Abstract
Background
The ankle-brachial index (ABI) is a critical diagnostic test for peripheral artery disease (PAD), albeit requiring technical expertise and dedicated resources. The advent of automatic ABI devices proposes a more accessible approach, necessitating fewer resources and less expertise. This study was conducted to gather data on PAD prevalence and to evaluate the correlation and efficacy of automatic ABI measurements vs traditional Doppler ABI measurements to understand their potential role in primary care settings.
Material/Methods
ABI measurements were obtained using both the Doppler method and an automatic plethysmographic device (Dopplex ABility, Huntleigh Healthcare).
Results
Of the 290 participants (mean age 67.6±7.4 years), Doppler ABI method identified 16.8% with abnormal results (<0.9), while the automatic method identified only 5.9%. The mean Doppler ABI was 1.05±0.15, and the mean automatic ABI was 1.12±0.13. The sensitivity of the automatic ABI measurements was 22.2%, and the specificity was 96.8%, with a positive predictive value of 57.1%, and a negative predictive value of 86.9%. Adjustments in the automatic assessment and inclusion of pulse wave velocity enhanced the diagnostic capabilities of the automatic ABI device.
Conclusions
While the automatic plethysmographic ABI device may lack the necessary diagnostic capabilities to replace the traditional Doppler ABI device as a standalone test in PAD diagnosis, it could still offer significant value in primary care settings if integrated with adjusted cut-off points and pulse wave velocity analysis.
Keywords: Peripheral Arterial Disease, Lower Extremity, Physicians, Primary Care
Background
Peripheral artery disease (PAD) is an atherosclerotic disease that most commonly affects the arteries of the lower extremities. In 2015, the estimated total number of cases of PAD worldwide reached 236 million, with the numbers continuing to rise [1]. PAD in the lower extremities is referred to as lower extremity arterial disease (LEAD). Symptoms can range from claudication to critical limb ischemia, sometimes leading to limb loss and even death [2]. Approximately 20% to 50% of patients with PAD are asymptomatic [2]. Due to nonspecific early symptoms and commonly asymptomatic presentation, the disease often remains undiagnosed or misdiagnosed [3]. Still, even in the asymptomatic stage, PAD increases cardiovascular risk and overall morbidity [4,5].
The ankle-brachial index (ABI) is recommended as the first-line noninvasive test for PAD in the lower extremities [6,7]. However, the traditional method of ABI measurement using a Doppler probe requires training and is time-consuming [6,8,9]. To address these challenges, automatic devices for ABI measurement have been developed to simplify the technique and provide consistent results [10–13]. Although there is promising evidence for oscillometric automatic devices, studies on plethysmographic devices are limited [11–13].
Automatic measurements have certain limitations, such as reduced accuracy in diabetic patients and overall higher values than those obtained with the Doppler ABI device [14,15]. Current guidelines recommend the use of traditional Doppler methods for ABI measurement over the use of automatic devices [6,16]. Nevertheless, research continues to assess the accuracy of new devices. This study aimed to evaluate the accuracy of automatic ABI measurements performed with the method of air plethysmography compared with those of Doppler ABI measurements.
Material and Methods
Study Population
Patients aged 50 years or older from a primary care clinic were invited to participate in the study. The inclusion criteria were an appropriate age and the ability to provide consent for study participation. Exclusion criteria included post-limb amputation, marked edema in either foot, skin lesions preventing the use of a blood pressure cuff, and the inability to remain supine during the examination.
Methods of Examination
Informed consent was obtained from all study participants. The examiner gathered the patients’ history, including information on PAD history, smoking, hypertension, diabetes, atrial fibrillation, coronary disease, chronic kidney disease, and medication usage. The researcher administered the Edinburgh questionnaire, a standardized tool, to assess participants for PAD symptoms. The Edinburgh questionnaire aims to identify typical claudication symptoms of PAD by asking participants about the presence of pain in the lower limbs and the situations in which the pain occurs and resolves. While the diagnostic value of the Edinburgh questionnaire has been previously assessed as weak [17], in this study, it was used to assess the presence of typical symptoms rather than as a diagnostic modality.
The examiner palpated the femoral, posterior tibial, and dorsalis pedis pulses, which are typically examined when suspecting LEAD. Carotid and femoral arteries, as well as the abdominal aorta, were auscultated to search for murmurs and physical examination signs of atherosclerosis in vascular beds. The patients’ weight and body mass index (BMI) were assessed using the Tanita MC780-MA device. Any BMI above 25.0 was categorized as abnormal.
