Abstract
Background and Aims
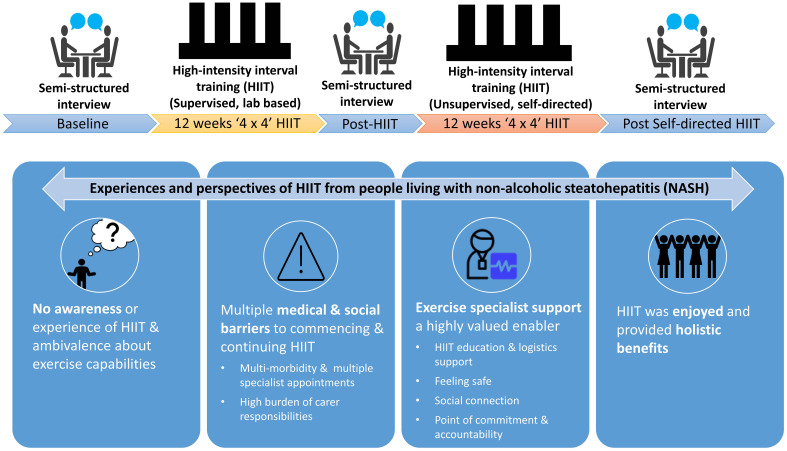
High-intensity interval training (HIIT) is a therapeutic option for people with nonalcoholic steatohepatitis (NASH). However, the perspectives and experiences of HIIT for people with NASH are unknown, limiting translation of research. We explored the experiences and perspectives of both professionally supervised and self-directed HIIT in people with NASH and evaluated participant-reported knowledge, barriers, and enablers to commencing and sustaining HIIT.
Methods
Twelve participants with NASH underwent 12 weeks of supervised HIIT (3 days/week, 4×4 minutes at 85–95% maximal heart rate, interspersed with 3 minutes active recovery), followed by 12-weeks of self-directed (unsupervised) HIIT. One-on-one, semistructured participant interviews were conducted by exercise staff prior to HIIT and following both supervised and self-directed HIIT to explore prior knowledge, barriers, enablers, and outcomes at each stage. Interviews were audio-recorded, transcribed, coded, and thematically analyzed by two independent researchers.
Results
Four dominant themes were identified: (1) no awareness of/experience with HIIT and ambivalence about exercise capabilities; (2) multiple medical and social barriers to commencing and continuing HIIT; (3) exercise specialist support was a highly valued enabler, and (4) HIIT was enjoyed and provided holistic benefits.
Conclusions
People with NASH may lack knowledge of and confidence for HIIT, and experience multiple complex barriers to commencing and continuing HIIT. Exercise specialist support is a key enabler to sustained engagement. These factors need to be addressed in future clinical programs to augment the uptake and long-term sustainability of HIIT by people with NASH so they can experience the range of related benefits.
Keywords: Nonalcoholic fatty liver disease, NAFLD, Exercise, Lifestyle, Qualitative, Patient-reported outcomes
Graphical abstract
Introduction
Non-alcoholic steatohepatitis (NASH) is a progressive form of nonalcoholic fatty liver disease (NAFLD), characterized by hepatic steatosis, hepatocyte injury, inflammation, and varying degrees of liver fibrosis. NASH affects ∼6% of the worldwide population and up to 30% of people with obesity.1,2 NASH is a burgeoning indication for liver transplantation3 with up to 20% of people with NAFLD progressing to NASH.2 With no approved pharmaceutical therapies, lifestyle modification including exercise and diet remains the frontline approach for the management of NAFLD, including those with NASH.4
While there is no targeted exercise prescription for NASH, general recommendations for NAFLD promote 150–200 minutes of moderate intensity exercise per week.4,5 However, most people with NAFLD are not physically active, with only ∼20% meeting physical activity recommendations.6,7 There is a growing interest in the role of physical activity performed at, or above, a vigorous intensity for the treatment of NASH, as emerging evidence suggests it is effective in other chronic disease populations,8–10 and population studies have shown an inverse association with severe fibrosis.6 High-intensity interval training (HIIT) involves single or repeated bouts of high-intensity exercise interspersed with periods of active or passive recovery. In NAFLD, HIIT has shown comparable reductions in hepatic steatosis to traditional moderate intensity continuous training.11 While evidence is limited to small studies with a wide range of training prescriptions, HIIT can improve diastolic function,12 hepatic stiffness13 and several metabolic pathways central to the pathogenesis of NASH.13,14
Owing to its vigorous nature, the safety of HIIT in clinical populations is often questioned. We and other researchers have previously demonstrated the safety of HIIT across a range of clinical patients including those with common comorbidities of NASH such as metabolic syndrome, hypertension, and musculoskeletal conditions.8,10,20,21 Clinical guidelines for the safe delivery and monitoring of HIIT in people with chronic disease22 emphasize the importance of medical screening, cardiopulmonary evaluation to inform programming, modest workload progression, and regular monitoring to identify any changes to medical status or medication that may preclude HIIT participation or affect heart rate response. It was recently shown that supervised HIIT (4×4 min at 85–95% maximal heart rate interspersed with 3 min lower intensity active recovery, three sessions per week for 12 weeks) was safe and feasible for people with NASH,23 and related chronic diseases such as metabolic syndrome and coronary heart disease,10,21,22 when adequately screened and monitored. To complement this research, and in line with the 2022 global public health agenda for NAFLD,24 it is important to also understand individual patients’ perceptions and experiences of HIIT.
There are established physiological mechanisms25–27 and comorbidities such as increased fatigue, heightened pain, musculoskeletal conditions and low mood28,29 which may predispose clinicians to assume that people with NASH would have low tolerance for vigorous exercise and low motivation. Most studies of exercise in NAFLD and NASH show poor maintenance of exercise by 6–12 months,15,16 and there is a paucity of data investigating patient factors that impact the sustainability of transitioning HIIT from supervised settings to self-directed.17–19 An understanding of people’s knowledge of HIIT, and perceived barriers and enablers to commencing and sustaining vigorous exercise, in both supervised and self-directed contexts is needed to inform the design and dissemination of acceptable and sustainable HIIT programs for people with NASH. Therefore, the aim of this study was to explore the experiences and perspectives of both professionally supervised and self-directed HIIT in people with NASH. We also evaluated participant knowledge, barriers, and enablers of commencing and sustaining HIIT.
Methods
Study design and setting
This qualitative study was designed and reported in accordance with the consolidated criteria for reporting qualitative research (COREQ) checklist.30 The evaluation was nested within a larger randomized controlled trial investigating the safety, feasibility, and efficacy of a 12-week supervised HIIT intervention for improving cardiometabolic health in people with NASH (Australia and New Zealand Clinical Trials Registry: ACTRN12616000305426). All procedures were in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments, and approved by the Metro South Hospital and Health Service’s Human Research Ethics Committee (HREC/15/QPAH/747) and The University of Queensland Human Research Ethics Committee (2016000010).
Participants were randomized into either HIIT exercise or control groups. Participants in the HIIT exercise group completed 12 weeks of supervised HIIT, followed by 12 weeks of self-directed (unsupervised) HIIT. Participants in the control group undertook 12 weeks of an attention control exercise program involving gentle stretching exercises designed to not elicit cardiometabolic benefit but still provide a social and participatory interaction similar to the HIIT exercise group. On completion, control group participants undertook 12 weeks of supervised HIIT followed by 12 weeks of self-directed (unsupervised) HIIT. Participants in the overarching trial were provided detailed information about the current qualitative study as part of consenting to the broader study. Written informed consent was obtained from all participants prior to commencing the study.
