Abstract
Background:
The aim of this study was to assess the effect of a training package based on the lived experience of substance abusers on sleep problems and mental health.
Materials and Methods:
The current study was performed on 70 subjects equally distributed into two groups of control and intervention, Data collection tools included the Pittsburgh Sleep Quality Index (PSQI), the General Health Questionnaire (GHQ), and the Basic Adlerian Scales for Interpersonal Success—Adult Form (BASIS-A) Inventory. Data analysis was administered using the independent t-test, paired t-test, and MANCOVA. Statistical significance was considered when the P value < 0.05.
Results:
A total of 70 subjects participated in this study; 7 (10.6%) were females and 59 (89.4%) were males, with a mean age of 36.29 ± 8.588 years. The total score of PSQI was 12.48 (±4.206) and 13.16 (±3.397) for control and intervention groups, respectively, and declined to 12.33 (±4.442) and 9.56 (±4.45) after the intervention. The intervention resulted in an improved score for scales of belonging, going along, taking charge, harshness, being liked by all, and striving for perfection. Whereas the total score of the GHQ is reduced for both groups, that in the intervention group showed a higher decrease, which was also statistically significant.
Conclusion:
The developed training package successfully improved participants’ sleep quality, mental health, and lifestyle.
Keywords: Lifestyle, mental health, methadone, sleep quality, substance-related disorders
INTRODUCTION
Concerning substance abuse, today's modern world faces two major problems: the high and increasing number of drug abusers and its high social, economic, and health burden.[1] Hence, there should be strategies to address this problem. Currently available strategies are primarily based on quit addiction programs. Despite their extensive domain (e.g. changing attitude, poor family relationships, aggression, low self-confidence, etc.) and relative success in quitting substance abuse, rates of substance abuse relapse are still high.[2,3,4] Some studies reported that approximately half of all recovering addicts experience a relapse in less than 1 year.[5,6,7] Hence, more tailored and comprehensive strategies are needed, based on how these people feel about the world (i.e. lived experience).[8]
National statistics indicate an increasing prevalence of drug abuse in Iran, particularly in recent years. Some even reported a prevalence of 2.7%,[9] which is 3 times higher than the global average.[10] Several reasons are mentioned for this issue, including the shared border with Afghanistan, which is the largest producer country of opium worldwide.[11] This issue reveals the low efficacy of currently used strategies to harness drug abuse. Hence, the country is in need of a novel strategy to address this severe problem.
Understanding the etiology of substance use and identifying potential areas of difficulty in withdrawing can provide valuable information to address the problems of those who suffer from addiction.[12] Hence, it can be argued that exploring the causal relationships between these areas of difficulty is a practical first step for facilitating withdrawal. In this line, the current study aimed to develop a mentally healthy lifestyle training package based on the lived experience of substance abusers under methadone maintenance treatment and expert opinions to address two major problems of drug abusers that increase the inclination toward relapse (i.e. sleep problems and mental health disorders).
MATERIALS AND METHODS
The current study was performed in three stages on males and females receiving outpatient methadone treatment for opioid addiction in Isfahan city of Iran in 2021. The first stage was a qualitative study intended to identify factors that contribute to substance abuse and attempts to quit, which provided the necessary information to develop a training package. In this line, a series of semi-structured interviews were conducted with those suffering from substance abuse under methadone maintenance treatment who were willing to share their lived experiences. The inclusion criteria were being older than 18 years old, willingness to participate in the study, history of methadone maintenance therapy (MMT) for at least three months, and not suffering from severe psychological disorders, based on the diagnosis of a well-experienced physician. Following a purposive sampling technique and considering the abovementioned criteria, interviewees were selected. The sampling was stopped upon reaching data saturation (n = 26). All face-to-face interviews were performed in a private room. This step intended to identify factors that either improve or worsen the quality of life (QoL) of substance abusers. Noteworthy results of the qualitative step are provided in another article.
