ABSTRACT
Aims and Objectives:
Special care dentistry (SCD) provides oral health care to disabled individuals in an environmental, cultural or social setting that supports their oral health. This study aimed to analyze the profiles of patients managed at an SCD clinic in a teaching hospital based on their sociodemographic background, medical condition or disability, dental diagnosis and treatment provided.
Materials and Methods:
This retrospective audit study included patients seen from the clinic‘s inception in January 2017 until June 2022, retrieved from the faculty’s record management system. The pattern of patients seen was arranged on an Excel sheet and analyzed using SPSS. Quantitative data were analyzed via descriptive analysis (frequency) and chi-square test (P < 0.05).
Results:
A 220% surge in the number of patients treated between January 2017 and June 2022, from two to 91 years old, with more male patients seen. Most patients had an intellectual disability (49.7%), followed by medical compromised (16.4%) and genetic conditions or syndromes (12.0%). 43% of had caries, which is more prevalent in women, and 31.6% had periodontal disease, with the majority being between the ages of 21 and 40. Periodontal treatment accounted for most of the dental treatment (76.1%). Even though only a small percentage of endodontic therapy was performed (2.4%), a significant association was found between the treatment, gender and age group of patients seen in the clinic.
Conclusion:
Considering their health profile, oral diagnosis and therapy, this study demonstrated the varied sorts of patients encountered in an SCD specialist clinic. This useful information will be beneficial in the development of a comprehensive care dentistry center for this community.
Keywords: Disability, special care dentistry, special health care needs, treatments of patients with special healthcare needs
INTRODUCTION
People who require special care dentistry (SCD) are those who need modified delivery of oral health care for multiple reasons, such as medical conditions, physical or intellectual disability, or psychiatric issues.[1] The Global Burden of Disease study determined that the oral health of patients with special health care needs (SHCN) is poor.[2] Most of the patients from this community requires altered dental management due to their condition but often refused by general practitioner as they lack knowledge and experience, as well as their clinic is not fully equipped for dealing with such patients.[1] Hence, the inclusion of SCD in the dental curriculum is one of the solutions advocated by various studies for coping with this situation.[3,4,5] Consequently, numerous nations have chosen to incorporate SCD clinical training within their programs. For instance, Australia, Japan, and the United States have integrated clinical training and lectures by SCD specialists alone or with pediatric dental specialists and anesthetists.[6]
In Malaysia, only three teaching hospitals with SCD specialists provide treatment for patients with SHCN in SCD specialist clinics. These are located in three separate states: Selangor, Kuala Lumpur, and Pahang. These centers are responsible for teaching dental undergraduates in SCD, but only two of the universities offer postgraduates training. The treatment offered includes oral health care education, treatment under pharmacological intervention such as sedation and general anesthesia, preventive oral health care and all types of dental treatment, including those requiring interprofessional and holistic care. These teaching hospitals’ accept referrals from primary clinics, private practitioners and their medical counterparts.[7]
A local study has explored the referral trend; however, it did not examine the number of patients seen based on their medical conditions, diagnoses or treatment patterns.[7] According to Hugo et al.,[4] ongoing research on oral health services to build a database containing timely and relevant data are crucial to analyze the oral health status of patients with SHCN. The purpose of this study was to analyze the profile of patients in an SCD clinic at a teaching hospital in Selangor based on their sociodemographic background, medical condition or disability, dental diagnoses, types of services and treatment provided.
MATERIALS AND METHODS
This was a situational study of patients attended the SCD specialist clinic in a teaching hospital in a suburb of Selangor. All patient data from the clinic’s inception in January 2017 to June 2022 were tracked and included in the study. The data were from the faculty’s Integrated Dental Record Management System (iDeRMS), and were collected from August 2021 until June 2022. Should there be any missing data in terms of their sociodemographic background, medical condition or disability, dental diagnoses and types of services provided, they were excluded from the study. Ethical approval was granted by the research ethics committee of the participating university (ref no: REC/08/2021 [MR/660]).
DATA COLLECTION
The data were categorized based on the patient’s age, disability or medical condition, dental diagnoses and types of treatment received. A standardized data sheet was used to organize the data, ensuring its uniformity. Data were arranged using Microsoft Excel version 16.62 by a single investigator.