Participants
Participants were recruited from a specialist hepatology outpatient clinic within a metropolitan public hospital and health service and were eligible for inclusion if they were adults 18–70 years of age, did not meet physical activity guidelines (undertook <150 minutes of moderate or <75 minutes of vigorous aerobic exercise per week or an equivalent combination of moderate-vigorous activity, and had NASH confirmed by liver biopsy. The exclusion criteria have been reported elsewhere (ANZCTR: ACTRN12616000305426) and included significant cardiac disease, hazardous alcohol use, and/or contraindications to exercise testing or training. To ensure safety in the parent study, participants were medically evaluated and screened by a cardiopulmonary exercise test with 12-lead electrocardiography under medical supervision. Referral to the study was provided by their treating physician, and therefore medical clearance to participate was provided prior to inclusion. All participants were consecutively invited to this qualitative study. Participants who did not complete the overarching study were still invited to return for an interview.
HIIT intervention
The supervised HIIT intervention consisted of four bouts of 4 minutes of high-intensity exercise intervals (85–95% heart rate maximum, HRmax) corresponding to a rating of perceived exertion (RPE) of 15–18 on the Borg 6–20 scale31 (license #5RYHYG), interspersed with 3 min recovery intervals (50–60% HRmax; RPE 11–13). This protocol was selected as the majority of evidence demonstrating the safety of HIIT in clinical populations have used this method.9,22,32 The prescription and monitoring of HIIT aligned with guidelines for HIIT in clinical populations.22 Given the fitness level of the current study participants, the absolute intensity of the high-intensity bouts was generally comparable to brisk walking up an incline. Sessions were completed on 3 days per week, for 12 weeks, at a university gymnasium. All training sessions were supervised by an accredited exercise professional. The majority of HIIT sessions were conducted individually with the maximum number of participants training at one time being two. All Control group sessions were conducted individually. HIIT sessions were preceded with a 5-minute warm up and followed by a 5-minute cool down. Participants progressed from at least one 4 minute interval in week 1 to the full 4×4 protocol by week 4. Heart rates were recorded at the end of each minute and RPE was checked in the final 15 s of each minute. Absolute training intensities were progressed according to adaptation, informed by heart rate response and RPE, in order to maintain a consistent relative exercise intensity for the 12-week intervention. Exercise mode was predetermined by an accredited exercise professional prior to the baseline cardiopulmonary exercise test, based on orthopedic limitations. While a treadmill was the study preferred exercise modality, other training modes (cycle ergometer, rowing ergometer, arm ergometer) were selected as appropriate by the accredited exercise professional according to their musculoskeletal capabilities. Following the supervised HIIT intervention, participants were then asked to complete 12-weeks of self-directed HIIT, using the same 4×4 minute protocol, adapted for the participant’s self-directed exercise environment (i.e., access to available exercise equipment at home, at a gym, or within their local environment). Participants were given a heart rate monitor (Polar; Polar Electro, Kempele, Finland), Borg RPE scale (license #5RYHYG), and an exercise journal to record self-directed HIIT sessions.
Data collection
Interviews on participant experiences and perceptions were conducted between June 2016 and November 2019. Participants undertook three individual audio-recorded semistructured interviews, at baseline, after supervised HIIT, and after completion of self-directed HIIT. Interview questions (Supplementary File 1) were developed by the multidisciplinary research team including exercise physiologists, a clinical health psychologist, dietitians, and hepatologists. The baseline interview focused on participants’ understanding of HIIT, feelings and expectations about HIIT as an exercise option, anticipated barriers/enablers to general exercise and self-efficacy related to HIIT. The post supervised-HIIT interviews focused on participant experience with HIIT including feelings and outcomes, barriers/enablers to HIIT, future intentions and self-efficacy to undertake self-directed HIIT. The post-self-directed HIIT interviews replicated the post-supervised HIIT interviews and included questions related to barriers and enablers to sustaining HIIT exercise as prescribed.
Interviews were conducted individually, either face-to-face (at the same setting as the intervention study) or via telephone, by one of two exercise specialists (female accredited exercise physiologists, including SK) who were known to the participants from the supervised training sessions. Interviews were scheduled within one week of completion of each timepoint, were recorded, then uploaded to a research data management system prior to deletion from the recording device. Contact with participants who had withdrawn from the study was attempted up to three times.
Participant characteristics
Baseline study assessments are described in detail elsewhere (ANZCTR: ACTRN12616000305426). In brief, participants completed a suite of physical health measures including body mass index (kg/m2), a detailed health history, health-related quality of life questionnaire33 and disease severity determined by NAFLD activity score.34 Cardiorespiratory fitness quantified as peak oxygen uptake () was determined by assessing pulmonary gas exchange during a symptom-limited cardiopulmonary exercise test (Parvo TrueOne 2400; ParvoMedics Inc., East Sandy, UT, USA). Cardiorespiratory fitness level was described according to standard sex- and age-specific percentiles.35,36
Data analysis
Interview audio-recordings were manually transcribed verbatim by research staff who were not involved in the interviewing process. Transcripts were de-identified by redacting any reference to participant names. Data were managed using Microsoft Excel and independently coded and analyzed for dominant themes and subthemes by two researchers (SK and IH) using a deductive style of thematic analysis37 with themes and subthemes identified and consolidated through consensus discussions. Dominant themes were then tabulated and crosschecked with exemplar quotes to validate interpretations and consistency. Identified dominant themes and subthemes were developed using both a deductive approach bound by the intent of the overarching trial investigating feasibility of HIIT as a therapy for NASH including patient knowledge, barriers, enablers and outcomes; and an inductive approach developed after consultative interpretation of the analysis. Final review and discussion involved all investigators. Exemplar quotes are notated with participant number and the time point of interview (baseline, post-HIIT or post self-directed HIIT).
Results
Fourteen individuals were recruited, with two participants withdrawing prior to baseline interview completion (COVID-related university closures n=1 and loss to follow-up n=1). Of the 12 people who commenced the intervention, including four (33%) who were randomized to the control group and then invited to complete the HIIT component, did not complete the study. Three dropped out during supervised HIIT due to competing time commitments, and one during self-directed HIIT due to loss to follow-up. Therefore, a total of 29 of a possible 36 interviews (81% response rate) from 12 individuals were conducted across the three time points; baseline (n=12), post-supervised HIIT (n=9), and after self-directed HIIT (n=8). No participant who withdrew from the study returned for an invited interview. Of the nine participants who completed the supervised HIIT program, session attendance was >90% and all adhered to the HIIT prescription. Of the eight participants completing the self-directed HIIT phase, self-reported adherence was poor. The median interview duration was 5 min 32 s (IQR 2 min 54 s to 9 min 39 s).
Demographic and clinical description of interviewed participants are shown in Table 1. Modalities initially prescribed for supervised HIIT included treadmill (n=7), cycle ergometer (n=3), rowing ergometer (n=1), and arm ergometer (n=1). For the self-directed HIIT, reported modalities included hill walking (n=2), treadmill (n=2), jogging (n=1), cycle ergometer (n=2), and boxing (n=1).
