Abstract
目的
探讨中老年人握力与其共病患病的关联。
方法
采用中国健康与养老追踪调查(CHARLS)基线数据(2011年)和第二轮随访数据(2015年),选取≥40岁人群作为研究对象。调查内容包括手握力、慢病患病状况、人口学变量、健康行为变量等。采用广义估计方程分析握力与共病的纵向关联。
结果
共纳入基线样本和随访样本共28 368人,平均年龄为(59.1±9.7)岁,最大96岁,最小40岁。其中男性6 239人,占比47.3%。调查对象第二轮随访中成功追访9 186名基线受访者,新增受访者5 994人,共15 180人。与基线相比,第二轮随访受访者女性更多(P=0.033)、年龄较大(P<0.001)。从基线到第二轮随访,最低握力分类Q1从23.4%增长到26.6%,最高握力分类Q4从26.5%降低到21.2%;3种以上慢病患病率从18.2%增长至24.2%;5种以上慢病患病率从3.3%增长至6.2%。调整混杂变量后,握力与时间的交互项有统计学意义(P<0.05)。按性别分层后,男性握力与随访时间交互项在两个模型中都有统计学意义(P<0.05)。交互项的边际效应图显示较低握力水平的受访者随着年龄增长,共病患病率增长更快。单独效应分析表明手握力与共病患病关联在基线时没有统计学意义,在4年后随访时手握力与共病患病关联有统计学意义。
结论
较低的基线握力受访者随时间推移,与更高的共病患病风险相关。握力可作为一种有效的中国中老年人筛查工具,有助于识别有较高慢病共病风险的老年人。
Keywords: 共病, 中老年人, 握力, 广义估计方程
Abstract
Objective
To investigate the potential association between multimorbidity and the handgrip strength of middle-aged and older adults.
Methods
The baseline (2011) and second-round follow-up (2015) data of China Health and Retirement Longitudinal Study (CHARLS) were used. Adults≥40 were selected as the subjects of the study. Variables incorporated in the study included handgrip strength, chronic disease prevalence, demographic variables, and health behavior variables. Generalized estimating equations were used to analyze the longitudinal association between handgrip strength and multimorbidity.
Results
A total of 28 368 middle-aged and older adults were included in the baseline and follow-up samples, with an average age of (59.1±9.7) years old, the oldest being 96 while the youngest being 40. Among them, 6 239 were male, accounting for 47.3%. In the second-round follow-up, 9 186 baseline respondents and 5 994 new respondents were covered, reaching a total of 15 180 respondents. Compared with the baseline, a higher proportion of the second-round follow-up respondents were female (P=0.033) and were older (P<0.001). From the baseline to the second-round follow-up, Q1, the lowest grip strength category, increased from 23.4% to 26.6%, while Q4, the highest grip strength category, decreased from 26.5% to 21.2%. The prevalence of having more than three chronic diseases increased from 18.2% to 24.2% and the prevalence of having more than five chronic diseases increased from 3.3% to 6.2%. After adjusting for confounding variables, the interaction items of handgrip strength and time showed statistical significance. After stratification by gender, the interaction items of male handgrip strength and follow-up time were statistically significant in both models (P<0.05). The marginal effect graph of the interactive item showed that the multimorbidity prevalence of respondents with lower handgrip levels grew faster with age. Individual effect analysis showed that the correlation between handgrip strength and multimorbidity was not statistically significant at baseline, but the follow-up done four years afterwards showed statistical significant correlation between handgrip strength and multimorbidity.
Conclusion
Respondents with lower baseline handgrip strength are associated with increasingly higher risk of multimorbidity over time. Handgrip strength can be used as an effective screening tool for middle-aged and older adults in China to identify those at higher risks of multimorbidity of chronic diseases.