The types of disability were grouped and modified based on the classification by the Ministry of Health Malaysia.[1] They were categorized as intellectual and physical disabilities, psychiatric disorders, medical compromise, genetic or chromosomal-related medical conditions, and more than one type of medical condition. The dental diagnoses were periodontal disease, dental caries, edentulism, oral mucosal lesions, dentoalveolar trauma, and malocclusion. The treatment received by the patients was categorized as periodontal treatment (scaling, polishing, and root debridement), restorative management (temporary or permanent fillings), prosthodontics (removable or fixed), orthodontic intervention, endodontics, surgical procedures, and comprehensive dental treatment under general anesthesia.
The variables analyzed were the associations between age, gender, medical conditions, dental diagnoses and treatment received by patients with SHCN seen in the university SCD clinic. However, a potential reporting bias may be observed in this investigation because the data acquired from the integrated system depended on what the practitioner reported, which was not explicitly calibrated for this study.
STATISTICAL ANALYSIS
The data were analyzed via frequency analysis and chi-square test (P < 0.05) using IBM SPSS version 28.0 to determine any association between the categorical variables.
A geographic mapping analysis was performed based on the patients’ home addresses to visualize the relative distance pattern to the clinic. The mapping was conducted using the Quantum Geographic Information System (QGIS version 3.8).
RESULTS
SOCIODEMOGRAPHIC CHARACTERISTICS
A total of 742 patients with SHCN were seen in the SCD clinic. More male patients than female patients attended the clinic, and their mean age was 22.09 years. The youngest was two years old, and the oldest was 91. The most common condition presented was intellectual disability (49.7%, n = 369). The patients’ sociodemographic characteristics are summarized in Table 1.
Table 1.
Sociodemographic characteristics of patients seen in the university SCD clinic (N = 742)
| Sociodemographic characteristic | Mean (SD) | n | % | |
|---|---|---|---|---|
| Gender | Male | 493 | 66.4 | |
| Female | 249 | 33.6 | ||
| Age (years) | 22.09 (21.2) | |||
| 0–20 | 495 | 66.7 | ||
| 21–40 | 99 | 13.3 | ||
| 41–60 | 72 | 9.7 | ||
| 61–80 | 71 | 9.6 | ||
| 81–100 | 5 | 0.7 | ||
| Medical condition or disability | Medical compromise | 122 | 16.4 | |
| Physical disability | 65 | 8.8 | ||
| Intellectual disability | 369 | 49.7 | ||
| Genetic syndromic | 96 | 12.9 | ||
| Psychiatric disorder | 14 | 1.9 | ||
| More than one disability | 76 | 10.2 |
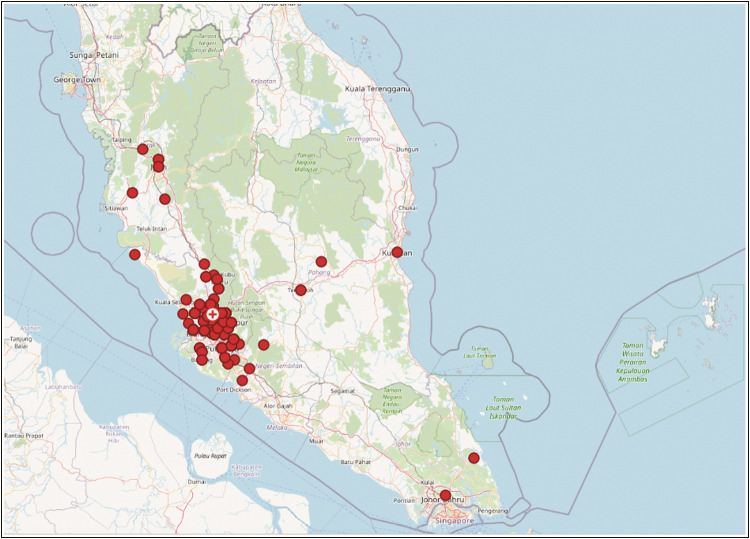
In terms of their geographical distributions, the locations plotted in Figure 1 present the homes of patients who attended the SCD clinic. Most were from the Klang Valley, which is within 40 km of the clinic. The furthest locations reported were Johor (306.3 km), Kuantan (201.39 km), and Ipoh (163.9 km).
Figure 1.
Locations of patients attending the university SCD clinic
A significant association existed between patients’ gender and the number of individuals with more than one disability (χ2 = 48.214, P < 0.001), which was noted in more male patients than female patients (78.9%, n = 60). A significant association was noted between patients’ age group and their medical conditions (χ2 = 704.456, P < 0.001); 90.2% (n = 333) were 0–20 years old.
