Abstract
We analyzed bone marrow and blood from human immunodeficiency virus type 1 (HIV-1)-infected individuals and described the HIV-1 quasispecies in these cellular compartments. HIV-1 isolates from the bone marrow of thrombocytopenic patients contained distinct amino acids in the V3 loop and infected T-cell lines, implicating this virus in the development of thrombocytopenia.
Human immunodeficiency virus type 1 (HIV-1) affects the hematopoietic system, causing various peripheral blood cytopenias, of which thrombocytopenia (TP) accounts for approximately 30% of the cases (25, 28). The direct involvement of HIV-1 in the pathogenesis of TP has been implicated by several studies. Viral transcripts have been detected in megakaryocytes of patients with TP (38, 76), and primary megakaryocytes and megakaryocytic cell lines have been shown to be infectable by HIV-1 (38, 47). In addition, suppressed megakaryocytopoiesis in HIV-1-infected patients and infection of megakaryocyte precursors by HIV-1 have been suggested to play a role in the development of TP (2, 6, 14, 72). Finally, ultrastructural studies of bone marrow biopsy specimens obtained from HIV-1-infected TP patients showed abnormal megakaryocyte morphology (77), and treatment of TP patients with zidovudine resulted in recovery of platelet counts (3, 49). However, conflicting results have been reported by several investigators who failed to detect infection of megakaryocytes and their precursors by HIV-1 (16, 39, 71, 74). Therefore, even though little doubt about the involvement of HIV-1 in the pathogenesis of TP exists, the mechanism by which HIV-1 causes suppression of megakaryocytopoiesis is not fully understood.
An important question in the pathogenesis of TP is whether in the bone marrow of patients with TP there exist HIV-1 strains that are involved in the development of thrombocytopenia. We studied HIV-1 sequence heterogeneity in the bone marrow of HIV-1-infected patients with and without TP in order to delineate the viral determinants associated with this disorder. We chose to analyze the third hypervariable loop (V3) of HIV-1 envelope glycoprotein gp120 because it has been shown to be involved in the pathogenesis of this virus. Specifically, the emergence of rapidly replicating, syncytium-inducing (SI) and non-syncytium-inducing (NSI) variants in the peripheral blood of HIV-1-infected individuals has been linked to changes in the V3 loop of HIV-1 (35, 65). Furthermore, a significant correlation between the emergence of highly replicating isolates in peripheral blood and the reduction of CD4+-cell counts and AIDS development has been described (62, 63). In addition, AIDS dementia in HIV-1-infected patients has been linked to changes in the V3 loop of HIV-1 (59). Finally, the V3 loop has been shown to elicit neutralizing antibodies to HIV-1 and to be involved in cellular tropism and coreceptor utilization (4, 5, 12, 13, 26, 32, 53, 56, 64, 68).
Our studies of HIV-1 sequence heterogeneity in the bone marrow of HIV-1-infected patients examined the quasispecies of this virus in the bone marrow and compared it to that in the blood. Furthermore, we constructed infectious molecular clones and characterized their cellular tropism. This study included 12 HIV-1-infected patients. Three of the patients (A, B, and C) were diagnosed with HIV-associated TP, which is defined by determination of platelet counts of <100,000/mm3 in the absence of antiretroviral therapy or invasion of the bone marrow by opportunistic infections or neoplasms. The bone marrow of patients with TP showed mild hypercellularity and megakaryocytic hyperplasia and dysplasia. Eight patients (D, F, G, H, I, J, K, and L) were diagnosed with various neoplasms or opportunistic infections, and the low platelet counts in some of these patients were the result of a myelodysplastic process. Finally, one patient (E) was asymptomatic (Table 1).
TABLE 1.
Patient list
| Patient | Disorder(s)a | No. of CD4+ T cells/μl of blood | No. of platelets (103)/mm3 of blood | Specimen obtainedb
|
|
|---|---|---|---|---|---|
| BM | Bld | ||||
| A | TP, A, L | 4 | 89 | + | − |
| Bc | TP | 69 | + | − | |
| C | TP | 20 | 35 | + | − |
| D | Nocardia infection | 3 | 224 | + | − |
| E | Asymptomatic | NDd | 183 | + | − |
| F | NHL | 80 | 60 | + | − |
| G | TB | 30 | 27 | + | − |
| H | HD | ND | 191 | + | − |
| I | Myeloma | 700 | 256 | + | − |
| J | HD | ND | 142 | + | + |
| K | HD | 61 | 279 | + | + |
| L | NHL | 241 | 258 | + | + |
TP, HIV-associated thrombocytopenia; A, anemia; L, leukopenia; NHL, non-Hodgkin’s lymphoma; TB, tuberculosis; HD, Hodgkin’s disease.
BM, bone marrow aspirate; Bld, blood. +, specimen obtained; −, no specimen obtained.
Records for this patient are not available.
ND, not determined.