The first step was followed by a literature review intended to identify factors that contribute to a mental healthy lifestyle training package. In this line, we systematically searched Scopus, Web of Sciences (ISI), PubMed databases, and national databases (SID and MagIran) to identify relevant studies from the time of inception of these databases to December 2020. In addition, Google Scholar was also mined to increase the chance of finding potentially relevant studies related to the topic. Also, the reference list of the selected articles was hand-searched. The designed training package was approved by four experts.
The third stage contained performing a study to assess the developed package. Based on the previous studies, the sample size was estimated as 32 subjects per group, with a 95% confidence interval and 80% statistical test power. Considering the possible withdrawal of patients, the final sample size for each group was determined to be 35 people (70 people in total).
The inclusion criteria were receiving MMT for at least 3 months, willingness to participate, ability to read and write, and no history of participation in similar research during the past 12 months. The exclusion criterion was suffering from a psychological disorder confirmed by a physician and changing the treatment protocol before initiating the intervention.
After evaluating the inclusion and exclusion criteria, a total of 97 subjects were selected using a convenient sampling technique. Then, following a comprehensive introduction to the study protocol, 22 cases refused to participate and five patients wanted to change their treatment protocol (and were excluded). Eventually, 70 subjects were randomized into two groups of intervention (n = 35) and control (n = 35) using the SPSS software.
The intervention group was divided into smaller sub-groups and received the five 60-minute sessions by a well-trained psychologist, following a discussion-based method. The first session was designed to motivate the participants to change their lifestyle (i.e. withdrawal), to familiarize them with self-monitoring, pros and cons of changed behavior, field notes about negative and harmful daily behaviors, and feedback on key factors. The second session was about coping strategies against negative emotions, identification of negative emotions, and motivation for using coping strategies. The next session intended to strengthen thought control, positive self-concept, and developing an appropriate plan, as well as assigning desirable home tasks. Eventually, the fourth session was about resilience against temptation for risky behaviors, learning how to follow a targeted life, and challenges related to these issues. The last session intended to empower participants regarding dimensions such as self-efficacy, identification of potentially risky behaviors, and developing a personalized plan to prevent potentially risky conditions. Noteworthily, each session contained reviewing the previous session and assigned homework.
People in the control group did not receive any special intervention except standard treatment with methadone, but after ending the study, a training package, which contained pamphlets and CDs, was provided to them.
Data collection tools included the Pittsburgh Sleep Quality Index (PSQI), the General Health Questionnaire (GHQ), and the Basic Adlerian Scales for Interpersonal Success—Adult Form (BASIS-A) Inventory, which were completed by the participants before and 1 month after the intervention.
The PSQI is a self-report questionnaire containing seven dimensions of subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction, with 19 individual items. The PSQI includes a scoring key for calculating seven sub-scores, each of which can range from zero to three. The total score can go from zero to 21, with a total score of five or more indicating poor sleep quality; the higher the score, the worse the sleep quality.
The PSQI has been administered in several settings, including research on individuals suffering from addiction,[13] and its validity and reliability are confirmed by several studies in Iran.[14,15,16]
The BASIS-A inventory was also used to collect data on participants’ current psychological functioning based on early childhood memories. The BASIS-A has 65 items and five major scales: belonging/social interest, taking charge, going along; wanting recognition, and being cautious and five supporting scales known as the HELPS scales, which consists of harshness, entitlement, liked by all, striving for perfection, and softness.
The items are scored on a five-point Likert scale, ranging from never (1) to always (5). The validity and reliability of the Persian version of BASIS-A are evaluated by Akbari et al.[17](2016).
The GHQ, 28 item version, was used to assess the severity of mental health problems. The GHQ is scored on a four-point Likert scale, ranging from zero to three, yielding a total score of zero to 84, with higher scores indicating worse conditions.[18] Taghavi[19](2002) evaluated the validity and reliability of the Persian version of the GHQ and reported a Cronbach alpha of 0.9. In addition, a researcher-developed form was used to collect data on the education level, employment status, and marital status of participants.
SPSS version 23 was used for analysis. Statistical significance was considered when the P value < 0.05. Quantitative data analysis was administered using MANCOVA, paired t-test, and Chi-square test.
