Abstract
Congenital epulis is a rare benign soft tissue lesion that occurs exclusively in neonates and usually develops from the alveolar mucosa at the frontal region of the maxilla. Lesions may be sessile or pedunculated, normal in color or reddish and vary in size from a few millimeters to a few centimeters. Although spontaneous regression has also been reported, surgical excision is indicated for large tumors that may obstruct the airway and make feeding the child difficult. In this case report, we present a rare case of congenital epulis involving the right side of the maxillary alveolar mucosa in a neonate delivered vaginally at Dhulikhel Hospital, Kavreplanchok, Nepal. The lesion was surgically removed by electrocautery, and histologic examination confirmed the clinical diagnosis of congenital epulis. No complications occurred after surgery, and when the child was examined 6 months later, no evidence of recurrence noticed.
Keywords: congenital epulis, neonates, maxillary alveolar mucosa, infant, Dhulikhel Hospital
INTRODUCTION
Congenital epulis is a rare benign soft tissue tumor that usually appears on the newborn’s anterior alveolar mucosa of the maxillary arch. The evidence of description about congenital epulis was recognized in the literature in 1871 by a German doctor, Dr Franz Ernst Christian Neumann, so it is also called as Neumann’s tumor. Other terminologies used to describe this tumor in the literature include congenital granular cell epulis, congenital granular cell lesion, congenital epulis of the infant, gingival granular cell tumor of the newborn, congenital granular cell myoblastoma and granular cell fibroblastoma [1]. This tumor has an extremely low incidence of roughly 0.0006%, and <250 cases have been described in the literature so far, with only two cases reported in Nepal [1–3].
Clinically, the tumor present as pedunculated or sessile mass protruding through the oral cavity of a newborn child and usually present as a single lesion; however, multiple lesions have been reported in 10% of cases [4]. The tumor has a higher female predominance than male (8:1) and ranges in size from a few millimeters to cm, with the largest size reported to date being 9 cm [4]. Though the tumor is benign and spontaneous regression has also been reported, surgical excision of tumor is usually recommended as it can interfere with newborn’s feeding and respiration with marked psychological impact on parent. No recurrence rate has been reported till date even after incomplete excision of tumor [3]. In this case report, we present a 2-day old newborn female patient who had a projecting mass from her mouth and was having trouble in breast feeding. The mass was surgically excised and was histologically identified as congenital epulis.
CASE REPORT
A 2-day old female patient delivered vaginally at Kathmandu University Dhulikhel Hospital referred to oral and maxillofacial surgery department with chief complain of difficulty in breast feeding because of protruding mass from the patient’s mouth. On examination there was presence of pedunculated pink colored fleshy mass of size ~2.5 cm / 2 cm protruding thorough patient’s oral cavity with base attached to the right-sided anterior alveolar region (Fig. 1). Based on clinical presentation, congenital epulis was made as provisional diagnosis. As the size of the mass was large and interfering with breast feeding, patient’s parent was counseled regarding surgical excision of the lesion. Routine preoperative investigations were sent, pediatric evaluation was also done and they suggest no other association of congenital anomalies followed by anesthesiology consultation. On the fifth day, the patient underwent excision of tumor mass using electrocautery (Fig. 2) under general anesthesia with intraoral intubation. Intraoperatively no bleeding was evident. The excised mass (Fig. 3) was sent for histopathological examination (Fig. 6), which shows presence of sheets of polygonal cells with eosinophilic granular cytoplasm with eccentrically placed nuclei with interspersed collagen fibers (HE stains, X10) suggestive of congenital epulis. Postoperatively, wound (Fig. 4) was cleaned gently with moist cotton every day and breast feeding was started the next day after surgery. Baby was discharged on the fourth postoperative day and kept on regular follow-up. The wound healed by secondary intension (Fig. 5) and was satisfactory and showed no signs of any recurrence after 6 months of follow up.
Figure 1.

Preoperative clinical photograph showing epulis mass protruding through oral cavity.
Figure 2.

Intraoperative clinical photograph showing electrocauterization of epulis mass.
Figure 3.

Excised epulis mass.
Figure 6.
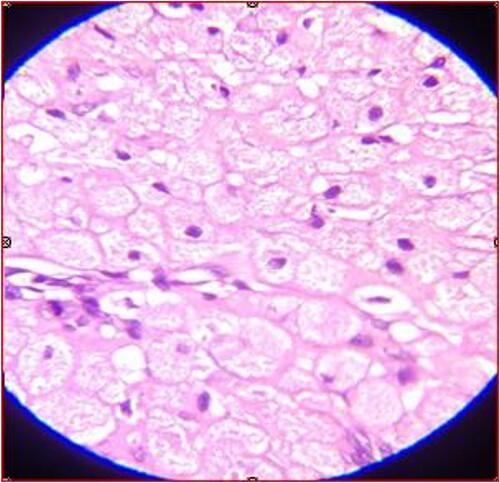
Microscopic feature of the tumor showing sheets of polygonal cells with eosinophilic granular cytoplasm (HE stains, X10).
Figure 4.

