Abstract
In this paper, a review of the literature was performed to critically evaluate relevant published research on diagnosis and treatment of Madelung’s deformity. Madelung’s deformity is a metaphyseal dysplasia of the distal radius, where the distal radial joint tilts to the volar and ulnar sides, combined with distal ulnar subluxation and elbow dislocation. The main pathogenic factors of this disease include idiopathic, hereditary and acquired factors. So far, it is believed that Madelung’s deformity is mainly associated with trauma, epiphyseal dysplasia, nutritional disorders, and gene deletion or mutation. It is more common in females, and is an autosomal dominant inheritance disease. Most patients suffer from this disease bilaterally. Madelung’s deformity may occur as a complication of Leri-Weill dyschondrosteosis. Most patients usually have no clinical symptoms in the early stage, and some patients come to the hospital due to wrist pain, stiffness, deformity and a shorter forearm. X-ray film is the main diagnostic method for this disease. Magnetic resonance imaging can show local soft tissue and bone abnormalities in the early stage, so it is used for the early diagnosis of this disease. The ulnar angle can be classified into different types based on the size of the distal radius palmar angle. For severe deformity and symptoms, surgical treatment is often required, including soft tissue release, distal radius osteotomy, ulnar shortening osteotomy, distal ulnar resection, and distal radioulnar joint fusion. Some procedures have better clinical results in relieving pain and improving mobility.
Keywords: Madelung’s deformity, Leri-Weill dyschondrosteosis, distal radioulnar joint, epidemiology, surgical treatment
Introduction
Madelung’s deformity is a rare deformity of the forearm and wrist, which was first described by Guillaume Dupuytren in 1834 [1]. In 1878, Otto Madelung discussed the pathological and anatomical changes and possible causes of this disease, and named this disease as Madelung’s deformity [2]. The term Manus valga was also proposed [3]. In 1929, Leri and Weill reported familial dwarfism characterized by short stature and Madelung’s deformity of the wrist [4], but this disease was not paid much attention on until the 1970s, with the imaging findings of Kozlowski et al. in 1971 describing it as chondroplasia [5-7]. Madelung’s deformity is a rare congenital malformation that occurs as a complication of Leri-Weill cartilage and osteogenesis disorders, it is hereditary in an autosomal dominant manner, females are more susceptible to this disease, with the incidence ratio of male to female of about 1:4, and most of patients suffer from bilateral onset [8]. Symptoms such as wrist pain and limited movement usually occur in older children or adolescents [2]. Madelung’s deformity is also commonly used to describe metaphyseal abnormalities of the distal radius caused by trauma, infection, dysplasia, Turner syndrome, or idiopathic causes, with progressive deformities of the distal ulna and wrist.
Pathological and anatomical features
The wrist joint is a composite joint composed of the radiocarpal joint, ulnar carpal joint, intercarpal joint and carpometacarpal joint, with flexion, extension, radial deviation, ulnar deviation and forearm rotation. The distal radioulnar joint is a complex part of the wrist, functionally. During hand and radius movements, weight bearing is transferred to the forearm via the distal ulna triangular fibrocartilage complex. Madelung’s deformity is characterized by dysplasia of the metaphyseal of the distal radius at the volar and ulnar sides. The distal joints of the radius are tilted toward the volar and ulnar sides, the radius is shortened and curved toward the volar and ulnar sides, the ulnar head protrudes dorsally, and the carpals are arranged in triangles [3,9,10], accompanied by a subluxation of the distal ulna and dislocation of the elbow. The hand is shifted to the volar and ulnar side relative to the wrist. The ulna is not involved and continues to grow lengthwise normally, with a prominent appearance. The distal radioulnar joint becomes unstable, and the carpal bone moves towards the palmar and proximal ends, resulting in limited movement, pain, and deformity [11]. It is mainly caused by stunted growth of the ulnar and palmar epiphyseal plates of the distal radius, and the asymmetric growth of the epiphyseal plates of the distal radius is the underlying cause of Madelung’s deformity. Although this disease is predominantly abnormal bones, ligament abnormalities are often associated with the disease progression. In 1992, Vickers and Nielsen described the Vickers ligament abnormalities accompanying Madelung’s deformity [12]. This abnormal volar radial lunate ligament could tie the lunate bone to the distal volar of the radius, resulting in lunate sinking and asymmetric growth of the distal epiphysis under pressure [12]. Ghatan believed that the volar radiolunate ligament aggravated the occurrence of the distal radius malformation [13]. Other researchers believed that Vickers ligament was a secondary change rather than the primary cause of the malformation, due to the formation of the thickened joint capsule formed that occupied the missing part of the lunate fossa on the palmar side [14].