PATIENT ATTENDANCE
A gradual increase occurred in the number of patients with SHCN who attended the SCD clinic from January 2017 to June 2022 (2017: 32 patients; 2018: 87 patients; 2019: 122 patients; 2020: 154 patients; 2021: 226 patients; 2022 [until June]: 121 patients).
DENTAL DIAGNOSES
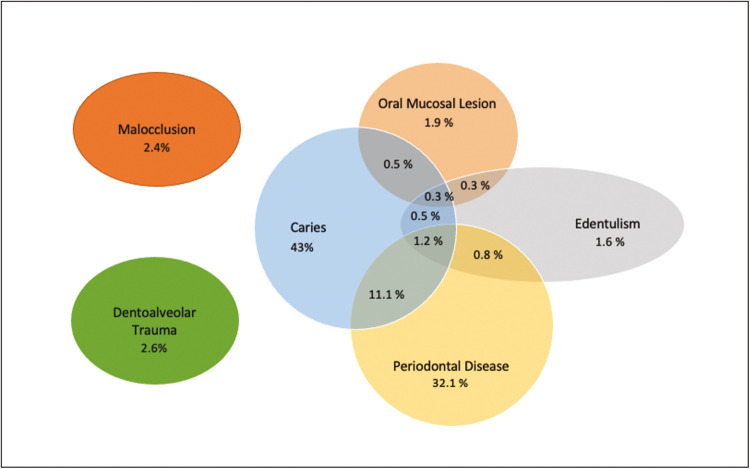
Dental caries and periodontal disease were the most prevalent conditions diagnosed, at 43% (n = 319) and 31.6% (n = 238), respectively. Other conditions reported were dentoalveolar trauma (2.6%, n = 19), malocclusion (2.4%, n = 18), edentulism (1.6%, n = 12) and oral mucosal lesion (1.9%, n = 14). In addition, more than one type of oral condition was also noted in some patients, such as caries and periodontal disease (11.1%, n = 82); caries and edentulism (0.5%, n = 4); oral mucosal lesion and caries (0.5%, n = 4); periodontal disease and edentulism (0.8%, n = 6); oral mucosal lesion and edentulism (0.3%, n = 2); caries, periodontal disease and edentulism (1.2%, n = 9); and caries, periodontal disease and oral mucosal lesion (0.3%, n = 2; Figure 2).
Figure 2.
Dental diagnoses of patients seen in the university SCD clinic, from January 2017 to June 2022
A significant association existed between gender and the number of patients with caries (χ2 = 6.860, P < 0.009), which was diagnosed in 62.2% of female patients. No significant association was noted for other diagnoses. In addition, significant associations were found between the age groups of patients and diagnosis with caries (χ2 = 13.628, P = 0.009), periodontal disease (χ2 = 53.181, P < 0.001), edentulism (χ2 = 89.725, P < 0.001), oral mucosal lesions (χ2 = 49.739, P < 0.001) and malocclusion (χ2 = 10.874, P < 0.029). The highest proportion of periodontal disease was noted in patients aged 21–40 years (69.7%).
Significant associations were observed between patients with different types of medical conditions and various dental diagnoses, except for dentoalveolar trauma [Table 2]. These were among those who presented with caries (χ2 = 12.050, P = 0.034), periodontal disease (χ2 = 36.196, P < 0.001), edentulism (χ2 = 72.941, P < 0.001), oral mucosal lesion (χ2 = 30.665, P < 0.001), and malocclusion (χ2 = 13.771, P = 0.017).
Table 2.
