Abstract
The ability of knowledge, attitude, and practice of intensive care unit (ICU) nurses to perform medical device‐related pressure injuries (MDRPIs) can affect the incidence of MDRPI in ICU patients. Therefore, in order to improve ICU nurses' understanding and nursing ability of MDRPIs, we investigated the non‐linear relationship (synergistic and superimposed relationships) between the factors influencing ICU nurses' ability of knowledge, attitude, and practice. A Clinical Nurses' Knowledge, Attitude, and Practice Questionnaire for the Prevention of MDRPI in Critically Ill Patients was administered to 322 ICU nurses from tertiary hospitals in China from January 1, 2022 to June 31, 2022. After the questionnaire was distributed, the data were collected and sorted out, and the corresponding statistical analysis and modelling software was used to analyse the data. IBM SPSS 25.0 software was used to conduct Single factor analysis and Logistic regression analysis on the data, so as to screen the statistically significant influencing factors. IBM SPSS Modeler18.0 software was used to construct a decision tree model of the factors influencing MDRPI knowledge, attitude, and practice of ICU nurses, and ROC curves were plotted to analyse the accuracy of the model. The results showed that the overall passing rate of ICU nurses' knowledge, attitude, and practice score was 72%. The statistically significant predictor variables ranked in importance were education background (0.35), training (0.31), years of working (0.24), and professional title (0.10). AUC = 0.718, model prediction performance is good. There is a synergistic and superimposed relationship between high education background, attended training, high years of working and high professional title. Nurses with the above factors have strong MDRPI knowledge, attitude, and practice ability. Therefore, nursing managers can develop a reasonable and effective scheduling system and MDRPI training program based on the study results. The ultimate goal is to improve the ability of ICU nurses to know and act on MDRPI and to reduce the incidence of MDRPI in ICU patients.
Keywords: decision trees; knowledge, attitude, and practice; medical devices; nurses; pressure injury
1. INTRODUCTION
The term “medical device‐related pressure injury (MDRPI)” was first introduced by Black et al. 1 The 2014 edition of the international Pressure Injury Prevention and Treatment: A Guide to Clinical Practice contains the first definition of MDRPIs. 2 The 2014 edition of the International Guidelines for the Prevention and Treatment of Pressure‐related Injuries: Clinical Practice provides the first specific definition of a MDRPI and suggests intervention strategies and guidance for the prevention of MDRPI. In 2016, a guideline developed by the US Pressure Ulcer Advisory Panel (NPUAP), 3 guidelines developed by the NPUAP expanded the definition of pressure injury to include “medical devices” and referred to pressure ulcers caused by medical devices as MDRPI.
MDRPI is a pressure injury caused by the use of medical devices used for diagnostic or therapeutic purposes, such as casts, ventilator masks, tracheal intubation machines to fix stents, etc. 4 The most common sites of injury are the nose, fingers and ears. 5 , 6 The shape of the injury is often consistent with the shape of the medical devices. The prevalence of MDRPI in critically ill patients in the intensive care unit (ICU) is due to the frequent use of various medical devices, extensive drug therapy and patients' own characteristics such as skin edema. 7 , 8 , 9 , 10 It is now one of the more serious adverse events in ICU patients. 11 , 12 Some studies ICU nurses, as the closest caregivers to critically ill patients play a critical role in identifying critically ill patients at risk of MDRPI. 13 , 14 The ability of ICU nurses to know and act on their knowledge of MDRPI largely determines their preventive and interventional behaviour toward patients at risk of developing MDRPI. 15 , 16 However, most studies have shown that ICU nurses have the problem of insufficient MDRPI ability of knowledge, attitude, and practice. 17
Therefore, It is necessary to investigate the factors influencing ICU nurses' ability of knowledge, attitude, and practice. However, most studies have only used traditional statistical methods to investigate the linear relationship between the factors influencing ICU nurses' knowledge, attitude, and practice competence, without predicting and evaluating the synergistic and superimposed effects between the factors influencing ICU nurses' knowledge, attitude, and practice competence, or ranking the importance of the influencing factors. Therefore, this study analysed the non‐linear relationships (synergistic and superimposed relationships) among the factors influencing ICU nurses' MDRPI knowledge, attitude, and practice ability through a decision tree algorithm. The ranking of the importance of influencing factors and exploring the differences of ICU nurses in MDRPI knowledge, attitude, and practice ability, providing reference for nursing managers to develop more accurate Scheduling systems and MDRPI training programs. Finally, the purpose of improving the MDRPI knowledge, attitude, and practice ability of ICU nurses and reducing the incidence of MDRPI in ICU patients is achieved.
2. MATERIALS AND METHODS
2.1. Approach
The study consists of three phases. The first stage is the distribution of the questionnaire, aiming to investigate the general information of ICU nurses and the current situation of pressure injuries related to medical devices. The second stage is data collection and collation, aiming to delete unqualified questionnaires or questionnaires with missing data to ensure that the final survey results are true and effective. The third stage is data analysis, including general data analysis, Single‐factor analysis, Logistic regression analysis and model construction, etc. The purpose is to obtain the factors affecting nurses' ability to know, belief and practice, and make the results more clear and accurate through figures and models.
2.2. Samples and setting
A medical device related pressure injury knowledge, attitude and practice questionnaire was administered to 322 ICU nurses from tertiary hospitals in China from January 1, 2022 to June 31, 2022. Sample size calculation: the ratio of the number of entries to the sample size was 1:5 to 10, 18 according to the ratio of 1:10, the number of predictor variables included in the study was 9, so the minimum sample size required was 90. Inclusion criteria: obtained professional qualification as a nurse; worked in ICU for more than 1 year. Exclusion criteria: nurses who were not on duty during the survey period (on leave, studying away, etc.); questionnaire response time less than 300 seconds. The respondents of this study gave their informed consent and voluntarily participated in this study. A total of 322 nurses were finally included according to the inclusion and exclusion criteria.
