Abstract
Background:
Traumatic pseudoaneurysms are rare but have a high mortality rate; therefore, immediate diagnosis is vital. Most pseudoaneurysms are in the internal carotid artery or peripheral arteries, while proximal middle cerebral artery pseudoaneurysms have rarely been reported. We present a case of ruptured traumatic pseudoaneurysm located at the M1-M2 bifurcation.
Case Description:
A 42-year-old man was injured in a motorcycle accident and his Glasgow coma scale score on admission was 7 (Eye opening1, Verbal response2, Motor response4 [E1V2M4]). Head computed tomography (CT) showed thick subarachnoid hemorrhage (SAH). We suspected a ruptured aneurysm, but three-dimensional CT angiography (3D-CTA) did not detect any vascular defects. Head magnetic resonance angiography showed progressive right M1 stenosis suggesting arterial dissection. 3D-CTA on day 20 showed a small aneurysm in the proximal portion of the M2. Although surgery was scheduled for day 26, suddenly left hemiparesis appeared on day 24. Head CT detected fresh SAH and emergency surgery was performed on day 25. We dissected around the ruptured point under M1 temporary occlusion with superficial temporal artery-M2 assist bypass. Contrary to our expectations, there was only a small laceration in the right M2 superior trunk. We trapped the laceration and the proximal portion of the M2 superior trunk while preserving antegrade blood flow from the M1 to the M2 inferior trunk. On the 5-month follow-up, the patient was able to walk independently.
Conclusion:
Unreasonably thick traumatic SAH or spastic stenosis after head injury may indicate a traumatic pseudoaneurysm and require repeated neurovascular evaluation. If a pseudoaneurysm is detected, immediate surgical intervention is mandatory.
Keywords: Bypass, Middle cerebral artery, Trapping surgery, Traumatic aneurysm

INTRODUCTION
Traumatic pseudoaneurysms are rare, which accounting for <1% of cerebral aneurysms, but have a high mortality rate.[5] Therefore, immediate diagnosis and subsequent surgical treatment are essential. However, early diagnosis is difficult before a devastating hemorrhage.[5] Most traumatic pseudoaneurysms are located in the internal carotid artery (ICA) or peripheral arteries, while proximal middle cerebral artery (MCA) pseudoaneurysms are very rare.[5,7,13] We present a case of ruptured traumatic pseudoaneurysm located at the M1-M2 bifurcation treated with bypass-assisted trapping surgery and we review the relevant literature.
CASE DESCRIPTION
History and diagnosis
Written informed consent for the publication of data and any related images was obtained from the patient.
A 42-year-old man was admitted to our hospital due to multiple injury sustained in a motorcycle accident. The Glasgow coma scale (GCS) score on admission was 7 (E1V2M4). Head computed tomography (CT) revealed thick subarachnoid hemorrhage (SAH) in the right Sylvian fissure [Figure 1a]. We initially considered the possibility of a ruptured aneurysm that caused consciousness disturbance before the accident rather than traumatic SAH caused by the accident. Therefore, we performed head CT angiography (CTA), but no suspicious vascular lesions were detected [Figure 1b]. Thoracic CT showed bilateral pneumothorax, lung contusion, multiple limb fractures, right hemothorax, and sternal fracture. The intensivist intubated the patient under sedation and performed thoracic drainage. Due to findings of pneumonia, antibiotics (sulbactam/ampicillin 2 g/day, i.v.) were administered for 12 days. On day 5, the patient was extubated, but his disturbance of consciousness persisted (GCS score=13, E3V4M6).
Figure 1:
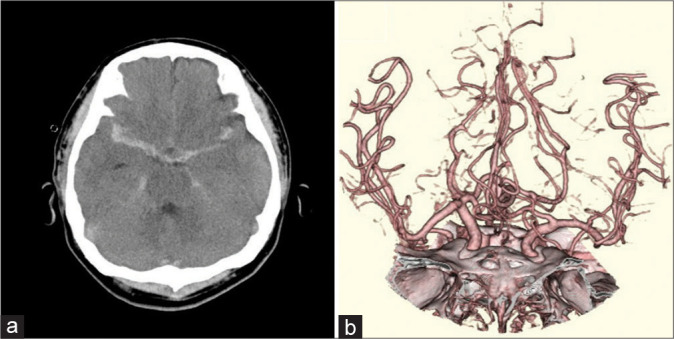
Initial imaging findings. (a) Axial computed tomography image showing thick traumatic subarachnoid hemorrhage. (b) Computed tomography angiography image showing no suspicious vascular abnormalities.