For Doppler ABI assessment, the patients’ arm blood pressure was manually measured with a sphygmomanometer, on both arms. Subsequently, ankle-level blood pressure on both legs was measured using a Doppler probe (Dopplex DMX Digital Doppler, Huntleigh Healthcare) to detect a signal on the posterior tibial artery. The higher of the 2 arm blood pressure values was used for ABI calculation in each leg. An automatic ABI measurement was then performed using the Dopplex ABility Automatic ABI System (Huntleigh Healthcare) device. ABI values below 0.9 were considered abnormal, and values above 1.3 were considered non-diagnostic. The Dopplex ABility device also provided a pulse volume waveform (PVW) graph, which was assessed by the researchers as normal or abnormal. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated for the automatic device using Doppler ABI results as the reference standard. These parameters were first assessed using the standard 0.9 ABI cut-off point and subsequently recalculated for other cut-off points from the literature. The sensitivity, specificity, PPV, and NPV were also recalculated for a joint analysis of automatic ABI and PVW, again using Doppler ABI as the reference standard.
The study received approval from the Bioethical Committee of the Medical University of Bialystok, Poland.
Statistical Analysis
Statistical analysis was performed using IBM SPSS Statistics 25 software. Data normality was assessed using the Shapiro-Wilk test, and most ABI results showed an abnormal distribution, except for Doppler ABI results on the right legs. The correlation between abnormal ABI and patient characteristics and the correlation between the 2 methods of ABI measurements were assessed. For assessing the agreement between automatic ABI measurements and Doppler ABI measurements, the Wilcoxon test was used, owing to the lack of normality in the assessed data. The Pearson correlation coefficient was used to assess the correlation between automatic and Doppler measurements. The level of statistical significance was set at α=0.05, with P values <0.05 considered statistically significant.
Results
Demographic Data
The demographic data of the participants in the study are presented in Table 1. The study included 290 patients, with a mean age of 67.6±7.4 years; 24.7% were men and 75.3% were women; and 71.7% of patients were current or past smokers. A total of 28 patients (9.7%) had coronary heart disease, 185 (63.8%) had hypertension, 46 (15.9%) had diabetes, 4 (1.4%) had chronic kidney disease, and 28 (9.7%) had atrial fibrillation. Additionally, 13 patients (4.5%) had experienced a previous acute coronary incident, 3 (1%) had a transient ischemic attack, and 6 (2.1%) had a history of cerebral stroke. Among the patients, 50 (17.2%) reported regularly taking glucose-lowering medication, 57 (19.7%) reported taking antiplatelet medication, 18 (6.2%) reported taking anticoagulants, 178 (61.4%) reported taking blood pressure-lowering medication, and 109 (37.6%) reported taking statins. Six patients (2.1%) reported being previously diagnosed and treated for PAD. To assess the presence of PAD symptoms, the Edinburgh questionnaire was administered, yielding positive results in 30 patients (10.3%). We found a significant correlation between a positive Edinburgh questionnaire score and an abnormal automatic ABI (Fisher’s exact test, P=0.02). However, there was no statistically significant correlation between a positive Edinburgh questionnaire and abnormal Doppler ABI (Fisher’s exact test, P=0.299). We did not find a statistically significant correlation between the use of PAD treatment medication and ABI values, for both automatic (χ2 test, P=0.68 for statins and Fisher’s exact test, P=0.16 for antiplatelet medication) and traditional (χ2 test, P=0.98 for statins and χ2 test, P=0.11 for antiplatelet medication) devices.
Table 1.
Demographics of the study participants.