2.3. Data collection
2.3.1. Data collection instruments
General information questionnaire
After reviewing relevant literature and data and combining with clinical practice, we developed our own general information questionnaire, including age, gender, department, years of working, professional title, position, education background, forms of employment, and MDRPI knowledge and skills training.
MDRPI knowledge, attitude, and practice questionnaire
The clinical nurses' knowledge, attitude, and practice questionnaire for the Prevention of MDRPI in critically ill patients was created by Yu‐ding Hu in 2018. 19 The scale is divided into three dimensions: “knowledge, attitude, and practice”, and the first dimension are to investigate the knowledge of ICU nurses about MDRPI, including the definition of MDRPI, causes of occurrence, prevalent sites, injury stages, criteria for different stages, risk factors, assessment tools, prevention measures, treatment points, learning initiatives, academic lectures or training, and whether they have cared for MDRPI patients. The second dimension is a survey on ICU nurses' attitudes toward MDRPI prevention and care, which includes participation in training to help nurses better prevent MDRPI occurrence, prevention is more important than treatment, the vast majority of MDRPI can be avoided, the importance of continuous assessment and daily care, the importance of MDRPI training, and the importance of developing standardised nursing processes in 9 parts. The third dimension is mainly a survey on ICU nurses' MDRPI prevention and nursing practice, mainly including the frequency of taking nursing measures to prevent the occurrence of MDRPI, the MDRPI occurrence reporting behaviour, and nursing examination recording behaviour in 14 parts. A total of 38 entries can be used to comprehensively evaluate the knowledge, attitude, and practice of clinical nurses in preventing MDRPI in critically ill patients. The scale uses the Likert 5‐point scale, with a total score of 38–190 and 114 points passing, the higher the score, the higher the level of clinical nurses' knowledge, attitude, and practice in preventing MDRPI in critically ill patients. The total scale Cronbach's α coefficient was 0.962, and the reliability was >0.9. When applying the scale survey, the survey completion time should be between 5 and 10 min.
2.3.2. Data collection method
With the consent of the hospital nursing department and the head nurses of the departments, questionnaires were distributed to nurses through the Questionnaire Star online platform. Nurses could fill in the questionnaires through their mobile phones or computer terminals, and each IP address could only be filled in once to avoid duplicate submissions from survey respondents. After the questionnaires were collected by the researcher, two people checked and double‐entered the data, eliminating those questionnaires that took less than 5 minutes to answer and those that showed obvious regularity of answers. In the end, 322 valid questionnaires were obtained.
2.4. Data analysis
SPSS 25.0 was used for data entry and analysis. Count data were expressed as number of cases (percentage), and comparisons between groups were made using the pearson χ 2 test, Pearson's continuous corrected χ 2 test or Fisher's exact probability method. Single‐factor analysis and Logistic regression analysis were used to screen candidate predictor variables, and chi‐square test was used for single‐factor analysis, with predictor inclusion criteria of 0.1 and 0.05, respectively. SPSS Modeller 18.0 was used to construct the CART classification tree model, setting the ratio of the training and test sets to 7:3, the number of random seeds to 2 147 371 679, the maximum tree depth was set to 10, and the tree model was pruned to prevent over fitting. The maximum risk difference was set to 1, the minimum number of records in the parent branch was 2%, the minimum number of records in the child branch was 1%, the significance level for both split nodes and merged categories was 0.05, and the model output was oriented from left to right. The predictive value of the model was assessed using the area under curve (AUC) of the receiver operating characteristic (ROC) curve.
2.5. Ethical considerations
Consent was obtained from the head nurses before the start of the study. The ICU nurses participating in the study participated in the study voluntarily. This study passed the review by the hospital ethics committee.
3. RESULTS
3.1. General information questionnaire for ICU nurses
A total of 322 nurses from 13 departments were included in the study, with the majority of nurses coming from specialist ICU. The male to female ratio was roughly 1:4. 61.8% of the nurses were aged 18 to 30 years. The highest proportion of nurses (32.2%) had 6 to 10 years of working experience. The highest proportion of nurses were general nurses (92.5%) and only 5% were pressure sore organisation liaison officer. The highest level of education background was a master's degree with only 4 (1.2%) and the highest number of nurses with a bachelor's degree (69.6%). Only 12.8% of the nurses had N3 or higher in the nursing competency level. The number of nurses who had not attended training was 90 (28%). The results are shown in Table 1.
TABLE 1.
General information on ICU nurses [n (%), N = 322].