RESULTS
A total of 70 subjects participated in this study, equally distributed to intervention and control groups. A total of 7 (10.6%) were females and 59 (89.4%) were males, with a mean age of 36.29 ± 8.588 years, ranging from 22 to 58. As shown in Figure 1, at the end of the intervention, three subjects were excluded due to their absence in more than three training sessions (the intervention group) and one due to partial filling of the questionnaires (the control group).
Figure 1.
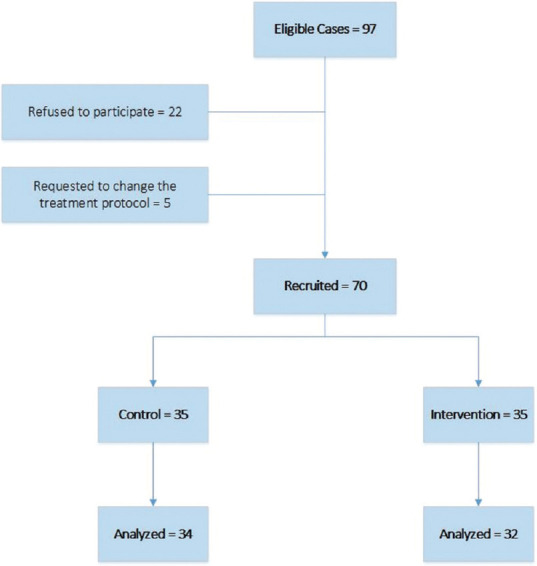
Flow diagram of study participants
There was no significant difference between the study groups concerning variables of age, education level, employment status, and marital status. The demographic characteristics of participants are provided in Table 1.
Table 1.
Demographic characteristics of participants
| Variable | Intervention Group (n=32) | Control Group (n=34) | P |
|---|---|---|---|
| Age (Mean±SD) | 35.22±9.554 | 37.29±7.574 | 0.330* |
| Sex (Frequency) | |||
| Male | 28 (87.5%) | 31 (91.2%) | 0.628** |
| Female | 4 (12.5%) | 3 (8.8%) | |
| Education (frequency) | |||
| High School | 11 (34.4%) | 15 (44.1%) | 0.624** |
| Diploma | 17 (53.1%) | 17 (50%) | |
| College education | 4 (12.5%) | 2 (5.9%) | |
| Employment status (frequency) | |||
| Employed | 13 (40.6%) | 14 (41.2%) | 0.964** |
| Unemployed | 19 (59.4%) | 20 (58.8%) | |
| Marital Status (Frequency) | |||
| Single | 16 (50%) | 9 (26.5%) | 0.075*** |
| Married | 16 (50%) | 25 (73.5%) |
*Independent t-test at a 5% level. **Chi-square test. ***Fisher’s exact test
Before the intervention, the total score of PSQI was 12.48 (±4.206) and 13.16 (±3.397) for the control and intervention groups, respectively. However, the values declined to 12.33 (±4.442) and 9.56 (±4.45), respectively, after providing the intervention. For itemized PSQI component scores and raw values, refer to Table 2.
Table 2.