Follow-up head magnetic resonance imaging (MRI) and diffusion-weighted imaging performed on day 7 showed small high-intensity areas in the bilateral hemispheres and corpus callosum, indicating diffuse axonal injury. Head magnetic resonance angiography (MRA) showed stenosis of the right M1 portion, suggesting traumatic SAH-induced vasospasm [Figure 2a]. However, we also considered the possibility of a dissecting lesion. We continued intensive care with medical treatment and conservative therapy for the diffuse axonal injury. In addition, we administered extracellular fluid to prevent ischemic complications due to cerebral vasospasm, but we did not administer antiplatelet therapy due to the possibility of MCA dissection.
Figure 2:
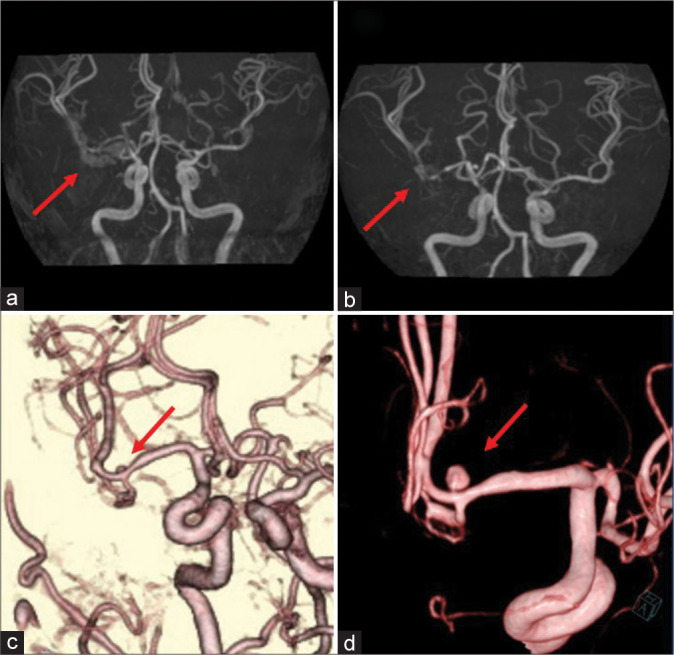
Follow-up preoperative imaging findings. (a) Magnetic resonance angiography image obtained on day 7 showing mild stenosis of the right M1 portion (arrow). (b) Follow-up magnetic resonance angiography image obtained on day 13 showing progression of the stenosis from M1 to the M1-M2 bifurcation (arrow). (c) Three-dimensional computed tomography angiography image obtained on day 20 showing a small 2.5-mm saccular aneurysm on the superior wall of the M2 superior trunk (arrow). (d) Three-dimensional digital subtraction angiography image obtained on day 23 showing enlargement of the saccular aneurysm (arrow).
On day 13, we performed follow-up MRA, which showed stenosis of the M1 portion extending to the M1-M2 bifurcation [Figure 2b]. Although the primary SAH was diffuse, the stenosis was limited to the right MCA. Therefore, we suspected MCA dissection and performed three-dimensional CTA on day 20, which revealed a small 2.5-mm saccular aneurysm on the superior wall of the M2 superior trunk [Figure 2c]. This suggested that the thick SAH was caused by a right MCA dissecting aneurysm. On digital subtraction angiography (DSA) performed on day 23, the maximal aneurysm diameter was 3.6 mm [Figure 2d].
Surgical treatment was scheduled for day 26; however, the patient suddenly developed left hemiparesis on day 24. Head CT detected fresh SAH around the right Sylvian fissure. We suspected pseudoaneurysm rupture; therefore, we sedated and intubated the patient. Emergency surgery was performed on day 25.