| General information | n (%) | General information | n (%) |
|---|---|---|---|
| Departments | Position | ||
| Obstetric ICU | 8 (2.50%) | General nurse | 298 (92.50%) |
| Cardiovascular ICU | 27 (8.40%) | Pressure sore | 16 (5%) |
| Respiratory medicine ICU | 41 (12.70%) | Organisation liaison | |
| Emergency department ICU | 16 (5.00%) | Officer | |
| ICU, burns unit | 25 (7.80%) | Head nurse | 8 (2.50%) |
| Orthopaedic ICU | 34 (10.60%) | Professional title | |
| Neurology ICU | 16 (5.00%) | Nurse | 112 (34.80%) |
| Neurosurgery ICU | 25 (7.80%) | Senior nurse | 129 (40.10%) |
| Gastroenterology ICU | 28 (8.70%) | Supervisor nurse | 78 (24.20%) |
| Cardiovascular medicine ICU | 21 (6.50%) | Associate chief nurse or above | 3 (0.90%) |
| Cardiothoracic surgery ICU | 25 (7.80%) | Education background | |
| Department of intensive care medicine | 39 (12.10%) | Masters or above | 4 (1.20%) |
| Coronary care unit | 17 (5.30%) | Bachelor degree | 224 (69.60%) |
| Gender | Three‐year college education or below | 94 (29.20%) | |
| Male | 60 (18.60%) | Forms of employment | |
| Female | 262 (81.40%) | Contract system | 261 (81.10%) |
| Age | Personnel agents | 6 (1.90%) | |
| 18 to 30 | 199 (61.80%) | Preparation | 55 (17.10%) |
| 31 to 40 | 110 (34.20%) | Nursing competence level | |
| >40 | 13 (4.00%) | N0 | 11 (3.40%) |
| Years of working | N1 | 135 (41.90%) | |
| 1 to 2 | 91 (28.30%) | N2 | 135 (41.90%) |
| 3 to 5 | 69 (21.40%) | N3 | 34 (10.60%) |
| 6 to 10 | 104 (32.30%) | N4 | 7 (2.20%) |
| 11 to 20 | 43 (13.40%) | Training | |
| >20 | 15 (4.70%) | Yes | 232 (72.00%) |
| No | 90 (28.00%) |
3.2. Assignment of factors influencing ICU nurses' MDRPI knowledge, attitude, and practice
The influencing variables in the general data are numbered and assigned to facilitate the analysis of the study data. The influence variables were all categorical variables, with successively assigned values 1, 2, 3, etc. The results are shown in Table 2.
TABLE 2.
Assignment of factors influencing ICU nurses' MDRPI knowledge, attitude, and practice.
| Variables | Number | Assignment |
|---|---|---|
| Age | X1 | 1: 18 to 30 years; 2: 31 to 40 years; 3: >40 years |
| Gender | X2 | 1: Male; 2: Female |
| Years of working | X3 | 1: 1 to 2 years; 2: 3 to 5 years; 3: 6 to 10 years; 4: 11 to 20 years; 5: >20 years |
| Professional title | X4 | 1: Nurse; 2: Senior nurse; 3: Supervisor nurse; 4: Associate chief nurse or above |
| Position | X5 | 1: General nurse; 2: Pressure Sore Organisation Liaison Officer; 3: Head nurse |
| Education background | X6 | 1: Masters or above; 2: Bachelor degree; 3: Three‐year college education or below |
| Form of employment | X7 | 1: Contract system; 2: Personnel Agents; 3: Preparation |
| Nursing competence Level | X8 | 1: N0; 2: N1; 3: N2; 4: N3; 5: N4 |
| Training | X9 | 1: Yes; 2: No |
3.3. Single‐factor analysis of ICU nurses' MDRPI knowledge, attitude, and practice scores
Univariate analysis of variance was conducted with the scores of knowledge, attitude, and practice as the dependent variables (dichotomous variable: pass and fail) and the general information of ICU nurses as the independent variables, as shown in Table 3. The results showed that the differences in the scores of knowledge, attitude, and practice of the independent variables were all statistically significant (P < .1).
TABLE 3.
Single‐factor analysis of ICU nurses' MDRPI knowledge, attitude, and practice scores [n (%)] (N = 322).
| Variables | Knowledge | Attitude | Practice | χ2 values | P‐value | |||
|---|---|---|---|---|---|---|---|---|
| Pass | Fail | Pass | Fail | Pass | Fail | |||
| Age | 161.30 | 0.033 | ||||||
| 18 to 30 | 135 (57.20%) | 64 (74.40%) | 164 (58.60%) | 35 (83.30%) | 160 (59.00%) | 39 (76.50%) | ||
| 31 to 40 | 88 (37.30%) | 22 (25.60%) | 103 (16.80%) | 7 (16.70%) | 99 (36.50%) | 11 (21.60%) | ||
| >40 | 13 (5.50%) | 0 | 13 (4.60%) | 0 | 12 (4.40%) | 1 (2.00%) | ||
| Gender | 126.70 | <0.001 | ||||||
| Male | 35 (14.80%) | 25 (29.10%) | 49 (17.50%) | 11 (26.20%) | 51 (18.80%) | 9 (17.60%) | ||
| Female | 201 (85.20%) | 61 (70.90%) | 231 (82.50%) | 31 (73.80%) | 220 (81.20%) | 42 (82.40%) | ||
| Years of working | 80.70 | <0.001 | ||||||
| 1 to 2 | 51 (21.60%) | 40 (46.50%) | 70 (25.00%) | 21 (50.00%) | 70 (25.80%) | 21 (41.20%) | ||