Etiology and epidemiology
Madelung’s deformity is a rare disease with an unknown incidence. In 1977, Flatt reported more than 1400 patients with congenital upper limb abnormalities, of whom only 1.7% suffered from Madelung’s deformity [15]. Minor malformations may exist for years before clinical symptoms appear. It is more common in females, with a male to female ratio of 1:4 [8,16,17]. The clinical symptoms mostly appear before the age of 20 [8,18-20].
The specific etiological factors and pathogenesis of Madelung’s deformity is also still unknown. Leri-Weill cartilage and bone formation disorders are characterized by Madelung’s deformity and may also be associated with proximal radius, tibia, and fibula malformations. Leri-weill syndrome is an autosomal dominant inheritance disease [21], while idiopathic Madelung’s deformity is sporadic. SHOX gene was first reported to be associated with idiopathic short stature and Turner syndrome in 1997 [22]. Shortly thereafter, SHOX gene point mutations were found in a family with Leri-Weill achondroplasia [23,24]. Hirschfcldova et al. believed that exon 6 mutation of GNAS gene was also closely associated with this disease [25-27]. Shahcherachi et al. [28] found that achondroplasia, hereditary multiple exogenous warts and Ollier’s disease were also caused by genetic changes, and local tumor growth destroying local epiphysis or cartilage growth plates could also cause malformations. Although current studies have demonstrated that changes in genes such as SHOX and GNAS affect changes of hormone levels in the body, resulting in uneven bone growth and deformity in the corresponding parts with further bone growth and maturation, it has not been confirmed which gene loci and what changes cause such deformities.
Clinical manifestations
The deformity is not obvious when the patient is young, and the clinical symptoms are more common in older children. After growth and development stopped, the deformity is no longer aggravated. Clinical manifestations included palmar inclination of the wrist, ulnar deviation deformity, limited wrist joint activity with loss of dorsiflexion activity, wrist pain, and abnormal protrusion of ulnar head, combined with distal radioulnar joint subluxation, elbow joint dislocation or palmar wrist joint dislocation, and limited forearm rotation function in severe cases. Most patients have no clinical symptoms in the early stage, and some patients experience wrist pain, stiffness, and deformity. Leri-Weill achondroplasia should be suspected if short stature and bilateral wrist malformations are present in patients [29].
Imaging examination
X-ray
The diagnosis of Madelung’s deformity is mainly based on X-ray film. The pathologic changes are not obvious in the early stage of this disease, and it is easy to diagnose in the middle and late stage because of definite clinical signs. Anteroposteric radiographs showed shorter radius, increased oblique angle of distal articular surface, loss and narrowing of distal ulnar epiphyseal plate of radius, widening gap of the distal radioulnar joint, and inverted triangle arrangement of proximal carpus. Lateral radiographs showed subluxation of the distal radioulnar joint with the dorsal subluxation of the ulnar head and radius bending to the palmar side (Figure 1A and 1B).
Figure 1.

Anteroposteric radiograph in (A) and lateral radiograph in (B) showing oblique angle of distal articular surface, subluxation of the distal radioulnar joint.
