Abstract
The etiology and outcomes of chemical burns vary worldwide, influenced by the local population structure, industry distribution, and geographical and social environments. The aim of this study was to evaluate the epidemiology of chemical burns among patients referred to a burn centre in the north of Iran. A single‐centre, retrospective study was conducted on patients with chemical burns between 2011 and 2021. Data collection was carried out using the hospital information system (HIS), and data collected from medical records included gender, age, marital status, occupations, burn season, place of residence, intention to burn, location of the accident, percent of total body surface area (%TBSA), the primary cause of burns, the body region of the burn, length of hospital stay (days), infection, and discharge status. The data were analysed using descriptive statistical methods and SPSS 24.0 software. Of the 10 133 burn patients treated in a burn centre in the north of Iran between 2011 and 2021, 1.2% had chemical burns. The average age of patients was 34.45 (SD = 22.16) years, and most chemical burns cases were male (70.6%, n = 89). Chemical burns occurred most frequently in patients aged 20 to 49 years (69.8%, n = 107), and most of the burns were accidental (84.9%, n = 107). The home was the most common place of chemical burn injury, accounting for 49.2% (62 cases), followed by the workplace (43.7%, n = 55), respectively. Most chemical burns occurred in the summer season (36.5%, n = 46), and acid (74.6%, n = 94) was the most common cause of chemical burns. The mean TBSA was 16.41 (SD = 15.10). The most common burn area was the lower limb (34.9%, n = 44), and the overall mortality rate was 4.8%. The average length of stay in the hospital was 6.53 (SD = 5.57) days. Community education on household safety, restricting non‐specialists' access to chemical substances, and the promotion of early consultation could reduce chemical burn prevalence and improve outcomes.
Keywords: acids, alkalies, burns, chemical, epidemiology
1. INTRODUCTION
Burn is one of the most destructive types of trauma that imposes many costs on patients and health care systems. 1 , 2 , 3 , 4 , 5 , 6 , 7 According to the World Health Organization (WHO), about 180 000 people die from burns annually. 8 Burns are the third cause of death from accidents in all age groups in Iran. 2 Despite all the advances in burn treatment, burn patients often have physical and socio‐psychological problems throughout the rest of their lives after a burn injury. 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 Chemical burns are one of the most important burns that often lead to severe disabilities. 2 , 18 In the modern era, due to industry development, a wide range of chemicals are used as medicines, cleaning and disinfecting products, solvents, pesticides, fertilisers, and other things. 19 , 20 Although chemical burns account for only 3% of burns, about 30% of burn deaths are due to chemical injuries. 20 Also, chemical burns include 1.4% to 8.5% of all hospitalizations caused by burns. 18 Many chemicals cause skin, eyes, and systemic side effects. 2 These chemicals are usually acidic or basic. 21 Fluoric acid, sulfuric acid, and hydrochloric acid are the most important acidic agents, and potassium hydroxide and sodium hydroxide are alkaline agents. Acids and bases damage tissue with different mechanisms. 2 Acids cause protein denaturation, coagulation necrosis, and thick scar formation. While alkaline agents cause liquid necrosis and usually cause deeper burns than acidic agents. 19 , 20 , 22 The type of disability differs depending on the nature of the factors involved and the type of injury. 2 Chemical burns may lead to permanent loss of eyes or severe damage to the digestive system. 23 Also, they often significantly decrease the patient's physical and mental quality of life. 8 Therefore, these types of burns need special attention. 23 The amount and concentration of the substance, the pH level, and the duration of contact with the agent and the contact surface affect the severity of chemical burns. 19 , 20 The factors causing chemical burns may differ based on the geographical area, the industrialization level, and the population type. 18 , 19 To prevent chemical burns and adopt effective laws to protect at‐risk populations, epidemiological studies on the prevalence and characteristics of this type of injury are essential. 2 , 18 Despite the studies conducted on the epidemiology of burns in Iran, few comprehensive studies of chemical burns have been done so far. So that there are only two epidemiological studies of burns caused by chemical and caustic substances in East Azerbaijan 20 and Shiraz. 2 Other studies examine only the incidence of acid burns and acid attacks or the epidemiology of burns from all causes in one region, medical centre, or one age group or gender. On the other hand, the importance of this study is because of the lasting effect of this type of burn, the impact of severe scars on the mental condition of patients, the lack of primary information in the province, and the need to evaluate long‐term complications in the future. Therefore, the present study was conducted to determine the most common causes of chemical burns and related factors in a burn centre in the north of Iran. The results of this analysis can help plan prevention strategies for high‐risk groups and correct the treatment of chemical burns.
