Abstract
目的
研究血尿素氮/肌酐(blood urea nitrogen-to-creatinine, BUN/Cr)比值在鉴别消化道出血部位中的诊断性能,以及BUN/Cr比值早期升高对于急性非静脉曲张性上消化道出血(acute nonvariceal upper gastrointestinal bleeding, ANVUGIB)患者临床结局事件的预测价值。
方法
回顾性纳入2020年5月–2021年5月于厦门大学附属中山医院诊断为消化道出血的成年患者。根据不同消化道出血部位分为:上消化道出血组、小肠近段出血组、小肠远段及结肠出血组。根据ANVUGIB患者入院后早期(6~48 h内)BUN/Cr比值动态变化情况分为:入院后BUN/Cr比值早期动态升高组和入院后BUN/Cr比值非早期动态升高组。通过受试者操作特征(receiver operating characteristic, ROC)曲线分析BUN/Cr比值对于鉴别消化道出血部位的诊断性能,以及探究入院后BUN/Cr比值早期动态升高、Rockall评分系统及其两者联合指标对ANVUGIB患者主要临床结局事件(因为任何原因死亡;再次出现消化道出血;需要急诊外科手术干预;需要急诊介入手术干预)的预测效能。
结果
共纳入266例消化道出血患者,其中上消化道出血组204例,小肠近段出血组15例,小肠远段及结肠出血组47例;ANVUGIB患者中,入院后BUN/Cr比值早期动态升高组16例,入院后BUN/Cr比值非早期动态升高组146例。BUN/Cr比值对鉴别上、下消化道出血的曲线下面积为0.831(95%CI:0.780~0.874),最佳截断值为34.59 mg/g;BUN/Cr比值对鉴别小肠近段出血、小肠远段及结肠出血的曲线下面积为0.901(95%CI:0.798~0.963),最佳截断值为19.27 mg/g。入院后BUN/Cr比值早期动态升高预测ANVUGIB患者主要临床结局事件的曲线下面积为0.806(95%CI:0.737~0.864),联合Rockall评分后的联合指标预测ANVUGIB患者主要临床结局事件的曲线下面积为0.909(95%CI:0.854~0.949)。
结论
BUN/Cr比值对于鉴别消化道出血部位具有较高的价值,且入院后BUN/Cr比值早期动态升高是预测ANVUGIB患者临床结局事件的可靠指标。
Keywords: 血尿素氮/肌酐比值, 消化道出血, 小肠出血, 急性非静脉曲张性上消化道出血, 预测价值
Abstract
Objective
To explore the diagnostic performance of blood urea nitrogen-to-creatinine (BUN/Cr) ratio in differentiating the site of gastrointestinal bleeding, and to assess the predictive value of early elevated BUN/Cr ratio for clinical outcomes in patients with acute nonvariceal upper gastrointestinal bleeding (ANVUGIB).
Methods
The adult patients diagnosed with gastrointestinal bleeding who were hospitalized in the Department of Gastroenterology, Zhongshan Hospital, Xiamen University between May 2020 and May 2021 were retrospectively enrolled. According to the site of gastrointestinal bleeding, the patients were divided into the upper gastrointestinal tract group, the proximal small intestinal bleeding group, and the distal small intestinal and colonic bleeding group. According to the early dynamic changes of BUN/Cr ratio within 6-48 hours after admission, patients with ANVUGIB were divided into early dynamic elevated BUN/Cr ratio group and non-early dynamic elevated BUN/Cr ratio group. Receiver operating characteristic (ROC) curve was used to analyze the diagnostic performance of BUN/Cr ratio in differentiating the site of gastrointestinal bleeding and examine the predictive efficacy of early dynamic elevated BUN/Cr ratio after admission, Rockall scoring system, and the combined indicator of the two for estimating the primary clinical outcomes in ANVUGIB patients.
Results
A total of 266 patients were enrolled. Among them, 204 cases were in the upper gastrointestinal bleeding group, 15 cases were in the proximal small intestinal bleeding group, and 47 cases were in the distal small intestinal and colonic bleeding group. In the ANVUGIB patients, 16 were in the group with early dynamic elevated BUN/Cr ratio after admission, and 146 were in the group with non-early dynamic elevated BUN/Cr ratio after admission. The area under the ROC curve of the BUN/Cr ratio was 0.831 (95% CI: 0.780-0.874), the optimal cut-off value being 34.59 mg/g for differentiation between upper and lower gastrointestinal bleeding. The area under the ROC curve of the BUN/Cr ratio was 0.901 (95% CI: 0.798-0.963) and the optimal cut-off value was 19.27 mg/g for differentiation between proximal small intestinal bleeding and the distal small intestinal and colonic bleeding. The area under the ROC curve of the early dynamic elevated BUN/Cr ratio after admission was 0.806 (95% CI: 0.737-0.864) for predicting the primary clinical outcome in patients with ANVUGIB. The area under the ROC curve of the combined indicator included the early dynamic elevated BUN/Cr ratio after admission and the Rockall scoring system was 0.909 (95% CI: 0.854-0.949) for predicting the primary clinical outcome in patients with ANVUGIB.