Mean score of PSQI, separated by the dimension and study groups before and after intervention
| Variable | Mean±SD | P1 | P2 | |
|---|---|---|---|---|
|
| ||||
| Before | After | |||
| Sleep quality | ||||
| Control | 1.71±0.9 | 1.79±0.845 | 0.414 | 0.004 |
| Intervention | 1.91±0.928 | 1.19±0.780 | 0.001 | |
| Sleep latency | ||||
| Control | 1.82±0.797 | 1.94±0.851 | 0.160 | 0.03 |
| Intervention | 1.78±0.751 | 1.47±0.879 | 0.001 | |
| Sleep duration | ||||
| Control | 1.68±0.843 | 1.82±0.869 | 0.257 | 0.118 |
| Intervention | 1.72±0.851 | 1.47±0.95 | 0.030 | |
| Habitual sleep efficiency | ||||
| Control | 2.06±0.776 | 1.94±0.851 | 0.353 | 0.016 |
| Intervention | 2.00±0.803 | 1.37±1.008 | 0.001 | |
| Sleep disturbances | ||||
| Control | 1.85±0.821 | 1.79±0.770 | 0.535 | 0.091 |
| Intervention | 1.78±0.832 | 1.44±0.914 | 0.025 | |
| Use of sleep medication | ||||
| Control | 1.91±0.866 | 2.00±0.853 | 0.325 | 0.012 |
| Intervention | 1.90±0.928 | 1.41±1.011 | 0.001 | |
| Daytime dysfunction | ||||
| Control | 2.03±0.758 | 2.12±0.729 | 0.325 | 0.0001 |
| Intervention | 1.87±0.833 | 1.16±0.847 | 0.0001 | |
| Total score | 13.06±4.83 | 13.41±0.426 | 0.245 | 0.001 |
| 12.97±5.01 | 9.50±4.805 | 0.0001 | ||
Most participants declared no problem in completing the questionnaire. Overall, the areas in which the participants scored higher (indicating worse problems) were daytime dysfunction, sleep latency, and sleep disturbances, whereas sleep quality scored very low.
Except for the sleep duration and sleep disturbance variables, at the end of the intervention, other subscales in the intervention group were improved compared to the control group, which was statistically significant.
The findings regarding various subscales of the healthy mental lifestyle before and after providing the intervention are shown in Table 3.
Table 3.
Score of the BASIS-A lifestyle scale in intervention and control groups
| Studied variable | Group | Before Mean±SD | After Mean±SD | P1 | P2 |
|---|---|---|---|---|---|
| Primary scales | |||||
| Belonging/Social Interest (5-35) | Control | 21.29±6.375 | 22.32±6.251 | 0.134 | 0.842 |
| Intervention | 18.34±5.677 | 21.09±6.826 | 0.020 | ||
| Going along (15-35) | Control | 22.38±4.843 | 23.03±4.352 | 0.279 | 0.064 |
| Intervention | 19.41±3.826 | 21.50±7.255 | 0.008 | ||
| Taking charge (8-40) | Control | 19.32±7.214 | 18.47±5.801 | 0.240 | 0.046 |
| Intervention | 21.37±7.525 | 23.25±9.425 | 0.033 | ||
| Wanting recognition (7-35) | Control | 23.03±4.352 | 22.35±4.861 | 0.262 | 0.139 |
| Intervention | 20.00±6.839 | 19.09±5.491 | 0.359 | ||
| Being Cautious (5-20) | Control | 18.29±3.138 | 17.91±3.554 | 0.273 | 0.286 |
| Intervention | 16.75±4.064 | 16.09±3.970 | 0.380 | ||
| Supportive scales | |||||
| Harshness (5-25) | Control | 15.65±4.249 | 14.82±4.123 | 0.328 | 0.240 |
| Intervention | 16.47±4.918 | 16.69±4.329 | 0.819 | ||
| Entitlement (6-30) | Control | 17.65±5.110 | 18.85±6.238 | 0.107 | 0.003 |
| Intervention | 21.34±6.680 | 19.16±6.821 | 0.011 | ||
| Being Liked by All (3-15) | Control | 9.58±3.482 | 9.03±3.204 | 0.186 | 0.023 |
| Intervention | 11.78±3.338 | 12.81±2.545 | 0.047 | ||
| Striving for Perfection (5-25) | Control | 13.68±4.484 | 14.23±2.675 | 0.377 | 0.004 |
| Intervention | 15.56±5.696 | 17.37±4.535 | 0.027 | ||
| Softness (5-20) | Control | 18.29±3.138 | 17.91±3.553 | 0.273 | 0.091 |
| Intervention | 16.87±3.471 | 15.58±3.607 | 0.073 | ||
| Total score (64-280) | Control | 179.17±26.585 | 178.94±25.416 | 0.853 | 0.542 |
| Intervention | 177.91±29.395 | 183.50±34.583 | 0.024 |
As shown in Table 3, for those in the intervention group, scales of belonging/social interest, going along, taking charge, being liked by all, entitlement, and striving for perfection improved, which all were statistically significant. Furthermore, the total score of those in the intervention group showed a statistically significant increase; meanwhile, for controls, it was slightly decreased and was not significant.