| n | % | |
|---|---|---|
| Demographic trait | ||
| Male sex | 71 | 24.7% |
| Female sex | 217 | 75.3% |
| Risk factors | ||
| Smoker | 208 | 71.7% |
| Abnormal body mass index | 213 | 73.7% |
| Comorbidities and previous cardiovascular incidents | ||
| Coronary heart disease | 28 | 9.7% |
| Atrial fibrillation | 28 | 9.7% |
| Hypertension | 185 | 63.8% |
| Diabetes | 46 | 15.9% |
| Chronic kidney disease | 4 | 1.4% |
| Acute coronary incident | 13 | 4.5% |
| Transient ischemic attack | 2 | 1.0% |
| Stroke | 6 | 2.1% |
| Medication | ||
| Glucose lowering medication | 50 | 17.2% |
| Antiplatelet medication | 57 | 19.7% |
| Anticoagulants | 18 | 6.2% |
| Blood pressure lowering medication | 178 | 61.4% |
| Statins | 109 | 37.6% |
| PAD indicators | ||
| Previous PAD diagnosis and treatment | 6 | 2.1% |
| Positive Edinburgh questionnaire | 30 | 10.3% |
| Abnormal Doppler ABI | 48 | 16.8% |
| Abnormal automatic ABI | 14 | 5.9% |
| Non-diagnostic Doppler ABI | 4 | 1.4% |
| Non-diagnostic automatic ABI | 8 | 3.4% |
ABI – ankle-brachial index; PAD – peripheral artery disease.
ABI Measurements
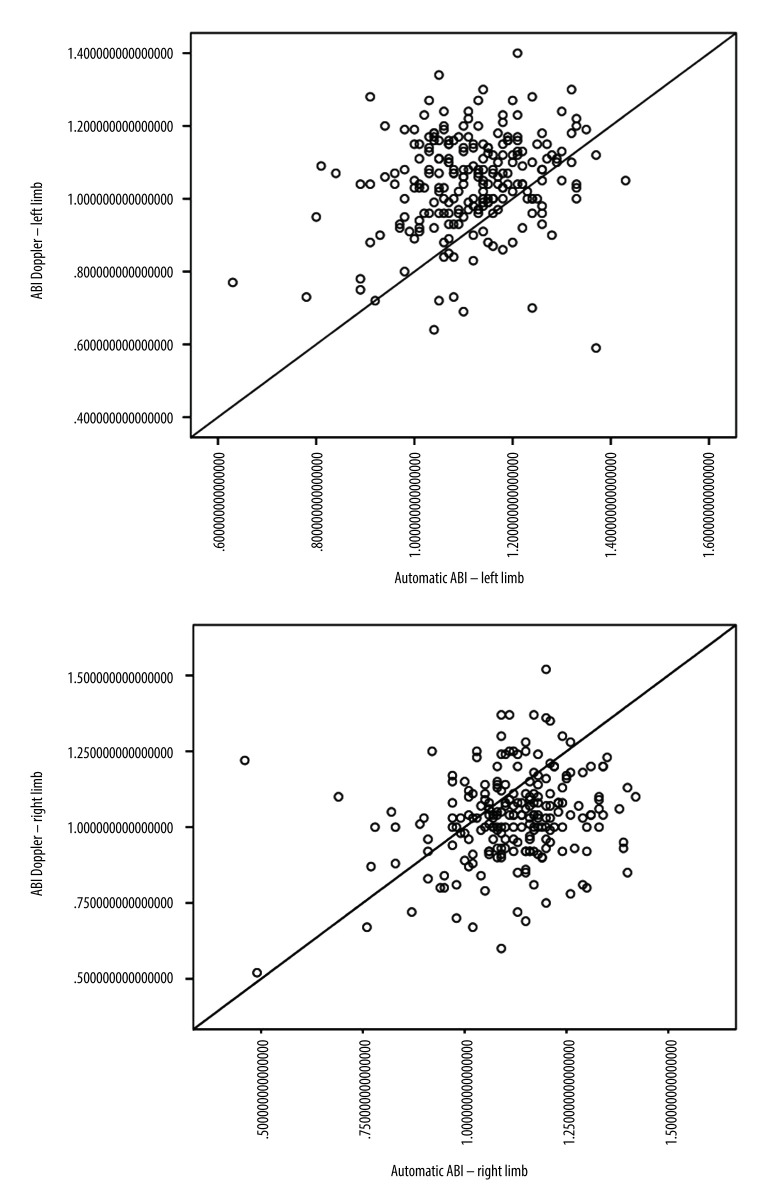
Doppler ABI measurements could not be obtained for 11 of the 580 limbs, mainly due to patient discomfort during cuff inflation. Automatic ABI measurements were not obtained for 131 of 580 limbs, mostly due to equipment error messages or patient discomfort during the examination. The mean automatic ABI for both legs was 1.12±0.13, while the mean Doppler ABI for both legs was 1.05±0.15. Abnormal Doppler ABI was found in 16.8% of the study population. In the 50–65 year age group, 13.5% of the population had abnormal ABI, while in the 65–80 year age group, 19% had abnormal ABI, and in the >80 year age group, 20% had abnormal ABI. For automatic ABI, 5.9% had abnormal ABI, comprising 4.1% of the 50–65 year age subgroup, 6.8% of the 65–80 year age subgroup, and 1.25% of the over 80 year age subgroup. The mean level of ABI in automatic measurements was higher than the mean level of ABI measured by Doppler (Figure 1), and the difference was statistically significant according to the Wilcoxon test. The level of effect, as indicated by the r value, was classified as moderate (Table 2). Using the standard cut-off ABI level of 0.9, the sensitivity of automatic measurements was 22.2%, and the specificity of automatic measurements was 96.8%. The positive predictive value (PPV) was 57.1%, and the negative predictive value (NPV) was 86.9%. ABI results above 1.3 were considered non-diagnostic and were omitted for the calculations of sensitivity, specificity, PPV, and NPV. The correlation between automatic and Doppler measurements was assessed using a Pearson correlation coefficient (Figure 2), and a low positive correlation was observed between the measurements, with r=0.23 for both limbs. We took into account previous publications that suggested different cut-off levels for PAD diagnosis when using automatic ABI measurements. In previous studies by Babaei et al and Davies et al, the optimal ABI cut-off levels were set at 1.2 and 1.04, respectively [18,19]. We conducted a simulation and assessed sensitivity, specificity, PPV, and NPV at the previously suggested levels. At the level of 1.2, we observed an improved sensitivity of 91.9%, but at the expense of considerably lower specificity, which decreased to 18.5%. The PPV and NPV for an automatic ABI cut-off level of 1.2 were 17.3% and 92.5%, respectively. The automatic ABI cut-off level of 1.04 resulted in a sensitivity of 54%, specificity of 78.9%, PPV of 32.2%, and NPV of 90.2%.