Conclusion
The BUN/Cr ratio shows rather reliable diagnostic performance for identifying the site of gastrointestinal bleeding, and the early dynamic elevated BUN/Cr ratio after admission is a reliable indicator for predicting clinical outcomes in patients with ANVUGIB.
Keywords: Blood urea nitrogen-to-creatinine ratio, Gastrointestinal bleeding, Small intestinal bleeding, Acute nonvariceal upper gastrointestinal bleeding, Predictive value
消化道出血是常见的临床急重症[1],早期明确出血部位对于合理选择治疗方案、挽救患者生命具有重要意义。据文献报道,氮质血症的一个主要发生原因即在于消化道出血,其中上消化道出血更易引发此症[2-3],因而血尿素氮/肌酐(blood urea nitrogen-to-creatinine, BUN/Cr)比值已被一些学者当成上、下消化道出血的鉴别参数进行分析,但目前尚无统一结论[4-7]。此外,入院后6~48 h内血尿素氮水平动态升高,可能反映了病程早期的液体复苏不足,被认为是一种能够有效预测急性非静脉曲张性上消化道出血(acute nonvariceal upper gastrointestinal bleeding, ANVUGIB)不良结局发生的独立因素[8]。但目前尚未有评分系统将入院后BUN/Cr比值早期动态变化作为评估ANVUGIB患者预后的指标。因此,本研究通过回顾性分析消化道出血患者的临床资料,评估BUN/Cr比值在鉴别消化道出血部位中的诊断性能,同时分析BUN/Cr早期升高对于ANVUGIB患者临床结局事件的预测价值。
1. 资料与方法
1.1. 研究对象
回顾性纳入2020年5月–2021年5月在厦门大学附属中山医院确诊为消化道出血的患者。纳入标准(全部满足):①年龄≥18岁;②消化道出血部位经手术、血管造影、钡剂造影或内镜检查证实;③临床资料、实验室检查结果完整。排除标准(满足其一):①慢性肾脏病患者;②入院前给予止血、输血等特殊干预的患者;③同时存在上、下消化道出血的患者;④痔疮出血患者。纳入的ANVUGIB患者符合《急性非静脉曲张性上消化道出血诊治指南》[9]中的相关诊断标准。同一患者住院超过一次时,选择首次住院病历资料纳入研究。本研究系回顾性研究,已申请免除知情同意,研究符合赫尔辛基宣言。
1.2. 研究方法
通过电子病历系统收集消化道出血患者以下资料:①一般资料:性别、年龄、心率、血压、既往消化道出血史、合并疾病。②入院时实验室检查结果:血常规、凝血功能、BUN、Cr、白蛋白等。对于ANVUGIB患者,进一步收集以下资料:①入院后早期(6~48 h内)再次采血化验的BUN/Cr比值结果;②Rockall评分分值[10];③主要临床结局事件:A.因为任何原因死亡;B.再次出现消化道出血;C.需要急诊外科手术干预;D.需要急诊介入手术干预;④次要临床结局事件:A.需要内镜干预;B.需要输血;C.住院天数。再次出现消化道出血定义为:新鲜呕血、鼻胃管里抽出新鲜血液、新鲜黑便或血便伴有实验室检查改变(24 h内血红蛋白下降≥20 g/L)或生命征变化〔收缩压≤100 mmHg(1 mmHg=0.133 kPa)或心率≥100 min−1〕。
根据消化道出血部位,将入组患者分为上消化道出血组、小肠近段出血组(空肠上段至回肠上段)、小肠远段(回肠中段至回肠下段)及结肠出血组。对于ANVUGIB患者,将两次BUN/Cr比值检测结果(入院时、入院后6~48 h内)进行比较,若患者入院后6~48 h内BUN/Cr比值高于入院时BUN/Cr比值,且入院后6~48 h内BUN/Cr比值的绝对值高于正常参考值上限,则称为入院后BUN/Cr比值早期动态升高组,反之为入院后BUN/Cr比值非早期动态升高组。
1.3. 统计学方法
非正态分布的计量资料用四分位数、中位数表示,组间比较采用Mann-Whitney秩和检验或Kruskal-Wallis秩和检验。正态分布的计量资料用
 表示,组间比较采用独立样本t检验或单因素方差分析。以频数和百分比表示计数资料,组间比较采用χ2检验或Fisher确切概率法。通过受试者操作特征(receiver operating characteristic, ROC)曲线中的曲线下面积(area under curve, AUC)及95%置信区间(confidence interval, CI)评估BUN/Cr比值鉴别消化道出血部位的诊断性能,最佳截断值采用约登指数最大值法进行计算,同时计算灵敏度和特异度。对于ANVUGIB患者,通过ROC曲线分析,比较入院后BUN/Cr比值早期动态升高、Rockall评分系统以及两者联合指标对主要临床结局事件的预测效能。α双侧=0.05。
表示,组间比较采用独立样本t检验或单因素方差分析。以频数和百分比表示计数资料,组间比较采用χ2检验或Fisher确切概率法。通过受试者操作特征(receiver operating characteristic, ROC)曲线中的曲线下面积(area under curve, AUC)及95%置信区间(confidence interval, CI)评估BUN/Cr比值鉴别消化道出血部位的诊断性能,最佳截断值采用约登指数最大值法进行计算,同时计算灵敏度和特异度。对于ANVUGIB患者,通过ROC曲线分析,比较入院后BUN/Cr比值早期动态升高、Rockall评分系统以及两者联合指标对主要临床结局事件的预测效能。α双侧=0.05。
2. 结果
2.1. 消化道出血患者基本情况