Keywords: Multimorbidity, Middle-aged and elderly people, Grip strength, Generalized estimating equation
共病最初是指老年人同时存在2种或多种慢病的情况,随着老年医学的发展,及医学工作者对于老年综合征/问题日益重视,共病的概念也相应地更新为“多种病态”(multimorbidity,MM)或“多种慢性状况”(multiple chronic conditions,MCC)。本研究中的共病是指MM,慢病则指慢性疾病[1]。慢病的患病率随着寿命增长而增加,由于我国人口老龄化程度的进一步加深,共病问题愈加严重,已成为严重影响我国居民身体健康和生活质量的重要公共卫生问题[2]。共病不仅严重影响个人身心健康和生活质量,还对国家卫生保健资源造成较大损耗[3]。当前并没有彻底治愈慢病的方法,因此,找到慢病共病的预测临床体征对共病防治有重要的公共卫生意义。已有研究表明握力是多种健康结局的预测因子[4]。一项系统综述表明,在不同研究样本中,中老年人低握力与过早死亡、残疾和其他与健康有关的并发症存在联系[5]。由于现有关于握力与共病关联性的研究多是基于横断面调查[6],而握力与共病之间可能存在相互作用,在判定握力与共病因果关联上存在缺陷。横断面研究的验证病因假说能力不足,缺乏更多纵向研究的证据,且国内外相关研究样本量不大、代表性不强,难以推广到整个人群或某一地区。因此,本研究基于中国健康与养老追踪调查(CHARLS)中2011年基线数据与2015年随访数据,拟合广义估计方程(GEE模型)探索中老年人握力与共病的纵向关联。
1. 对象与方法
1.1. 研究对象
数据资料来源于中国健康与养老追踪调查(China Health and Retirement Longitudinal Study,CHARLS)基线调查(2011年)和第二轮随访(2015年)。具体调查方法参见文献[7]。参照有关研究对中老年的界值[8],本研究选取≥40岁人群作为研究对象。纳入标准为:①受访者在基线和第二次随访中均完成手握力测试;②受访者年龄≥40岁。排除标准为:受访者的社会人口学特征变量、健康行为变量和健康状态变量存在缺失值。
1.2. 研究变量及测量方法
1.2.1. 共病
询问受访者“是否被医生诊断出患有慢性疾病?”。慢性疾病包括14种类型:高血压,血脂异常,糖尿病或高血糖,癌症或恶性肿瘤,慢性肺部疾病,肝病,心脏病,中风,肾脏病,胃或其他消化系统疾病,神经或精神疾病,与记忆有关的疾病,关节炎或风湿病,哮喘。根据受访者的回答,我们将其分为两类,即共病患者与非共病患者。虽然共病的概念是两种或两种以上疾病的存在,但文献表明,关于最佳分界点或最佳数目以及应包括哪些疾病尚无共识[9]。为尽可能反映研究对象在随访期间共病状态的变化,综合考虑分界点的灵敏度及研究结果在不同研究间的可比性,在参考国内外现有中老年人共病研究的基础上[10],采用了两种共病分界点定义,分别是受访者患有3种以上慢病和受访者患有5种以上慢病,本研究同时分析这两种患者的数据特征。
1.2.2. 手握力
通过中国南通WCS-100测力计测量调查对象的握力。每只手各测2次,4个握力测量结果中测值最大的1个数据用于统计分析。考虑到肌肉力量在性别上的差异,在对握力分类时男女采用不同的分类标准[11]。基于握力得分的四分位数,将男性握力分为4类:≤34.0 kg,34.1~40.0 kg,40.1~ 45.2 kg和>45.2 kg,将女性握力分为4类:≤22.5 kg,22.6~ 27.0 kg,27.1~ 31.0 kg和>31.0 kg。
1.2.3. 混杂因素
参考国内外先前关于中老年人共病危险因素的研究[6]。从CHARLS数据中选择一般人口学变量(性别、年龄、居住地、婚姻状况、受教育水平)、健康行为变量(吸烟、饮酒、睡眠时间)、健康状态(自评健康状况、摔倒、疼痛)等变量进行分析。
1.3. 统计学方法
定量资料采用
 表示,定性资料采用频数和百分比描述。采用卡方检验、秩和检验和单因素方差分析来比较基线和第二轮随访样本间的基本特征差异。
表示,定性资料采用频数和百分比描述。采用卡方检验、秩和检验和单因素方差分析来比较基线和第二轮随访样本间的基本特征差异。
纵向数据(longitudinal data)指在不同时间测量相同的观察单位(个人)或不同条件下多次测量得到的资料,同一对象多次测量之间有相关性。采用广义估计方程(generalized estimating equation,GEE)探究不同握力暴露与中老年人共病的纵向关联。选择GEE是因为它扩展了广义线性模型并允许进一步分析纵向数据,较好解决纵向数据中因变量相关的问题,且模型相对稳健。按性别分层,进行联合测试,探究握力与时间整体的交互作用,两个模型分别使用了两种共病分界点定义。进一步进行单独效应分析,探索不同时间点(基线、随访)握力对共病的影响。数据分析使用STATA 15.0软件,α=0.05。
2. 结果
2.1. 调查对象一般情况
表1列出了样本的基线及第二次随访时的样本特征。基线调查对象13 188例,其中男性6 239例(47.3%)。调查对象平均年龄为(59.1±9.7)岁,最大96岁,最小40岁。已婚者有11 524例(87.4%),8 304例(62.9%)的调查对象户口在农村。受教育程度方面,小学及以上学历者占54.2%。第二轮随访(wave3)中成功追访9 186例基线受访者,新增受访者5 994人,共15 180人。与基线相比,第二轮随访受访者男性更少〔6 988例 (46.0%),P=0.033〕、年龄更大〔(59.6±10.5)岁,P<0.001〕,受教育水平也存在一定差异(P=0.011)。但已婚人数占比〔13 304例 (87.6%)〕、农村户口人数占比〔9 472 (62.4%)〕与基线相比差异无统计学意义。此外,与基线相比,第二轮随访受访者在饮酒、自评健康、摔倒、疼痛状况、听力方面存在差异(P<0.05)。从基线到第二次随访,最低握力分类Q1从23.4%增长到26.6%,最高握力分类Q4从26.5%降低到21.2%;3种以上慢病患病率从18.2%增长至24.2%;5种以上慢病患病率从3.3%增长至6.2%。见表2。
表 1. Sociodemographic characteristics of Chinese aged over 40.