| 3 to 5 | 51 (21.60%) | 18 (20.90%) | 56 (20.00%) | 13 (31.00%) | 56 (20.70%) | 13 (25.50%) | ||
| 6 to 10 | 85 (36.00%) | 19 (22.10%) | 99 (35.40%) | 5 (11.90%) | 93 (34.30%) | 11 (21.60%) | ||
| 11 to 20 | 35 (14.80%) | 8 (9.30%) | 40 (14.30%) | 3 (7.10%) | 38 (14.00%) | 5 (9.80%) | ||
| >20 | 14 (5.90%) | 1 (1.20%) | 15 (5.40%) | 0 | 14 (5.20%) | 1 (2.00%) | ||
| Professional title | 116.20 | <0.001 | ||||||
| Nurse | 66 (28.00%) | 46 (53.50%) | 86 (30.70%) | 26 (61.90%) | 86 (31.70%) | 26 (51.00%) | ||
| Senior nurse | 103 (43.60%) | 26 (30.20%) | 115 (41.10%) | 14 (33.30%) | 110 (40.60%) | 19 (37.30%) | ||
| Supervisor nurse | 64 (27.10%) | 14 (16.30%) | 76 (27.10%) | 2 (4.80%) | 73 (26.90%) | 5 (9.80%) | ||
| Associate chief nurse or above | 3 (1.30%) | 0 | 3 (1.10%) | 0 | 2 (0.70%) | 1 (2.00%) | ||
| Position | 508.30 | <0.001 | ||||||
| General nurse | 215 (91.10%) | 83 (96.50%) | 257 (91.80%) | 41 (97.60%) | 249 (91.90%) | 49 (96.10%) | ||
| Pressure sore organisation liaison officer | 13 (5.50%) | 3 (3.50%) | 15 (5.40%) | 1 (2.40%) | 15 (5.50%) | 1 (2.00%) | ||
| Head nurse | 8 (3.40%) | 0 | 8 (2.90%) | 0 | 7 (2.60%) | 1 (2.00%) | ||
| Education background | 228.00 | <0.001 | ||||||
| Masters or above | 4 (1.70%) | 0 | 4 (1.40%) | 0 | 1 (1.50%) | 0 | ||
| Bachelor degree | 175 (74.20%) | 49 (57.00%) | 204 (72.90%) | 20 (47.60%) | 198 (73.10%) | 26 (51.00%) | ||
| Three‐year college education or below | 57 (24.20%) | 37 (43.00%) | 72 (25.70%) | 22 (52.40%) | 69 (25.50%) | 25 (49.00%) | ||
| Form of employment | 341.20 | <0.001 | ||||||
| Contract system | 182 (77.10%) | 79 (91.90%) | 221 (78.90%) | 40 (95.20%) | 215 (79.30%) | 46 (90.20%) | ||
| Personnel Agents | 6 (2.50%) | 0 | 6 (2.10%) | 0 | 6 (2.20%) | 0 | ||
| Preparation | 48 (20.30%) | 7 (8.10%) | 53 (18.90%) | 2 (4.80%) | 50 (18.50%) | 5 (9.80%) | ||
| Nursing Competence Level | 264.60 | <0.001 | ||||||
| N0 | 6 (2.50%) | 5.8 (5.80%) | 6 (2.10%) | 5 (11.90%) | 4 (1.50%) | 7 (13.70%) | ||
| N1 | 86 (36.40%) | 49 (57.00%) | 111 (39.60%) | 24 (57.10%) | 110 (40.60%) | 25 (49.00%) | ||
| N2 | 108 (45.80%) | 27 (31.40%) | 123 (43.90%) | 12 (28.60%) | 118 (43.50%) | 17 (33.30%) | ||
| N3 | 29 (12.30%) | 5 (5.80%) | 33 (11.80%) | 1 (2.40%) | 32 (11.80%) | 2 (3.90%) | ||
| N4 | 7 (3.00%) | 0 | 7 (2.50%) | 0 | 7 (2.60%) | 0 | ||
| Training | 250.70 | <0.001 | ||||||
| Yes | 183 (81.80%) | 38 (44.20%) | 210 (75.00%) | 21 (50.00%) | 203 (74.90%) | 28 (54.90%) | ||
| No | 43 (18.20%) | 48 (55.80%) | 70 (25.00%) | 21 (50.00%) | 68 (25.10%) | 23 (45.10%) | ||
Note: 0 cells (0.0%) have an expected frequency of less than 5 and the pearson χ2 test was chosen.
3.4. Logistic regression analysis of general information of ICU nurses
In this study, the total score of ICU nurses' MDRPI knowledge, attitude, and practice was used as the dependent variable, and the statistically significant independent variables were screened out from the univariate analysis and included in the logistic analysis to select candidate predictor variables for the construction of the decision tree model, as shown in Table 4. The results show that years of working, professional title, education background and training are associated with high and low scores of knowledge, attitude, and practice, and can be included as predictors in the CART decision tree algorithm.
TABLE 4.
Logistic regression analysis of ICU nurses' total knowledge, attitude, and practice scores
| Variables | B coefficient | Standard coefficient | Wald values | P‐value | OR value | 95% CI |
|---|---|---|---|---|---|---|
| Constants | −3.85 | 0.12 | 58.14 | .010 | 0.02 | … |
| Age | 0.15 | 0.24 | 5.63 | .734 | 1.16 | 0.49–2.75 |
| Gender | −0.16 | 0.03 | 3.88 | .647 | 0.86 | 0.44–1.67 |
| Years of working | −0.66 | 0.12 | 14.33 | .014 | 0.52 | 0.31–0.88 |
| Professional title | 0.86 | 0.17 | 7.20 | .020 | 2.37 | 1.15–4.88 |
| Position | −0.62 | 0.54 | 3.32 | .301 | 0.54 | 0.33–0.75 |
| Education background | 1.04 | 0.26 | 14.55 | .003 | 2.83 | 1.42–5.62 |
| Form of employment | −0.35 | 0.20 | 5.34 | .128 | 0.71 | 0.45–1.11 |
| Nursing competence level | 0.12 | 0.17 | 9.92 | .719 | 1.13 | 0.58–2.20 |
| Training | 0.94 | 0.27 | 22.24 | .001 | 2.55 | 1.50–4.33 |
Note: …: Indicates no data output from the system.