At present, imaging studies tend to establish measurement indicators and diagnostic criteria for deformities in the early stage of Madelung’s deformity. In healthy people, the distal articular angle of the ulnar and radius is 150° and the carpal angle is 131.5°. In the Madelung’s deformity patients, the articular surface angle and carpal angle of the distal ulnar and radius became smaller or even acute. Mc-Carroll et al. [30] identified four imaging parameters for Madelung’s deformity, including ulnar tilt, lunate sinking, lunate fossa angle, and palmarcarpal displacement. Ulnar tilt, defined on anteroposterior radiographs as an acute angle between the longitudinal axis of the ulna and the tangents of the proximal scaphoid and lunate bones. Lunate sinking, defined on orthographic radiographs as the distance, in millimeters, between the nearest point of the lunate and the line perpendicular to the longitudinal axis of the ulna and passing through the articular surface of the distal ulna. The lunate fossa angle is defined as the acute angle between the longitudinal axis of the ulna and the radial lunate fossa on orthographic radiographs. Palmar carpal displacement, defined on lateral radiographs as the distance in millimeters between the farthest point of the palmar lunate or cephalic bone perpendicular to the longitudinal axis of the ulna. Ulnar tilt lunate sinking and palmarcarpal displacement are reliable and repeatable radiographic measurements of the severity of Madelung’s deformity. McCarroll et al. proposed the criteria for early diagnosis: lunate sinking ≥4 mm, lunate fossa Angle ≥40°, ulnar tilt ≥33°, palmarcarpal displacement ≥20 mm; when any of these measurements are greater than or equal to the critical value, Madelung’s deformity may be diagnosed, and the lunate fossa angle is particularly useful for early diagnosis [31,32]. Ghatan verified these measurement parameters with high observer consistency, and believed they could be used for early diagnosis of Madelung malformation by clinicians [13].
Magnetic resonance imaging (MRI)
MRI can clearly show triangular-fibrous cartilage complex (TFCC), Vickers ligament and hypoulnar joint injury which can be used as an effective auxiliary examination (Figure 2). Stehling performed MRI examination on patients with Madelung’s deformity and confirmed the existence of Vickers ligament and abnormal thickening of the volar radiolunate ligament [33]. There is no objective criterion for the diagnostic value of MRI in this disease. Vickers and Nielsen advocated the use of MRI, suggesting that early identification of the thickened palmar radioular lunate (Vickers) ligaments could be used for preventive resection [12]. Other studies confirmed abnormal thickening of the Vickers ligament and the palmar deltoid ligament [34,35]. Farr et al. reported that MRI was a good but not completely reliable examination method, and Vickers ligaments are present in most cases of Madelung’s deformity, but not in all cases [36]. The clinical value of MRI in patients with Madelung’s deformity has not been rigorously evaluated and is not a routine examination at present.
Figure 2.

MRI showing triangular-fibrous cartilage complex (TFCC) injury.
Treatment
Non-surgical treatment
The natural history of Madelung’s deformity is rarely reported, and patients may remain asymptomatic into adulthood. As the disease progresses, instability of the radioulnar joint, radiocarpal arthritis, and ulnar deformity may eventually occur. Treatment for these symptoms remains controversial. Nonsurgical treatments include non-steroidal anti-inflammatory drugs (NSAIDs) and immobilization. Pratyush reported a 19-year-old patient, who experienced pain, deformity, and limited movement for 5 years, received small splint immobilization and NSAIDs for analgesia, and had pain and symptoms relief after 6 months of follow-up [37]. In a long-term follow-up of a group of patients with immature bone development, Nielsen found that most patients experienced relief from pain and other symptoms 10 years later, suggesting that surgery should be postponed until bone maturity, but the natural history of untreated Madelung’s deformity is unknown due to the lack of long-term prospective case-control studies [18].
For patients with severe deformity and obvious symptoms, the wear and tear of extensor tendon is a non-operative complication, which is mainly caused by repeated friction stimulation of extensor finger tendon in dorsal subluxation of ulnar head. The extensor tendon of the ulnar finger is often involved. Ducloyer reported 6 cases of spontaneous digitor-extensor tendon rupture in patients with Madelung’s deformity, suggesting that early surgical treatment might avoid the occurrence of this complication [32].