Third postoperative clinical photograph.
Figure 5.

Sixth month postoperative clinical photograph.
DISCUSSION
Congenital epulis is most commonly seen in neonates, with a mass developing from the gingiva and spreading over the maxillary alveolar ridge, generally near the lateral incisors or canines [5]. The term epulis, which means ‘on the gums’ or ‘gum boil’ in Greek, is derived from the word [3]. Other locations of this tumor have been documented, including the mandibular gingiva and tongue, as well as many locations at the same time [6]. It is estimated to be twice as common on the maxilla as it is on the mandible [7]. Many theories such as myoblastic, odontogenic, neurogenic, fibroblastic, histiocytic, endocrinologic or basically reactive factors has been suggested as the possible etiology of congenital epulis [6]. Though the lesion shows female predilection, no direct association with specific hormones has been identified, since endogenous hormone receptors have not been found in the lesions [8]. Melanotic neuroectodermal tumor of infancy (MNTI), hemangioma, fibroma, embryonal rhabdomyosarcoma, granuloma, malignant granular cell myoblastoma, chondrogenic and osteogenic sarcoma and schwannoma are all possible differential diagnosis for congenital epulis [9]. Published reports suggest that, this lesion has also been diagnosed prenatally, which helps parents mentally prepare for the postnatal circumstances [3]. Sadly, no prenatal diagnosis was performed in this case.
Although spontaneous regression has been described, large lesions interfering with feeding and respiration require immediate surgical excision, whereas small lesions can be watched for spontaneous remission. There have been no reports of lesion recurrence or malignant change to yet [8]. In such circumstances, electrocautery under general anesthesia is generally advised [10]. For smaller lesions or where intubation is impossible, excision under local anesthetic can be an alternative technique of treatment [10]. This lesion has a very good postoperative prognosis, and spontaneous regression may occur despite inadequate excision [8].
Though congenital epulis is a benign tumor that is uncommon, clinicians must be well-versed in its management in order to limit aggressive treatment and assist parents in dealing with the situation appropriately.
Contributor Information
Dilip Rauniyar, Department of Oral and Maxillofacial Surgery, Kathmandu University School of Medical Sciences, Dhulikhel 45210, Nepal.
Chandan Upadhyaya, Department of Oral and Maxillofacial Surgery, Kathmandu University School of Medical Sciences, Dhulikhel 45210, Nepal.
Nitesh Chaurasia, Department of Oral and Maxillofacial Surgery, Kathmandu University School of Medical Sciences, Dhulikhel 45210, Nepal.
Siddhartha Sharma, Department of Oral and Maxillofacial Surgery, Kathmandu University School of Medical Sciences, Dhulikhel 45210, Nepal.
Anima Bhandari, Department of Oral and Maxillofacial Surgery, Kathmandu University School of Medical Sciences, Dhulikhel 45210, Nepal.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
DATA AVAILABILITY
Data included in this article are obtained from articles published online.
References
- 1. Agarwal M. Congenital granular cell tumor in an infant: a case report. Annals of Woman and Child Health 2016;2:C9–12. [Google Scholar]
- 2. Singh A, Ghosh S, Yadav AK, Panthee A. Congenital granular cell tumor: report of a case with literature review and differential diagnosis. Clin Case Rep 2022;10:e05580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sigdel B, Baidya R, Shrestha P, Shrestha S. Congenital granular cell epulis: a rare diagnosis. J Pathol Nepal 1970;1:69–72. [Google Scholar]
- 4. Bosanquet D, Roblin G. Congenital epulis: a case report and estimation of incidence. Int J Otolaryngol 2009;2009:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ritwik P, Brannon RB, Musselman RJ. Spontaneous regression of congenital epulis: a case report and review of the literature. J Med Case Reports 2010;4:331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Merglova V, Mukensnabl P, Andrle P. Congenital epulis. Case Rep 2012;2012:bcr0120125483–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Yuwanati M, Mhaske S, Mhaske A. Congenital granular cell tumor – a rare entity. J Neonatal Surg 2015;4:17. [PMC free article] [PubMed] [Google Scholar]
- 8. Kang MJ, Kang SH. Congenital epulis in a newborn. J Korean Assoc Oral Maxillofac Surg 2022;48:382–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kumar R, Jaiswal S, Singhal A, Garg R. Congenital granular cell lesion: a rare tumor of new born. J Oral Maxillofac Pathol 2013;17:440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Silva GCC, Vieira TC, Vieira JC, Martins CR, Carvalho E. Congenital granular cell tumor (congenital epulis): a lesion of multidisciplinary interest. Med Oral Patol Oral Cir Bucal 2007;12:E428–30. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data included in this article are obtained from articles published online.