Medical conditions and dental diagnoses of patients with SHCN seen in the university SCD clinic (N = 742)
| Caries % (n) | Periodontal disease % (n) | Edentulism % (n) | Oral mucosal lesion % (n) | Dento-alveolar trauma % (n) | Malocclusion % (n) | |
|---|---|---|---|---|---|---|
| Medical compromise | 45.9 (56) | 60.7 (74) | 16.4 (20) | 9.8 (12) | 4.1 (5) | 0 (0) |
| Physical disability | 47.7 (31) | 72.3 (47) | 12.3 (8) | 0 (0) | 1.5 (1) | 0 (0) |
| Intellectual disability | 58.0 (214) | 39.6 (146) | 20.3 (1) | 1.4 (5) | 2.7 (10) | 4.9 (18) |
| Genetic syndrome | 60.4 (58) | 44.8 (43) | 0 (0) | 1.0 (1) | 2.1 (2) | 1.0 (1) |
| More than one disability | 63.2 (48) | 43.4 (33) | 2.6 (2) | 1.3 (1) | 3.9 (3) | 1.3 (1) |
| Psychiatric disorder | 35.7 (5) | 64.3 (9) | 7.1 (1) | 1 (1) | 0 (0) | 7.1 (1) |
| χ 2 | 12.050 | 36.196 | 72.941 | 30.665 | 2.075 | 13.771 |
| P-value | 0.034 | <0.001 | <0.001 | <0.001 | 0.839 | 0.017 |
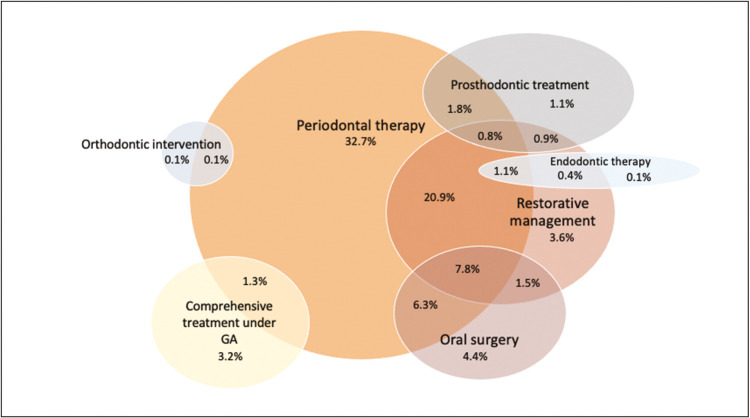
DENTAL TREATMENT RECEIVED
The most common treatment performed was periodontal treatment (76.1%, n = 565), followed by restorations (39.9%, n = 296), exodontia (22%, n = 163), comprehensive care under general anesthetics (10.5%, n = 78), prosthodontic treatment (6.7%, n = 50), endodontic therapy (2.4%, n = 18), and orthodontic intervention (0.3%, n = 2). Additionally, some patients received multiple treatments, as seen in Figure 3.
Figure 3.
Dental treatment done for patients with SHCN at the university SCD clinic
A significant association was observed between gender and the number of patients who received endodontic therapy (χ2 = 4.004, P = 0.045), with more females (4.0%, n = 10) seen than males. Furthermore, a significant association was noted between age and endodontic treatment (χ2 = 31.374, P < 0.001), with 11.1% (n = 8) from the age group 41–60 years. For prosthodontic treatment, 35.2% (n = 25) were aged 61–80 years (χ2 = 217.354, P < 0.001).
In addition, a significant association was observed between the medical condition and patients receiving restorative treatment, endodontics, prosthodontic therapy, oral surgical interventions, and comprehensive dental management under general anesthesia [Table 3].
Table 3.
Treatment received based on medical conditions
| Periodontal treatment, % (n) | Restorative therapy, % (n) | Endodontic treatment, % (n) | Prosthodontic management, % (n) | Orthodontic intervention, % (n) | Oral surgery, % (n) | General anesthesia, % (n) | |
|---|---|---|---|---|---|---|---|
| Medical compromise | 73.0 (89) | 44.3 (54) | 6.6 (8) | 25.4 (31) | 0 (0) | 29.5 (36) | 2.5 (3) |
| Physical disability | 78.5 (51) | 60.0 (39) | 3.1 (2) | 18.5 (12) | 0 (0) | 26.2 (17) | 1.5 (1) |
| Intellectual disability | 77.2 (285) | 35.0 (129) | 1.6 (6) | 0 (0) | 0.5 (2) | 21.4 (79) | 13.3 (49) |
| Genetic syndrome | 76.0 (73) | 33.3 (32) | 0 (0) | 0 (0) | 0 (0) | 13.5 (13) | 14.6 (14) |
| More than one disability | 77.6 (59) | 44.7 (34) | 0(0) | 3.9 (3) | 0 (0) | 15.8 (12) | 14.5 (11) |
| Psychiatric disorder | 57.1 (8) | 57.1 (8) | 14.3 (2) | 28.6 (4) | 0 (0) | 42.9 (6) | 0 (0) |
| χ 2 | 3.995 | 19.880 | 22.507 | 127.05 | 2.027 | 14.011 | 21.582 |
| P-value | 0.550 | 0.001 | <0.001 | <0.001 | 0.845 | 0.016 | <0.001 |
DISCUSSION
This study was conducted at the SCD Clinic, Faculty of Dentistry, a teaching hospital in Selangor, which began its operation in January 2017. At its inception, the clinic was operated by an SCD specialist and a pediatric specialist. The clinic provides treatment for individuals with SHCN across all ages. The two specialists working conjointly in the same clinical settings offer a smooth transition from pediatric to adult care, which is crucial, especially for individuals with SHCN.[8] As a result, a successful transition facilitated by this clinic attracts more patients yearly, and it has gained popularity among individuals with SHCN.