Surgical treatment
Surgery should be considered for patients with severe deformities or persistent pain and limited movement. Limited movement of the wrist is usually characterized by wrist ulnar deviation and limited dorsiflexion. The extent of rotation is still debated, and Roderick reported that compared to supination, pronation movement is significantly limited in patients with Madelung’s deformity [38].
There is no consensus on the surgical indication of Madelung’s deformity. Dos Reis reported 18 patients with Madelung’s deformity received osteotomy for correction, and 14 patients were mainly treated with wrist deformity [39]. JeanMichel believed that wrist pain and limited movement were basic surgical indications [40]. There are a variety of surgical methods, some of which can relieve postoperative pain, improve the range of movement, and achieve better clinical results. However, a large sample of long-term follow-up results is still needed as evidence.
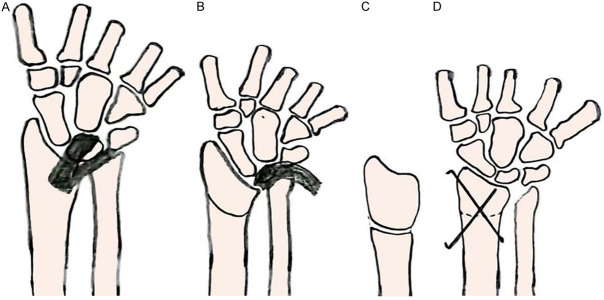
Ligament release
Vickers identified two significant pathologic changes in the Madelung’s deformity, namely, growth inhibition of the epiphyseal plate of the distal radius, resulting in volar and ulnar arcuate alteration of the distal radius, and the presence of Vickers ligaments. Vickers ligament may tie the lunate to the volar side of the distal radius, exacerbating the distal radial deformity. Vickers recommended that both lesions should be removed through a volar transverse incision. Resection was performed at the bridge of the distal radius epiphyseal plate to prevent the reconstruction of the bridge, and Vickers ligament was also excised [12] (Figure 3A, 3B).
Figure 3.
Vickers ligament was excised in picture (A and B), Distal radius fornix osteotomy and fixcationg in picture (B-D).
The effect of early prophylactic Vickers ligamentectomy in children with mild skeletal immaturity is unclear. Ghatan suggested combined ulna shortening or distal ulna epiphyseal block and Vickers ligamentectomy for mild Madelung’s deformity [13]. Ulnar shortening may relieve the symptoms of ulnar dorsal subluxation. Vickers ligament release ease the pain and improved lunate sinking [41].
Distal radius fornix osteotomy combined with ligament release
Vicker’s ligamentectomy significantly relieved wrist pain and improved wrist range of motion, but did not alter the remaining wrist deformity. For severe Madelung’s deformity, distal radius osteotomy combined with ligamentectomy was performed (Figure 3B-D). A retrospective analysis of patients with severe Madelung’s deformity was conducted, and distal radius osteotomy combined with ligament release resulted in the relief of malformation and wrist range of motion and pain [42].
Ulnar and radius osteotomy combined with distal radioulnar arthroplasty
Radioulnar arthroplasty was performed to correct the distal radius deformity and to fix the unstable and painful radioulnar joint. Closed or open wedge osteotomy may be performed. It was reported that the combination of ulnar shortening osteotomy and distal radius osteotomy was used to treat severe Madelung’s deformity of adolescent patients, and postoperative follow-up showed that the malformation was eliminated, pain was alleviated and joint functions were improved [43] (Figure 4A, 4B). Schroven et al. [44] suggested that radioulnar osteoplasty with ulnar head preservation could stabilize the radioulnar joint, preserve the structure of the radiocarpal joint, and avoid progressive aggravation of ulnar head subluxation. Sauve-Kapandji (SK) surgery combined with distal radioulnar arthrodesis and the creation of a prosthetic radioulnar joint was used to save radioulnar instability or arthritis and improve partial wrist joint function [45] (Figure 5).
Figure 4.