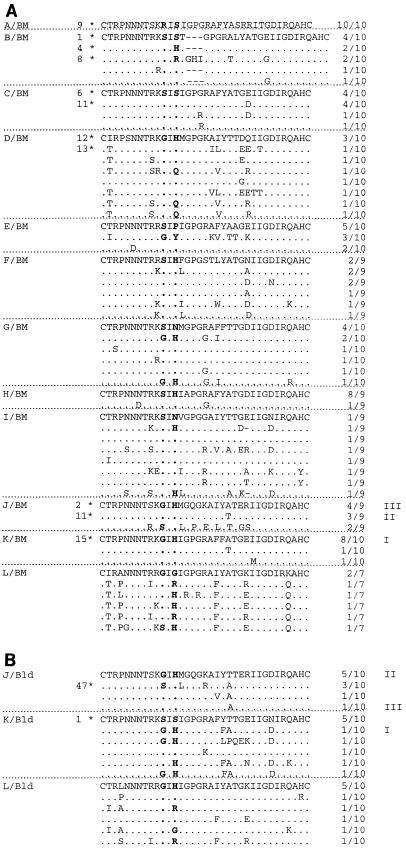
Bone marrow mononuclear cells (BMMC) and peripheral blood mononuclear cells (PBMC) were isolated by Ficoll-Hypaque gradient centrifugation; this was done without prior cocultivation to avoid adaptation of the virus to tissue culture conditions. Total DNA was isolated from BMMC or PBMC (58) and PCR amplified by using a set of nested primers. The sequences of these primers and their locations on HXB2 (GenBank accession no. K03455) are as follows: JA9, 5′ GAATTCCACAGTACAATGTACACATG 3′, nucleotides (nt) 6952 to 6971; JA10, 5′ GAATTCAGATCTGTCAATTTCACGGA 3′, nt 7040 to 7059; JA11, 5′ GAATTCGGGTCCCCTCCTGAGGATTG 3′, nt 7319 to 7338; and JA12, 5′ GAATTCACAGTAGAAAAATTCCCCTC 3′, nt 7359 to 7378. The internal primers, JA10 and JA11, include the BglII and PpuMI restriction sites, respectively. The first round of PCR was performed with primers JA9 and JA12 (30 μM each) in a 100-μl reaction volume, using 10 μl of each patient’s bone marrow or blood cell lysate (the equivalent of 106 BMMC or PBMC) as the template, whereas the second round of PCR was performed with primers JA10 and JA11 (30 μM each), using 10 μl of the first PCR mixture as the template. For both rounds of PCR, 0.2 mM each deoxyribonucleoside triphosphate, 1.5 mM MgCl2, and 0.5 U of Taq polymerase (Gibco BRL) were added to the reaction mixture. DNA was amplified for 30 cycles consisting of 94°C for 2 min, 55°C for 1 min, and 72°C for 1 min. The PCR-amplified V3 loop sequences were cloned into the pCR-TRAP vector (GenHunter Corp.), and on average 10 clones per patient sample (147 clones total) were sequenced on both strands to achieve more than 99% sequence accuracy. The amino acid sequences were deduced from the nucleotide sequences (GenBank accession no. AF094977 to AF095123) and aligned (Fig. 1). The V3 loops of all patients’ clones were 35 amino acids long, with the exception of that for patient B, which exhibited a 3-amino-acid insertion in one sequence, and that for patient I, which exhibited a single-amino-acid deletion in two sequences (Fig. 1). Only three clones had inactivating mutations in the V3 loop, and these were not included in our subsequent analyses.
FIG. 1.
Alignment of V3 loop amino acid sequences of HIV-1 from bone marrow (A) and blood (B). The most prominent sequence for each patient is shown, using the one-letter amino acid code. The ratio to the right indicates the frequency of the sequence in each patient’s bone marrow or blood sample. Identical amino acids and deletions are represented by dots and dashes, respectively. Amino acid insertions are shown where they occur, but dashes are introduced into the rest of the sequences to optimize alignment. Boldfaced amino acids designate positions 11 and 13 of the V3 loop. Asterisks indicate the V3 loop sequences used to construct HIV-1 molecular clones, and the numbers next to them indicate the corresponding molecular clones. Roman numerals I, II, and III designate amino acid sequences that are identical in the bone marrow and blood of two of the patients.
To estimate the number of nucleotides misincorporated by Taq polymerase into the sequences shown in Fig. 1, the V3 loop of HXB2 was PCR amplified under identical conditions, several clones were sequenced, and the percentage of nucleotides misincorporated into the sequence was calculated. Of 4,720 nt sequenced, 6 nt were misincorporated into HXB2 by Taq polymerase, making the level of Taq-introduced error 0.13%. For the V3 loop sequences shown in Fig. 1, we expected the introduction of 19 or 20 nt substitutions whereas 395 nt substitutions were identified (data not shown). Therefore, the sequences obtained are representative of the sequences present in the bone marrow and peripheral blood of the patients.
To determine how the HIV-1 quasispecies in the bone marrow compares to that in the blood, we compared the V3 loop amino acid sequences from the bone marrow of patients L, K, and J (L/BM, K/BM, and J/BM, respectively [Fig. 1A]) to the amino acid sequences from the blood of the same patients (L/Bld, K/Bld, and J/Bld, respectively [Fig. 1B]). For patient L, common sequences were not observed in the blood and bone marrow. For patients K and J, a minor sequence observed in the blood was the major sequence in the bone marrow, and the major sequence in the blood of patient J was a minor sequence in the bone marrow. Therefore, the HIV-1 quasispecies in the bone marrow and blood differ, with some sequences being present in both compartments but in different frequencies.
The V3 loop nucleotide sequences were aligned by using the CLUSTAL algorithm (31), and phylogenetic relationships among them were estimated by the neighbor-joining method (54). The reference isolate ELI (subtype D) was used to root the tree. All sites in which there were gaps were excluded from our analyses, and all algorithms were implemented by CLUSTALW (30). Phylogenetic analysis showed that each patient’s sequences formed monophyletic clusters, verifying the absence of cross-contamination between samples (Fig. 2). As expected, since all patients lived and became infected in the United States, all patients’ sequences conformed to the subtype B consensus (data not shown).
FIG. 2.
Rooted phylogenetic tree showing the V3 loop sequences of HIV-1 from the bone marrow of 12 patients and the blood of 3 of the patients. The scale bar indicates 5% divergence, at the nucleotide level, between any two sequences. BM, bone marrow; Bld, blood.
To determine whether the HIV-1 sequences sustained in the bone marrow of TP patients were distinct from those of patients without TP, the V3 loop amino acid sequences of the two groups were compared. To facilitate this comparison, the consensus amino acid sequences were compiled by calculating the frequency of each amino acid for every position in the V3 loop (Fig. 3). Important amino acid differences between the sequences of patients with and without TP were observed at positions 11 and 13 of the V3 loop, whereas conservative changes were observed at the rest of the positions in the V3 loop (Fig. 3). Specifically, in patients with TP, position 11 was occupied by serine or arginine, whereas in patients without TP, arginine was never observed at position 11 and was replaced by glycine, a smaller and more flexible amino acid. Similarly, in patients with TP, position 13 was occupied predominantly by serine (87%) and histidine and arginine were present at low frequencies (7%). In patients without TP, position 13 was occupied predominantly by histidine (63%) and, most importantly, serine was never observed at this position. Therefore, in patients with TP, the amino acids arginine and serine preferentially occupied positions 11 and 13 of the HIV-1 V3 loop whereas the amino acids glycine and histidine were selected against in these positions. The statistical significance of the amino acid distribution at positions 11 and 13 of the HIV-1 V3 loop was determined by the chi-square test. The presence of serine, arginine, or glycine at position 11 of the V3 loop was not statistically significant (P = 0.141), while that of serine, histidine, asparagine, or proline at position 13 of the V3 loop was significant (P = 0.009), although this makes no allowance for multiple comparisons. Since the number of patients studied was small (12 in total), the statistical significance of our results is difficult to assess.
FIG. 3.