Therefore, a wide age range was noted in the data collected because the cases seen in the clinic range from infants to geriatrics. An SCD specialist treats patients aged 16 years and above, whereas patients below 16 years old are seen by a pediatric dentist.[7] More than half of the patients seen in the SCD clinic were children and young people age between 0 and 20 years old. This was followed by the age groups of 21–40 years, 61–80 years, 41–60 years, and 81–100 years. The study noted that most patients diagnosed with dental caries, dentoalveolar trauma, and malocclusion were below 20 years old. These findings are similar to various studies that have reported that the prevalence of such diagnoses is high in patients with SHCN in that age group. These studies have suggested that the creation and implementation of oral health policy providing an equitable oral health care system for these individuals, as well as continuous care from childhood to adulthood, is essential.[9,10,11] Periodontal disease was primarily diagnosed in patients aged 21–40, and the proportion of caries and edentulism was highest in those aged 81–100. These findings were expected because the prevalence of caries is high in the elderly, especially when their medical conditions and polypharmacy further complicate their oral health. The caries risk in older adults has also been reported to increase by 60% with a low stimulated saliva rate.[12]
This study also found that more male patients were seen in the clinic than female patients. Apart from being more dominant in the statistics of individuals with disabilities,[13] males are more susceptible to oral health diseases such as periodontitis and oral cancer due to behavior such as poor oral health care and tobacco use.[14] However, in this study, a significant association was noted between being female and diagnosis of dental caries, which resulted in more endodontic treatment received among them. Studies agree with this finding because caries prevalence in women is higher due to tooth eruption occurring earlier in girls, which causes earlier exposure to a cariogenic diet, as well as due to genetic predisposition.[14]
In addition, this study captured the geographical locations of patients who attended the clinic. Surprisingly, the clinic received patients from other states as well, albeit the clinic is located in the state of Selangor. Some patients who attended the clinic came from Johor, which is in the south of the country, and a few were from the northern part of Malaysia. This is due to the limited number of SCD clinics, although the number of individuals with disabilities is high. For instance, no SCD clinics are available in Johor or Perak, although they have the most significant number of individuals with disabilities after Selangor.[13] Furthermore, a study in Saudi Arabia reported that one of the difficulties faced in obtaining oral health care for patients with SHCN was geographical distance.[15] A similar situation can be seen in the findings of this study because a few patients traveled as far as several hundred kilometers to attend this clinic. This finding is not surprising because not only do patients need to commute quite a distance because dental clinics in Malaysia are unevenly distributed,[16] but most dental practitioners are uncomfortable treating patients with SHCN.[3] Hence, increasing the number of SCD clinics is recommended to reduce difficulties for patients with SHCN.
An increase occurred in the number of patients seen yearly, which reflects the statistical report by the Department of Social Welfare Malaysia that the number of people with SHCN has increased.[13] The greatest number of patients seen in the clinic had an intellectual disability, followed by medical compromise, genetic or chromosomal-related medical conditions, physical disability and psychiatric disorders. National data suggested that physical disability was the highest reported impairment in 2020.[13] However, this study reported intellectual disability as the most prevalent type seen in the clinic. This finding justifies the high oral health burden for patients with intellectual disabilities because they noted higher caries and periodontal disease rates.[17]
The dental diagnoses noted a high prevalence of caries and periodontal disease. These findings are in coherent to the pattern of oral diseases reported in the National Oral Health Policy 2022.[18] Furthermore, a high plaque score, untreated dental caries and inflammation of the gingiva are among the most seen oral health conditions in patients with SHCN and remain a significant health challenge.[2,17] Such findings have shown that collaboration between SCD and various departments in promoting a multidisciplinary approach is essential to ensure that each patient can be managed and treated holistically.