Ulnar shortening osteotomy and distal radius osteotomy in anteroposteric view (A) and lateral view (B).
Figure 5.

Sauve-Kapandji (SK) surgery.
Radial osteotomy
Radial osteotomy alone can also be used to correct the malformation characterized by the volar and ulnar angulation of the distal radius. A previous study reported that after radial osteotomy, all malformations were corrected, distal ulnar joint was stable, the mobility of wrist joint improved, and no adverse complications happened during postoperative follow-up [46]. Michae et al. [47] reported 11 patients, of whom 8 underwent a simple radial open wedge osteotomy to correct the inherent deformity of the radius and improve the radioulnar joint chimerism.
Ulnar osteotomy
Pain in patients with Madelung’s deformity is mainly caused by dorsal protrusion of the ulnar head and ulnar carpal joint abnormalities. Researchers suggest distal ulnar resection for adult patients with epiphyseal growth and development stopping and ulnar inclination of distal radius >45°. Bruno reported symptomatic patients with Madelung’s deformity treated by simple ulnar shortening, in which there were only mild bone malformation and ulnar joint symptoms caused by dorsal ulnar subluxation, and the patients’ bones were mature at the time of treatment [38].
The main indications for Madelung’s deformity are wrist pain and limited movement. For growing children without symptoms, regular check-ups are required. Patients with unstable osteoarthritis of the radioulnar joint and malformed carpal ulnar joint require surgical intervention once their deformity worsens progressively. For patients with unclosed epiphyseal plates, ligamentolysis combined with osteotomy might be used. If the ulnar length is normal, a radial osteotomy combined with ulnar epiphyseal fixation is performed. If the ulna is too long, ulnar shortening should be performed.
Problems and prospects
Plain radiographs are used to diagnose Madelung’s deformity. As the disease develops into the middle and late stages, characteristic changes occur. Three-dimensional (3D) CT can visually display the spatial position relationship between radius and ulna, as well as the three-dimensional changes of wrist deformity, which is helpful to design the osteotomy plane and angle before surgery. However, most patients first see a doctor in adolescence when it is difficult to use CT for diagnosis due to high doses of radiation. MRI can show abnormalities of ligaments and epiphysis, which is easy for early diagnosis, but there is no clear evaluation index at present. In the future, EOS imaging could aid diagnosis by providing more detailed images of malformations while effectively reducing radiation exposure.
There is no unified surgical method for Madelung’s deformity. Both radial and ulnar ostetomy and ligament ectomy can improve the clinical symptoms, but with intraoperative vascular and nerve damage, and postoperative infection risk. Therefore, it is imperative to seek minimally invasive and precise treatment, and 3D printed models and computer navigation technology used to guide personalized surgery might shorten the operation time, reduce blood loss and improve the success rate of surgery. Future research should focus on etiology, objective assessment, and development of treatment guidelines.
Disclosure of conflict of interest
None.
References
- 1.Leçons Orales de Clinique Chirurgicale, faites à l’Hôtel Dieu de Paris. Med Chir Rev. 1834;21:289–330. [PMC free article] [PubMed] [Google Scholar]
- 2.Madelung O. Die spontane subluxation de hand nach vorne. Verhandlungen der deutschen Gesellschaft fur Chirurgie. 1878;7:259–276. [Google Scholar]
- 3.Arora AS, Chung KC. Otto W. Madelung and the recognition of Madelung’s deformity. J Hand Surg Am. 2006;31:177–182. doi: 10.1016/j.jhsa.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 4.Leri A, Weill JA. Une affection congénitale et symétrique du développement osseux: La dyschondrostéose. Bull Mem Soc Med Hop Paris. 1929;53:1491–1494. [Google Scholar]
- 5.Kozlowski K, Zychowicz C. Dyschondrosteosis. Acta Radiol Diagn (Stockh) 1971;11:459–466. doi: 10.1177/028418517101100502. [DOI] [PubMed] [Google Scholar]
- 6.Silverman FN. Mesomelic dwarfism. In: Kaufmann HJ, editor. Progress in Pediatric Radiology. Basel: Karger; 1973. p. 546. [Google Scholar]
- 7.Weerakkody Y, Gaillard AF. Madelung deformity: musculoskeletal, paediatrics, radiopaedia. Accessed from: https://radiopaedia.org/articles/madelung-deformity.