The V3 loop consensus sequences from bone marrow HIV-1 sequences of patients with and without TP. Subscripts designate the frequency of each amino acid for every position in the V3 loop. The TP consensus was compiled from the 30 amino acid sequences of patients A to C. The non-TP consensus was compiled from the 83 amino acid sequences of patients D to L.
The cellular tropism of the bone marrow HIV-1 isolates was studied by constructing 11 molecular clones with V3 loop sequences from the bone marrow of three patients with TP (A, B, and C) and three patients without TP (D, J, and K) (Table 2). Two molecular clones with V3 loop sequences, from the blood of two patients (J and K), were also constructed to compare the cellular tropism of the bone marrow isolates to that of the blood isolates (Table 2). The construction of the molecular clones was done in two steps. The V3 loop sequences were isolated from the PCR-TRAP vector by BglII and PpuMI digestion and subcloned into BglII- and PpuMI-digested vector pSP65env. The pSP65env vector contains the SalI-BsaBI fragment of the HXB2 envelope gene (nt 5785 to 7554). The SalI-BsaBI fragments from pSP65env were cloned into the SalI- and BsaBI-digested p120 full-length molecular clone. p120 is a chimeric HIV-1 molecular clone that contains the envelope gene sequence from HXB2 (nt 5785 to 8474) substituted into the NL4-3 backbone (GenBank accession no. M19921). The molecular clones were analyzed by restriction enzyme digestion, using enzymes unique to each sequence, to verify the presence of the expected V3 loop in each clone (data not shown). High-titer viral stocks were prepared by transfection of 293T cells with the molecular clones, and p24gag titers were determined.
TABLE 2.
Infection of cells with HIV-1 molecular clones
| Molecular clonea | Fold increase in RT activity after infection ofb:
|
||||||
|---|---|---|---|---|---|---|---|
| Donor PBMC
|
Donor MΦ
|
T-cell line:
|
|||||
| 1 | 2 | 1 | 2 | MT-2 | Jurkat | Hut78 | |
| A/BM9 | 38 | — | — | — | 98 | 357 | — |
| B/BM1 | — | 19 | — | — | — | — | — |
| B/BM4 | — | 21 | — | — | — | — | — |
| B/BM8 | 59 | — | — | — | 192 | 415 | 26 |
| C/BM6 | 57 | 11 | 29 | 9.8 | — | — | — |
| C/BM11 | 56 | 7.6 | 22 | 17 | — | — | — |
| D/BM12 | — | 25 | — | — | — | — | — |
| D/BM13 | 33 | 22 | — | — | — | — | — |
| J/BM2 | — | — | — | — | — | — | — |
| J/BM11 | — | 16 | — | — | — | — | — |
| K/BM15 | 66 | 10 | 150 | 64 | — | — | — |
| J/Bld47 | 38 | 12 | — | — | 234 | — | — |
| K/Bld1 | 55 | 9.5 | 6.6 | 5.2 | — | — | — |
HIV-1 molecular clones from TP patients are underlined.
Numerical values represent the fold increase in reverse transcriptase (RT) activity above the background, and dashes represent background levels of RT activity (3 × 103 to 5 × 103 cpm/ml). The time points shown are at the peak of RT activity. MΦ, primary macrophages.
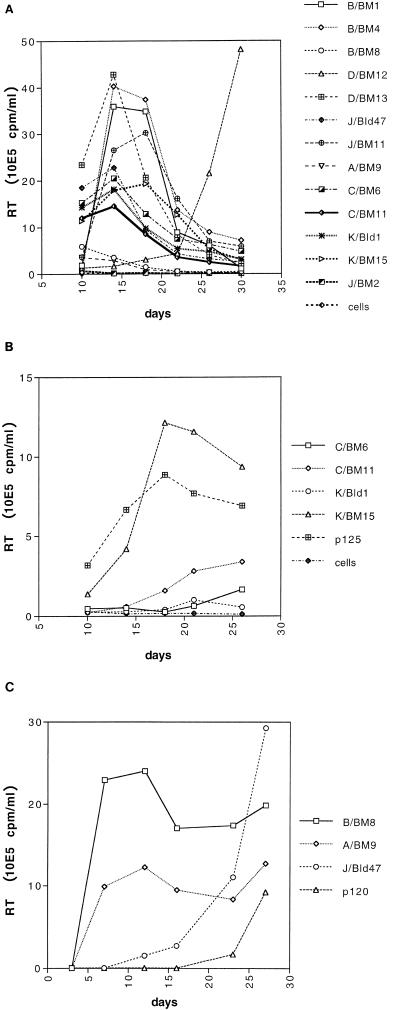
The HIV-1 molecular clones were used to infect PBMC, primary macrophages, and the T-cell lines MT-2, Jurkat, and Hut78. PBMC were activated in a solution containing 10 μg of phytohemagglutinin A per ml and 50 U of recombinant interleukin-2 per ml for 3 days and then maintained in interleukin-2. Primary macrophages were maintained in a solution containing 500 U of macrophage colony-stimulating factor per ml and were infected after 7 days in culture. Cells (106) were infected with approximately 500 ng of p24gag overnight, in triplicate, and with macrophages and PBMC from two different donors. The ability of the HIV-1 molecular clones to infect PBMC and primary macrophages was donor dependent (Table 2). C/BM6, C/BM11, D/BM13, K/BM15, J/Bld47, and K/Bld1 were able to replicate in both donors’ PBMC, albeit with different kinetics. However, A/BM9, B/BM1, B/BM4, B/BM8, D/BM12, and J/BM11 replicated in the PBMC of only one donor. Similarly, C/BM6, C/BM11, K/BM15, and K/Bld1 were able to replicate in macrophages of both donors but with different kinetics. Figures 4A and B show the results of representative infections of PBMC and primary macrophages with the HIV-1 molecular clones. The ability of the molecular clones to replicate in T-cell lines was determined by infecting MT-2, Jurkat, and Hut78 cells with the viruses (Table 2). B/BM8 was able to replicate in all three T-cell lines, whereas A/BM9 replicated in MT-2 and Jurkat cells and J/Bld47 replicated only in MT-2 cells. The molecular clones which infected MT-2 cells (A/BM9, B/BM8, and J/Bld47) also formed syncytia in these cells (SI isolates) (Fig. 4C). J/BM2 was unable to infect PBMC, primary macrophages, or T-cell lines but infected HeLa cells expressing surface human CD4, CXCR4, and CCR5, suggesting that J/BM2 is a functional clone but that its infectivity is low (data not shown). In conclusion, four (A/BM9, B/BM8, C/BM6, and C/BM11) of six HIV-1 isolates from the bone marrow of patients with TP replicated in T-cell lines or primary macrophages. In contrast, HIV-1 isolates from the bone marrow of patients without TP did not replicate in T-cell lines, and only one of five isolates (K/BM15) replicated in primary macrophages.