中国40岁及以上中老年人的社会人口学特征
| Characteristics of respondents | 2011 (n=13 188) | 2015 (n=15 180) | P |
| Education level/case (%) | 0.011 | ||
| Illiterate | 3 641 (27.6) | 4 262 (28.1) | |
| Below elementary school | 2 403 (18.2) | 2 732 (18.0) | |
| Primary school | 2 993 (22.7) | 3 267 (21.5) | |
| Junior high school | 2 716 (20.6) | 3 085 (20.3) | |
| High school | 1 202 (9.1) | 1 532 (10.1) | |
| College and above | 233 (1.8) | 302 (1.9) | |
| Smoking status/case (%) | 0.981 | ||
| No | 7 962 (60.4) | 9 161 (60.4) | |
| Yes | 5 226 (39.6) | 6 019 (39.6) | |
| Drinking /case (%) | 0.001 | ||
| No | 8 883 (67.4) | 9 858 (64.9) | |
| Less than 1 time/month | 1 049 (7.9) | 1 326 (8.7) | |
| More than once a month | 3 256 (24.7) | 3 996 (26.4) | |
| Sleeping time/case (%) | 0.293 | ||
| <6 h | 3858 (29.3) | 4369 (28.8) | |
| 6-9 h | 8 751 (66.3) | 10 187 (67.1) | |
| >9 h | 579 (4.4) | 624 (4.1) | |
| Self-rated health/case (%) | <0.001 | ||
| Very good | 784 (5.9) | 1 860 (12.2) | |
| good | 2 238 (17.0) | 1 891 (12.5) | |
| Fair | 6 882 (51.7) | 8 013 (52.8) | |
| Poor | 2832 (21.5) | 2701 (17.8) | |
| Very poor | 522 (3.9) | 715 (4.7) | |
| Wearing glasses/case (%) | 0.985 | ||
| No | 11 692 (88.7) | 11 039 (88.9) | |
| Yes | 1 432 (10.8) | 4 105 (10.6) | |
| Blindness | 64 (0.5) | 36 (0.5) | |
| Hearing/case (%) | <0.001 | ||
| Excellent | 184 (1.4) | 327 (2.2) | |
| Very good | 1 776 (13.5) | 2 498 (16.5) | |
| good | 3 863 (29.3) | 2 546 (16.8) | |
| Fair | 5 531 (41.9) | 7 945 (52.3) | |
| Poor | 1 834 (13.9) | 1 864 (12.3) | |
| fall(s) (last year)/case (%) | 0.035 | ||
| No | 11 058 (83.9) | 12 586 (82.9) | |
| Yes | 203 (16.1) | 2 594 (17.1) | |
| Pain/case (%) | <0.001 | ||
| No | 8 821 (66.9) | 10 606 (69.9) | |
| Yes | 4 367 (33.1) | 4 574 (30.1) | |
表 2. Grip strength and chronic multimorbidities in Chinese over 40 years old.