- 8.Anton JI, Reitz GB, Spiegel MB. Madelung’s deformity. Ann Surg. 1938;108:411–439. doi: 10.1097/00000658-193809000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harley BJ, Carter PR, Ezaki M. Volar surgical correction of Madelung’s deformity. Tech Hand Up Extrem Surg. 2002;6:30–35. doi: 10.1097/00130911-200203000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Canale ST. Campbell’s Operative Orthopedics. 10th ed. St. Louis: Mosby; 2002. Madelung deformity; p. 76. [Google Scholar]
- 11.Waters PM, Bae DS. Pediatric hand and upper limb surgery: a practical guide. Philadelphia: Wolters Kluwer Health; 2012. [Google Scholar]
- 12.Vickers D, Nielsen G. Madelung deformity: surgical prophylaxis (physiolysis) during the late growth period by resection of the dyschondrosteosis lesion. J Hand Surg Br. 1992;17:401–407. doi: 10.1016/s0266-7681(05)80262-1. [DOI] [PubMed] [Google Scholar]
- 13.Ghatan AC, Hanel DP. Madelung deformity. J Am Acad Orthop Surg. 2013;21:372–382. doi: 10.5435/JAAOS-21-06-372. [DOI] [PubMed] [Google Scholar]
- 14.Munns C, Glass I. SHOX-related haploinsuffi ciency disorders. In: Pagon R, Bird T, Dolan C, editors. Gene reviews. Seattle: University of Washington; 2005. [Google Scholar]
- 15.Flatt AE. The congenital hand anomalies. St. Louis: CV Mosby; 1977. p. 50. [Google Scholar]
- 16.Kelikian H. Congenital deformities of the hand and forearm. Philadelphia, PA: Saunders; 1974. [Google Scholar]
- 17.Ross JL, Scott C Jr, Marttila P, Kowal K, Nass A, Papenhausen P, Abboudi J, Osterman L, Kushner H, Carter P, Ezaki M, Elder F, Wei F, Chen H, Zinn AR. Phenotypes associated with SHOX deficiency. J Clin Endocrinol Metab. 2001;86:5674–5680. doi: 10.1210/jcem.86.12.8125. [DOI] [PubMed] [Google Scholar]
- 18.Nielsen JB. Madelung’s deformity. A follow-up study of 26 cases and a review of the literature. Acta Orthop Scand. 1977;48:379–384. doi: 10.3109/17453677708992012. [DOI] [PubMed] [Google Scholar]
- 19.Schmidt-Rohlfing B, Schwöbel B, Pauschert R, Niethard FU. Madelung deformity: clinical features, therapy and results. J Pediatr Orthop B. 2001;10:344–348. [PubMed] [Google Scholar]
- 20.Green DP, Hotchkiss RN, Pederson WC, Wolfe SW. Green’s Operative Hand Surgery, 5th ed. Philadelphia, PA: Elsevier; 2005. Deformities of the wrist and forearm; pp. 1484–1491. [Google Scholar]
- 21.Roubicek M, Arriazu MC, Isaac G. SHOX deficiency phenotypes. J Clin Endocrinol Metab. 2003;88:4004. doi: 10.1210/jc.2002-020285. [DOI] [PubMed] [Google Scholar]
- 22.Rao E, Weiss B, Fukami M, Rump A, Niesler B, Mertz A, Muroya K, Binder G, Kirsch S, Winkelmann M, Nordsiek G, Heinrich U, Breuning MH, Ranke MB, Rosenthal A, Ogata T, Rappold GA. Pseudoautosomal deletions encompassing a novel homeobox gene cause growth failure in idiopathic short stature and Turner syndrome. Nat Genet. 1997;16:54–63. doi: 10.1038/ng0597-54. [DOI] [PubMed] [Google Scholar]