FIG. 4.
Replication kinetics of HIV-1 isolates in activated PBMC (A), primary macrophages (B), and MT-2 cells (C). p120 and p125 are T-cell-tropic and macrophage-tropic HIV-1 molecular clones, respectively. Activated PBMC and primary macrophages correspond to donor 2 of Table 2. Supernatants were assayed for reverse transcriptase (RT) activity (expressed as counts per minute per milliliter of supernatant) every 4 days. Each point represents the average of three independent measurements.
Even though bone marrow is the major hematopoietic organ in the adult human (37, 50), very little is known about the biological characteristics of HIV-1 in this cellular compartment. HIV-1 infection results in hematopoietic suppression in the bone marrow, but the mechanisms of this suppression are not completely understood. HIV-1 infection of mature hematopoietic cells has been demonstrated for megakaryocytes (38, 47, 76), and this virus has been shown to be cytopathic for megakaryocytic cell lines (36). In addition, CD34+ hematopoietic precursors have been shown to be infected by HIV-1 (6, 7, 57, 58). Dysregulated production of cytokines by HIV-1-infected bone marrow stromal cells has been suggested to cause hematopoietic dysfunction in the absence of progenitor-cell infection (1, 16, 48). Finally, viral proteins have been shown to be cytotoxic for cells in the bone marrow (42, 73, 75). However, hematopoietic dysfunction in the bone marrow is also caused by factors that are secondary to HIV-1 infection, such as drug toxicity and invasion of the bone marrow by neoplasms or opportunistic pathogens (29, 41, 43). Therefore, several factors are involved in HIV-associated hematopoietic dysfunction. Infection of mature hematopoietic cells, progenitor cells, and bone marrow stromal cells is clearly involved in HIV-associated hematopoietic dysfunction, and it should be distinguished from the hematopoietic dysfunction caused by the action of opportunistic infections, neoplasms, or drug toxicity.
Further support for the potential of retroviruses to infect megakaryocytes and platelets comes from studies on murine retroviruses. Murine retroviruses have been shown to induce thrombocytopenia in several strains of mice. Thrombocytopenia in these mice was not the result of spleen enlargement or destruction of megakaryocytes by leukemic cells in the bone marrow; rather, direct infection of megakaryocytes by murine retroviruses was demonstrated (18, 19).
The present study was performed to delineate the HIV-1 V3 loop determinants that are associated with the development of HIV-associated hematopoietic dysfunction and specifically TP. Two groups of patients were analyzed, patients with TP and patients with hematopoietic dysfunction caused by the invasion of bone marrow by neoplasms or opportunistic pathogens (Table 1). One asymptomatic patient was also included in our analyses. Sequence analysis of the HIV-1 V3 loop from the bone marrow of HIV-1-infected patients identified specific amino acids that distinguish patients with TP from the control patients without TP at positions 11 and 13 (Fig. 3). The role of the amino acids at these positions in cellular tropism and syncytium formation has been demonstrated for HIV-1 isolates from peripheral blood (5, 10, 11, 21, 35, 44, 45, 68, 69). However, we did not observe a correlation between the amino acids at positions 11 and 13 of the HIV-1 V3 loop and the cellular tropism and SI phenotype of the HIV-1 bone marrow isolates. Additional determinants outside the V3 loop may be involved in the development of the viral phenotype, as has been shown for the SI phenotype of HIV-1 (27). Our molecular clones include the V3 loop and portions of the C2 and C3 regions of the HIV-1 envelope gene. Molecular clones that encompass the full-length HIV-1 envelope gene are being constructed to study the involvement of viral determinants beyond the region of the V3 loop in the development of TP.
Sequence analysis of the HIV-1 V3 loop identified the distribution of HIV-1 in bone marrow and blood. Most HIV-1 sequences in the bone marrow appeared to be unique to this compartment, whereas some sequences were present in both bone marrow and blood but at different frequencies. A similar sequence distribution of HIV-1 has been reported for various lymphoid or nonlymphoid tissues and peripheral blood of asymptomatic and AIDS patients (17, 21, 51, 66). Bone marrow is a tissue rich in cells producing a multitude of cytokines and growth factors, and it contains numerous cell types susceptible to infection by HIV-1 (1, 22, 28, 33, 40, 46, 48, 52, 61, 67, 70). Therefore, the HIV-1 quasispecies in this compartment may be unique. Alternatively, the presence of HIV-1 in the bone marrow may be the result of blood filtration of this tissue. Our data cannot distinguish between the two possibilities, and conflicting results on the existence of unique quasispecies in lymphoid tissue have been reported (60, 66).
Construction of infectious molecular clones with HIV-1 V3 loop sequences from the bone marrow of patients with and without TP was used to determine the cellular tropism of the bone marrow isolates. Specifically, four of six isolates from patients with TP replicated in T-cell lines or primary macrophages, whereas none of the isolates from patients without TP replicated in T-cell lines and only one of five non-TP patient isolates replicated in primary macrophages. The bone marrow isolates exhibited different abilities to infect T-cell lines in vitro. Nevertheless, all T-cell-line-tropic isolates induced the formation of syncytia on MT-2 cells (SI isolates). We cannot explain the differential infection of lymphoid cell lines by the bone marrow HIV-1 isolates; however, similar observations have been reported by others (8, 15, 23). In addition, the cellular tropism of some bone marrow isolates was restricted to PBMC, with these isolates being unable to establish a productive infection in T-cell lines or primary macrophages. HIV-1 primary isolates unable to infect primary macrophages and lymphoid cell lines have been isolated from peripheral blood and the central nervous system of asymptomatic patients by several investigators (8, 9, 24, 33, 34, 65).
We did not observe a correlation between CD4+-cell counts and the presence of T-cell-line-tropic, SI isolates in the bone marrow. Specifically, patient C, who had TP, and patient D, who lacked TP, had low CD4+-cell counts, but molecular clones constructed with V3 loop sequences from these patients were NSI and did not replicate in T-cell lines. Since we did not construct molecular clones with all HIV-1 sequences from the bone marrow of these patients, the cellular tropism of the rest of the sequences is not known. However, we constructed molecular clones with the most-prominent sequences in the bone marrow, and therefore the cellular tropism of these isolates should be representative of the predominant HIV-1 strains in this tissue. Isolation of NSI, macrophage-tropic isolates from patients with late-stage disease has been reported by several investigators (20, 55, 63, 65).