中国40岁及以上中老年人的握力水平和慢病共病患病状况
| Characteristics of respondents | 2011 (n=13 188) | 2015 (n=15 180) | P |
| Grip strength/case (%) | <0.001 | ||
| First quantile (Q1) | 308 (23.4) | 4 037 (26.6) | |
| Second quantile (Q2) | 3 302 (25.0) | 4 111 (27.1) | |
| Third place (Q3) | 3 305 (25.1) | 3 807 (25.1) | |
| Fourth quartile (Q4) | 3 501 (26.5) | 3 225 (21.2) | |
| Suffering from more than 3 chronic diseases/case (%) | <0.001 | ||
| Yes | 2 402 (18.2) | 3 676 (24.2) | |
| No | 10 786 (81.8) | 11 504 (75.8) | |
| Suffering from more than 5 chronic diseases/case (%) | <0.001 | ||
| Yes | 436 (3.3) | 937 (6.2) | |
| No | 12 752 (96.7) | 14 243 (93.8) | |
2.2. 握力与多重慢病共病的关系
图1和表3为中老年人握力和共病纵向关联的GEE模型分析结果。使用广义估计方程同时纳入基线与第二次随访数据以分析握力与共病的纵向关联,在两个模型(Model 1、Model 2)中分别使用两种共病分界点(慢病数≥3,慢病数≥5),查看不同共病分界点对握力与共病关联的影响并增加结果与其他研究的可比较性。在控制了所有混杂因素后,握力与时间的交互项有显著的统计学意义,说明不同握力在基线和第二次随访中与共病的关联存在差异。按性别分层后,男性握力与随访时间交互项在两个模型中都有显著的统计学意义,女性握力(Q3、Q4)与随访时间交互项在模型1中显著〔比值比(OR)=0.55,95%可信区间(CI):0.33~0.90,OR=0.54,95%CI:0.34~0.86)〕,在模型2中不显著(P>0.05)。在广义估计方程模型结果的基础上,交互项的边际效应图显示,不同握力的男女受访者在基线和第二次随访中共病患病率的变化。从不同握力四分位数的斜率变化中可以看出,较低握力(Q1)受访者随着年龄增长,共病患病率增长更快。其他因素的回归结果显示,居住地、学历、年龄、自评健康、视力、听力、摔倒和疼痛等因素与共病患病存在显著关联,而婚姻、性别与共病患病的关联没有统计学意义。
图 1.
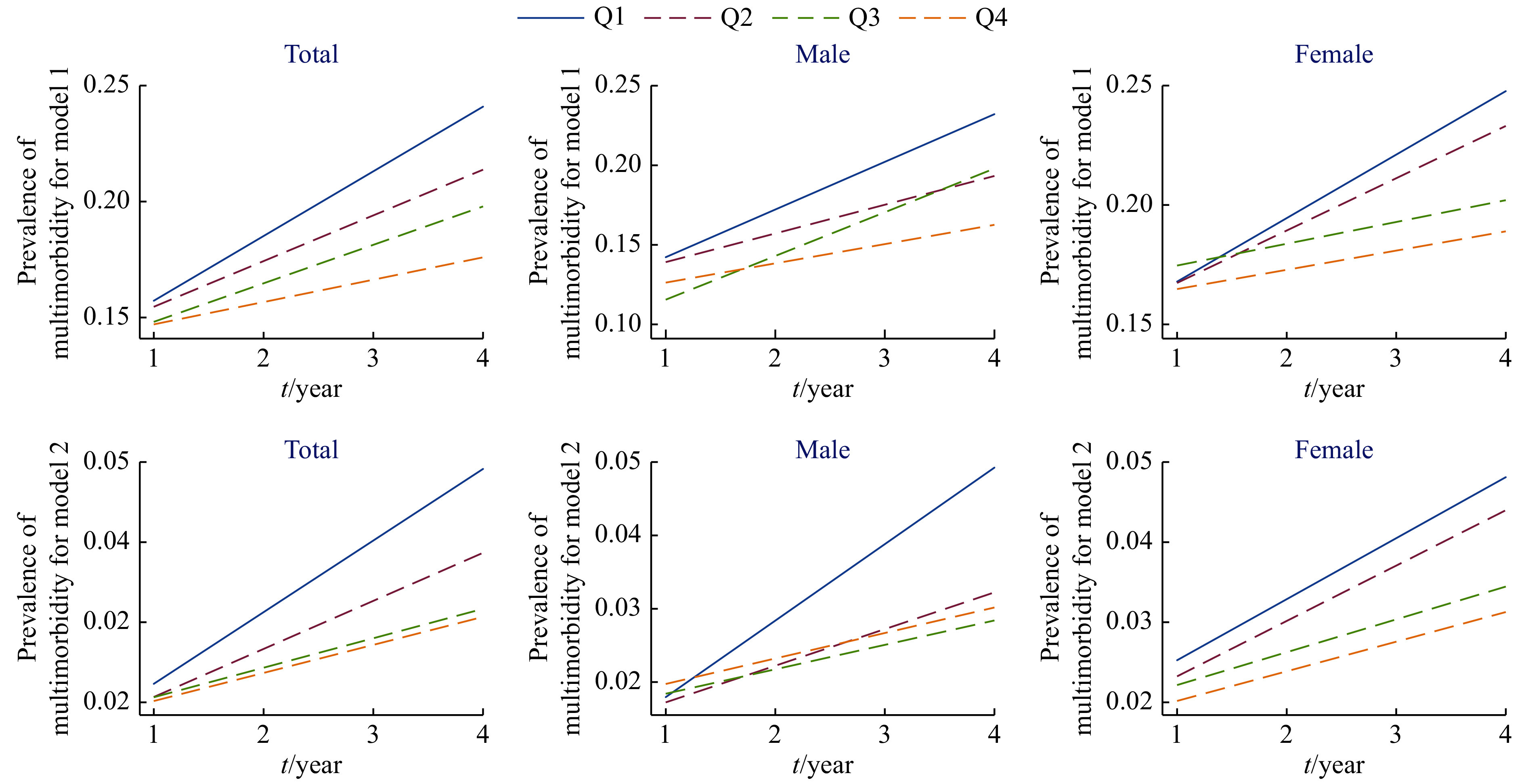
Longitudinal correlation between grip strength and cognitive changes in middle-aged and elderly Chinese: based on generalized estimating equations
中国中老年人握力与认知变化之间的纵向关联:基于广义估计方程
The model 1 and model 2 marked in the figure refer to the longitudinal correlation between grip strength and cognitive changes at different multimorbidity cut-off value. “Q1” is the GS first quartile, “Q2” is the GS second quartile, “Q3” is the GS third quartile, “Q4” is the GS fourth quartile.