Figure 1.

Ankle-Brachial index level comparison in automatic and Doppler measurements.
Table 2.
Ankle-brachial index (ABI) level comparison in automatic and Doppler measurements by Wilcoxon test.
| Doppler ABI | Automatic plethysmographic ABI | Z | P | r | |||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||
| Left limbs | 1.05 | 0.13 | 1.12 | 0.12 | −6.39 | <0.001 | 0.43 |
| Right limbs | 1.03 | 0.15 | 1.12 | 0.14 | −7.10 | <0.001 | 0.48 |
Figure 2.
Correlation between automatic and Doppler results.
Furthermore, previous studies have shown that the diagnostic quality of automatic plethysmographic devices can be improved when the pulse volume waveform (PVW) is also considered during diagnosis. We performed an analysis of sensitivity, specificity, PPV, and NPV for a joint result of ABI and PVW measured by the plethysmographic device. Whenever either the ABI or PVW were abnormal, the result was classified as positive. For an abnormal automatic ABI, we used the 0.9 cut-off point. In the ABI and PVW analysis, we found that the sensitivity of the device was 67.6%, specificity was 51.5%, PPV was 20.5%, and NPV was 89.6%. When adjusting the cut-off points, we observed a sensitivity of 97.3%, specificity of 10%, PPV of 16.6%, and NPV of 95.2% with the 1.2 cut-off, and a sensitivity of 78.4%, specificity of 69.5%, PPV of 19.7%, and NPV of 91.1% with the 1.04 cut-off for the automatic ABI device (Table 3).
Table 3.
Sensitivity and specificity of automatic plethysmographic ankle-brachial index (ABI) at different cut-off levels, with and without pulse volume waveform (PVW) analysis.
| ABI Cut-off | 0.9 | 1.04 | 1.2 | |||
|---|---|---|---|---|---|---|
| Without PVW analysis | With PVW analysis | Without PVW analysis | With PVW analysis | Without PVW analysis | With PVW analysis | |
| Sensitivity | 22.2% | 67.6% | 54% | 78.4% | 91.9% | 97.3% |
| Specificity | 96.8% | 51.5% | 78.9% | 69.5% | 18.5% | 10% |
Discussion
The literature search reveals a good number of studies on automatic oscillometric ABI devices; however, there are fewer studies on plethysmographic devices. A recent review of automatic ABI devices assessed air plethysmography, the method used by the device analyzed in this study, as the least reliable of the currently available methods of automatic ABI assessment [20]. The available studies that assess its reliability vary in their clinical applicability assessment, with estimates of sensitivity at the standard cut-off for diagnosis ranging from 20% to 79% [18,21]. However, some of the authors analyzing the plethysmographic devices point to their potential applicability as a screening test in non-specialized settings, especially after adjustments of the cut-off point [18,19,22].