Patients with physical disabilities were reported to have the highest percentage of periodontal disease in this study. The Centers for Disease Control and Prevention defined disability as a condition of the body (impairment) that causes activity limitation and participation restriction. In this case, it can be explained that the impaired physical activity of patients caused incapability in performing oral self-care and difficulty in maintaining good oral hygiene, leading to periodontal disease.[19] Furthermore, the lack of attendance by patients with physical disabilities, despite representing the most reported disabilities, reflects various studies finding that physical barriers such as difficulty in accessing the facility and a lack of disabled-friendly infrastructure hinder them from seeking dental treatment.[20,21]
The study reported a significant proportion of medically compromised patients with oral mucosal lesions. Studies have shown that the medications taken, underlying psychological problems and oral manifestations of the condition itself harm oral health.[22] In addition, oral mucosal lesions such as candidiasis and aphthous stomatitis are commonly seen in immunocompromised patients.[23] Therefore, thorough intraoral assessment is vital because some intraoral lesions may be underlying signs and symptoms of an individual’s systemic condition.
However, surprisingly, no patients with genetic or syndromic conditions were diagnosed with edentulism in this study, whereas other studies have reported various cases of hypodontia and hyperdontia in this group.[24,25] Hence, the findings of this study suggest further investigation of the SCD clinic’s data, which is required to identify appropriate diagnosis and management of the patients seen.
The study noted that patients who attended the SCD clinic presented with multiple dental treatment needs, highlighting the importance of multidisciplinary intervention in managing patients with SHCN. This is because they may be presented with various risk factors, numerous treatment needs and complexities in management to ensure a comprehensive approach to patient care. A careful approach is needed because dental treatment for a person with SHCN is often complicated by physical, mental or social disability.[26] Interestingly, a high proportion of patients with psychiatric disorders who attended the clinic had received restorative, endodontic and prosthodontic treatment, as well as oral surgery. Such comprehensive care supports various studies that have stated that most antipsychotic drugs lead to xerostomia and eventually cause an extreme caries risk.[27] In addition, oral health neglect is common in these patients.[28] Hence, prevention, such as the application of topical fluoride and frequent recall visits, are necessary to ensure a reduction in caries risk and oral health diseases.[29]
The clinic in this study treats patients with disabilities as well as their caregivers. However, the pattern of treatment and dental diagnoses of caregivers were not analyzed because this study focused on the needs of patients with SHCN. Reducing caregiver burden is one of the various actions that provide health benefits to patients with SHCN, including improving their oral health conditions and compliance with dental appointments and performing proper oral hygiene care according to the instructions given.[30,31] Hence, for the benefit of the patients and their caregivers, this clinic provides treatment for their caregivers as well.
This study has several limitations. The data collected were solely based on the faculty’s iDeRMS system, which was initiated in 2017, and physical folders were used before the introduction of the system. Hence, some data might be missing from the transitional period, although every effort was made to ensure all data were included. Furthermore, the patient’s sociodemographic information such as socioeconomic status, ethnicity, religion, nationality and others were not collected for this study.
In addition, this study was done based on a localized institute, and may not reflect the study population of individuals with SHCN in Malaysia in entirely. However, findings of this study do provide important information to report situations in a teaching hospital, which is one of the healthcare service facilities that provide treatment for this group of patient cohort. As such, these findings serve as guidance for other teaching hospitals and service providers in terms of patients’ profiles as well as treatment needs and demands, which information could be used for future planning and development of SCD practice in this country and potentially worldwide.
CONCLUSION
This study shows a gradual increase in the number of patients who attended the SCD clinic over the years of a study period, with a significantly higher number of patients within 0–20-year-old category. Caries was the most prevalent condition, reported significantly higher among the female patients. There were also significant associations between the types of medical conditions with the different oral problems, namely caries, periodontal disease, edentulism, oral mucosal lesion, and malocclusion. In addition, this study reported periodontal therapy as the most common treatment provided, whereas receipt of endodontic treatment was significantly higher among female patients.
FUTURE SCOPE/CLINICAL SIGNIFICANCE
The analysis from this study provides insight into patients’ profiles in the SCD clinic based on their social demographics, health profile and treatment needs. This information is crucial for the further development of the services as well as teaching and learning purposes at an institutional level. The findings may also serve as valuable references for other institutions and service providers in this country and worldwide for similar purposes.
FINANCIAL SUPPORT AND SPONSORSHIP
Geran Penyelidikan Khas UiTM 600-RMC/GPK 5/3(187/2020).
CONFLICTS OF INTEREST
There are no conflicts of interest.
AUTHORS CONTRIBUTIONS
The authors confirm the contribution to the paper as follows; TYI: study concepts, literature research, data acquisition, statistical analysis and manuscript preparation. IWM: Study concepts, defined intellectual content, statistical analysis and manuscript review. MYPM: defined intellectual content, manuscript review. MSA: conceived the study idea, statistical analysis and manuscript review. All the authors approved the final version of the manuscript.