2. MATERIALS AND METHODS
2.1. Study design and setting
A retrospective, single‐centre study was conducted of all chemical burns admitted to the emergency department of a burns centre in the north of Iran between 2011 and 2021. This centre is the only burn centre in Guilan province, with 55 beds in the burn ward and 10 beds in the burn ICU. It has approximately 700 admissions annually, covering all burn patients in the province and some adjacent provinces. All information was obtained from the hospital information system (HIS). Burn patients' records were selected according to the International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD‐10), categories for burns and corrosions codes (T20‐T32). The inclusion criteria for the study include a hospitalisation period of more than 24 h. We excluded subjects with chemical burns who were referred to hospitals for outpatient care and readmission.
Patients' information was collected through a researcher‐made information registration form, including a demographic and incident‐related section, by a trained questioner through medical records. The data collected from medical records included gender, age, marital status, occupations, burn season, place of residence, intention to burn, location of the accident, percent of total body surface area (%TBSA), the primary cause of burns, the body region of the burn, length of hospital stay (days), infection, and discharge status.
2.2. Statistical analysis
Statistics analysis was conducted using the SPSS software package (version 24.0, SPSS Inc., Chicago, IL, USA). There was no missing data. Continuous variables are presented as means, and standard deviation (SD) and categorical variables are presented as frequencies and percentages.
2.3. Ethics
The Guilan University of Medical Sciences Ethics Committee approved this study (IR.GUMS.REC.1401.202). This was a retrospective study, and the patient's consent was not used.
3. RESULTS
3.1. Tendency of chemical burns
Of 10 133 burn patients hospitalised in our burn centre between 2011 and 2021, 1.2% (n = 126) had chemical burns. Figure 1 shows the frequency of chemical burn patients hospitalised each year. Our data showed that since 2018, the frequency of chemical burns has declined, although a slight fluctuation in this trend was observed between 2018 and 2019.
FIGURE 1.
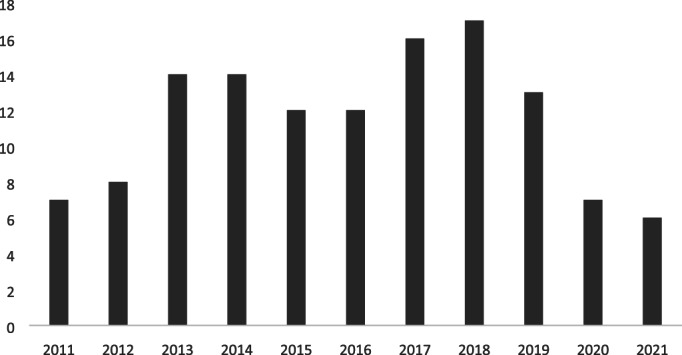
The number of chemical burns from 2011 to 2021.
3.2. Basic demographic characteristics
The mean age of patients was 34.45 (SD = 22.16) years, ranging from 1 to 94 years old. The 30 to 39 age group (28.6%, n = 36) accounted for the highest proportion of total chemical burns, followed by the 20 to 29 age group (21.4%, n = 27) and the 40 to 49 age group (19.8%, n = 25). Most chemical burn patients were male (70.6%, n = 89), married (73.0%, n = 92), and lived in urban areas (63.5%, n = 80). Workers accounted for the majority (66.7%, n = 84), followed by unemployment (20.6%, n = 26), housewives (5.6%, n = 7), and clerks (4.0%, n = 5) (Table 1).