- 23.Belin V, Cusin V, Viot G, Girlich D, Toutain A, Moncla A, Vekemans M, Le Merrer M, Munnich A, Cormier-Daire V. SHOX mutations in dyschondrosteosis (Leri-Weill syndrome) Nat Genet. 1998;19:67–69. doi: 10.1038/ng0198-67. [DOI] [PubMed] [Google Scholar]
- 24.Shears DJ, Vassal HJ, Goodman FR, Palmer RW, Reardon W, Superti-Furga A, Scambler PJ, Winter RM. Mutation and deletion of the pseudoautosomal gene SHOX cause Leri-Weill dyschondrosteosis. Nat Genet. 1998;19:70–73. doi: 10.1038/ng0198-70. [DOI] [PubMed] [Google Scholar]
- 25.Hirschfeldova K, Solc R, Baxova A, Zapletalova J, Kebrdlova V, Gaillyova R, Prasilova S, Soukalova J, Mihalova R, Lnenicka P, Florianova M, Stekrova J. SHOX gene defects and selected dysmorphic signs in patients of idiopathic short stature and Léri-Weill dyschondrosteosis. Gene. 2012;491:123–127. doi: 10.1016/j.gene.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 26.Rump P, Jongbloed JD, Sikkema-Raddatz B, Mundlos S, Klopocki E, van der Luijt RB. Madelung deformity in a girl with a novel and de novo mutation in the GNAS gene. Am J Med Genet A. 2011;155A:2566–2570. doi: 10.1002/ajmg.a.34218. [DOI] [PubMed] [Google Scholar]
- 27.Sanchez J, Perera E, Jan de Beur S, Ding C, Dang A, Berkovitz GD, Levine MA. Madelung-like deformity in pseudohypoparathyroidism type 1b. J Clin Endocrinol Metab. 2011;96:E1507–1511. doi: 10.1210/jc.2011-1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shahcheraghi GH, Peyman M, Mozafarian K. Madelung deformity and extensor tendon rupture. Am J Orthop (Belle Mead NJ) 2015;44:E242–244. [PubMed] [Google Scholar]
- 29.Kozin SH, Zlotolow DA. Madelung deformity. J Hand Surg Am. 2015;40:2090–2098. doi: 10.1016/j.jhsa.2015.03.033. [DOI] [PubMed] [Google Scholar]
- 30.Fagg PS. Reverse Madelung’s deformity with nerve compression. J Hand Surg Br. 1988;13:23–27. doi: 10.1016/0266-7681_88_90045-9. [DOI] [PubMed] [Google Scholar]
- 31.McCarroll HR Jr, James MA, Newmeyer WL 3rd, Manske PR. Madelung’s deformity: diagnostic thresholds of radiographic measurements. J Hand Surg Am. 2010;35:807–812. doi: 10.1016/j.jhsa.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 32.Ducloyer P, Leclercq C, Lisfranc R, Saffar P. Spontaneous ruptures of the extensor tendons of the fingers in Madelung’s deformity. J Hand Surg Br. 1991;16:329–333. doi: 10.1016/0266-7681(91)90064-u. [DOI] [PubMed] [Google Scholar]
- 33.Stehling C, Langer M, Nassenstein I, Bachmann R, Heindel W, Vieth V. High resolution 3.0 Tesla MR imaging findings in patients with bilateral Madelung’s deformity. Surg Radiol Anat. 2009;31:551–557. doi: 10.1007/s00276-009-0476-0. [DOI] [PubMed] [Google Scholar]
- 34.Jebson PJ, Blair WF. Bilateral spontaneous extensor tendon ruptures in Madelung’s deformity. J Hand Surg Am. 1992;17:277–280. doi: 10.1016/0363-5023(92)90405-e. [DOI] [PubMed] [Google Scholar]
- 35.McCarroll HR Jr, James MA, Newmeyer WL 3rd, Molitor F, Manske PR. Madelung’s deformity: quantitative assessment of x-ray deformity. J Hand Surg Am. 2005;30:1211–1220. doi: 10.1016/j.jhsa.2005.06.024. [DOI] [PubMed] [Google Scholar]