In conclusion, we determined the biological characteristics of HIV-1 in the bone marrow of HIV-1-infected patients and identified distinct amino acids in the V3 loop that distinguish patients with TP from those without TP. Our data suggest that AIDS patients with hematopoietic dysfunction caused by the invasion of bone marrow by neoplasms or opportunistic pathogens sustain HIV-1 strains with an NSI phenotype. On the contrary, two of three patients with HIV-associated hematopoietic dysfunction and TP have SI HIV-1 strains in the bone marrow. Therefore, the presence of SI HIV-1 strains in the bone marrow may constitute another mechanism for the development of TP, either by infection of megakaryocytes or their precursors or by infection of cells of the bone marrow microenvironment. We are presently investigating the ability of the bone marrow isolates to infect megakaryocytes and their precursors in CD34+-cell cultures.
Acknowledgments
The authors thank Suzanne E. Pontow and Chia-Suei Hung for helpful discussions and critical review of the manuscript, Tom Blackwell for performing the statistical analysis, Carol Lin for technical assistance, and Nancy Vander Hayden for isolating some of the BMMC and for valuable suggestions.
This work was supported by grants from the Public Health Service (HL53744 and A124745).
REFERENCES
- 1.Bahner I, Kearns K, Coutinho S, Leonard E H, Kohn D B. Infection of human marrow stroma by human immunodeficiency virus-1 (HIV-1) is both required and sufficient for HIV-1-induced hematopoietic suppression in vitro: demonstration by gene modification of primary human stroma. Blood. 1997;90:1787–1798. [PubMed] [Google Scholar]
- 2.Ballem P J, Belzberg A, Devine D V, Lyster D, Spruston B, Chambers H, Doubroff P, Mikulash K. Kinetic studies of the mechanism of thrombocytopenia in patients with human immunodeficiency virus infection. N Engl J Med. 1992;327:1779–1784. doi: 10.1056/NEJM199212173272503. . (Comments, 327:1812–1813, 1992, and 328:1785–1786, 1993.) [DOI] [PubMed] [Google Scholar]
- 3.Boyar A, Beall G. HIV-seropositive thrombocytopenia: the action of zidovudine. AIDS. 1991;5:1351–1356. [PubMed] [Google Scholar]
- 4.Carrillo A, Ratner L. Human immunodeficiency virus type 1 tropism for T-lymphoid cell lines: role of the V3 loop and C4 envelope determinants. J Virol. 1996;70:1301–1309. doi: 10.1128/jvi.70.2.1301-1309.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carrillo A, Trowbridge D B, Westervelt P, Ratner L. Identification of HIV-1 determinants for T lymphoid cell line infection. Virology. 1993;197:817–824. doi: 10.1006/viro.1993.1664. [DOI] [PubMed] [Google Scholar]
- 6.Chelucci C, Federico M, Guerriero R, Mattia G, Casella I, Pelosi E, Testa U, Mariani G, Hassan H J, Peschle C. Productive human immunodeficiency virus-1 infection of purified megakaryocytic progenitors/precursors and maturing megakaryocytes. Blood. 1998;91:1225–1234. [PubMed] [Google Scholar]
- 7.Chelucci C, Hassan H J, Locardi C, Bulgarini D, Pelosi E, Mariani G, Testa U, Federico M, Valtieri M, Peschle C. In vitro human immunodeficiency virus-1 infection of purified hematopoietic progenitors in single-cell culture. Blood. 1995;85:1181–1187. [PubMed] [Google Scholar]
- 8.Cheng-Mayer C, Seto D, Tateno M, Levy J A. Biologic features of HIV-1 that correlate with virulence in the host. Science. 1988;240:80–82. doi: 10.1126/science.2832945. [DOI] [PubMed] [Google Scholar]
- 9.Cheng-Mayer C, Weiss C, Seto D, Levy J A. Isolates of human immunodeficiency virus type 1 from the brain may constitute a special group of the AIDS virus. Proc Natl Acad Sci USA. 1989;86:8575–8579. doi: 10.1073/pnas.86.21.8575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chesebro B, Wehrly K, Nishio J, Perryman S. Macrophage-tropic human immunodeficiency virus isolates from different patients exhibit unusual V3 envelope sequence homogeneity in comparison with T-cell-tropic isolates: definition of critical amino acids involved in cell tropism. J Virol. 1992;66:6547–6554. doi: 10.1128/jvi.66.11.6547-6554.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chesebro B, Wehrly K, Nishio J, Perryman S. Mapping of independent V3 envelope determinants of human immunodeficiency virus type 1 macrophage tropism and syncytium formation in lymphocytes. J Virol. 1996;70:9055–9059. doi: 10.1128/jvi.70.12.9055-9059.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choe H, Farzan M, Sun Y, Sullivan N, Rollins B, Ponath P D, Wu L, Mackay C R, LaRosa G, Newman W, Gerard N, Gerard C, Sodroski J. The beta-chemokine receptors CCR3 and CCR5 facilitate infection by primary HIV-1 isolates. Cell. 1996;85:1135–1148. doi: 10.1016/s0092-8674(00)81313-6. [DOI] [PubMed] [Google Scholar]
- 13.Cocchi F, DeVico A L, Garzino-Demo A, Cara A, Gallo R C, Lusso P. The V3 domain of the HIV-1 gp120 envelope glycoprotein is critical for chemokine-mediated blockade of infection. Nat Med. 1996;2:1244–1247. doi: 10.1038/nm1196-1244. . (Comment, 3:367–368, 1997.) [DOI] [PubMed] [Google Scholar]
- 14.Cole J L, Marzec U M, Gunthel C J, Karpatkin S, Worford L, Sundell I B, Lennox J L, Nichol J L, Harker L A. Ineffective platelet production in thrombocytopenic human immunodeficiency virus-infected patients. Blood. 1998;91:3239–3246. [PubMed] [Google Scholar]
- 15.Connor R I, Mohri H, Cao Y, Ho D D. Increased viral burden and cytopathicity correlate temporally with CD4+ T-lymphocyte decline and clinical progression in human immunodeficiency virus type 1-infected individuals. J Virol. 1993;67:1772–1777. doi: 10.1128/jvi.67.4.1772-1777.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.De Luca A, Teofili L, Antinori A, Iovino M S, Mencarini P, Visconti E, Tamburrini E, Leone G, Ortona L. Haemopoietic CD34+ progenitor cells are not infected by HIV-1 in vivo but show impaired clonogenesis. Br J Haematol. 1993;85:20–24. doi: 10.1111/j.1365-2141.1993.tb08640.x. [DOI] [PubMed] [Google Scholar]
