Dear Editor
We have read with interest the article by Michela Lai et al entitled “Cutaneous squamous cell carcinoma in patients with chronic lymphocytic leukemia: a systematic review of the literature” [1].
Cutaneous squamous cell carcinoma (cSCC) is the second most common malignant neoplasm of the skin. Immunosuppressed patients can develop cSCC more frequently than average population, and these cancers seem to behave more aggressively with a lower degree of differentiation [2]. Naturally, hematologic patients have an immunosuppressed status due to their disease and to its treatment.
Immunotherapy (IT) is assuming an important role in the treatment of cSCC: cemiplimab, an inhibitor of Programmed Death receptor-1 (PD-1) has been approved for patients affected by cSCC, not eligible to curative surgery and radiotherapy. However, the use of immunotherapy in hematologic patients with cSCC is still under study, for this population is often excluded from clinical trials [3].
Herein we present the case of a hematologic patient affected by cSCC treated with cemiplimab.
A 73-year-old man showed a painful, ulcerated firm nodule of the lower left hemilip (Figure 1A) and a nodular ulcerated lesion in the submental region (Figure 1B). The patient also complained about remarkable fatigue. He has been suffering from myelodysplastic syndrome (MDS) for around two years. A diagnosis of a type 2 Refractory Anemia with Excess of Blasts (RAEB-2) was made after bone marrow aspiration (2016 WHO classification). The patient was under treatment with systemic antibiotics and 5-azacytidine.
Figure 1.
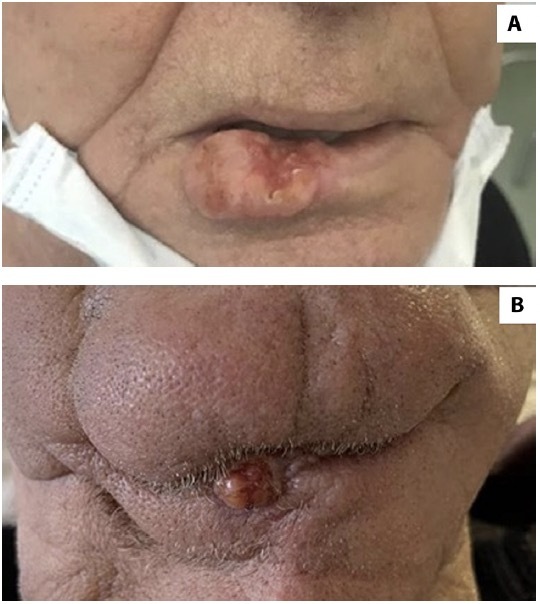
(A) Lower left hemilip lesion before excisional biopsy. (B) Submental lesion.
Excisional (free margins) skin biopsy of the labial lesion revealed a G3 cSCC, with skeletal muscle and bone invasion (pT3 according to AJCC staging system). No biopsy was performed for the ulcerated lesion of the submental region. The patient underwent a positron emission computed tomography (PET/CT) with 18-fluorodeoxyglucose that showed two areas of pathologic tracer uptake in the lower left hemilip, extended to the jaw, and in the submental region. In addition, the exam documented mildly increased tracer uptake in the humeral and femoral diaphyses, referable to the MDS, and some pathologic cervical adenopathies.
Thus, the patient started treatment with cemiplimab, 350 mg every three weeks. After five administrations, marked clinical improvement of the submental region was observed (Figure 2) while there was no local relapse in the labial region. Moreover, the patient reported notable pain and fatigue reduction.
Figure 2.

Submental region after cemiplimab treatment.
Results of laboratory tests performed before starting cemiplimab and after 15 weeks of therapy are reported in Table 1.
Table 1.
Results of laboratory tests performed before starting cemiplimab (W0) and after 15 weeks (W15) of therapy.
| W0 | W15 | |
|---|---|---|
| Hemoglobin | 8.6 g/dl | 10.7 g/dl |
| Neutrophils | 0.4 x103/μl | 0.5 x103/μl |
| Lymphocytes | 0.2 x103/μl | 0.7 x103/μl. |
| Platelets | 50 x103/μl | 74 x 103/μl |
The PD-1/PD-L1 axis is involved in the pathogenesis of many hematological malignancies. For this reason, anti-PD1 drugs might have a promising role for their treatment. In chronic lymphocytic leukemia (CLL), PD-1 is expressed on CD4+ and CD8+ T cells, and proliferation of these cells is associated with a negative prognosis. In fact, patients with advanced CLL stage have an increased number of PD1+ CD4+ T cells in the peripheral blood. PD-1 blockade has also shown a significant benefit in CLL patients with Richter syndrome [3].
Concerning MDS pathogenesis, pathological medullary progenitor cells (CD34+), show an increased expression of checkpoint molecules, including PD1, which interfere with an effective T-cell-receptor (TCR) signaling and correct presentation of the antigens to T-lymphocytes. Because of this, the use of immunotherapy is suggested in association with demethylating agents, such as azacytidine [4]. These agents increase the expression of molecules such as cancer/testis antigens, which are highly immunogenic. This synergistic effect might elicit an increased immune response against the pathologically altered bone marrow progenitor cells of MDS. Phase 2 trials regarding the association of demethylating agents with various types of immunotherapies, including nivolumab (an anti-PD-1) are ongoing, and preliminary results seem promising [5].
In our case, cemiplimab was successful for cSCC treatment, as expected. Moreover, we suppose that cemiplimab in combination with 5-azacytidine improved MDS control.
Footnotes
Funding: None.
Competing Interests: None.
Authorship: All authors have contributed significantly to this publication.
References
- 1.Lai M, Pampena R, Cornacchia L, et al. Cutaneous squamous cell carcinoma in patients with chronic lymphocytic leukemia: a systematic review of the literature. Int J Dermatol. 2022;61(5):548–557. doi: 10.1111/ijd.15813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tam S, Yao CMKL, Amit M, et al. Association of Immunosuppression With Outcomes of Patients With Cutaneous Squamous Cell Carcinoma of the Head and Neck. JAMA Otolaryngol Head Neck Surg. 2020;146(2):128–135. doi: 10.1001/jamaoto.2019.3751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ding W, LaPlant BR, Call TG, et al. Pembrolizumab in patients with CLL and Richter transformation or with relapsed CLL. Blood. 2017;129(26):3419–3427. doi: 10.1182/blood-2017-02-765685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wong KK, Hassan R, Yaacob NS. Hypomethylating Agents and Immunotherapy: Therapeutic Synergism in Acute Myeloid Leukemia and Myelodysplastic Syndromes. Front Oncol. 2021 Feb 25;11:624742. doi: 10.3389/fonc.2021.624742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jelinek T, Mihalyova J, Kascak M, Duras J, Hajek R. PD-1/PD-L1 inhibitors in haematological malignancies: update 2017. Immunology. 2017;152(3):357–371. doi: 10.1111/imm.12788. [DOI] [PMC free article] [PubMed] [Google Scholar]