Table 1. Baseline characteristics of interview participants.
| Characteristic (n=12) | Value |
|---|---|
| Male Sex, n (%) | 8 (67) |
| Age in years, mean±SD | 57±10 |
| Body mass index in kg/m2, mean±SD | 39.4±7.3 |
| Body weight in kg, mean±SD | 120.1±31.3 |
| Cardiorespiratory fitness | |
| in mL/kg/min, mean±SD | 20.9±9.1 |
| Percentile, median (range) | 7th (5th–73rd) |
| Exercise capacity (time on test in seconds), mean±SD | 626.0±178.6 |
| Respiratory exchange ratio at peak capacity | 1.1 (0.1) |
| NAFLD activity score, median (range) | 5 (3–7) |
| Fibrosis, median (range) | 2 (1a–4) |
| F0/1, n (%) | 2 (17) |
| F2, n (%) | 5 (41) |
| F3, n (%) | 3 (25) |
| F4, n (%) | 2 (17) |
| Comorbidities, median (range) | 6 (2–14) |
| Type 2 diabetes, n (%) | 9 (75) |
| Metabolic syndrome, n (%) | 12 (100) |
| Hypertension, n (%) | 11 (92) |
| Musculoskeletal conditions, n (%) | 12 (100) |
| 0 | 0 (0) |
| 1 | 5 (42) |
| 2–3 | 6 (50) |
| >3 | 1 (8) |
| Fatigue domain-CLDQ, mean±SD score/7# | 4.3±1.1 |
| Body pain-CLDQ, mean±SD score/7# | 2.8±1.2 |
| Medications prescribed | |
| Total number of prescribed medications, median (range) | 8 (2–28) |
| Anti-hyperglycemic | 8 (67%) |
| Insulin | 4 (33%) |
| Biguanide | 8 (67%) |
| Sulfonylurea | 2 (17%) |
| DPP-4 inhibitor | 1 (8%) |
| SGLT2 inhibitor | 6 (50%) |
| Antihypertensive | 10 (83%) |
| Cholesterol/lipid lowering | 10 (83%) |
| Beta-blocker | 4 (33%) |
, cardiorespiratory fitness (peak rate of oxygen consumption); percentiles are based on age- and sex-specific cutoffs; #Mean score from CLDQ refers to that experienced in the previous 2 weeks. Responses are a Likert scale ranging from 1 (most impairment) to 7 (least impairment). The fatigue domain comprises an average of five questions. Body pain relates to a single question within the broader systemic symptom domain. NAFLD activity score ranges from 0–8 with ≥ 5 considered more severe disease. CLDQ, chronic liver disease questionnaire; DPP-4, dipeptidyl peptidase-4; NAFLD, nonalcoholic fatty liver disease; SD, standard deviation; SGLT2, sodium-glucose cotransporter-2.
Four dominant themes with subthemes were identified. They related to participant prior knowledge and expectations of HIIT, barriers and enablers to commencing and continuing HIIT in supervised and unsupervised settings, and outcomes experienced (Table 2): (1) no awareness of/experience with HIIT and ambivalence about exercise capabilities; (2) multiple medical and social barriers to commencing and continuing HIIT; (3) exercise specialist support was a highly valued enabler; and (4) HIIT was enjoyed and provided holistic benefits.
Table 2. Themes and subthemes with illustrative quotes.
| Theme | Subtheme | Illustrative quotes |
|---|---|---|
| No awareness of/experience with HIIT and ambivalence about exercise capabilities | N.A | I understand very little of it at the moment, until I actually get shown what I am supposed to be doing (12 Baseline). I have seen some of it on the Biggest Loser and stuff like that. But they were using ropes and things like, um, weights and things so I don’t know (06 Baseline). I’m not fit you know…. I don’t know if I can do HIIT, it might be too high to achieve (06 Baseline). I am nervous, uh, unsure about my heart rate going high, um, my, I have been told I probably can’t get my heart rate up high because of my size (10 Baseline). Oh, I’m feeling positive about starting the program. Um, how the body handles it as we go on, that is another question (12 Baseline). That’s what I am scared about with the home-based that, without that motivational part of it (09 post self-directed HIIT) |
| Multiple medical and social barriers to commencing and continuing HIIT | Multimorbidities and multifarious specialist appointments | Yeah just joints, knees, feet and work (13 Baseline). Well, the only thing that I can see that would stop me is pain…pain in my knee, everything else will be fine (17 Baseline). At the moment, I don’t want to push myself too much, ……. because of the knee and the ankle, and now my hips hurting and my arms are hurting, I am starting to find it very difficult to do what I need to do to get work (13 post self-directed HIIT). Um, I have, and my wife, we have many appointments. ……. I have appointments for my NASH and my knees and diabetes and my wife has health conditions too (08 Baseline) |
| High burden of carer responsibilities | Well, my husband has dementia, I am his carer so I will need to bring him with me (10 Baseline). The only thing that got in the way was getting my husband ready to get here. That was quite stressful. But he then got into a routine, and he really enjoyed coming over…… I was worried that I would send him a bit more confused (10 Post-HIIT). …….If my husband gets sick, and I need to be with him and get him places, and you know, to appointments, or be with him in hospital or whatever and that is very unpredictable (16 Baseline) | |
| Exercise specialist support was a highly valued enabler | HIIT education and logistics support | I guess being told what to do and how to do it. (04 Baseline). I understand very little of it at the moment, until I actually get shown what I am supposed to be doing (12 Baseline). I won’t be as confident, because I won’t be familiar with the machine. And you girls won’t be there, and I won’t have that support. But, um I think I am confident enough within myself to do it, but I can imagine people who aren’t confident, or who don’t go out a lot, or who have never been to a gym before (10 post self-directed HIIT). We put the monitor on and then we go in [to the gym], the only problem was the fact that the monitor, um the watch lost contact on the treadmill, I couldn’t figure out why… it would just lose it and go away (14 post self-directed HIIT). You know, whether I will be able to create the situation where I am getting the, you know, the heart rate up, and doing the four intervals. Whether I can actually do that and sustain that, or whether, I will find that it felt like too much and I couldn’t finish it. That worries me (16 post self-directed HIIT). The positivity of the controlled sessions means that I have the power to do it, I have the ability to do it, and that’s what has kept me doing it (09 Post-HIIT). Well, I would come here, everything would be set, I would have the ah, um, hate, the heart rate monitor, and all that all set-up, all made for myself. The machine was generally in my place ……we would do the HIIT, I would recover, and then I would go home (08 Post-HIIT). Very difficult to organize myself to do it. Life gets in the way (13 post self-directed HIIT) |
| Feeling safe | The positivity of the controlled sessions means that I have the power to do it, I have the ability to do it, and that’s what has kept me doing it (09 post self-directed HIIT). It has been really great because there’s different people available, um physical stuff, like with my foot. It was a bit of a pain, but we always just kept looking for a way around that (16 Post-HIIT). I think the arm ergometer, ah, the equipment to get my heart rate up without my knees being limiting. I think I will be good on that and that will help (08 Baseline) | |
| Social connection | Um well, the people that were taking me on the day, they were always really encouraging, and it was ah, it was a pleasure to interact with them, they are all very nice people, so it was never a drag to have to come in, it was always something to look forward to (17 Post-HIIT). The team, if it wasn’t for that team, I would have gone home long ago (11 Post-HIIT). I have enjoyed the social part of it (09 Post-HIIT). I mean, I always find that I make it difficult because, like if I had, if I was doing it with someone else, I would honor the commitment better (16 post self-directed HIIT). The motivational part of it I think is, you know, what worries me is that when this part of it stops, just going on the home-based that, I might think well I’m a bit tired tonight, I will do it tomorrow night. And before you know it, the week is gone, and then another weeks gone and That’s what I am scared about with the home-based that, without that motivational part of it, the support, having professional support, not just support, but having somebody who knows what they are doing, who knows how, how the program is done, how the program is run (09 Post-HIIT) | |