In our study, the mean automatic ABI was found to be 0.07 points higher than the measurements from the Doppler method. The tendency to achieve higher results in the automatic measurements observed in our study has been found in previous works. For instance, similar results were observed previously by van der Slegt et al in a study that showed that automatic ABI measurements are significantly 0.105 points higher than Doppler ABI measurements [23]. In a study by Babaei et al comparing automatic plethysmographic measurements to Doppler ABI, higher mean ABI values were recorded by the automatic device than the Doppler, leading the authors to propose using a higher cut-off value in automatic measurements for optimal diagnostic value [18]. A higher cut-off value was also suggested in a study by Davies et al, even though the mean levels of Doppler and plethysmographic ABI in that study were comparable (1.11±0.14 for Doppler ABI and 1.10±0.14 for plethysmographic ABI) [19]. The sensitivity and specificity of the plethysmography device in our study were 22.2% and 96.8%, respectively. Previous studies have shown a wide range of assessed sensitivity and specificity in this type of device. In a study by Babaei et al, which compared the device to a Doppler ultrasound scan, a sensitivity of 20% and a specificity of 95.6% were observed [18], which are very similar to the results found in our study. Different levels were observed in a study by Lewis et al, in which the sensitivity amounted to 79% and the specificity to 91%, and when pulse volume waveform was analyzed alongside plethysmographic ABI, the sensitivity reached 100% and the specificity 76% [21]. A similar high diagnostic value of a plethysmographic device was found in a study by Davies et al, who observed a sensitivity of 70% and specificity of 96%. Interestingly, studies by Babaei et al and Davies et al both observed improved sensitivity, and thus a diagnostic value of the test, after adjusting the cut-off value to a higher level for plethysmographic measurements [18,19]. Given that in our study, the overall mean automatic ABI level was found to be higher than the Doppler ABI level, we analyzed other potential cut-off points for plethysmographic measurements, adjusting the point based on the previous literature. The cut-off point of 1.2 resulted in a sensitivity of 91.9%, while lowering the specificity to 18.5%. The cut-off point of 1.04, based on the work of Davies et al [19], still established a reasonable specificity but increased sensitivity only to 54%, which is still not enough to consider plethysmographic ABI a reliable diagnostic test. Just as in the study of Lewis et al [21], we observed improved diagnostic quality of the device while combining automatic ABI and PVW analysis; however, the improvement was not to as high a level as previously observed. A more noticeable improvement in the diagnostic capability was found when we combined the elevated cut-off point for the automatic device with ABI and PVW analysis. The sensitivity at the level of 22.2% found in our study is not high enough to consider automatic plethysmographic ABI as a standalone test for LEAD diagnosis. Similarly, Millen et al have found automatic ABI accuracy as suboptimal [24], and van der Slegt et al, who analyzed automatic ABI measurements in postoperative settings, found them not clinically applicable [23]. In the Polish primary care setting, the Doppler ABI device is mostly inaccessible. Primary care workers point to time restraints as one of the most important limitations to performing ABI in primary care [25]. With the broad range of symptoms of LEAD, many of them nonspecific, and the lack of access to ABI measurements early in the diagnostic process, many of the patients remain undiagnosed.
Furthermore, referring all patients with potential LEAD symptoms to specialized care creates longer waiting times, which subsequently delays the diagnosis. Even with low diagnostic performance of automatic devices to confirm LEAD, the strong potential to exclude LEAD might still prove useful in primary care and decrease the number of unnecessary specialist referrals. Furthermore, to reach acceptable levels of sensitivity of the automatic test, an adjustment of the cut-off point might be necessary. While using 1.2 as a cut-off point for PAD diagnosis in automatic measurement, the test reached a sensitivity of 91.9%. However, this improvement came at the expense of specificity. Future studies may point us to the ideal cut-off point for automatic ABI measurements. Additionally, analyzing PVW alongside ABI can further improve diagnostic capability, which can eventually result in a sufficient diagnostic modality.