共纳入266例消化道出血患者,平均年龄(53.67±16.48)岁,男性198例,女性68例。按出血部位不同,将患者分为3组,其中上消化道出血组204例,小肠近段出血组15例,小肠远段及结肠出血组47例。3组患者的舒张压、既往消化道出血史、血小板水平、BUN值、Cr值、BUN/Cr比值差异有统计学意义(P<0.05),其余基本情况差异均无统计学意义(P>0.05)。进一步两两比较中,小肠远段及结肠出血组与上消化道出血组比较,舒张压、既往消化道出血史、血小板水平、BUN值、BUN/Cr比值差异均有统计学意义(P<0.05);小肠远段及结肠出血组与小肠近段出血组比较,血小板水平、BUN值、BUN/Cr比值差异有统计学意义(P<0.05);小肠近段出血组与上消化道出血组比较,BUN值、Cr值差异有统计学意义(P<0.05);其余指标差异均无统计学意义(P>0.05)。见表1。
表 1. Baseline data of patients with gastrointestinal bleeding.
消化道出血患者基本情况
| Variable | UGIB group (n=204) | Proximal small intestines group (n=15) | Distal small intestines and colon group (n=47) | Test statistics | P |
| GIB: Gastrointestinal bleeding; UGIB: Upper gastrointestinal bleeding; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; CAVDs: Cardiovascular diseases; CEVDs: Cerebrovascular diseases; INR: International normalized ratio; BUN: Blood urea nitrogen; Cr: Creatinine; *P<0.05, vs. UGIB group;#P<0.05, vs. proximal small intestines group. 1 mmHg=0.133 kPa. | |||||
| Male/case (%) | 156 (76.47) | 10 (66.67) | 32 (68.09) | χ2=1.916 | 0.384 |
| Age/yr. | 54.56±16.25 | 50.00±15.60 | 50.98±17.61 | F=1.298 | 0.275 |
| Heart rate/min−1 | 92.03±17.57 | 90.33±19.36 | 93.06±16.07 | F=0.150 | 0.860 |
| SBP/mmHg | 112.03±19.98 | 118.00±17.75 | 117.81±21.37 | F=1.990 | 0.139 |
| DBP/mmHg | 66.57±13.47 | 69.20±13.73 | 72.17±14.76* | F=3.279 | 0.039 |
| Previous GIB/case (%) | 78 (38.24) | 6 (40.00) | 31 (66.00)* | χ2=12.030 | 0.002 |
| Comorbidities/case (%) | |||||
| Hypertension | 62 (30.39) | 4 (26.67) | 10 (21.28) | χ2=1.584 | 0.453 |
| Diabetes mellitus | 34 (16.67) | 1 (6.67) | 2 (4.26) | χ2=5.610 | 0.060 |
| CAVDs and CEVDs | 26 (12.75) | 1 (6.67) | 3 (6.38) | χ2=1.883 | 0.390 |
| Cirrhosis | 19 (9.31) | 1 (6.67) | 0 (0.00) | − | 0.058 |
| Hemoglobin/(g/L) | 95.85±27.13 | 85.40±25.15 | 102.21±29.59 | F=2.295 | 0.103 |
| Platelet/(×109 L−1) | 231.50±88.60 | 174.80±88.54 | 316.10±127.27*, # | F=18.686 | <0.001 |
| Albumin/(g/L) | 36.19±4.58 | 34.25±4.95 | 35.80±5.78 | F=1.174 | 0.311 |
| INR | 1.09±0.25 | 1.02±0.30 | 1.07±0.10 | F=0.865 | 0.422 |
| BUN/(mg/dL) | 32.61±13.94 | 24.09±6.46* | 12.78±5.25*, # | F=48.864 | <0.001 |
| Cr/(mg/dL) | 0.87±0.27 | 0.72±0.18* | 0.80±0.30 | F=3.087 | 0.047 |
| BUN/Cr ratio | 38.69±15.69 | 36.04±16.90 | 16.78±6.69*, # | F=43.139 | <0.001 |
2.2. ANVUGIB患者基本情况
共纳入162例ANVUGIB患者,平均年龄(54.04±16.08)岁,男性122例,女性40例。其中,入院后BUN/Cr比值早期动态升高组16例,入院后BUN/Cr比值非早期动态升高组146例。两组患者的白蛋白、BUN、BUN/Cr比值、Rockall评分系统分级(低危:0~2分,中危:3~4分,高危:≥5分)差异有统计学意义(P<0.05),其余基本情况差异均无统计学意义(P>0.05)。见表2。
表 2. Baseline data of patients with acute nonvariceal upper gastrointestinal bleeding (ANVUGIB).