| A point of commitment and accountability | I think committing to something, I feel um, I need to do it now (07 Baseline). I guess being told what to do and how to do it, and just committing (04 Baseline). oh, well I think coming in to a regular session, you know, really commit and um, with the right equipment for my body size (10 Baseline). Um yeah, I figured that if I could make the commitment, if you guys could make the commitment for my benefit, then it was in my interest to make the commitment and I was cool with that. (09 Post-HIIT). Um while I am confident to do it and I have geared up to do it, I just find that ……… I may go home and say oh I’ll do a thing tomorrow night, whereas coming here, I know I had to do it and I wanted to do it. (09 Post-HIIT). I would come here [supervised setting] to do anything, but I still probably wouldn’t go to a gym (09 Post-HIIT). Um, telling other people, like even if I am not doing it with someone, telling other people….that I am going to do it, and having someone say, “did you do that?”, helps (16 post self-directed). I have a treadmill at home, I have some hills out on the street I can walk, so there’s the gym….so, I possibly could [do HIIT at home], But I need to be pushed too, I will need to be pushed to do it (07, Post-HIIT). There’s been some weeks where I haven’t done it [due to] health ….. there are some weeks where I have, but it wasn’t my favorite part of the thing, you know, it’s very very hard doing it by yourself (09 post self-directed HIIT). Um, the fact that, well in my case, when I get home, psychologically I am home and I tend to unwind, and you hop on the treadmill and you think, 10–15 minutes will do me, instead of a 40 minute session (09 post self-directed HIIT). ..hard to fit in, unless I did it first thing you know, a priority, and sometimes I’d commit to it and just get it done, you know, but um other times I think I would do it later and then never did. Its um not like I don’t really have the time, but things just come up, like family issues, and I need to pick up my grandson or just friends call by and um, I just didn’t prioritize it (07 post self-directed HIIT) | |
| HIIT was enjoyable and provided holistic benefits | It was good, I enjoyed it, a lot (17 Post-HIIT). Absolutely marvelous. I have never done anything like this before and it has been a real pleasant experience (08 Post-HIIT). Well, the most notable thing is the energy that I have. I get a lot more done…. More energy and more confident that I can do it (10 Post-HIIT). I have got more confident, I found I could remember more, It improved my memory… [more confident in] everything throughout my whole life, I felt a lot more confident (11 Post-HIIT). My knee, I was um, actually surprised it felt better after the exercise (13 Post-HIIT). And I feel more flexible in the legs, being on the bike really helped with my knees (17 Post-HIIT). I am not having trouble getting out of bed in the morning physically, I can swing my legs, my sciatica, ah, is going away, and in conjunction with the leg exercises I am doing, I feel like I am turning the clock back (08 Post-HIIT). Um, overall, physically I feel much healthier and much stronger. …… And this has enabled me to get back to the same level of strength and wellbeing I felt…… Its ah, you know I have recovered my base physical strength (08 Post-HIIT). Something I have noticed greatly has changed is my breathing, the indigestion has sort of gone, um, because of this program…. (07 Post-HIIT). I don’t think, oh God I gotta walk up a flight of stairs. Ah well I just know that I can walk up that flight of stairs or walk to the shops or do the full round of shopping without fearing that I’ve got to get back to the car because my back is hurting or whatever. So I do feel stronger muscularly (10 Post-HIIT). Um, before it was difficult for me to put shoes on, I had to sit down to put shoes on. Now I can stand and put shoes on. And just basic, um, not losing my breath so much (17 Post-HIIT). Yeah I have to do this, I gotta do this. And it actually helped me out with certain things in my life. So it gave me a lot more stamina riding motorbikes and stuff like that, which is what I like to do (13 post self-directed HIIT). Oh I loved it. Yeah, it was really, um, well it really helped me because I don’t usually do exercise and I am not good at being consistent about it. So, it was helpful to have to come. And I guess, I wouldn’t of, if I didn’t enjoy it, I wouldn’t have made myself keep coming. (16 Post-HIIT). I was very nervous in the beginning, but as time went on, I enjoyed it more and more, just as time went on, I slipped more into the way things were going and it was great I enjoyed it (11 Post-HIIT). Ah I just generally feel like I have more energy ….. I just notice that I walk with a bit more of a spring in my step and you know, I haven’t been sick even, you know, [when] other people being sick around me and I haven’t got sick (16 Post-HIIT) |
HIIT, high-intensity interval training.
No awareness of/experience with HIIT and ambivalence about exercise capabilities
Prior to the intervention, it was rare for participants to be aware of HIIT as a training option and none had previous experience with HIIT prescriptions.
“I have not heard of it at all before now (09 Baseline).”
While there was general enthusiasm to commence exercise in this research setting, this coexisted with nervousness and trepidation about their capability to perform HIIT.
“I’m looking forward to it. I think. Um I might find it hard, but I will just try it out (04 Baseline).”
After experiencing HIIT, there was some surprise expressed by participants associated with the degree of physical response experienced without injury.
“But most times when I go [to] the gym, I hurt myself, and do a ligament or something, but that hasn’t happened…..It was quite enlightening to me really (10 Post-HIIT).”
A lack of confidence in exercise capabilities to continue HIIT in a self-directed manner remained in some participants at the end of the 12-weeks supervised program.
“You know, whether I will be able to create the situation where I am getting the, you know, the heart rate up and doing the four intervals. Whether I can actually do that and sustain that, or whether, I will find that it felt like too much and I couldn’t finish it. That worries me (16 Post-HIIT).”
Multiple medical and social barriers to commencing and continuing HIIT
Participants anticipated, and some described experiencing, generalized barriers to exercise. These included: work and study commitments, travel time burden related to attending exercise sessions and changes to usual routine. However, additional complex barriers to commencing supervised HIIT and continuing self-directed HIIT were also highlighted:
Multimorbidities
The presence of significant multimorbidities among participants was ubiquitous, such as musculoskeletal limitations, diabetes, significant fatigue, and low mood. This complex medical phenotype was a pervasive barrier to the participants commencing exercise. The impact of acute illness was the most identified reason for non-attendance during the supervised HIIT program.
“Mainly just illness [makes HIIT difficult], I think that’s all, that’s all it has been, just illness (07 Post-HIIT).”
Multimorbidity impacted on the participants ceasing or reducing the frequency of self-directed HIIT. Injury, illness, or medical procedures often resulted in temporary pauses in HIIT during the self-directed phase, and HIIT was then never reinstated. It was expressed by one participant that when they stopped exercising, the bodily pain they had previously experienced returned quickly. This pain may then have been a motivational and/or functional barrier to recommencing HIIT without external support from exercise supervisors.
“Um, when I was doing the exercises, my pains in the knee were markedly reduced. They got better and better over the time. What happened once I stopped, and it happened very quickly once I stopped, was that the pain went back to where it was. (17 post self-directed HIIT).”
Multifarious specialist appointments
Most participants with multimorbidity had established links with the healthcare system and experienced a high burden of multifarious specialist appointments that could be a barrier to attending exercise sessions.
“Um, I have, and my wife, we have many appointments. ……. I have appointments for my NASH and my knees and diabetes and my wife has health conditions too. (08 Baseline).”
High burden of carer responsibilities
Obligations related to caregiver responsibilities that negatively impacted attendance to and sustaining frequency of HIIT appointments.
“Um, I had to basically stop doing it. I just don’t get the time anymore because I am now a full-time carer for my wife. (08 post self-directed HIIT).”
Exercise specialist support was a highly valued enabler
HIIT education and logistics support
With very limited to no prior knowledge or experience with HIIT, the majority of participants relied on the exercise specialist for HIIT education and logistical support managing equipment (e.g. exercise equipment and heart rate devices), and specialist monitoring of exercise was also highly valued.
“Well, I would come here, everything would be set, I would have the ah, um, hate, the heart rate monitor and all that all set-up, all made for myself. The machine was generally in my place ……we would do the HIIT, I would recover and then I would go home. (08 Post-HIIT).”