表 3. Longitudinal correlation between grip strength and multimorbidities in Chinese over 40 years old.
中国40岁及以上中老年人握力与共病的纵向关联
| Variable | Model 1a | Model 2b | |||
| OR (95%CI) | P | OR (95%CI) | P | ||
| OR: Odds ratio; CI: Confidence interval. Boldfaced numbers indicate statistical significance. All models use generalized estimating equations with different cut-off value of multimorbidity and control all confounding factors. a: The cut-off value of multimorbidity in model 1 is suffering from 3 or more chronic diseases; b: The cut-off value of multimorbidity in model 2 is suffering from 5 or more chronic diseases. | |||||
| Total | |||||
| Grip strength (GS) | |||||
| Q1 (GS first quartile) | 1 | 1 | |||
| Q2 (GS second quartile) | 0.98 (0.86-1.11) | 0.762 | 0.92 (0.71-1.19) | 0.551 | |
| Q3 (GS third quartile) | 0.93 (0.81-1.06) | 0.302 | 0.92 (0.7-1.21) | 0.566 | |
| Q4 (GS fourth quartile) | 0.92 (0.8-1.06) | 0.263 | 0.9 (0.67-1.2) | 0.480 | |
| GS×Time | |||||
| Q1×follow-up time | 1 | 1 | |||
| Q2×follow-up time | 0.87 (0.74-1.02) | 0.101 | 0.84 (0.61-1.14) | 0.271 | |
| Q3×follow-up time | 0.83 (0.7-0.98) | 0.031 | 0.68 (0.49-0.94) | 0.020 | |
| Q4×follow-up time | 0.72 (0.61-0.86) | <0.001 | 0.67 (0.48-0.94) | 0.021 | |
| Male | |||||
| Grip strength (GS) | |||||
| Q1 (≤34.0 kg) | 1 | 1 | |||
| Q2 (34.1–40.0 kg) | 0.97 (0.8-1.17) | 0.79 | 0.95 (0.64-1.42) | 0.837 | |
| Q3 (40.1–45.2 kg) | 0.78 (0.63-0.97) | 0.026 | 1.02 (0.67-1.57) | 0.905 | |
| Q4 (>45.2 kg) | 0.87 (0.7-1.07) | 0.192 | 1.1 (0.72-1.68) | 0.654 | |
| GS×Time | |||||
| Q1×follow-up time | 1 | 1 | |||
| Q2×follow-up time | 0.81 (0.64-1.02) | 0.084 | 0.67 (0.42-1.05) | 0.085 | |
| Q3×follow-up time | 1.03 (0.8-1.33) | 0.783 | 0.55 (0.33-0.90) | 0.018 | |
| Q4×follow-up time | 0.73 (0.57-0.93) | 0.013 | 0.54 (0.34-0.86) | 0.009 | |
| Female | |||||
| Grip strength (GS) | |||||
| Q1 (≤22.5 kg) | 1 | 1 | |||
| Q2 (22.6–27.0 kg) | 0.99 (0.83-1.18) | 0.966 | 0.91 (0.65-1.29) | 0.626 | |
| Q3 (27.1–31.0 kg) | 1.04 (0.87-1.25) | 0.597 | 0.87 (0.61-1.25) | 0.462 | |
| Q4 (>31.0 kg) | 0.97 (0.81-1.17) | 0.815 | 0.79 (0.53-1.17) | 0.247 | |
| GS×Time | |||||
| Q1×follow-up time | 1 | 1 | |||
| Q2×follow-up time | 0.92 (0.74-1.15) | 0.504 | 0.99 (0.65-1.50) | 0.967 | |
| Q3×follow-up time | 0.73 (0.58-0.91) | 0.006 | 0.8 (0.52-1.23) | 0.319 | |
| Q4×follow-up time | 0.72 (0.57-0.91) | 0.007 | 0.8 (0.5-1.28) | 0.359 | |
2.3. 单独效应分析
在联合测试(纵向数据)分析握力与时间交互作用的基础上,通过单独效应测试(横截面子样本:基线样本和第二次随访样本)进一步观察不同时间点握力对共病的影响,以佐证联合测试中关于握力时间交互作用与共病的关联。分析结果显示,在基线样本中,在两种不同共病分界点定义下,手握力与共病患病的关系均没有统计学意义(P>0.05);第二次随访时,相比于Q1握力,中老年人群中Q3(the GS third quartile)、Q4(the GS fourth quartile)握力与共病患病率显著相关(P<0.001)。在共病分界点为≥5种慢病患病的模型中,相比于Q1握力,Q2、Q3、Q4握力均与共病患病率显著相关(P<0.05)。相比于基线样本,第二次随访样本中握力与共病的关联更加显著,如表4。结果佐证了表3中握力与时间交互作用与共病患病的关联,提示较低握力者共病患病率增长更快。
表 4. Correlation between grip strength and multimorbidity at different time points.