Surgical strategy and treatment
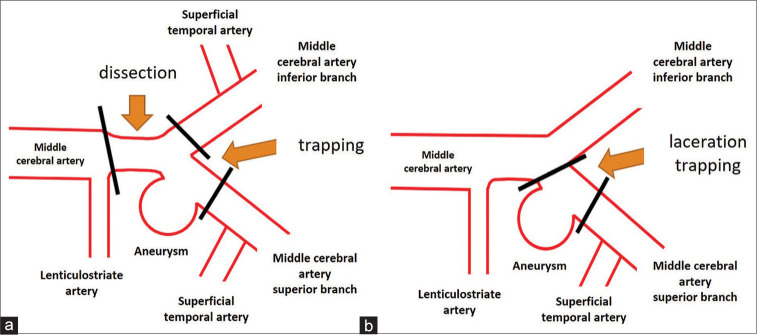
The actual length of the dissecting lesion was uncertain, but we suspected that the stenosis from the right M1 portion to the M1-M2 bifurcation reflected the dissecting lesion and that the left hemiparesis was induced by lenticulostriate artery (LSA) thrombosis caused by M1 dissection. Based on this, we considered M1-M2 trapping and vascular reconstruction. Fortunately, the frontal and parietal branches of the right superficial temporal artery (STA) were well-developed and double-barrel low-flow bypass seemed to be sufficient for reconstruction of the M2 lesion. Hence, we decided to perform M1-M2 trapping surgery assisted by an STA-MCA double-barrel bypass [Figures 3a and 3b].
Figure 3:
Schematic presentation of the planned and the actual surgical strategies. (a) Preoperatively, middle cerebral artery M1-M2 trapping surgery assisted by superficial temporal artery-middle cerebral artery double-barrel bypass was planned. (b) As the laceration was limited to the superior wall of the M2 superior trunk, M2 clipping was performed assisted by superficial temporary artery-M2 superior trunk bypass to trap the lacerated point and preserve antegrade blood flow from M1 to the M2 inferior trunk. Despite the mild stenosis at the origin of the M2 inferior trunk, superficial temporal artery-M2 inferior trunk bypass was not performed.
Surgery was performed under general anesthesia with monitoring of somatosensory and motor evoked potentials of the extremities. Both STA branches were harvested and frontotemporal craniotomy was performed in the usual fashion. When we removed the cranial bone, we found a hard bony process attached the surface of the dura mater along the middle meningeal artery [Figure 4a]. We elevated the right frontal lobe, evacuated the cerebrospinal fluid from the carotid cistern, and secured the right ICA. Next, we dissected the distal Sylvian fissure and secured the M2 superior and inferior trunks. We found a fibrin clot on the proximal portion of the M2 superior trunk, suggesting the rupture point. Therefore, we dissected the proximal Sylvian fissure from the terminal ICA to the distal M1. Contrary to our expectation, we found no obvious M1 dissection. Since the fibrin clot we observed was located on the superior wall of the M2 superior trunk, we decided to perform a STA-M2 (superior trunk) bypass before identifying the rupture point and selected the frontal branch as the donor artery. After completion of the STA-M2 bypass, we performed dissection around the rupture point. LSAs were found behind M1 and preserved. We removed the clot at the rupture point under M1 temporary occlusion and a small laceration of approximately 10-mm was revealed along the superior wall of the M2 superior trunk [Figure 4b], which indicated that the aneurysm was a pseudoaneurysm. We attempted to trap the lacerated point to preserve antegrade blood flow from M1 to the M2 inferior trunk and to avoid LSA thrombosis due to distal M1 blind allay. Although the origin of the M2 inferior trunk was slightly stenosed, only a proximal M2 clip was performed, and the lacerated point was trapped with titanium clips [Figures 3b and 4c]. Indocyanine green video angiography showed perfect patency of the STA-M2 bypass, antegrade blood flow from the M1 to the M2 inferior trunk, and LSA [Figure 4d].