ANVUGIB患者基本情况
| Variable | Early dynamic elevated
BUN/Cr ratio group (n=16) |
Non-early dynamic elevated
BUN/Cr ratio group (n=146) |
Test statistics | P |
| GIB: Gastrointestinal bleeding; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; INR: International normalized ratio; BUN: Blood urea nitrogen; Cr: Creatinine. 1 mmHg=0.133 kPa. | ||||
| Male/case (%) | 12 (75.00) | 110 (75.34) | χ2<0.001 | 1.000 |
| Age/yr. | 56.81±17.38 | 53.74±15.97 | t=0.725 | 0.470 |
| Heart rate/min−1 | 94.56±15.28 | 90.28±17.14 | t=0.958 | 0.340 |
| SBP/mmHg | 114.81±20.83 | 110.10±17.58 | t=0.999 | 0.319 |
| DBP/mmHg | 67.75±14.52 | 65.66±13.03 | t=0.601 | 0.549 |
| Previous GIB/case (%) | 4 (25.00) | 57 (39.04) | χ2=1.211 | 0.271 |
| Hemoglobin/(g/L) | 99.56±37.26 | 95.56±25.80 | t=0.419 | 0.681 |
| Platelet/×109 L−1 | 244.13±94.34 | 238.97±86.76 | t=0.224 | 0.823 |
| Albumin/(g/L) | 33.51±5.34 | 36.82±4.05 | t=−3.003 | 0.003 |
| INR | 1.07±0.12 | 1.08±0.20 | t=−0.003 | 0.974 |
| BUN/(mg/dL) | 27.19±10.60 | 34.29±13.86 | t=−1.984 | 0.049 |
| Cr/(mg/dL) | 0.94±0.24 | 0.86±0.25 | t=1.382 | 0.181 |
| BUN/Cr ratio | 29.74±12.93 | 41.10±15.11 | t=−2.892 | 0.004 |
2.3. ANVUGIB患者临床结局事件比较
入院后BUN/Cr比值早期动态升高组患者出现主要临床结局事件、再次出现消化道出血、需要急诊外科手术干预、需要急诊介入手术干预、住院时间较入院后BUN/Cr比值非早期动态升高患者均增加(P<0.05),其余临床结局事件差异均无统计学意义(P>0.05)。见表3。
表 3. Clinical outcomes of patients with ANVUGIB.
ANVUGIB患者临床结局事件
| Variable | Dynamic elevated
BUN/Cr ratio group (n=16) |
Non-dynamic elevated
BUN/Cr ratio group (n=146) |
Test statistics | P |
| GIB: Gastrointestinal bleeding; BUN: Blood urea nitrogen; Cr: Creatinine. | ||||
| Primary clinical outcomes/case (%) | 11 (68.75) | 6 (4.11) | χ2=57.450 | <0.001 |
| Death for any reason | 1 (6.25) | 0 (0.00) | − | 0.099 |