The results of the GHQ are provided in Table 4.
Table 4.
Comparison of mean (SD) of GHQ scores in study groups
| Variable | Mean±SD | P1 | P2 | |
|---|---|---|---|---|
|
| ||||
| Before | After | |||
| Physical | ||||
| Control | 16.79±3.39 | 15.85±2.16 | 0.010 | 0.0001 |
| Intervention | 16.69±1.82 | 13.81±2.22 | 0.0001 | |
| Anxiety | ||||
| Control | 15.68±2.47 | 15.09±2.45 | 0.094 | 0.029 |
| Intervention | 17.03±2.389 | 13.87±19.13 | 0.001 | |
| Social function | ||||
| Control | 16.05±2.25 | 15.62±2.17 | 0.240 | 0.005 |
| Intervention | 17.06±2.36 | 14.09±2.1 | 0.001 | |
| Depression | ||||
| Control | 17.19±2.42 | 18.41±2.25 | 0.316 | 0.0001 |
| Intervention | 15.94±3.13 | 12.41±2.22 | 0.0001 | |
| Total score | ||||
| Control | 66.44±4.931 | 64.97±6.23 | 0.113 | 0.0001 |
| Intervention | 66.72±5.61 | 54.18±5.05 | 0.0001 | |
Whereas the total score of the GHQ is reduced for both groups, those in the intervention group experienced a higher decrease, which was also statistically significant. At the end of the intervention, other subscales in the intervention group improved compared to the control group, which was statistically significant.
DISCUSSION
This study aimed to develop a healthy mental lifestyle package based on the lived experience of substance abusers living in Isfahan (Iran) and evaluated the effect of this package on mental health, lifestyle, and sleep of patients. Initially, a series of face-to-face interviews and a literature review were conducted to identify effective factors that can be included in the package. Overall, the findings indicated that the intervention could improve the sleep quality of those in the intervention group.
Regarding the severity of mental health problems, the GHQ showed reduced scores for both groups, with a higher and significant reduction for those in the intervention group. In the same vein, a study conducted in the Zanjan province of Iran reported that those suffering from addiction are in need of supportive psychological intervention; otherwise, they will face considerable reductions in mental health quality.[20] Furthermore, whereas the resilience of those in the control group slightly reduced, the other group showed a considerable improvement. Davies et al.[21](2015) argued about developing a lifestyle balance model to enhance the QoL of those living with addiction. They mentioned that the developed model could considerably enhance the resilience of participants against daily difficulties. Similar results are reported by Mahboub et al.[22](2021).
The developed intervention reduced sleep problems among those in the intervention group, which was statistically significant. Several epidemiological studies describe the positive impact of habitual intervention on improving sleep problems. For instance, following a meta-analysis design, Cappuccio et al.[23] reported a pooled odds ratio of 1.55 for the habitual intervention in 23 studies of adults. Similar findings are echoed in several studies on this topic.[24,25,26] Whereas this has not always been the case, since the onset of the COVID-19 pandemic, sleep is increasingly recognized as a major lifestyle contributor to health,[27,28] which indicates the necessity of finding appropriate solutions. In addition, periods of acute withdrawal are accompanied by increased sleep latency,[29] that is, declined total sleep duration, which is in line with the present study's findings.
In addition, the developed package was associated with a decreased score of habitual sleep efficiency for both groups. However, it was only significant for those in the intervention group. In this line, several studies mentioned the positive impact of following a healthy lifestyle in improving overall health. For instance, Elizabeth[30](2021) argued that following a healthy lifestyle results in an optimal balance of healthy behavior that in turn improves overall health, including mental health.