This desire for logistic support persisted after the supervised program with several participants describing an inability to procure equipment for home and that HIIT prescription was not easily translated to their own environment. When self-directed, participants felt unable to manage all aspects of HIIT themselves such as equipment set-up and maintenance, heart rate, and time monitoring, warm-ups / cool-downs. While participants were encouraged by staff to facilitate their exercise environment to be enabling (i.e., just having a treadmill is not enough, it must be enticing to use), there was heterogeneity among participants in how logistics such as scheduling, routine, and access to equipment were self-managed. For some, home gym equipment was preferred over external gym providers, which were at times considered unfamiliar and costly. There seemed to be a greater degree of confidence to continue to do self-directed HIIT in those participants who had chosen to continue activities that did not require equipment (e.g., walking).
“[it’s] Awkward [doing HIIT at home] because while you are there, it is a matter of you controlling everything, yourself. You are monitoring the lot, you are monitoring your thing, the cool down, the HIIT part, you know, ….. when you gotta speed [up], monitoring controls. (09 post self-directed HIIT).”
Feeling safe
Supervision from the exercise specialist created a feeling of safety and supported participants to gain confidence during the HIIT intervention. The role of expert exercise prescription, direction, and advice during the supervised HIIT program was highly valued as an enabler. This included the ability to tailor the exercise prescription (notably the modality) to individual needs.
“Well the fact that it was supervised, both in terms of, you know, keeping me disciplined and keeping me safe, and learning that I can feel really bad, but because of being monitored, by people that know what they are talking about, I know that I am okay…….So, it was, that really helped me to learn it was okay, and to trust that it was okay (16 Post-HIIT).”
Social connection
The supervised HIIT with exercise specialists also generated social connection and social support which was highly valued by participants and strongly influenced motivation for HIIT. The social support of the exercise specialist was consistently raised as an enabler to complete the HIIT sessions and there was a desire not to disappoint themselves, the exercise specialists, or the research team. A personal connection with the instructor/s was valued. Participants who joined a gym and accessed other exercise specialists during the self-directed HIIT period seemed to maintain HIIT activity, albeit lower than during the supervised intervention phase.
“I mean it really helps to have somebody encouraging you and to get to know people and, like, three very different but very lovely people. Like, it was almost, I hate to say it, it was almost like a social occasion, catching up, having a chat in between things [intervals], it’s interesting (16 Post HIIT).”
A point of commitment and accountability
Accountability was a critical enabler for participation in HIIT. Mentally committing to the program and the accountability to the exercise specialists was perceived as a strong enabler during the supervised HIIT program. Many participants predicted that the loss of accountability to the exercise specialist would negatively impact self-directed continuation of the HIIT as prescribed. Success with self-directed HIIT was often linked to appointing alternative external points of commitment and accountability and without this, frequency of HIIT decreased significantly. The loss of scheduled appointments with expert supervision was commonly stated as a key factor reducing motivation to commit to self-directed HIIT.
“So when I was coming here, it’s, I was scheduled to come here. It’s like, I treat like it was a doctor’s appointment, or a hospital appointment, something like that. When I am home……. I will either do something or I don’t do something depends on how I feel (13 post self-directed HIIT).”
HIIT was enjoyed and provided holistic benefits
During the supervised HIIT sessions, participants unanimously reported positive experiences with expressed feelings of enjoyment of the HIIT program.
“It was enjoyable, mentally and physically beneficial for me (09 Post-HIIT).”
Participants’ experiences of supervised HIIT were associated with perceptions of increased energy, fitness, strength, and flexibility. There were multiple reports of benefits experienced across multimorbidities including muscular, orthopedic and nerve pain and gastroenterological symptoms (e.g., gastro-esophageal reflux resolved).
“Ah I just generally feel like I have more energy ….. I just notice that I walk with a bit more of a spring in my step and you know, I haven’t been sick even, you know, [when] other people being sick around me and I haven’t got sick (16 Post-HIIT).”
In addition, participants described HIIT resulted in a greater ability to cope with activities of daily living and stimulated more active routines in other aspects of their life.
“But more importantly, from my behalf, is where I work, at the start of the program I would not have thought about going up the road to the shop to get a coffee or lunch, well now it is second nature, I just walk up. It’s not far, it’s only 500 meters or whatever, but I don’t even think about it now, I just do it. (09 Post-HIIT).”
Discussion
With the growing body of evidence of the clinical efficacy of HIIT for treatment of NAFLD,11,14 incorporating participants’ experience to inform the translation of research into a service design that enables exercise prescription is crucial. To our knowledge, this is the first evaluation of experiences and perceptions of both professionally supervised and self-directed HIIT in people with NASH. In the context of naïve exposure to HIIT, people with NASH can have low knowledge of and confidence for HIIT and are faced with multiple complex barriers to commencing and continuing HIIT. The involvement of an exercise specialist was a key enabler to sustained engagement, which provided participants with a range of holistic benefits.
Participants in this study had multimorbidity with significant musculoskeletal limitations, which is typical of people presenting to liver clinics with NASH.38,39 Complex multimorbidity was a pervasive barrier to exercise and impacted both physical and mental aspects of commencing and continuing with HIIT. Musculoskeletal limitations to exercise were ubiquitous and added to the mixed emotions of enthusiasm and trepidation experienced when attempting a new physical activity targeted at treating their chronic illness. Reflective of the high burden of comorbidities within the study cohort, the participants reported that multifarious specialist appointments interfered with attendance to exercise sessions. It was apparent that the siloed design of the local health system is experienced by patients with multiple comorbidities, all requiring medical input, as lacking in co-ordination. This has the unintentional consequence of creating a perceived barrier to attending HIIT sessions. This highlights the need for a highly flexible exercise service delivery that accommodates patient schedules while maintaining structured engagement to promote accountability and social connection.
Despite HIIT consistently ranking in the top fitness trends since 2014 by the American College of Sports Medicine40 and the rapid rise in the number of publications involving HIIT,41 there was a lack of awareness of HIIT, as well as no experience with HIIT in this patient cohort. This highlights a discordance between academic knowledge of HIIT and clinical treatments offered to patients and emphasizes the importance of raising awareness of both clinicians and patients to assist translation of research demonstrating the value of HIIT into routine practice. HIIT prescription involves several variables which are integrated into the prescribed HIIT regimen (i.e., number, duration, and intensity of intervals; type and length of recovery; and mode of exercise). For the study participants, it was clear that the exercise professional was highly valued for their governance of HIIT prescription (i.e., expertise in educating patients about HIIT, assisting logistics related to equipment use, generating a feeling of safety while exercising, creating social connections) and being a point of accountability that enabled strong commitment to the program. The lack of regular supervision by the exercise specialist contributed to reduced participation in self-directed environments due to the loss of the multiple enablers associated with exercise specialist support. This highlights a critical issue regarding accessibility and translatability of HIIT. The supervised program was free for participants, and this may have influenced the fact that neither cost nor affordability of HIIT was raised at any time as a possible barrier, although no financial support was offered for self-directed training options. Cost has been raised by others as a key barrier to exercise participation in people with NASH29,39 and further research exploring low cost, accessible exercise support is urgently needed. This may be particularly important for high priority groups including indigent, rural, and remotely located and indigenous peoples where cost and access can be key barriers to exercise adoption and maintenance. Strategies to promote affordable access to exercise support could include telehealth, mHealth or eHealth technologies42–45 as well as group-based exercise session to reduce individual cost and/or providing hospital community health infrastructure.