ETHICAL POLICY AND INSTITUTIONAL REVIEW BOARD STATEMENT
Ethics approval was granted by the research ethics committee in accordance to the ICH Good Clinical Practice Guidelines, Malaysian Good Clinical Practice Guidelines and the Declaration of Helsinki, by the participating university (ref no: REC/08/2021[MR/660]).
PATIENT DECLARATION OF CONSENT
Not applicable.
DATA AVAILABILITY STATEMENT
The data set used in the current study is available in the Integrated Dental Record Management System (iDeRMS).
ACKNOWLEDGEMENTS
The authors thank Ministry of Higher Education and Universiti Sains Islam Malaysia for the financial support for the postgraduate programme. The authors also thank Puan Nazifas Mohd Hussein for the assistance in accessing data from iDeRMS, as well as Puan Najibah Abdul Razak for the guidance of the statistical analysis.
REFERENCES
- 1.Ministry of Health Malaysia. Special Care Dentistry E-book. Oral Health Programme (OHP), Ministry of Health Malaysia. 2021 [Google Scholar]
- 2.Bernabe E, Marcenes W, Hernandez CR, Bailey J, Abreu LG, Alipour V, et al. Global, regional, and national levels and trends in burden of oral conditions from 1990 to 2017: A systematic analysis for the global burden of disease 2017 study. J Dent Res. 2020;99:362–73. doi: 10.1177/0022034520908533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ahmad MS, Razak IA, Borromeo GL. Special needs dentistry: Perception, attitudes and educational experience of Malaysian dental students. Eur J Dent Educ. 2015;19:44–52. doi: 10.1111/eje.12101. [DOI] [PubMed] [Google Scholar]
- 4.Hugo FN, Kassebaum NJ, Marcenes W, Bernabé E. Role of dentistry in global health: Challenges and research priorities. J Dent Res. 2021;100:681–5. doi: 10.1177/0022034521992011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lim M, Liberali S, Calache H, Parashos P, Borromeo G. Perspectives of the public dental workforce on the dental management of people with special needs. Aust Dent J. 2021;66:304–13. doi: 10.1111/adj.12836. [DOI] [PubMed] [Google Scholar]
- 6.Naimie Z, Ahmad NA, Shoaib LA, Safii SH, Mohamed Rohani M. Curriculum for special care dentistry: Are we there yet? J Int Oral Health. 2020;12:1–7. [Google Scholar]
- 7.Ahmad MS, Shafie N, Redhuan T, Mokhtar I. Referral pattern and treatment needs of patients managed at a Malaysian special care dentistry clinic. JInt Oral Health. 2019;11:299–303. [Google Scholar]
- 8.Chavis S, Canares G. The transition of patients with special health care needs from pediatric to adult-based dental care: A scoping review. Pediatr Dent. 2020;42:101–9. [PubMed] [Google Scholar]
- 9.American Academy of Pediatric Dentistry. Management of Dental Patients with Special Health Care Needs. The Reference Manual of Pediatric Dentistry Chicago, Ill: American Academy of Pediatric Dentistry; 2021. pp. 287–94. [Google Scholar]
- 10.da Silva SN, Gimenez T, Souza RC, Mello-Moura ACV, Raggio DP, Morimoto S, et al. Oral health status of children and young adults with autism spectrum disorders: Systematic review and meta-analysis. Int J Paediatr Dent. 2017;27:388–98. doi: 10.1111/ipd.12274. [DOI] [PubMed] [Google Scholar]
- 11.Ningrum V, Bakar A, Shieh TM, Shih YH. The oral health inequities between special needs children and normal children in Asia: A systematic review and meta-analysis. Healthcare (Basel) 2021;9:410. doi: 10.3390/healthcare9040410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chan AKY, Tamrakar M, Jiang CM, Lo ECM, Leung KCM, Chu CH. Common medical and dental problems of older adults: A narrative review. Geriatrics. 2021;6:76. doi: 10.3390/geriatrics6030076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Department of Social Welfare of Malaysia. Statistics Report. 2020;2021:33. [Google Scholar]