- 17.Delwart E L, Mullins J I, Gupta P, Learn G H, Jr, Holodniy M, Katzenstein D, Walker B D, Singh M K. Human immunodeficiency virus type 1 populations in blood and semen. J Virol. 1998;72:617–623. doi: 10.1128/jvi.72.1.617-623.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dennis L H, Brodsky I. Thrombocytopenia induced by the Friend leukemia virus. J Natl Cancer Inst. 1965;35:993–999. [PubMed] [Google Scholar]
- 19.Dennis L H, Brodsky I. A dose-response curve employing thrombocytopenia induced by the Friend leukemia virus. Proc Soc Exp Biol Med. 1965;120:683–685. doi: 10.3181/00379727-120-30624. [DOI] [PubMed] [Google Scholar]
- 20.Dittmar M T, Simmons G, Donaldson Y, Simmonds P, Clapham P R, Schulz T F, Weiss R A. Biological characterization of human immunodeficiency virus type 1 clones derived from different organs of an AIDS patient by long-range PCR. J Virol. 1997;71:5140–5147. doi: 10.1128/jvi.71.7.5140-5147.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Donaldson Y K, Bell J E, Holmes E C, Hughes E S, Brown H K, Simmonds P. In vivo distribution and cytopathology of variants of human immunodeficiency virus type 1 showing restricted sequence variability in the V3 loop. J Virol. 1994;68:5991–6005. doi: 10.1128/jvi.68.9.5991-6005.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Doweiko J P. Hematologic aspects of HIV infection. AIDS. 1993;7:753–757. doi: 10.1097/00002030-199306000-00001. . (Editorial.) [DOI] [PubMed] [Google Scholar]
- 23.Dumitrescu O, Kalish M L, Kliks S C, Bandea C I, Levy J A. Characterization of human immunodeficiency virus type 1 isolates from children in Romania: identification of a new envelope subtype. J Infect Dis. 1994;169:281–288. doi: 10.1093/infdis/169.2.281. [DOI] [PubMed] [Google Scholar]
- 24.Evans L A, McHugh T M, Stites D P, Levy J A. Differential ability of human immunodeficiency virus isolates to productively infect human cells. J Immunol. 1987;138:3415–3418. [PubMed] [Google Scholar]
- 25.Fauci A S. Host factors and the pathogenesis of HIV-induced disease. Nature. 1996;384:529–534. doi: 10.1038/384529a0. [DOI] [PubMed] [Google Scholar]
- 26.Gorny M K, Xu J Y, Gianakakos V, Karwowska S, Williams C, Sheppard H W, Hanson C V, Zolla-Pazner S. Production of site-selected neutralizing human monoclonal antibodies against the third variable domain of the human immunodeficiency virus type 1 envelope glycoprotein. Proc Natl Acad Sci USA. 1991;88:3238–3242. doi: 10.1073/pnas.88.8.3238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Groenink M, Fouchier R A, Broersen S, Baker C H, Koot M, van’t Wout A B, Huisman H G, Miedema F, Tersmette M, Schuitemaker H. Relation of phenotype evolution of HIV-1 to envelope V2 configuration. Science. 1993;260:1513–1516. doi: 10.1126/science.8502996. . (Comment, 268:115, 1995.) [DOI] [PubMed] [Google Scholar]
- 28.Harbol A W, Liesveld J L, Simpson-Haidaris P J, Abboud C N. Mechanisms of cytopenia in human immunodeficiency virus infection. Blood Rev. 1994;8:241–251. doi: 10.1016/0268-960x(94)90112-0. [DOI] [PubMed] [Google Scholar]
- 29.Harnly M E, Swan S H, Holly E A, Kelter A, Padian N. Temporal trends in the incidence of non-Hodgkin’s lymphoma and selected malignancies in a population with a high incidence of acquired immunodeficiency syndrome (AIDS) Am J Epidemiol. 1988;128:261–267. doi: 10.1093/oxfordjournals.aje.a114966. . (Comment, 130:1069–1071, 1989.) [DOI] [PubMed] [Google Scholar]
- 30.Higgins D G, Bleasby A J, Fuchs R. CLUSTAL V: improved software for multiple sequence alignment. Comput Appl Biosci. 1992;8:189–191. doi: 10.1093/bioinformatics/8.2.189. [DOI] [PubMed] [Google Scholar]
- 31.Higgins D G, Sharp P M. CLUSTAL: a package for performing multiple sequence alignment on a microcomputer. Gene. 1988;73:237–244. doi: 10.1016/0378-1119(88)90330-7. [DOI] [PubMed] [Google Scholar]
- 32.Hwang S S, Boyle T J, Lyerly H K, Cullen B R. Identification of the envelope V3 loop as the primary determinant of cell tropism in HIV-1. Science. 1991;253:71–74. doi: 10.1126/science.1905842. [DOI] [PubMed] [Google Scholar]
- 33.Ichimura H, Kliks S C, Visrutaratna S, Ou C Y, Kalish M L, Levy J A. Biological, serological, and genetic characterization of HIV-1 subtype E isolates from northern Thailand. AIDS Res Hum Retroviruses. 1994;10:263–269. doi: 10.1089/aid.1994.10.263. [DOI] [PubMed] [Google Scholar]
- 34.Jolly P E. Replicative characteristics of primary isolates of the human immunodeficiency virus type 1 in peripheral blood mononuclear cells, primary macrophages and CD4+ transformed T-cell lines. Cell Mol Biol. 1997;43:1057–1065. [PubMed] [Google Scholar]
- 35.Kuiken C L, de Jong J-J, Baan E, Keulen W, Tersmette M, Goudsmit J. Evolution of the V3 envelope domain in proviral sequences and isolates of human immunodeficiency virus type 1 during transition of the viral biological phenotype. J Virol. 1992;66:4622–4627. doi: 10.1128/jvi.66.7.4622-4627.1992. . (Erratum, 66:5704.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kunzi M S, Groopman J E. Identification of a novel human immunodeficiency virus strain cytopathic to megakaryocytic cells. Blood. 1993;81:3336–3342. [PubMed] [Google Scholar]
- 37.Lichtman M A. The ultrastructure of the hemopoietic environment of the marrow: a review. Exp Hematol. 1981;9:391–410. [PubMed] [Google Scholar]
- 38.Louache F, Bettaieb A, Henri A, Oksenhendler E, Farcet J P, Bierling P, Seligmann M, Vainchenker W. Infection of megakaryocytes by human immunodeficiency virus in seropositive patients with immune thrombocytopenic purpura. Blood. 1991;78:1697–1705. [PubMed] [Google Scholar]