Study Limitations
A potential limitation of our study was the use of Doppler ABI as the reference standard to assess automatic ABI accuracy in LEAD diagnosis. While Doppler ABI is considered a first-line tool in LEAD diagnosis, its diagnostic performance is not considered perfect, and using a more sensitive diagnostic modality might have proved more beneficial for the study [26].
Conclusions
Overall, we found that nearly 20% of our primary care patients over 50 years of age had abnormal Doppler ABI values, consistent with the diagnosis of LEAD. In most of our patients, the disease was asymptomatic and undiagnosed. We observed that the diagnostic capability of automatic plethysmographic ABI, especially the low sensitivity, is insufficient to introduce it as a standalone test in LEAD diagnosis. However, adjusting the cut-off point to a higher level and considering PVW may improve its diagnostic applicability, especially in a non-specialized setting.
Footnotes
Publisher’s note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher
Declaration of Figures’ Authenticity
All figures submitted have been created by the authors who confirm that the images are original with no duplication and have not been previously published in whole or in part.
Financial support: The work was financially supported by a research grant from the university where it was conducted
Conflict of interest: The authors declare no conflicts of interest. The work was not funded by ArjoHuntleigh, the company producing the analyzed device, or any other commercial company
References
- 1.Horváth L, Németh N, Fehér G, et al. Epidemiology of peripheral artery disease: Narrative review. Life (Basel) 2022;12(7):1041. doi: 10.3390/life12071041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McDermott MM, Guralnik JM, Ferrucci L, et al. Asymptomatic peripheral arterial disease is associated with more adverse lower extremity characteristics than intermittent claudication. Circulation. 2008;117(19):2484–91. doi: 10.1161/CIRCULATIONAHA.107.736108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schorr EN, Peden-McAlpine C, Treat-Jacobson D, Lindquist R. Characterization of the peripheral artery disease symptom experience. Geriatr Nurs. 2015;36(4):293–300. doi: 10.1016/j.gerinurse.2015.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Behroozian AA, Beckman JA. Asymptomatic peripheral artery disease: Silent but deadly. Prog Cardiovasc Dis. 2021;65:2–8. doi: 10.1016/j.pcad.2021.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aday AW, Matsushita K. Epidemiology of peripheral artery disease and polyvascular disease. Circ Res. 2021;128(12):1818–32. doi: 10.1161/CIRCRESAHA.121.318535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Primary Panel. Abramson BL, Al-Omran M, Anand SS, et al. Canadian Cardiovascular Society 2022 guidelines for peripheral arterial disease. Can J Cardiol. 2022;38(5):560–87. doi: 10.1016/j.cjca.2022.02.029. [DOI] [PubMed] [Google Scholar]
- 7.Aboyans V, Ricco JB, Bartelink MEL, et al. ESC Scientific Document Group. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS): Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS) Eur Heart J. 2018;39(9):763–816. doi: 10.1093/eurheartj/ehx095. [DOI] [PubMed] [Google Scholar]
- 8.Nexøe J, Damsbo B, Lund JO, Munck A. Measurement of blood pressure, ankle blood pressure and calculation of ankle brachial index in general practice. Fam Pract. 2012;29(3):345–51. doi: 10.1093/fampra/cmr094. [DOI] [PubMed] [Google Scholar]
- 9.Yap Kannan R, Dattani N, Sayers RD, Bown MJ. Survey of ankle-brachial pressure index use and its perceived barriers by general practitioners in the UK. Postgrad Med J. 2016;92(1088):322–27. doi: 10.1136/postgradmedj-2015-133375. [DOI] [PubMed] [Google Scholar]
- 10.Vega J, Romaní S, Garcipérez FJ, Vicente L, et al. [Peripheral arterial disease: Efficacy of the oscillometric method]. Rev Esp Cardiol. 2011;64(7):619–21. doi: 10.1016/j.recesp.2010.10.019. [in Spanish] [DOI] [PubMed] [Google Scholar]