Prior to beginning the HIIT intervention, participants were enthusiastic and excited, although they also reported nervousness and a lack of confidence in their own physical capabilities. A lack of confidence to exercise without supervision and a fear of falling have previously been identified as a key barriers to physical activity in NAFLD.38,39,46 Clinicians, including exercise specialists, need to address patient confidence to facilitate exercise adoption (e.g., via graduated introduction to HIIT, providing mastery experiences, providing reassurance, and education). Other studies have identified that patients understand exercise is important and have a strong desire to be more physically active,39,46 especially with the support of exercise specialists.38 When given a choice, patients do prefer exercise over pharmacotherapies for NAFLD management.38 Moreover, the uncertainty in patient capabilities for lifestyle change also influences clinician perceptions of patients47 and may act as a barrier to discussing HIIT as a training option, or even prioritizing exercise prescription in treatment plans.39,48 Medical clinicians commonly report feeling ill-equipped to support tailored exercise prescription with a lack of accessible resources, little to no formal training (despite an expressed desire for training49) and limited time during consultations.48,50 While generalized lifestyle information related to management of NAFLD is readily available, most clinicians do not give personalized recommendations or refer to exercise specialists51 and patients are left wanting more after their clinical interactions.48,51,52 These issues may be greater with HIIT, given its vigorous nature.
External regulators of behavior including supervision and social support are critical enablers for sustaining exercise routines in NAFLD.51 The transition from short-term supervised to long-term self-directed exercise programs within research settings has been ubiquitously associated with reduced participation and regression of health benefits.15,16 Participants in this study predicted and reported difficulties with maintaining HIIT once supervised sessions ceased. Removal of supervision has been documented as a barrier to sustained exercise in all studies examining HIIT beyond the supervised clinical setting.53 However, those who pre-empted this and recruited social supports (e.g., attending a gym with a friend or family member) were more likely to sustain engagement with regular HIIT training, albeit with generally lower intensity/volume to that in the supervised phase of the intervention. Exercise enjoyment is an important predictor of exercise behavior, with higher levels of enjoyment resulting in more positive attitudes toward exercise and therefore more positive intentions to exercise in the future.54 An acute session of HIIT appears more enjoyable than an acute session of traditional moderate intensity continuous training across a diversity of healthy and clinical groups, despite significantly higher heart rate, blood lactate, and perceived exertion.55 Our findings corroborate this, with HIIT being unanimously enjoyed during the supervised sessions by the participants. Despite this, participation decreased when self-directed. This suggests that the high level of enjoyment experienced may not have been enough to offset other barriers such as low self-efficacy and lack of specialized supervision. Moreover, it highlights the social benefit of supervised exercise for people with NASH.
Impaired physical functioning and ability to accomplish activities of daily life have been identified as key contributors to reduced health-related quality of life in people with NASH.29 Study participants reported wide-ranging beneficial outcomes of HIIT training, commonly related to higher energy levels and lower fatigue. This is noteworthy given the age, severity of NASH, and multimorbidity present in the study cohort. Although exercise is effective at improving fatigue associated with NASH,56 fatigue itself and lack of energy are reported as barriers to initiating and finishing exercise sessions in people with NAFLD.29,38,39 HIIT may be a strategic training option for NASH given its potential beneficial impact on energy levels. In this study, generalized improvements in perceived strength, flexibility, gastroenterological symptoms, and pain added to the holistic nature of HIIT benefits and translated into reported improvements in activities of daily living.
The study findings should be considered within the context of its limitations. Participants were recruited to an exercise trial which introduces bias (patient cohort interested in exercise, with intentions to commit to HIIT three times per week). Interviewers were known to participants, which may have influenced responses, and as participants did not review transcripts, they were unable to add further perspectives. There was a dropout rate of 33%, which is similar to what has been observed in supervised exercise trials in NAFLD.57 Moreover, perspectives and experiences of people who did not complete the intervention and did not accept the invitation to return for interview were not captured. We also did not capture the perspectives of care providers, notably hepatologists and exercise professionals, which would provide further valuable data to inform healthcare models and future directions for HIIT intervention translation. While time efficiency is often described as a key advantage of HIIT, this did not appear relevant for this patient group who undertook minimal hours of physical activity at baseline, so even time efficient physical activity was still an increased time investment overall. Finally, patient experiences are one part of the HIIT for NASH research agenda, and the results of the current study need to be considered in the context of other evidence, such as safety.
Collectively, evaluation of perceptions and experiences of people with NASH demonstrates that supervised HIIT was enjoyed and beneficial despite initial ambivalence and many complex medical and social barriers. Shared patient experiences highlight key considerations for the implementation of HIIT into clinical practice. Recommendations for future interventions are outlined in Supplementary File 2. While benefits are multifaceted, numerous barriers to HIIT as a training option remain. Embedding exercise specialists into clinical care pathways is critical to maximize uptake and sustainability of HIIT programs for people with NASH.
Supporting information
Acknowledgments
The authors would like to acknowledge Chloe Salisbury for her research assistance.
Abbreviations
- HIIT
high-intensity interval training
- NAFLD
nonalcoholic fatty liver disease
- NASH
nonalcoholic steatohepatitis
- RPE
rating of perceived exertion
Ethical statement
The evaluation was nested within a larger randomized controlled trial investigating the safety, feasibility, and efficacy of a 12-week supervised HIIT intervention for improving cardiometabolic health in people with NASH (Australia and New Zealand Clinical Trials Registry: ACTRN12616000305426). All procedures were in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments, and approved by the Metro South Hospital and Health Service’s Human Research Ethics Committee (HREC/15/QPAH/747) and The University of Queensland Human Research Ethics Committee (2016000010).
Data sharing statement
No additional data are available.