- 39.Louache F, Henri A, Bettaieb A, Oksenhendler E, Raguin G, Tulliez M, Vainchenker W. Role of human immunodeficiency virus replication in defective in vitro growth of hematopoietic progenitors. Blood. 1992;80:2991–2999. [PubMed] [Google Scholar]
- 40.Lyman S D, Jacobsen S E. c-kit ligand and Flt3 ligand: stem/progenitor cell factors with overlapping yet distinct activities. Blood. 1998;91:1101–1134. [PubMed] [Google Scholar]
- 41.Maciejewski J P, Bruening E E, Donahue R E, Mocarski E S, Young N S, St. Jeor S C. Infection of hematopoietic progenitor cells by human cytomegalovirus. Blood. 1992;80:170–178. [PubMed] [Google Scholar]
- 42.Maciejewski J P, Weichold F F, Young N S. HIV-1 suppression of hematopoiesis in vitro mediated by envelope glycoprotein and TNF-α. J Immunol. 1994;153:4303–4310. [PubMed] [Google Scholar]
- 43.Miles S A, Mitsuyasu R T, Moreno J, Baldwin G, Alton N K, Souza L, Glaspy J A. Combined therapy with recombinant granulocyte colony-stimulating factor and erythropoietin decreases hematologic toxicity from zidovudine. Blood. 1991;77:2109–2117. [PubMed] [Google Scholar]
- 44.Milich L, Margolin B, Swanstrom R. V3 loop of the human immunodeficiency virus type 1 Env protein: interpreting sequence variability. J Virol. 1993;67:5623–5634. doi: 10.1128/jvi.67.9.5623-5634.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Milich L, Margolin B H, Swanstrom R. Patterns of amino acid variability in NSI-like V3 sequences and a linked change in the CD4-binding domain of the HIV-1 env protein. Virology. 1997;239:108–118. doi: 10.1006/viro.1997.8821. [DOI] [PubMed] [Google Scholar]
- 46.Mohle R, Green D, Moore M A, Nachman R L, Rafii S. Constitutive production and thrombin-induced release of vascular endothelial growth factor by human megakaryocytes and platelets. Proc Natl Acad Sci USA. 1997;94:663–668. doi: 10.1073/pnas.94.2.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Monte D, Groux H, Raharinivo B, Plouvier B, Dewulf J, Clavel T, Grangette C, Torpier G, Auriault C, Capron A, et al. Productive human immunodeficiency virus-1 infection of megakaryocytic cells is enhanced by tumor necrosis factor-alpha. Blood. 1992;79:2670–2679. [PubMed] [Google Scholar]
- 48.Moses A V, Williams S, Heneveld M L, Strussenberg J, Rarick M, Loveless M, Bagby G, Nelson J A. Human immunodeficiency virus infection of bone marrow endothelium reduces induction of stromal hematopoietic growth factors. Blood. 1996;87:919–925. . (Comment, 88:1897–1898, 1996.) [PubMed] [Google Scholar]
- 49.Oksenhendler E, Bierling P, Ferchal F, Clauvel J P, Seligmann M. Zidovudine for thrombocytopenic purpura related to human immunodeficiency virus (HIV) infection. Ann Intern Med. 1989;110:365–368. doi: 10.7326/0003-4819-110-5-365. [DOI] [PubMed] [Google Scholar]
- 50.Orkin S H. Hematopoiesis: how does it happen? Curr Opin Cell Biol. 1995;7:870–877. doi: 10.1016/0955-0674(95)80072-7. [DOI] [PubMed] [Google Scholar]
- 51.Poss M, Martin H L, Kreiss J K, Granville L, Chohan B, Nyange P, Mandaliya K, Overbaugh J. Diversity in virus populations from genital secretions and peripheral blood from women recently infected with human immunodeficiency virus type 1. J Virol. 1995;69:8118–8122. doi: 10.1128/jvi.69.12.8118-8122.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rafii S, Shapiro F, Pettengell R, Ferris B, Nachman R L, Moore M A, Asch A S. Human bone marrow microvascular endothelial cells support long-term proliferation and differentiation of myeloid and megakaryocytic progenitors. Blood. 1995;86:3353–3363. [PubMed] [Google Scholar]
- 53.Rusche J R, Javaherian K, McDanal C, Petro J, Lynn D L, Grimaila R, Langlois A, Gallo R C, Arthur L O, Fischinger P J, et al. Antibodies that inhibit fusion of human immunodeficiency virus-infected cells bind a 24-amino acid sequence of the viral envelope, gp120. Proc Natl Acad Sci USA. 1988;85:3198–3202. doi: 10.1073/pnas.85.9.3198. . (Errata, 85:8697, 1988, and 86:1667, 1989.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Saitou N, Nei M. The neighbor-joining method: a new method for reconstructing phylogenetic trees. Mol Biol Evol. 1987;4:406–425. doi: 10.1093/oxfordjournals.molbev.a040454. [DOI] [PubMed] [Google Scholar]
- 55.Schuitemaker H, Kootstra N A, de Goede R E Y, de Wolf F, Miedema F, Tersmette M. Monocytotropic human immunodeficiency virus type 1 (HIV-1) variants detectable in all stages of HIV-1 infection lack T-cell line tropism and syncytium-inducing ability in primary T-cell culture. J Virol. 1991;65:356–363. doi: 10.1128/jvi.65.1.356-363.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Speck R F, Wehrly K, Platt E J, Atchison R E, Charo I F, Kabat D, Chesebro B, Goldsmith M A. Selective employment of chemokine receptors as human immunodeficiency virus type 1 coreceptors determined by individual amino acids within the envelope V3 loop. J Virol. 1997;71:7136–7139. doi: 10.1128/jvi.71.9.7136-7139.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stanley S K, Kessler S W, Justement J S, Schnittman S M, Greenhouse J J, Brown C C, Musongela L, Musey K, Kapita B, Fauci A S. CD34+ bone marrow cells are infected with HIV in a subset of seropositive individuals. J Immunol. 1992;149:689–697. [PubMed] [Google Scholar]