| Recurrent GIB | 11 (68.75) | 5 (3.42) | χ2=61.988 | <0.001 |
| Emergency surgical therapy | 2 (12.50) | 0 (0.00) | − | 0.009 |
| Emergency interventional therapy | 2 (12.50) | 2 (1.37) | − | 0.049 |
| Secondary clinical outcomes | ||||
| Endoscopic therapy/case (%) | 4 (25.00) | 20 (13.70) | χ2=0.701 | 0.402 |
| Blood transfusion therapy/case (%) | 8 (50.00) | 55 (37.67) | χ2=0.922 | 0.337 |
| Length of stay/d | 16.75±15.93 | 7.64±4.46 | t=2.277 | 0.038 |
2.4. BUN/Cr鉴别消化道出血部位的诊断性能
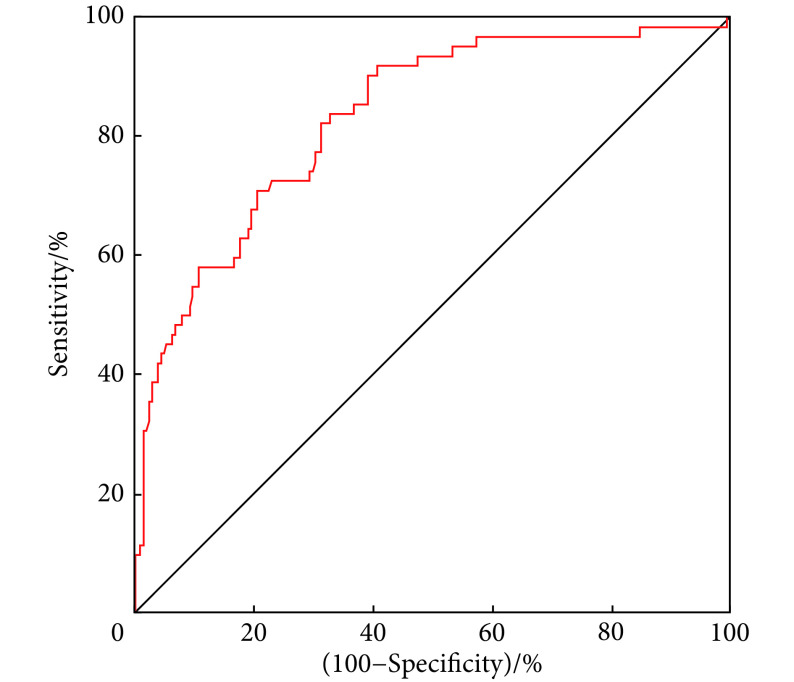
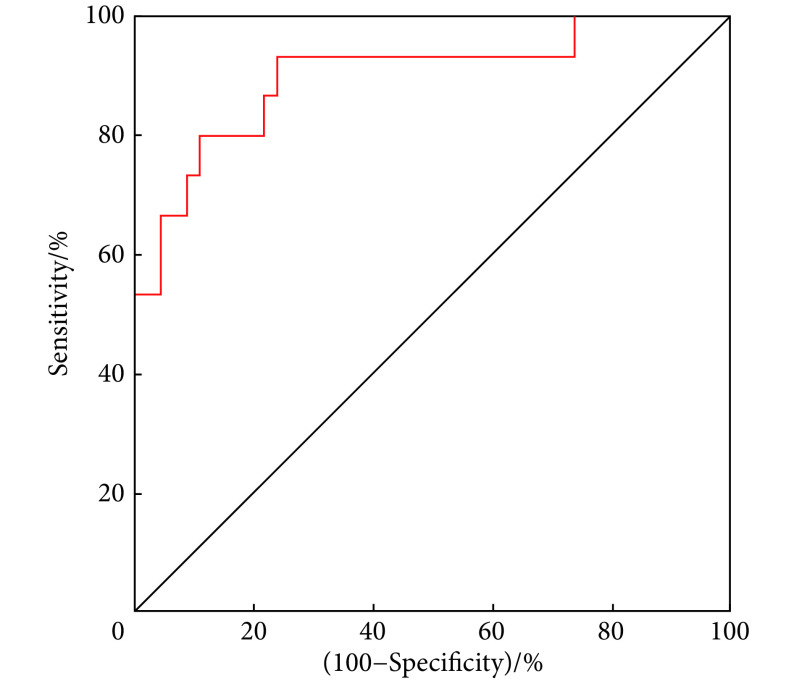
本研究运用ROC曲线及AUC分析BUN/Cr比值鉴别消化道出血的诊断性能,结果显示,BUN/Cr比值鉴别上消化道出血、下消化道出血的AUC值为0.831(95%CI:0.780~0.874),最佳截断值为34.59 mg/g,对应的灵敏度为91.94%,特异度为59.31%。在对于下消化道出血的进一步分析中,BUN/Cr比值鉴别小肠近段出血、小肠远段及结肠出血的AUC值为0.901(95%CI:0.798~0.963),最佳截断值为19.27 mg/g,对应的灵敏度为93.33%,特异度为76.09%。见图1、图2。
图 1.
ROC curve of the BUN/Cr ratio to differentiate the bleeding site between the upper (n=204) and lower gastrointestinal tract (n=62)
BUN/Cr比值鉴别上消化道出血(n=204)与下消化道出血(n=62)的ROC曲线
图 2.
ROC curve of the BUN/Cr ratio to differentiate the bleeding site between the proximal small intestines group (n=15) and the distal small intestines and colon group (n=47)
BUN/Cr比值鉴别小肠近段(n=15)与小肠远段及结肠出血(n=47)的ROC曲线
2.5. 入院后BUN/Cr比值早期动态升高、Rockall评分系统及其联合指标对ANVUGIB患者主要临床结局事件的预测价值
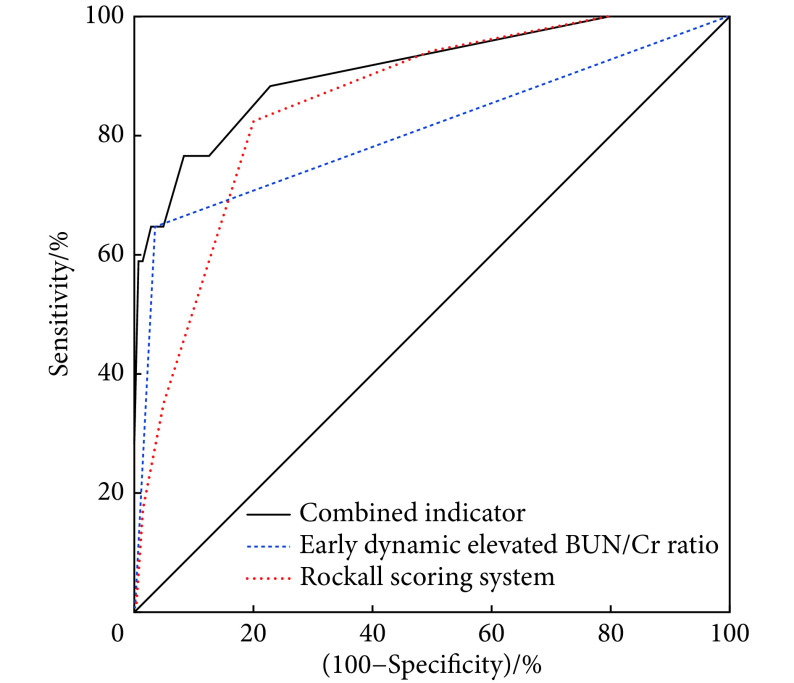
ROC曲线分析显示,入院后BUN/Cr比值早期动态升高、Rockall评分、两者联合指标预测ANVUGIB患者主要临床结局事件的AUC值分别为:0.806(95%CI:0.737~0.864)、0.855(95%CI:0.791~0.905)、0.909(95%CI:0.854~0.949)。Rockall评分系统的最佳截断值为4分,敏感度为82.35%,特异度为80.00%。见图3。将3种评价指标的AUC值进行比较,结果显示(表4)入院后BUN/Cr比值早期动态升高与Rockall评分预测ANVUGIB患者主要临床结局事件的差异无统计学意义(P>0.05),入院后BUN/Cr比值早期动态升高与联合指标预测ANVUGIB患者主要临床结局事件的差异有统计学意义(P<0.05)。
图 3.