不同时间点握力与共病的关联
| Grip strength | OR (95%CI) | P |
| OR: Odds ratio; CI: Confidence interval. Boldfaced numbers indicate statistical significance. All models use binary logistic regression with different subsamples and control all confounding factors. The cut-off value of multimorbidity in model 1 is suffering from 3 or more chronic diseases. The cut-off value of multimorbidity in model 2 is suffering from 5 or more chronic diseases. | ||
| Baseline sample (model 1) | ||
| Q1 | 1 | |
| Q2 | 1.04 (0.91-1.18) | 0.585 |
| Q3 | 1.04 (0.90-1.20) | 0.586 |
| Q4 | 1.09 (0.94-1.27) | 0.258 |
| Wave3 (model 1) | ||
| Q1 | 1 | |
| Q2 | 0.85 (0.77-0.95) | 0.003 |
| Q3 | 0.78 (0.69-0.87) | <0.001 |
| Q4 | 0.67 (0.60-0.76) | <0.001 |
| Baseline sample (model 2) | ||
| Q1 | 1 | |
| Q2 | 1.01 (0.78-1.34) | 0.888 |
| Q3 | 1.09 (0.82-1.46) | 0.541 |
| Q4 | 1.16 (0.85-1.58) | 0.363 |
| Wave3 (model 2) | ||
| Q1 | 1 | |
| Q2 | 0.76 (0.64-0.91) | 0.002 |
| Q3 | 0.62 (0.51-0.75) | <0.001 |
| Q4 | 0.59 (0.48-0.74) | <0.001 |
3. 讨论
本研究利用CHARLS数据中基线调查和第二次随访调查共28 366例≥40岁调查样本,使用GEE分析手握力与中老年人共病的纵向关联。结果显示,与高握力者相比,低握力者在基线时共病患病概率更高,随着年龄的增长,共病患病率增长更快。握力与共病的纵向关联可能存在性别差异,按性别分层后,在不同的共病分界点定义的两个GEE模型中,关联在男性受访者中均显著,而在女性受访者中较不稳定。
较低的握力一般被认为与中老年人的早死、残疾和虚弱有关。目前握力与共病的研究较少,且多是横断面研究。最早的一篇文献发表于在2013年,CHEUNG等[12]对1 145名中国香港中老年人握力和共病关联进行调查分析,在控制了混杂因素后,较低的握力与男性和女性患多种慢病的概率增加显著相关。MONTES等[13](2020)调查了1 336名巴西60岁以上老年人,分析共病与握力的关联,结果显示手握力与共病显著相关,且这种关联在男性中更加显著。本研究中也出现了相似的性别差异,即男性握力与共病的关联似乎更加显著。这可能与男女性在生理因素尤其是激素上的内在差异有关[12],性激素水平是影响男性握力的重要因素[14]。女性绝经期间和绝经后睾丸激素显著降低,这可能也有助于解释老年男性较高的握力及握力与共病关联的性别差异[15]。握力与虚弱的研究结果也显示男性握力是比年龄更重要的虚弱预测因素,女性则相反[16]。性类固醇加生长激素干预显著增加男性肌肉力量,而不是女性[14]。PESSINI等[17](2016)发现男性和女性慢病与握力间关联不同,癌症和抑郁症与女性低握力有关,糖尿病、慢性肺病和冠心病与男性低握力有关。
握力与共病间的作用机制目前仍不明确。握力是肌肉力量的一般性指标,先前研究认为除残疾以外,握力与各种健康结局的关联不是直接关联,更可能是握力反映了导致结局发生的其他潜在变量,如衰弱、营养和活力[18]。40岁以后中老年人肌肉质量每十年减少5%,肌肉力量的逐渐丧失将导致肌肉减少症(sarcopenia),这被认为与老年人高死亡风险有关[19]。SZULC等[20](2016)发现肌肉力量与帕金森病、糖尿病发病率和低水平的游离睾丸激素呈负相关。患抑郁症的人具有高浓度的肿瘤坏死因子-α和白介素,对降低肌肉强度有影响[21]。有队列研究发现握力是冠心病的最佳预测指标,而胰岛素抵抗、慢性炎症和腹部肥胖的减少可能是肌肉力量改善冠心病预后部分机制[22]。这些研究表明,握力可能是由多种生理系统控制,并作为一种其他生理系统的生物标志。虽然目前研究没有建立握力和整体健康间的因果关系,但有研究表明,增强握力有利于肌肉系统以外的生理系统,5到6周的等距握力训练已被证明可以降低静息状态下的动脉血压[23]。此外,肌肉还会产生大量的细胞因子和生长激素,被认为与慢性心力衰竭等多种慢病相关[24]。通过阻力训练提高肌力可能是改善一般健康和降低多种慢性疾病风险的可行策略。
