105-019-01031-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahmed HM, Hashem AA. Accessory roots and root canals in human anterior teeth: a review and clinical considerations. Int Endod J. 2016;49:724–736. doi: 10.1111/iej.12508. [DOI] [PubMed] [Google Scholar]
- 16.Pini NP, de-Marchi LM, Gribel BF, Ubaldini AL, Pascotto RC. Analysis of the golden proportion and width/height ratios of maxillary anterior dentition in patients with lateral incisor agenesis. J Esthet Restor Dent. 2012;24:402–414. doi: 10.1111/j.1708-8240.2012.00533.x. [DOI] [PubMed] [Google Scholar]
- 17.Hamasni FM, Majzoub ZAK. Effect of patient- and surgery-related factors on supracrestal tissue reestablishment after crown lengthening procedure. Quintessence Int. 2019;50:792–801. doi: 10.3290/j.qi.a43152. [DOI] [PubMed] [Google Scholar]
- 18.Sheng Y, Guo HM, Bai YX, Li S. Dehiscence and fenestration in anterior teeth: comparison before and after orthodontic treatment. J Orofac Orthop. 2020;81:1–9. doi: 10.1007/s00056-019-00196-4. [DOI] [PubMed] [Google Scholar]
- 19.Levine DF, Handelsman M, Ravon NA. Crown lengthening surgery: a restorative-driven periodontal procedure. J Calif Dent Assoc. 1999;27:143–151. [PubMed] [Google Scholar]
- 20.Dawadi A, Humagain M, Sapkota B, Subba M, Neupane M, Lamichhane S. Crown lengthening surgery for enhancing restorative treatment in esthetic zone. Kathmandu Univ Med J (KUMJ) 2021;19:278–281. [PubMed] [Google Scholar]
- 21.Silva CO, Rezende RI, Mazuquini AC, Leal VC, Amaral GSA, Guo X, Tatakis DN. Aesthetic crown lengthening and lip repositioning surgery: pre- and post-operative assessment of smile attractiveness. J Clin Periodontol. 2021;48:826–833. doi: 10.1111/jcpe.13461. [DOI] [PubMed] [Google Scholar]