References
- 1.Dufour JF, Scherer R, Balp MM, McKenna SJ, Janssens N, Lopez P, et al. The global epidemiology of nonalcoholic steatohepatitis (NASH) and associated risk factors–A targeted literature review. Endocrine and Metabolic Science. 2021;3:100089. doi: 10.1016/j.endmts.2021.100089. [DOI] [Google Scholar]
- 2.Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 3.Noureddin M, Vipani A, Bresee C, Todo T, Kim IK, Alkhouri N, et al. NASH Leading Cause of Liver Transplant in Women: Updated Analysis of Indications For Liver Transplant and Ethnic and Gender Variances. Am J Gastroenterol. 2018;113(11):1649–1659. doi: 10.1038/s41395-018-0088-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328–357. doi: 10.1002/hep.29367. [DOI] [PubMed] [Google Scholar]
- 5.European Association for the Study of the Liver (EASL), European Association for the Study of Diabetes (EASD), European Association for the Study of Obesity (EASO) EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64(6):1388–1402. doi: 10.1016/j.jhep.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 6.Kistler KD, Brunt EM, Clark JM, Diehl AM, Sallis JF, Schwimmer JB, NASH CRN Research Group Physical activity recommendations, exercise intensity, and histological severity of nonalcoholic fatty liver disease. Am J Gastroenterol. 2011;106(3):460–468. doi: 10.1038/ajg.2010.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gerber L, Otgonsuren M, Mishra A, Escheik C, Birerdinc A, Stepanova M, et al. Non-alcoholic fatty liver disease (NAFLD) is associated with low level of physical activity: a population-based study. Aliment Pharmacol Ther. 2012;36(8):772–781. doi: 10.1111/apt.12038. [DOI] [PubMed] [Google Scholar]
- 8.Weston KS, Wisløff U, Coombes JS. High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: a systematic review and meta-analysis. Br J Sports Med. 2014;48(16):1227–1234. doi: 10.1136/bjsports-2013-092576. [DOI] [PubMed] [Google Scholar]
- 9.Rognmo Ø, Moholdt T, Bakken H, Hole T, Mølstad P, Myhr NE, et al. Cardiovascular risk of high- versus moderate-intensity aerobic exercise in coronary heart disease patients. Circulation. 2012;126(12):1436–1440. doi: 10.1161/CIRCULATIONAHA.112.123117. [DOI] [PubMed] [Google Scholar]
- 10.Taylor JL, Holland DJ, Keating SE, Leveritt MD, Gomersall SR, Rowlands AV, et al. Short-term and Long-term Feasibility, Safety, and Efficacy of High-Intensity Interval Training in Cardiac Rehabilitation: The FITR Heart Study Randomized Clinical Trial. JAMA Cardiol. 2020;5(12):1382–1389. doi: 10.1001/jamacardio.2020.3511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sabag A, Barr L, Armour M, Armstrong A, Baker CJ, Twigg SM, et al. The Effect of High-intensity Interval Training vs Moderate-intensity Continuous Training on Liver Fat: A Systematic Review and Meta-Analysis. J Clin Endocrinol Metab. 2022;107(3):862–881. doi: 10.1210/clinem/dgab795. [DOI] [PubMed] [Google Scholar]
- 12.Hallsworth K, Thoma C, Hollingsworth KG, Cassidy S, Anstee QM, Day CP, et al. Modified high-intensity interval training reduces liver fat and improves cardiac function in non-alcoholic fatty liver disease: a randomized controlled trial. Clin Sci (Lond) 2015;129(12):1097–1105. doi: 10.1042/CS20150308. [DOI] [PubMed] [Google Scholar]
- 13.Oh S, So R, Shida T, Matsuo T, Kim B, Akiyama K, et al. High-Intensity Aerobic Exercise Improves Both Hepatic Fat Content and Stiffness in Sedentary Obese Men with Nonalcoholic Fatty Liver Disease. Sci Rep. 2017;7:43029. doi: 10.1038/srep43029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hamasaki H. Perspectives on Interval Exercise Interventions for Non-Alcoholic Fatty Liver Disease. Medicines (Basel) 2019;6(3):83. doi: 10.3390/medicines6030083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pugh CJ, Sprung VS, Jones H, Richardson P, Shojaee-Moradie F, Umpleby AM, et al. Exercise-induced improvements in liver fat and endothelial function are not sustained 12 months following cessation of exercise supervision in nonalcoholic fatty liver disease. Int J Obes (Lond) 2016;40(12):1927–1930. doi: 10.1038/ijo.2016.123. [DOI] [PubMed] [Google Scholar]
- 16.O’Gorman P, Naimimohasses S, Monaghan A, Kennedy M, Melo AM, Ní Fhloinn D, et al. Improvement in histological endpoints of MAFLD following a 12-week aerobic exercise intervention. Aliment Pharmacol Ther. 2020;52(8):1387–1398. doi: 10.1111/apt.15989. [DOI] [PubMed] [Google Scholar]
- 17.Jung ME, Locke SR, Bourne JE, Beauchamp MR, Lee T, Singer J, et al. Cardiorespiratory fitness and accelerometer-determined physical activity following one year of free-living high-intensity interval training and moderate-intensity continuous training: a randomized trial. Int J Behav Nutr Phys Act. 2020;17:25. doi: 10.1186/s12966-020-00933-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roy M, Williams SM, Brown RC, Meredith-Jones KA, Osborne H, Jospe M, et al. High-Intensity Interval Training in the Real World: Outcomes from a 12-Month Intervention in Overweight Adults. Med Sci Sports Exerc. 2018;50(9):1818–1826. doi: 10.1249/MSS.0000000000001642. [DOI] [PubMed] [Google Scholar]
- 19.Jabardo-Camprubí G, Donat-Roca R, Sitjà-Rabert M, Milà-Villarroel R, Bort-Roig J. Drop-out ratio between moderate to high-intensity physical exercise treatment by patients with, or at risk of, type 2 diabetes mellitus: A systematic review and meta-analysis. Physiol Behav. 2020;215:112786. doi: 10.1016/j.physbeh.2019.112786. [DOI] [PubMed] [Google Scholar]
- 20.Sabag A, Way KL, Sultana RN, Keating SE, Gerofi JA, Chuter VH, et al. The Effect of a Novel Low-Volume Aerobic Exercise Intervention on Liver Fat in Type 2 Diabetes: A Randomized Controlled Trial. Diabetes Care. 2020;43(10):2371–2378. doi: 10.2337/dc19-2523. [DOI] [PubMed] [Google Scholar]
- 21.Ramos JS, Dalleck LC, Borrani F, Mallard AR, Clark B, Keating SE, et al. The effect of different volumes of high-intensity interval training on proinsulin in participants with the metabolic syndrome: a randomised trial. Diabetologia. 2016;59(11):2308–2320. doi: 10.1007/s00125-016-4064-7. [DOI] [PubMed] [Google Scholar]
- 22.Taylor JL, Holland DJ, Spathis JG, Beetham KS, Wisløff U, Keating SE, et al. Guidelines for the delivery and monitoring of high intensity interval training in clinical populations. Prog Cardiovasc Dis. 2019;62(2):140–146. doi: 10.1016/j.pcad.2019.01.004. [DOI] [PubMed] [Google Scholar]
- 23.Keating SE, Croci I, Wallen MP, Cox ER, Thuzar M, Pham U, et al. High-Intensity Interval Training is Safe, Feasible and Efficacious in Nonalcoholic Steatohepatitis: A Randomized Controlled Trial. Dig Dis Sci. 2022 doi: 10.1007/s10620-022-07779-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lazarus JV, Mark HE, Anstee QM, Arab JP, Batterham RL, Castera L, et al. Advancing the global public health agenda for NAFLD: a consensus statement. Nat Rev Gastroenterol Hepatol. 2022;19(1):60–78. doi: 10.1038/s41575-021-00523-4. [DOI] [PubMed] [Google Scholar]
- 25.Cortez-Pinto H, Chatham J, Chacko VP, Arnold C, Rashid A, Diehl AM. Alterations in liver ATP homeostasis in human nonalcoholic steatohepatitis: a pilot study. JAMA. 1999;282(17):1659–1664. doi: 10.1001/jama.282.17.1659. [DOI] [PubMed] [Google Scholar]
- 26.Canada JM, Abbate A, Collen R, Billingsley H, Buckley LF, Carbone S, et al. Relation of Hepatic Fibrosis in Nonalcoholic Fatty Liver Disease to Left Ventricular Diastolic Function and Exercise Tolerance. Am J Cardiol. 2019;123(3):466–473. doi: 10.1016/j.amjcard.2018.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Croci I, Byrne NM, Choquette S, Hills AP, Chachay VS, Clouston AD, et al. Whole-body substrate metabolism is associated with disease severity in patients with non-alcoholic fatty liver disease. Gut. 2013;62(11):1625–1633. doi: 10.1136/gutjnl-2012-302789. [DOI] [PubMed] [Google Scholar]