3.5. Decision tree algorithm model
The total knowledge, attitude, and practice score were used as the target variable and years of working, professional title, education background and training were included in the CART tree model as predictor variables. The number of nodes in the tree model was 18, pruned to leave nodes 1, 2, 5, 6, 9, 10, 17 and 18, and the number of terminal nodes was 3, with a depth of 4. The results of the tree model showed that a total of 5 predictive model groupings of factors influencing the knowledge, attitude, and practice score were formed, namely trained, untrained and working years >5 years, untrained and working years 3 to 5 years, untrained and years of work 1 to 2 years and college degree, untrained and 1 to 2 years of working and bachelor's degree. Specific results are shown in Figure 1. The importance of the predictor variables for the total knowledge, attitude and practice score were ranked as education background (0.35), training (0.31), years of working (0.24) and professional title (0.10), Specific results are shown in Figure 2.
FIGURE 1.
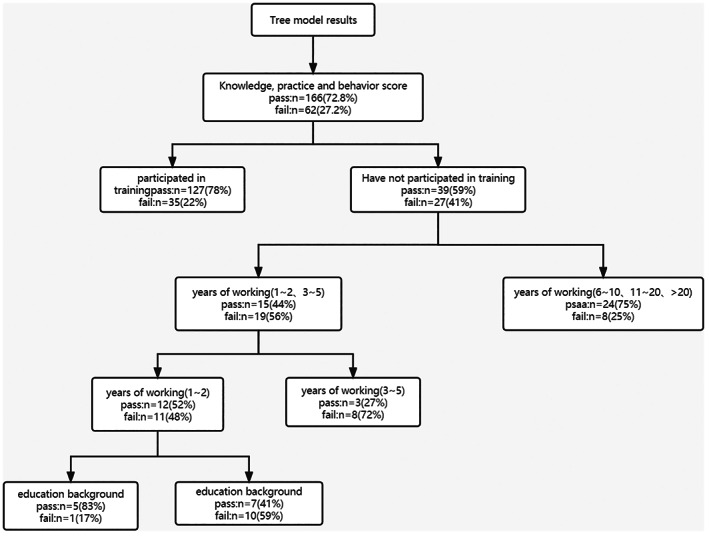
Simple decision tree model for ICU nurses' MDRPI total knowledge and trustworthiness scores.
FIGURE 2.
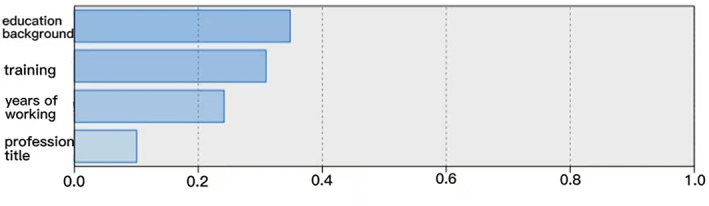
Importance sorting of the predictor variables.
3.6. ROC curve to assess the predictive value of the model
The subject working characteristic curve showed a specificity of 79.00%, a sensitivity of 77.80% and an area under the ROC curve of 0.718, Specific results are shown in Figure 3.
FIGURE 3.
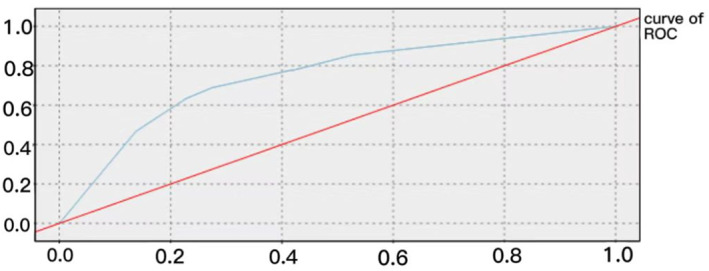
Subject work characteristic curve (ROC).
4. DISCUSSION
4.1. ICU nurses' MDRPI knowledge, attitude, and practice still do not meet clinical needs
ICU nurses scored 53.89 ± 9.45 for knowledge, 37.48 ± 6.05 for attitude and 56.44 ± 9.46 for practice, for a total score of 147.81 ± 21.03, with pass rates of 73.10%, 86.70%, 83.90% and 72.00% respectively. The knowledge, attitude, and practice scores showed that the ICU nurses' knowledge about MDRPI was far from meeting the clinical needs, which is consistent with Erbay Dalli Ö, et al.'s findings. 20 The questionnaire found that the majority of ICU nurses had never taken the initiative to learn about MDRPI and its progress, and very few had attended training, lectures or cared for MDRPI patients. ICU nurses showed more positive attitudes toward MDRPI care, which is consistent with the findings of Beeckman D. et al. 21 However, their awareness of prevention was weak, with nearly 1 in 5 nurses still neutral or opposed to the avoidability of MDRPI, the importance of continuous assessment, daily attention and the development of standardised processes, indicating that ICU nurses are still not sufficiently aware of MDRPI prevention in their daily nursing practice. With approximately 80% of clinical adverse events occurring due to problems with the operation of the treatment facility in question, it is important to strengthen ICU nurses' proficiency in the use of medical devices to increase their awareness of the prevention of MDRPI. In addition, the survey showed that most ICU nurses chose sometimes or often more than consistently for questions such as the number of times they checked patients' skin per shift, the number of times the oxygen saturation finger cuffs were changed, the number of times they kept the skin under the device clean and dry, and the number and time they relaxed the blood pressure cuff. It is evident that ICU nurses also have many deficiencies in the prevention of critical care patient behaviour, in line with Khojastehfar S et al.'s findings. 22 Currently in clinical practice stage 2 and above pressure injuries are included in the nursing professional quality control indicators and all pressure injuries must be reported, but only 54.85% of ICU nurses in this study would promptly report a patient who had a MDRPI, and there were deficiencies in the preventive care practice of ICU nurses for MDRPI and in the reporting of MDRPI after it had occurred.