- 11.Khan SZ, Awn-Bin-Zafar, Waris N, et al. Comparison of ankle-brachial index (ABI) measured by an automated oscillometric apparatus with that by standard hand-held doppler in patients with Type-2 diabetes. Pak J Med Sci. 2019;35(4):1167–72. doi: 10.12669/pjms.35.4.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hageman D, van den Houten MML, Pesser N, et al. Diagnostic accuracy of automated oscillometric determination of the ankle-brachial index in peripheral artery disease. J Vasc Surg. 2021;73(2):652–60. doi: 10.1016/j.jvs.2020.05.077. [DOI] [PubMed] [Google Scholar]
- 13.Ichihashi S, Desormais I, Hashimoto T, et al. Accuracy and reliability of the ankle brachial index measurement using a multicuff oscillometric device versus the Doppler method. Eur J Vasc Endovasc Surg. 2020;60(3):462–68. doi: 10.1016/j.ejvs.2020.06.013. [DOI] [PubMed] [Google Scholar]
- 14.Ichihashi S, Hashimoto T, Iwakoshi S, Kichikawa K. Validation study of automated oscillometric measurement of the ankle-brachial index for lower arterial occlusive disease by comparison with computed tomography angiography. Hypertens Res. 2014;37(6):591–94. doi: 10.1038/hr.2014.34. [DOI] [PubMed] [Google Scholar]
- 15.Diehm N, Dick F, Czuprin C, et al. Oscillometric measurement of ankle-brachial index in patients with suspected peripheral disease: Comparison with Doppler method. Swiss Med Wkly. 2009;139(25–26):357–63. doi: 10.4414/smw.2009.12636. [DOI] [PubMed] [Google Scholar]
- 16.National Institute for Health and Care Excellence. Guidance. NICE; [accessed on 19 May 2022]. Recommendations. Peripheral Arterial Disease: Diagnosis and Management. Available from: https://www.nice.org.uk/guidance/cg147/chapter/Recommendations#diagnosis. [Google Scholar]
- 17.Boylan L, Nesbitt C, Wilson L, et al. Investigators OBOTN. Reliability of the Edinburgh Claudication Questionnaire for identifying symptomatic PAD in general practice. Angiology. 2021;72(5):474–79. doi: 10.1177/0003319720984882. [DOI] [PubMed] [Google Scholar]
- 18.Babaei MR, Malek M, Rostami FT, et al. Non-invasive vascular assessment in people with type 2 diabetes: Diagnostic performance of Plethysmographic-and-Doppler derived ankle brachial index, toe brachial index, and pulse volume wave analysis for detection of peripheral arterial disease. Prim Care Diabetes. 2020;14(3):282–89. doi: 10.1016/j.pcd.2019.09.005. [DOI] [PubMed] [Google Scholar]
- 19.Davies JH, Williams EM. Automated plethysmographic measurement of the ankle-brachial index: A comparison with the Doppler ultrasound method. Hypertens Res. 2016;39(2):100–6. doi: 10.1038/hr.2015.124. [DOI] [PubMed] [Google Scholar]
- 20.Danieluk A, Chlabicz S. Automated measurements of ankle-brachial index: A narrative review. J Clin Med. 2021;10(21):5161. doi: 10.3390/jcm10215161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lewis JE, Williams P, Davies JH. Non-invasive assessment of peripheral arterial disease: Automated ankle brachial index measurement and pulse volume analysis compared to duplex scan. SAGE Open Med. 2016;4:2050312116659088. doi: 10.1177/2050312116659088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lewis J, Hawkins M, Barree P, et al. A comparison between a new automatic system and Doppler method for obtaining ankle brachial pressures. J Foot Ankle Res. 2010;3:O15. [Google Scholar]
- 23.van der Slegt J, Verbogt NP, Mulder PG, et al. The clinical applicability of an automated plethysmographic determination of the ankle-brachial index after vascular surgery. Vascular. 2016;24(5):545–48. doi: 10.1177/1708538115625379. [DOI] [PubMed] [Google Scholar]
- 24.Millen RN, Thomas KN, Majumder A, et al. Accuracy and repeatability of the Dopplex ability. Expert Rev Med Devices. 2018;15(3):247–51. doi: 10.1080/17434440.2018.1431121. [DOI] [PubMed] [Google Scholar]
- 25.Danieluk A, Niemcunowicz-Janica A, Windak A, Chlabicz S. Diagnosis and treatment of lower extremity arterial disease – a survey among family medicine trainees in Poland. Int J Environ Res Public Health. 2023;20(2):1392. doi: 10.3390/ijerph20021392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alagha M, Aherne TM, Hassanin A, et al. Diagnostic performance of ankle-brachial pressure index in lower extremity arterial disease. Surg J (N Y) 2021;7(3):e132–e37. doi: 10.1055/s-0041-1731444. [DOI] [PMC free article] [PubMed] [Google Scholar]