ROC curve of the early dynamic elevated BUN/Cr ratio after admission (n=16), Rockall scoring system (n=44), and the combined indicator (n=11) for predicting the primary clinical outcomes in patients with ANVUGIB
入院后BUN/Cr比值早期动态升高(n=16)、Rockall评分系统(n=44)及其联合指标(n=11)预测ANVUGIB患者主要临床结局事件的ROC曲线
表 4. Comparison of the area under the ROC curve of the early dynamic elevated BUN/Cr ratio after admission (n=16), the Rockall scoring system (n=44), and the combined indicator (n=11) for predicting the primary outcomes in patients with ANVUGIB .
入院后BUN/Cr比值早期动态升高(n=16)、Rockall评分系统(n=44)及其联合指标(n=11)预测ANVUGIB患者主要临床结局事件的曲线下面积比较
| Scoring method | Early dynamic elevated BUN/Cr ratio | ||||
| ΔAUC | SE | 95% CI | Z | P | |
| Rockall scoring system | 0.055 | 0.065 | −0.072-0.182 | 0.844 | 0.399 |
| Combined indicator | 0.108 | 0.046 | 0.018-0.199 | 2.349 | 0.019 |
3. 讨论
早期明确出血部位并进行有效干预是降低消化道出血患者死亡率、再出血率的关键环节。临床实践中的上消化道出血与下消化道出血一般借助呕血、血便状况进行鉴别,但在相关因素(出血部位、出血量、肠道积血停留时间等)影响下,血便的颜色变化很大,使得其应用具有一定的局限性。因此,需要寻找一种能够快速、无创判断出血部位的方法,特别对于不能耐受侵入性操作的危重症患者尤为重要。此外,对于小肠出血,气囊辅助小肠镜是最主要的诊治方法之一,目前主要依赖病史、临床症状、影像学检查等来选择进镜途径,但在实际临床工作中,由于种种原因,患者经常无法及时完成相关检查,此时也需要一种指标能够指导小肠镜的进镜途径。
消化道出血引起氮质血症的机制有两种,即肠源性氮质血症和低灌注性氮质血症。前者的原因在于肠道吸收了大量的血液蛋白质分解产物,进入血液时会暂时性增加尿素氮浓度,就此引发氮质血症。后者的原因在于血容量下降、肾脏灌注减少,并弱化肾脏排泄功能,导致低灌注性氮质血症[11-12]。在本研究中,与小肠远段及结肠出血组比较,上消化道出血组和小肠近段出血组BUN水平明显升高,且位置越高,BUN水平升高越明显,这与血液在肠道中有更多的时间进行分解吸收有关,且上消化道出血组患者中以胃十二指肠消化性溃疡和食管胃底静脉曲张破裂出血为主,其出血量往往较大,更容易导致血容量下降。而小肠远段及结肠出血组基本上很少引起BUN水平升高,出血量较小,以及出血部位多位于结肠,不会过多吸收血液营养物质与代谢产物是可能原因。
在既往研究中,RICHARDS等[13]对126例成年消化道出血患者进行分析,发现BUN/Cr比值≥36 mg/g可以用作鉴别上消化道出血、下消化道出血的标准。URASHIMA等[5]纳入85例儿童消化道出血患者,证实当以BUN/Cr比值≥30 mg/g作为上、下消化道出血鉴别标准时,对应的灵敏度和特异度分别为68.8%、98.0%。同时,有国外研究者采用BUN/Cr比值≥35 mg/g[14],以及国内研究者采用BUN/Cr比值≥28.5 mg/g[15]为诊断上、下消化道出血的分界值。在本研究中,鉴别上、下消化道出血时,BUN/Cr比值的最佳截断值为34.59 mg/g,灵敏度为91.94%,特异度为59.31%,与上述国内外研究结果较为接近。同时本研究对下消化道出血部位进一步分析,对小肠近段出血组、小肠远段及结肠出血组进行了鉴别,其最佳截断值为19.27 mg/g,且具有较高的灵敏度和特异度,但是由于小肠出血患者少见且较难确诊,本研究中纳入的患者数量有限,其截断值有待进一步大样本研究来证实。
消化道出血患者病情严重程度已被证实与BUN水平相关[2, 16],且BUN/Cr比值是上消化道出血患者30 d死亡率的独立危险因素[17]。BUN水平通常会在出血几小时后升高,且峰值会在1~2 d出现,3~4 d回归正常[18],出血早期,血细胞比容、血红蛋白水平由于受到血液浓缩的影响,可以无显著变化,通常在1~3 d后方可真实体现出血的程度[19],因此与血红蛋白水平相比,BUN/Cr比值在早期识别消化道出血严重程度方面具有优势。此外,也有研究指出BUN/Cr在溶血性尿毒症综合征、急性心衰中具有重要的预测价值[20-21]。
目前研究发现,BUN水平早期升高与急性胰腺炎及消化道出血患者预后相关[8, 22-23]。在WU等[22]的研究中,急性胰腺炎患者入院24 h BUN水平较入院时每升高5 mg/dL,患者死亡风险就会显著增加(OR=2.2,95%CI:1.8~2.7)。在KARSAN等[23]的研究中,入院24 h BUN水平每升高10 mg/dL,消化道出血患者的死亡风险增加,通常会提高30%。KUMAR等[8]研究发现,入院6~48 h内BUN水平升高是ANVUGIB患者不良结局事件的预测因素。在本研究中,对于ANVUGIB患者,入院后BUN/Cr比值早期动态升高组与非早期动态升高组患者间主要临床结局事件和住院时间存在明显差异,进一步的ROC曲线分析中证实了入院后BUN/Cr比值早期动态升高对于主要临床结局事件具有较高的预测价值,且联合Rockall评分系统后,两者联合指标的预测效能得到进一步提高。对于ANVUGIB患者,恢复血容量是早期处理与治疗的关键步骤,患者入院后BUN/Cr比值早期动态升高反映出血早期液体复苏不足,以及再出血可能,从而导致更差的临床结局事件出现,因此,对于该类患者,在经过临床医师全方位评估后,若无明显禁忌症,可以考虑给与更加积极的液体复苏。