4.2. More positive attitude toward prevention among highly educated nurses
The results of the tree model showed that nurses with a bachelor's degree had a higher score pass rate than nurses with a college degree, and nurses with >5 years of work experience also had a higher score pass rate than nurses with 3 to 5 years of work experience, which may be related to the more extensive access to MDRPI knowledge and more positive attitudes toward prevention among nurses with higher education. The results of a study by Zhang YB. et al. showed that nurses' education degree was associated with MDRPI prevention attitudes, and the knowledge, attitude, and practice scores of nurses with bachelor's degree and above were 0.978 units higher than those of nurses with low education, but the results of their study showed no correlation between nurses' education and knowledge scores, which is inconsistent with the results of the present study, which could be the result of using a different scale instrument for nurses. 23 It can be seen that education background, as the first predictor variable in the order of importance, occupies an important position in the judgement of ICU nurses' knowledge, attitude, and practice. Moreover, the survey of this study found that nurses with specialist education still accounted for 29.2% in tertiary hospitals. Therefore, clinical managers should focus more on the educational upgrading and re‐education of nurses with low education. In addition, the relationship between knowledge, attitude, and practice is positively correlated, and the preventive attitude of ICU nurses with MDRPI largely determines the thickness of their accumulated knowledge and the generation of preventive behaviour. 24 In clinical work, the tutorial system can be implemented to improve the prevention attitude of low‐educated nurses to high‐risk MDRPI patients, and finally achieve the purpose of promoting their active study.
4.3. Nurses who have received MDRPI training are more competent in knowledge, attitude, and practice
Education background and training of ICU nurses about MDRPI are very important to prevent the occurrence and prognosis of MDRPI in critically ill patients, and the incidence of MDRPI is also a key indicator to assess the quality of care. 25 The lack of knowledge of MDRPI prevention and care among ICU nurses is one of the main reasons for the hinder development of their preventive attitudes and practice. 26 The results of the tree model showed that whether or not they had received MDRPI training as the root node, the knowledge score of nurses who had received training was 56.38 ± 8.80 and passed 78.4%, and the knowledge score of nurses who had not received training was 47.57 ± 7.80. In addition, the results of the importance ranking of the predictor variables showed that the importance of training was 0.31, which was second only to education. This shows that training in MDRPI‐related knowledge and skills plays an important role in improving ICU nurses' ability of knowledge, attitude, and practice. In addition, the results of a cross‐sectional study by Lotfi M et al. showed that the development of relevant training programs could improve nurses' attitudes toward MDRPI prevention and nursing executive competence. 27 There is a synergistic relationship between ICU nurses' education background, whether or not they have attended training, years of working and professional title, which have the same effect on ICU nurses' MDRPI knowledge, attitude, and practice competencies. Therefore, nursing managers should reconsider the allocation of charge nurses for patients at high risk of MDRPI based on the synergistic relationship between the four influencing factors, and arrange nurses with high education background, have experience in training, extensive work experience and high professional title to care for patients at high risk of MDRPI occurrence as much as possible. In addition, Wang SL et al. noted that knowledge education, the adoption of PE foam‐bound gloves, and regular audits of ICU nurses' standards of nursing behaviour were effective in reducing the occurrence of MDRPI. 28 Therefore, nursing managers should develop more reasonable and effective training programs based on the synergistic relationship between the influencing factors, and a group‐led model can be implemented in the training, in which a nurse who has participated in the training and has high education is arranged to teach two to three nurses who have not participated in the training and have low education. Training methods should be lively and interesting, such as group discussion and exchange, case study workshops, role‐playing and audition methods, and regular self‐critical and reflective brainstorming activities. Some studies have pointed out that regular self‐critical behaviour and reflection can improve the competence of nurses. 29 Lead teachers can control the whole process of training activities and create a positive and good learning atmosphere to reduce nurses' training fatigue, improve ICU nurses' training motivation, and stimulate ICU nurses' interest and initiative in learning. 30
4.4. Years of working and professional title as influencing factors of ICU nurses' ability of knowledge, attitude, and practice
The more experience ICU nurses have, the more positive their practice behaviours are to prevent the occurrence of MDRPI. And their work experience is improved with the increase of working years. 23 Nursing as a highly practical discipline, the degree of their accumulated work experience largely determines the quality of their care. In another study on nurses' knowledge, attitude, and practice about pressure ulcer prevention, it was pointed out that nurses' attitudes toward pressure ulcer prevention were related to their accumulated knowledge and years of working, and the higher their years of working, the more solid their knowledge and the more positive their attitudes toward prevention. 29 Therefore, nurses with high working years should be assigned to care for patients at high risk of MDRPI such as tracheal intubation and breathing masks in order to minimise the occurrence of MDRPI in patients. The professional title as one of the influencing factors of ICU nurses' ability of knowledge, attitude, and practice was pruned in the CART tree model, but this does not mean that the professional title has no role in predicting ICU nurses' ability of knowledge, attitude, and practice. This may be due to the fact that professional title has the same influencing effect as years of working, and according to clinical experience, nurses with higher years of working have higher professional titles. The non‐linear relationship between professional title and other influencing factors was not reflected in the tree model, but professional title is a predictor of ICU nurses' ability to knowledge, attitude, and practice with confidence.