TABLE 1.
Baseline characteristics of burns patients (n = 126).
| Variables | N | Percentage (%) |
|---|---|---|
| Age | ||
| <10 | 10 | 7.9 |
| 10 to 19 | 6 | 4.8 |
| 20 to 29 | 27 | 21.4 |
| 30 to 39 | 36 | 28.6 |
| 40 to 49 | 25 | 19.8 |
| 50 to 59 | 14 | 11.1 |
| >60 | 8 | 6.3 |
| Gender | ||
| Male | 89 | 70.6 |
| Female | 37 | 29.4 |
| Marital status | ||
| Single | 34 | 27.0 |
| Married | 92 | 73.0 |
| Occupations | ||
| Worker | 84 | 66.7 |
| House wife | 7 | 5.6 |
| Clerk | 5 | 4.0 |
| Retired | 4 | 3.2 |
| Unemployment | 26 | 20.6 |
| Place of residence | ||
| Urban | 80 | 63.5 |
| Rural | 46 | 36.5 |
| Season distribution | ||
| Spring | 25 | 19.8 |
| Summer | 46 | 36.5 |
| Autumn | 26 | 20.6 |
| Winter | 29 | 23.0 |
| TBSA (%) | ||
| <10 | 55 | 43.7 |
| 11 to 20 | 39 | 31.0 |
| 21 to 30 | 14 | 11.1 |
| 31 to 40 | 6 | 4.8 |
| 41 to 50 | 5 | 4.0 |
| >50 | 7 | 5.6 |
| The body region of burn | ||
| Head and Neck | 14 | 11.1 |
| Trunk | 23 | 18.3 |
| Upper limb | 30 | 23.8 |
| Lower limb | 44 | 34.9 |
| Total body | 15 | 11.9 |
| Intention to burn | ||
| Self‐immolation | 2 | 1.6 |
| Accidental | 107 | 84.9 |
| Assault)Homicidal( | 7 | 5.6 |
| Unknown | 10 | 7.9 |
| Location of the accident | ||
| Home | 62 | 49.2 |
| Workplace | 55 | 43.7 |
| Outdoor | 9 | 7.1 |
| Discharge status | ||
| Recovered | 120 | 95.2 |
| Death | 6 | 4.8 |
| Infection | 23 | 18.3 |
| Length of stay (Mean [SD]) | 6.53 (SD = 5.57) | |
3.3. Location and causes of chemical burns
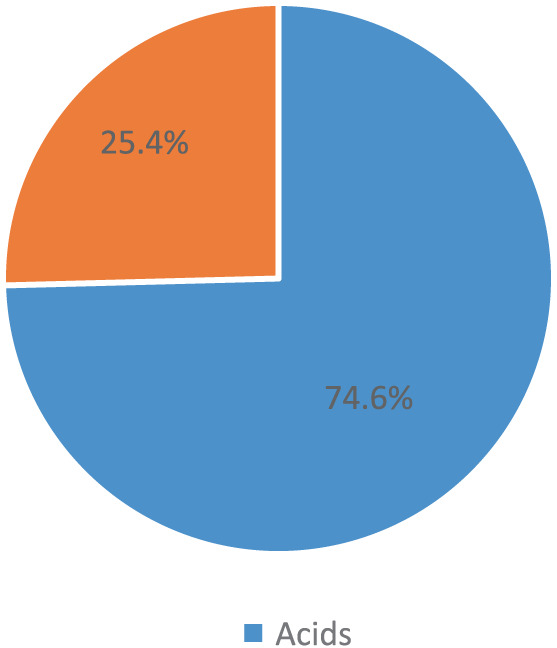
The majority of the chemical burns were accidental (84.9%, n = 107). Also, seven assault cases (5.6%) and two self‐immolation cases (1.6%) using chemicals were observed during the study period. Most burns occurred at home (49.2%, n = 62) and workplace (43.7%, n = 55). Acid (74.6%) was the most common cause of injury (Figure 2).