本研究也存在一定的局限性。首先,作为本研究中重要的结局变量,慢病患病情况来自于受访者的自我报告。同时,我们也无法得到慢病的严重程度及其在随访期间的进程变化,这些都可能会对结果产生影响。其次,本次研究的握力及其分类是基于中国中老年人群,由于不同人种间握力的差异,可能无法推广到所有的中老年人[25]。第三,本研究没能控制膳食结构、体力活动、体质量指数、虚弱等重要混杂因素,对研究结果精确性存在影响。最后,本研究无法确定肌肉力量(握力)与共病患病率之间的关联是直接的,还是肌肉力量是某种导致共病的其他因素的替代指标。在未来的研究中,可以进行老年人肌肉力量的训练,以检验维持肌肉力量是否可以有效预防共病的发生。同时,该指标在三级医院、基层医院、公卫调查等场景中的实际应用是下一步的研究方向。
综上所述,本研究发现手握力与中老年人共病间存在纵向关联,并且在男性中更加显著。在未来,多维度的老年病学评估中可应用握力计作为筛查工具,有助于识别有较高健康风险者,应对我国逐渐增长的老年化及其带来的多重疾病。
Funding Statement
国家社会科学基金项目(No. 17BRK009)资助
Contributor Information
潇杨 董 (Xiao-yang DONG), Email: 2997427978@qq.com.
毅 刘 (Yi LIU), Email: 934102749@qq.com.
References
- 1.张可可, 朱鸣雷, 刘晓红 老年人"共病"问题概述. 中华老年多器官疾病杂志. 2016;15(8):587–590. [Google Scholar]
- 2.崔娟, 毛凡, 王志会 中国老年居民多种慢性病共存状况分析. 中国公共卫生. 2016;32(1):66–69. [Google Scholar]
- 3.张可可, 朱鸣雷, 刘晓红, 等 北京部分社区老年人共病及老年综合征调查分析. 中国实用内科杂志. 2016;36(5):419–421. [Google Scholar]
- 4.SOOHYUN P, JINKYUNG C, DONGHYUN K, et al Handgrip strength, depression, and all-cause mortality in Korean older adults. BMC Geriatr. 2019;19(1):127. doi: 10.1186/s12877-019-1140-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DAVY V, BRENDON S, JOSEPH F, et al Handgrip strength, chronic physical conditions and physical multimorbidity in middle-aged and older adults in six low- and middle income countries. Eur J Intern Med. 2019;61:96–102. doi: 10.1016/j.ejim.2018.11.007. [DOI] [PubMed] [Google Scholar]
- 6.KANG Y, PARK S, KIM S, et al Handgrip strength among korean adolescents with metabolic syndrome in 2014–2015. J Clin Densitom. 2020;23(2):271–277. doi: 10.1016/j.jocd.2018.09.002. [DOI] [PubMed] [Google Scholar]
- 7.宁满秀, 余平平 农村中老年慢性病患者就诊行为与影响因素研究——基于CHARLS数据的实证分析. 中国卫生政策研究. 2016;9(5):35–41. doi: 10.3969/j.issn.1674-2982.2016.05.007. [DOI] [Google Scholar]
- 8.罗淳 关于人口年龄组的重新划分及其蕴意. 人口研究. 2017;41(5):16–25. [Google Scholar]
- 9.MARTIN F, MOIRA S, MARIE E, et al A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med. 2012;10(2):142–151. doi: 10.1370/afm.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DAVY V, BRENDON S, JOSEPH F, et al Associations between handgrip strength and mild cognitive impairment in middle-aged and older adults in six low- and middle-income countries. Int J Geriatr Psych. 2019;34(4):609–616. doi: 10.1002/gps.5061. [DOI] [PubMed] [Google Scholar]
- 11.RAČIĆ M , PAVLOVIĆ J , IVKOVIĆ N. Handgrip strength cut-off values for the undernutrition risk screening among elderly men and women in Bosnia and Herzegovina. J Aging Res, 2019, 2019: 5726073[2020-09-27]. https://dx.doi.org/10.1155/2019/5726073.