4.5. Building multidisciplinary collaborative teams
ICU patients are characterised by critical conditions and complex diseases, and the influencing factors are different for different diseases, so the prevention and management of MDRPI is a great challenge for ICU nurses. In contrast, multidisciplinary teamwork can reduce nurses' stress while also improving their attitude toward MDRPI prevention and teamwork. 26 , 31 Studies have pointed out that the use of measures such as developing standard work processes for multidisciplinary teams and using skin protection devices under masks can largely reduce the occurrence of MDRPI. 32 The multidisciplinary collaborative team should include the patient's primary care physician, charge nurse, and caregiver together. A standardised MDRPI prevention process can be developed on the basis of multidisciplinary teamwork, and a standardised prevention process can help improve the execution of nurses. In addition, it has been noted that verbal prompts and alerts are facilitators of preventive behaviours among ICU nurses. 33 ICU nurses have a heavy workload, and the setting of verbal prompts and alerts can reduce their workload to a certain extent, but nowadays, pressure alert devices are not set for tracheal intubation fixed stents and breathing masks, which are most prone to MDRPI, in clinical practice. Therefore, in the future, a pressure alarm for MDRPI high‐risk devices can be further considered to prompt regular interventions by ICU nurses.
5. CONCLUSION
The results of this study showed that ICU nurses' MDRPI knowledge, attitude, and practice need to be improved. And there are no systematic prevention and interventions for patients at risk for MDRPI, and there is a lack of appropriate guidelines to guide the implementation of their routine care. 34 Educational background, training, years of working and professional title have a synergistic effect in predicting the ability of ICU nurses to knowledge, attitude, and practice. Therefore, nursing managers can accurately identify ICU nurses with different characteristics according to the results of this study, and use nurses with better MDRPI knowledge, attitude and practice as responsible nurses for patients at risk of MDRPI according to the flexible scheduling system of the department as much as possible, in order to reduce the incidence of MDRPI in ICU patients.
FUNDING INFORMATION
This study was funded by Health Commission Science and Technology Planning project of Jiangxi of China (SKJP220229804).
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
ACKNOWLEDGEMENTS
The authors wish to thank all ICU nurses who participated in this study.
Sun X‐X, Chen R‐B, Fang P‐P, et al. Model construction of factors influencing intensive care unit nurses' medical device‐related pressure injury knowledge, attitude, and practice. Int Wound J. 2023;20(7):2582‐2593. doi: 10.1111/iwj.14129
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. Black JM, Cuddigan JE, Walko MA, Didier LA, Lander MJ, Kelpe MR. Medical device related pressure ulcers in hospitalized patients. Int Wound J. 2010;7(5):358‐365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel, Pan Pacific Pressure Injury Alliance . Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. revised ed. Perth: Cambridge Media; 2014. [Google Scholar]
- 3. Edsberg LE, Black JM, Goldberg M, McNichol L, Moore L, Sieggreen M. Revised national pressure ulcer advisory panel pressure injury staging system: revised pressure injury staging system. J Wound Ostomy Continence Nurs. 2016;43(6):585‐597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pittman J, Gillespie C. Medical device‐related pressure injuries. Crit Care Nurs Clin North Am. 2020;32(4):533‐542. [DOI] [PubMed] [Google Scholar]
- 5. Barakat‐Johnson M, Lai M, Wand T, Li M, White K, Coyer F. The incidence and prevalence of medical device‐related pressure ulcers in intensive care: a systematic review. J Wound Care. 2019;28(8):512‐521. [DOI] [PubMed] [Google Scholar]
- 6. Dang W, Liu Y, Zhou Q, et al. Risk factors of medical device‐related pressure injury in intensive care units. J Clin Nurs. 2022;31(9–10):1174‐1183. [DOI] [PubMed] [Google Scholar]
- 7. Celik S, Taskin Yilmaz F, Altas G. Medical device‐related pressure injuries in adult intensive care units [published online ahead of print, 2022 Sep 15]. J Clin Nurs. 2022. [DOI] [PubMed] [Google Scholar]
- 8. Brophy S, Moore Z, Patton D, O'Connor T, Avsar P. What is the incidence of medical device‐related pressure injuries in adults within the acute hospital setting? A systematic review. J Tissue Viability. 2021;30(4):489‐498. [DOI] [PubMed] [Google Scholar]
- 9. de Assis IIC, Estevam Dos Santos J, Valadares Sinicio Abib ML, et al. Medical device‐related pressure injury in an intensive care unit: a cross‐sectional study. Wound Manag Prev. 2021;67(11):26‐32. [PubMed] [Google Scholar]
- 10. Nan R, Su Y, Pei J, et al. Characteristics and risk factors of nasal mucosal pressure injury in intensive care units. J Clin Nurs. 2023;32(1‐2):346‐356. [DOI] [PubMed] [Google Scholar]
- 11. Rivera J, Donohoe E, Deady‐Rooney M, Douglas M, Samaniego N. Implementing a pressure injury prevention bundle to decrease hospital‐acquired pressure injuries in an adult critical care unit: an evidence‐based, pilot initiative. Wound Manag Prev. 2020;66(10):20‐28. [PubMed] [Google Scholar]