FIGURE 2.
The seasonal distribution of chemical burn
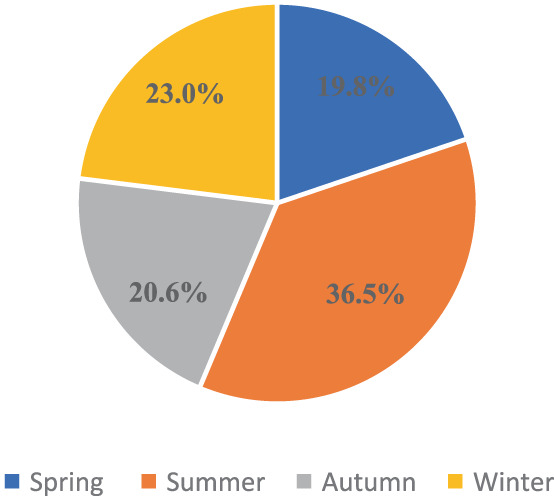
3.4. Season distribution
Figure 3 displays the distribution of chemical burns by season. Chemical burns occurred more frequently in the summer (36.5%, n = 46) than in the winter (23.0%, n = 29), autumn (20.6%, n = 26), and spring (19.8%, n = 25).
FIGURE 3.
Nature of chemical burn
3.5. Extent of chemical burns
The average burn area was 16.4 (SD = 15.1%) of the TBSA, with a 2% to 90% TBSA range. Regarding TBSA, 55 patients (43.7%) had a TBSA <10%, 39 (31.0%) had a TBSA of 11% to 20%, 14 (11.1%) had a TBSA between 21% and 30%, and 18 (14.2%) had TBSA≥31%.
3.6. Sites of chemical burns
The lower limb region was found to be the most common body region for burns, accounting for 34.9% (n = 44) of the total injury.
3.7. Length of stay (LOS) and mortality
The LOS in the hospital was 6.53 (SD = 5.57) days. The mortality prevalence in chemical burns was 4.8% (n = 6).
4. DISCUSSION
In some parts of the world, chemical burns are widespread, and their prevalence has grown over the past few decades. Chemical damage can be catastrophic and cause considerable morbidity if not treated effectively. On the other hand, epidemiological analyses of chemical burns are essential to understanding the incidence characteristics and adopting effective preventive actions. Therefore, the aim of this study was to evaluate the incidence and characteristics of chemical burns among the patients referred to a burn centre in the north of Iran from 2011 to 2021.
The present study's incidence rate of chemical burns was 1.2%, which was similar to other studies. 18 , 24 However, compared with developed countries, the incidence of chemical burns in Iran is low. 25 The present study confirmed previous findings that acidic substances are the most common aetiology for chemical burns. 2 , 19 , 23 , 26 The best way to cure acid chemical burns is to wash them immediately with copious amounts of water. Also, chemical burns caused by alkalis accounted for only 25.4% of burns, similar to a study conducted in southwestern China. 23 Strong alkalis can destroy tissue by dehydrating cells, liquefying proteins, and saponifying lipids. Therefore, it is essential to emphasise the need for prompt diagnoses and treatments for alkali burns.
Moreover, most chemical burns occurred between the ages of 20 and 49. The working age is the most common age group in which chemical burns occur. 27 In a study in China, it was reported that the working age of 30 to 49 years old comprised 67.25% of all chemical burn admissions. 26
The ratio of hospitalised chemical burn patients from urban areas was higher than in rural areas.