- 12.CHEUNG C, NGUYEN U, AU E, et al Association of handgrip strength with chronic diseases and multimorbidity. Age (Dordr) 2012;35(3):929–941. doi: 10.1007/s11357-012-9385-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.MONTES M C, BORTOLOTTO C, TOMASI E, et al. Grip strength and multimorbidity among community-dwelling elderly from Southern Brazil. Nutrition, 2019, 71: 110636[2020-09-27]. https://dx.doi.org/10.1016/j.nut.2019.110636.
- 14.HANIFE M, YANG A W H, ROBINSON S R Measurement of hand grip strength in the elderly:a scoping review with recommendations. J Bodywork Mov Ther. 2020;24(1):235–243. doi: 10.1016/j.jbmt.2019.05.029. [DOI] [PubMed] [Google Scholar]
- 15.MICHAEL Y L, GOLD R, MANSON J, et al Hormone therapy and physical function change among older women in the Women's Health Initiative. Menopause. 2010;17(2):295–302. doi: 10.1097/gme.0b013e3181ba56c7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.BERNARD C, DABIS F, DE REKENEIRE N Physical function, grip strength and frailty in people living with HIV in sub‐Saharan Africa: systematic review. Trop Med Int Health. 2017;22(5):516–525. doi: 10.1111/tmi.12852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.PESSINI J, BARBOSA A, TRINDADE E Chronic diseases, multimorbidity, and hand grip strength among older adults from Southern Brazil. Rev Nutr. 2016;29:43–52. doi: 10.1590/1678-98652016000100005. [DOI] [Google Scholar]
- 18.LEE W J, PENG L N, CHIOU S T, et al. Physical health indicators improve prediction of cardiovascular and all-cause mortality among middle-aged and older people: a national population-based study. Sci Rep, 2017, 7: 40427[2020-09-27]. https://www.nature.com/articles/srep40427. doi: 10.1038/srep40427.
- 19.GARCIA P A, DIAS J M D, ROCHA A S S, et al Relation offunctional capacity, strength and muscle mass in elderly women with osteopenia and osteoporosis. Physiother Res. 2015;22(2):126–132. doi: 10.590/1809-2950/13154522022015. [DOI] [Google Scholar]
- 20.SZULC P, FEYT C, CHAPURLAT R High risk of fall, poor physical function, and low gripstrength in men with fracture-the STRAMBO study. J Cachexia Sarcopenia Muscle. 2016;7(3):299–311. doi: 10.1002/jcsm.12066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.DOWLATI Y, HERRMANN N, SWARDFAGER W, et al A meta-analysis of cytokines in major depression. Biol Psychiatry. 2010;67(5):446–457. doi: 10.1016/j.biopsych.2009.09.033. [DOI] [PubMed] [Google Scholar]
- 22.ARTERO E G, LEE D C, LAVIE C J, et al Effects of muscular strength on cardiovascular risk factors and prognosis. J Cardiopulm Rehabil Prev. 2012;32(6):351–358. doi: 10.1097/HCR.0b013e3182642688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.HESS N C, CARLSON D J, INDER J D, et al Clinically meaningful blood pressure reductions with low intensity isometric handgrip exercise. A randomized trial. Physiol Res. 2016;65(3):461–468. doi: 10.33549/physiolres.933120. [DOI] [PubMed] [Google Scholar]
- 24.PETER K, LOTHAR H Postnatal body growth is dependent on the transcription factors signal transducers and activators of transcription 5a/b in muscle: a role for autocrine/paracrine insulin-like growth factor Ⅰ. Endocrinology. 2007;148(4):1489–1497. doi: 10.1210/en.2006-1431. [DOI] [PubMed] [Google Scholar]
- 25.LAWMAN H G, TROIANO R P, PERNA F M, et al Associations of relative handgrip strength and cardiovascular disease biomarkers in U. S. adults, 2011–2012. Am J Prev Med. 2016;50(6):677–683. doi: 10.1016/j.amepre.2015.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]