- 12. Coyer F, Miles S, Gosley S, et al. Pressure injury prevalence in intensive care versus non‐intensive care patients: a state‐wide comparison. Aust Crit Care. 2017;30(5):244‐250. [DOI] [PubMed] [Google Scholar]
- 13. Arnold‐Long M, Ayer M, Borchert K. Medical device‐related pressure injuries in Long‐term acute care hospital setting. J Wound Ostomy Continence Nurs. 2017;44(4):325‐330. [DOI] [PubMed] [Google Scholar]
- 14. Erbay Dallı Ö, Ceylan İ, Kelebek GN. Incidence, characteristics and risk factors of medical device‐related pressure injuries: an observational cohort study. Intensive Crit Care Nurs. 2022;69:103180. [DOI] [PubMed] [Google Scholar]
- 15. Tan JJM, Cheng MTM, Hassan NB, He H, Wang W. Nurses' perception and experiences towards medical device‐related pressure injuries: a qualitative study. J Clin Nurs. 2020;29(13–14):2455‐2465. [DOI] [PubMed] [Google Scholar]
- 16. Karadag A, Hanönü SC, Eyikara E. A prospective, descriptive study to assess nursing staff perceptions of and interventions to prevent medical device‐related pressure injury. Ostomy Wound Manage. 2017;63(10):34‐41. [PubMed] [Google Scholar]
- 17. Ghazanfari MJ, Karkhah S, Maroufizadeh S, et al. Knowledge, attitude, and practice of Iranian critical care nurses related to prevention of pressure ulcers: a multicenter cross‐sectional study. J Tissue Viability. 2022;31(2):326‐331. [DOI] [PubMed] [Google Scholar]
- 18. Ming‐Long W. SPSS Statistics in Practice—Questionnaire Analysis and Applications [M]. Beijing: Science Press; 2003. [Google Scholar]
- 19. Yu‐Ding H. Construction and application of the clinical nurses prevention medical device related pressure injury of critically ill patients for the knowledge, attitude, practice assessment scale[D]. Hebei: North China University of Science and Technology; 2018. [Google Scholar]
- 20. Erbay Dalli Ö, Kelebek GN. Knowledge, perception and prevention performance of intensive care unit nurses about medical device‐related pressure injuries. J Clin Nurs. 2022;31(11–12):1612‐1619. [DOI] [PubMed] [Google Scholar]
- 21. Beeckman D, Defloor T, Demarré L, Van Hecke A, Vanderwee K. Pressure ulcers: development and psychometric evaluation of the attitude towards pressure ulcer prevention instrument (APuP). Int J Nurs Stud. 2010;47(11):1432‐1441. [DOI] [PubMed] [Google Scholar]
- 22. Khojastehfar S, Najafi Ghezeljeh T, Haghani S. Factors related to knowledge, attitude, and practice of nurses in intensive care unit in the area of pressure ulcer prevention: a multicenter study. J Tissue Viability. 2020;29(2):76‐81. [DOI] [PubMed] [Google Scholar]
- 23. Zhang YB, He L, Gou L, et al. Knowledge, attitude, and practice of nurses in intensive care unit on preventing medical device‐related pressure injury: a cross‐sectional study in western China. Int Wound J. 2021;18(6):777‐786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tayebi Myaneh Z, Rafiei H, Hosseinigolafshani SZ, Rashvand F. Relationship between practice and attitude regarding pressure injury among intensive care nurses in Iran: a descriptive, correlational study. Wound Manag Prev. 2020;66(6):27‐34. [PubMed] [Google Scholar]
- 25. Jackson D, Sarki AM, Betteridge R, Brooke J. Medical device‐related pressure ulcers: a systematic review and meta‐analysis. Int J Nurs Stud. 2019;92:109‐120. [DOI] [PubMed] [Google Scholar]
- 26. Tayyib N, Coyer F, Lewis P. Pressure injury prevention in a Saudi Arabian intensive care unit: registered nurse attitudes toward prevention strategies and perceived facilitators and barriers to evidence implementation. J Wound Ostomy Continence Nurs. 2016;43(4):369‐374. [DOI] [PubMed] [Google Scholar]
- 27. Lotfi M, Aghazadeh AM, Asgarpour H, Nobakht A. Iranian nurses' knowledge, attitude and behaviour on skin care, prevention and management of pressure injury: a descriptive cross‐sectional study. Nurs Open. 2019;6(4):1600‐1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wang SL, Chuang PY, Su WC. Application of care bundles to reduce medical‐device‐related pressure injury (MDRPI) incidence in a coronary care unit. Hu Li Za Zhi. 2018;65(3):80‐87. Chinese. [DOI] [PubMed] [Google Scholar]
- 29. Jin J, Yi YJ. Patient safety competency and the new nursing care delivery model. J Nurs Manag. 2019;27(6):1167‐1175. [DOI] [PubMed] [Google Scholar]
- 30. Hu L, Sae‐Sia W, Kitrungrote L. Predictors of pressure injury prevention practices among ICU nurses in China. Adv Skin Wound Care. 2021;34(11):582‐587. [DOI] [PubMed] [Google Scholar]
- 31. Lancaster G, Kolakowsky‐Hayner S, Kovacich J, Greer‐Williams N. Interdisciplinary communication and collaboration among physicians, nurses, and unlicensed assistive personnel. J Nurs Scholarsh. 2015;47(3):275‐284. [DOI] [PubMed] [Google Scholar]
- 32. Arundel L, Irani E, Barkema G. Reducing the incidence of medical device‐related pressure injuries from use of CPAP/BiPAP masks: a quality improvement project. J Wound Ostomy Continence Nurs. 2021;48(2):108‐114. [DOI] [PubMed] [Google Scholar]
- 33. Everett Day S, Koirala B, McIltrot K. Repositioning strategies to prevent pressure injuries in the ICU: integrative review on implementation factors. Adv Skin Wound Care. 2022;35(6):344‐351. [DOI] [PubMed] [Google Scholar]
- 34. Saleh MYN, Ibrahim EIM. Prevalence, severity, and characteristics of medical device related pressure injuries in adult intensive care patients: a prospective observational study. Int Wound J. 2022;20(1):109‐119. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