Most of the chemical burns occurred at home. There needs to be increased community awareness regarding household chemicals. Because Guilan Province is not considered one of the country's industrial areas, it can justify the high domestic chemical burns compared with other studies. However, a study in Bulgaria showed that the prevalence of domestic chemical burns is higher than that of industrial chemical burns. 28 In addition, our study found that 43.7% of chemical burns occurred in the workplace. For personal protection in the workplace against chemical burns, it is necessary to use personal protective equipment, such as masks and protective equipment, when working with machinery or chemicals. These findings emphasise the importance of workplace safety and draw attention to many businesses’ weaknesses in occupational development and training, equipment maintenance, and production management.
In the present study, in terms of jobs, most of the chemical burns occurred among workers. According to research conducted in China, “workers” accounted for 64.7% of all hospitalisations for chemical burns. 29 This study's results showed that the incidence of chemical burns in males was higher than in females. This could be due to men's involvement in a more dangerous work environment than females. In contrast, a study conducted in India found that women (54%) sustained injuries more frequently than men, 19 which may potentially be related to the high rates of assault (29%) and suicide (13%). In comparison to other seasons, summer was the most common time for chemical burns. This was likely because summer is a busy period for municipal industrial production and construction, which consisted of a study by Maghsoudi et al. 20 Regarding the anatomical location of chemical burns, the lower limb was the most common area for chemical burns, which is similar to previous studies. 29 However, other research indicated that the most common burn regions were the head, face, neck, or upper extremities. 19 , 26
In this study, the average LOS was 6.53 ± 5.57 days, which was significantly lower than in other studies. 23 , 26 Considering that LOS and mortality increase with increasing TBSA. Compared with other studies, the short LOS of chemical burn patients in this study is probably related to the low average TBSA. In comparison with a study by Barillo et al., the mortality rate in our population was lower. 30 This may be because most patients in the present study had a burn percentage of less than 10% (TBSA<10).
4.1. Limitations
One of the limitations of the current research is the small sample size of chemical burn patients. Also, because of the lack of registration of the type of chemical substance leading to burns in the patient's medical records, we could not perform further analysis on the acidic and alkaline substances. In addition, only six deaths from chemical burns were reported in the current study. Because of insufficient data, it was impossible to analyse the risk factors associated with death.
4.2. Implications for health managers and policymakers
According to the present study and the existing limitations, it is suggested to use registry systems suitable for the region. Because of the lack of data, using the data in regions similar to those investigated in terms of urban and industrial elements can help understand the existing solutions better; on the other hand, teaching prevention strategies and necessary home preliminary measures can be a practical approach, especially if it is compatible with the traditional environment of that region.
4.3. Suggestions for future studies
It is recommended that future studies, while addressing the epidemiology of chemical burns in a multicentre and with a larger population, consider variables affecting the epidemiology of chemical burns and different burn factors.
5. CONCLUSION
The study's results showed that men and those who lived in cities were more likely to have chemical burns. The prevalence of chemical burns at home and then at work was higher than in other cases. The chemical burns rate among workers was higher than in other occupational groups. Also, to decrease the frequency of chemical burns, it is advised to teach prevention strategies to protect people from chemical burns. Community education on household safety, restricting non‐specialists’ access to chemical substances, and the promotion of early consultation could reduce chemical burn prevalence and improve outcomes.
FUNDING INFORMATION
The authors received no financial support for the research, authorship, and publication of this article.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest.
ETHICS STATEMENT
This research was approved by the Ethics Committee of Guilan University of Medical Sciences (IR.GUMS.REC.1401.202). Patient informed consent was not acquired due to the use of previously gathered data from the hospital information system; nevertheless, the names of patients were not gathered from the database for ethical reasons.