Figure 4:
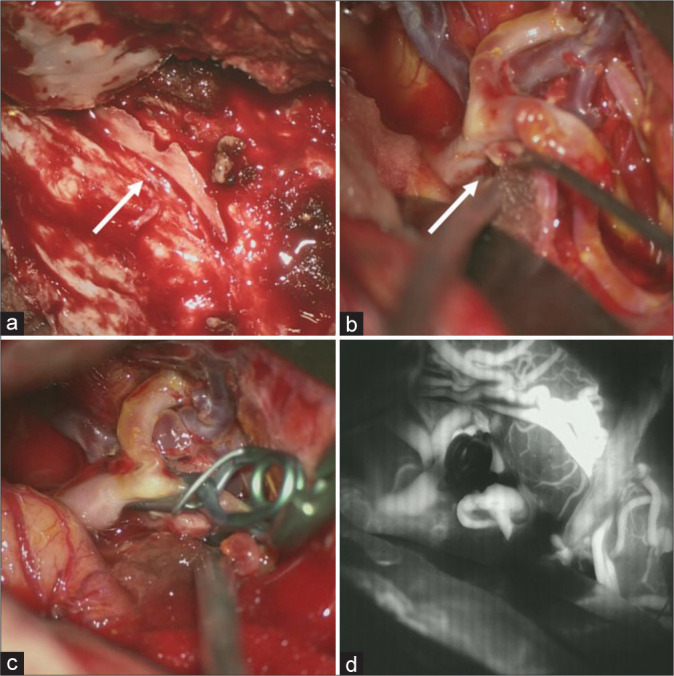
Intraoperative findings. (a) A hard bony process is seen (arrow) attached on the surface of the dura matter along the middle meningeal artery. (b) A small laceration on the superior wall of the M2 superior trunk is observed, indicating pseudoaneurysm (arrow). (c) Trapping of the laceration point with preservation of antegrade blood flow from M1 to the M2 inferior trunk assisted by superficial temporal artery-M2 (superior trunk) bypass, despite the mild stenosis of the origin of the M2 inferior trunk. (d) Indocyanine green video angiography image showing perfect patency of the superficial temporal artery-M2 bypass, antegraded blood flow from M1 to the M2 inferior trunk and complete obliteration of the laceration on the M2 superior trunk.
Postoperative course
We administered antiplatelet therapy with ozagrel sodium (80 mg/day), edaravone (60 mg/day), fasudil hydrochloride hydrate (90 mg/day), and cilostazol (200 mg/day) for 2 weeks. Follow-up head MRI/A on day 39 showed no additional infarctions. Postoperative DSA on day 56 showed excellent bypass patency with a mild stenotic lesion at the M1-M2 bifurcation and M2 inferior trunk [Figure 5]. Cilostazol (200 mg/day) was administered for the MCA stenosis. The patient was transferred to a rehabilitation hospital on day 89 with severe left hemiparesis (manual muscle test grade = 1). On the 5-month follow-up at the outpatient clinic, the left hemiparesis had improved slightly and the patient could walk independently (modified Rankin Scale score = 3).
Figure 5:
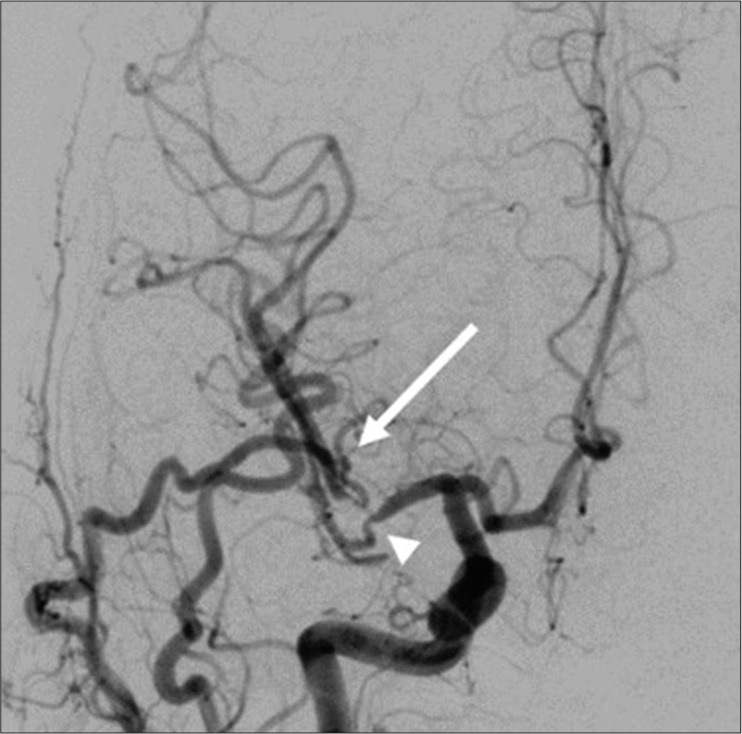
Postoperative imaging findings. Postoperative digital subtraction angiography image obtained on day 56 showing excellent bypass patency (arrow) with a mild stenotic lesion of the M1-2 bifurcation and M2 inferior trunk (arrowhead).