本研究不足之处:①本研究为单中心回顾性研究,其结果仍需要进一步的多中心研究加以证实;②临床决策受到医师对治疗方案的选择、患者经济情况及治疗意愿等因素影响,从而可能对患者的预后产生影响;③部分患者由于缺少初诊时及入院后6~48 h内BUN/Cr比值资料,被排除在研究之外,增加了选择偏倚;④由于患者入院后BUN/Cr比值的再次测量的时间节点不一致,可能增加了混杂偏倚。
综上所述,BUN/Cr比值对于鉴别消化道出血部位有较高的价值,且入院后BUN/Cr比值早期动态升高是预测ANVUGIB患者临床结局指标的可靠指标。
* * *
利益冲突 所有作者均声明不存在利益冲突
Contributor Information
佳兴 冯 (Jia-xing FENG), Email: jiaxingfeng05@gmail.com.
顺天 蔡 (Shun-tian CAI), Email: nktianxingjian@163.com.
References
- 1.NABLE J V, GRAHAM A C Gastrointestinal bleeding. Emerg Med Clin North Am. 2016;34(2):309–325. doi: 10.1016/j.emc.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 2.TOMIZAWA M, SHINOZAKI F, HASEGAWA R, et al Patient characteristics with high or low blood urea nitrogen in upper gastrointestinal bleeding. World J Gastroenterol. 2015;21(24):7500–7505. doi: 10.3748/wjg.v21.i24.7500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.何霞, 马万明, 刘莉 消化道出血与血清尿素氮的相关性分析. 检验医学与临床. 2012;9(10):1175–1177. doi: 10.3969/j.issn.1672-9455.2012.10.011. [DOI] [Google Scholar]
- 4.ERNST A A, HAYNES M L, NICK T G, et al Usefulness of the blood urea nitrogen/creatinine ratio in gastrointestinal bleeding. Am J Emerg Med. 1999;17(1):70–72. doi: 10.1016/S0735-6757(99)90021-9. [DOI] [PubMed] [Google Scholar]
- 5.URASHIMA M, TOYODA S, NAKANO T, et al BUN/Cr ratio as an index of gastrointestinal bleeding mass in children. J Pediatr Gastroenterol Nutr. 1992;15(1):89–92. doi: 10.1097/00005176-199207000-00014. [DOI] [PubMed] [Google Scholar]
- 6.KIM K S, KANG C H, KIM J Y Availability of blood urea nitrogen/creatinine ratio in gastrointestinal bleeding with melena in children. Pediatr Gastroenterol Hepatol Nutr. 2015;18(1):30–38. doi: 10.5223/pghn.2015.18.1.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.MACHLAB S, GARCIA-IGLESIAS P, MARTINEZ-BAUER E, et al Diagnostic utility of nasogastric tube aspiration and the ratio of blood urea nitrogen to creatinine for distinguishing upper and lower gastrointestinal tract bleeding. Emergencias. 2018;30(6):419–423. [PubMed] [Google Scholar]
- 8.KUMAR N L, CLAGGETT B L, COHEN A J, et al Association between an increase in blood urea nitrogen at 24 hours and worse outcomes in acute nonvariceal upper GI bleeding. Gastrointest Endosc. 2017;86(6):1022–1027e1. doi: 10.1016/j.gie.2017.03.1533. [DOI] [PubMed] [Google Scholar]
- 9.《中华内科杂志》编辑委员会, 《中华医学杂志》编辑委员会, 《中华消化杂志》编辑委员会, 等 急性非静脉曲张性上消化道出血诊治指南(2018年, 杭州). 中华内科杂志. 2019;58(3):173–180. [Google Scholar]
- 10.ROCKALL T A, LOGAN R F, DEVLIN H B, et al Risk assessment after acute upper gastrointestinal haemorrhage. Gut. 1996;38(3):316–321. doi: 10.1136/gut.38.3.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.COHN T D, LANE M, ZUCKERMAN S, et al Induced azotemia in humans following massive protein and blood ingestion and the mechanism of azotemia in gastrointestinal hemorrhage. Am J Med Sci. 1956;231(4):394–401. doi: 10.1097/00000441-195604000-00004. [DOI] [PubMed] [Google Scholar]