- 14.Lipsky MS, Su S, Crespo CJ, Hung M. Men and oral health: A review of sex and gender differences. Am J Mens Health. 2021;15:155798832110163. doi: 10.1177/15579883211016361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alfaraj A, Halawany HS, Al-Hinai MT, Al-Badr AH, Alalshaikh M, Al-Khalifa KS. Barriers to dental care in individuals with special healthcare needs in Qatif, Saudi Arabia: A caregiver’s perspective. Patient Prefer Adherence. 2021;15:69–76. doi: 10.2147/PPA.S291255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Md Bohari NF, Kruger E, John J, Tennant M. Analysis of dental services distribution in Malaysia: A geographic information systems-based approach. Int Dent J. 2019;69:223–9. doi: 10.1111/idj.12454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ward LM, Cooper SA, Hughes-McCormack L, Macpherson L, Kinnear D. Oral health of adults with intellectual disabilities: A systematic review. J Intellect Disabil Res. 2019;63:1359–78. doi: 10.1111/jir.12632. [DOI] [PubMed] [Google Scholar]
- 18.Ministry of Health Malaysia. National Oral Health Policy.Putrajaya. Oral Health Programme (OHP), Ministry of Health Malaysia. 2022 [Google Scholar]
- 19.Mun SJ, Jeon HS, Choi ES, Lee R, Kim SH, Han SY. Oral health status of inpatients with varying physical activity limitations in rehabilitation wards. Medicine (Baltimore) 2021;100:e26880. doi: 10.1097/MD.0000000000026880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.da Rosa SV, Moysés SJ, Theis LC, Soares RC, Moysés ST, Werneck RI, et al. Barriers in access to dental services hindering the treatment of people with disabilities: A systematic review. Int J Dent. 2020;2020:1–17. doi: 10.1155/2020/9074618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khan AJ, Md Sabri BA, Ahmad MS. Factors affecting provision of oral health care for people with special health care needs: A systematic review. Saudi Dental J. 2022;34:527–37. doi: 10.1016/j.sdentj.2022.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abiko Y, Paudel D, Matsuoka H, Moriya M, Toyofuku A. Psychological backgrounds of medically compromised patients and its implication in dentistry: A narrative review. Int J Environ Res Public Health. 2021;18:8792. doi: 10.3390/ijerph18168792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Meyer U, Kleinheinz J, Handschel J, Kruse-Lösler B, Weingart D, Joos U. Oral findings in three different groups of immunocompromised patients. J Oral Pathol Med. 2000;29:153–8. doi: 10.1034/j.1600-0714.2000.290402.x. [DOI] [PubMed] [Google Scholar]
- 24.Scott AM, Reed WM, Ajwani S, Parmenter TR. Panoramic radiographs and dental patients with down syndrome: A scoping review. Spec Care Dentist. 2023;43:199–220. doi: 10.1111/scd.12762. [DOI] [PubMed] [Google Scholar]
- 25.Subasioglu A, Savas S, Kucukyilmaz E, Kesim S, Yagci A, Dundar M. Genetic background of supernumerary teeth. Eur J Dent. 2015;09:153–8. doi: 10.4103/1305-7456.149670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dougall A, Fiske J. Access to special care dentistry. Part 1: Access. Br Dent J. 2008;204:605–16. doi: 10.1038/sj.bdj.2008.457. [DOI] [PubMed] [Google Scholar]
- 27.Cockburn N, Pradhan A, Taing MW, Kisely S, Ford PJ. Oral health impacts of medications used to treat mental illness. J Affect Disorder. 2017;223:184–93. doi: 10.1016/j.jad.2017.07.037. [DOI] [PubMed] [Google Scholar]
- 28.Kenny A, Dickson-Swift V, Gussy M, Kidd S, Cox D, Masood M, et al. Oral health interventions for people living with mental disorders: Protocol for a realist systematic review. Int J Mental Health Syst. 2020;14:24. doi: 10.1186/s13033-020-00357-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Featherstone JDB, Crystal YO, Alston P, Chaffee BW, Doméjean S, Rechmann P, et al. Evidence-based caries management for all ages-practical guidelines. Front Oral Health. 2021;2:657518. doi: 10.3389/froh.2021.657518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chi DL, McManus BM, Carle AC. Caregiver burden and preventive dental care use for US children with special health care needs: A stratified analysis based on functional limitation. Matern Child Health J. 2014;18:882–90. doi: 10.1007/s10995-013-1314-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wan Roselan WN, Bawawi SN, Baharuddin IH, Wan Mokhtar I. Parents’ oral health promotion efforts for their children with down syndrome and the children’s oral health. Spec Care Dentist. 2022 doi: 10.1111/scd.12774. [published online ahead of print,10 Sep 2022] [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data set used in the current study is available in the Integrated Dental Record Management System (iDeRMS).