- 36.Farr S, Martínez-Alvarez S, Little KJ, Henstenburg J, Ristl R, Stauffer A, Soldado F, Zlotolow DA. The prevalence of Vickers’ ligament in Madelung’s deformity: a retrospective multicentre study of 75 surgical cases. J Hand Surg Eur Vol. 2021;46:384–390. doi: 10.1177/1753193420981522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shahi P, Sudan A, Sehgal A, Meher D, Meena U. Madelung deformity of the wrist managed conservatively. Cureus. 2020;12:e8225. doi: 10.7759/cureus.8225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bruno RJ, Blank JE, Ruby LK, Cassidy C, Cohen G, Bergfield TG. Treatment of Madelung’s deformity in adults by ulna reduction osteotomy. J Hand Surg Am. 2003;28:421–426. doi: 10.1053/jhsu.2003.50073. [DOI] [PubMed] [Google Scholar]
- 39.dos Reis FB, Katchburian MV, Faloppa F, Albertoni WM, Laredo Filho J Jr. Osteotomy of the radius and ulna for the Madelung deformity. J Bone Joint Surg Br. 1998;80:817–824. doi: 10.1302/0301-620x.80b5.8691. [DOI] [PubMed] [Google Scholar]
- 40.Laffosse JM, Abid A, Accadbled F, Knör G, Sales de Gauzy J, Cahuzac JP. Surgical correction of Madelung’s deformity by combined corrective radioulnar osteotomy: 14 cases with four-year minimum follow-up. Int Orthop. 2009;33:1655–1661. doi: 10.1007/s00264-008-0711-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Del Core M, Beckwith T, Phillips L, Ezaki M, Stutz C, Oishi SN. Long-term outcomes following vickers ligament release and growth modulation for the treatment of Madelung deformity. J Pediatr Orthop. 2020;40:e306–e311. doi: 10.1097/BPO.0000000000001504. [DOI] [PubMed] [Google Scholar]
- 42.Leti Acciaro A, Garagnani L, Lando M, Lana D, Sartini S, Adani R. Modified dome osteotomy and anterior locking plate fixation for distal radius variant of Madelung deformity: a retrospective study. J Plast Surg Hand Surg. 2022;56:121–126. doi: 10.1080/2000656X.2021.1934845. [DOI] [PubMed] [Google Scholar]
- 43.Bebing M, de Courtivron B, Pannier S, Journeau P, Fitoussi F, Morin C, Violas P. Madelung’s deformity in children: clinical and radiological results from a French national multicentre retrospective study. Orthop Traumatol Surg Res. 2020;106:1339–1343. doi: 10.1016/j.otsr.2020.03.036. [DOI] [PubMed] [Google Scholar]
- 44.Schroven I, De Smet L, Zachee B, Steenwerckx A, Fabry G. Radial osteotomy and Sauvé-Kapandji procedure for deformities of the distal radius. Acta Orthop Belg. 1995;61:1–5. [PubMed] [Google Scholar]
- 45.Giberson-Chen CC, Leland HA, Benavent KA, Harper CM, Earp BE, Rozental TD. Functional outcomes after Sauve-Kapandji arthrodesis. J Hand Surg Am. 2020;45:408–416. doi: 10.1016/j.jhsa.2019.11.014. [DOI] [PubMed] [Google Scholar]
- 46.Saffar P, Badina A. Treatment of Madelung’s deformity. Chir Main. 2015;34:279–285. doi: 10.1016/j.main.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 47.Murphy MS, Linscheid RL, Dobyns JH, Peterson HA. Radial opening wedge osteotomy in Madelung’s deformity. J Hand Surg Am. 1996;21:1035–1044. doi: 10.1016/S0363-5023(96)80312-1. [DOI] [PubMed] [Google Scholar]