Eftekhari H, Sadeghi M, Mobayen M, et al. Epidemiology of chemical burns: An 11‐year retrospective study of 126 patients at a referral burn centre in the north of Iran. Int Wound J. 2023;20(7):2788‐2794. doi: 10.1111/iwj.14155
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Mobayen M, Zolfagharzadeh H, Feizkhah A, et al. Application of cell appendages for the management of burn wounds. Burn J Int Soc Burn Inj. 2022;48:S0305‐S4179. [DOI] [PubMed] [Google Scholar]
- 2. Abbasi H, Dehghani A, Mohammadi AA, Ghadimi T, Keshavarzi A. The Epidemiology of Chemical Burns Among the Patients Referred to Burn Centers in Shiraz, Southern Iran, 2008–2018. Bull Emerg Trauma. 2021;9(4):195‐200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Akhoondian M, Zabihi MR, Yavari S, et al. Identification of TGF‐β1 expression pathway in the improvement of burn wound healing. Burn J Int Soc Burn Inj. 2022;48(8):2007‐2010. [DOI] [PubMed] [Google Scholar]
- 4. Rangraz Jeddi F, Mobayen M, Feizkhah A, Farrahi R, Heydari S, Bagheri Toolaroud P. Cost analysis of the treatment of severe burn injuries in a tertiary burn center in Northern Iran. Iran. Red. Crescent. Med. J. [Internet]. 2022. [cited 2023 Mar 7] 24(5). Available from: https://www.ircmj.com/index.php/IRCMJ/article/view/1522 [Google Scholar]
- 5. Mehrabi A, Falakdami A, Mollaei A, et al. A systematic review of self‐esteem and related factors among burns patients. Ann Med Surg. 2022;84:104811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Parvizi A, Haddadi S, Ghorbani Vajargah P, et al. A systematic review of life satisfaction and related factors among burns patients. Int Wound J. 2023;1‐13. 10.1111/iwj.14120 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 7. Zabihi MR, Akhoondian M, Tajik MH, Mastalizadeh A, Mobayen M, Karkhah S. Burns as a risk factor for glioblastoma. Burns. 2023;49(1):236‐241. [DOI] [PubMed] [Google Scholar]
- 8. Almarghoub MA, Alotaibi AS, Alyamani A, et al. The epidemiology of burn injuries in Saudi Arabia: a systematic review. J Burn Care Res. 2020;41(5):1122‐1127. [DOI] [PubMed] [Google Scholar]
- 9. Norouzkhani N, Ghazanfari MJ, Falakdami A, et al. Implementation of telemedicine for burns management: challenges and opportunities. Burns. 2023;49(2):482‐484. [DOI] [PubMed] [Google Scholar]
- 10. Norouzkhani N, Chaghian Arani R, Mehrabi H, et al. Effect of virtual reality‐based interventions on pain during wound care in burn patients; a systematic review and meta‐analysis. Arch Acad Emerg Med [Internet]. 2022. [cited 2023Mar.7];10(1):e84. Available from: https://journals.sbmu.ac.ir/aaem/index.php/AAEM/article/view/1756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Farzan R, Firooz M, Ghorbani Vajargah P, et al. Effects of aromatherapy with Rosa damascene and lavender on pain and anxiety of burn patients: A systematic review and meta‐analysis. Int Wound J. 2023;1‐14. 10.1111/iwj.14093 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 12. Miri S, Hosseini SJ, Ghorbani Vajargah P, et al. Effects of massage therapy on pain and anxiety intensity in patients with burns: A systematic review and meta‐analysis. Int Wound J. 2023;1‐19. 10.1111/iwj.14089 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 13. Asadi K, Aris A, Fouladpour A, Ghazanfari MJ, Karkhah S, Salari A. Is the assessment of sympathetic skin response valuable for bone damage management of severe electrical burns? Burn J Int Soc Burn Inj. 2022;48(8):2013‐2014. [DOI] [PubMed] [Google Scholar]