- 12.MOSS G. Editorial: Cause of azotemia after gastrointestinal hemorrhage. Examining an old wives' tale. Am J Surg, 1975, 130(3): 269[2022-04-06]. https://doi.org/10.1016/0002-9610(75)90382-7.
- 13.RICHARDS R J, DONICA M B, GRAYER D Can the blood urea nitrogen/creatinine ratio distinguish upper from lower gastrointestinal bleeding? J Clin Gastroenterol. 1990;12(5):500–504. doi: 10.1097/00004836-199010000-00004. [DOI] [PubMed] [Google Scholar]
- 14.ZIA ZIABARI S M, RIMAZ S, SHAFAGHI A, et al. Blood urea nitrogen to creatinine ratio in differentiation of upper and lower gastrointestinal bleedings; a diagnostic accuracy study. Arch Acad Emerg Med, 2019, 7(1): e30[2022-04-06]. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6637801/.
- 15.李应华, 王安秀, 吴玉怀, 等 血尿素氮/肌酐比值在上、下消化道出血鉴别诊断中的应用. 大理大学学报. 2020;5(2):80–83. doi: 10.3969/j.issn.2096-2266.2020.02.018. [DOI] [Google Scholar]
- 16.AL-NAAMANI K, ALZADJALI N, BARKUN A N, et al Does blood urea nitrogen level predict severity and high-risk endoscopic lesions in patients with nonvariceal upper gastrointestinal bleeding? Can J Gastroenterol. 2008;22(4):399–403. doi: 10.1155/2008/207850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.WU K H, SHIH H A, HUNG M S, et al The association between blood urea nitrogen to creatinine ratio and mortality in patients with upper gastrointestinal bleeding. Arab J Gastroenterol. 2018;19(4):143–147. doi: 10.1016/j.ajg.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 18.中国医师协会急诊医师分会, 中华医学会急诊医学分会, 全军急救医学专业委员会, 等 急诊上消化道出血急诊诊治流程专家共识. 中国急救医学. 2021;41(1):1–10. doi: 10.3969/j.issn.1002-1949.2021.01.001. [DOI] [Google Scholar]
- 19.柏愚 急性非静脉曲张性上消化道出血诊治指南(2015年, 南昌). 中华内科杂志. 2016;55(2):164–168. [Google Scholar]
- 20.KEENSWIJK W, VANMASSENHOVE J, RAES A, et al Blood urea nitrogen to serum creatinine ratio is an accurate predictor of outcome in diarrhea-associated hemolytic uremic syndrome, a preliminary study. Eur J Pediatr. 2017;176(3):355–360. doi: 10.1007/s00431-016-2846-z. [DOI] [PubMed] [Google Scholar]
- 21.OTTO C M Heartbeat: Blood urea nitrogen to creatinine ratio predicts outcome in acute heart failure. Heart. 2017;103(6):399–401. doi: 10.1136/heartjnl-2017-311339. [DOI] [PubMed] [Google Scholar]
- 22.WU B U, JOHANNES R S, SUN X, et al Early changes in blood urea nitrogen predict mortality in acute pancreatitis. Gastroenterology. 2009;137(1):129–135. doi: 10.1053/j.gastro.2009.03.056. [DOI] [PubMed] [Google Scholar]
- 23.KARSAN S S, NORDSTROM C, HUANG E S, et al 1081 early changes in blood urea nitrogen strongly predict mortality in acute gastrointestinal bleeding. Gastroenterology. 2012;142(5):S-193. doi: 10.1016/S0016-5085(12)60724-0. [DOI] [Google Scholar]