DISCUSSION
Traumatic cerebral pseudoaneurysms are very rare but have a high mortality rate of up to 50%.[5,10,13] Although immediate diagnosis is vital, it is rarely possible until cerebral hemorrhage occurs.[1,5] Namely, vascular abnormalities may not be observed in the early stage of injury, and traumatic aneurysms have also been reported to develop in the late phase.[5,11]
In our case, head CT showed SAH predominantly in the right Sylvian fissure. In addition, the patient had severe consciousness disturbance compared to the degree of cerebral contusion. Therefore, we considered the possibility that endogenous SAH may have caused the consciousness disturbance and induced the traffic accident. However, no vascular abnormalities were observed on CTA. Head MRA on day 7 did not show a cerebral aneurysm but detected progression of the stenosis from the right M1 to M2. Concerning about the possibility of SAH due to MCA dissection, we performed repeated neurovascular evaluation. CTA performed on day 20 confirmed the appearance of an aneurysm on the right MCA. The previous studies have also reported difficulty in diagnosing traumatic cerebral pseudoaneurysms[1,5] and late development of aneurysms.[5,11] Hence, in cases of unreasonably thick traumatic SAH or diffuse cerebral vascular stenosis, as in the present case, traumatic cerebral pseudoaneurysm should be suspected. In addition to this, even if there is no vascular abnormalities at the time of admission, vascular evaluation should be performed 2 weeks later to detect vascular abnormalities early.
Traumatic cerebral aneurysms have a higher rupture rate than normal cerebral aneurysms because of their fragility; therefore, early therapeutic intervention is necessary when they are detected.[5] The average time from injury to aneurysm rupture is 21 days.[2,4,8,12] In this case, the aneurysm was detected on day 20, but enlarged on day 23; thus, we planned direct surgery on day 26. However, the aneurysm ruptured on day 24, approximately 3 weeks after the injury, which is consistent with previously reported findings. The time from traumatic aneurysm detection to aneurysm enlargement and rupture was only 3 days. This indicates that traumatic cerebral aneurysms are more likely to rupture in the short time and that early therapeutic intervention is necessary. In our case, deep sedation was administered once the aneurysm was confirmed to be enlarged on day 23.
Various treatment options have been reported for traumatic cerebral aneurysms, including endovascular treatment.[3,6] Initially, we planned to trap the dissected area under STA-M2 double-barrel bypass. However, the actual laceration was limited to the superior wall of the M2 superior trunk, which was much shorter than we had expected preoperatively. Therefore, trapping was performed only for the lacerated area on the M2 superior trunk with preservation of the M2 inferior trunk and antegrade blood flow from M1 to the M2 inferior trunk. Although the M2 inferior trunk origin was slightly stenosed, the bypass of the M2 inferior trunk was not performed [Figure 3b].
Traumatic cerebral aneurysms are common in the ICA and vertebral arteries and have also been reported in the cortical branches of the anterior cerebral artery and MCA.[5,7,10,13] However, traumatic cerebral aneurysms occurring at the proximal MCA have rarely been reported.[7] The mechanism of traumatic aneurysm formation is thought to be movement of the intracranial vessel and impact against adjacent rigid structures, such as the cerebral flax, skull, and dura mater.[9] We identified a developed sphenoid ridge during craniotomy that was located near the M1-M2 bifurcation [Figure 4a]. We speculate that this rigid structure may have been associated with the development of the proximal MCA aneurysm in our case.
CONCLUSION
In cases of unreasonably thick SAH or extensive cerebral vasospasm after head trauma, continuous neurovascular evaluation is mandatory to detect late emergence of traumatic pseudoaneurysms, even if no vascular abnormalities are detected in the primary neurovascular evaluation. Immediate surgical intervention is necessary once a traumatic cerebral aneurysm is confirmed.
Footnotes
How to cite this article: Somiya D, Sakamoto Y, Maeda K, Takasu S, Takemoto M, Choo J, et al. Ruptured proximal middle cerebral artery traumatic pseudoaneurysm treated with bypass-assisted trapping surgery: A case report. Surg Neurol Int 2023;14:263.