The evidence suggests that mental health problems may contribute more significantly to sleep problems; hence, the usage of sleep medications can address mental health problems.[31,32]
Concerning the daytime dysfunction scale, the intervention could reduce the overall score, whereas those in the control group showed an increased score. In this regard, a randomized clinical trial by Hawkins et al. (2021) mentioned that lifestyle interventions could improve sleep quality and daytime dysfunctions.[33] Nam et al.[34](2015) reported that lifestyle interventions were associated with declined daytime fatigue, insomnia, and dream disorders.
The results demonstrated improved status of some primary scales and supportive subscales of the BASIS-A Inventory regarding participants’ current psychological functioning for those in the intervention group. However, it was only significant for taking charge, entitlement, being liked by all, and striving for perfection. These results are consistent with previous studies, indicating the positive impact of lifestyle-based interventions on mental health and lifestyle.[35,36,37,38] For instance, Ozpolat et al.[39](2012) argued that individuals who follow lifestyle-based interventions experience improved psychological well-being, including personal growth, purpose in life, and self-acceptance. Concerning these findings, it can be argued that an improved sense of belonging and going along translates into the declined need for recognition and softness; meanwhile, improved mental health status results in more endeavors to achieve perfection, leading to declined entitlement.
This study had limitations, including not following up with participants to investigate long-term effects. Besides, participants were selected from a single center in the city of Isfahan; hence, caution should be taken when generalizing the findings. Also, the number of studied patients was small and there is a need for studies with a larger sample size.
CONCLUSION
The results of this study permit an optimistic conclusion regarding the effectiveness of the proposed healthy training package on mental health, some dimensions of mental lifestyle, and sleep.
Ethics approval and consent for publication
Written informed consent was obtained from all participants after a comprehensive introduction to the study protocol. In addition, they were permitted to discontinue their cooperation at any time during the study. The Ethics Committee of the Islamic Azad University of Yazd approved the study protocol (IR.IAU.YAZD.REC.1400.025).
The authors certify that they have obtained all appropriate patient consent forms. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Financial support and sponsorship
The authors did not receive any financial support for this study.
Conflicts of interest
The authors have no potential conflicts of interest to disclose.
Acknowledgements
The authors of this article are grateful to all the patients and staff of outpatient addiction treatment centers who cooperated in the implementation of this project.
REFERENCES
- 1.Roos CR, Bowen S, Witkiewitz K. Baseline patterns of substance use disorder severity and depression and anxiety symptoms moderate the efficacy of mindfulness-based relapse prevention. J Consult Clin Psychol. 2017;85:1041–51. doi: 10.1037/ccp0000249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Petrova HA, Kytianova IP, Kozyakov RV. Social and personal factors of stable remission for people with drug addictions.Psychol. Russ: State Art. 2015;8:126–38. [Google Scholar]
- 3.Appiah R, Danquah SA, Nyarko K. Precipitants of substance abuse relapse in Ghana: A qualitative exploration. J Drug Issues. 2017;47:104–15. [Google Scholar]
- 4.Sharma AK, Upadhyaya S, Bansal P, Nijhawan M, Sharma D. A study of factors affecting relapse in substance abuse. Indian J Life Sci. 2012;2:28–33. [Google Scholar]