- 58.Steinberg H N, Crumpacker C S, Chatis P A. In vitro suppression of normal human bone marrow progenitor cells by human immunodeficiency virus. J Virol. 1991;65:1765–1769. doi: 10.1128/jvi.65.4.1765-1769.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Strizki J M, Albright A V, Sheng H, O’Connor M, Perrin L, González-Scarano F. Infection of primary human microglia and monocyte-derived macrophages with human immunodeficiency virus type 1 isolates: evidence of differential tropism. J Virol. 1996;70:7654–7662. doi: 10.1128/jvi.70.11.7654-7662.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tamalet C, Lafeuillade A, Yahi N, Vignoli C, Tourres C, Pellegrino P, de Micco P. Comparison of viral burden and phenotype of HIV-1 isolates from lymph nodes and blood. AIDS. 1994;8:1083–1088. doi: 10.1097/00002030-199408000-00007. [DOI] [PubMed] [Google Scholar]
- 61.Tavassoli M, Friedenstein A. Hemopoietic stromal microenvironment. Am J Hematol. 1983;15:195–203. doi: 10.1002/ajh.2830150211. [DOI] [PubMed] [Google Scholar]
- 62.Tersmette M, de Goede R E Y, Al B J M, Winkel I N, Gruters R A, Cuypers H T, Huisman H G, Miedema F. Differential syncytium-inducing capacity of human immunodeficiency virus isolates: frequent detection of syncytium-inducing isolates in patients with acquired immunodeficiency syndrome (AIDS) and AIDS-related complex. J Virol. 1988;62:2026–2032. doi: 10.1128/jvi.62.6.2026-2032.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tersmette M, Gruters R A, de Wolf F, de Goede R E Y, Lange J M A, Schellekens P T A, Goudsmit J, Huisman H G, Miedema F. Evidence for a role of virulent human immunodeficiency virus (HIV) variants in the pathogenesis of acquired immunodeficiency syndrome: studies on sequential HIV isolates. J Virol. 1989;63:2118–2125. doi: 10.1128/jvi.63.5.2118-2125.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Travis B M, Dykers T I, Hewgill D, Ledbetter J, Tsu T T, Hu S L, Lewis J B. Functional roles of the V3 hypervariable region of HIV-1 gp160 in the processing of gp160 and in the formation of syncytia in CD4+ cells. Virology. 1992;186:313–317. doi: 10.1016/0042-6822(92)90088-7. [DOI] [PubMed] [Google Scholar]
- 65.van’t Wout A B, Blaak H, Ran L J, Brouwer M, Kuiken C, Schuitemaker H. Evolution of syncytium-inducing and non-syncytium-inducing biological virus clones in relation to replication kinetics during the course of human immunodeficiency virus type 1 infection. J Virol. 1998;72:5099–5107. doi: 10.1128/jvi.72.6.5099-5107.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.van’t Wout A B, Ran L J, Kuiken C L, Kootstra N A, Pals S T, Schuitemaker H. Analysis of the temporal relationship between human immunodeficiency virus type 1 quasispecies in sequential blood samples and various organs obtained at autopsy. J Virol. 1998;72:488–496. doi: 10.1128/jvi.72.1.488-496.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wachinger M, Saermark T, Erfle V. Influence of amphipathic peptides on HIV-1 production in persistently infected T lymphoma cells. FEBS Lett. 1992;309:235–241. doi: 10.1016/0014-5793(92)80780-k. [DOI] [PubMed] [Google Scholar]
- 68.Westervelt P, Gendelman H E, Ratner L. Identification of a determinant within the human immunodeficiency virus type 1 surface envelope glycoprotein critical for productive infection of primary monocytes. Proc Natl Acad Sci USA. 1991;88:3097–3101. doi: 10.1073/pnas.88.8.3097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Westervelt P, Trowbridge D B, Epstein L G, Blumberg B M, Li Y, Hahn B H, Shaw G M, Price R W, Ratner L. Macrophage tropism determinants of human immunodeficiency virus type 1 in vivo. J Virol. 1992;66:2577–2582. doi: 10.1128/jvi.66.4.2577-2582.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wickenhauser C, Lorenzen J, Thiele J, Hillienhof A, Jungheim K, Schmitz B, Hansmann M L, Fischer R. Secretion of cytokines (interleukins-1α, -3, and -6 and granulocyte-macrophage colony-stimulating factor) by normal human bone marrow megakaryocytes. Blood. 1995;85:685–691. [PubMed] [Google Scholar]
- 71.Zauli G, Re M C, Davis B, Sen L, Visani G, Gugliotta L, Furlini G, La Placa M. Impaired in vitro growth of purified (CD34+) hematopoietic progenitors in human immunodeficiency virus-1 seropositive thrombocytopenic individuals. Blood. 1992;79:2680–2687. [PubMed] [Google Scholar]
- 72.Zauli G, Re M C, Gugliotta L, Visani G, Vianelli N, Furlini G, La Placa M. Lack of compensatory megakaryocytopoiesis in HIV-1-seropositive thrombocytopenic individuals compared with immune thrombocytopenic purpura patients. AIDS. 1991;5:1345–1350. doi: 10.1097/00002030-199111000-00010. [DOI] [PubMed] [Google Scholar]
- 73.Zauli G, Re M C, Visani G, Furlini G, La Placa M. Inhibitory effect of HIV-1 envelope glycoproteins gp120 and gp160 on the in vitro growth of enriched (CD34+) hematopoietic progenitor cells. Arch Virol. 1992;122:271–280. doi: 10.1007/BF01317189. [DOI] [PubMed] [Google Scholar]
- 74.Zauli G, Re M C, Visani G, Furlini G, Mazza P, Vignoli M, La Placa M. Evidence for a human immunodeficiency virus type 1-mediated suppression of uninfected hematopoietic (CD34+) cells in AIDS patients. J Infect Dis. 1992;166:710–716. doi: 10.1093/infdis/166.4.710. [DOI] [PubMed] [Google Scholar]
- 75.Zauli G, Vitale M, Gibellini D, Capitani S. Inhibition of purified CD34+ hematopoietic progenitor cells by human immunodeficiency virus 1 or gp120 mediated by endogenous transforming growth factor β1. J Exp Med. 1996;183:99–108. doi: 10.1084/jem.183.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zucker-Franklin D, Cao Y Z. Megakaryocytes of human immunodeficiency virus-infected individuals express viral RNA. Proc Natl Acad Sci USA. 1989;86:5595–5599. doi: 10.1073/pnas.86.14.5595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zucker-Franklin D, Termin C S, Cooper M C. Structural changes in the megakaryocytes of patients infected with the human immune deficiency virus (HIV-1) Am J Pathol. 1989;134:1295–1303. [PMC free article] [PubMed] [Google Scholar]