- 28.Golabi P, Otgonsuren M, Cable R, Felix S, Koenig A, Sayiner M, et al. Non-alcoholic Fatty Liver Disease (NAFLD) is associated with impairment of Health Related Quality of Life (HRQOL) Health Qual Life Outcomes. 2016;14:18. doi: 10.1186/s12955-016-0420-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Doward LC, Balp MM, Twiss J, Slota C, Cryer D, Brass CA, et al. Development of a Patient-Reported Outcome Measure for Non-Alcoholic Steatohepatitis (NASH-CHECK): Results of a Qualitative Study. Patient. 2021;14(5):533–543. doi: 10.1007/s40271-020-00485-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 31.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–381. [PubMed] [Google Scholar]
- 32.Wewege MA, Ahn D, Yu J, Liou K, Keech A. High-Intensity Interval Training for Patients With Cardiovascular Disease-Is It Safe? A Systematic Review. J Am Heart Assoc. 2018;7(21):e009305. doi: 10.1161/JAHA.118.009305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Younossi ZM, Guyatt G, Kiwi M, Boparai N, King D. Development of a disease specific questionnaire to measure health related quality of life in patients with chronic liver disease. Gut. 1999;45(2):295–300. doi: 10.1136/gut.45.2.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41(6):1313–1321. doi: 10.1002/hep.20701. [DOI] [PubMed] [Google Scholar]
- 35.Kaminsky LA, Imboden MT, Arena R, Myers J. Reference Standards for Cardiorespiratory Fitness Measured With Cardiopulmonary Exercise Testing Using Cycle Ergometry: Data From the Fitness Registry and the Importance of Exercise National Database (FRIEND) Registry. Mayo Clin Proc. 2017;92(2):228–233. doi: 10.1016/j.mayocp.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 36.Kaminsky LA, Arena R, Myers J. Reference Standards for Cardiorespiratory Fitness Measured With Cardiopulmonary Exercise Testing: Data From the Fitness Registry and the Importance of Exercise National Database. Mayo Clin Proc. 2015;90(11):1515–1523. doi: 10.1016/j.mayocp.2015.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 38.Glass O, Liu D, Bechard E, Guy CD, Pendergast J, Mae Diehl A, et al. Perceptions of Exercise and Its Challenges in Patients With Nonalcoholic Fatty Liver Disease: A Survey-Based Study. Hepatol Commun. 2022;6(2):334–344. doi: 10.1002/hep4.1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stine JG, Soriano C, Schreibman I, Rivas G, Hummer B, Yoo E, et al. Breaking Down Barriers to Physical Activity in Patients with Nonalcoholic Fatty Liver Disease. Dig Dis Sci. 2021;66(10):3604–3611. doi: 10.1007/s10620-020-06673-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thompson WR. Now Trending: Worldwide Survey of Fitness Trends for 2014. ACSM’s Health & Fitness Journal. 2013;17(6):10–20. doi: 10.1249/FIT.0b013e3182a955e6. [DOI] [Google Scholar]
- 41.You Y, Li W, Liu J, Li X, Fu Y, Ma X. Bibliometric Review to Explore Emerging High-Intensity Interval Training in Health Promotion: A New Century Picture. Front Public Health. 2021;9:697633. doi: 10.3389/fpubh.2021.697633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brown RC, Coombes JS, Jungbluth Rodriguez K, Hickman IJ, Keating SE. Effectiveness of exercise via telehealth for chronic disease: a systematic review and meta-analysis of exercise interventions delivered via videoconferencing. Br J Sports Med. 2022;56:1042–1052. doi: 10.1136/bjsports-2021-105118. [DOI] [PubMed] [Google Scholar]
- 43.Motz V, Faust A, Dahmus J, Stern B, Soriano C, Stine JG. Utilization of a Directly Supervised Telehealth-Based Exercise Training Program in Patients With Nonalcoholic Steatohepatitis: Feasibility Study. JMIR Form Res. 2021;5(8):e30239. doi: 10.2196/30239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lim SL, Johal J, Ong KW, Han CY, Chan YH, Lee YM, et al. Lifestyle Intervention Enabled by Mobile Technology on Weight Loss in Patients With Nonalcoholic Fatty Liver Disease: Randomized Controlled Trial. JMIR Mhealth Uhealth. 2020;8(4):e14802. doi: 10.2196/14802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hallsworth K, McPherson S, Anstee QM, Flynn D, Haigh L, Avery L. Digital Intervention With Lifestyle Coach Support to Target Dietary and Physical Activity Behaviors of Adults With Nonalcoholic Fatty Liver Disease: Systematic Development Process of VITALISE Using Intervention Mapping. J Med Internet Res. 2021;23(1):e20491. doi: 10.2196/20491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Frith J, Day CP, Robinson L, Elliott C, Jones DE, Newton JL. Potential strategies to improve uptake of exercise interventions in non-alcoholic fatty liver disease. J Hepatol. 2010;52(1):112–116. doi: 10.1016/j.jhep.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 47.Mayr HL, Kelly JT, Macdonald GA, Russell AW, Hickman IJ. Clinician Perspectives of Barriers and Enablers to Implementing the Mediterranean Dietary Pattern in Routine Care for Coronary Heart Disease and Type 2 Diabetes: A Qualitative Interview Study. J Acad Nutr Diet. 2022;122(7):1263–1282. doi: 10.1016/j.jand.2022.01.012. [DOI] [PubMed] [Google Scholar]
- 48.Hallsworth K, Dombrowski SU, McPherson S, Anstee QM, Avery L. Using the theoretical domains framework to identify barriers and enabling factors to implementation of guidance for the diagnosis and management of nonalcoholic fatty liver disease: a qualitative study. Transl Behav Med. 2020;10(4):1016–1030. doi: 10.1093/tbm/ibz080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Carrard J, Pandya T, Niederhauser L, Infanger D, Schmidt-Trucksaess A, Kriemler S. Should sports and exercise medicine be taught in the Swiss undergraduate medical curricula? A survey among 1764 Swiss medical students. BMJ Open Sport Exerc Med. 2019;5(1):e000575. doi: 10.1136/bmjsem-2019-000575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lu KD, Cooper D, Dubrowski R, Barwick M, Radom-Aizik S. Exploration of Barriers and Facilitators to Implementing Best Practice in Exercise Medicine in Primary Pediatric Care-Pediatrician Perspectives. Pediatr Exerc Sci. 2021;33(4):162–169. doi: 10.1123/pes.2020-0214. [DOI] [PubMed] [Google Scholar]
- 51.Jang Y, Lee JY, Kim SU, Kim B. A qualitative study of self-management experiences in people with non-alcoholic fatty liver disease. Nurs Open. 2021;8(6):3135–3142. doi: 10.1002/nop2.1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Avery L, Exley C, McPherson S, Trenell MI, Anstee QM, Hallsworth K. Lifestyle Behavior Change in Patients With Nonalcoholic Fatty Liver Disease: A Qualitative Study of Clinical Practice. Clin Gastroenterol Hepatol. 2017;15(12):1968–1971. doi: 10.1016/j.cgh.2017.06.011. [DOI] [PubMed] [Google Scholar]
- 53.Ekkekakis P, Biddle SJH. Extraordinary claims in the literature on high-intensity interval training (HIIT): IV. Is HIIT associated with higher long-term exercise adherence? Psychol Sport Exerc. 2023;64:102295. doi: 10.1016/j.psychsport.2022.102295. [DOI] [PubMed] [Google Scholar]
- 54.Kwan BM, Bryan AD. Affective response to exercise as a component of exercise motivation: Attitudes, norms, self-efficacy, and temporal stability of intentions. Psychol Sport Exerc. 2010;11(1):71–79. doi: 10.1016/j.psychsport.2009.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Thum JS, Parsons G, Whittle T, Astorino TA. High-Intensity Interval Training Elicits Higher Enjoyment than Moderate Intensity Continuous Exercise. PLoS One. 2017;12(1):e0166299. doi: 10.1371/journal.pone.0166299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gerber LH, Weinstein AA, Mehta R, Younossi ZM. Importance of fatigue and its measurement in chronic liver disease. World J Gastroenterol. 2019;25(28):3669–3683. doi: 10.3748/wjg.v25.i28.3669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pugh CJ, Spring VS, Kemp GJ, Richardson P, Shojaee-Moradie F, Umpleby AM, et al. Exercise training reverses endothelial dysfunction in nonalcoholic fatty liver disease. Am J Physiol Heart Circ Physiol. 2014;307(9):H1298–H1306. doi: 10.1152/ajpheart.00306.2014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.