- 5.Connors GJ, Maisto SA. Relapse in the addictive behaviors. Clin Psychol Rev. 2006;26:107–8. doi: 10.1016/j.cpr.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 6.Curry J, Silva S, Rohde P, Ginsburg G, Kratochvil C, Simons A, et al. Recovery and recurrence following treatment for adolescent major depression. Arch Gen Psychiatry. 2011;68:263–9. doi: 10.1001/archgenpsychiatry.2010.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Betancourt CA, Kitsantas P, Goldberg DG, Hawks BA. Substance use relapse among veterans at termination of treatment for substance use disorders. Mil Med. 2021:usab280. doi: 10.1093/milmed/usab280. [DOI] [PubMed] [Google Scholar]
- 8.Holmes MV. Human genetics and drug development. N Engl J Med. 2019;380:1076–9. doi: 10.1056/NEJMe1901565. [DOI] [PubMed] [Google Scholar]
- 9.Eskandarieh S, Jafari F, Yazdani S, Hazrati N, Saberi-Zafarghandi MB. Compulsory maintenance treatment program amongst Iranian injection drug users and its side effects. Int J High Risk Behav Addict. 2014;3:e21765. doi: 10.5812/ijhrba.21765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Soroosh D, Neamatshahi M, Zarmehri B, Nakhaee S, Mehrpour O. Drug-induced prolonged corrected QT interval in patients with methadone and opium overdose. Subst Abuse Treat Prev Policy. 2019;14:1–5. doi: 10.1186/s13011-019-0196-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moradinazar M, Najafi F, Jalilian F, Pasdar Y, Hamzeh B, Shakiba E, et al. Prevalence of drug use, alcohol consumption, cigarette smoking and measure of socioeconomic-related inequalities of drug use among Iranian people: Findings from a national survey. Subst Abuse Treat Prev Policy. 2020;15:39. doi: 10.1186/s13011-020-00279-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moos RH. Theory-based active ingredients of effective treatments for substance use disorders. Drug Alcohol Depend. 2007;88:109–21. doi: 10.1016/j.drugalcdep.2006.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khayat MA, Qari MH, Almutairi BS, Shuaib BH, Rambo MZ, Alrogi MJ, et al. Sleep quality and internet addiction level among university students. Egypt J Hosp Med. 2018;73:7042–7. [Google Scholar]
- 14.Moghaddam JF, Nakhaee N, Sheibani V, Garrusi B, Amirkafi A. Reliability and validity of the Persian version of the Pittsburgh sleep quality index (PSQI-P) Sleep Breath. 2012;16:79–82. doi: 10.1007/s11325-010-0478-5. [DOI] [PubMed] [Google Scholar]
- 15.Khosravi A, Emamian MH, Wong YL, Hashemi H, Khabazkhoob M, Grzybowski A, Saw SM, et al. Components of Pittsburgh sleep quality index in Iranian adult population: An item response theory model. Sleep Med×. 2021;3:100038. doi: 10.1016/j.sleepx.2021.100038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nazifi M, Mokarami H, Akbaritabar A, Kalte HO, Rahi A. Psychometric properties of the Persian translation of Pittsburgh sleep quality index. Health Scope. 2014;3:e15547. [Google Scholar]
- 17.Akbari F, Farazmand S, Bahmani B. The relationship between subjective evaluation of stressors and depression in menopausal women: The mediating role of life satisfaction. Pract Clin Psychol. 2016;4:183–90. [Google Scholar]
- 18.Gao F, Luo N, Thumboo J, Fones C, Li SC, Cheung YB. Does the 12-item general health questionnaire contain multiple factors and do we need them? Health Qual Life Outcomes. 2004;2:63. doi: 10.1186/1477-7525-2-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taghavi S. Validity and reliability of the general health questionnaire (GHQ-28) in college students of Shiraz university. J Psychol. 2002;5:381–98. [Google Scholar]
- 20.Rostami F, Fathi E, Varzaneh AH, Daneshpour M. Factors impacting why women stay in marital life with substance dependent husbands: A grounded theory study. J Community Health Res. 2021;10:205–17. [Google Scholar]
- 21.Davies G, Elison S, Ward J, Laudet A. The role of lifestyle in perpetuating substance use disorder: The lifestyle balance model. Subst Abuse Treat Prev Policy. 2015;10:1–8. doi: 10.1186/1747-597X-10-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mahboub N, Honein-AbouHaidar G, Rizk R, de Vries N. People who use drugs in rehabilitation, from chaos to discipline: Advantages and pitfalls: A qualitative study. PLoS One. 2021;16:e0245346. doi: 10.1371/journal.pone.0245346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–26. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Giri PA, Baviskar MP, Phalke DB. Study of sleep habits and sleep problems among medical students of Pravara institute of medical sciences Loni, Western Maharashtra, India. Ann Med Health Sci Res. 2013;3:51–4. doi: 10.4103/2141-9248.109488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kay-Lambkin FJ, Thornton L, Lappin JM, Hanstock T, Sylvia L, Jacka F, et al. Study protocol for a systematic review of evidence for lifestyle interventions targeting smoking, sleep, alcohol/other drug use, physical activity, and healthy diet in people with bipolar disorder. Syst Rev. 2016;5:1–7. doi: 10.1186/s13643-016-0282-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shochat T. Impact of lifestyle and technology developments on sleep. Nat Sci Sleep. 2012;4:19–31. doi: 10.2147/NSS.S18891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.St-Onge M-P, Grandner MA, Brown D, Conroy MB, Jean-Louis G, Coons M, et al. Sleep duration and quality: Impact on lifestyle behaviors and cardiometabolic health: A scientific statement from the American Heart Association. Circulation. 2016;134:e367–86. doi: 10.1161/CIR.0000000000000444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gupta R, Grover S, Basu A, Krishnan V, Tripathi A, Subramanyam A, et al. Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J Psychiatry. 2020;62:370–8. doi: 10.4103/psychiatry.IndianJPsychiatry_523_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fathi HR, Yoonessi A, Khatibi A, Rezaeitalab F, Rezaei-Ardani A. Crosstalk between sleep disturbance and opioid use disorder: A narrative review. Addict Health. 2020;12:140–58. doi: 10.22122/ahj.v12i2.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Elizabeth B, Wanda D, Apriyanti E. The correlation between sleep quality and the prevalence of obesity in school-age children. J Public Health Res. 2021;10:jphr.2021.2331. doi: 10.4081/jphr.2021.2331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chapman JB, Lehman CL, Elliott J, Clark JD. Sleep quality and the role of sleep medications for veterans with chronic pain. Pain Med. 2006;7:105–14. doi: 10.1111/j.1526-4637.2006.00110.x. [DOI] [PubMed] [Google Scholar]
- 32.Kwan KS, Roberts LJ, Swalm DM. Sexual dysfunction and chronic pain: the role of psychological variables and impact on quality of life. Eur J Pain. 2005;9:643–52. doi: 10.1016/j.ejpain.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 33.Hawkins M, Marcus B, Pekow P, Rosal MC, Tucker KL, Spencer RM, et al. The impact of a randomized controlled trial of a lifestyle intervention on sleep among latina postpartum women. Ann Behavioral Med. 2021;55:892–903. doi: 10.1093/abm/kaaa118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nam S, Stewart KJ, Dobrosielski DA. Lifestyle intervention for sleep disturbances among overweight or obese individuals. Behav Sleep Med. 2016;14:343–50. doi: 10.1080/15402002.2015.1007992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tanaka H, Shirakawa S. Sleep health, lifestyle and mental health in the Japanese elderly: Ensuring sleep to promote a healthy brain and mind. J Psychosom Res. 2004;56:465–77. doi: 10.1016/j.jpsychores.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 36.ZubiaVeqar M. Hussain ME.Sleep quality improvement and exercise: A review. Int J Sci Res Publ. 2012;2:1–8. [Google Scholar]
- 37.Lederman O, Ward PB, Firth J, Maloney C, Carney R, Vancampfort D, et al. Does exercise improve sleep quality in individuals with mental illness.A systematic review and meta-analysis? J Psychiatr Res. 2019;109:96–106. doi: 10.1016/j.jpsychires.2018.11.004. [DOI] [PubMed] [Google Scholar]
- 38.Vaingankar JA, Müller-Riemenschneider F, Chu AHY, Subramaniam M, Tan LWL, Chong SA, et al. Sleep duration, sleep quality and physical activity, but not sedentary behaviour, are associated with positive mental health in a multi-ethnic Asian population: A cross-sectional evaluation. Int J Environ Res Public Health. 2020;17:8489. doi: 10.3390/ijerph17228489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ozpolat AR, Isgor IY, Sezer F. Investigating psychological well being of university students according to lifestyles. Proc Soc Behav Sci. 2012;47:256–62. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, upon reasonable request.