Contributor Information
Daiki Somiya, Email: daiki0413somiya@gmail.com.
Yusuke Sakamoto, Email: usakamoto420@gmail.com.
Kenko Maeda, Email: kenkouc200@gmail.com.
Syuntaro Takasu, Email: syuntaro@xj.commufa.jp.
Masaya Takemoto, Email: nutake0105@gmail.com.
Jungsu Choo, Email: jonsu_the_sankakukin@yahoo.co.jp.
Mizuka Ikezawa, Email: mizuka_ike@yahoo.co.jp.
Fumihiro Sago, Email: f.sagoh@gmail.com.
Kohei Doba, Email: ramona.sukaira0220@gmail.com.
Akira Ikeda, Email: a.ikeda.chukyo@gmail.com.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
REFERENCES
- 1.Buckingham MJ, Crone KR, Ball WS, Tomsick TA, Berger TS, Tew JM., Jr Traumatic intracranial aneurysms in childhood: Two cases and a review of the literature. Neurosurgery. 1988;22:398–408. doi: 10.1227/00006123-198802000-00022. [DOI] [PubMed] [Google Scholar]
- 2.Burton C, Velasco F, Dorman J. Traumatic aneurysm of a peripheral cerebral artery. Review and case report. J Neurosurg. 1968;28:468–74. doi: 10.3171/jns.1968.28.5.0468. [DOI] [PubMed] [Google Scholar]
- 3.Cohen JE, Gomori JM, Segal R, Spivak A, Margolin E, Sviri G, et al. Results of endovascular treatment of traumatic intracranial aneurysms. Neurosurgery. 2008;63:476–86. doi: 10.1227/01.NEU.0000324995.57376.79. [DOI] [PubMed] [Google Scholar]
- 4.Holmes B, Harbaugh RE. Traumatic intracranial aneurysms: A contemporary review. J Trauma. 1993;35:855–60. [PubMed] [Google Scholar]
- 5.Larson PS, Reisner A, Morassutti DJ, Abdulhadi B, Harpring JE. Traumatic intracranial aneurysms. Neurosurg Focus. 2000;8:e4. doi: 10.3171/foc.2000.8.1.1829. [DOI] [PubMed] [Google Scholar]
- 6.Niu Y, Zhou S, Tang J, Miao H, Zhu G, Chen Z. Treatment of traumatic intracranial aneurysm: Experiences at a single center. Clin Neurol Neurosurg. 2020;189:105619. doi: 10.1016/j.clineuro.2019.105619. [DOI] [PubMed] [Google Scholar]
- 7.Ohta M, Matsuno H. Proximal M2 false aneurysm after head trauma--case report. Neurol Med Chir (Tokyo) 2001;41:131–4. doi: 10.2176/nmc.41.131. [DOI] [PubMed] [Google Scholar]
- 8.Parkinson D, West M. Traumatic intracranial aneurysms. J Neurosurg. 1980;52:11–20. doi: 10.3171/jns.1980.52.1.0011. [DOI] [PubMed] [Google Scholar]
- 9.Rumbaugh CL, Bergeron RT, Talalla A, Kurze T. Traumatic aneurysms of the cortical cerebral arteries. Radiographic aspects. Radiology. 1970;96:49–54. doi: 10.1148/96.1.49. [DOI] [PubMed] [Google Scholar]
- 10.Shi Y, Gao Y, Liu Y, Cui W, Zhou G, Wang L, et al. Treatment of traumatic intracranial pseudoaneurysms: A single-center experience. Front Neurol. 2021;12:690284. doi: 10.3389/fneur.2021.690284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith DR, Kempe LG. Cerebral false aneurysm formation in closed head trauma; case report. J Neurosurg. 1970;32:357–9. doi: 10.3171/jns.1970.32.3.0357. [DOI] [PubMed] [Google Scholar]
- 12.Voelker JL, Ortiz O. Delayed deterioration after head trauma due to traumatic aneurysm. W V Med J. 1997;93:317–9. [PubMed] [Google Scholar]
- 13.Zheng Y, Lu Z, Shen J, Xu F. Intracranial pseudoaneurysms: Evaluation and management. Front Neurol. 2020;11:582. doi: 10.3389/fneur.2020.00582. [DOI] [PMC free article] [PubMed] [Google Scholar]