- 14. Salari A, Fouladpour A, Aris A, Ghazanfari MJ, Karkhah S, Asadi K. Osteoporosis in electrical burn injuries. Burn J Int Soc Burn Inj. 2022;48:S0305‐S4179. [DOI] [PubMed] [Google Scholar]
- 15. Chen J, Li‐Tsang CWP, Yan H, et al. A survey on the current status of burn rehabilitation services in China. Burns. 2013;39(2):269‐278. [DOI] [PubMed] [Google Scholar]
- 16. Ghazanfari M, Mazloum S, Rahimzadeh N, et al. Burns and pregnancy during the COVID‐19 pandemic. Burn J Int Soc Burn Inj. 2022;48:2015‐2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Akhoondian M, Zabihi MR, Yavari S, et al. Radiation burns and fertility: a negative correlation. Burn J Int Soc Burn Inj. 2022;48(8):2017‐2019. [DOI] [PubMed] [Google Scholar]
- 18. Koh D‐H, Lee S‐G, Kim H‐C. Incidence and characteristics of chemical burns. Burns [Internet]. 2017;43(3):654‐664. Available from: https://www.sciencedirect.com/science/article/pii/S030541791630345X [DOI] [PubMed] [Google Scholar]
- 19. Akhtar MS, Ahmad I, Khurram MF, Kanungo S. Epidemiology and outcome of chemical burn patients admitted in burn unit of JNMC Hospital, Aligarh Muslim University, Aligarh, Uttar Pradesh, India: A 5‐year experience. J Family Med Prim Care. 2015;4(1):106‐109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Maghsoudi H, Gabraely N. Epidemiology and outcome of 121 cases of chemical burn in East Azarbaijan province. Iran Inj. 2008;39(9):1042‐1046. [DOI] [PubMed] [Google Scholar]
- 21. Nguyen A, Chamberlain K, Holland AJA. Paediatric chemical burns: a clinical review. Eur J Pediatr. 2021;180(5):1359‐1369. [DOI] [PubMed] [Google Scholar]
- 22. Akelma H, Karahan ZA. Rare chemical burns: review of the literature. Int Wound J. 2019;16(6):1330‐1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wang Y, Yu X, Qian W, et al. Epidemiologic investigation of chemical burns in Southwestern China from 2005 to 2016. J Burn Care Res. 2018;39(6):1006‐1016. [DOI] [PubMed] [Google Scholar]
- 24. Seo DK, Kym D, Yim H, et al. Epidemiological trends and risk factors in major burns patients in South Korea: a 10‐year experience. Burns. 2015;41(1):181‐187. [DOI] [PubMed] [Google Scholar]
- 25. Greenwood JE, Tan JL, Ming JCT, Abell AD. Alkalis and skin. J Burn Care Res. 2016;37(2):135‐141. [DOI] [PubMed] [Google Scholar]
- 26. Ye C, Wang X, Zhang Y, et al. Ten‐year epidemiology of chemical burns in western Zhejiang Province, China. Burns [Internet]. 2016;42(3):668‐674. Available from: https://www.sciencedirect.com/science/article/pii/S0305417915003940 [DOI] [PubMed] [Google Scholar]
- 27. Ramakrishnan KM, Mathivanan T, Jayaraman V, Babu M, Shankar J. Current scenario in chemical burns in a developing country: Chennai, India. Ann Burns Fire Disasters. 2012;25(1):8. [PMC free article] [PubMed] [Google Scholar]
- 28. Vaglenova E. Chemical Burns‐Epidemiology. Ann Burns Fire. Disasters. 1997;10:16‐19. [Google Scholar]
- 29. Xie Y, Tan Y, Tang S. Epidemiology of 377 patients with chemical burns in Guangdong province. Burns. 2004;30(6):569‐572. [DOI] [PubMed] [Google Scholar]
- 30. Barillo DJ, Cancio LC, Goodwin CW. Treatment of white phosphorus and other chemical burn injuries at one burn center over a 51‐year period. Burns. 2004. Aug;30(5):448‐452. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


